Abstract
While research on homeless adolescents and young adults evidencing substance use disorder is increasing, there is a dearth of information regarding effective interventions, and more research is needed to guide those who serve this population. The current study builds upon prior research showing promising findings of the Community Reinforcement Approach (CRA) (Slesnick, Prestopnik, Meyers, & Glassman, 2007). Homeless adolescents and young adults between the ages of 14 to 20 years were randomized to one of three theoretically distinct interventions: (1) CRA (n = 93), (2) Motivational Enhancement Therapy (MET, n = 86), or (3) Case Management (CM, n = 91). The relative effectiveness of these interventions was evaluated at 3, 6, and 12 months post-baseline. Findings indicated that substance use and associated problems were significantly reduced in all three interventions across time. Several moderating effects were found, especially for sex and history of childhood abuse. Findings show little evidence of superiority or inferiority of the three interventions and suggest that drop-in centers have choices for addressing the range of problems that these adolescents and young adults face.
Keywords: Homeless adolescents and young adults, substance use disorders, treatment outcomes
1. Introduction
Homeless adolescents and young adults are considered one of the most vulnerable populations worldwide with an estimated 100 million globally (UNESCO, 2007), and 500,000 to 2.8 million in the U.S. alone (Bucher, 2008; Cooper, 2006). A multitude of studies document high rates of alcohol and drug use, sexual risk behaviors and physical and mental health vulnerabilities (Robertson & Toro, 1999). Homeless adolescents and young adults frequently report histories of childhood physical and/or sexual abuse (Robertson & Toro, 1999) and are disconnected from family, housing and social services (Gaetz, 2004). The purpose of this study was to identify the most effective intervention for addressing substance use, as well as secondary outcomes including housing, mental health problems, and victimization among three theoretically distinct but empirically-supported interventions: the Community Reinforcement Approach (CRA, Meyers & Smith, 1995), Motivational Enhancement Therapy (MET, Miller & Rollnick, 2013) and case management (CM).
Substance use disorders are common among homeless adolescents and young adults, with studies estimating that 69 to 86 percent meet diagnostic criteria for at least one substance use disorder (Baer, Ginzler, & Peterson, 2003; Kipke, Montogemery, Simon, & Iverson, 1997). In addition to the direct negative effects of substance use, there are significant social, legal and physical health consequences (Edidin, Ganim, Hunter, & Karnik, 2012). For example, substance use is associated with other mental health disorders (Johnson, Whitbeck, & Hoyt, 2005) and increases adolescent’s and young adult’s risk of victimization on the streets (Greene, Ennett, & Ringwalt, 1997; Whitbeck, Hoyt, & Yoder, 1999). Substance use can inhibit one’s exit from homelessness and increases the potential for chronic homelessness into adulthood (Greene et al., 1997; Robertson & Toro, 1999). Overall, treatment for substance use disorders is a priority when intervening with homeless adolescents and young adults, not only because of the high prevalence of substance use disorders in this population, but also because of the multitude of negative consequences associated with it.
Furthermore, the problems experienced by homeless youth are interrelated, and the treatment of substance use problems has been associated with improvements in other affected domains including depressive symptoms, internalizing and externalizing problems, coping and victimization experiences (Slesnick et al., 2007; Williams & Chang, 2000). Despite the challenges experienced by these youth, current research offers limited guidance regarding how to intervene and treat this population (Eddin et al., 2012; Robertson & Toro, 1999). Homeless youth present with challenges not faced by those who are not experiencing homelessness. In particular, they are less connected to familial, institutional or other supports, and rarely enter substance use treatment on a voluntary basis, though they can be engaged in treatment through outreach (Fisk, Rakfeldt, & McCormack, 2006). Because of the range of difficulties, providing substance use treatment for people who are homeless cannot be separated from the larger needs for assistance with housing, employment and income (Kertesz et al., 2007; Milby et al., 2000). For example, recovery outcomes can be enhanced, and social isolation diminished, through the use of advocates who assertively link persons who are homeless to community-based support programs (National Alliance to End Homelessness, 2006).
Recent reviews of the adolescent substance use treatment literature identify several effective individual, group, and family interventions (Tanner-Smith et al., 2013; Waldron & Turner, 2008). Some evidence suggests that family therapy interventions outperform other interventions, but more research supporting this conclusion is needed (Tanner-Smith et al., 2013). Given the range of available effective treatment options, researchers suggest that cost effectiveness (Tanner-Smith et al., 2013) and response to treatment (Waldron & Turner, 2008) should be considered when selecting a treatment. However, as noted, very few intervention studies have been conducted with homeless youth, and those few studies targeted a wide range of outcomes using various interventions. In two recent literature reviews, Altena and colleagues (2010) identified 11intervention studies while Slesnick and colleagues (2009) identified 14 studies. These few studies tested individual, family, group, and street-based interventions focused on substance use, mental health, sexual and HIV risk, and employment.
Identifying effective interventions is also complicated by the fact that subgroups of runaway and homeless adolescents and young adults exist, with different intervention needs among them (Chamberlain & MacKenzie, 2004; Haber & Toro, 2004). That is, presence on the streets is considered a marker of problem severity. Shelter-recruited adolescents tend to be younger, and often have never spent a night on the streets (Robertson & Toro, 1999). Family reunification is the primary goal of runaway shelters, with family therapy a recommended approach (Slesnick, Dashora, Letcher, Erdem, & Serovich, 2009; Teare, Peterson, Furst, & Authier, 1994). In contrast, street-living homeless adolescents and young adults rarely access institutional settings (shelters, foster care) or family for assistance because these systems are no longer perceived to meet their needs (Marshall & Bhugra, 1996). Community-based interventions offered in low-demand settings such as drop-in centers are recommended for street-living adolescents and young adults (Chamberlain & MacKenzie, 2004). Drop-in centers offer youth a bridge from the streets to the mainstream, with few requirements placed upon youth (Slesnick et al., 2008). These centers usually address basic needs and seek to connect youth to more intensive services as trust develops. Promising interventions for street-living adolescents and young adults include case management, brief motivational interviewing, and behavioral interventions (Altena, Brilleslijper-Kater, & Wolf, 2010; Slesnick et al., 2009). Information on the relative performance of these promising interventions can offer evidence supporting intervention options for those seeking to serve this population.
1.1. Interventions
Traditionally, case management has been standard care for those experiencing homelessness (Zerger, 2002). Few studies have examined the effectiveness of case management as a standalone intervention for homeless adolescents and young adults. However, the Substance Abuse and Mental Health Services Administration (SAMHSA) identified brief strengths-based case management (Rapp et al., 2008) as an evidenced-based intervention for substance use. Both Altena and colleagues (2010) and Slesnick and colleagues (2009) note that only one randomized clinical trial has examined the efficacy of case management with homeless adolescents and young adults. Cauce and colleagues (1994) found no significant differences between an intensive and standard case management with both conditions showing reductions in internalizing and externalizing problems, depression, anxiety, substance use, and days spent homeless. Despite the limited research, case management continues to be a common approach used in community programs that serve homeless individuals (Zerger, 2002). However, given that case management does not provide targeted substance use treatment, it was expected to show inferior substance use outcomes to CRA and MET.
Three studies have tested MET with homeless youth (Baer, Garrett, Beadnell, Wells, & Peterson, 2007; Peterson, Baer, Wells, Ginzler, & Garrett, 2006) and shelter-residing youth (Slesnick et al, 2013). Peterson et al. (2006) found that MET had no impact on alcohol or marijuana use, though other illicit drug use was reduced at the one month follow-up in a sample of street-recruited homeless adolescents and young adults. Baer et al. (2007) sought to improve upon the findings of Peterson and colleagues by enhancing engagement strategies. However, few positive outcomes were observed. In contrast, utilizing a sample of substance using runaway adolescents recruited from a runaway shelter, Slesnick et al. (2013) found that substance use reductions were significant for those assigned to MET even to two years post-treatment. Few differences between MET, family systems therapy and the Community Reinforcement Approach were observed; adolescents in MET showed a quicker decline in their substance use but a faster relapse compared with those receiving family therapy. The differences in outcomes may be due to the different samples utilized. That is, Baer and Peterson recruited street-living youth with higher problem severity, while Slesnick and colleagues worked with more stable shelter-recruited adolescents with relatively lower problem severity.
The Community Reinforcement Approach (CRA, Meyers & Smith, 1995) is an operant-based behavioral intervention that has shown great success with homeless adults (Smith, Meyers, & DeLaney, 1998), runaway and homeless youth (Slesnick, Prestopnik, Meyers, & Glassman, 2007; Slesnick et al., 2013) and adolescent marijuana abusers (Godley, et al., 2010). Higgins and colleagues have conducted several trials of CRA plus contingent reinforcement with adults who abuse cocaine (e.g., Higgins et al., 1995, 2000). The CRA counseling portion of their intervention is similar to the CRA counseling provided in the current study, however, a major focus of their intervention is the addition of an incentive program which requires participants to participate in weekly urinalysis screenings in order to earn vouchers. Also, Azrin and colleagues developed a family behavioral therapy intervention using operant-based procedures (Azrin et al., 2001). Similar to CRA used in the current study, their behavioral intervention helps youth identify aspects of their environment that reinforce negative behaviors, and helps youth and families develop alternative reinforcing behaviors and plans to avoid negative environmental situations. Unlike CRA used in the current study, their intervention focuses largely on the youth's family and also utilizes contingency management.
Research indicates that outcomes of treatment for substance use disorders are moderated by age, sex, ethnicity and history of childhood abuse. For example, Winters (1999) suggests that substance use treatments for adolescents need to be aware of the influence of age on treatment. When sex differences are observed on treatment outcomes, females tend to have better outcomes compared to males (Greenfield et al., 2007). While African Americans tend to report lower treatment completion compared to Whites (Milligan et al., 2004), Slesnick and colleagues (2013) found that among runaway adolescents, minority youth reported more reductions in substance use, but also relapsed sooner compared to White youth. Although some studies report similar treatment outcomes among those who report childhood abuse compared to those who do not (Oviedo-Joeke et al., 2011; Slesnick, Bartle-Haring, & Gangamma, 2006), other studies report that individuals with a childhood abuse history have less positive treatment outcomes compared to individuals without an abuse history (Sacks et al., 2008).
1.2. Current Study
The current study compared treatment outcomes for homeless youth evidencing substance use disorder assigned to CM, CRA or MET provided through a local drop-in center. It was hypothesized that adolescents and young adults receiving each treatment would show significant improvements in the primary outcome, alcohol and drug use, as well as the secondary outcomes including depressive symptoms, internalizing/externalizing problems, victimization, homelessness, and coping from baseline to the 12-month follow-up. This study follows the stage model of intervention development (Carroll & Rounsaville, 2003; Rounsaville, Carroll, & Onken, 2001). In a prior Stage 1 trial (Slesnick et al., 2007), the substance use treatment, CRA, was tested with homeless adolescents and young adults and was compared to treatment as usual through a drop-in center. Overall, CRA evidenced superior outcomes to drop-in center services alone across a range of outcomes including substance use, depressive symptoms and homelessness (Slesnick et al., 2007). The current study is a Stage II trial in which the promising CRA intervention was compared to other viable, or empirically supported, interventions (Brigham, Feaster, Wakim, & Dempsey, 2009; Carroll & Rounsaville, 2003). Though comparison to services as usual would have been a reasonable control condition, since CRA already showed superior outcomes to services as usual, the question of interest was how CRA would compare to other promising interventions. Overall, it was expected that those receiving CRA would exhibit more improvements in all outcome variables than the other two treatments during the 12-month period. In addition, research suggests that substance use outcomes may be moderated by age, sex, ethnicity and a history of childhood abuse (Greenfield et al., 2007; Milligan et al., 2004; Sacks et al., 2008; Slesnick et al., 2013), and these moderators were tested in the current study. Differences between CRA and the other two treatments on the outcomes of interest were expected to be particularly pronounced for older youth, females, Whites, and youth without a history of child abuse.
2. Methods
2.1. Participants
Homeless adolescents and young adults (n = 270) were recruited from the only drop-in center serving homeless adolescents and young adults in Central Ohio. Eligible participants met the criteria of homelessness as defined by the McKinney-Vento Act (2002) as those who lack a fixed, regular, and adequate nighttime residence; lives in a welfare hotel, or place without regular sleeping accommodations; or lives in a shared residence with other persons due to the loss of one’s housing or economic hardship. Of those approached for participation in the study, 34% were eligible and 75% of those agreed to participate. Eligible participants were recruited between October 2006 to December 2009, were between the ages of 14 to 20 years, and met Diagnostic and Statistical Manual for Mental Disorders-IV (American Psychiatric Association, 2000) for abuse or dependence for Psychoactive Substance Use or Alcohol Disorder, as assessed by the Computerized Diagnostic Interview Schedule (CDIS, Shaffer, 1992). All but four participants (one 14-year old, three 15-year olds) were between the ages of 16-20 years. A summary of the demographic characteristics for the current sample is presented in the Table 1.
Table 1.
Demographic characteristics of the sample
| MET (n = 86) | CRA (n = 93) | CM (n = 91) | Total (n = 270) | |
|---|---|---|---|---|
| Sex [n(%)] | ||||
| Female | 38 (44.19%) | 43 (46.24%) | 47 (51.65%) | 128 (47.41%) |
| Sexual orientation [n(%)] | ||||
| Straight | 70 (81.40%) | 72 (77.42%) | 67 (73.62%) | 209 (77.41%) |
| Gay/Lesbian | 4 (4.65%) | 6 (6.45%) | 5 (5.49%) | 15 (5.56%) |
| Bisexual | 6 (6.98%) | 13 (13.98%) | 13 (14.29%) | 32 (11.85%) |
| Transgendered | 0 | 0 | 1 (1.10%) | 1 (0.37%) |
| Unsure | 3 (3.49%) | 0 | 0 | 3 (1.11%) |
| Race [n(%)] | ||||
| African American | 54 (62. 79%) | 63 (67.74%) | 60 (65.93%) | 177 (65.56%) |
| White, not Hispanic | 17 (19.77%) | 16 (17.20%) | 20 (21.98%) | 53 (19.6%) |
| Hispanic | 3 (3.49%) | 0 | 3 (3.30%) | 6 (2.22%) |
| Native American | 1 (1.16%) | 0 | 1 (1.10%) | 2 (0.74%) |
| Asian American | 0 | 1 (1.08%) | 0 | 1 (0.37%) |
| Other | 11 (12.79%) | 13 (13.98%) | 7 (7.69%) | 31 (11.48%) |
| Age [Mean (SD)] | 18.69 (1.32) | 18.70 (1.34) | 18.84 (1.11) | 18.74 (1.26) |
| Age at first time homelessness [Mean (SD)] | 16.15 (2.61) | 15.81 (3.54) | 15.72 (4.01) | 15.89 (3.44) |
| Number of days currently without shelter | 87.33 (208.32) | 49.02 (124.93) | 71.89 (185.26) | 69.20 (175.94) |
| [Mean (SD)] | ||||
| First time using drugs under 15 [n(%)] | 66 (76.74%) | 68 (73.12%) | 70 (76.92%) | 204 (75.56%) |
| History of physical or sexual abuse [n(%)] | ||||
| Physical abuse | 36 (41.86%) | 34 (36.56%) | 48 (52.75%) | 118 (43.70%) |
| Sexual abuse | 21 (24.42%) | 25 (26.88%) | 35 (38.46%) | 81 (30.00%) |
2.2. Procedure
A research assistant (RA) engaged and screened homeless youth at the drop-in center to determine basic eligibility for the study. After determining eligibility and interest, written informed consent was obtained from young adults who were 18 years or older and assent was obtained for youth under 18 years prior to beginning the assessment battery. Consent from parents/guardians was not required given high rates of abuse and neglect among homeless minors, and because street living minors often do not want, or know how, to contact their guardian. Requiring consent from parents would result in many minors not receiving potentially helpful intervention, and would skew research findings towards those youth with more stable family environments (Meade & Slesnick, 2002). And, in fact, the Code of Federal regulations, part 46.408(c) states that “In addition to the provisions for waiver contained in §46.116 of Subpart A, if the IRB determines that a research protocol is designed for conditions or for a subject population for which parental or guardian permission is not a reasonable requirement to protect the subjects (for example, neglected or abused children), it may waive the consent requirements in Subpart A of this part and paragraph (b) of this section.” If it was suggested that child abuse or neglect had occurred or currently takes place, Public Children’s Services Agency (PCSA) of the State of Ohio was notified. In order to mitigate potential negative effects on youth (e.g., breakdown of trust) the staff member discussed the purpose (legal and clinical), of reporting to PCSA, and addressed the youths’ concerns and fears. Youth were informed that if staff became of aware of their intent to seriously harm another person, staff would need to report the information to both the police and the intended victim. In the case of suicide, if the client was acutely suicidal, they were secured an evaluation at a local hospital that provides twenty-four hour mental health crisis intervention, stabilization and assessment for Franklin County, Ohio residents.
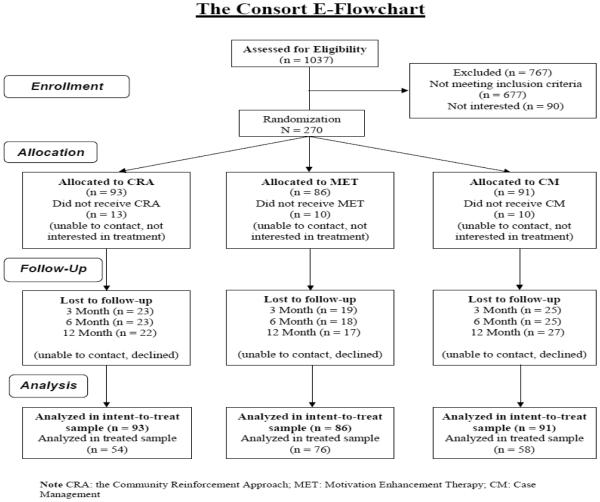
Following the baseline assessment, a computerized randomization program was used to assign participants to CRA (n = 93, 34.44%), MET (n = 86, 31.85%), or Case Management (CM) (n = 91, 33.70%). MET included two 1-hour sessions, while CRA and CM had twelve 1-hour sessions. Each intervention condition also included two 1-hour HIV prevention sessions. Therefore, the total number of sessions was 4 for MET, and 14 for CRA and CM. All sessions were completed within 6 months of the baseline assessment interview. In each condition, therapists and case managers were available 24 hours for crises. Follow-up assessments were conducted at 3, 6 and 12 months post-baseline. Participants were reimbursed with a $25 gift card at completion of the baseline assessment battery, a $50 gift card for at each follow-up assessment, and a $5 gift card for each session attended. All research procedures were approved by the Institutional Review Board at The Ohio State University. The study design and flow of participants are presented in Figure 1.
Figure 1.
The CONSORT Flowchart
2.3. Treatment conditions
CRA is an operant-based therapy with the goal to help individuals restructure their environment so that drug use or other maladaptive behaviors are no longer reinforced and other positive behaviors are reinforced. CRA treatment procedures are detailed in a book written by the developers (Meyers & Smith, 1995). Therapists follow a standard set of core procedures and a menu of optional treatment modules matched to clients’ needs (Meyers & Smith, 1995). The core session topics include (1) a functional analysis of using behaviors, (2) refusal skills training, and (3) relapse prevention (4) job skills, (5) social skills training including communication and problem-solving skills, (6) social and recreational counseling, (7) anger management and affect regulation. Each area of focus is determined based upon the goals of counseling, and intervention components are repeated until the participant and therapist agree that the goal has been achieved. Additional optional modules are included based upon each clients’ needs and strengths. Because the intervention is tailored to the unique needs and environmental context of individual clients, it is easily adapted to the multiple and various circumstances of those experiencing homelessness (e.g., limited recreational/social reinforcers).
Motivational Interviewing (MI; Miller & Rollnick, 2013) assumes that the responsibility and capability for change lie within the client, and need to be evoked (rather than created or instilled). Four principles guide the practice of MI: express accurate empathy, develop discrepancy, roll with resistance and support self-efficacy. An adaptation of MI that has been well-tested, both with adults and with adolescents, is motivational enhancement therapy (MET) which includes feedback. Session 1 begins with open-ended MI, to establish therapeutic rapport and elicit client change talk in regards to their substance use. Next, the client is given specific feedback about their substance use from the baseline assessment, within an MI counseling style. This period of feedback often continues into Session 2. The therapist continues to focus on enhancing intrinsic motivation for change, transitioning as appropriate into the negotiation of a change plan and evoking commitment to the plan. Sessions 1 and 2 directly paralleled Sessions 1 and 2 of the MET manual developed for Project MATCH (Miller, Zweben, DiClemente, & Rychtarik, R. G., 1992). The MATCH manual required only minor modifications which was completed by Joseph “Bo” Miller in consultation with Dr. William R. Miller and the first author. Although the frequency of MET sessions was lower than the other treatments, the duration of the treatment was matched with the other, longer treatments so that sessions were spaced over the course of the treatment period.
Using a Strengths-Based Case Management (CM) model (Rapp et al., 2008), case managers seek to link participants to resources within the community. The initial case management meeting provides an opportunity to gather information. The case manager reviews each of six general areas with the participant to gather a history and picture of the current situation: (1) housing needs; (2) health/mental health care, including alcohol/drug use intervention; (3) food; (4) legal issues, (5) employment and (6) education. Consistent with a Strengths-Based CM Approach, the case manager takes responsibility for securing needed services for the youth and remains a support for the youth as he/she traverses the system of care. The strengths-based approach also includes the following features: 1) dual focus on client and environment, 2) use of paraprofessional personnel, 3) a focus on client strengths rather than deficits, 4) a high degree of responsibility given to the client in directing and influencing the intervention that he/she receives from the system and the outreach worker. Once this review is complete, an initial intervention plan is developed with specific goals and objectives. A manual and goal development sheets were developed by the first author. Service is not restricted to the office and includes transportation of clients to appointments, interviews, and related activities.
2.4. Therapist training and fidelity
Four therapists were trained in MET, four in CRA and four case managers in CM, by that intervention’s clinical supervisor. Training included manual review, didactic training and extensive role play over a period of two days, as well as weekly supervision with audiotape review with the intervention supervisor throughout the study. Therapists included master’s level counselors, marriage and family therapists or social workers. Case managers were bachelor’s level social work students, and counseling was not provided. CM sessions were often conducted in the field and were not recorded because it was not considered feasible. However, CM was closely supervised during weekly supervision with the use of checklists documenting the number of service needs in each of several domains identified by individual clients. Therefore, fidelity coding was only performed on CRA and MET.
Fifty out of 457 (11%) CRA sessions and thirty-five out of 145 (24 %) MET sessions were coded for adherence and competence. These tapes were randomly selected, thus not all therapists had an equal number of tapes coded. Adherence was operationalized as the average number of procedures used during a session with the use of more procedures indicating better adherence. The CRA procedures included: 1) linking positive rewards to non-substance using/non-problematic behavior, 2) linking negative consequences to substance using/problematic behavior, 3) examining the triggers of substance use/problematic behaviors, 4) provide positive reinforcement/support of non-using positive behavior, 5) teaching skills supporting positive behaviors, 6) communicating in an upbeat and optimistic style, 7) explaining how substance using/problematic behavior leads to problems, 8) identifying and reinforcing prosocial and recreational activities to compete with substance using/problematic behavior, and 9) identifying and discussing the function of drug using/problematic behavior.
The MET procedures included: 1) providing objective, unbiased information about client’s substance use, 2) avoiding power struggles/rolling with resistance, 3) listening to client’s perspective on his/her substance use, 4) demonstrating confidence in the client’s ability to make changes, 5) examining pros and cons of substance use, 6) demonstrating interest of client’s goals and values, 7) using logic to demonstrate the seriousness of substance use, 8) not allowing the client to minimize his/her drug use, 9) assuming an expert role in the treatment process, and 10) encouraging the client to contribute ideas about how to change the problem. In order to assess competency, the CRA and MET procedures were rated on a scale from 1 (very poor) to 7 (exceptional).
The average number of procedures used was 5.60 during a CRA session (SD = 2.18, range 2.00 – 9.00) out of 9 potential procedures, and 10 during a MET session (SD = 0) out of 10 potential procedures. That is, good therapist adherence was found among CRA sessions while excellent adherence was found among MET sessions. Therapist competence was 5.21 on average for CRA sessions (SD = 0.72, range 3.66 – 7.00) and 5.39 for MET sessions (SD = 0.38, range 4.22 – 6.00), both of which were in the "done well" range. Inter-rater reliability for 13 double-coded CRA tapes for procedure occurrence (adherence) was Kappa = 0.72, while the rater reliability of the CRA procedure rating (competence) was ICC = 0.81. Inter-rater reliability for 19 double-coded MET tapes for procedure occurrence (adherence) was Kappa = 0.98, while the rater reliability of the MET procedure rating (competence) was ICC = 0.77.
2.5. Measures
Demographic variables
A demographic questionnaire was administered at baseline. Several variables were dummy coded including ethnicity (1 representing African Americans, and 0 representing other ethnicities), sex (1 representing females and 0 representing males) and childhood physical and sexual abuse history (1 indicating the childhood abuse, and 0 indicating no abuse history).
Primary outcomes (substance use)
Quantity and frequency of alcohol and drug use was measured by the Form90 developed for the NIAAA funded Project MATCH (Miller, 1996), which combines the timeline follow-back method (Sobell & Sobell, 1992) and grid averaging. Substance use is queried for the period of 90 days prior to the last use of alcohol or illicit drugs. Kappa’s for different drug classes range from 0.74 to 1.0 (Tonigan, Miller, & Brown, 1997; Westerberg, Tonigan, & Miller, 1998) and the questionnaire has shown good reliability and validity with substance abusing runaway adolescents (Slesnick, & Tonigan, 2004). As further validation of self-reported drug use, urine toxicology screens were collected at baseline, 6 and 12 months post-baseline.
Secondary outcomes
As a measure of depressive symptoms, the Beck Depression Inventory-II (BDI-II; Beck, Steer, & Brown, 1996) is composed of 21 items with total scores ranging from 0 to 63. Higher scores indicate higher levels of depressive symptoms. Excellent internal reliability was observed in the current study, with reliabilities ranging from 0.94 and 0.95.
Internalizing and externalizing problems were assessed using the Youth Self-Report of the Child Behavior Checklist (YSR; Achenbach, 1991). Items are rated using a 3-point Likert scale, with higher scores indicating more problem behaviors. In the current study, the internal consistency of the internalizing scale ranged from 0.90 to 0.93 across different time points, and from 0.90 to 0.93 for the externalizing scale.
The adolescent version of the Coping Inventory for Stressful Situations (CISS; Endler & Parker, 1990) was used to measure coping. The three factor analytically-derived subscales are: (1) task-oriented coping, (2) emotion-oriented coping, and (3) avoidance-oriented coping. The scale is a valid multidimensional coping measure, and has shown adequate construct validity with adolescent and clinical populations (Endler & Parker, 1990). In the current study, reliabilities ranged from 0.94 to 0.95 for the task-oriented subscale, from 0.91 to 0.93 for the emotion-oriented scale, and from 0.89 to 0.90 for the avoidance-oriented scale.
In order to estimate victimization experiences, participants were asked to report if they have ever been assaulted or physically attacked, robbed, burglarized, raped, or sexually assaulted (other than rape) during the last 3 months (for baseline, 3-month and 6-month follow-ups) or the last 6 months (for 12-month follow-up), with “no” coded as 0 and “yes” coded as 1. Homelessness was estimated as the percentage of homeless days (“Total number of days living homeless, or with others, no rent”) during the past 90 days on the Form 90.
2.6. Analytic strategies
This study used an intent to treat (ITT) design which consisted of the entire sample of 270 participants. Outcomes for the treated sample were also examined, and consisted of 188 participants who attended 25% or more of the total possible treatment sessions (4 for CRA and CM, 1 for MET). A 25% treatment completion rate for CRA and CM is consistent with the Washington Circle Performance for Outpatient Treatment’s treatment engagement definition of at least two additional sessions after the initial treatment session (Garrick, Lee, Horgan, Acevedo, & Washington Public Sector Workgroup, 2009). Additionally, others have similarly chosen a 1-6 session cut-offs for the treated sample (Waldron, Slesnick, Brody, Turner, & Peterson, 2001; Joanning et al., 1992; Linehan, Schmidt, Craft, Kanter, & Comtois, 1999; Manuel et al., 2012; Slesnick & Prestopnik, 2009). Hierarchical linear modeling analysis was conducted using the HLM7 software (HLM; Raudenbush, Bryk, & Congdon, 2011) to compare the relative treatment effects on the primary (alcohol and drug use) and secondary outcomes (depressive symptoms, internalizing/externalizing, task-, emotion-, and avoidance-oriented coping, victimization, and homelessness) over time, using CM as the reference group. Treatment attendance (the number of sessions attended divided by the maximum number of sessions allowed for that specific treatment condition) was included as a predictor of the overall time effect, in order to control for the dosage of treatment. Previous research has linked higher treatment attendance with better outcomes (e.g., Dale et al., 2011; Reardon, Cukrowicz, Reeves, & Joiner, 2002; Schumacher et al., 1995). However, some studies report that treatment attendance is not a consistent predictor of treatment outcome (e.g., Collins, Malone, & Larimer, 2012; Slesnick, Erdem, Bartle-Haring, & Brigham, 2013). Since MET has a much smaller dosage compared to CRA/CM, the percentage of sessions attended was used to represent treatment attendance. Demographic variables, including age, sex, ethnicity, and history of physical and sexual abuse, were entered as predictors of the linear time effect in the preliminary analyses in order to test possible moderating effects. Only the variables exhibiting significant effects in the preliminary analyses were kept in the final model. Effect sizes (Cohen’s d; Cohen, 1988; Lipsey & Wilson, 2001) and the 95% Confidence Interval (CI) of primary outcomes were calculated for each treatment group using the baseline and the 6-month data.
And finally, clinical significance of the pre-to-post changes was analyzed for all outcome variables. Clinical significance, as separate from statistical significance, is defined as the extent to which therapy moves someone outside the range of the dysfunctional population (Jacobson, Follette, & Revenstorf, 1994). A reliable change index (RC) determines whether the magnitude of change for a client is statistically reliable. In this study, an RC (Jacobson & Truax, 1991) was calculated for each participant, using the formula [(XPost-treatment at 6months – XPre-treatment) / Sdiff]. As recommended by Jacobson and Truax (1991), RC > 1.96 was operationalized as the threshold for improvement in clinical outcomes, whereas 1.96 ≤ RC ≥ 1.96 referred to some change that was not clinically significant. Finally, RC < 1.96 was defined as deterioration.
3. Results
3.1. Preliminary Analysis
Data screening for randomization
Participants in the three treatment conditions did not differ in age, sex, ethnicity or childhood history of sexual abuse or physical abuse (p’s > 0.05). The majority of participants were between the ages of 16-20 years (98%). Further, the sample was too small to test by age group, with a limited number of 16 year olds (n = 14) and 17 year olds (n= 25). In addition, there was no significant difference in baseline frequency of alcohol use, quantity of alcohol use, or frequency of drug use (p’s > 0.05) across treatment conditions.
Convergent validity of self-report and urine toxicology
The details of the urine screen results are presented in Table 2. Urine screens were compared to the Form 90 data at baseline, the 6 and 12 month follow-ups. Both urine screens and the Form 90 data showed that the most commonly used drug was marijuana, followed by alcohol, opiates and cocaine. Overall, the self-reported Form 90 data converged with urine screens. Only a very small number of participants who reported no drug use on the Form 90 had positive drug screens (13 at baseline, 13 at 6-month and 7 at 12-month follow-up), and their Form 90 data were excluded from the analyses.
Table 2.
Urine screen test results
| Baseline | 6-month Follow-up | 12-month Follow- up |
|
|---|---|---|---|
| Number of available urine screen test results |
242 | 128 | 99 |
| Positive for: | n (%) | n (%) | n (%) |
| Amphetamines | 3 (1.2) | 3 (2.3) | 1 (1.0) |
| Bezoylecgonine | 7 (2.9) | 2 (1.6) | 5 (5.1) |
| Methamphetamines | 1 (0.4) | 1 (0.8) | 2 (2.0) |
| Morphine | 9 (3.7) | 3 (2.3) | 1 (1.0) |
| Phencyclidine | 0 | 1 (0.8) | 0 |
| Tetrahydrocannabinol | 203 (83.9) | 97 (75.2) | 76 (77.6) |
Follow-up attrition
In the current clinical trial, the follow-up rates at 3, 6 and 12 months were 75%, 76% and 76%, respectively. Chi-square test showed that attrition did not differ across treatment conditions (p > 0.05). Independent-sample t tests showed no differences among follow-up completers and drop-outs in terms of their primary outcomes (p’s > 0.05). Little’s MCAR test was not significant either [Χ2(3961) = 4030.80, p > 0.05]. Therefore, the current data were assumed to be missing completely at random.
Distributional characteristics of primary and secondary outcomes and differences between the ITT and the treated samples
Percent days of alcohol use and average standard ethanol content (SECs) were skewed (skewness ranged from 2.43 to 5.01). After transformation using natural logs (Ln), the skewness of these variables fell within the normal range (under 1.96). The ITT sample and the treated sample did not differ on age, sex, ethnicity, or the distribution of physical or sexual abuse (all p’s > 0.05). Independent samples t-tests did not show significant differences between the two samples among primary and secondary outcomes at baseline (all p’s > 0.05).
Treatment attendance and therapist effects
Because the three treatments had different maximum number of sessions (14 for CRA and CM, 4 for MET), treatment attendance was represented using the percentage of sessions attended divided by the maximum number of sessions allowed (range from 0 to 100%). In the ITT sample, the mean session attendance was 73% for MET (2.9 sessions), 42% for CRA (5.8 sessions), and 47% for CM (6.5 sessions). Among those assigned to CM, only a small number of participants reported receiving therapy for substance use or emotional problems at the 3-month (n = 9), 6-month (n=7) and 12-month (n = 6) follow-up assessment. Therefore, the small percentage of participants accessing outside treatment was considered trivial, and the impact was not accounted for in the analyses. The average treatment attendance in MET was significantly higher than the attendance in CRA (mean difference = 0.33, SE = 0.05, p < 0.001), and in CM (mean difference = 0.26, SE = 0.05, p < 0.001). There was no significant difference between CRA and CM. The same pattern was also found in the treated sample. Therefore, treatment attendance was controlled when analyzing longitudinal changes in the outcome variables. Univariate analysis was used to analyze the therapist effects. Frequency of alcohol and drug use was used as the dependent variable, therapist was used as the independent variable, and age, sex, ethnicity, treatment condition and baseline level were control variables. The analysis was conducted with the 3- and the 6-month follow-up respectively. Results showed no significant therapist effects on alcohol and drug use at the 3- and the 6-month follow-ups (all p’s > 0.05). In other words, there was no evidence suggesting that one therapist had better client outcomes in alcohol and drug use than other therapists in the same treatment condition at the 3- and the 6-month follow-ups.
3.2. Analyses with the ITT sample
Primary outcomes
In the first step, baseline demographic differences were controlled and only treatment-related factors were entered in the Level-2 model, so that the main effect of treatment could be analyzed. Significant reductions were found in frequency of alcohol use [βCM = −0.11, SE= 0.04, t(260) = −2.81, p < 0.01; βMET = −0.16, SE = 0.04, t(260) = −3.91, p < 0.001; βCRA = −0.15, SE = 0.04, t(260) = −3.72, p < 0.001], SECs [βCM = −0.09, SE= 0.03, t(260) = −3.63, p < 0.001; βMET = −0.11, SE = 0.02, t(260) = −4.24, p < 0.001; βCRA = −0.09, SE= 0.02, t(260) = −3.70, p < 0.001], and frequency of drug use [βCM = −2.92, SE = 1.26, t(260) = −2.31, p < 0.05; βMET = −2.70, SE = 1.30, t(260) = −2.08, p < 0.05; βCRA = −4.94, SE = 1.22, t(260) = −4.05, p < 0.001] in each treatment condition. There was no significant difference between treatment conditions (p’s > 0.05). In other words, the three treatment conditions exhibited reductions among primary outcomes equivalently. In addition, all three treatments exhibited medium to high effect sizes (ds ranged from −0.29 to −0.71) on primary outcomes from baseline to the 6-month follow-up (see Table 3).
Table 3.
Means, standard deviations, and effect sizes of the outcome variables
| Variables | n | MET | n | CRA | n | CM |
|---|---|---|---|---|---|---|
| Mean (SD) | Mean (SD) | Mean (SD) | ||||
|
Percent days of any drug use
except tobacco and alcohol |
||||||
| Baseline | 81 | 68.36 (36.20) | 89 | 58.76 (39.34) | 87 | 55.47 (34.67) |
| 3-m FU | 66 | 45.67 (43.24) | 70 | 53.60 (40.76) | 66 | 49.38 (40.66) |
| 6-m FU | 62 | 48.36 (40.85) | 64 | 41.20 (39.10) | 63 | 43.92 (40.73) |
| 12-m FU | 67 | 49.21 (40.97) | 69 | 40.17 (39.87) | 60 | 46.30 (38.86) |
| Percent days of alcohol use* | ||||||
| Baseline | 81 | 16.70 (23.92) | 89 | 15.11 (23.45) | 87 | 12.42 (18.36) |
| 3-m FU | 66 | 8.50 (14.07) | 70 | 10.36 (15.65) | 66 | 10.13 (18.38) |
| 6-m FU | 62 | 6.23 (14.93) | 64 | 8.80 (18.27) | 63 | 11.88 (21.66) |
| 12-m FU | 67 | 8.94 (18.41) | 69 | 6.66 (11.82) | 60 | 9.37 (18.58) |
| Average SEC* | ||||||
| Baseline | 81 | 3.65 (6.26) | 89 | 4.05 (7.53) | 87 | 3.03 (6.18) |
| 3-m FU | 66 | 2.76 (5.26) | 70 | 2.70 (5.40) | 65 | 2.78 (4.54) |
| 6-m FU | 62 | 1.61 (2.32) | 64 | 1.69 (2.31) | 63 | 1.41 (2.98) |
| 12-m FU | 67 | 1.65 (3.24) | 69 | 1.89 (3.91) | 60 | 1.78 (2.82) |
| BDI-II total score | ||||||
| Baseline | 72 | 15.51 (13.06) | 78 | 15.88 (14.65) | 82 | 14.53 (12.64) |
| 3-m FU | 56 | 10.95 (12.68) | 61 | 15.18 (15.05) | 53 | 9.69 (9.20) |
| 6-m FU | 61 | 8.52 (10.07) | 61 | 11.95 (14.34) | 54 | 9.72 (9.77) |
| 12-m FU | 62 | 7.96 (10.46) | 62 | 12.74 (12.63) | 56 | 8.42 (11.11) |
| YSR Internalizing | ||||||
| Baseline | 86 | 18.25 (11.24) | 89 | 18.04 (13.06) | 90 | 18.39 (11.94) |
| 3-m FU | 64 | 16.30 (11.40) | 70 | 18.45 (13.39) | 64 | 15.24 (10.66) |
| 6-m FU | 68 | 13.38 (10.16) | 68 | 17.28 (12.34) | 65 | 14.24 (10.50) |
| 12-m FU | 68 | 17.92 (11.79) | 70 | 17.19 (12.37) | 64 | 15.39 (10.78) |
| YSR Externalizing | ||||||
| Baseline | 86 | 15.16 (8.57) | 89 | 15.13 (10.75) | 90 | 16.33 (10.59) |
| 3-m FU | 65 | 15.20 (10.27) | 70 | 14.83 (10.62) | 64 | 13.70 (9.26) |
| 6-m FU | 68 | 12.10 (9.56) | 68 | 14.35 (10.51) | 65 | 13.14 (9.30) |
| 12-m FU | 68 | 16.99 (10.18) | 70 | 13.76 (9.79) | 64 | 13.37 (9.76) |
|
CISS Task-oriented
Coping |
||||||
| Baseline | 84 | 52.99 (15.78) | 88 | 51.47 (15.77) | 86 | 53.21 (13.86) |
| 3-m FU | 61 | 53.51 (15.77) | 66 | 50.58 (17.50) | 62 | 54.10 (13.88) |
| 6-m FU | 66 | 54.27 (15.32) | 64 | 50.72 (17.30) | 62 | 53.08 (13.52) |
| 12-m FU | 64 | 55.86 (12.22) | 70 | 53.04 (16.04) | 58 | 54.69 (15.51) |
| CISS Emotion-oriented Coping | ||||||
| Baseline | 82 | 45.78 (15.43) | 85 | 45.88 (15.71) | 87 | 44.78 (13.69) |
| 3-m FU | 60 | 44.63 (15.18) | 65 | 42.65 (16.39) | 61 | 44.79 (13.44) |
| 6-m FU | 64 | 42.77 (14.76) | 64 | 41.98 (16.46) | 61 | 40.44 (12.40) |
| 12-m FU | 65 | 45.42 (13.21) | 64 | 44.80 (14.61) | 56 | 42.27 (13.33) |
|
CISS Avoidance-oriented
Coping |
||||||
| Baseline | 83 | 49.96 (14.30) | 87 | 48.28 (14.65) | 87 | 50.63 (11.86) |
| 3-m FU | 62 | 51.76 (14.44) | 68 | 49.32 (16.01) | 62 | 52.24 (11.40) |
| 6-m FU | 65 | 51.22 (13.71) | 65 | 46.89 (15.32) | 60 | 49.65 (12.28) |
| 12-m FU | 64 | 52.08 (10.83) | 66 | 50.23 (14.07) | 60 | 50.35 (13.48) |
| Percentage of homeless days | ||||||
| Baseline | 86 | 68.68 (38.39) | 93 | 65.23 (19.05) | 91 | 60.84 (38.21) |
| 3-m FU | 66 | 45.61 (45.57) | 70 | 48.33 (44.54) | 66 | 46.34 (44.15) |
| 6-m FU | 68 | 23.41 (36.52) | 69 | 37.44 (43.01) | 65 | 27.01 (39.19) |
| 12-m FU | 69 | 21.89 (35.31) | 70 | 20.85 (34.95) | 64 | 20.51 (35.13) |
| Victimization experience [n(%)] | ||||||
| Baseline | ||||||
| Yes | 24 (27.91%) | 29 (31.18%) | 33 (36.26%) | |||
| No | 58 (67.44%) | 58 (62.37%) | 51 (56.04%) | |||
| 3-m FU | ||||||
| Yes | 20 (23.26%) | 23 (24.73%) | 22 (24.18%) | |||
| No | 46 (53.49%) | 47 (50.54%) | 43 (47.25%) | |||
| 6-m FU | ||||||
| Yes | 16 (18.60%) | 15 (16.13%) | 15 (16.48%) | |||
| No | 52 (60.47%) | 53 (56.99%) | 50 (54.95%) | |||
| 12-m FU | ||||||
| Yes | 18 (20.93%) | 15 (16.13%) | 16 (17.58%) | |||
| No | 50 (58.14%) | 54 (58.06%) | 48 (52.75%) | |||
|
| ||||||
| Effect size | d [95% CI] | d [95% CI] | d [95% CI] | |||
|
| ||||||
|
Percent days of any drug use
except tobacco and alcohol |
−0.52 [−0.86, −0.19] | −0.45 [−0.77, −0.12] | −0.31 [−0.64, 0.02] | |||
| Percent days of alcohol use* | −0.71 [−1.05, −0.36] | −0.42 [−0.74, −0.09] | −0.29 [−0.61, 0.04] | |||
| Average SEC* | −0.45 [−0.78, −0.11] | −0.49 [−0.81, −0.16] | −0.57 [−0.90, −0.23] | |||
Means and SDs from raw scores were presented in the Table 3 but ln-transformed scores were used in the HLM analyses
In the second step, demographic variables were entered as the predictors of the linear time effects. Sex and a history of physical abuse were found to moderate the trend of the frequency of alcohol and drug use (see Table 4). Specifically, females exhibited significantly more reductions in the frequency of alcohol use [β = −0.12, SE = 0.04, t(259) = −2.74, p < 0.01] than males. Moreover, those with physical abuse histories showed fewer reductions in the frequency of drug use than those without a history of physical abuse [β = 3.17, SE = 1.35, t(258) = 2.35, p < 0.05].
Table 4.
Results for the multilevel modeling analysis of all outcome variables using intent-to-treat sample
| Frequency of alcohol use | SEC | Frequency of drug use | BDI-II | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
| ||||||||||||
| Fixed Effect | b | SE | p-value | b | SE | p-value | b | SE | p-value | b | SE | p-value |
| For Intercept | ||||||||||||
| Intercept | 1.62*** | 0.09 | <0.001 | 0.99*** | 0.05 | <0.001 | 51.33*** | 3.52 | <0.001 | 9.72*** | 1.24 | <0.001 |
| Sex | 2.96 | 1.60 | 0.07 | |||||||||
| Ethnicity | 8.64*b | 4.09 | 0.04 | |||||||||
| Age | 0.14** | 0.05 | <0.01 | 2.02*** | 0.62 | 0.001 | ||||||
| Sexual abuse | 1.99 | 1.46 | 0.17 | |||||||||
| Physical abuse | 0.37** | 0.12 | <0.01 | 6.32*** | 1.59 | <0.001 | ||||||
| For Time slope | ||||||||||||
| Intercept | −0.04 | 0.05 | 0.37 | −0.09*** | 0.02 | <0.001 | −2.94 | 1.62 | 0.07 | −0.49 | 0.47 | 0.30 |
| Treatment attendance | 0.05a | 0.06 | 0.46 | 0.08* | 0.04 | 0.03 | −1.56 | 1.96 | 0.43 | −0.11 | 0.53 | 0.83 |
| MET | −0.07 | 0.06 | 0.21 | −0.02 | 0.03 | 0.58 | 0.10 | 1.71 | 0.95 | −0.16 | 0.46 | 0.72 |
| CRA | −0.05 | 0.05 | 0.38 | 0.001 | 0.03 | 0.97 | 1.94a | 1.66 | 0.24 | 0.55 | 0.45 | 0.22 |
| Sex | −0.12** | 0.04 | <0.01 | −2.57a | 1.96 | 0.06 | −1.13*b | 0.46 | 0.01 | |||
| Ethnicity | ||||||||||||
| Age | −0.39*b | 0.18 | 0.03 | |||||||||
| Sexual abuse | ||||||||||||
| Physical abuse | 3.17* | 1.35 | 0.02 | −1.18* | 0.45 | 0.01 | ||||||
|
| ||||||||||||
| Random Effect | ||||||||||||
|
| ||||||||||||
| Intercept variance | 0.68*** | 0.31*** | 614.17*** | 96.90*** | ||||||||
| Linear slope variance | 0.01* | 0.02** | 13.39* | 1.64* | ||||||||
| Level-1 residual variance | 1.02 | 0.39 | 855.60 | 64.96 | ||||||||
| Estimated parameters | 12 | 9 | 12 | 16 | ||||||||
| Deviance statistic | 2646.35 | 1844.25 | 8253.23 | 5627.07 | ||||||||
| df | 6 | 3 | 6 | 10 | ||||||||
| Χ2test | 28.42*** | 4.57 | 14.97* | 41.07*** | ||||||||
|
| ||||||||||||
| Fixed Effect | YSR Internalizing | YSR Externalizing | Percentage of homelessness | Victimization | ||||||||
| b | SE | p-value | b | SE | p-value | b | SE | p-value | b | SE | p-value | |
|
| ||||||||||||
| For Intercept | ||||||||||||
| Intercept | 12.78*** | 0.99 | <0.001 | 12.04*** | 0.77 | <0.001 | 52.69*** | 3.66 | <0.001 | −0.76*** | 0.12 | <0.001 |
| Sex | 1.08 | 1.16 | 0.35 | |||||||||
| Ethnicity | 11.44**b | 4.45 | 0.01 | |||||||||
| Age | 2.22 | 1.27 | 0.08 | |||||||||
| Sexual abuse | 3.79** | 1.31 | <0.01 | 2.34*b | 1.09 | 0.03 | ||||||
| Physical abuse | 6.69*** | 1.34 | <0.001 | 5.28*** | 1.17 | <0.001 | ||||||
| For Time slope | ||||||||||||
| Intercept | −0.10 | 0.38 | 0.79 | 0.17 | 0.34 | 0.61 | −8.01*** | 1.90 | <0.001 | −0.28** | 0.11 | 0.01 |
| Treatment attendance | −0.81 | 0.52 | 0.12 | −0.66 | 0.46 | 0.15 | −0.97 | 1.90 | 0.61 | 0.06 | 0.13 | 0.66 |
| MET | 0.99*b | 0.45 | 0.03 | 1.19** | 0.39 | <0.01 | −0.16 | 1.62 | 0.92 | 0.06 | 0.11 | 0.57 |
| CRA | 0.49 | 0.44 | 0.27 | 0.26 | 0.38 | 0.50 | 1.01 | 1.59 | 0.53 | −0.01 | 0.10 | 0.90 |
| Sex | −0.18* | 0.08 | 0.03 | |||||||||
| Ethnicity | −6.19** | 1.79 | <0.001 | |||||||||
| Age | ||||||||||||
| Sexual abuse | 0.22* | 0.09 | 0.01 | |||||||||
| Physical abuse | −1.60*** | 0.41 | <0.001 | −1.14** | 0.36 | <0.01 | 2.54* | 1.30 | 0.05 | 0.27** | 0.09 | <0.01 |
|
| ||||||||||||
| Random Effect | Variance | Χ2test | ||||||||||
|
| ||||||||||||
| Intercept variance | 62.08*** | 53.59*** | 227.26* | |||||||||
| Linear slope variance | 1.10 | 1.91*** | 1.44 | |||||||||
| Level-1 residual variance | 66.90 | 43.26 | 1295.73 | |||||||||
| Estimated parameters | 13 | 12 | 13 | 11 | ||||||||
| Deviance statistic | 6379.36 | 6088.32 | 8784.26 | 2526.07 | ||||||||
| df | 7 | 6 | 7 | 6 | ||||||||
| Χ2test | 50.63*** | 39.86*** | 20.85** | 21.43** | ||||||||
|
| ||||||||||||
| Fixed Effect | CISS Task-oriented | CISS Emotion-oriented | CISS Avoidance-oriented | |||||||||
| b | SE | p-value | b | SE | p-value | b | SE | p-value | ||||
|
| ||||||||||||
| For Intercept | ||||||||||||
| Intercept | 51.93*** | 0.89 | <0.001 | 40.90*** | 1.17 | <0.001 | 49.50*** | 0.79 | <0.001 | |||
| Sex | ||||||||||||
| Ethnicity | ||||||||||||
| Age | ||||||||||||
| Sexual abuse | 3.67*b | 1.53 | 0.02 | |||||||||
| Physical abuse | 5.26** | 1.77 | <0.01 | |||||||||
| For Time slope | ||||||||||||
| Intercept | 0.52 | 0.50 | 0.30 | −1.01a | 0.61 | 0.10 | −0.46a | 0.53 | 0.39 | |||
| Treatment attendance | −0.67 | 0.76 | 0.38 | −1.56*b | 0.69 | 0.03 | −1.28 | 0.67 | 0.06 | |||
| MET | 0.46 | 0.66 | 0.48 | 1.53* | 0.60 | 0.01 | 0.90a | 0.59 | 0.13 | |||
| CRA | −0.48 | 0.64 | 0.45 | 0.39 | 0.58 | 0.51 | −0.34 | 0.57 | 0.55 | |||
| Sex | 1.27** | 0.48 | <0.01 | 1.04* | 0.46 | 0.03 | ||||||
| Ethnicity | ||||||||||||
| Age | ||||||||||||
| Sexual abuse | ||||||||||||
| Physical abuse | −1.18 | 0.61 | 0.05 | |||||||||
|
| ||||||||||||
| Random Effect | ||||||||||||
|
| ||||||||||||
| Intercept variance | 105.00*** | 96.02*** | 68.35*** | |||||||||
| Linear slope variance | 3.14* | 0.93* | 2.02* | |||||||||
| Level-1 residual variance | 138.75 | 124.18 | 127.44 | |||||||||
| Estimated parameters | 9 | 13 | 10 | |||||||||
| Deviance statistic | 6436.74 | 6332.75 | 6295.39 | |||||||||
| df | 3 | 7 | 4 | |||||||||
| Χ2test | 2.25 | 35.29*** | 10.33* | |||||||||
p< 0.001;
p< 0.01;
p< 0.05; ;
parameter estimate showed statistical significance in the treated sample;
parameter estimate showed non-significance in the treated sample.
Secondary outcomes
The main effect of treatment was analyzed first with baseline demographic variables controlled. Significant decreases in depressive symptoms (BDI-II) were found in all three treatment conditions [βCM = −1.68, SE = 0.36, t(257) = −4.74, p < 0.001; βMET = −1.62, SE = 0.37, t(257) = −4.38, p < 0.001; βCRA= −0.91, SE= 0.34, t(257) = −2.60, p < 0.01], so were percent days of homelessness during the past 90 days [βCM = −10.99, SE= 1.27, t(263) = −8.66, p < 0.001; βMET = −11.07, SE= 1.32, t(263) = −838, p < 0.001; βCRA = −10.38, SE= 1.24, t(263) = −8.35, p < 0.001]. At the 12-month follow-up, 74 participants reported a homeless experience within the prior 3 months and 24 participants reported a homeless experience at every follow-up assessment. None of the three treatment conditions exhibited significant change in task- or emotion-oriented coping (all p’s > 0.05). Those who were assigned to CM or CRA exhibited significant reductions in the likelihood of being victimized [βCM = −0.28, SE = 0.11, t(256) = −2.60, p < 0.01; βCRA = −0.29, SE = 0.12, t(256) = −2.44, p < 0.05], whereas those in the MET condition only exhibited a trend [βMET = −0.22, SE = 0.12, t(256) = −1.90, p = 0.06]. Those who were assigned to CM also showed significant decreases in YSR Internalizing [β = −0.88, SE= 0.34, t(261) = −2.61, p< 0.01] and YSR Externalizing [β = −0.72, SE= 0.29, t(261) = −2.45, p< 0.05], whereas those who were assigned to the other two conditions did not. MET was the only condition in which participants showed significant increases in avoidance-oriented coping [β = 0.91, SE = 0.46, t(261) = 1.97, p < 0.05].
Significant group differences were observed between CM and MET in the trajectories of YSR internalizing and externalizing scores and CISS emotion-oriented subscale scores. Specifically, those who were assigned to MET exhibited significantly fewer reductions in internalizing [β = 1.10, SE = 0.46, t(261) = 2.40, p < 0.05] and externalizing [β = 1.28, SE = 0.40, t(261) = 3.20, p < 0.01] behaviors as well as emotion-oriented coping [β = 1.42, SE = 0.61, t(261) = 2.33, p < 0.05] than those who were assigned to CM. A number of moderating effects were found among the demographic variables on the changes in secondary outcomes as well (see Table 3). Females exhibited significantly more reductions in depressive symptoms and the likelihood of being victimized than males, as well as greater increases in emotion-oriented and avoidance-oriented coping (all p’s < 0.05). African Americans exhibited significantly more reductions in percent days of homelessness over time than those in other ethnic groups [β = −6.19, SE = 1.79, t(261) = −3.46, p < 0.001]. Older participants showed significantly more reductions in depressive symptoms [β = −0.39, SE = 0.18, t(254) = −2.17, p < 0.05]. Those who reported a history of physical abuse at baseline exhibited significantly more reductions in depressive symptoms, internalizing and externalizing behaviors [all p’s < 0.05, see Table 3], and significantly more reduction in emotion-oriented coping [β = −1.18, SE = 0.61, t(259) = −1.93, p = 0.05]. However, participants with a history of physical abuse exhibited significantly fewer reductions in the likelihood of being victimized [β = 0.27, SE = 0.09, t(256) = 3.15, p < 0.01] and fewer reductions in percent days of homelessness [β = 2.55, SE = 1.30, t(261) = 1.96, p = 0.05]. Those with a history of sexual abuse also exhibited significantly fewer reductions in the likelihood of being victimized [β = 0.22, SE = 0.09, t(256) = 2.51, p < 0.05].
3.3. Analyses with the treated sample
Analyses with the treated sample yielded very similar results to the ITT analyses, with a few exceptions. There was a significant difference between CRA and CM in terms of reductions in frequency of drug use in the treated sample, which was not significant in the ITT sample. Specifically, those in the CRA condition showed a greater reduction in frequency of drug use than those in the CM [β = −4.21, SE = 1.95, t(177) = −2.16, p< 0.05]. In addition, those in the CM condition exhibited a greater reduction in avoidance-oriented coping skills than those in the MET [β = −1.39, SE = 0.68, t(180) = −2.02, p < 0.05] Moreover, the group differences between MET and CM in reductions among internalizing behaviors were not significant in the treated sample [β = 0.96, SE = 0.50, t(180) = 1.92, p = 0.057]. Therefore, with the treated sample, all three treatments yielded equivalent reductions in internalizing behaviors. Some of the moderating effects, such as the effect of sex on depressive symptoms, became nonsignificant in the treated sample (see Table 4).
3.4. Clinical significance
Table 5 shows the distribution of participants who exhibited improvement, non-significant change, and deterioration in all primary and secondary outcomes except victimization experience by treatment group. For most of the outcomes, more than 50% of the participants in each treatment group exhibited clinically significant improvement post-treatment. That is, many participants (ranging from 33.8% to 67.6%) showed clinically significant reductions in the primary and secondary outcomes by the 6-month follow-up.
Table 5.
Distributions of different categories of clinical significance among primary and secondary outcome variables
| Variable | MET | CRA | CM | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Group 1 | Group 2 | Group 3 | Group 1 | Group 2 | Group 3 | Group 1 | Group 2 | Group 3 | |
| Frequency of alcohol use | 12 (20.3%) | 19 (32.2%) | 28 (47.5%) | 15 (24.2%) | 16 (25.8%) | 31 (50.0%) | 20 (33.9%) | 13 (22.0%) | 26 (44.1%) |
| SECs | 16 (27.1%) | 14 (23.7%) | 29 (49.2%) | 10 (16.1%) | 17 (27.4%) | 35 (56.5%) | 11 (18.6%) | 16 (27.1%) | 32 (54.2%) |
| Frequency of drug use | 14 (23.7%) | 10 (16.9%) | 35 (59.3%) | 14 (22.6%) | 15 (24.2 %) | 33 (53.2%) | 18 (30.5%) | 8 (13.6%) | 33 (55.9%) |
| BDI total score | 12 (23.1%) | 10 (19.2%) | 30 (57.7%) | 11 (20.8%) | 11 (20.8%) | 31 (58.5%) | 17 (34.0%) | 7 (14.0%) | 26 (52.0%) |
| YSR Internalizing | 18 (26.5%) | 10 (14.7%) | 40 (58.8%) | 26 (40.0%) | 11 (16.9%) | 28 (43.1%) | 20 (30.8%) | 11 (16.9%) | 34 (52.3%) |
| YSR Externalizing | 21 (30.9%) | 10 (14.7%) | 37 (54.4%) | 25 (38.5%) | 6 (9.2%) | 34 (52.3%) | 21 (32.3%) | 9 (13.8%) | 35 (53.8%) |
| CISS Task-oriented | 30 (46.2%) | 13 (20.0%) | 22 (33.8%) | 21 (34.4%) | 14 (23.0%) | 26 (42.6%) | 18 (30.5%) | 17 (28.8%) | 24 (40.7%) |
| CISS Emotion-oriented | 18 (29.5%) | 14 (23.0%) | 29 (47.5%) | 20 (32.8%) | 10 (16.4%) | 31 (50.8%) | 19(32.8%) | 11 (19.0%) | 28 (48.3%) |
| CISS Avoidance-oriented | 30 (46.9%) | 8 (12.5%) | 26 (40.6%) | 21 (33.9%) | 16 (25.8%) | 25 (40.3%) | 22 (38.6%) | 14 (24.6%) | 21 (36.8%) |
| Percent days of homelessness | 9 (13.2%) | 13 (19.1%) | 46 (67.6%) | 9 (13.0%) | 19 (27.5%) | 41 (59.4%) | 10 (15.4%) | 12 (18.5%) | 43 (66.2%) |
*Group 1: Deteriorated; Group 2: Non-significant change; Group 3: Improved.
4. Discussion
Adding to a very small number of studies, the current study offers findings from a comparative effectiveness trial of three empirically-supported interventions for homeless adolescents and young adults evidencing substance use disorder. Each intervention has shown efficacy in treating substance use problems and for those experiencing homelessness. Of interest in this study was whether differential support would be found for CRA, previously found to show significant improvements in multiple domains compared to drop-in center services alone (Slesnick et al., 2007). Treatment providers want to know which treatment is most effective for use with this population, and this study offers some preliminary conclusions.
4.1. Clinical Implications
Primary Outcome
Participants in all three interventions exhibited decreasing trends in the average frequency of alcohol or drug use and average SECs (see Table 3). In regard to frequency of alcohol and drug use, the ITT analysis showed no differences among the three treatments, with all showing statistically significant reductions to 12-months. Even though CM did not target substance use directly, it performed similarly to the two other evidence-based, manualized treatment models. This finding supports the continued use of CM by drop-in centers, and implies that drop-in centers may not need to transition to new, and potentially more expensive, intervention models. However, at least in the treated sample, CRA showed a significantly greater reduction in drug use frequency compared to CM. Therefore, in the treated sample, the findings suggest that a targeted substance use treatment (CRA) is more effective. It should be noted that although reductions in the primary outcomes were statically significant in all three interventions, at the 12-month follow-up assessment, the average frequency of drug use was still high, with participants reporting using illicit drugs on 40% to 50% of the prior 90 days. It may be the case that improvements in substance use without housing are limited. Therefore, the current findings suggest that these three treatments have significant harm reduction potential.
Of potentially greatest significance to the field, the current findings offer evidence indicating that homeless youth, who were not seeking treatment for substance use disorders, and for whom the program did not provide housing, can be successfully engaged into treatment and have successful outcomes, with between 54-59% of the sample showing clinically significant improvement across time on most outcomes. Unlike the findings of Baer and Peterson (2007), this study indicates that those assigned to MET showed significantly reduced alcohol and drug use even to 12 months post-baseline, findings similar to those with younger adolescents residing in a runaway shelter (Slesnick et al., 2013). Also, these findings support the use of case management as a stand-alone intervention, as found by Cauce et al. (1994). Overall, the findings in this study showing significant improvements over time, but few differences between conditions, mirror those with the more stable adolescents recruited from a runaway shelter (Slesnick et al., 2013) as well as housed adolescents (Dennis et al., 2004; Godley et al. 2010).
Secondary Outcomes
Significant reductions in depressive symptoms and homelessness were observed in all three intervention conditions. A few differences were found between interventions on other secondary outcomes. While no intervention condition exhibited significant improvements in task- or emotion-oriented coping, those assigned to MET improved significantly in avoidance-oriented coping. Also, only those who were assigned to CM showed significant decreases in internalizing and externalizing behaviors. CM helped youth manage their lives, likely reducing stress and leading to the observed improvements in mental health and other outcomes. Significant decreases in victimization experiences were also found among those in the CM and CRA condition but not MET.
Improvement in one domain is often associated with improvement in other domains, as Jessor and Jessor’s problem behavior syndrome would predict (1977). That is, many theorists and researchers understand the problem behaviors of adolescents within a network of correlated behaviors (Jessor & Jessor, 1977). The mechanism associated with this change is not well-understood. For example, coping skills are considered to underlie many problem behaviors and resilient outcomes (Campbell-Sills, Cohan, & Stein, 2006), and treatments often seek to increase coping skills. In this study, coping strategies showed little change. When stressors are extreme and out of one’s control, and one could argue that homelessness meets this criteria, then task-oriented coping may be less salient for changing behavior because homeless youth may have little agency to impact the structural factors associated with their situation (Kidd & Carroll, 2007). Future research might determine that factors associated with change, not assessed in this study, such as self-efficacy, therapeutic bonding, commitment to change, and perhaps the experience of unconditional positive regard, are at the root of change in these three interventions. In fact, Bandura (1977) argues that self-efficacy is at the root of all change, with the experience of success preceding the implementation of prosocial and promotive behaviors.
Moderators
Sex and childhood abuse had more moderating effects than age and ethnicity. Compared to males, females showed a greater reduction in alcohol and drug use frequency, converging with other studies indicating that females are more likely than males to show better alcohol and drug use outcomes (Greenfield et al., 2007; Slesnick, Erdem, Collins, Bantchevska, & Katafiasz, 2011). Females also showed significantly more improvements in several of the secondary outcomes compared to males. One possibility for this finding is that females tend to be more socially oriented (Eagly, Wood, & Diekman, 2000), and may respond more powerfully to the relational aspects (e.g., alliance) associated with these interventions. In addition, this study showed that a history of childhood physical abuse (but not sexual abuse) was associated with poorer drug use and homelessness outcomes. Similarly, Naar-King et al. (2002) examined treatments for behavior problem youth and found that sexually abused youth did not differ in outcomes from the nonabused group, but physically abused youth showed poorer treatment outcomes. Possibly, those with histories of physical abuse also experience negative sequaelae associated with physical trauma such as traumatic brain injury and/or other comorbid conditions which have also been shown to negatively impact treatment outcomes (Graham & Cardon, 2008). Finally, confirming findings from previous studies showing that childhood victimization predicts greater victimization on the streets (Robertson & Toro, 1999; Thrane, Hoyt, Whitbeck, & Yoder, 2006), fewer reductions in street victimization were observed among those who experienced childhood physical and sexual abuse.
4.2. Limitations
This research is limited in that all adolescents and young adults were recruited as a sample of convenience, and in one city, from the only drop-in center in central Ohio. Cities vary in racial/ethnic distribution and substance use patterns (Edidin et al., 2012) and the participants recruited in this study might not be representative of those from other parts of the country. Also, those who agreed to participate in this research study might be more (or less) motivated for treatment than those who refused to participate. Further, participants interacted with each other at the drop-in center, possibly leading to some amount of contamination of treatment conditions. The consequence of contamination bias is a reduction in the observed treatment effects (Torgerson, 2001), creating problems for interpretation. Melis et al. (2011) suggest that when individual randomization is optimal, increasing the sample size is necessary to dilute the contamination effects.
While participants were provided a $5 food gift card for each session attended in this study, drop-in centers could offer other food items to encourage treatment attendance (e.g., choice of a selection of food items, usually obtained through food banks). On average, participants attended about half of the available sessions, likely due to their chaotic lifestyles. But, in fact, we consider it a success to have engaged these youth in multiple treatment sessions, especially since they were homeless and were not originally seeking treatment for substance use disorders. The session completion rates reported here are similar to other adolescent substance use treatment studies with more stable, housed youth, with Godley et al. (2014) reporting that 68% of adolescents completed 4 or more CM sessions (out of 12 sessions total) (versus an average of 7.3 sessions and 64% in this sample completing 4 or more sessions). Dennis et al. (2004) reported an average of 7.9 hours of adolescent-CRA sessions attended (versus the ITT average of 6.2 sessions in the current study). Finally, it must be acknowledged that a large number of statistical comparisons were made, increasing the potential for Type I error, or the potential for the results to be due to chance. But, this limitation is balanced by the strengths of: (1) measuring multiple outcomes, and (2) reporting all of the outcomes in one paper, rather than in separate papers.
4.3. Conclusions and Future Directions
This is the second randomized clinical trial indicating that substance use treatment, specifically CRA, is effective with street living homeless adolescents and young adults. The first trial indicated that CRA was superior to treatment as usual (TAU), or standard drop-in services (Slesnick et al., 2007). As such, the current trial did not include a TAU condition, and all interventions were considered viable intervention options (Carroll & Rounsaville, 2003). Although some evidence was found for CRA to have superior drug use outcomes in the treated sample, no other differences between the three interventions were observed and evidence for the superiority or inferiority of interventions was not provided. Drop-in centers have a unique opportunity to engage homeless adolescents and young adults into more intensive treatments including substance use treatment. Providing access to treatment within the drop-in center is likely more effective than referring clients to other treatment programs. That is, drop-in centers are typically considered a bridge between the streets and the mainstream, and are low-demand settings. Many young people experiencing homelessness have had negative experiences with family, school and typical services within systems meant to serve them, such as shelters or foster care. This population is considered difficult to engage and to serve given low levels of trust, transportation and stability. Those who do not want treatment or intervention cannot be called or visited at their home, and accessing other programs is complicated by lack of insurance and transportation. Anecdotally, successful treatment requires the development of a trusting relationship which may be key to further change. In summary, this study adds to a very small body of literature seeking to identify effective interventions for treating homeless youth evidencing substance use disorder. The findings suggest that drop-in centers have a choice of efficacious interventions when serving this group, though given fewer sessions, MET may be a more cost-effective option (Dennis et al., 2004).
Highlights.
Three empirically-supported substance use treatments are tested with a sample of homeless youth.
Youth in all three treatment conditions showed improvements in substance use and associated problems across time.
Treatment outcomes were moderated by sex and childhood abuse history.
Acknowledgement
This research was supported by NIDA grant R01 DA13549 to the first author.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Achenbach T. Integrative guide for the 1991 CBCL/4-18, YSR, and TRF profiles. Department of Psychiatry, University of Vermont; Burlington: 1991. [Google Scholar]
- Altena A, Brilleslijper-Kater S, Wolf J. Effective interventions for homeless youth: A systematic review. American Journal of Preventive Medicine. 2010;38(6):637–645. doi: 10.1016/j.amepre.2010.02.017. [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association . Diagnostic and Statistical Manual of Mental Disorders-IV-TR. 4th American Psychiatric Association; Washington, DC: 2000. [Google Scholar]
- Auerswald C, Eyre S. Youth homelessness in San Francisco: A life cycle approach. Social Science & Medicine. 2002;54(10):1497–1512. doi: 10.1016/s0277-9536(01)00128-9. [DOI] [PubMed] [Google Scholar]
- Azrin NH, Donohue B, Teichner GA, Crum T, Howell J, DeCato LA. A controlled evaluation and description of individual-cognitive problem solving and family-behavior therapies in dually-diagnosed conduct-disordered and substance-dependent youth. Journal of Child & Adolescent Substance Abuse. 2001;11(1):1–43. [Google Scholar]
- Baer J, Garrett S, Beadnell B, Wells E, Peterson P. Brief motivational intervention with homeless adolescents: evaluating effects on substance use and service utilization. Psychology of Addictive Behaviors. 2007;21(4):582–586. doi: 10.1037/0893-164X.21.4.582. [DOI] [PubMed] [Google Scholar]
- Baer J, Ginzler J, Peterson P. DSM-IV alcohol and substance abuse and dependence in homeless youth. Journal of Studies on Alcohol. 2003;64(1):5–15. doi: 10.15288/jsa.2003.64.5. [DOI] [PubMed] [Google Scholar]
- Bandura A. Self-efficacy: toward a unifying theory of behavioral change. Psychological Review. 1977;84(2):191–215. doi: 10.1037//0033-295x.84.2.191. [DOI] [PubMed] [Google Scholar]
- Beck A, Steer R, Brown G. BDI-II, Beck depression inventory: Manual. 2 Harcourt Brace; Boston, MA: 1996. [Google Scholar]
- Brigham GS, Feaster DJ, Wakim PG, Dempsey CL. Choosing a control group in effectiveness trials of behavioral drug abuse treatments. Journal of Substance Abuse Treatment. 2009;37(4):388–397. doi: 10.1016/j.jsat.2009.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bucher C. Towards a needs-based typology of homeless youth. Journal of Adolescent Health. 2008;42:549–554. doi: 10.1016/j.jadohealth.2007.11.150. [DOI] [PubMed] [Google Scholar]
- Carroll KM, Rounsaville BJ. Bridging the gap: A hybrid model to link efficacy and effectiveness research in substance abuse treatment. Psychiatric Services. 2003;54(3):333–339. doi: 10.1176/appi.ps.54.3.333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Campbell-Sills L, Cohan S, Stein M. Relationship of resilience to personality, coping, and psychiatric symptoms in young adults. Behaviour Research and Therapy. 2006;44(4):585–599. doi: 10.1016/j.brat.2005.05.001. [DOI] [PubMed] [Google Scholar]
- Cauce A, Morgan C, Wagner V, Moore E, Sy J, Wurzbacher K, Blanchard T. Effectiveness of intensive case management for homeless adolescents: Results of a 3-month follow-up. Journal of Emotional and Behavioral Disorders. 1994;2:219–227. [Google Scholar]
- Chamberlain C, MacKenzie D. Youth homelessness: Four policy proposals. Australian Housing and Urban Research Institute: Final Report. 2004 [Google Scholar]
- Cohen J. Statistical Power Analysis for the Behavioral Science. 2nd Erlbaum; Hillsdale, NJ: 1988. [Google Scholar]
- Collins SE, Malone DK, Larimer ME. Motivation to change and treatment attendance as predictors of alcohol-use outcomes among project-based Housing First residents. Addictive Behaviors. 2012;37:931–939. doi: 10.1016/j.addbeh.2012.03.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cooper E. The runaway and homeless youth program: Administration, funding, and legislative actions. 2006 CRS Report for Congress. [Google Scholar]
- Dale V, Coulton S, Godfrey C, Copello A, Hodgson R, Heather N, Orford J, Raistrick D, Slegg G, Tober G. Exploring treatment attendance and its relationship to outcome in a randomized controlled trial of treatment for alcohol problems: Secondary analysis of the UK Alcohol Treatment Trial (UKATT) Alcohol and Alcoholism. 2011;46:592–599. doi: 10.1093/alcalc/agr079. [DOI] [PubMed] [Google Scholar]
- Dennis M, Godley S, Diamond G, Tims F, Babor T, Donaldson J, Funk R. The cannabis youth treatment (CYT) study: Main findings from two randomized trials. Journal of Substance Abuse Treatment. 2004;27:197–213. doi: 10.1016/j.jsat.2003.09.005. [DOI] [PubMed] [Google Scholar]
- Eagly A, Wood W, Diekman A. Social role theory of sex differences and similarities: A current appraisal. In: Eckes T, Trautner HM, editors. The Developmental Social Psychology of Gender. Erlbaum; Mahwah, NJ: 2000. pp. 123–174. [Google Scholar]
- Edidin J, Ganim Z, Hunter S, Karnik N. The mental and physical health of homeless youth: A literature review. Child Psychiatry and Human Development. 2012;43(3):354–375. doi: 10.1007/s10578-011-0270-1. [DOI] [PubMed] [Google Scholar]
- Endler NS, Parker JDA. Coping Inventory for Stressful Situations (CISS): Manual. Multi-Health Systems; Toronto: 1990. [Google Scholar]
- Fisk D, Rakfeldt J, McCormack E. Assertive outreach: an effective strategy for engaging homeless persons with substance use disorders into treatment. The American Journal of Drug and Alcohol Abuse. 2006;32(3):479–486. doi: 10.1080/00952990600754006. [DOI] [PubMed] [Google Scholar]
- Gaetz S. Safe streets for whom? Homeless youth, social exclusion, and criminal victimization. Canadian Journal of Criminology and Criminal Justice. 2004;46(4):423–456. [Google Scholar]
- Garrick D, Lee MT, Horgan CM, Acevedo A, Washington Public Sector Workgroup Adapting Washington Circle performance measures for public sector substance abuse treatment systems. Journal of Substance Abuse Treatment. 2009;36(3):265–277. doi: 10.1016/j.jsat.2008.06.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Godley S, Garner B, Passetti L, Funk R, Dennis M, Godley M. Adolescent outpatient treatment and continuing care: main findings from a randomized clinical trial. Drug and Alcohol Dependence. 2010;110(1):44–54. doi: 10.1016/j.drugalcdep.2010.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Godley MD, Godley SH, Dennis ML, Funk RR, Passetti LL, Petry NM. A randomized trial of assertive continuing care and contingency management for adolescents with substance use disorders. Journal of Consulting and Clinical Psychology. 2014;82(1):40–51. doi: 10.1037/a0035264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Graham D, Cardon A. An update on substance use and treatment following traumatic brain injury. Annals of the New York Academy of Sciences. 2008;1141(1):148–162. doi: 10.1196/annals.1441.029. [DOI] [PubMed] [Google Scholar]
- Greene J, Ennett S, Ringwalt C. Substance use among runaway and homeless youth in three national samples. American Journal of Public Health. 1997;87(2):229–235. doi: 10.2105/ajph.87.2.229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greenfield S, Brooks A, Gordon S, Green C, Kropp F, et al. Substance abuse treatment entry, retention, and outcome in women: A review of the literature. Drug and Alcohol Dependence. 2007;86(1):1–21. doi: 10.1016/j.drugalcdep.2006.05.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haber MG, Toro PA. Homelessness among families, children, and adolescents: An ecological–developmental perspective. Clinical Child and Family Psychology Review. 2004;7(3):123–164. doi: 10.1023/b:ccfp.0000045124.09503.f1. [DOI] [PubMed] [Google Scholar]
- Higgins ST, Budney AJ, Bickel WK, Badger GJ, Foerg FE, Ogden D. Outpatient behavioral treatment for cocaine dependence: one-year outcome. Experimental and Clinical Psychopharmacology. 1995;3(2):205–212. [Google Scholar]
- Higgins ST, Wong CJ, Badger GJ, Ogden DEH, Dantona RL. Contingent reinforcement increases cocaine abstinence during outpatient treatment and 1 year of follow-up. Journal of Consulting and Clinical Psychology. 2000;68(1):64–72. doi: 10.1037//0022-006x.68.1.64. [DOI] [PubMed] [Google Scholar]
- Jacobson NS, Follette WC, Revenstorf D. Psychotherapy outcome research: Methods for reporting variability and evaluating clinical significance. Behavior Therapy. 1984;17:308–311. [Google Scholar]
- Jacobson N, Truax P. Clinical significance: A statistical approach to define meaningful change in psychotherapy research. Journal of Consulting and Clinical Psychology. 1991;59(1):12–19. doi: 10.1037//0022-006x.59.1.12. [DOI] [PubMed] [Google Scholar]
- Jessor R, Jessor SL. Problem behavior and psychosocial development: A longitudinal study of youth. Academic Press; New York: 1977. [Google Scholar]
- Joanning H, Thomas F, Quinn W, Mullen R. Treating adolescent drug abuse: A comparison of family systems therapy, group therapy, and family drug education. Journal of Marital and Family Therapy. 1992;18:345–356. [Google Scholar]
- Johnson K, Whitbeck L, Hoyt D. Substance abuse disorders among homeless and runaway adolescents. Journal of Drug Issues. 2005;35(4):799–816. doi: 10.1177/002204260503500407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kertesz SG, Mullins AN, Schumacher JE, Wallace D, Kirk K, Milby JB. Long-term housing and work outcomes among treated cocaine-dependent homeless persons. The Journal of Behavioral Health Services & Research. 2007;34(1):17–33. doi: 10.1007/s11414-006-9041-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kidd S, Carroll M. Coping and suicidality among homeless youth. Journal of Adolescence. 2007;30(2):283–296. doi: 10.1016/j.adolescence.2006.03.002. [DOI] [PubMed] [Google Scholar]
- Kipke M, Montgomery S, Simon T, Iverson E. Substance abuse disorders among runaways and homeless youth. Substance Use and Misuse. 1997;32:969–986. doi: 10.3109/10826089709055866. [DOI] [PubMed] [Google Scholar]
- Linehan MM, Schmidt H, Dimeff LA, Craft JC, Kanter J, Comtois KA. Dialectical behavior therapy for patients with Borderline Personality Disorder and drug-dependence. The American journal on addictions. 1999;8(4):279–292. doi: 10.1080/105504999305686. [DOI] [PubMed] [Google Scholar]
- Lipsey MW, Wilson DB. Practical Meta-analysis. Sage; Beverly Hills, CA: 2001. [Google Scholar]
- Manuel JK, Austin JL, Miller WR, McCrady BS, Tonigan JS, Meyers RJ, Bogenschutz MP. Community Reinforcement and Family Training: A pilot comparison of group and self-directed delivery. Journal of Substance Abuse Treatment. 2012;43(1):129–136. doi: 10.1016/j.jsat.2011.10.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marshall EJ, Bhugra D. Services for the mentally ill homeless. In: Bhugra D, editor. Homelessness and Mental Health. Cambridge University Press; Cambridge, UK: 1996. pp. 99–109. [Google Scholar]
- McKinney-Vento Homeless Assistance Act, Re-Authorized 2002. 42 U.S.C. 11431 et seq 725.
- Meade M, Slesnick N. Ethical considerations for research and treatment with runaway and homeless adolescents. Journal of Psychology. 2002;136(4):449–463. doi: 10.1080/00223980209604171. PMC2430768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Melis RJF, Teerenstra S, Olde Rikkert MGM, Borm GF. Pseudo cluster randomization: Balancing the disadvantages of cluster and individual randomization. Evaluation & the Health Professions. 2011;34(2):151–163. doi: 10.1177/0163278710361925. [DOI] [PubMed] [Google Scholar]
- Meyers R, Smith J. Clinical guide to alcohol treatment: The Community Reinforcement Approach. Guilford Press; New York: 1995. [Google Scholar]
- Milby J, Schumacher J, Wallace D, Freedman M, Vuchinich R. To house or not to house: the effects of providing housing to homeless substance abusers in treatment. American Journal of Public Health. 2005;95(7):1259–1265. doi: 10.2105/AJPH.2004.039743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller W. Project MATCH Monograph Series. Vol. 5. U.S. Dept. of Health; Bethesda, MD: 1996. Form 90 a structured assessment interview for drinking and related problem behaviors. [Google Scholar]
- Miller WR, Zweben A, DiClemente CC, Rychtarik RG. Motivational Enhancement Therapy manual: A clinical research guide for therapists treating individuals with alcohol abuse and dependence (Volume 2, Project MATCH Monograph Series) National Institute on Alcohol Abuse and Alcoholism; Rockville, MD: 1992. [Google Scholar]
- Miller W, Rollnick S. Motivational Interviewing: Preparing people for change. 3rd Guilford Press; New York: 2013. [Google Scholar]
- Milligan C, Nich C, Carroll K. Ethnic differences in substance abuse treatment retention, compliance, and outcome from two clinical trials. Psychiatric Services. 2004;55:167. doi: 10.1176/appi.ps.55.2.167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Naar-King S, Silvern L, Ryan V, Sebring D. Type and severity of abuse as predictors of psychiatric symptoms in adolescence. Journal of Family Violence. 2002;17:133–149. [Google Scholar]
- National Alliance to End Homelessness . Promising strategies to end family homelessness. Author; Washington, DC: 2006. [Google Scholar]
- Oviedo-Joekes E, Marchand K, Guh D, Marsh D, Brissette S, et al. History of reported sexual or physical abuse among long-term heroin users and their response to substitution treatment. Addictive Behaviors. 2011;36(1):55–60. doi: 10.1016/j.addbeh.2010.08.020. [DOI] [PubMed] [Google Scholar]
- Peterson P, Baer J, Wells E, Ginzler J, Garrett S. Short-term effects of a brief motivational intervention to reduce alcohol and drug risk among homeless adolescents. Psychology of Addictive Behaviors. 2006;20(3):254. doi: 10.1037/0893-164X.20.3.254. [DOI] [PubMed] [Google Scholar]
- Rapp RC, Otto AL, Lane DT, Redko C, McGatha S, Carlson RG. Improving linkage with substance abuse treatment using brief case management and motivational interviewing. Drug and Alcohol Dependence. 2008;94(1):172–182. doi: 10.1016/j.drugalcdep.2007.11.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Raudenbush S, Bryk A, Congdon R. HLM 7: Hierarchical linear and nonlinear modeling [computer software] Scientific Software International; Lincolnwood, IL: 2011. [Google Scholar]
- Reardon ML, Cukrowicz KC, Reeves MD, Joiner TE. Duration and regularity of therapy attendance as predictors of treatment outcome in an adult outpatient population. Psychotherapy Research. 2002;12:273–285. [Google Scholar]
- Robertson M, Toro P. Homeless youth: Research, intervention, and policy. In: Fosburg L, Dennis D, editors. Practical lessons: The 1998 National Symposium on Homelessness Research. U.S. Department of Housing and Urban Development; Washington DC: 1999. pp. 3–32. [Google Scholar]
- Rounsaville BJ, Carroll KM, Onken LS. A stage model of behavioral therapies research: Getting started and moving on from stage I. Clinical Psychology: Science and Practice. 2001;8(2):133–142. [Google Scholar]
- Sacks JY, McKendrick K, Banks S. The impact of early trauma and abuse on residential substance abuse treatment outcomes for women. Journal of Substance Abuse Treatment. 2008;34(1):90–100. doi: 10.1016/j.jsat.2007.01.010. [DOI] [PubMed] [Google Scholar]
- Schumacher JE, Milby JB, Caldwell E, Raczynski J, Engle M, Michael M, Carr J. Treatment outcome as a function of treatment attendance with homeless persons abusing cocaine. Journal of Addictive Diseases. 1995;14:73–85. doi: 10.1300/j069v14n04_05. [DOI] [PubMed] [Google Scholar]
- Shaffer D. Diagnostic Interview Schedule for Children -2.3 Version. Columbia Univ; NY: 1992. [Google Scholar]
- Slesnick N, Bartle-Haring S, Gangamma R. Predictors of substance use and family therapy outcome among physically and sexually abused runaway adolescents. Journal of Marital and Family Therapy. 2006;32(3):261–281. doi: 10.1111/j.1752-0606.2006.tb01606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Slesnick N, Dashora P, Letcher A, Erdem G, Serovich J. A review of services and interventions for runaway and homeless youth: Moving forward. Children Youth Services Review. 2009;31:731–742. doi: 10.1016/j.childyouth.2009.01.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Slesnick N, Erdem G. Efficacy of ecologically-based treatment with substance-abusing homeless mothers: Substance use and housing outcomes. Journal of Substance Abuse Treatment. 2013;45(5):416–425. doi: 10.1016/j.jsat.2013.05.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Slesnick N, Erdem G, Bartle-Haring S, Brigham GS. Intervention with substance-abusing runaway adolescents and their families: Results of a randomized clinical trial. Journal of Consulting and Clinical Psychology. 2013;81(4):600–614. doi: 10.1037/a0033463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Slesnick N, Erdem G, Collins J, Bantchevska D, Katafiasz H. Predictors of treatment attendance among adolescent substance abusing runaways: A comparison of family and individual therapy modalities. Journal of Family Therapy. 2011;33(1):66–84. [Google Scholar]
- Slesnick N, Prestopnik JL. Comparison of family therapy outcome with alcohol-abusing, runaway adolescents. Journal of Marital and Family Therapy. 2009;35(3):255–277. doi: 10.1111/j.1752-0606.2009.00121.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Slesnick N, Prestopnik J, Meyers R, Glassman M. Treatment outcome for homeless, street-living youth. Addictive Behaviors. 2007;32:1237–1251. doi: 10.1016/j.addbeh.2006.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Slesnick N, Tonigan J. Assessment of alcohol and other drugs used by runaway youths: A test-retest study of the Form 90. Alcoholism Treatment Quarterly. 2004;22:21–34. doi: 10.1300/J020v22n02_03. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith JE, Meyers RJ, Delaney HD. The community reinforcement approach with homeless alcohol dependent individuals. Journal of Consulting and Clinical Psychology. 1998;66:541–548. doi: 10.1037//0022-006x.66.3.541. [DOI] [PubMed] [Google Scholar]
- Sobell LC, Sobell MB. Timeline follow-back. In: Litten R, Allen J, editors. Measuring alcohol consumption. Humana Press; Totowa, NJ: 1992. pp. 41–72. [Google Scholar]
- Substance Abuse Mental Health Service Administration National Registry for Evidence Based Practice: Brief Strengths Based Case Management for Substance Abuse. 2014 Retrieved from: http://www.nrepp.samhsa.gov/ViewIntervention.aspx?id=58.
- Tanner-Smith EE, Wilson SJ, Lipsey MW. The comparative effectiveness of outpatient treatment for adolescent substance abuse: a meta-analysis. Journal of Substance Abuse Treatment. 2013;44(2):145–158. doi: 10.1016/j.jsat.2012.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Teare JF, Peterson RW, Furst D, Authier K. Treatment implementation in a short-term emergency shelter program. Child Welfare: Journal of Policy, Practice, and Program. 1994 [Google Scholar]
- Thrane L, Hoyt D, Whitbeck L, Yoder K. Impact of family abuse on running away, deviance, and street victimization among homeless rural and urban youth. Child Abuse & Neglect. 2006;30(10):1117–1128. doi: 10.1016/j.chiabu.2006.03.008. [DOI] [PubMed] [Google Scholar]
- Tonigan J, Miller W, Brown J. The reliability of Form 90: An instrument for assessing alcohol treatment outcome. Journal of Studies on Alcohol. 1997;58:358–364. doi: 10.15288/jsa.1997.58.358. [DOI] [PubMed] [Google Scholar]
- Torgerson DJ. Contamination in trials: Is cluster randomisation the answer? British Medical Journal. 2001;322:355–357. doi: 10.1136/bmj.322.7282.355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- UNESCO Street Children. 2007 Retrieved January 22, 2009, from http://portal.unesco.org/shs/en/ev.phpURL_ID=11403&URL_DO=DO_TOPIC&URL_SECT ION=201.html.
- Waldron HB, Turner CW. Evidence-based psychosocial treatments for adolescent substance abuse. Journal of Clinical Child & Adolescent Psychology. 2008;37(1):238–261. doi: 10.1080/15374410701820133. [DOI] [PubMed] [Google Scholar]
- Waldron H.B, Slesnick, N., Brody JL, Turner CW, Peterson TR. Treatment outcomes for adolescent substance abuse at 4-and 7-month assessments. Journal of Consulting and Clinical Psychology. 2001;69(5):802. [PubMed] [Google Scholar]
- Westerberg V, Tonigan J, Miller W. Reliability of Form 90D: An instrument for quantifying drug use. Substance Use. 1998;19:179–189. doi: 10.1080/08897079809511386. [DOI] [PubMed] [Google Scholar]
- Whitbeck LB, Hoyt DR, Yoder KA. A risk-amplification model of victimization and depressive symptoms among runaway and homeless adolescents. American Journal of Community Psychology. 1999;27(2):273–296. doi: 10.1023/A:1022891802943. [DOI] [PubMed] [Google Scholar]
- Williams RJ, Chang SY. A comprehensive and comparative review of adolescent substance abuse treatment outcome. Clinical Psychology: Science and Practice. 2000;7(2):138–166. [Google Scholar]
- Winters K. Treating adolescents with substance use disorders: An overview of practice issues and treatment outcome. Substance Abuse. 1999;20(4):203–225. doi: 10.1080/08897079909511407. [DOI] [PubMed] [Google Scholar]
- Zerger S. Substance abuse treatment: What works for homeless people? A review of the literature. National Health Care for the Homeless; Nashville, TN: 2002. [Google Scholar]