Abstract
Rhabdomyolysis is characterized by severe acute muscle injury resulting in muscle pain, weakness, and/or swelling with release of myofiber contents into the bloodstream. Symptoms develop over hours to days following an inciting factor and may be associated with dark pigmentation of the urine. Serum creatine kinase and urine myoglobin levels are markedly elevated. The clinical examination, history, laboratory studies, muscle biopsy, and genetic testing are useful tools for diagnosis of rhabdomyolysis, and they can help differentiate acquired from inherited causes of rhabdomyolysis. Acquired causes include substance abuse, medication or toxic exposures, electrolyte abnormalities, endocrine disturbance, and autoimmune myopathies. Inherited predisposition to rhabdomyolysis can occur with disorders of glycogen metabolism, fatty acid beta-oxidation, and mitochondrial oxidative phosphorylation. Less common inherited causes of rhabdomyolysis include structural myopathies, channelopathies, and sickle cell disease. This review focuses on the differentiation of acquired and inherited causes of rhabdomyolysis and proposes a practical diagnostic algorithm.
Keywords: Rhabdomyolysis, Symptoms, Etiology, Metabolic myopathy, Inherited myopathy
INTRODUCTION
Rhabdomyolysis is a condition characterized by severe acute muscle injury resulting in muscle pain, weakness, and/or swelling with release of myofiber contents into the bloodstream. This review will focus on acquired and inherited causes of rhabdomyolysis, with an emphasis on the diagnostic evaluation. Rhabdomyolysis caused by crush injury and hypoxic/ischemic injury is reviewed elsewhere1–3
CLINICAL FEATURES OF RHABDOMYOLYSIS
The characteristic clinical features of rhabdomyolysis include myalgia, muscle weakness, and muscle swelling which develop over hours to days4, 5. In a case series of 37 pediatric patients with elevated creatine kinase (CK) ≥ 1000 U/L, the most common presenting symptoms were muscle pain (84%), weakness (73%) and muscle swelling (8.1%)6. In a case series of 77 adult patients hospitalized with rhabdomyolysis, 50% reported muscle pain, and 15% experienced muscle swelling7. In another series of adult patients, 52% presented with muscle swelling8. Historically, observation of dark colored urine (pigmenturia) caused by myoglobin excretion has been considered an important clinical feature for diagnosis of rhabdomyolysis. In 1 case series as many as 80% of adults in had dark urine9. However, in the pediatric population, pigmenturia has been seen or reported ranging from 5.3%6 to 68% of cases10.
Muscle weakness may or may not be present between episodes of rhabdomyolysis. In some metabolic myopathies, fixed weakness is absent in childhood but develops in adulthood. In some muscular dystrophies associated with rhabdomyolysis, muscle atrophy or hypertrophy may be noted.
Many diseases associated with rhabdomyolysis include extra-muscular manifestations that will not be covered in detail here. Acquired causes, especially, may present in the setting of multisystem organ failure. However, it should be noted that glycogen storage diseases may present with extra-muscular manifestations, such as liver dysfunction or hepatomegaly, especially when the disease manifests in neonates or infants. In contrast, those that present in adulthood more frequently have predominant muscle disease. In the mitochondrial disorders, there is a very wide spectrum of potential extra-muscular manifestations. These can include cardiomyopathies, endocrinopathies, and encephalopathies. In patients with rhabdomyolysis who have other organ system involvement, the constellation of these disorders may help guide the diagnostic evaluation.
TESTING IN PATIENTS WITH RHABDOMYOLYSIS
Biochemical diagnosis
Establishing a diagnosis of rhabdomyolysis is based primarily on the appearance of myoglobin in the urine (myoglobinuria) or by a marked elevation in serum CK levels. Following muscle injury, plasma myoglobin increases rapidly and is cleared quickly through renal excretion, and a normal level is re-established within 24 hours11. In contrast, serum CK levels rise 2–12 hours after onset of muscle injury, peak at 3–5 days after injury, and decline over the subsequent 6–10 days12, 13. Given that not all patients present within 24 hours of muscle damage, measurement of CK levels may provide the most reliable biochemical marker of rhabdomyolysis and its severity. Authors of several large case series of rhabdomyolysis agree that CK elevation 5 times the upper limit of normal is the defining biochemical abnormality for this condition4–7, 14, 15. However, some studies suggest using a higher value16–18. It should be noted that chronic muscle diseases, such as inflammatory myopathies and muscular dystrophies may present with CK levels well above 5 times the normal limit. The presence of acute symptoms of muscle pain, weakness, and swelling differentiate rhabdomyolysis from these conditions.
Serum lactate
After the onset of intense activity or isometric exercise, anaerobic metabolism predominates. In this circumstance, muscle glycogen is broken down into glucose, which is then metabolized to pyruvate19, 20. Normally, pyruvate is converted into lactate. However, in cases where defects of the respiratory chain preclude using lactate or pyruvate as an energy source, an abnormal lactate: pyruvate ratio may be measured. In addition, elevated serum lactate in the resting period indicates an underlying mitochondrial myopathy.
Forearm exercise test (FET)
First described by McArdle in the initial report of what is now known as myophosphorylase deficiency21, a revised protocol described in 1970 assesses changes in the levels of lactate, pyruvate, and ammonia following isometric exercise22. To perform this test, a catheter is inserted into the antecubital vein, and baseline measurements are obtained. Thereafter, a blood pressure cuff is inflated above the elbow to produce stasis. The subject is then asked to repeatedly squeeze an ergometer against resistance for 1 minute. Then, the subject stops squeezing, and the blood pressure cuff around the arm is deflated. Samples obtained at 1, 3, 5, 6, 10, and 15 minutes later are measured for lactate, pyruvate, and ammonia levels. In individuals without metabolic disease, lactate is expected to increase 3- to 5-fold within the first 3 minutes of exercise followed by a gradual decrease over the next 12 minutes to baseline levels23. Failure of lactate and ammonia levels to increase indicates submaximal effort. A decreased or inadequate rise in lactate with an adequate rise in ammonia indicates a disruption in glycogen metabolism to pyruvate, which is the typical defect in glycogen storage disease. An elevation in pyruvate with inadequate rise in lactate level can help distinguish lactate dehydrogenase deficiency24.
In individuals with glycogen storage disorders, the ischemic isometric exercise may induce painful cramping and may cause muscle damage. If forearm muscle cramping is severe, the test should be aborted. In fact, Kazemi-Esfarjani, et al. have shown that a modified protocol without induction of ischemia is more comfortable, less damaging, and as reliable as the original protocol25. For this reason, we recommend use of the non-ischemic FET for evaluation of suspected disorders of glycogen metabolism.
Acylcarnitine profile
Analysis of the acylcarnitine profile by mass spectrometry may be useful in the diagnosis of fatty acid oxidation disorders. In a study of 31 asymptomatic patients with recurrent rhabdomyolysis, a diagnosis of fatty acid oxidation disorder was achieved in 7 who had abnormal serum acylcarnitine profiles26. Whether this test has higher yield at the time of muscle symptoms or rhabdomyolysis compared to the resting state is unclear. In the discussion below, we will comment on typical acylcarnitine abnormalities associated with specific metabolic myopathies. We typically check interictal acylcarnitine profiles in patients with suspected fatty acid oxidation disorders and may also seek to obtain the same studies at the time of acute muscle symptoms or rhabdomyolysis, if they recur.
Graded exercise testing
Graded increases in exercise intensity alter inspired oxygen and expired carbon dioxide concentrations. Specifically, in metabolically normal individuals during low-intensity exercise, oxygen consumption is balanced with carbon dioxide production. With higher intensity exercise, oxygen consumption cannot keep pace with demand, and the production of carbon dioxide is greater, thus triggering an increased ventilatory rate. This ventilatory threshold signifies the transition of metabolism from the aerobic to anaerobic state and coincides with increased production of lactate. The respiratory exchange ratio (RER) represents the rate of carbon dioxide production relative to oxygen consumption. Interestingly, at different levels of exercise, the duration before reaching the ventilatory threshold and the RER at the point of exhaustion can help differentiate between defects in glycogen metabolism, fatty acid metabolism, and respiratory chain dysfunction27. It should be noted, however, that abnormalities on graded exercise testing may be seen in deconditioned individuals who may not have an underlying metabolic myopathy.
Muscle biopsy
Muscle biopsy is an important test in patients with suspected metabolic myopathies. In the case of rhabdomyolysis, the timing of muscle biopsy is important. In the case of overwhelming necrosis associated with rhabdomyolysis, there is concern that underlying features of inherited myopathies could be obscured. Thus, we suggest that, if indicated, a muscle biopsy should be obtained once the patient has recovered from rhabdomyolysis. In patients with myalgia, muscle biopsy as a tool for diagnosis is thought to have the highest yield when patients present with 1 or more of the following characteristics: myoglobinuria, presence of a second wind phenomenon, muscle hypertrophy/atrophy, CK levels greater than 2–3 times normal levels, or the presence of a myopathic EMG28. Specific stains can help to identify histopathological features suggestive of certain causes of rhabdomyolysis. For example, in patients with mitochondrial myopathies, Gömöri-Trichrome (GT) staining may show ragged red fibers, and oxidative stains succinyl dehydrogenase (SDH) and cytochrome oxidase (COX) may show SDH-dark and/or COX-negative fibers. Periodic acid-Schiff (PAS) and H&E staining may demonstrate the presence of increased glycogen or glycogen-containing vacuoles, which can guide the diagnosis of of glycogen storage disease. Increased lipid content in myofibers may suggest a disorder of fatty acid oxidation or mitochondrial cytopathy. If specific conditions are suspected, muscle immunohistochemistry can identify enzyme deficiencies, such as myophosphorylase or phosphofructokinase deficiency. In glycogen storage diseases, activities of specific enzymes can be studied in the muscle. Specific respiratory chain functions may be assessed and may be helpful to evaluate respiratory chain functions in suspected mitochondrial disease.
Genetic testing
Numerous options are now available for genetic testing in suspected cases of inherited muscle disease. These include single gene testing, genetic panel tests, targeted exome sequencing, whole exome sequencing, and mitochondrial genome testing. The technologies used for these evaluations are quickly evolving and beyond the scope of this review. However, in the discussion that follows, we will discuss recommendations for genetic testing in association with specific suspected conditions.
ACQUIRED CAUSES OF RHABDOMYOLYSIS
Alcohol and Illicit Substances
Several reports indicate that acute and/or chronic exposure to alcohol and illicit drugs may be a common trigger of rhabdomyolysis. In 1 study, 28 of 93 (30%) hospitalized patients with a CK >5000 U/L had a significant history of substance abuse16. In another series of 77 hospitalized patients with CK >500 U/L, 82% had a history of chronic alcoholism, acute alcohol intoxication, positive serum screen for drugs of abuse, and/or admitted drug use7. A large series of 475 patients with rhabdomyolysis included 163 (35%) cases caused by illicit drugs and/or alcohol4. In addition to acute and chronic alcohol intoxication29–31, there are reports of rhabdomyolysis induced by heroin32, cocaine33–35, and methamphetamine36, 37. Ecstasy (3,4-methylenedioxy-methamphetamine)38 and LSD (lysergic acid diethylamide)39–41 have been associated with acute-onset rhabdomyolysis in the setting of hyperthermia and muscle rigidity. Delayed-onset rhabdomyolysis has also been attributed to ecstasy abuse42. The increased risk of rhabdomyolysis with each of these substances has been attributed to direct toxic effect of the drug or contaminants, increased sympathomimetic stimulation, and/or nutritional deficiency in the setting of addiction. Given its prevalence, obtaining a history of substance use is a critical part of a rhabdomyolysis evaluation. Furthermore, since patients with rhabdomyolysis can present in an obtunded and comatose state as a result of toxic and metabolic exposures8, 29, 30, 43, clinicians should have a low clinical threshold to suspect rhabdomyolysis in this setting and screen for this condition by checking serum CK.
Prescription Medications
Prescription medications associated with rhabdomyolysis are numerous (see Table 1). Anti-psychotic medications that trigger the neuroleptic malignant syndrome are a notable cause of rhabdomyolysis in series of adults and children4, 44, 45 and in multiple case reports recently reviewed by Packard, et al.46. Among the psychiatric medications, antidepressants have also been associated with rhabdomyolysis47, 48. Although HMG Co-A reductase inhibitors (statin medications) are frequently associated with mild muscle complaints, rhabdomyolysis is extremely infrequent49, 50, probably occurring in just 0.4 per 10, 000 person-years51. Risk factors for muscle side-effects of statins, reviewed by Mammen, et al., are numerous and include advanced age, systemic or infectious illness, underlying hepatic disease, alcohol abuse, and major surgery52. Administration of statins in the setting of hypothyroidism also increases the risk of rhabdomyolysis53. Statin-related rhabdomyolysis risk may be increased markedly with co-administration of fibrates. A review of the FDA post-marketing database of rhabdomyolysis reports (CK ≥10,000) found that, of 866 cases reported between 1987 and 2001, 44% were related to combination therapy compared to statins alone18. Of note, some data suggest that there are fewer instances of rhabdomyolysis with a fenofibrate-statin combination than with a gemfibrozil-statin combination54. In addition, the risk of statin-induced rhabdomyolysis in patients taking CYP3A4-metabolized forms of this medication (e.g., simvastatin, atorvastatin and pravastatin) increases with co-administration of other CYP450 metabolized medications, including calcium channel blockers55, amiodarone56, macrolide antibiotics57, and HIV-protease inhibitors58. Of note, the risk of statin-triggered myopathy is particularly increased in patients with a single-nucleotide polymorphism located within the SLCO1B1 gene, which encodes a transport protein involved in regulation of hepatic statin uptake59.
Table 1.
Selected Medications Associated with Rhabdomyolysis
| Amino-caproic acid |
| Antidepressants |
| Tricyclic antidepressants |
| Venlafaxine |
| Sertraline |
| Escitalopram |
| Anti-histamines |
| Anti-psychotics |
| Aripriprazole |
| Clozapine |
| Haloperidol |
| Olanzapine |
| Risperidone |
| Quetiapine |
| Anti-retrovirals |
| Tenofovir/Abicavir |
| Raltegravir |
| Colchicine |
| Colchicine + clarithromycin |
| Colchicine + cyclosporine/tacrolimus |
| Daptomycin |
| Depakote |
| Interferon alpha |
| Lithium |
| Ofloxacin/Levofloxacin |
| Statins (increased risk with hypothyroidism, certain genetic polymorphisms, liver disease, and diabetes) |
| Statin + fibrates |
| Stain + CYP450 inhibitors |
| Statin + CYP3A4 inhibitors |
| Diltiazem/amiodarone/verapamil |
| Macrolide antibiotics (erythromycin/clarithromycin) |
| Protease inhibitors |
| Stiglaglipin |
| Colchicine |
| Statin + Daptomycin |
| Statin + Fluconazole |
| Statin + tacrolimus/cyclosporine |
Metabolic/Electrolyte/Endocrine Disturbance
Rhabdomyolysis can occur as a result of electrolyte abnormalities (hypokalemia, hypophosphatemia, hyponatremia, and hypernatremia) in the setting of endocrine diseases such as diabetes60–63, thyroid dysfunction64, 65, primary hyperaldosteronism66, primary adrenal insufficiency67, central diabetes insipidus68, postpartum hypernatremia69, and pituitary dysfunction70. Cases of rhabdomyolysis have also been attributed to electrolyte disturbances (primarily hypokalemia and hyponatremia) in the setting of laxative and diuretic misuse/abuse71–73. Rhabdomyolysis can be the presenting event in cases of inherited or acquired renal tubular dysfunction with profound hypokalemia, or it can be triggered by illness or discontinuation of medical treatment74, 75. These causes can be screened for with serum and urine electrolyte panels and studies of endocrine function.
Poisons/Toxins
Venoms, toxins, pesticides, and poisons are relatively rare causes of rhabdomyolysis. Venom from several snakes can cause rhabdomyolysis by direct myotoxicity and/or from muscle ischemia related to coagulopathy76, 77. Wasp stings78 and spider bites79 have also been associated with rhabdomyolysis. Ingestion of European quail that feed on hemlock seeds may cause rhabdomyolysis80. Haff disease, a rare sporadic syndrome of rhabdomyolysis, develops after eating Buffalo fish that are thought to contain an unidentified toxin81. Ingestion of certain mushroom species is also associated with rhabdomyolysis82, 83. Furthermore, pesticides and chemical poisonings can cause rhabdomyoysis15. Of note, patients with these toxic exposures often present with rhabdomyolysis as just 1 feature of widespread systemic illness. This highlights the importance of screening for rhabdomyolysis in suspected toxic exposure.
Autoimmune Myopathies
The autoimmune myopathies are a heterogeneous family of diseases, including dermatomyositis and polymyositis, characterized by muscle weakness, elevated CK levels, and lymphocytic infiltrates on muscle biopsy. Affected patients require immunosuppressive agents to control their disease. Although the onset of myositis is typically subacute, it may present acutely with typical features of rhabdomyolysis, including muscle pain and marked CK elevation. Indeed, autoimmune myositis has been described in a significant proportion of adult and pediatric rhabdomyolysis cases4, 84. As patients with myositis often have other systemic manifestations of autoimmunity, these features may help guide clinicians to the correct diagnosis. For example, the presence of heliotrope rash and/or Gottron papules, are pathognomonic for dermatomyositis85. Additional features of systemic autoimmunity seen in patients with dermatomyositis and polymyositis include arthritis, interstitial lung disease, and fever.
As noted above, we do not usually recommend muscle biopsy at the time of acute rhabdomyolysis presentation, since delaying biopsy allows muscle cells to regenerate and ensures that overwhelming necrosis does not obscure the underlying pathology indicative of certain inherited conditions. However, since rapid initiation of immunosuppressive therapy may be indicated in suspected myositis, biopsy may be required to confirm the presence of lymphocytic cellular infiltrates and/or perifascicular atrophy. Of note, patients with immune-mediated necrotizing myopathy may have prominent necrosis on muscle biopsy without inflammation, making a histologic diagnosis of an autoimmune process challenging. In these cases, testing for antibodies associated with autoimmune necrotizing myopathies (i.e., anti-signal recognition particle or anti-HMG-CoA reductase autoantibodies) may facilitate making the correct diagnosis.
GENETIC CAUSES OF RHABDOMYOLYSIS
If the history, physical exam, and initial laboratory evaluation do not reveal an acquired cause for rhabdomyolysis, then the possibility of an inherited susceptibility should be considered. Genetic conditions that predispose to rhabdomyolysis include metabolic myopathies, muscular dystrophies, and channelopathies. Many of these conditions are associated with exercise intolerance and exertional rhabdomyolysis. Although numerous distinct inherited muscle diseases are associated with rhabdomyolysis, the differential diagnosis may be restricted based on the precise clinical features. Thus, it is important to determine whether there is baseline muscle weakness, a history of exercise intolerance, or, if present, the pattern of exercise that precipitates rhabdomyolysis. Also, because muscle pain, weakness, and dark urine may not always be sufficiently severe to prompt consultation with a physician, it is important to ask the patient about a history of these symptoms. Although these are inherited conditions, a family history of exercise intolerance or rhabdomyolysis may not be elicited, because the majority of these conditions are autosomal recessive.
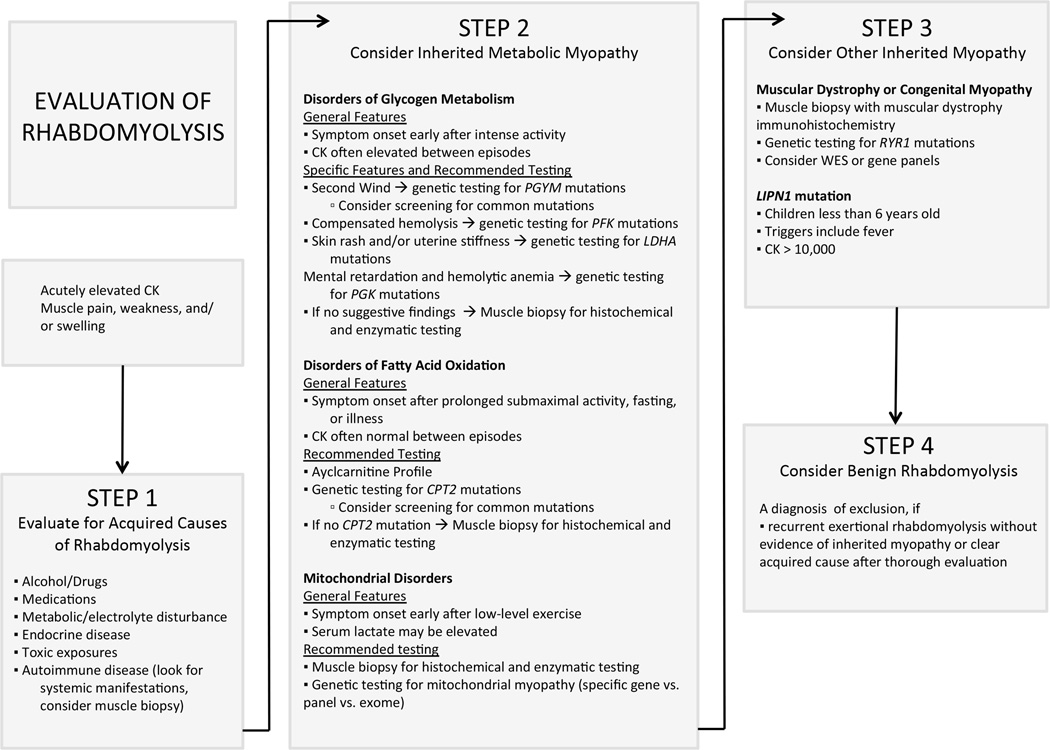
As discussed below, abnormalities in laboratory tests, muscle biopsy findings, and functional testing can be used further guide decision-making in the diagnostic evaluation of rhabdomyolysis. In cases where an inherited predisposition to rhabdomyolysis is suspected, specific clinical features should prompt the clinician to proceed to targeted genetic testing. Patients in whom there are non-specific clinical features, or in cases where initial genetic testing is inconclusive, we recommend muscle biopsy with enzyme immunohistochemistry and testing of glycolytic enzyme activity. Muscle biopsy investigations for diagnosis of rhabdomyolysis are listed in Table 2. Alternatively, if available, the clinician may pursue testing via an appropriate next generation gene panel or whole exome sequencing. A suggested approach to diagnosis is summarized in Figure 1.
Table 2.
Muscle Biopsy Investigations for Diagnosis of Rhabdomyolysis
| Glycogen Storage Disorders |
| Routine histochemistry to evaluate for PAS-positive vacuoles |
| Enzyme immunohistochemistry (muscle phosphorylase or PFK) |
| Direct testing of enzymatic activity on frozen muscle |
| Glycogen content and structure |
| Muscle phosphorylase activity |
| Phosphofructokinase activity |
| Lactate dehydrogenase activity |
| Phosphorylase b activity |
| Phosphoglycreate kinase activity |
| Phosphoglycerate mutase activity |
| Phosphoglucomutase activity |
| Fatty Acid Oxidation Disorders |
| Routine histochemistry to evaluate for abnormal lipid content |
| Muscle carnitine and acylcarnitine levels |
| Testing of enzymatic activity for beta-oxidation and carnitine transport |
| Mitochondrial Myopathies |
| Ragged-red fibers on Gomori Trichrome staining |
| Immunohistochemistry to evaluate COX and SDH activity |
| Electron microscopy to evaluate mitochondrial structure and distribution |
| Mitochondrial content and Co-enzyme 10 levels |
| Photometric evaluation of electron transport chain activity (fresh muscle is preferable) |
| Oxidative phosphorylation activity of complexes I-V (fresh muscle only) |
| Genetic testing for mutations in mitochondrial DNA in muscle tissue) |
| Autoimmune myopathies |
| Dermatomyositis |
| Routine histochemistry: perifascicular atrophy (pathognomonic) and perivascular inflammation |
| Polymyositis/Inclusion body myositis |
| Routine histochemistry: non-necrotic myofibers surrounded and invaded by inflammatory cells and/or rimmed vacuoles |
| Muscular dystrophies |
| Features of necrotizing myopathy |
| Fibrosis |
| Increased internalized nuclei |
| Degeneration and regeneration |
| Abnormal immunohistochemistry for dystrophin, sarcoglycans, dysferlin, fukutin, or anoctamin-5 |
| RYR1-related myopathy |
| Immunohistochemistry demonstrating central cores or multiminicores on NADH, COX, SDH stains |
Figure 1.
A diagnostic algorithm for patients with rhabdomyolysis.
Metabolic Myopathies Associated with Rhabdomyolysis
Muscle energetics and metabolic myopathies
Metabolic myopathies associated with rhabdomyolysis can be differentiated by several features which are summarized in Table 3. Various types of exercise, fasting, fever, and illness are important triggers of rhabdomyolysis, and these patterns can be helpful in narrowing the differential diagnosis for metabolic myopathies.
Table 3.
General characteristics of metabolic diseases associated with rhabdomyolysis. Symptoms of muscle injury include muscle pain, cramping, weakness, and fatigue.
| Metabolic Category |
Typical Triggers | Interictal CK Level |
Interictal Weakness |
Muscle biopsy Features |
|---|---|---|---|---|
| Glycogen storage disorders | Onset early after intense exercise or isometric activity | Elevated | More likely in adults | Increased glycogen, subsarcolemmal PAS-positive vacuoles |
| Fatty Acid Oxidation Disorders | Onset later after prolonged submaximal activity, or in setting of fever, fasting or illness. | Normal | Rare | Increased lipid content |
| Mitochondrial Disorders | Onset early or later after submaximal activity or leisurely activity, or in the setting of fasting fever or illness | Normal or elevated | Possible | Mitochondrial proliferation and/or abnormal lipid content |
During physical activity, muscle contraction and relaxation rely upon a constant source of ATP. When exercise continues in the absence of adequate ATP production, muscle damage and rhabdomyolysis may result. A framework for understanding metabolic myopathies (and formulating a differential diagnosis) requires a brief explanation of energy sources available to and required by the muscle during different modes of activity19, 20.
In the fed state, at rest, and with low-intensity or prolonged activity, the primary source of energy for muscle is fatty acid metabolism. Therefore, disorders of fatty acid metabolism present after prolonged submaximal activity and during periods of fasting or illness, when the main source of energy is through fatty acid beta-oxidation. After initiation of moderate-intensity exercise, muscle first utilizes free glucose from the blood and glucose derived primarily from liver glycogen stores before switching to fatty acid metabolism. During maximum-intensity bursts of activity or during isometric contraction, muscle relies on anaerobic metabolism with breakdown of muscle glycogen to glucose and ultimately to pyruvate. Thus, disorders affecting muscle glycogen metabolism cause muscle symptoms and injury early in association with intense or isometric activity. ATP production via oxidative phosphorylation requires a supply of oxygen. Thus, disorders of mitochondrial oxidative phosphorylation present when aerobic metabolic pathways predominate.
Disorders of Glycogen Metabolism
Enzymes involved in the metabolism of glycogen to glucose and glucose to pyruvate are relatively frequent targets of mutations in patients with an inherited predisposition to rhabdomyolysis. In patients with dysfunctional glycogen metabolism, rhabdomyolysis most characteristically occurs early after onset of moderate to intense activity, short bursts of intense activity, and isometric activity. Many patients also have elevated CK levels between rhabdomyolysis episodes. Characteristic diagnostic features of disorders of glycogen metabolism are listed in Table 4. Below, we discuss characteristics of several individual disorders of glycogen metabolism in detail.
Table 4.
Characteristic Diagnostic Features of Disorders of Glycogen Metabolism
| Disorder of Glycogen Metabolism |
Inheritance | Non-ischemic Forearm Exercise Test Response. |
Multisystem Infolvement and Other Characteristic Features |
|---|---|---|---|
| Muscle Phosphorylase Deficiency | Recessive | Inadequate lactate | Second-wind phenomenon |
| Phosphofructokinase Deficiency | Recessive | Inadequate lactate | Hemolysis |
| Phosphoglycerate Kinase Deficiency | X-linked | Inadequate lactate | Hemolysis Encephalopathy |
| Lactate Dehydrogenase Deficiency | Recessive | Inadequate lactate Excessive pyruvate | Uterine stiffness in pregnancy Seasonal rash |
| Phosphoglucomutase Deficiency | Recessive | Normal lactate, Excessive ammonia | Hepatopathy Bifid uvula |
| Phosphorylase b Deficiency | X-linked | Normal lactate | |
| Phosphoglycerate Mutase Deficiency | Recessive | Normal lacate | Muscle biopsy with tubular aggregates |
Muscle phosphorylase deficiency
This condition is caused by a mutation in the muscle phosphorylase gene PYGM. PYGM encodes a muscle-specific enzyme that converts glycogen to glucose during periods of anaerobic exercise. The prevalence of pathologic mutations in this gene is approximately 1 in 100,00086. Symptom onset typically occurs in childhood to adolescence with muscle pain, cramping, and stiffness,87 often within minutes after onset of intense activity. If the activity level is maintained after symptoms begin, severe muscle contractures occur, and about half of patients develop rhabdomyolysis88–90.
The characteristic clinical feature of muscle phosphorylase deficiency, which differentiates it from the other glycogen storage diseases, is the “second wind phenomenon.” This phenomenon is characterized by resolution of fatigue and pain with rest for a few minutes after onset of symptoms, and is caused by recruitment of free circulating glucose brought on by glycogenolysis in organs other than muscle91. After this rest period, patients are able to resume activity. The second wind phenomenon is experienced by the majority of patients, as many as 86% in a Spanish series of 239 cases90.
In a case series of 32 patients reported by Aquaron, et al. the majority (30/32) had elevated CK at rest, and a minority (7/32) had weakness89. In the Martin, et al. series of 54 patients with phosphorylase deficiency, the findings were similar: fixed weakness was seen in 14/54 patients, all of whom were older than age 40 years88. On the FET, most patients have an absent lactate response, and a small group have an inadequate lactate response, reflecting partial enzyme activity. Typical muscle biopsy findings include myopathic features, increased glycogen accumulation on PAS-staining, and absence of immunohistochemical muscle phosphorylase staining87.
Muscle phosphorylase deficiency is the most commonly reported of the glycogen metabolic disorders. Therefore, when rhabdomyolysis is triggered by short-duration, high-intensity exercise, the patient gives a history of the second wind phenomenon, the CK is elevated at baseline, and interictal strength is normal (at least in younger patients), we recommend proceeding directly to genetic testing to confirm the diagnosis. Of note, different mutations are common among individuals of different ethnic backgrounds. In individuals of European, U.S, and Spanish descent, nonsense mutation pArg50* is seen in over 50% of patients88–90. In a smaller series of patients in Japan, the pArg50* mutation was not observed92.
Phosphofructokinase (PFK) deficiency
Mutations in the PFKM gene, which encodes a glycolytic enzyme that catalyzes the phosphorylation of fructose 6-phosphate to fructose 1, 6 bisphosphate, cause PFK deficiency. This rare autosomal recessive condition was first described in 3 Japanese siblings with easy fatigability and onset of weakness and stiffness provoked by vigorous or prolonged exertion; one sibling developed myoglobinuria93.
Muscle symptoms, especially exercise intolerance, often occur first in childhood. Many patients, however, do not present until adulthood because of the mild nature of the condition94. Rhabdomyolysis is rare93, 95. Interestingly, these patients tend to feel more fatigued prior to or during exercise after a high carbohydrate meal, because use of free glucose from the blood is blocked96. In fact, they may have better exercise performance in fasting states or with increased circulating free fatty acids, as they are able to use this fuel during oxidative exercise96. Affected patients typically have elevated CK levels at baseline, but weakness is rare, particularly in patients under age 50 years97–100. There is typically absent or subnormal increase in lactate on the IET101. The muscle biopsy can show mild myopathic features, and PAS-positive vacuoles may be present. PFK enzyme immunohistochemistry shows decreased or absent PFK activity. Although the muscle PFK isoform is expressed in cardiac myocytes, a mild hypertrophic cardiomyopathy has been described in only 1 patient101.
Muscle PFK is composed of 4 muscle subunits, and red blood cell PFK contains 2 of 4 muscle subunits. Thus, a unique feature of phosphofructokinase deficiency is compensated hemolysis, which can be exacerbated in situations that worsen muscle symptoms102. This is associated with a baseline reticulocytosis and hyperuricemia in most patients.
Thus, for the patient with exercise-induced rhabdomyolysis who gives a history of exercise intolerance, no second wind phenomenon, elevation of resting CK, and laboratory evidence of compensated hemolysis, we recommend proceeding directly to genetic testing for mutations in the PFKM gene.
Muscle lactate dehydrogenase (LDH) deficiency (OMIM #612933)
Muscle LDH deficiency is a recessive condition caused by mutations in the LDHA gene (OMIM 612933) that disrupt the ability of the enzyme to interconvert pyruvate and lactate. The first cases were described in Japan24, 103, but the condition has also been described in Caucasians104, 105. The condition is characterized by onset of muscle pain, stiffness, and cramping in the setting of strenuous activity; one child had first onset of symptoms during a 100-meter dash at age 9 years106. Exertional pigmenturia is a frequently reported symptom, and there are several reports of rhabdomyolysis with renal failure104, 106, 107.
Resting CK levels are usually elevated24, 104, 106, 107. Following exercise, there is a large increase in CK, but a smaller than expected increase in serum LDH106, 107; this biochemical discrepancy is a unique feature of muscle LDH deficiency. The FET shows an absent or inadequate lactate response along with an exaggerated increase in pyruvate levels24. Muscle biopsy pathology is infrequently described, but nonspecific myopathic changes have been described104.
There are 2 unique clinical features of patients with muscle LDH deficiency. First, some women experience only mild exercise intolerance but develop prominent uterine stiffness during pregnancy that requires delivery by Cesarean section106, 108. Second, muscle LDH deficiency has been associated with an erythematous rash on the extensor surfaces of the extremities which worsens during the summer105, 109, 110.
Thus, in a patient with rhabdomyolysis in the context of strenuous activity, no second wind phenomenon, the presence of a seasonal erythematous rash on extensor surfaces, or uterine stiffness during pregnancy genetic testing for LDH deficiency is suggested.
Muscle phosphorylase b kinase deficiency
Muscle phosphorylase b kinase deficiency is associated with mutations in the PHKA1 gene, located on the X chromosome; this enzyme encodes the muscle-specific isoform of the regulatory alpha-subunit of phosphorylase b kinase. This is a cAMP-dependent protein kinase composed of 4 subunits that catalyzes phosphorylation and activation of myophosphorylase. Despite its role in activation of myophosphorylase, this condition presents slightly differently from myophosphorylase deficiency111–122. Patients present in childhood or as young-adults with exercise-induced muscle pain and cramping. Some have intermittent exercise-induced pigmenturia. Unlike those with myophosphorylase deficiency, contracture in response to strenuous or prolonged exercise is not reported commonly, and there is no second wind phenomenon. Furthermore, there are no reports of severe rhabdomyolysis with acute renal failure. The majority of patients are male, but early childhood hypotonia without hepatic features was described in 2 girls with phosphorylase b kinase deficiency111, 112.
There are a few biochemical features to help to distinguish phosphorylase b kinase deficiency from other muscle glycogen storage diseases. The baseline CK level may or may not be elevated123. In the FET, there is typically a normal rise in lactate and ammonia121, 123. During submaximal cycling exercise testing in 1 patient with known PHKA1 mutation, lactate failed to increase to the same degree as controls121, suggesting that abnormality of phosphorylase b kinase activity is more disruptive to glycogen metabolism and energy production during submaximal dynamic exercise than on strenuous isometric exercise120.
There are several reports of patients with muscle phosphorylase b kinase deficiency due to mutations in the PHKA1 gene,115, 116, 118, 119, 121, 122. Two features, however, suggest that the protein dysfunction causing muscle phosphorylase b kinase deficiency extends beyond mutations in PHKA1 and other genes encoding subunits of muscle phosphorylase b kinase protein. PHKA1 is found on the X-chromosome, and, while a majority of patients described with deficient phosphorylase b kinase activity in the muscle biopsy are male, there are several reports of affected females111, 112, 124 suggesting autosomal inheritance in some patients. Additionally, when Burwinkel, et al screened 6 patients with reduced muscle phosphorylase b kinase activity for mutations in 8 genes encoding components of the enzyme, only 1 mutation in 1 gene, PHKA1, was found in a single patient118.
Because the genetic causes of decreased muscle phosphorylase b kinase activity are not fully defined, we recommend muscle biopsy with enzyme testing in suspected cases.
Phosphoglycerate kinase deficiency (OMIM# 300653)
Phosphoglycerate kinase deficiency is an X-linked disorder caused by a mutation in the PGK1 gene (OMIM 311800), which encodes the enzyme catalyzing the final step in the glycolytic pathway with formation of 3-phosphoglycerate and ATP. There is a brain isozyme and a muscle isozyme. An intermediate isozyme composed of both subunit types is expressed variably in other tissues, but deficiency of this isozyme manifests most frequently in red blood cells as hemolytic anemia. Reports of isolated myopathies with decreased phosphoglycerate kinase activity are rare125–129. Most cases of PGK deficiency manifest with 1 or more combinations of myopathy, encephalopathy, and/or hemolytic anemia. The combination of epileptic encephalopathy and myopathy can manifest as rhabdomyolysis presenting after seizures130. Patients with rhabdomyolysis have similar characteristics of childhood exercise intolerance with painful muscle cramps. Pigmenturia is seen in almost all patients. Rhabdomyolysis with acute renal failure has been described125, 126, 130.
Biochemically, affected patients share common features with other muscle glycogen storage disorders125–129. Resting CK may be normal or elevated. The FET induces early fatigue with cramping, and there is absent or inappropriately low rise in lactate. The muscle biopsy can be normal or show vacuoles containing PAS-positive material. As in PFK deficiency, blood testing may reveal the presence of a hemolytic anemia. Although the presence of encephalopathy or an X-linked inheritance pattern would suggest the former, distinguishing between phosphoglycerate kinase and phosphofructokinase deficiency may be difficult. If clinically suspected, we recommend either genetic testing for both diseases or performance of a muscle biopsy with PFK immunohistochemistry and muscle enzyme testing.
Phosphoglycerate mutase deficiency
Phosphoglycerate mutase deficiency is caused by a mutation in the PGAM2 gene, which encodes an enzyme that catalyzes conversion of 3-phosphoglycerate (3PG) to 2-phosphoglycerate (2PG). The first case described in 1981 was a 52 year old man with adolescent-onset muscle pain, stiffness, weakness, and pigmenturia after strenuous activity131. In subsequent reports, most patients present with muscle pain, contracture, and myoglobinuria after strenuous exercise132–140. The majority of patients described so far are of African American descent.
Baseline CK levels are often elevated. The FET shows slightly reduced or normal lactate elevation. Muscle biopsy can show increased glycogen content with PAS positive subsarcolemmal vacuoles, or it can be normal. Tubular aggregates are sometimes seen on muscle biopsy139, 141.
As with other patients who do not have unique distinguishing features of a particular metabolic myopathy, these patients may be diagnosed by muscle biopsy, including enzymatic testing. Alternatively, sending an appropriate gene sequencing panel or whole exome sequencing may be used to facilitate diagnose.
Phosphoglucomutase deficiency
Phosphoglucomutase deficiency is an autosomal recessive condition caused by a mutation in the PGM1 gene, which encodes an enzyme that catalyzes the transfer of phosphate between the 1 and 6 positions of the glucose molecule. The first case report of phosphoglucomutase was of a 35 year-old man with recurrent activity-induced muscle cramping and pigmenturia associated with strenuous exercise142. He had an elevated resting CK level, a myopathic EMG, and an FET showing a normal lactate response with excessive ammonia elevation. His muscle biopsy showed subsarcolemmal vacuoles containing normally structured glycogen and decreased phosphoglucomutase activity. Thereafter, a mutation was confirmed in the PGM1 gene.
More recently, Tegtmeyer, et al. identified 19 individuals from 16 families with mutations in the PGM1 gene143. At birth, a bifid uvula was present in just over 80% of the patients. Later, all patients developed hepatopathy. Exercise intolerance with recurrent rhabdomyolysis was reported in about half of patients. Malignant hyperthermia with severe rhabdomyolysis occurred in 2 patients. The authors concluded that mutations in PGM1 cause both a glycogen storage disorder and a mixed-type disorder of congenital glycosylation. Resting CK levels and FET results were not described.
Thus, phosphoglucomutase deficiency is a rare condition with rhabdomyolysis that can occur as an isolated feature or together with hepatopathy. The presence of a bifid uvula, which was not reported in the patient described by Stojkovic, et al., may prompt one to perform genetic testing for mutations in PGM1. Otherwise, unless a gene panel or whole exome sequencing is readily available, muscle biopsy with enzymatic testing may be the most efficient way of diagnosing this disease.
Disorders of Fatty Acid Oxidation Associated with Rhabdomyolysis
Mutations in enzymes involved in the metabolism of fatty acids and transport of acyl-CoA conjugated fatty acids across the mitochondrial membrane are a cause of rhabdomyolysis often triggered by prolonged submaximal activity, fasting, stress, and/or illness. Other characteristic features of these diseases include a normal baseline CK level, acylcarnitine abnormalities, and muscle biopsies showing evidence of a lipid storage myopathy. It should be noted that patients who are not in a catabolic state may not show the specific abnormalities which indicate the underlying fatty acid oxidation disorder.
Carnitine palmitoyltransferase II (CPTII) deficiency
CPTII is a protein located in the mitochondrial inner membrane that functions (along with CPTI located in the outer mitochondrial membrane) to transfer acyl-CoA-conjugated long chain fatty acids from the cytosol into the mitochondrial matrix for beta-oxidation. Mutations in the CPT2 gene,are the most common cause of rhabdomyolysis due to fatty acid oxidation disorders144. The condition manifests in late childhood to early adolescence and, for unknown reasons, more commonly in males145, 146. Typically, prolonged muscle exercise causes weakness, pain, cramping, and pigmenturia; these symptoms may also be precipitated by cold, fasting, illness, or emotional stress145–148. In younger children, rhabdomyolysis is more likely to be due to illness or fasting and may be accompanied by encephalopathy and non-ketotic hypoglycemia147. Valproic acid149 and anesthesia150 have also been identified as triggers. In contrast to the glycogen storage diseases, which may affect the exercised muscle in isolation, CPTII deficient patients may experience diffuse weakness. Consequently, monitoring for respiratory failure is necessary in severe rhabdomyolysis in CPTII deficiency148, 151. Furthermore, up to 30% of patients may develop acute renal failure due to rhabdomyolysis146, 148.
Despite potentially severe weakness when in crisis145, 146, the majority of patients with recurrent rhabdomyolysis have normal CK levels and neurological examinations between episodes151; elevated baseline CK levels were reported in just 10% of patients in 1 series152. Anchichini, et al. reviewed the muscle biopsies from 23 patients and found that typical histopathological findings include internalized nuclei (91%), type 2 fiber prevalence (65%), and lipid droplets (40%)145. On FET, lactate and ammonia responses are normal151. Elevation of plasma long-chain acylcarnitine species, particularly C16:0 and C18:1, on mass spectrometry strongly suggests CPTII deficiency153. In CPTII deficiency, no significant difference was noted in acylcarnitine profile testing between symptomatic and asymptomatic patients, and interictal acylcarnitine profile abnormalities may not be apparent if the patient is metabolically stable and well-rested145.
In patients with suggestive clinical features of CPTII deficiency, we recommend genetic screening for common CPT2 mutations (p.S113L and p.P50H in addition to several others)145, 146, 148. Normal C16:0 and C18:1 acylcarnitine levels should not necessarily preclude genetic testing if the clinical suspicion for a CPT2 mutation is high. If common mutation screening does not confirm the cause, full sequencing of the gene should be considered. If gene testing is inconclusive, muscle biopsy may be performed to check for CPTII activity by radioisotope assay154, 155. Finally, it should be noted that heterozygous carriers of CPT2 mutations can manifest with subtle symptoms due to a partial inability to metabolize long-chain fatty acids156.
Other fatty acid oxidation disorders
Intra-mitochondrial fatty acid oxidation can be impaired by mutations in the acyl-coA dehydrogenases. The most commonly described is very long-chain AcylCoA dehydrogenase deficiency (VLCAD). In a case series of 13 patients with VLCAD, the onset of muscle symptoms was typically in mid-to-late childhood with symptoms of exercise intolerance and recurrent pigmenturia triggered by activity, cold-exposure, or fasting157. Younger patients may manifest with hepatopathy or cardiomyopathy and recurrent hypoglycemia. Rhabdomyolysis with acute renal failure has been reported. These patients have normal interictal CK levels and muscle strength. Muscle biopsy can show mitochondrial proliferation and/or increased lipid content, especially in type I myofibers157.
Mutations with similar clinical presentations are described with mitochondrial tri-functional protein (MTP) deficiency, in which mutation causes decreased long-chain 3-hydroxyacylCoA dehydrogenase (LCHAD) activity158–160. Patients with the adult onset form of this disease are rare, but they present with exercise intolerance, recurrent pigmenturia, and often with a length-dependent axonal sensory-motor neuropathy. Long-chain and 3-hydroxy long-chain acylcarnitine species may be elevated. Medium chain acyl-CoA dehydrogenase (MCAD) deficiency is a rare cause of recurrent rhabdomyolysis and is usually with associated encephalopathy161.
Mitochondrial Myopathies Associated with Rhabdomyolysis
Mutations in components of the mitochondrial respiratory chain that impair oxidative phosphorylation and ATP production may cause multisystem disease, sometimes including skeletal muscle. However, we emphasize only those mitochondrial disorders that have been associated with rhabdomyolysis.
Intact mitochondrial function and respiratory chain activity is necessary for aerobic and anaerobic exercise. Consequently, muscle symptoms may occur early with strenuous exercise or later after relatively low levels of activity. Patients often report excessive fatigue out of proportion to weakness. CK and lactate levels can be elevated or normal.
In rhabdomyolysis patients with suspected mitochondrial myopathy based on clinical features (e.g., other organ system involvement, external ophthalmoplegia, etc) or maternal inheritance pattern, muscle biopsy is often performed to confirm mitochondrial dysfunction. Ragged red fibers (RRF), which represent muscle cells with increased subsarcolemmal accumulations of mitochondria, are one of the most common histological abnormalities associated with mitochondrial diseases, and muscle fibers with absent cytochrome oxidase activity, known as COX-negative fibers, are also suggestive of mitochondrial disease162, 163. In healthy individuals, COX-negative fibers and RRF numbers increase with age164. Based on the modified Walker criteria for mitochondrial disease165, greater than 2% RRF is considered abnormal at any age. For COX-negative fibers, a number greater than 2% is considered abnormal in patients less than age 50 years. At ≥ age 50 years, the presence of greater than 5% COX-negative fibers is considered abnormal. Importantly, RRF and/or COX negative fibers may be increased in patients with other conditions, including autoimmune myopathy166, occulopharyngeal muscular dystrophy167, or myasthenia gravis168. Thus, the clinical history and additional features seen on the muscle biopsy are important in determining the significance of RRF and COX-negative fibers.
After muscle biopsy, testing of respiratory chain enzyme activity can be performed. As with interpretation of the histopathological features, it is important to recognize that reduced activity may be due to primary or secondary mitochondrial abnormalities169. If muscle biopsy reveals evidence of mitochondrial disease, but respiratory enzyme activity analysis does not reveal the specific deficiency, genetic testing may be considered. It is important to recognize that disorders of mitochondrial function can arise from mutations in either the mitochondrial or nuclear genomes. When caused by mutations in nuclear DNA, mitochondrial disease may be inherited in either an autosomal dominant or recessive pattern. Mitochondrial genome mutations are transmitted maternally and can result in heteroplasmy, whereby some cells or organs contain a higher burden of mutant mitochondrial genomes than others. Because of this phenomenon, muscle tissue as the source of mitochondrial DNA will have the highest yield in patients with muscle symptoms such as rhabdomyolyis169.
Coenzyme Q10 deficiency was first described in 2 sisters with onset of early exertional fatigue beginning in childhood and episodic rhabdomyolysis170. These sisters, and other described patients, also had encephalopathy, ataxia, and/or progressive proximal weakness. Some patients with coenzyme Q deficiency have seizure disorders with recurrent rhabdomyolysis following convulsions170–172. Illness may also be also a provoking factor170. The patients have elevations in venous lactate and lactate/pyruvate ratio.
Cytochrome c mutations have been reported in patients with adult-onset rhabdomyolysis. This was triggered in 1 patient by walking and, in another patient, symptoms began 3 hours after heavy lifting173, 174. Another patient developed muscle pain and pigmenturia first with a viral illness and a second time after exercise175.
Cytochrome b mutation has been associated with rhabdomyolysis in a patient with late-childhood onset fatigue and pain with exercise176. He experienced rhabdomyolysis after shoveling snow and subsequently developed progressive muscle weakness. The lactate level was chronically elevated. Baseline CK level was normal.
COX I mutation has been reported in a patient with childhood onset of exercise intolerance, especially with endurance activities177. He developed recurrent rhabdomyolysis at age 22 years. The resting lactate and CK levels were normal.
Mitochondrial DNA tRNA mutations are also described in association with rhabdomyolysis. For example, a 36 year-old woman with recurrent rhabdomyolysis triggered by intense exercise was found to have a mutation in the tRNA-isoleucine gene178. Another mutation in the tRNA-leucine gene (identical to a mutation described in MELAS) was reported in a 65-year-old woman with recurrent rhabdomyolysis triggered by dehydration or minor trauma179.
Mutation in the MT-CO2 gene was described recently in an adult man with onset of exercise intolerance and recurrent rhabdomyolysis in childhood180. He had mild weakness on exam at age 43 years. Resting CK was normal, and resting lactate was normal or elevated.
Structural Myopathies
Although patients with structural myopathies typically present with progressive muscle weakness as the most prominent muscle feature, some patients with these disorders may also experience rhabdomyolysis.
Dystrophinopathy
Several case reports and small series describe patients with dystrophin gene mutations and exercise- induced rhabdomyolysis. Not all cases specifically describe the activities provoking the episodes. In 3 cases described by Figrella-Branger, et al., the baseline CK level was elevated, and EMG was normal. One of the patients had both calf hypertrophy and dilated cardiomyopathy at the age 21 years181. The muscle biopsies of all 3 patients revealed absent immunohistochemical staining to the Dys 1 antibody, which labels the rod domain. Two additional patients with recurrent rhabdomyolysis after prolonged exercise were found to have an identical mutation in exon 15 of the dystrophin gene182. These patients may be more likely to have baseline weakness on physical examination.
LGMD2I
Five patients with limb-girdle muscular dystrophy 2I (LGMD2I) and exercise-induced rhabdomyolysis were found to have identical mutations in the FKRP gene encoding fukutin-related protein183. Onset of muscle pain and cramping after activity was reported during late childhood, adolescence, and early adulthood. Baseline CK was markedly elevated, and patients who experienced rhabdomyolysis developed baseline weakness.
Dysferlinopathy
A patient without previous history of exercise intolerance was found to have a mutation in the dysferlin gene, following presentation with rhabdomyolysis at age 15 years184. He had no weakness, but his baseline CK remained elevated, prompting muscle biopsy. The muscle biopsy showed a necrotizing myopathy with severe type 2 fiber predominance. Immunohistochemical staining revealed absent dysferlin.
Ano-5 myopathy
Exercise intolerance with muscle pain and myoglobinuria is described in association with mutation in the anoctamin-5 gene185, 186. Baseline CK levels were elevated. In a patient with exercise intolerance and muscle pain, the muscle biopsy is described as a mild necrotizing myopathy with congophilic deposits of amyloid in some myofibers186.
Sarcoglycanopathy
A 5-year old boy developed rhabdomyolysis associated with infection and was later diagnosed with alpha-sarcoglycan deficiency187. Another boy had onset of easy fatigability and was found to have elevated CK levels at age 8 years, prompting muscle biopsy with normal metabolic evaluation and normal genetic testing for dystrophinopathy188. Subsequent episodes of recurrent rhabdomyolysis led to repeat muscle biopsy, which showed reduced alpha-sarcoglycan staining on immunohistochemistry. Exercise-induced recurrent rhabdomyolysis was also described in a 12 year-old boy with beta-sarcoglycanopathy189. All patients had elevated baseline CK levels.
FHSD
In a series of 122 cases of fascioscapulohumeral muscular dystrophy (FSHD), 1 patient was described with myoglobinuria190.
Channelopathies
RYR1 gene mutations have historically been associated with central core disease, multiminicore disease, and malignant hyperthermia191, 192. More recently, Dlamini, et al describe 24 patients from 14 families with exercise intolerance and/or rhabdomyolysis who were found to have mutations in RYR1193. Fifteen of 24 patients presented with rhabdomyolysis, and 10 had recurrent episodes. The most common trigger was exercise, but events were also triggered by heat exposure, illness, and alcohol consumption. Mild proximal weakness was detected in 5 of 24 patients, and ptosis was present in 2 families. Interval CK levels were normal in most patients. Muscle stiffness in response to cold was described by 3 patients. In the available muscle biopsies from 15 patients, most showed fiber size variability, increased internalized nuclei, type 1 fiber predominance, and core-like areas on oxidative stains. The link between exertional heat stroke, rhabdomyolysis, and susceptibility to malignant hyperthermia has not been characterized fully194, 195.
SCN4A gene mutation was recently discovered in an 8 year-old girl with recurrent rhabdomyolysis triggered by emotional stress, exercise, and infection196. Baseline CK levels between the attacks were normal or mildly elevated. Her examination showed proximal weakness and mild thenar percussion myotonia. The EMG showed myotonic discharges. On her muscle biopsy, she had a non-vacuolar necrotizing myopathy.
Lipin-1
Mutations in the LPIN1 gene have been recently described in pediatric patients with recurrent rhabdomyolysis. The LIPN1 gene encodes Lipin-1, a phosphatidate phosphatase which is important for triacylglycerol and phospholipid biosynthesis and acts as a transcriptional co-activator. It was first described in 3 related healthy children with recurrent rhabdomyolysis triggered by febrile illness197. The children had normal CK and strength between episodes. In this original description, 22 other children with recurrent rhabdomyolysis were screened, and 4 additional cases with similar characteristics were identified. Muscle biopsies showed increased lipid content in 2 muscle biopsies, and the others were normal.
Michot, et al. screened a group of 29 patients under age 5 years with recurrent rhabdomyolysis and CK levels > 10,000 U/L and found homozygous or compound heterozygous LPIN1 mutations in 59%198. The average age was 21 months. Fever and/or fasting were the triggering factors in all patients in whom a trigger was reported. In 3 patients, fever, fasting, and local anesthesia were reported to be triggers. One patient developed rhabdomyolysis following exposure to general anesthesia.
In another series, which included a subset of patients with recurrent severe rhabdomyolysis (CK > 10,000 U/L) where the first episode occurred at < age 6 years, there was a LPIN1 mutation in 37% and in 19% of patients with severe rhabdomyolysis in adult and pediatric age groups198. LPIN1 mutations were not found in other patients in the series with mild rhabdomyolysis (CK < 10,000) or patients with myalgias. Episodes of rhabdomyolysis in the Lipin-1 patients were triggered most frequently by febrile illness and less frequently by intense exercise, anesthesia, or fasting. Six patients had mild proximal weakness. Six other patients died of cardiac arrhythmia, which was attributed to possible hyperkalemia. Forty percent of heterozygotes report exercise-induced myalgia or cramping. Three adults with heterozygous mutations in LPIN1 have been described with statin-induced myopathy197.
Sickle Cell Disease
In patients with homozygous sickle cell disease (HgSS), rhabdomyolysis can occur in the setting of intravascular coagulation in sickle cell crisis; this may be triggered by stress, illness, metabolic acidosis, and/or dehydration199. Rhabdomyolysis with acute renal failure, and sometimes sudden death, is reported in athletes (often football players) and military recruits with heterozygous sickle cell (HgSc) trait following intense exertion or heat illness200–203.
“Benign Exertional Rhabdomyolysis”
A condition known as “benign exertional rhabdomyolysis” has been described in otherwise healthy people who develop muscle pain, elevated CK levels, and/or pigmenturia following intense exercise. This has been documented particularly well in military recruits undergoing basic training. Similar elevations in CK and/or myoglobin have also been described in asymptomatic ice skaters and marathon runners204, 205. Of note, individuals in better physical condition and with lower BMI show a smaller degree of post-exercise increase in CK levels compared to unconditioned athletes206–208. Also, serum CK levels rose higher following high-intensity exercise than for moderate-intensity exercise on a treadmill206. There may be some influence of race and gender, as baseline and post-exercise CK levels have been shown to be elevated in men compared to women209 and in blacks compared to whites209, 210. In one study of exertional rhabdomyolysis, men were 4.1 times more likely to have had exertional rhabdomyolysis than women211. Interestingly, when CK levels are followed in all basic training participants, some recruits remain asymptomatic despite CK elevations that are associated with muscle symptoms in other individuals208, 210, 212.
Emerging evidence suggests that certain genetic factors influence the likelihood of developing benign exertional rhabdomyolysis. For example, single nucleotide polymorphisms in CKMM (CK muscle isoform), ACTN3 (alpha Actinin-3), and MYLK2 (myosin light chain kinase) have been associated with this condition211, 213. However, in some cases of exertional rhabdomyolysis, no acquired or genetic cause can be identified despite extensive evaluation. In the opinion of the authors, many of these individuals probably have other, unidentified, genetic susceptibility for exertional rhabdomyolysis.
CONCLUSION
When patients present with symptoms of muscle pain, cramping, and/or pigmenturia (especially in the context of exertion, fasting, or illness) the finding of an elevated CK level during or immediately after an acute episode indicates that the symptoms are most likely due to rhabdomyolysis.
Once the diagnosis of rhabdomyolysis is established, the physician should inquire about previous episodes, other affected family members, medication exposure, illicit drug use, and alcohol history. Important initial laboratory assessments include electrolyte analysis, toxicology screening, and thyroid function tests to look for evidence of acquired, and treatable, causes of rhabdomyolysis. In the acute phase, we do not recommend a muscle biopsy unless autoimmune myopathy is considered in the differential diagnosis and immunotherapy would be indicated. Rather, we prefer to defer diagnostic muscle biopsies for at least a month (and preferably longer) after an episode of acute rhabdomyolysis.
Figure 1 summarizes a diagnostic approach in the evaluation of rhabdomyolysis. If no acquired cause of rhabdomyolysis is identified, we suggest attempting to categorize the patient into 1 of 4 groups to help guide subsequent testing for inherited muscle disease:
Glycogen storage disease. In these patients rhabdomyolysis is often triggered by short periods of intense exercise, often accompanied by pain and cramping; contractures may occur with prolonged strenuous activity or isometric exercise; baseline CK level may be elevated.
Disorders of fatty acid metabolism. Symptoms of pain and cramping are triggered by prolonged low-to-moderate intensity activity; contractures are not a prominent feature; the CK is often normal between episodes.
Mitochondrial myopathy. Muscle symptoms are triggered soon after exercise and/or after prolonged activity; excessive and early fatigue is a major complaint. The interictal CK level can be normal or abnormal; elevated lactate level or lactate/pyruvate ratio may be found.
Structural muscle disease. Symptoms of pain and cramping are triggered by prolonged low-to-moderate intensity activity; contractures are not a prominent feature; the CK is typically elevated between episodes.
If patients easily fit into 1 of the first 2 groups, and especially if they have some very characteristic feature of a specific disease (e.g., the second wind phenomenon in myophosphorylase deficiency), then genetic testing may be considered without performing a muscle biopsy. If genetic testing is unsuccessful, a muscle biopsy should be performed followed by appropriate histologic, immunohistochemical, and enzymatic analyses.
If mitochondrial myopathy is suspected, a muscle biopsy is usually suggested to confirm the presence of mitochondrial dysfunction and to obtain the best tissue for subsequent genetic analysis. A muscle biopsy may also be considered in patients with suspected structural myopathies in whom the differential diagnosis remains broad even after an otherwise extensive evaluation; appropriate testing of the tissue may provide important clues to facilitate diagnosis (e.g., absence of sarcoglycan staining).
In patients in whom an acquired or intrinsic cause of rhabdomyolysis cannot be easily identified, the physician is faced with the question of the utility and cost of further evaluation (e.g., whole exome sequencing). In general, after a single episode of rhabdomyolysis where no acquired cause is identified, we do not necessarily pursue additional testing or muscle biopsy unless there is additional evidence suggesting an inherited muscle disease. However, in the case of recurrent rhabdomyolysis, we will pursue genetic testing and/or muscle biopsy. In patients with recurrent rhabdomyolysis with no clear acquired cause or specific clinical features in whom muscle biopsy and enzymatic testing are normal, we would consider gene panels and/or whole exome sequencing. Currently, we consider benign exertional rhabdomyolysis to be a diagnosis of exclusion. As clinical genetic testing and whole exome sequencing become more widely available, we expect that additional genetic factors that predispose individuals to recurrent rhabdomyolysis will be identified.
Acknowledgments
This work was supported [in part] by the Intramural Research Program of the National Institute of Arthritis and Musculoskeletal and Skin Diseases of the National Institutes of Health.
ABBREVIATIONS
- CK
creatine kinase
- COX
cytochrome oxidase
- CPTII
carnitine palmitoyltransferase type 2
- EMG
electromyography
- FET
Forearm exercise test
- GT
Gömöri trichrome
- LDH
lactate dehydrogenase
- PAS
Periodic acid-Schiff
- PFK
phosphofructokinase
- RER
respiratory exchange ratio
- SDH
succinyl dehydrogenase
REFERENCES
- 1.Malinoski DJ, Slater MS, Mullins RJ. Crush injury and rhabdomyolysis. Crit Care Clin. 2004;20:171–192. doi: 10.1016/s0749-0704(03)00091-5. [DOI] [PubMed] [Google Scholar]
- 2.Huerta-Alardin AL, Varon J, Marik PE. Bench-to-bedside review: Rhabdomyolysis -- an overview for clinicians. Crit Care. 2005;9:158–169. doi: 10.1186/cc2978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Zimmerman JL, Shen MC. Rhabdomyolysis. Chest. 2013;144:1058–1065. doi: 10.1378/chest.12-2016. [DOI] [PubMed] [Google Scholar]
- 4.Melli G, Chaudhry V, Cornblath DR. Rhabdomyolysis: an evaluation of 475 hospitalized patients. Medicine (Baltimore) 2005;84:377–385. doi: 10.1097/01.md.0000188565.48918.41. [DOI] [PubMed] [Google Scholar]
- 5.Alpers JP, Jones LK., Jr Natural history of exertional rhabdomyolysis: a population-based analysis. Muscle Nerve. 2010;42:487–491. doi: 10.1002/mus.21740. [DOI] [PubMed] [Google Scholar]
- 6.Chen CY, Lin YR, Zhao LL, Yang WC, Chang YJ, Wu KH, et al. Clinical spectrum of rhabdomyolysis presented to pediatric emergency department. BMC Pediatr. 2013;13 doi: 10.1186/1471-2431-13-134. 134-2431-13-134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gabow PA, Kaehny WD, Kelleher SP. The spectrum of rhabdomyolysis. Medicine (Baltimore) 1982;61:141–152. doi: 10.1097/00005792-198205000-00002. [DOI] [PubMed] [Google Scholar]
- 8.Koffler A, Friedler RM, Massry SG. Acute renal failure due to nontraumatic rhabdomyolysis. Ann Intern Med. 1976;85:23–28. doi: 10.7326/0003-4819-85-1-23. [DOI] [PubMed] [Google Scholar]
- 9.Grossman RA, Hamilton RW, Morse BM, Penn AS, Goldberg M. Nontraumatic rhabdomyolysis and acute renal failure. N Engl J Med. 1974;291:807–811. doi: 10.1056/NEJM197410172911601. [DOI] [PubMed] [Google Scholar]
- 10.Zepeda-Orozco D, Ault BH, Jones DP. Factors associated with acute renal failure in children with rhabdomyolysis. Pediatr Nephrol. 2008;23:2281–2284. doi: 10.1007/s00467-008-0922-y. [DOI] [PubMed] [Google Scholar]
- 11.Koskelo P, Kekki M, Wager O. Kinetic behaviour of 131-I-labelled myoglobin in human beings. Clin Chim Acta. 1967;17:339–347. doi: 10.1016/0009-8981(67)90207-0. [DOI] [PubMed] [Google Scholar]
- 12.Clarkson PM, Nosaka K, Braun B. Muscle function after exercise-induced muscle damage and rapid adaptation. Med Sci Sports Exerc. 1992;24:512–520. [PubMed] [Google Scholar]
- 13.Poels PJ, Gabreels FJ. Rhabdomyolysis: a review of the literature. Clin Neurol Neurosurg. 1993;95:175–192. doi: 10.1016/0303-8467(93)90122-w. [DOI] [PubMed] [Google Scholar]
- 14.Blanco JR, Zabalza M, Salcedo J, Echeverria L, Garcia A, Vallejo M. Rhabdomyolysis of infectious and noninfectious causes. South Med J. 2002;95:542–544. [PubMed] [Google Scholar]
- 15.Park JS, Seo MS, Gil HW, Yang JO, Lee EY, Hong SY. Incidence, etiology, and outcomes of rhabdomyolysis in a single tertiary referral center. J Korean Med Sci. 2013;28:1194–1199. doi: 10.3346/jkms.2013.28.8.1194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Veenstra J, Smit WM, Krediet RT, Arisz L. Relationship between elevated creatine phosphokinase and the clinical spectrum of rhabdomyolysis. Nephrol Dial Transplant. 1994;9:637–641. doi: 10.1093/ndt/9.6.637. [DOI] [PubMed] [Google Scholar]
- 17.de Meijer AR, Fikkers BG, de Keijzer MH, van Engelen BG, Drenth JP. Serum creatine kinase as predictor of clinical course in rhabdomyolysis: a 5-year intensive care survey. Intensive Care Med. 2003;29:1121–1125. doi: 10.1007/s00134-003-1800-5. [DOI] [PubMed] [Google Scholar]
- 18.Chang JT, Staffa JA, Parks M, Green L. Rhabdomyolysis with HMG-CoA reductase inhibitors and gemfibrozil combination therapy. Pharmacoepidemiol Drug Saf. 2004;13:417–426. doi: 10.1002/pds.977. [DOI] [PubMed] [Google Scholar]
- 19.Smit GP, Rake J, Akman H, DiMauro S. The Glycogen Storage Diseases and Related Disorders. In: Fernandes John, Saudubray Jean-Marie, Berghe vd Georges, et al., editors. Inborn Metabolic Diseases. Springer Berlin Heidelberg; 2006. pp. 101–119. [Google Scholar]
- 20.Kahler SG. Metabolic Myopathies. In: Hoffmann GF, Zschocke J, Nyhan WL, editors. Inherited Metabolic Diseases: A Clinical Approach. Springer; 2009. pp. 161–176. [Google Scholar]
- 21.McArdle B. Myopathy due to a defect in muscle glycogen breakdown. Clin Sci. 1951;10:13–35. [PubMed] [Google Scholar]
- 22.Munsat TL. A standardized forearm ischemic exercise test. Neurology. 1970;20:1171–1178. doi: 10.1212/wnl.20.12.1171. [DOI] [PubMed] [Google Scholar]
- 23.Coleman RA, Stajich JM, Pact VW, Pericak-Vance MA. The ischemic exercise test in normal adults and in patients with weakness and cramps. Muscle Nerve. 1986;9:216–221. doi: 10.1002/mus.880090305. [DOI] [PubMed] [Google Scholar]
- 24.Kanno T, Sudo K, Takeuchi I, Kanda S, Honda N, Nishimura Y, et al. Hereditary deficiency of lactate dehydrogenase M-subunit. Clin Chim Acta. 1980;108:267–276. doi: 10.1016/0009-8981(80)90013-3. [DOI] [PubMed] [Google Scholar]
- 25.Kazemi-Esfarjani P, Skomorowska E, Jensen TD, Haller RG, Vissing J. A nonischemic forearm exercise test for McArdle disease. Ann Neurol. 2002;52:153–159. doi: 10.1002/ana.10263. [DOI] [PubMed] [Google Scholar]
- 26.Al-Thihli K, Sinclair G, Sirrs S, Mezei M, Nelson J, Vallance H. Performance of serum and dried blood spot acylcarnitine profiles for detection of fatty acid beta-oxidation disorders in adult patients with rhabdomyolysis. J Inherit Metab Dis. 2014;37:207–213. doi: 10.1007/s10545-012-9578-7. [DOI] [PubMed] [Google Scholar]
- 27.Elliot DL, Buist NR, Goldberg L, Kennaway NG, Powell BR, Kuehl KS. Metabolic myopathies: evaluation by graded exercise testing. Medicine (Baltimore) 1989;68:163–172. [PubMed] [Google Scholar]
- 28.Kyriakides T, Angelini C, Schaefer J, Mongini T, Siciliano G, Sacconi S, et al. EFNS review on the role of muscle biopsy in the investigation of myalgia. Eur J Neurol. 2013;20:997–1005. doi: 10.1111/ene.12174. [DOI] [PubMed] [Google Scholar]
- 29.Hewitt SM, Winter RJ. Rhabdomyolysis following acute alcohol intoxication. J Accid Emerg Med. 1995;12:143–144. doi: 10.1136/emj.12.2.143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Muthukumar T, Jha V, Sud A, Wanchoo A, Bambery P, Sakhuja V. Acute renal failure due to nontraumatic rhabdomyolysis following binge drinking. Ren Fail. 1999;21:545–549. doi: 10.3109/08860229909045195. [DOI] [PubMed] [Google Scholar]
- 31.Kishore B, Thurlow V, Kessel B. Hypokalaemic rhabdomyolysis. Ann Clin Biochem. 2007;44:308–311. doi: 10.1258/000456307780480882. [DOI] [PubMed] [Google Scholar]
- 32.Kosmadakis G, Michail O, Filiopoulos V, Papadopoulou P, Michail S. Acute kidney injury due to rhabdomyolysis in narcotic drug users. Int J Artif Organs. 2011;34:584–588. doi: 10.5301/IJAO.2011.8509. [DOI] [PubMed] [Google Scholar]
- 33.Roth D, Alarcon FJ, Fernandez JA, Preston RA, Bourgoignie JJ. Acute rhabdomyolysis associated with cocaine intoxication. N Engl J Med. 1988;319:673–677. doi: 10.1056/NEJM198809153191103. [DOI] [PubMed] [Google Scholar]
- 34.Byard RW, Summersides G, Thompson A. Confluent muscle pallor: a macroscopic marker of cocaine-induced rhabdomyolysis. Forensic Sci Med Pathol. 2011;7:364–366. doi: 10.1007/s12024-011-9229-6. [DOI] [PubMed] [Google Scholar]
- 35.Kotbi N, Oliveira E, Francois D, Odom A. Mania, cocaine, and rhabdomyolysis: a case report. Am J Addict. 2012;21:570–571. doi: 10.1111/j.1521-0391.2012.00287.x. [DOI] [PubMed] [Google Scholar]
- 36.Richards JR, Johnson EB, Stark RW, Derlet RW. Methamphetamine abuse and rhabdomyolysis in the ED: a 5-year study. Am J Emerg Med. 1999;17:681–685. doi: 10.1016/s0735-6757(99)90159-6. [DOI] [PubMed] [Google Scholar]
- 37.Eilert RJ, Kliewer ML. Methamphetamine-induced rhabdomyolysis. Int Anesthesiol Clin. 2011;49:52–56. doi: 10.1097/AIA.0b013e3181ffc0e5. [DOI] [PubMed] [Google Scholar]
- 38.Russell T, Riazi S, Kraeva N, Steel AC, Hawryluck LA. Ecstacy-induced delayed rhabdomyolysis and neuroleptic malignant syndrome in a patient with a novel variant in the ryanodine receptor type 1 gene. Anaesthesia. 2012;67:1021–1024. doi: 10.1111/j.1365-2044.2012.07226.x. [DOI] [PubMed] [Google Scholar]
- 39.Mercieca J, Brown EA. Acute renal failure due to rhabdomyolysis associated with use of a straitjacket in lysergide intoxication. Br Med J (Clin Res Ed) 1984;288:1949–1950. doi: 10.1136/bmj.288.6435.1949. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Behan WM, Bakheit AM, Behan PO, More IA. The muscle findings in the neuroleptic malignant syndrome associated with lysergic acid diethylamide. J Neurol Neurosurg Psychiatry. 1991;54:741–743. doi: 10.1136/jnnp.54.8.741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Berrens Z, Lammers J, White C. Rhabdomyolysis After LSD Ingestion. Psychosomatics. 2010;51:356–356.e3. doi: 10.1176/appi.psy.51.4.356. [DOI] [PubMed] [Google Scholar]
- 42.Halachanova V, Sansone RA, McDonald S. Delayed rhabdomyolysis after ecstasy use. Mayo Clin Proc. 2001;76:112–113. doi: 10.4065/76.1.112. [DOI] [PubMed] [Google Scholar]
- 43.Narayan N, Griffiths M, Patel HD. Gluteal compartment syndrome with severe rhabdomyolysis. BMJ Case Rep. 2013;2013 doi: 10.1136/bcr-2013-010370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Star K, Iessa N, Almandil NB, Wilton L, Curran S, Edwards IR, et al. Rhabdomyolysis reported for children and adolescents treated with antipsychotic medicines: a case series analysis. J Child Adolesc Psychopharmacol. 2012;22:440–451. doi: 10.1089/cap.2011.0134. [DOI] [PubMed] [Google Scholar]
- 45.Jankovic SR, Stosic JJ, Vucinic S, Vukcevic NP, Ercegovic GV. Causes of rhabdomyolysis in acute poisonings. Vojnosanit Pregl. 2013;70:1039–1045. doi: 10.2298/vsp1311039j. [DOI] [PubMed] [Google Scholar]
- 46.Packard K, Price P, Hanson A. Antipsychotic Use and Risk of Rhabdomyolysis. J Pharm Pract. 2014 doi: 10.1177/0897190013516509. [DOI] [PubMed] [Google Scholar]
- 47.Huang SS, Yang HY, Lin YC, Chan CH. Low-dose venlafaxine-induced severe rhabdomyolysis: a case report. Gen Hosp Psychiatry. 2012;34:436.e5–436.e7. doi: 10.1016/j.genhosppsych.2012.01.016. [DOI] [PubMed] [Google Scholar]
- 48.Lewien A, Kranaster L, Hoyer C, Elkin H, Sartorius A. Escitalopram-related rhabdomyolysis. J Clin Psychopharmacol. 2011;31:251–253. doi: 10.1097/JCP.0b013e31820f4f84. [DOI] [PubMed] [Google Scholar]
- 49.Silva MA, Swanson AC, Gandhi PJ, Tataronis GR. Statin-related adverse events: a meta-analysis. Clin Ther. 2006;28:26–35. doi: 10.1016/j.clinthera.2006.01.005. [DOI] [PubMed] [Google Scholar]
- 50.Silva M, Matthews ML, Jarvis C, Nolan NM, Belliveau P, Malloy M, et al. Meta-analysis of drug-induced adverse events associated with intensive-dose statin therapy. Clin Ther. 2007;29:253–260. doi: 10.1016/j.clinthera.2007.02.008. [DOI] [PubMed] [Google Scholar]
- 51.Garcia-Rodriguez LA, Masso-Gonzalez EL, Wallander MA, Johansson S. The safety of rosuvastatin in comparison with other statins in over 100,000 statin users in UK primary care. Pharmacoepidemiol Drug Saf. 2008;17:943–952. doi: 10.1002/pds.1603. [DOI] [PubMed] [Google Scholar]
- 52.Mammen AL, Amato AA. Statin myopathy: a review of recent progress. Curr Opin Rheumatol. 2010;22:644–650. doi: 10.1097/BOR.0b013e32833f0fc7. [DOI] [PubMed] [Google Scholar]
- 53.Yeter E, Keles T, Durmaz T, Bozkurt E. Rhabdomyolysis due to the additive effect of statin therapy and hypothyroidism: a case report. J Med Case Rep. 2007;1:130. doi: 10.1186/1752-1947-1-130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Jones PH, Davidson MH. Reporting rate of rhabdomyolysis with fenofibrate + statin versus gemfibrozil + any statin. Am J Cardiol. 2005;95:120–122. doi: 10.1016/j.amjcard.2004.08.076. [DOI] [PubMed] [Google Scholar]
- 55.Hu M, Mak VW, Tomlinson B. Simvastatin-induced myopathy, the role of interaction with diltiazem and genetic predisposition. J Clin Pharm Ther. 2011;36:419–425. doi: 10.1111/j.1365-2710.2010.01184.x. [DOI] [PubMed] [Google Scholar]
- 56.Marot A, Morelle J, Chouinard VA, Jadoul M, Lambert M, Demoulin N. Concomitant use of simvastatin and amiodarone resulting in severe rhabdomyolysis: a case report and review of the literature. Acta Clin Belg. 2011;66:134–136. doi: 10.2143/ACB.66.2.20625533. [DOI] [PubMed] [Google Scholar]
- 57.Patel AM, Shariff S, Bailey DG, Juurlink DN, Gandhi S, Mamdani M, et al. Statin toxicity from macrolide antibiotic coprescription: a population-based cohort study. Ann Intern Med. 2013;158:869–876. doi: 10.7326/0003-4819-158-12-201306180-00004. [DOI] [PubMed] [Google Scholar]
- 58.Mikhail N, Iskander E, Cope D. Rhabdomyolysis in an HIV-infected patient on anti-retroviral therapy precipitated by high-dose pravastatin. Curr Drug Saf. 2009;4:121–122. doi: 10.2174/157488609788173080. [DOI] [PubMed] [Google Scholar]
- 59.SEARCH Collaborative Group. Link E, Parish S, Armitage J, Bowman L, Heath S, et al. SLCO1B1 variants and statin-induced myopathy--a genomewide study. N Engl J Med. 2008;359:789–799. doi: 10.1056/NEJMoa0801936. [DOI] [PubMed] [Google Scholar]
- 60.Chanson P, de Rohan-Chabot P, Loirat P, Lubetzki J. Nontraumatic rhabdomyolysis during diabetic ketoacidosis. Diabetologia. 1986;29:674–675. doi: 10.1007/BF00869272. [DOI] [PubMed] [Google Scholar]
- 61.Wang LM, Tsai ST, Ho LT, Hu SC, Lee CH. Rhabdomyolysis in diabetic emergencies. Diabetes Res Clin Pract. 1994;26:209–214. doi: 10.1016/0168-8227(94)90062-0. [DOI] [PubMed] [Google Scholar]
- 62.Kutlu AO, Kara C, Cetinkaya S. Rhabdomyolysis without detectable myoglobulinuria due to severe hypophosphatemia in diabetic ketoacidosis. Pediatr Emerg Care. 2011;27:537–538. doi: 10.1097/PEC.0b013e31821dc68a. [DOI] [PubMed] [Google Scholar]
- 63.Sani MA, Campana-Salort E, Begu-LeCorroller A, Baccou M, Valero R, Vialettes B. Non-traumatic rhabdomyolysis and diabetes. Diabetes Metab. 2011;37:262–264. doi: 10.1016/j.diabet.2011.03.003. [DOI] [PubMed] [Google Scholar]
- 64.Cakir M, Mahsereci E, Altunbas H, Karayalcin U. A case of rhabdomyolysis associated with thyrotoxicosis. J Natl Med Assoc. 2005;97:732–734. [PMC free article] [PubMed] [Google Scholar]
- 65.Farias Moeller R, Zecavati N, Sherafat-Kazemzadeh R, Aleinikoff S, Rennert W. Adolescent with Rhabdomyolysis due to Undiagnosed Hypothyroidism. Case Rep Pediatr. 2011;2011:670–673. doi: 10.1155/2011/670673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Grifoni E, Fabbri A, Ciuti G, Matucci Cerinic M, Moggi Pignone A. Hypokalemia-induced rhabdomyolysis. Intern Emerg Med. 2014;9:487–488. doi: 10.1007/s11739-013-1033-8. [DOI] [PubMed] [Google Scholar]
- 67.Lau SY, Yong TY. Rhabdomyolysis in acute primary adrenal insufficiency complicated by severe hyponatraemia. Intern Med. 2012;51:2371–2374. doi: 10.2169/internalmedicine.51.7879. [DOI] [PubMed] [Google Scholar]
- 68.Kung AW, Pun KK, Lam KS, Yeung RT. Rhabdomyolysis associated with cranial diabetes insipidus. Postgrad Med J. 1991;67:912–913. doi: 10.1136/pgmj.67.792.912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Naik KR, Saroja AO, Narayanappa G. Electromyographic and histological features of postpartum hypernatremic rhabdomyolysis. Ann Indian Acad Neurol. 2013;16:664–667. doi: 10.4103/0972-2327.120485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Soresi M, Brunori G, Citarrella R, Banco A, Zasa A, Di Bella G, et al. Late-onset Sheehan's syndrome presenting with rhabdomyolysis and hyponatremia: a case report. J Med Case Rep. 2013;7 doi: 10.1186/1752-1947-7-227. 227-1947-7-227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Merante A, Gareri P, Marigliano NM, De Fazio S, Bonacci E, Torchia C, et al. Laxative-induced rhabdomyolysis. Clin Interv Aging. 2010;5:71–73. doi: 10.2147/cia.s8832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Mas A, Chillaron JJ, Esteve E, Navalpotro I, Supervia A. Severe rhabdomyolysis and hyponatremia induced by picosulfate and bisacodyl during the preparation of colonoscopy. Rev Esp Enferm Dig. 2013;105:180–181. doi: 10.4321/s1130-01082013000300016. [DOI] [PubMed] [Google Scholar]
- 73.Ruisz W, Stollberger C, Finsterer J, Weidinger F. Furosemide-induced severe hypokalemia with rhabdomyolysis without cardiac arrest. BMC Womens Health. 2013;13:30. doi: 10.1186/1472-6874-13-30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.von Vigier RO, Ortisi MT, La Manna A, Bianchetti MG, Bettinelli A. Hypokalemic rhabdomyolysis in congenital tubular disorders: a case series and a systematic review. Pediatr Nephrol. 2010;25:861–866. doi: 10.1007/s00467-009-1388-2. [DOI] [PubMed] [Google Scholar]
- 75.Cherif E, Ben Hassine L, Kechaou I, Khalfallah N. Hypokalemic rhabdomyolysis: an unusual presentation of Sjogren's syndrome. BMJ Case Rep. 2013;2013 doi: 10.1136/bcr-2013-201345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Isbister GK, Hooper MR, Dowsett R, Maw G, Murray L, White J. Collett's snake (Pseudechis colletti) envenoming in snake handlers. QJM. 2006;99:109–115. doi: 10.1093/qjmed/hcl007. [DOI] [PubMed] [Google Scholar]
- 77.Johnston CI, Brown SG, O'Leary MA, Currie BJ, Greenberg R, Taylor M, et al. Mulga snake (Pseudechis australis) envenoming: a spectrum of myotoxicity, anticoagulant coagulopathy, haemolysis and the role of early antivenom therapy - Australian Snakebite Project (ASP-19) Clin Toxicol (Phila) 2013;51:417–424. doi: 10.3109/15563650.2013.787535. [DOI] [PubMed] [Google Scholar]
- 78.Akdur O, Can S, Afacan G. Rhabdomyolysis secondary to bee sting. Case Rep Emerg Med. 2013;2013:258–421. doi: 10.1155/2013/258421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Hubbard JJ, James LP. Complications and outcomes of brown recluse spider bites in children. Clin Pediatr (Phila) 2011;50:252–258. doi: 10.1177/0009922810388510. [DOI] [PubMed] [Google Scholar]
- 80.Korkmaz I, Kukul Guven FM, Eren SH, Dogan Z. Quail consumption can be harmful. J Emerg Med. 2011;41:499–502. doi: 10.1016/j.jemermed.2008.03.045. [DOI] [PubMed] [Google Scholar]
- 81.Paul V, Shamah S, Garankina O, Wolf L, Shia Lin Y. Rhabdomyolysis after fish consumption: Haff's disease. QJM. 2014;107:67–68. doi: 10.1093/qjmed/hct172. [DOI] [PubMed] [Google Scholar]
- 82.Bedry R, Baudrimont I, Deffieux G, Creppy EE, Pomies JP, Ragnaud JM, et al. Wild-mushroom intoxication as a cause of rhabdomyolysis. N Engl J Med. 2001;345:798–802. doi: 10.1056/NEJMoa010581. [DOI] [PubMed] [Google Scholar]
- 83.Lee PT, Wu ML, Tsai WJ, Ger J, Deng JF, Chung HM. Rhabdomyolysis: an unusual feature with mushroom poisoning. Am J Kidney Dis. 2001;38:E17. doi: 10.1053/ajkd.2001.27725. [DOI] [PubMed] [Google Scholar]
- 84.Mannix R, Tan ML, Wright R, Baskin M. Acute pediatric rhabdomyolysis: causes and rates of renal failure. Pediatrics. 2006;118:2119–2125. doi: 10.1542/peds.2006-1352. [DOI] [PubMed] [Google Scholar]
- 85.Kagan LJ. Myoglobinemia in inflammatory myopathies. JAMA. 1977;237:1448–1452. doi: 10.1001/jama.237.14.1448. [DOI] [PubMed] [Google Scholar]
- 86.Haller RG. Treatment of McArdle disease. Arch Neurol. 2000;57:923–924. doi: 10.1001/archneur.57.7.923. [DOI] [PubMed] [Google Scholar]
- 87.Miteff F, Potter HC, Allen J, Teoh H, Roxburgh R, Hutchinson DO. Clinical and laboratory features of patients with myophosphorylase deficiency (McArdle disease) J Clin Neurosci. 2011;18:1055–1058. doi: 10.1016/j.jocn.2010.12.033. [DOI] [PubMed] [Google Scholar]
- 88.Martin MA, Rubio JC, Buchbinder J, Fernandez-Hojas R, del Hoyo P, Teijeira S, et al. Molecular heterogeneity of myophosphorylase deficiency (McArdle's disease): a genotype-phenotype correlation study. Ann Neurol. 2001;50:574–581. [PubMed] [Google Scholar]
- 89.Aquaron R, Berge-Lefranc JL, Pellissier JF, Montfort MF, Mayan M, Figarella-Branger D, et al. Molecular characterization of myophosphorylase deficiency (McArdle disease) in 34 patients from Southern France: identification of 10 new mutations. Absence of genotype-phenotype correlation. Neuromuscul Disord. 2007;17:235–241. doi: 10.1016/j.nmd.2006.12.014. [DOI] [PubMed] [Google Scholar]
- 90.Lucia A, Ruiz JR, Santalla A, Nogales-Gadea G, Rubio JC, Garcia-Consuegra I, et al. Genotypic and phenotypic features of McArdle disease: insights from the Spanish national registry. J Neurol Neurosurg Psychiatry. 2012;83:322–328. doi: 10.1136/jnnp-2011-301593. [DOI] [PubMed] [Google Scholar]
- 91.Braakhekke JP, de Bruin MI, Stegeman DF, Wevers RA, Binkhorst RA, Joosten EM. The second wind phenomenon in McArdle's disease. Brain. 1986;109(Pt 6):1087–1101. doi: 10.1093/brain/109.6.1087. [DOI] [PubMed] [Google Scholar]
- 92.Tsujino S, Shanske S, DiMauro S. Molecular genetic heterogeneity of myophosphorylase deficiency (McArdle's disease) N Engl J Med. 1993;329:241–245. doi: 10.1056/NEJM199307223290404. [DOI] [PubMed] [Google Scholar]
- 93.Tarui S, Okuno G, Ikura Y, Tanaka T, Suda M, Nishikawa M. Phosphofructokinase Deficiency in Skeletal Muscle. a New Type of Glycogenosis. Biochem Biophys Res Commun. 1965;19:517–523. doi: 10.1016/0006-291x(65)90156-7. [DOI] [PubMed] [Google Scholar]
- 94.Argov Z, Barash V, Soffer D, Sherman J, Raben N. Late-onset muscular weakness in phosphofructokinase deficiency due to exon 5/intron 5 junction point mutation: a unique disorder or the natural course of this glycolytic disorder? Neurology. 1994;44:1097–1100. doi: 10.1212/wnl.44.6.1097. [DOI] [PubMed] [Google Scholar]
- 95.Exantus J, Ranchin B, Dubourg L, Touraine R, Baverel G, Cochat P. Acute renal failure in a patient with phosphofructokinase deficiency. Pediatr Nephrol. 2004;19:111–113. doi: 10.1007/s00467-003-1321-z. [DOI] [PubMed] [Google Scholar]
- 96.Haller RG, Lewis SF. Glucose-induced exertional fatigue in muscle phosphofructokinase deficiency. N Engl J Med. 1991;324:364–369. doi: 10.1056/NEJM199102073240603. [DOI] [PubMed] [Google Scholar]
- 97.Hays AP, Hallett M, Delfs J, Morris J, Sotrel A, Shevchuk MM, et al. Muscle phosphofructokinase deficiency: abnormal polysaccharide in a case of late-onset myopathy. Neurology. 1981;31:1077–1086. doi: 10.1212/wnl.31.9.1077. [DOI] [PubMed] [Google Scholar]
- 98.Zenella A, Mariani M, Meola G, Fagnani F, Sirchia G. Phosphofructokinase (PFK) deficiency due to a catalytically inactive mutant M-type subunit. Am J Hematol. 1982;12:215–225. doi: 10.1002/ajh.2830120303. [DOI] [PubMed] [Google Scholar]
- 99.Vora S, DiMauro S, Spear D, Harker D, Danon MJ. Characterization of the enzymatic defect in late-onset muscle phosphofructokinase deficiency. New subtype of glycogen storage disease type VII. J Clin Invest. 1987;80:1479–1485. doi: 10.1172/JCI113229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Danon MJ, Servidei S, DiMauro S, Vora S. Late-onset muscle phosphofructokinase deficiency. Neurology. 1988;38:956–960. doi: 10.1212/wnl.38.6.956. [DOI] [PubMed] [Google Scholar]
- 101.Musumeci O, Bruno C, Mongini T, Rodolico C, Aguennouz M, Barca E, et al. Clinical features and new molecular findings in muscle phosphofructokinase deficiency (GSD type VII) Neuromuscul Disord. 2012;22:325–330. doi: 10.1016/j.nmd.2011.10.022. [DOI] [PubMed] [Google Scholar]
- 102.Vora S, Corash L, Engel WK, Durham S, Seaman C, Piomelli S. The molecular mechanism of the inherited phosphofructokinase deficiency associated with hemolysis and myopathy. Blood. 1980;55:629–635. [PubMed] [Google Scholar]
- 103.Maekawa M, Kanda S, Sudo K, Kanno T. Estimation of the gene frequency of lactate dehydrogenase subunit deficiencies. Am J Hum Genet. 1984;36:1204–1214. [PMC free article] [PubMed] [Google Scholar]
- 104.Tsujino S, Shanske S, Brownell AK, Haller RG, DiMauro S. Molecular genetic studies of muscle lactate dehydrogenase deficiency in white patients. Ann Neurol. 1994;36:661–665. doi: 10.1002/ana.410360418. [DOI] [PubMed] [Google Scholar]
- 105.Nazzari G, Crovato F. Annually recurring acroerythema and hereditary lactate dehydrogenase M-subunit deficiency. J Am Acad Dermatol. 1992;27:262–263. doi: 10.1016/s0190-9622(08)80735-9. [DOI] [PubMed] [Google Scholar]
- 106.Kanno T, Sudo K, Maekawa M, Nishimura Y, Ukita M, Fukutake K. Lactate dehydrogenase M-subunit deficiency: a new type of hereditary exertional myopathy. Clin Chim Acta. 1988;173:89–98. doi: 10.1016/0009-8981(88)90359-2. [DOI] [PubMed] [Google Scholar]
- 107.Kanno T, Maekawa M. Lactate dehydrogenase M-subunit deficiencies: clinical features, metabolic background, and genetic heterogeneities. Muscle Nerve Suppl. 1995;3:S54–S60. doi: 10.1002/mus.880181413. [DOI] [PubMed] [Google Scholar]
- 108.Miyajima H, Takahashi Y, Suzuki M, Shimizu T, Kaneko E. Molecular characterization of gene expression in human lactate dehydrogenase-A deficiency. Neurology. 1993;43:1414–1419. doi: 10.1212/wnl.43.7.1414. [DOI] [PubMed] [Google Scholar]
- 109.Yoshikuni K, Tagami H, Yamada M, Sudo K, Kanno T. Erythematosquamous skin lesions in hereditary lactate dehydrogenase M-subunit deficiency. Arch Dermatol. 1986;122:1420–1424. [PubMed] [Google Scholar]
- 110.Takayasu S, Fujiwara S, Waki T. Hereditary lactate dehydrogenase M-subunit deficiency: lactate dehydrogenase activity in skin lesions and in hair follicles. J Am Acad Dermatol. 1991;24:339–342. doi: 10.1016/0190-9622(91)70047-6. [DOI] [PubMed] [Google Scholar]
- 111.Ohtani Y, Matsuda I, Iwamasa T. A female case of glycogen storage myopathy due to phosphorylase kinase deficiency. J Inherit Metab Dis. 1982;5:71–72. doi: 10.1007/BF01799992. [DOI] [PubMed] [Google Scholar]
- 112.Iwamasa T, Fukuda S, Tokumitsu S, Ninomiya N, Matsuda I, Osame M. Myopathy due to glycogen storage disease: pathological and biochemical studies in relation to glycogenosome formation. Exp Mol Pathol. 1983;38:405–420. doi: 10.1016/0014-4800(83)90080-1. [DOI] [PubMed] [Google Scholar]
- 113.Abarbanel JM, Bashan N, Potashnik R, Osimani A, Moses SW, Herishanu Y. Adult muscle phosphorylase "b" kinase deficiency. Neurology. 1986;36:560–562. doi: 10.1212/wnl.36.4.560. [DOI] [PubMed] [Google Scholar]
- 114.Clemens PR, Yamamoto M, Engel AG. Adult phosphorylase b kinase deficiency. Ann Neurol. 1990;28:529–538. doi: 10.1002/ana.410280410. [DOI] [PubMed] [Google Scholar]
- 115.Wehner M, Clemens PR, Engel AG, Kilimann MW. Human muscle glycogenosis due to phosphorylase kinase deficiency associated with a nonsense mutation in the muscle isoform of the alpha subunit. Hum Mol Genet. 1994;3:1983–1987. doi: 10.1093/hmg/3.11.1983. [DOI] [PubMed] [Google Scholar]
- 116.Bruno C, Manfredi G, Andreu AL, Shanske S, Krishna S, Ilse WK, et al. A splice junction mutation in the alpha(M) gene of phosphorylase kinase in a patient with myopathy. Biochem Biophys Res Commun. 1998;249:648–651. doi: 10.1006/bbrc.1998.9211. [DOI] [PubMed] [Google Scholar]
- 117.Bak H, Cordato D, Carey WF, Milder D. Adult-onset exercise intolerance due to phosphorylase b kinase deficiency. J Clin Neurosci. 2001;8:286–287. doi: 10.1054/jocn.1999.0230. [DOI] [PubMed] [Google Scholar]
- 118.Burwinkel B, Hu B, Schroers A, Clemens PR, Moses SW, Shin YS, et al. Muscle glycogenosis with low phosphorylase kinase activity: mutations in PHKA1, PHKG1 or six other candidate genes explain only a minority of cases. Eur J Hum Genet. 2003;11:516–526. doi: 10.1038/sj.ejhg.5200996. [DOI] [PubMed] [Google Scholar]
- 119.Wuyts W, Reyniers E, Ceuterick C, Storm K, de Barsy T, Martin JJ. Myopathy and phosphorylase kinase deficiency caused by a mutation in the PHKA1 gene. Am J Med Genet A. 2005;133A:82–84. doi: 10.1002/ajmg.a.30517. [DOI] [PubMed] [Google Scholar]
- 120.Haller RG. Fueling around with glycogen: the implications of muscle phosphorylase b kinase deficiency. Neurology. 2008;70:1872–1873. doi: 10.1212/01.wnl.0000312284.43608.46. [DOI] [PubMed] [Google Scholar]
- 121.Orngreen MC, Schelhaas HJ, Jeppesen TD, Akman HO, Wevers RA, Andersen ST, et al. Is muscle glycogenolysis impaired in X-linked phosphorylase b kinase deficiency? Neurology. 2008;70:1876–1882. doi: 10.1212/01.wnl.0000289190.66955.67. [DOI] [PubMed] [Google Scholar]
- 122.Preisler N, Orngreen MC, Echaniz-Laguna A, Laforet P, Lonsdorfer-Wolf E, Doutreleau S, et al. Muscle phosphorylase kinase deficiency: a neutral metabolic variant or a disease? Neurology. 2012;78:265–268. doi: 10.1212/WNL.0b013e31824365f9. [DOI] [PubMed] [Google Scholar]
- 123.Wilkinson DA, Tonin P, Shanske S, Lombes A, Carlson GM, DiMauro S. Clinical and biochemical features of 10 adult patients with muscle phosphorylase kinase deficiency. Neurology. 1994;44:461–466. doi: 10.1212/wnl.44.3_part_1.461. [DOI] [PubMed] [Google Scholar]
- 124.Carrier H, Maire I, Vial C, Rambaud G, Flocard F, Flechaire A. Myopathic evolution of an exertional muscle pain syndrome with phosphorylase b kinase deficiency. Acta Neuropathol. 1990;81:84–88. doi: 10.1007/BF00662642. [DOI] [PubMed] [Google Scholar]
- 125.Rosa R, George C, Fardeau M, Calvin MC, Rapin M, Rosa J. A new case of phosphoglycerate kinase deficiency: PGK Creteil associated with rhabdomyolysis and lacking hemolytic anemia. Blood. 1982;60:84–91. [PubMed] [Google Scholar]
- 126.DiMauro S, Dalakas M, Miranda AF. Phosphoglycerate kinase deficiency: another cause of recurrent myoglobinuria. Ann Neurol. 1983;13:11–19. doi: 10.1002/ana.410130104. [DOI] [PubMed] [Google Scholar]
- 127.Tonin P, Shanske S, Miranda AF, Brownell AK, Wyse JP, Tsujino S, et al. Phosphoglycerate kinase deficiency: biochemical and molecular genetic studies in a new myopathic variant (PGK Alberta) Neurology. 1993;43:387–391. doi: 10.1212/wnl.43.2.387. [DOI] [PubMed] [Google Scholar]
- 128.Aasly J, van Diggelen OP, Boer AM, Bronstad G. Phosphoglycerate kinase deficiency in two brothers with McArdle-like clinical symptoms. Eur J Neurol. 2000;7:111–113. doi: 10.1046/j.1468-1331.2000.00012.x. [DOI] [PubMed] [Google Scholar]
- 129.Spiegel R, Gomez EA, Akman HO, Krishna S, Horovitz Y, DiMauro S. Myopathic form of phosphoglycerate kinase (PGK) deficiency: a new case and pathogenic considerations. Neuromuscul Disord. 2009;19:207–211. doi: 10.1016/j.nmd.2008.12.004. [DOI] [PubMed] [Google Scholar]
- 130.Sugie H, Sugie Y, Nishida M, Ito M, Tsurui S, Suzuki M, et al. Recurrent myoglobinuria in a child with mental retardation: phosphoglycerate kinase deficiency. J Child Neurol. 1989;4:95–99. doi: 10.1177/088307388900400203. [DOI] [PubMed] [Google Scholar]
- 131.DiMauro S, Miranda AF, Khan S, Gitlin K, Friedman R. Human muscle phosphoglycerate mutase deficiency: newly discovered metabolic myopathy. Science. 1981;212:1277–1279. doi: 10.1126/science.6262916. [DOI] [PubMed] [Google Scholar]
- 132.Bresolin N, Ro YI, Reyes M, Miranda AF, DiMauro S. Muscle phosphoglycerate mutase (PGAM) deficiency: a second case. Neurology. 1983;33:1049–1053. doi: 10.1212/wnl.33.8.1049. [DOI] [PubMed] [Google Scholar]
- 133.Kissel JT, Beam W, Bresolin N, Gibbons G, DiMauro S, Mendell JR. Physiologic assessment of phosphoglycerate mutase deficiency: incremental exercise test. Neurology. 1985;35:828–833. doi: 10.1212/wnl.35.6.828. [DOI] [PubMed] [Google Scholar]
- 134.Tsujino S, Shanske S, Sakoda S, Fenichel G, DiMauro S. The molecular genetic basis of muscle phosphoglycerate mutase (PGAM) deficiency. Am J Hum Genet. 1993;52:472–477. [PMC free article] [PubMed] [Google Scholar]
- 135.Vita G, Toscano A, Bresolin N, Meola G, Fortunato F, Baradello A, et al. Muscle phosphoglycerate mutase (PGAM) deficiency in the first Caucasian patient: biochemistry, muscle culture and 31P-MR spectroscopy. J Neurol. 1994;241:289–294. doi: 10.1007/BF00868435. [DOI] [PubMed] [Google Scholar]
- 136.Vissing J, Schmalbruch H, Haller RG, Clausen T. Muscle phosphoglycerate mutase deficiency with tubular aggregates: effect of dantrolene. Ann Neurol. 1999;46:274–277. [PubMed] [Google Scholar]
- 137.Hadjigeorgiou GM, Kawashima N, Bruno C, Andreu AL, Sue CM, Rigden DJ, et al. Manifesting heterozygotes in a Japanese family with a novel mutation in the muscle-specific phosphoglycerate mutase (PGAM-M) gene. Neuromuscul Disord. 1999;9:399–402. doi: 10.1016/s0960-8966(99)00039-5. [DOI] [PubMed] [Google Scholar]
- 138.Vissing J, Quistorff B, Haller RG. Effect of fuels on exercise capacity in muscle phosphoglycerate mutase deficiency. Arch Neurol. 2005;62:1440–1443. doi: 10.1001/archneur.62.9.1440. [DOI] [PubMed] [Google Scholar]
- 139.Oh SJ, Park KS, Ryan HF, Jr, Danon MJ, Lu J, Naini AB, et al. Exercise-induced cramp, myoglobinuria, and tubular aggregates in phosphoglycerate mutase deficiency. Muscle Nerve. 2006;34:572–576. doi: 10.1002/mus.20622. [DOI] [PubMed] [Google Scholar]
- 140.Tonin P, Bruno C, Cassandrini D, Savio C, Tavazzi E, Tomelleri G, et al. Unusual presentation of phosphoglycerate mutase deficiency due to two different mutations in PGAM-M gene. Neuromuscul Disord. 2009;19:776–778. doi: 10.1016/j.nmd.2009.08.007. [DOI] [PubMed] [Google Scholar]
- 141.Salameh J, Goyal N, Choudry R, Camelo-Piragua S, Chong PS. Phosphoglycerate mutase deficiency with tubular aggregates in a patient from Panama. Muscle Nerve. 2013;47:138–140. doi: 10.1002/mus.23527. [DOI] [PubMed] [Google Scholar]
- 142.Stojkovic T, Vissing J, Petit F, Piraud M, Orngreen MC, Andersen G, et al. Muscle glycogenosis due to phosphoglucomutase 1 deficiency. N Engl J Med. 2009;361:425–427. doi: 10.1056/NEJMc0901158. [DOI] [PubMed] [Google Scholar]
- 143.Tegtmeyer LC, Rust S, van Scherpenzeel M, Ng BG, Losfeld ME, Timal S, et al. Multiple phenotypes in phosphoglucomutase 1 deficiency. N Engl J Med. 2014;370:533–542. doi: 10.1056/NEJMoa1206605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Tonin P, Lewis P, Servidei S, DiMauro S. Metabolic causes of myoglobinuria. Ann Neurol. 1990;27:181–185. doi: 10.1002/ana.410270214. [DOI] [PubMed] [Google Scholar]
- 145.Anichini A, Fanin M, Vianey-Saban C, Cassandrini D, Fiorillo C, Bruno C, et al. Genotype-phenotype correlations in a large series of patients with muscle type CPT II deficiency. Neurol Res. 2011;33:24–32. doi: 10.1179/016164110X12767786356390. [DOI] [PubMed] [Google Scholar]
- 146.Joshi PR, Deschauer M, Zierz S. Carnitine palmitoyltransferase II (CPT II) deficiency: genotype-phenotype analysis of 50 patients. J Neurol Sci. 2014;338:107–111. doi: 10.1016/j.jns.2013.12.026. [DOI] [PubMed] [Google Scholar]
- 147.Yasuno T, Kaneoka H, Tokuyasu T, Aoki J, Yoshida S, Takayanagi M, et al. Mutations of carnitine palmitoyltransferase II (CPT II) in Japanese patients with CPT II deficiency. Clin Genet. 2008;73:496–501. doi: 10.1111/j.1399-0004.2008.00986.x. [DOI] [PubMed] [Google Scholar]
- 148.Fanin M, Anichini A, Cassandrini D, Fiorillo C, Scapolan S, Minetti C, et al. Allelic and phenotypic heterogeneity in 49 Italian patients with the muscle form of CPT-II deficiency. Clin Genet. 2012;82:232–239. doi: 10.1111/j.1399-0004.2011.01786.x. [DOI] [PubMed] [Google Scholar]
- 149.Kottlors M, Jaksch M, Ketelsen UP, Weiner S, Glocker FX, Lucking CH. Valproic acid triggers acute rhabdomyolysis in a patient with carnitine palmitoyltransferase type II deficiency. Neuromuscul Disord. 2001;11:757–759. doi: 10.1016/s0960-8966(01)00228-0. [DOI] [PubMed] [Google Scholar]
- 150.Katsuya H, Misumi M, Ohtani Y, Miike T. Postanesthetic acute renal failure due to carnitine palmityl transferase deficiency. Anesthesiology. 1988;68:945–948. doi: 10.1097/00000542-198806000-00021. [DOI] [PubMed] [Google Scholar]
- 151.Bonnefont JP, Demaugre F, Prip-Buus C, Saudubray JM, Brivet M, Abadi N, et al. Carnitine palmitoyltransferase deficiencies. Mol Genet Metab. 1999;68:424–440. doi: 10.1006/mgme.1999.2938. [DOI] [PubMed] [Google Scholar]
- 152.Wieser T, Deschauer M, Olek K, Hermann T, Zierz S. Carnitine palmitoyltransferase II deficiency: molecular and biochemical analysis of 32 patients. Neurology. 2003;60:1351–1353. doi: 10.1212/01.wnl.0000055901.58642.48. [DOI] [PubMed] [Google Scholar]
- 153.Gempel K, Kiechl S, Hofmann S, Lochmuller H, Kiechl-Kohlendorfer U, Willeit J, et al. Screening for carnitine palmitoyltransferase II deficiency by tandem mass spectrometry. J Inherit Metab Dis. 2002;25:17–27. doi: 10.1023/a:1015109127986. [DOI] [PubMed] [Google Scholar]
- 154.Norum KR. Palmityl-Coa:carnitine Palmityltransferase. Purification from Calf-Liver Mitochondria and some Properties of the Enzyme. Biochim Biophys Acta. 1964;89:95–108. [PubMed] [Google Scholar]
- 155.Zierz S, Engel AG. Regulatory properties of a mutant carnitine palmitoyltransferase in human skeletal muscle. Eur J Biochem. 1985;149:207–214. doi: 10.1111/j.1432-1033.1985.tb08913.x. [DOI] [PubMed] [Google Scholar]
- 156.Orngreen MC, Duno M, Ejstrup R, Christensen E, Schwartz M, Sacchetti M, et al. Fuel utilization in subjects with carnitine palmitoyltransferase 2 gene mutations. Ann Neurol. 2005;57:60–66. doi: 10.1002/ana.20320. [DOI] [PubMed] [Google Scholar]
- 157.Laforet P, Acquaviva-Bourdain C, Rigal O, Brivet M, Penisson-Besnier I, Chabrol B, et al. Diagnostic assessment and long-term follow-up of 13 patients with Very Long-Chain Acyl-Coenzyme A dehydrogenase (VLCAD) deficiency. Neuromuscul Disord. 2009;19:324–329. doi: 10.1016/j.nmd.2009.02.007. [DOI] [PubMed] [Google Scholar]
- 158.Olpin SE, Clark S, Andresen BS, Bischoff C, Olsen RK, Gregersen N, et al. Biochemical, clinical and molecular findings in LCHAD and general mitochondrial trifunctional protein deficiency. J Inherit Metab Dis. 2005;28:533–544. doi: 10.1007/s10545-005-0533-8. [DOI] [PubMed] [Google Scholar]
- 159.Boutron A, Acquaviva C, Vianey-Saban C, de Lonlay P, de Baulny HO, Guffon N, et al. Comprehensive cDNA study and quantitative analysis of mutant HADHA and HADHB transcripts in a French cohort of 52 patients with mitochondrial trifunctional protein deficiency. Mol Genet Metab. 2011;103:341–348. doi: 10.1016/j.ymgme.2011.04.006. [DOI] [PubMed] [Google Scholar]
- 160.Liewluck T, Mundi MS, Mauermann ML. Mitochondrial trifunctional protein deficiency: a rare cause of adult-onset rhabdomyolysis. Muscle Nerve. 2013;48:989–991. doi: 10.1002/mus.23959. [DOI] [PubMed] [Google Scholar]
- 161.Ruitenbeek W, Poels PJ, Turnbull DM, Garavaglia B, Chalmers RA, Taylor RW, et al. Rhabdomyolysis and acute encephalopathy in late onset medium chain acyl-CoA dehydrogenase deficiency. J Neurol Neurosurg Psychiatry. 1995;58:209–214. doi: 10.1136/jnnp.58.2.209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Collins S, Byrne E, Dennett X. Contrasting histochemical features of various mitochondrial syndromes. Acta Neurol Scand. 1995;91:287–293. doi: 10.1111/j.1600-0404.1995.tb07007.x. [DOI] [PubMed] [Google Scholar]
- 163.Bourgeois JM, Tarnopolsky MA. Pathology of skeletal muscle in mitochondrial disorders. Mitochondrion. 2004;4:441–452. doi: 10.1016/j.mito.2004.07.036. [DOI] [PubMed] [Google Scholar]
- 164.Pesce V, Cormio A, Fracasso F, Vecchiet J, Felzani G, Lezza AM, et al. Age-related mitochondrial genotypic and phenotypic alterations in human skeletal muscle. Free Radic Biol Med. 2001;30:1223–1233. doi: 10.1016/s0891-5849(01)00517-2. [DOI] [PubMed] [Google Scholar]
- 165.Bernier FP, Boneh A, Dennett X, Chow CW, Cleary MA, Thorburn DR. Diagnostic criteria for respiratory chain disorders in adults and children. Neurology. 2002;59:1406–1411. doi: 10.1212/01.wnl.0000033795.17156.00. [DOI] [PubMed] [Google Scholar]
- 166.Chariot P, Ruet E, Authier FJ, Labes D, Poron F, Gherardi R. Cytochrome c oxidase deficiencies in the muscle of patients with inflammatory myopathies. Acta Neuropathol. 1996;91:530–536. doi: 10.1007/s004010050462. [DOI] [PubMed] [Google Scholar]
- 167.Pauzner R, Blatt I, Mouallem M, Ben-David E, Farfel Z, Sadeh M. Mitochondrial abnormalities in oculopharyngeal muscular dystrophy. Muscle Nerve. 1991;14:947–952. doi: 10.1002/mus.880141004. [DOI] [PubMed] [Google Scholar]
- 168.Martignago S, Fanin M, Albertini E, Pegoraro E, Angelini C. Muscle histopathology in myasthenia gravis with antibodies against MuSK and AChR. Neuropathol Appl Neurobiol. 2009;35:103–110. doi: 10.1111/j.1365-2990.2008.00965.x. [DOI] [PubMed] [Google Scholar]
- 169.Thorburn DR, Chow CW, Kirby DM. Respiratory chain enzyme analysis in muscle and liver. Mitochondrion. 2004;4:363–375. doi: 10.1016/j.mito.2004.07.003. [DOI] [PubMed] [Google Scholar]
- 170.Ogasahara S, Engel AG, Frens D, Mack D. Muscle coenzyme Q deficiency in familial mitochondrial encephalomyopathy. Proc Natl Acad Sci U S A. 1989;86:2379–2382. doi: 10.1073/pnas.86.7.2379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171.Sobreira C, Hirano M, Shanske S, Keller RK, Haller RG, Davidson E, et al. Mitochondrial encephalomyopathy with coenzyme Q10 deficiency. Neurology. 1997;48:1238–1243. doi: 10.1212/wnl.48.5.1238. [DOI] [PubMed] [Google Scholar]
- 172.Di Giovanni S, Mirabella M, Spinazzola A, Crociani P, Silvestri G, Broccolini A, et al. Coenzyme Q10 reverses pathological phenotype and reduces apoptosis in familial CoQ10 deficiency. Neurology. 2001;57:515–518. doi: 10.1212/wnl.57.3.515. [DOI] [PubMed] [Google Scholar]
- 173.McFarland R, Taylor RW, Chinnery PF, Howell N, Turnbull DM. A novel sporadic mutation in cytochrome c oxidase subunit II as a cause of rhabdomyolysis. Neuromuscul Disord. 2004;14:162–166. doi: 10.1016/j.nmd.2003.10.011. [DOI] [PubMed] [Google Scholar]
- 174.Marotta R, Chin J, Kirby DM, Chiotis M, Cook M, Collins SJ. Novel single base pair COX III subunit deletion of mitochondrial DNA associated with rhabdomyolysis. J Clin Neurosci. 2011;18:290–292. doi: 10.1016/j.jocn.2010.06.001. [DOI] [PubMed] [Google Scholar]
- 175.Keightley JA, Hoffbuhr KC, Burton MD, Salas VM, Johnston WS, Penn AM, et al. A microdeletion in cytochrome c oxidase (COX) subunit III associated with COX deficiency and recurrent myoglobinuria. Nat Genet. 1996;12:410–416. doi: 10.1038/ng0496-410. [DOI] [PubMed] [Google Scholar]
- 176.Andreu AL, Hanna MG, Reichmann H, Bruno C, Penn AS, Tanji K, et al. Exercise intolerance due to mutations in the cytochrome b gene of mitochondrial DNA. N Engl J Med. 1999;341:1037–1044. doi: 10.1056/NEJM199909303411404. [DOI] [PubMed] [Google Scholar]
- 177.Karadimas CL, Greenstein P, Sue CM, Joseph JT, Tanji K, Haller RG, et al. Recurrent myoglobinuria due to a nonsense mutation in the COX I gene of mitochondrial DNA. Neurology. 2000;55:644–649. doi: 10.1212/wnl.55.5.644. [DOI] [PubMed] [Google Scholar]
- 178.Emmanuele V, Sotiriou E, Shirazi M, Tanji K, Haller RG, Heinicke K, et al. Recurrent myoglobinuria in a sporadic patient with a novel mitochondrial DNA tRNA(Ile) mutation. J Neurol Sci. 2011;303:39–42. doi: 10.1016/j.jns.2011.01.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 179.Blum S, Robertson T, Klingberg S, Henderson RD, McCombe P. Atypical clinical presentations of the A3243G mutation, usually associated with MELAS. Intern Med J. 2011;41:199–202. doi: 10.1111/j.1445-5994.2010.02379.x. [DOI] [PubMed] [Google Scholar]
- 180.Vissing CR, Duno M, Olesen JH, Rafiq J, Risom L, Christensen E, et al. Recurrent myoglobinuria and deranged acylcarnitines due to a mutation in the mtDNA MT-CO2 gene. Neurology. 2013;80:1908–1910. doi: 10.1212/WNL.0b013e3182929fb2. [DOI] [PubMed] [Google Scholar]
- 181.Figarella-Branger D, Baeta Machado AM, Putzu GA, Malzac P, Voelckel MA, Pellissier JF. Exertional rhabdomyolysis and exercise intolerance revealing dystrophinopathies. Acta Neuropathol. 1997;94:48–53. doi: 10.1007/s004010050671. [DOI] [PubMed] [Google Scholar]
- 182.Veerapandiyan A, Shashi V, Jiang YH, Gallentine WB, Schoch K, Smith EC. Pseudometabolic presentation of dystrophinopathy due to a missense mutation. Muscle Nerve. 2010;42:975–979. doi: 10.1002/mus.21823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 183.Lindberg C, Sixt C, Oldfors A. Episodes of exercise-induced dark urine and myalgia in LGMD 2I. Acta Neurol Scand. 2012;125:285–287. doi: 10.1111/j.1600-0404.2011.01608.x. [DOI] [PubMed] [Google Scholar]
- 184.Moody S, Mancias P. Dysferlinopathy presenting as rhabdomyolysis and acute renal failure. J Child Neurol. 2013;28:502–505. doi: 10.1177/0883073812444607. [DOI] [PubMed] [Google Scholar]
- 185.Hicks D, Sarkozy A, Muelas N, Koehler K, Huebner A, Hudson G, et al. A founder mutation in Anoctamin 5 is a major cause of limb-girdle muscular dystrophy. Brain. 2011;134:171–182. doi: 10.1093/brain/awq294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 186.Milone M, Liewluck T, Winder TL, Pianosi PT. Amyloidosis and exercise intolerance in ANO5 muscular dystrophy. Neuromuscul Disord. 2012;22:13–15. doi: 10.1016/j.nmd.2011.07.005. [DOI] [PubMed] [Google Scholar]
- 187.Ceravolo F, Messina S, Rodolico C, Strisciuglio P, Concolino D. Myoglobinuria as first clinical sign of a primary alpha-sarcoglycanopathy. Eur J Pediatr. 2014;173:239–242. doi: 10.1007/s00431-013-2151-z. [DOI] [PubMed] [Google Scholar]
- 188.Mongini T, Doriguzzi C, Bosone I, Chiado-Piat L, Hoffman EP, Palmucci L. Alpha-sarcoglycan deficiency featuring exercise intolerance and myoglobinuria. Neuropediatrics. 2002;33:109–111. doi: 10.1055/s-2002-32374. [DOI] [PubMed] [Google Scholar]
- 189.Cagliani R, Comi GP, Tancredi L, Sironi M, Fortunato F, Giorda R, et al. Primary beta-sarcoglycanopathy manifesting as recurrent exercise-induced myoglobinuria. Neuromuscul Disord. 2001;11:389–394. doi: 10.1016/s0960-8966(00)00207-8. [DOI] [PubMed] [Google Scholar]
- 190.Pastorello E, Cao M, Trevisan CP. Atypical onset in a series of 122 cases with FacioScapuloHumeral Muscular Dystrophy. Clin Neurol Neurosurg. 2012;114:230–234. doi: 10.1016/j.clineuro.2011.10.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 191.Fletcher JE, Tripolitis L, Hubert M, Vita GM, Levitt RC, Rosenberg H. Genotype and phenotype relationships for mutations in the ryanodine receptor in patients referred for diagnosis of malignant hyperthermia. Br J Anaesth. 1995;75:307–310. doi: 10.1093/bja/75.3.307. [DOI] [PubMed] [Google Scholar]
- 192.Jungbluth H, Zhou H, Hartley L, Halliger-Keller B, Messina S, Longman C, et al. Minicore myopathy with ophthalmoplegia caused by mutations in the ryanodine receptor type 1 gene. Neurology. 2005;65:1930–1935. doi: 10.1212/01.wnl.0000188870.37076.f2. [DOI] [PubMed] [Google Scholar]
- 193.Dlamini N, Voermans NC, Lillis S, Stewart K, Kamsteeg EJ, Drost G, et al. Mutations in RYR1 are a common cause of exertional myalgia and rhabdomyolysis. Neuromuscul Disord. 2013;23:540–548. doi: 10.1016/j.nmd.2013.03.008. [DOI] [PubMed] [Google Scholar]
- 194.Carsana A. Exercise-induced rhabdomyolysis and stress-induced malignant hyperthermia events, association with malignant hyperthermia susceptibility, and RYR1 gene sequence variations. Scientific World Journal. 2013;2013:531465. doi: 10.1155/2013/531465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 195.Thomas J, Crowhurst T. Exertional heat stroke, rhabdomyolysis and susceptibility to malignant hyperthermia. Intern Med J. 2013;43:1035–1038. doi: 10.1111/imj.12232. [DOI] [PubMed] [Google Scholar]
- 196.Lee E, Chahin N. A patient with mutation in the SCN4A p.M1592v presenting with fixed weakness, rhabdomyolysis, and episodic worsening of weakness. Muscle Nerve. 2013;48:306–307. doi: 10.1002/mus.23803. [DOI] [PubMed] [Google Scholar]
- 197.Zeharia A, Shaag A, Houtkooper RH, Hindi T, de Lonlay P, Erez G, et al. Mutations in LPIN1 cause recurrent acute myoglobinuria in childhood. Am J Hum Genet. 2008;83:489–494. doi: 10.1016/j.ajhg.2008.09.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 198.Michot C, Hubert L, Brivet M, De Meirleir L, Valayannopoulos V, Muller-Felber W, et al. LPIN1 gene mutations: a major cause of severe rhabdomyolysis in early childhood. Hum Mutat. 2010;31:E1564–E1573. doi: 10.1002/humu.21282. [DOI] [PubMed] [Google Scholar]
- 199.Devereux S, Knowles SM. Rhabdomyolysis and acute renal failure in sickle cell anaemia. Br Med J (Clin Res Ed) 1985;290:1707. doi: 10.1136/bmj.290.6483.1707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 200.Kark JA, Posey DM, Schumacher HR, Ruehle CJ. Sickle-cell trait as a risk factor for sudden death in physical training. N Engl J Med. 1987;317:781–787. doi: 10.1056/NEJM198709243171301. [DOI] [PubMed] [Google Scholar]
- 201.Rosenthal MA, Parker DJ. Collapse of a young athlete. Ann Emerg Med. 1992;21:1493–1498. doi: 10.1016/s0196-0644(05)80068-x. [DOI] [PubMed] [Google Scholar]
- 202.Thogmartin JR, Wilson CI, Palma NA, Ignacio SS, Shuman MJ, Flannagan LM. Sickle cell trait-associated deaths: a case series with a review of the literature. J Forensic Sci. 2011;56:1352–1360. doi: 10.1111/j.1556-4029.2011.01774.x. [DOI] [PubMed] [Google Scholar]
- 203.Shelmadine BD, Baltensperger A, Wilson RL, Bowden RG. Rhabdomyolysis and acute renal failure in a sickle cell trait athlete: a case study. Clin J Sport Med. 2013;23:235–237. doi: 10.1097/JSM.0b013e3182625a37. [DOI] [PubMed] [Google Scholar]
- 204.Ono I. Studies on myoglobinuria. Tohoku J Exp Med. 1953;57:273–281. doi: 10.1620/tjem.57.273. [DOI] [PubMed] [Google Scholar]
- 205.Kobayashi Y, Takeuchi T, Hosoi T, Yoshizaki H, Loeppky JA. Effect of a marathon run on serum lipoproteins, creatine kinase, and lactate dehydrogenase in recreational runners. Res Q Exerc Sport. 2005;76:450–455. doi: 10.1080/02701367.2005.10599318. [DOI] [PubMed] [Google Scholar]
- 206.Fowler WM, Jr, Chowdhury SR, Pearson CM, Gardner G, Bratton R. Changes in serum enzyme levels after exercise in trained and untrained subjects. J Appl Physiol. 1962;17:943–946. doi: 10.1152/jappl.1962.17.6.943. [DOI] [PubMed] [Google Scholar]
- 207.Hunter JB, Critz JB. Effect of training on plasma enzyme levels in man. J Appl Physiol. 1971;31:20–23. doi: 10.1152/jappl.1971.31.1.20. [DOI] [PubMed] [Google Scholar]
- 208.Alpers JP, Jones LK., Jr Natural history of exertional rhabdomyolysis: a population-based analysis. Muscle Nerve. 2010;42:487–491. doi: 10.1002/mus.21740. [DOI] [PubMed] [Google Scholar]
- 209.Meltzer HY. Factors affecting serum creatine phosphokinase levels in the general population: the role of race, activity and age. Clin Chim Acta. 1971;33:165–172. doi: 10.1016/0009-8981(71)90264-6. [DOI] [PubMed] [Google Scholar]
- 210.Olerud JE, Homer LD, Carroll HW. Incidence of acute exertional rhabdomyolysis. Serum myoglobin and enzyme levels as indicators of muscle injury. Arch Intern Med. 1976;136:692–697. doi: 10.1001/archinte.136.6.692. [DOI] [PubMed] [Google Scholar]
- 211.Deuster PA, Contreras-Sesvold CL, O'Connor FG, Campbell WW, Kenney K, Capacchione JF, et al. Genetic polymorphisms associated with exertional rhabdomyolysis. Eur J Appl Physiol. 2013;113:1997–2004. doi: 10.1007/s00421-013-2622-y. [DOI] [PubMed] [Google Scholar]
- 212.Demos MA, Gitin EL, Kagen LJ. Exercise myoglobinemia and acute exertional rhabdomyolysis. Arch Intern Med. 1974;134:669–673. [PubMed] [Google Scholar]
- 213.Clarkson PM, Hoffman EP, Zambraski E, Gordish-Dressman H, Kearns A, Hubal M, et al. ACTN3 and MLCK genotype associations with exertional muscle damage. J Appl Physiol (1985) 2005;99:564–569. doi: 10.1152/japplphysiol.00130.2005. [DOI] [PubMed] [Google Scholar]