Abstract
Background
Health self-efficacy (the confidence to take care of one’s health) is a key component in ensuring individuals are active partners in their health and health care. The purpose of this study was to determine the association between financial hardship and health self-efficacy among African American men; and to determine if unmet medical need due to cost potentially mediates this association.
Methods
Cross sectional analysis was conducted using data from a convenience sample of African-American men who attended a one-day annual community health fair in Northeast Ohio (N=279). Modified Poisson regression models were estimated to obtain the relative risk of reporting low health self-efficacy. After adjusting for socio-demographic characteristics, those reporting financial hardship were 2.91 times (exp(β)=2.91; CI: 1.24, 6.83; p<.05) more likely to report low health self-efficacy. When unmet medical need due to cost was added to the model the association between financial hardship and low health self-efficacy was no longer statistically significant.
Conclusion
Our results suggest that the association between financial hardship and health self-efficacy can be explained by unmet medical need due to cost. Possible intervention efforts among African American men with low financial resources should consider expanding clinical and community-based health assessments to capture financial hardship and unmet medical need due to cost as potential contributors to low health self-efficacy.
Keywords: Health self-efficacy, financial hardship, African American men, unmet medical need
Introduction
Across a range of health outcomes, African American men fare poorly compared to other populations. African American men have the highest all-cause mortality rate in the United States(Hoyert & Xu, 2012), and deaths from cardiovascular disease and cancer largely account for this inequity(Pickle, Mungiole, Jones, & White, 1996). One factor that has been predictive of both health behaviors and health outcomes in a number of populations is self-efficacy.(Jackson, Tucker, & Herman, 2007; Tucker, Butler, Loyuk, Desmond, & Surrency, 2009) According to Social Cognitive Theory (SCT), self-efficacy is defined as having the belief and confidence to execute the necessary actions in order to achieve a desired outcome in a specific domain.(Bandura, 1986; Strecher, DeVellis, Becker, & Rosenstock, 1986) Those with high self-efficacy expect favorable results from their efforts and view challenges to their efforts as surmountable.(Bandura, 2004) In the health domain, self-efficacy (referred to as health self-efficacy) has been described as an individual’s belief that they can manage their health. (Lee, Hwang, Hawkins, & Pingree, 2008; Namkoong et al., 2010) Research studies on health self-efficacy among African American men have generally focused on specific behaviors (e.g. medication adherence(Elder et al., 2012), condom use,(Raiford, Seth, Braxton, & DiClemente, 2013) physical activity(Griffith, Allen, Johnson-Lawrence, & Langford, 2013)) and detecting or treating specific diseases (e.g. prostate cancer(Kendrick, Montgomery, Ouattara, & Flaskerud, 2009)), with higher health self-efficacy being associated with more positive outcomes.
Health self-efficacy can be influenced by the social and physical environment in which one is managing health or navigating a health system. (Bandura, 1977) For instance, individuals with low socioeconomic status, and medically underserved racial/ethnic minority groups, often report lower confidence in caring for their health and preventing health problems(Scheppers, van, Dekker, Geertzen, & Dekker, 2006). Previous research indicates that limited financial resources have been shown to reduce one’s health self-efficacy, making it difficult to access health care and perform healthy behaviors. (Ku, 20009; Lynch, Kaplan, & Salonen, 1997; Shelton, Goldman, Emmons, Sorensen, & Allen, 2011; Williams, 2003; Xanthos, Treadwell, & Holden, 2010)
African American men are exposed to many social and environmental conditions and stressors that have a negative impact on their health and health behavior(Xanthos et al., 2010) In particular, African Americans have the highest unemployment rate (12.7% for men and 12.6% for women in Jan 2012); and, from 2008–2010, African Americans were 60% more likely to live in an area with double-digit unemployment rates (United States Department of Labor, 2012). Additionally, African American men face lower wages, with average African American men’s wages being 76.3 percent of the average wages earned by white men(United States Department of Labor, 2012). A 2013 poll of African Americans revealed that 50% reported their personal finances as not so good or poor; and those in this group were also less likely to be confident they could pay for a major illness and more likely to report having a serious problem paying for medical bills in the previous year (NPR, Robert Wood Johnson Foundation, & Harvard School of Public Health, 2013). Research on hardships shows that African Americans are more likely to report hardships than whites, even after controlling for demographic and other socioeconomic indicators (Bauman, 1998; Williams, Mohammed, Leavell, & Collins, 2010). Among the many stressors encountered by African American men, the experience of financial hardship can be most pernicious as it limits choices as one navigates daily life while often leading to an accumulation of subsequent stressors.(Lincoln, 2007; Pearlin, Mullan, Semple, & Skaff, 1990) More specifically, the experience of financial hardship often forces already disadvantaged households to choose among necessities such as paying monthly bills, food, and health care.(Boushey, Brocht, Gundersen, & Bernstein, 2001)
SCT posits that self-efficacy is a critical determinant of health behavior; (Bandura, 2004) and self-efficacy has been shown to be positively associated with individual and neighborhood level socioeconomic circumstances (Boardman & Robert, 2000; Siahpush, McNeill, Borland, & Fong, 2006; Gecas, 1989). Boardman and Robert (2000) contend that the positive association between SES and self-efficacy is largely explained by complex and autonomous occupations of high SES individuals that increase self-efficacy, and the substantial resources afforded high SES individuals that increase their likelihood of encountering mastery experiences. Yet, few extant studies have examined the influence of socioeconomic circumstances on the health self-efficacy among men specifically, and those available use traditional measures of socioeconomic status (i.e. education and income). Conventional measures of SES may not adequately capture day-to-day financial circumstances; in particular, these measures do not capture how well families are “making ends meet” or experiencing financial hardship. Financial hardship has been generally defined and measured following the work of Pearlin(Pearlin, Lieberman, Menaghan, & Mullan, 1981; Pearlin, 1989; Pearlin & Schooler, 1978a) as the difficulty one is having meeting monthly financial obligations (i.e. paying monthly bills).(Lantz, House, Mero, & Williams, 2005) Research consistently demonstrates a robust association between financial hardship and certain health behaviors(Macy, Chassin, & Presson, 2013; Kendrick et al., 2009; Siahpush, Borland, & Scollo, 2003; Siahpush, Spittal, & Singh, 2007), self-rated health(Tucker-Seeley, Harley, Stoddard, & Sorensen, 2013), morbidity(Tucker-Seeley, Li, Sorensen, & Subramanian, 2011; Butterworth, Rodgers, & Windsor, 2009; Hope, Power, & Rodgers, 1999; Price, Choi, & Vinokur, 2002), and mortality(Tucker-Seeley, Li, Subramanian, & Sorensen, 2009), even after controlling for conventional measures of SES. Research has also shown that financial hardship is negatively associated with psychosocial factors similar to self-efficacy(Elstad, 1998; Pearlin et al., 1981; Mirowsky & Ross, 1984) such as mastery(Vinokur & Schul, 1997) and internal locus of control.(Lindstrom & Rosvall, 2012; Krause, 1987)
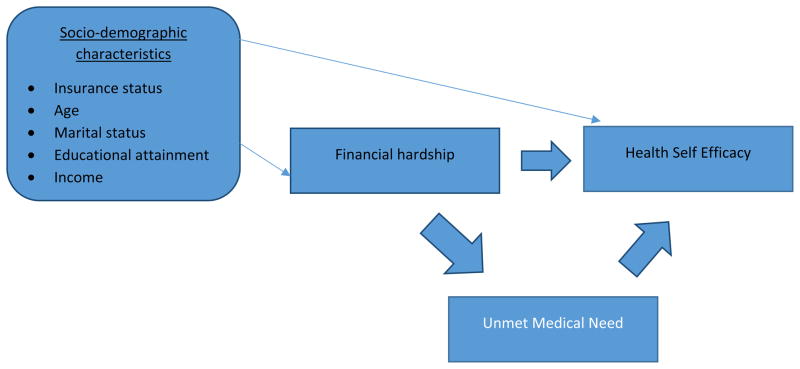
To further explicate the socioeconomic determinants of health self-efficacy, the aim of this study was to investigate the association between health self-efficacy and a nuanced measure of socioeconomic circumstances (e.g. financial hardship) among African American men. Previous research on financial hardship suggests the assessment of traditional socioeconomic indicators along with multiple indicators of hardship (e.g. problems paying bills, unmet medical need) to better understand and unpack the nature of the hardship experience. (Boushey et al., 2001; Ennis, Hobfoll, & Schroder, 2000; Pearlin et al., 1981; Avison & Turner, 1988). Our hypotheses were informed by the conceptualization of financial hardship as a chronic hardship experience (occurring more frequently) and unmet medical need due to cost as an acute hardship experience (occurring less frequently). We hypothesized that financial hardship would be negatively associated with health self-efficacy and that unmet medical need due to cost would attenuate the association between financial hardship and health self-efficacy but not completely mediate this association. We hypothesized that this association would remain even after controlling for potentially confounding socio-demographic factors such as insurance status, education, income, and marital status (see figure 1).
Figure 1.
Conceptual model of the association between financial hardship and health self-efficacy
Methods
Data Source
Respondents for this study were recruited from an annual minority men’s health fair hosted by a large health system in Northeast Ohio. Participants consisted of a cross-sectional, convenience sample of African American men aged 18 and older who could read and write in English. African American males attending the fair were approached by graduate student volunteers; those who gave oral consent were given a 47-item anonymous paper-based survey attached to a clipboard to complete onsite. The survey was developed using an 8th grade reading level and several volunteers were on hand to assist participants with completing the survey, though assistance was rarely requested. The instrument took approximately ten minutes to complete and participants were not compensated. Both the Institutional Review Boards at the medical system and the author’s academic institution approved the study. Of the 1,200 total health fair attendees, 311 completed the survey. Subjects were excluded from analysis if they were missing values on the outcome variable (N=15) or the independent variables (N=53). The final sample used for analysis was N=243.
Measures
Outcome Variable
Health self-efficacy was operationalized in this study using the following question: “Overall, how confident are you about your ability to take good care of your health?” The response options were “not confident at all, a little confident, somewhat confident, very confident, and completely confident.” We dichotomized this variable with a cut-off at the lowest two categories (Low health self-efficacy = not confident at all and a little confident vs. High health self-efficacy = somewhat confident, very confident, and completely confident). This item was originally utilized in the 2008 Health Information National Trends Survey (HINTS), a nationally representative survey of cancer-related knowledge, information- seeking and health behaviors among U.S. adults and sponsored by the National Cancer Institute; details about the design and implementation of HINTS and this specific item are available at http://hints.cancer.gov. This single measure has previously been used to characterize health self-efficacy (Wallace, Chisolm, Abdel-Rasoul, & DeVoe, 2013).
Independent Variables
Primary exposure variable
To assess financial hardship, respondents were asked the following question: “How difficult is it for you or your family to meet monthly payments on bills?” The response options were “not at all difficult, not very difficult, somewhat difficult, very difficult, and extremely difficult. We dichotomized this variable into high financial hardship (somewhat difficult, very difficult, and extremely difficult) and low financial hardship (not at all difficult and not very difficult). This item has been used previously as an indicator of financial hardship (Lantz et al., 2005; Pearlin & Schooler, 1978b).
Potentially confounding socio-demographic characteristics that we hypothesized were associated with health self-efficacy and financial hardships were included as covariates in our models. The covariates included: insurance status, age, marital status, educational attainment, and income. Unmet medical need was assessed as a potentially mediating variable by asking respondents the following question: “Was there a time in the past 12 months when you needed to see a doctor but could not because of cost?” Response options were “yes” or “no”.
Statistical Analysis
Bivariate and multivariable tests were conducted to investigate the association between health self-efficacy and financial hardship. Chi-square exact tests were conducted to estimate the difference in health self-efficacy between those reporting financial hardship and those not reporting financial hardship and across categories of the categorical socio-demographic characteristics. T-tests were conducted to estimate differences in age across categories of health self-efficacy and financial hardship. Modified Poisson regression models were estimated in SAS© 9.2 (Proc Genmod using Poisson distribution and log link) to obtain the relative risk of low health self-efficacy. We estimated three models: (1) a simple model including only the primary exposure, financial hardship; (2) model adjusting for potentially confounding socio-demographic characteristics; and (3) a model to evaluate if unmet medical need attenuated the association between financial hardship and health self-efficacy.
Results
Table 1 lists the frequency distributions for the socio-demographic variables across the primary predictor (financial hardship) and outcome variable (health self-efficacy). Bivariate analyses revealed statistically significant differences in health self-efficacy across categories of financial hardship (p<.01) and unmet medical need (p<.01). However, we did not find statistically significant differences across the socio-demographic characteristics in health self-efficacy (See Table 1). Tests of differences in financial hardship across categories of the socio-demographic characteristics revealed that those without health insurance (p<.001) and lower income (p<.001) were more likely to report financial hardship.
Table 1.
Bivariate associations between demographic and socioeconomic characteristics, financial hardship, and health self-efficacy among a sample of African American men
| Financial Hardship N (%) | Health Self-efficacy | P-value | ||||||
|---|---|---|---|---|---|---|---|---|
|
| ||||||||
| N | % | No | Yes | High * | Low | Financial Hardship | Health Self efficacy | |
| Total | 243 (100%) | 191 (79%) | 52 (21%) | 222 (91%) | 21 (9%) | p< .01 | ||
| Insurance Status | p<.001 | p=.25 | ||||||
| Insured | 103 | 42% | 93 (90%) | 10 (10%) | 97 (94%) | 6 (6%) | ||
| Uninsured | 140 | 58% | 98 (70%) | 42 (30%) | 125 (89%) | 15 (11%) | ||
| Marital Status | p=.06 | p=.45 | ||||||
| Married | 68 | 28% | 59 (87%) | 9 (13%) | 64 (94%) | 4 (6%) | ||
| Not Married | 175 | 72% | 132 (75%) | 43 (25%) | 158 (90%) | 17 (10%) | ||
| Educational attainment | p=.35 | p=1.0 | ||||||
| High School graduate or less | 113 | 47% | 92 (81%) | 21 (19%) | 103 (91%) | 10 (9%) | ||
| Some college or more | 130 | 53% | 99 (76%) | 31 (24%) | 119 (92%) | 11 (8%) | ||
| Income | p<.001 | p=.36 | ||||||
| ≤ $30,000 | 160 | 66% | 114 (71%) | 46 (29%) | 143 (89%) | 17(11%) | ||
| $31,000 ≤ $60,000 | 58 | 24% | 54 (93%) | 4 (7%) | 55 (95%) | 3 (5%) | ||
| ≥ $61,000 | 25 | 10% | 23 (92%) | 2 (8%) | 24 (96%) | 1 (4%) | ||
| Unmet medical need due to cost | p<.001 | p<.01 | ||||||
| No | 143 | 59% | 127 (89%) | 16 (11%) | 137 (96%) | 6 (4%) | ||
| Yes | 100 | 41% | 64 (64%) | 36 (36%) | 85 (85%) | 15 (15%) | ||
| Average age (STD) | 52 (12.57) | 53 (13.26) | 50 (9.35) | 50 (8.67) | 52 (12.88) | p=.07 | p=.29 | |
The results of the multivariable tests are listed in Table 2. The simple model showed that those reporting financial hardship were 3.65 times more likely to report low health self-efficacy than those not reporting financial hardship. After adjusting for socio-demographic characteristics, those reporting financial hardship were 2.87 times more likely to report low health self-efficacy. When unmet medical need was added to the model, the association between financial hardship and health self-efficacy became non-significant, which suggests that this variable mediates this association.
Table 2.
Relative Risk (95% Confidence Intervals) for the Simple and Multivariable Association Between Financial Hardship and Low Health Self-Efficacy
p<.01;
p<.05
Model 1: Simple model with primary exposure (financial hardship) and outcome (health self-efficacy)
Model 2: Model 1 + socio-demographic characteristics (age, marital status, educational attainment, income, insurance status)
Model 3: Model 2 + unmet medical need due to cost
Discussion
This is the first study of which the authors are aware to examine the association between financial hardship and health self-efficacy among African American men. The results of this study revealed a negative association between financial hardship and health self-efficacy; and the association remained significant even after controlling for more traditional measures of SES such as education and income. Furthermore, we also determined that having unmet health needs due to cost appears to mediate the association between financial hardship and health self-efficacy.
Having access to quality health care is a significant determinant of health outcomes,(McGibbon, Etowa, & McPherson, 2008)and African American men are more likely to report poor quality of care compared to White and Asian men.(Felix-Aaron et al., 2005) Data from qualitative and quantitative studies reveals that African American men feel that their race substantially negatively influences the quality of the care they receive (Woods, Montgomery, Belliard, Ramirez-Johnson, & Wilson, 2004). As such, if African American men have the perception that they will receive substandard health care due to race, then the results presented in this study of experiencing financial hardship, having difficulty meeting health needs due to the cost, and also feeling less capable of maintaining health presents substantial barriers for African American men to engage in a complex health care system and manage their health and warrants further investigation.
This potential cascade of unequal vulnerability reinforces the necessity of understanding the impact of financial instability on the health of African American men. While low-income status and financial hardship are correlated, they are not interchangeable(Short, 2005); and many studies on the social determinants of health have begun utilizing measures of socioeconomic circumstances (e.g. financial hardship) that capture the differential demands on economic resources across households;(Perry, 2002; Whelan, Layte, Maitre, & Nolan, 2001) In the present study we attempted to better understand the socioeconomic circumstances of African American men by focusing on financial hardship and unmet medical need due to cost in addition to the traditional measure of SES (e.g. education and income). In particular, the financial hardship variable utilized in this study was intended to gauge the potential impact of more specific chronic proximal barriers to meeting health needs; and the measure of unmet medical need due to cost was meant to capture an acute proximal barrier to meeting health needs. Thus, the unique contributions of this study are the further explication of the association between socioeconomic circumstances and health self-efficacy and illustration of the multidimensional aspect of socioeconomic circumstances that influence this critical determinant of health behavior. In particular, our findings show the positive association between financial hardship and low health self-efficacy and the mediating role of unmet medical need due to cost in that association among African American men.
Implications for Practice
These findings are particularly relevant for health educators and social care practitioners working with African American men with few socioeconomic resources. Our results call attention to the need for a better understanding of how unmet medical needs due to cost and financial hardship work to reduce health self-efficacy and help to contextualize the difficulties some African American men may face. The findings of our study also demonstrate the need for information on unmet medical needs due to cost and financial hardship along with traditional measures of SES to be included in clinical and community-based health assessments aimed at identifying barriers to care for African American men. Health educators may want to utilize this type of information to identify and target African American men who lack the adequate confidence and resources to engage in preventive health behaviors or chronic disease self-management; and who might benefit most from interventions better tailored to their social (financial) circumstances.
Strengths/Limitations
This study uses a cross-sectional design, thus causality cannot be inferred. In addition, a convenience sample was used which may limit generalizability and introduces selection bias – as does our relatively low response rate. Our measures of financial hardship and unmet medical need did not include an assessment of how often these hardships occurred; thus conceptualizing financial hardship as a chronic hardship experience and unmet medical need due to cost as an acute hardship experience was an assumption of our modeling efforts. Additionally, while the sample of men who participated in our study are similar in terms of education, income, employment, and marital status to national samples of African American men (e.g. Current Population Survey)(DeNavas-Walt, Proctor, & Smith, 2010), they may also exhibit more health-seeking behaviors than national samples, given they were recruited from a health fair. Lastly, the prevalence of self-reported financial hardship was relatively low at 21%; and our model did not include an explicit health behavior as an outcome. These limitations notwithstanding, the strengths of this study include the use of a more precise measure of socioeconomic circumstances and an examination of factors that potentially mediate the relationship between financial hardship and health self-efficacy in a sample of African American men.
Conclusion
Given the lack of a statistically significant difference in health self-efficacy across the socio-demographic characteristics in our study and the statistically significant association between health self-efficacy and financial hardship and unmet medical need due to cost, the results of our study suggest the need for further explication of the psychosocial/socioeconomic environment of African American men beyond traditional indicators of socio-demographic characteristics. A better understanding of the mechanisms by which some socioeconomic and psychosocial factors influence health self-efficacy among African American men may contribute to the design of interventions on the social determinants of the health, health behavior, and health care for underserved men. More specifically, by explicating the role of financial hardship on health self-efficacy and the mediating impact of unmet health needs due to cost among African American men in this study, our results inform the practice of social workers, nurses, and other clinicians who may need to better understand the often unspoken rationale for delaying or avoiding preventive health care utilization, medication compliance, or other recommended health behaviors. This presents an opportunity specifically for community-based health educators and clinicians to engage African American men on these potential issues by expanding when possible, existing assessments that capture socioeconomic status to include financial hardship and the cost of care as potential barriers to health self-efficacy and to care in general. Once measured, social service or patient advocate programs could be utilized to potentially reduce the impact of these barriers. Our goal in conducting this study was to highlight the need for greater explication of the socioeconomic condition of African American men beyond the traditional measures of education and income; and to encourage the development of tailor-made support programs that target the financial barriers African American men encounter when managing their health and seeking health care.
Contributor Information
Reginald D. Tucker-Seeley, Center for Community-Based Research, Dana-Farber Cancer Institute/Department of Social and Behavioral Sciences, Harvard School of Public Health.
Jamie A. Mitchell, Email: Jamie.Mitchell@Wayne.edu, School of Social Work, Wayne State University, 337 Thompson Home, 4756 Cass Avenue, Detroit, MI 48202, Office: (313) 577-4408, Fax: (313) 577-8770.
Deirdre Shires, Email: Deirdre.Shires@wayne.edu, School of Social Work, Wayne State University, Thompson Home, 4756 Cass Avenue, Detroit, MI, 48202, Phone: 313-577-4400.
Charles S. Modlin, Jr., Email: ModlinC@ccf.org, Glickman Urological & Kidney Institute, The Cleveland Clinic Foundation; Desk Q-10-1, 9500 Euclid Avenue, Cleveland, OH 44195, Phone: (216) 445-7550.
Reference List
- Avison WR, Turner RJ. Stressful life events and depressive symptoms: disaggregating the effects of acute stressors and chronic strains. Journal of health and social behavior. 1988;29:253–264. [PubMed] [Google Scholar]
- Bandura A. Self-efficacy: toward a unifying theory of behavioral change. Psychol Rev. 1977;84:191–215. doi: 10.1037//0033-295x.84.2.191. [DOI] [PubMed] [Google Scholar]
- Bandura A. Social Foundations of Thought and Action. Upper Saddle River, NJ: Prentice Hall; 1986. Self-efficacy; pp. 390–453. [Google Scholar]
- Bandura A. Health promotion by social cognitive means. Health Educ Behav. 2004;31:143–164. doi: 10.1177/1090198104263660. [DOI] [PubMed] [Google Scholar]
- Bauman K. Direct measures of poverty as indicators of economic need: Evidence from The Survey of Income and Program Participation. 1998 Rep. No. Population Division, U.S. Bureau of the Census, Technical Working Paper No. 30. [Google Scholar]
- Boardman JD, Robert SA. Neighborhood socioeconomic status and perceptions of self-efficacy. Sociological Perspectives. 2000;43:117–136. [Google Scholar]
- Boushey H, Brocht C, Gundersen B, Bernstein J. Hardships in America: The Real Story of Working Families. Washington DC: Economic Policy Institute; 2001. [Google Scholar]
- Butterworth P, Rodgers B, Windsor TD. Financial hardship, socio-economic position and depression: Results from the PATH Through Life Survey. Social Science & Medicine. 2009;69:229–237. doi: 10.1016/j.socscimed.2009.05.008. [DOI] [PubMed] [Google Scholar]
- DeNavas-Walt C, Proctor BD, Smith JC. Income, Poverty, and Health Insurance Coverage in the United States: 2009. Washington, D.C: U.S. Government Printing Office; 2010. pp. P60–238. Rep. No. U.S. Census Bureau Current Population Reports. [Google Scholar]
- Elder K, Ramamonjiarivelo Z, Wiltshire J, Piper C, Horn WS, Gilbert KL, et al. Trust, medication adherence, and hypertension control in Southern African American men. Am J Public Health. 2012;102:2242–2245. doi: 10.2105/AJPH.2012.300777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elstad JI. The psycho-social perspective on social inequalities in health. Sociology of Health and Illness. 1998;20:598–618. [Google Scholar]
- Ennis NE, Hobfoll SE, Schroder KEE. Money doesn't talk, it swears: How economic stress and resistance resources impact inner-city women's depressive mood. American Journal of Community Psychology. 2000;28:149–173. doi: 10.1023/A:1005183100610. [DOI] [PubMed] [Google Scholar]
- Felix-Aaron K, Moy E, Kang M, Patel M, Chesley FD, Clancy C. Variation in quality of men's health care by race/ethnicity and social class. Med Care. 2005;43:I72–I81. doi: 10.1097/00005650-200503001-00011. [DOI] [PubMed] [Google Scholar]
- Gecas V. The social psychology of self-efficacy. Annual Review of Sociology. 1989;15:291–316. [Google Scholar]
- Griffith DM, Allen JO, Johnson-Lawrence V, Langford A. Men on the Move: A Pilot Program to Increase Physical Activity Among African American Men. Health Educ Behav. 2013 doi: 10.1177/1090198113496788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hope S, Power C, Rodgers B. Does financial hardship account for elevated psychological distress in lone mothers? Social science & medicine (1982) 1999;49:1637–1649. doi: 10.1016/s0277-9536(99)00251-8. [DOI] [PubMed] [Google Scholar]
- Hoyert DL, Xu J. Deaths: Preliminary Data for 2011. National Vital Statistics Reports [Electronic version] 2012 [PubMed] [Google Scholar]
- Jackson ES, Tucker CM, Herman KC. Health value, perceived social support, and health self-efficacy as factors in a health-promoting lifestyle. J Am Coll Health. 2007;56:69–74. doi: 10.3200/JACH.56.1.69-74. [DOI] [PubMed] [Google Scholar]
- Kendrick L, Montgomery S, Ouattara D, Flaskerud JH. African american men and self-efficacy in preventing prostate cancer. Issues Ment Health Nurs. 2009;30:342–343. doi: 10.1080/01612840902754669. [DOI] [PubMed] [Google Scholar]
- Krause N. Chronic strain, locus of control, and distress in older adults. Psychol Aging. 1987;2:375–382. doi: 10.1037//0882-7974.2.4.375. [DOI] [PubMed] [Google Scholar]
- Ku L. CHARGING THE POOR MORE FOR HEALTH CARE: COST-SHARING IN MEDICAID. Center on Budget and Policy Priorities; 2009. [Electronic version] Available: http://www.cbpp.org/archiveSite/5-7-03health.pdf. [Google Scholar]
- Lantz PM, House JS, Mero RP, Williams DR. Stress, life events, and socioeconomic disparities in health: results from the Americans' Changing Lives Study. J Health Soc Behav. 2005;46:274–288. doi: 10.1177/002214650504600305. [DOI] [PubMed] [Google Scholar]
- Lee SY, Hwang H, Hawkins R, Pingree S. Interplay of negative emotion and health self-efficacy on the use of health information and its outcomes. Communication Research. 2008;35:358–381. [Google Scholar]
- Lincoln KD. Financial Strain, Negative Interactions, and Mastery: Pathways to Mental Health Among Older African Americans. J Black Psychol. 2007;33:439–462. doi: 10.1177/0095798407307045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lindstrom M, Rosvall M. Marital status, social capital and health locus of control: a population-based study. Public Health. 2012;126:790–795. doi: 10.1016/j.puhe.2012.06.001. [DOI] [PubMed] [Google Scholar]
- Lynch JW, Kaplan GA, Salonen JT. Why do poor people behave poorly? Variation in adult health behaviours and psychosocial characteristics by stages of the socioeconomic lifecourse. Soc Sci Med. 1997;44:809–819. doi: 10.1016/s0277-9536(96)00191-8. [DOI] [PubMed] [Google Scholar]
- Macy JT, Chassin L, Presson CC. Predictors of health behaviors after the economic downturn: a longitudinal study. Soc Sci Med. 2013;89:8–15. doi: 10.1016/j.socscimed.2013.04.020. Epub;%2013 Apr 29., 8–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McGibbon E, Etowa J, McPherson C. Health-care access as a social determinant of health. Can Nurse. 2008;104:22–27. [PubMed] [Google Scholar]
- Mirowsky J, Ross CE. Mexican culture and its emotional contraditions. Journal of health and social behavior. 1984;25:2–13. [PubMed] [Google Scholar]
- Namkoong K, Shah DV, Han JY, Kim SC, Yoo W, Fan D, et al. Expression and reception of treatment information in breast cancer support groups: how health self-efficacy moderates effects on emotional well-being. Patient Educ Couns. 2010;81(Suppl):S41–7. S41–S47. doi: 10.1016/j.pec.2010.09.009. Epub;%2010 Nov 1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- NPR, Robert Wood Johnson Foundation, & Harvard School of Public Health. African American's Lives Today 2013 [Google Scholar]
- Pearlin LI. The Sociological Study of Stress. Journal of health and social behavior. 1989;30:241–256. [PubMed] [Google Scholar]
- Pearlin LI, Lieberman MA, Menaghan EG, Mullan JT. The stress process. Journal of health and social behavior. 1981;22:337–356. [PubMed] [Google Scholar]
- Pearlin LI, Mullan JT, Semple SJ, Skaff MM. Caregiving and the stress process: an overview of concepts and their measures. Gerontologist. 1990;30:583–594. doi: 10.1093/geront/30.5.583. [DOI] [PubMed] [Google Scholar]
- Pearlin LI, Schooler C. The structure of coping. Journal of health and social behavior. 1978a;19:2–21. [PubMed] [Google Scholar]
- Pearlin LI, Schooler C. The structure of coping. Journal of health and social behavior. 1978b;19:2–21. [PubMed] [Google Scholar]
- Perry B. The mismatch between income measures and direct outcome measures of poverty. Social Policy Journal of New Zealand. 2002;19:101–127. [Google Scholar]
- Pickle LW, Mungiole M, Jones GK, White AA. Atlas of United States Mortality. US Department of Health and Human Services Public Health Service; 1996. Electronic version. [Google Scholar]
- Price RH, Choi JN, Vinokur AD. Links in the chain of adversity following job loss: How financial strain and loss of personal control lead to depression, impaired functioning, and poor health. Journal of Occupational Health Psychology. 2002;7:302–312. doi: 10.1037//1076-8998.7.4.302. [DOI] [PubMed] [Google Scholar]
- Raiford JL, Seth P, Braxton ND, DiClemente RJ. Masculinity, condom use self-efficacy and abusive responses to condom negotiation: the case for HIV prevention for heterosexual African-American men. Sex Health. 2013;10:467–469. doi: 10.1071/SH13011. [DOI] [PubMed] [Google Scholar]
- Scheppers E, van DE, Dekker J, Geertzen J, Dekker J. Potential barriers to the use of health services among ethnic minorities: a review. Fam Pract. 2006;23:325–348. doi: 10.1093/fampra/cmi113. [DOI] [PubMed] [Google Scholar]
- Shelton RC, Goldman RE, Emmons KM, Sorensen G, Allen JD. An investigation into the social context of low-income, urban Black and Latina women: implications for adherence to recommended health behaviors. Health Educ Behav. 2011;38:471–481. doi: 10.1177/1090198110382502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Short K. Material and Financial Hardship and Income-Based Poverty Measures in the USA. Journal of Social Policy. 2005;34:21–38. [Google Scholar]
- Siahpush M, Borland R, Scollo M. Smoking and financial stress. Tobacco control. 2003;12:60–66. doi: 10.1136/tc.12.1.60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Siahpush M, McNeill A, Borland R, Fong GT. Socioeconomic variations in nicotine dependence, self-efficacy, and intention to quit across four countries: findings from the International Tobacco Control (ITC) Four Country Survey. Tob Control. 2006;15(Suppl 3):iii71–iii75. doi: 10.1136/tc.2004.008763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Siahpush M, Spittal M, Singh GK. Association of smoking cessation with financial stress and material well-being: Results from a prospective study of a population-based national survey. American Journal of Public Health. 2007;97:2281–2287. doi: 10.2105/AJPH.2006.103580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Strecher VJ, DeVellis BM, Becker MH, Rosenstock IM. The role of self-efficacy in achieving health behavior change. Health Educ Q. 1986;13:73–92. doi: 10.1177/109019818601300108. [DOI] [PubMed] [Google Scholar]
- Tucker CM, Butler AM, Loyuk IS, Desmond FF, Surrency SL. Predictors of a health-promoting lifestyle and behaviors among low-income African American mothers and white mothers of chronically ill children. J Natl Med Assoc. 2009;101:103–110. doi: 10.1016/s0027-9684(15)30821-x. [DOI] [PubMed] [Google Scholar]
- Tucker-Seeley RD, Harley AE, Stoddard AM, Sorensen GG. Financial hardship and self-rated health among low-income housing residents. Health Educ Behav. 2013;40:442–448. doi: 10.1177/1090198112463021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tucker-Seeley RD, Li Y, Sorensen G, Subramanian SV. Lifecourse socioeconomic circumstances and multimorbidity among older adults. BMC Public Health. 2011;11:313. 313–11. doi: 10.1186/1471-2458-11-313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tucker-Seeley RD, Li Y, Subramanian SV, Sorensen G. Financial hardship and mortality among older adults using the 1996–2004 Health and Retirement Study. Ann Epidemiol. 2009;19:850–857. doi: 10.1016/j.annepidem.2009.08.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- United States Department of Labor. The African American Labor Force in the Recovery 2012 [Google Scholar]
- Vinokur AD, Schul Y. Mastery and inoculation against setbacks as active ingredients in the JOBS intervention for the unemployed. J Consult Clin Psychol. 1997;65:867–877. doi: 10.1037//0022-006x.65.5.867. [DOI] [PubMed] [Google Scholar]
- Wallace LS, Chisolm DJ, Abdel-Rasoul M, DeVoe JE. Survey mode matters: adults' self-reported statistical confidence, ability to obtain health information, and perceptions of patient-health-care provider communication. J Health Psychol. 2013;18:1036–1045. doi: 10.1177/1359105312470125. [DOI] [PubMed] [Google Scholar]
- Whelan CT, Layte R, Maitre B, Nolan B. Income, deprivation, and economic strain: An analysis of the European Community Household Panel. European Sociological Review. 2001;17:357–372. [Google Scholar]
- Williams DR. The health of men: structured inequalities and opportunities. Am J Public Health. 2003;93:724–731. doi: 10.2105/ajph.93.5.724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams DR, Mohammed SA, Leavell J, Collins C. Race, socioeconomic status, and health: complexities, ongoing challenges, and research opportunities. Ann N Y Acad Sci. 2010;1186:69–101. doi: 10.1111/j.1749-6632.2009.05339.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Woods VD, Montgomery SB, Belliard JC, Ramirez-Johnson J, Wilson CM. Culture, black men, and prostate cancer: what is reality? Cancer Control. 2004;11:388–396. doi: 10.1177/107327480401100606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xanthos C, Treadwell HM, Holden KB. Social determinants of health among African American men. Journal of Men's Health. 2010;7:11–19. [Google Scholar]