Abstract
Improving mitochondrial oxidant scavenging may be a viable strategy for the treatment of insulin resistance and diabetes. Mice overexpressing the mitochondrial matrix isoform of superoxide dismutase (sod2tg mice) and/or transgenically expressing catalase within the mitochondrial matrix (mcattg mice) have increased scavenging of O2˙ˉ and H2O2, respectively. Furthermore, muscle insulin action is partially preserved in high fat (HF)-fed mcattg mice. The goal of the current study was to test the hypothesis that increased O2˙ˉ scavenging alone or in combination with increased H2O2 scavenging (mtAO mice) enhances in vivo muscle insulin action in the HF-fed mouse. Insulin action was examined in conscious, unrestrained and unstressed wild type (WT), sod2tg, mcattg and mtAO mice using hyperinsulinemic-euglycemic clamps (insulin clamps) combined with radioactive glucose tracers following sixteen weeks of normal chow or HF (60% calories from fat) feeding. Glucose infusion rates, whole body glucose disappearance, and muscle glucose uptake during the insulin clamp were similar in chow- and HF-fed WT and sod2tg mice. Consistent with our previous work, HF-fed mcattg mice had improved muscle insulin action, however, an additive effect was not seen in mtAO mice. Insulin-stimulated Akt phosphorylation in muscle from clamped mice was consistent with glucose flux measurements. These results demonstrate that increased O2˙ˉ scavenging does not improve muscle insulin action in the HF-fed mouse alone or when coupled to increased H2O2 scavenging.
Introduction
Overnutrition can lead to the development of insulin resistance and type 2 diabetes. Increased production of mitochondrial oxidant species has been proposed as central to the etiology of diet-induced insulin resistance [1]. In the presence of overnutrition, the mitochondrial electron transport system (ETS) is overloaded with electrons donated from reducing equivalents (e.g. NADH and FADH2), resulting in the increased production of membrane impermeable superoxide ion (O2˙ˉ). In the mitochondrial matrix, O2˙ˉ is dismutated by manganese superoxide dismutase (SOD2) to hydrogen peroxide (H2O2). Both O2˙ˉ and H2O2 have been proposed to serve as metabolic sensors functionally linking redox biology to insulin sensitivity [2, 3]. Increased O2˙ˉ scavenging by increased SOD2 activity has been proposed to have beneficial effects on muscle insulin sensitivity. This proposal is complicated by the fact that O2˙ˉ scavenging comes at the expense of increased H2O2 production [4].
Transgenic overexpression of SOD2 (sod2 tg) is a genetic model of enhanced mitochondrial O2˙ˉ scavenging. Overexpression of SOD2 protects against radiation-induced cell death [5], oxygen injury [6], and peroxidative damage to membrane lipids [7]. SOD2 overexpression has also been shown to enhance mitochondrial oxidative capacity [8] and inhibit tumor cell growth [9, 10], effects that are linked to increased production or accumulation of H2O2 [9, 11, 12]. Mice with transgenic expression of catalase, a peroxisomal enzyme, within the mitochondrial matrix (mcat tg) are a model of enhanced mitochondrial H2O2 scavenging in striated muscle [13]. mcat tg mice have increased lifespan [13] and we have recently demonstrated that mcat tg mice are partially protected against diet-induced insulin resistance [3].
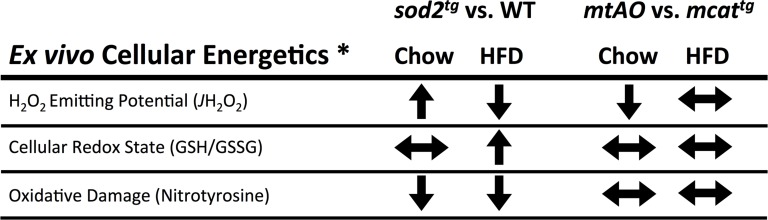
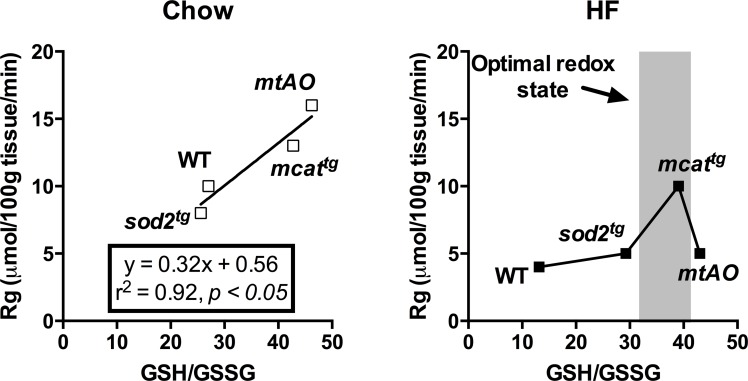
In a previous report, we examined the independent and combined effects of enhanced scavenging of O2˙ˉ and H2O2 in the muscle of HF-fed mice using sod2 tg, mcat tg and mtAO double transgenic mice generated by crossing sod2 tg and mcat tg [4]. In that report, it was found that cellular redox state (GSH/GSSG), mitochondrial oxidant emitting potential (JH2O2) and oxidative damage (nitrotyrosine accumulation) are differentially altered by HF feeding (Summarized in Fig 1). In particular, HF diet-induced elevations in JH2O2 and oxidation of the cellular redox environment (decreased GSH/GSSG) are ameliorated in both sod2 tg and mcat tg mice. Furthermore, mtAO mice have additive protection from HF diet-induced elevations in JH2O2 relative to mcat tg mice. Altogether, these findings suggest that enhanced scavenging of O2˙ˉ may improve muscle insulin action in the HF-fed mouse.
Fig 1. Summary of effects of diet and transgenic expression of SOD2 and/or catalase on oxidant production and cellular redox state.
* Data adapted from Kang et al. 2012 [4].
In the current report, we tested the hypothesis that enhanced mitochondrial O2˙ˉ scavenging improves insulin action in HF-fed mice. To assess insulin action, hyperinsulinemic-euglycemic clamps (insulin clamp) combined with isotopic glucose tracers were performed in conscious, unrestrained and unstressed animals. This hypothesis was tested in sod2 tg mice with normal H2O2 scavenging capacity and mtAO mice with enhanced H2O2 scavenging capacity.
Methods and Materials
Animals and Ethical Approvals
All mice were on the C57BL/6J background and housed in cages under conditions of controlled temperature and humidity with a 12-h light/dark cycle. As we have done previously [4], sod2 tg mice with ~3 fold overexpression of SOD2 in muscle were bred with mcat tg mice generously provided by Dr. Peter Rabinovitch of the University of Washington [13]. This breeding scheme generated four distinct genotypes: wild type (WT), sod2 tg, mcat tg and double transgenic (mtAO) mice. All mice were fed either a chow or HF diet (F3282, BioServ), which contains 60% calories as fat, for 16 weeks. Body composition was determined using an mq10 nuclear magnetic resonance analyzer (Brucker Optics). The Vanderbilt University Medical Center and the East Carolina University Animal Care and Use Committees approved all animal procedures.
Hyperinsulinemic-Euglycemic Clamp
In preparation for a hyperinsulinemic-euglycemic, hereafter referred to as an insulin clamp, mice had catheters implanted in the left carotid artery and the right jugular vein for blood sampling and intravenous infusion, respectively, at least 5 days prior to the study [14]. The insulin clamp procedure used in these studies is unique in that it has been validated from a number of standpoints including: stability of blood glucose over time, absence of stress (no increase in catecholamine concentrations), insulin levels and absence of a fall in hematocrit [14]. The entire insulin clamp procedure has been visually published [15] and described in depth [14, 16] previously. Readers are also referred to a publicly available guide to the surgery and clamp procedure that is maintained by the Vanderbilt Mouse Metabolic Phenotyping Center, found at: (http://www.mc.vanderbilt.edu/documents/mmpc/files/2012%20Lab%20Manual(1).pdf).
In the current study, the insulin clamp coupled with isotopic tracer techniques was performed in a total of 75 conscious, unstressed mice. Mice were fasted for 5 hours beginning at ~ 7 am on the day of the insulin clamp. Ninety minutes prior to starting the insulin infusion (-90 min), [3-3H]glucose was primed (2.4 μCi) and continuously infused at 0.04 μCi/min into the jugular vein catheter and then increased to 0.12 μCi/min during the insulin clamp. Baseline blood or plasma parameters were determined as the mean of values obtained in arterial blood collected at -15 and -5 min. At time 0, infusion of human insulin (4 mU/kg/min) was started and continued for the entire clamp (155 min). This amount of insulin is a high, but physiological, concentration that was used to ensure insulin stimulation in tissues of HF-fed mice but allow for discrimination of differences between groups. During the insulin infusion, blood glucose was clamped at ~150 mg/dL by a variable infusion of exogenous glucose (50% dextrose). Mice received heparinized saline-washed erythrocytes from donor mice at 5 μL/min to prevent a fall of hematocrit. Blood glucose was monitored and the glucose infusion rate (GIR) was adjusted every 10 min throughout the clamp. Whole blood samples (~ 50 μl) were taken from 80–120 min for the determination of plasma [3-3H]glucose. Blood samples were taken to measure plasma insulin at t = 100 and 120min. At 120min, 13μCi of 2-[14C]deoxyglucose ([14C]2-DG) was administered as an intravenous bolus. Blood samples were then taken at 2, 15, 25, and 35min following the bolus for the determinations of plasma [14C]2-DG levels. After the last blood sample was taken, mice were anesthetized with phenobarbital and tissues were removed and frozen in liquid nitrogen.
Processing of Plasma and Tissue Samples
Plasma insulin was determined using an insulin ELISA kit (Millipore). Non-esterified fatty acid (NEFA) concentrations were measured using an enzymatic colorimetric assay (NEFA C kit, Wako Chemicals). Radioactivity of plasma and tissue samples was measured as previously described [14].
Glucose appearance (Ra) and disappearance (Rd) rates were calculated using non-steady state equations [17]. Endogenous glucose production (EndoRa) was determined by subtracting the glucose infusion rate from total Ra. A glucose metabolic index for tissues (Rg) was calculated as described previously [18].
Western Blotting
Gastrocnemius muscle samples were homogenized in buffer containing (pH = 7.5): 50 mM Tris, 1 mM EDTA, 1 mM EGTA, 10% glycerol, 1% Triton X-100, 1 mM DTT, 1 mM PMSF, 5 μg/mL protease inhibitor cocktail, 50 mM NaF, 5 mM sodium pyrophosphate, and centrifuged at 13,000xg for 20min at 4°C. The protein concentration was then determined and homogenates were run on SDS-PAGE gels. Phosphorylated and total Akt/PKB were probed using phospho-Akt (Ser473) and Akt primary antibodies (Cell Signaling) and IRdye 800CW secondary antibodies (LI-COR Biosciences). Band densities were quantified using Odyssey (LI-COR Biosciences) software.
Statistical Analysis
Data are expressed as mean ± SEM. Statistical comparisons were made between WT and sod2 tg mice or mcat tg and mtAO mice using unpaired student’s t-test or two-way ANOVA with Tukey post-hoc test when appropriate. The significance level was set at p<0.05.
Results
Basal metabolic characteristics
WT, sod2 tg, mcat tg, and mtAO mice were fed either normal chow or a HF diet for 16 weeks and studied at 19 weeks of age. On normal chow, no genotype differences were observed in body weight; however, mtAO mice displayed lower fasting glucose and insulin compared to mcat tg littermates (Table 1). HF feeding increased body weight, basal 5-h fasting glucose and insulin as expected in all genotypes and was not affected by SOD2 overexpression. Basal arterial NEFA levels were not altered by genotype or diet. The percentage of body fat was increased by HF feeding, but not affected by genotype.
Table 1. Basal (5h-fasted) and insulin clamp characteristics of sod2 tg, mcat tg, and mtAO mice.
| Chow | HF Diet | Chow | HF Diet | |||||
|---|---|---|---|---|---|---|---|---|
| WT | sod2 tg | WT | sod2 tg | mcat tg | mtAO | mcat tg | mtAO | |
| n (female/male) | 11 (4/7) | 9 (4/5) | 11 (5/6) | 10 (4/6) | 6 (3/3) | 7 (4/3) | 11 (6/5) | 10 (5/5) |
| Body weight (g) | 24 ± 1 | 25 ± 1 | 36 ± 2 † | 35 ± 2 † | 23 ± 2 | 24 ± 1 | 33 ± 2 † | 33 ± 2 † |
| Fat Mass (%) | 9 ± 1 | 10 ± 1 | 30 ± 2 † | 33 ± 4 † | 9 ± 1 | 9 ± 1 | 28 ± 3 † | 26 ± 5 † |
| Arterial Glucose (mg∙dL -1) | ||||||||
| Basal | 121 ± 6 | 129 ± 5 | 158 ± 8 † | 150 ± 4 † | 132 ± 8 | 110 ± 7 § | 134 ± 5 | 142 ± 5 † |
| Insulin clamp ƒ | 156 ± 3 | 149 ± 6 | 155 ± 3 | 147 ± 7 | 151 ± 6 | 156 ± 2 | 159 ± 3 | 155 ± 3 |
| Insulin (ng∙mL -1) | ||||||||
| Basal | 0.7 ± 0.1 | 0.8 ± 0.1 | 1.8 ± 0.5 † | 1.5 ± 0.4 † | 0.8 ± 0.1 | 0.4±0.1 § | 1.6 ± 0.3 † | 1.5 ± 0.3 † |
| Insulin clamp ƒ | 2.8 ± 0.5 | 2.8 ± 0.3 | 3.5 ± 0.3 | 3.6 ± 0.4 | 3.4 ± 0.7 | 3.6 ± 0.6 | 3.7 ± 0.4 | 3.0 ± 0.3 |
| NEFA (mM) | ||||||||
| Basal | 0.9±0.10 | 1.0±0.06 | 0.7±0.04 | 0.8±0.08 | 0.9±0.08 | 0.8±0.06 | 0.7±0.04 | 0.7±0.03 |
| Insulin clamp ƒ | 0.4±0.05 | 0.5±0.04 | 0.5±0.05 | 0.4±0.03 | 0.4±0.03 | 0.3±0.02 | 0.4±0.03 | 0.4±0.04 |
ƒ Data are presented as the average of values obtained from 80–120 min during the hyperinsulinemic-euglycemic clamp.
† p<0.05 compared to Chow within the same genotype.
§ p<0.05 compared to Chow mcat tg.
All data are expressed as mean ± SEM.
Hyperinsulinemic-euglycemic clamps
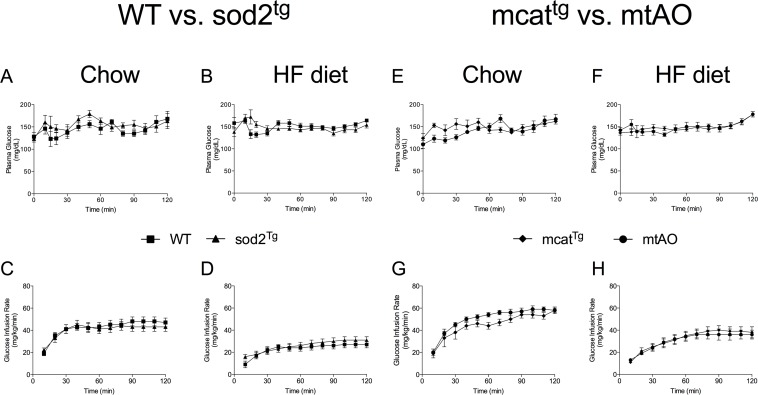
Blood glucose was maintained at ~150 mg/dL during the insulin clamp in all groups of mice using a variable glucose infusion (Table 1, Fig 2A, 2B, 2E and 2F). Infusion of insulin (4 mU/kg/min) increased plasma insulin to a similar extent in all groups of mice (Table 1). Insulin-induced suppression of arterial NEFA was not affected by genotype. HF feeding decreased glucose infusion rate (GIR) in all four genotypes relative to chow, but, consistent with our previous findings [3], GIR was partially protected in HF-fed mcat tg mice compared to WT (average GIR during steady state: WT -27.18 ± 3.335, mcat tg -40.55 ± 4.424, p<0.05). GIR was not improved in chow or HF-fed sod2 tg or mtAO mice compared to WT (Fig 2C and 2D) or mcat tg (Fig 2G and 2H) mice, respectively.
Fig 2. SOD2 overexpression does not augment glucose infusion rates in HF-fed mice during an insulin clamp.
(A-D) Blood glucose was maintained at ~150 mg/dL in all groups (diet and genotype) during the insulin clamp by variable venous infusion of 50% glucose. (E-H) Glucose infusion rate (GIR) over the 120-minute duration of the insulin clamp.
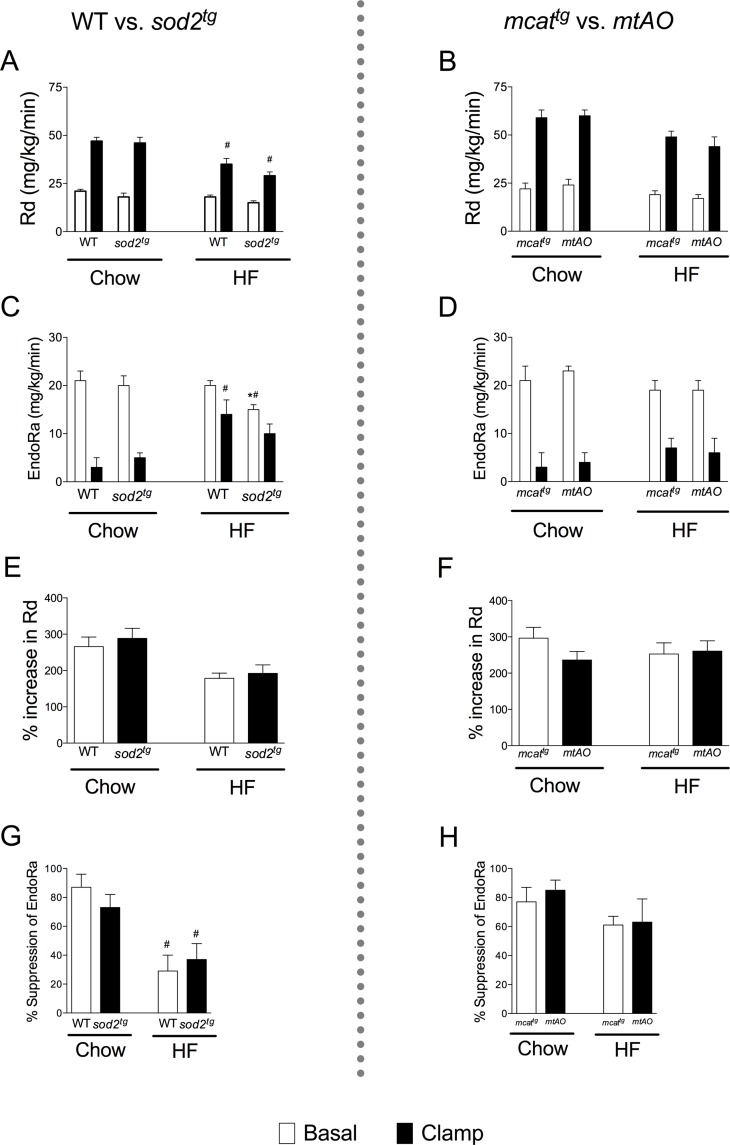
HF diet-induced impairment of clamp Rd was not attenuated in sod2 tg compared to WT (Fig 3A) or mtAO in relation to mcat tg (Fig 3C). Basal, but not insulin-suppressed, endoRa was decreased in HF-fed sod2 tg mice, but not chow-fed sod2 tg mice compared to WT (Fig 3B). EndoRa was not affected under basal or insulin clamp conditions in chow or HF-fed mtAO mice (Fig 3D). The percentage increase in Rg (Fig 3E and 3F) and suppression of EndoRa (Fig 3G and 3H) in response to insulin were not altered by SOD2 overexpression.
Fig 3. Rates of endogenous glucose production (EndoRa) and glucose disappearance (Rd) during the insulin clamp.
Rd was calculated using the tracer [3-3H]glucose dilution method in SOD2 overexpressing WT (A) and mcat tg (B) mice. EndoRa was determined by subtracting the glucose infusion rate from total Ra in sod2 overexpressing WT (C) and mcat tg (D) mice. Insulin-stimulated increase in Rg (E and F) and suppression of EndoRa (G and H) are presented as percentage (%) of basal rates. *p<0.05 compared with sod2 tg overexpressing mice (WT or mcat tg) within a diet; # p<0.05 compared with chow within a genotype.
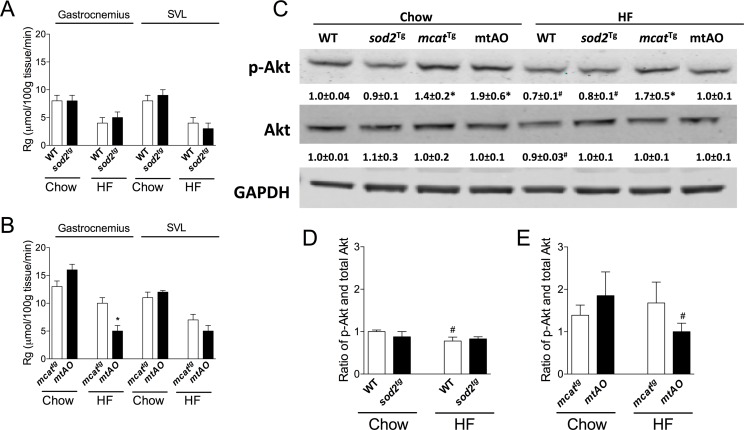
SOD2 overexpression did not augment Rg in chow- or HF-fed WT (Fig 4A) mice. Gastrocnemius Rg in normal chow-fed mtAO mice was not changed but was decreased in HF-fed mtAO mice compared to mcat tg (Fig 4B). SVL Rg in mtAO and mcat tg mice was not different (data not shown).
Fig 4. Divergent effects of SOD2 overexpression on muscle glucose uptake (Rg) and insulin signaling in HF-fed WT and mcat tg mice.
Non-metabolizable glucose analog [14C]2-deoxyglucose was administered as an intravenous bolus to determine muscle glucose uptake (Rg) using liquid scintillation counting in SOD2 overexpressing WT (A) and mcat tg (B) mice. Insulin signaling was measured in tissue homogenates extracted from gastrocnemius, applied to 4–12% SDS-PAGE gel and Western blotted with anti-phospho-Akt (Ser473) or anti-total Akt antibodies. Values are expressed as mean ± SEM of integrated intensity and representative bands are presented (C). Ratio of phosphorylated-Akt to total Akt was calculated in SOD2 overexpressing WT (D) and mcattg (E) mice. n = 4–6. *p<0.05 compared with sod2 tg or WT within a diet; # p<0.05 compared with chow within a genotype. SVL, superficial vastus lateralis.
Insulin signaling
Insulin signaling was assessed in gastrocnemius by measuring the ratio of phosphorylated to total expression of Akt, a hub of the insulin signaling cascade (Fig 4C). The ratio of phosphorylated to total Akt was not altered in chow- or HF-fed sod2 tg mice (Fig 4D). However, the ratio of phosphorylated to total Akt was decreased in HF-fed mtAO compared to mcat tg mice (Fig 3E). Overall Akt phosphorylation was consistent with observed differences in muscle glucose uptake.
Discussion
Genetic models that modulate the cellular redox environment, like those used in the present study, may provide insight into targets that could be used to treat insulin resistance and diabetes. In this report, we tested the hypothesis that increased O2˙ˉ scavenging capacity by SOD2 overexpression would prevent muscle insulin resistance in HF-fed mice. The data provided do not support this hypothesis as enhanced scavenging of O2˙ˉ failed to improve muscle insulin action in vivo. This conclusion is based on findings in both sod2 tg mice and mtAO mice that have enhanced scavenging of both O2˙ˉ and H2O2. The current study made conclusions based on evaluations of both male and female mice with no regard for estrous cycle. There is considerable evidence that female sex hormones (e.g. estrogen and progesterone) impact insulin sensitivity (reviewed by [19]). Moreover, progesterone, but not estrogen, has been demonstrated to increase mitochondrial oxidant production in non-menopausal women [20]. Therefore, the unknown contribution of these factors is a caveat to the findings presented here.
Previous studies have demonstrated that HF-fed sod2 tg mice display improved glucose [2, 21] and insulin tolerance [2]. Glucose tolerance is determined by the insulin secretory response, insulin clearance, non-insulin-mediated glucose disposal, and insulin-mediated glucose disposal [22]. Notably, numerous studies have shown that oxidative stress impairs insulin secretion [23, 24]. The increased oxidative burden incurred by overexpression of SOD2 in the pancreas would be predicted to cause glucose intolerance independent of changes in muscle insulin action. The measurement of insulin tolerance is also complicated by numerous factors including hypoglycemic counterregulation and the variable stimulus due to a spike of insulin [22]. SOD2 overexpressing HF-fed mice were reported to have a very small improvement on insulin tolerance compared to WT (~15%), but still remained considerably impaired in relation to the insulin tolerance in lean mice [2]. The present study, in which we clearly show that insulin action is unaffected by SOD2 overexpression, is largely consistent with the previous measurement of insulin tolerance. Moreover, our finding complements recent work demonstrating that heterozygous knockout of SOD2 does not impair insulin action in chow- or HF-fed mice [25]. Notably, overexpression of sod2 in skeletal muscle using in vivo electroporation has been shown to enhance glucose uptake in the HF-fed rat [26]. However, it should be noted that sod2 overexpression in this report was accompanied by an increase in the activity of glutathione peroxidase, which catalyzes the breakdown of H2O2, and a decrease in protein carbonylation. Thus, the net effect of increased sod2 expression in this model was reduction, not oxidation, of the cellular redox environment. Therefore, we contend that the enhanced insulin sensitivity observed by sod2 overexpression in this report was a consequence of enhanced scavenging of H2O2, not O2˙ˉ.
Previous work has demonstrated that H2O2 can either increase [27] or decrease [28, 29] skeletal muscle insulin signaling and glucose uptake. H2O2-mediated impairments in insulin signaling are associated with a selective loss of insulin receptor substrate (IRS)-1 and IRS-2 proteins, in part related to a p38 mitogen-activated protein kinase-dependent mechanism [30]. A recent paper has demonstrated that both mcat tg and mtAO mice are protected against oxidation of the cellular glutathione pool on both chow and HF diet [4] (Fig 1). Importantly, when considered in the context of the current report, these previous findings reveal a paradoxical situation where, despite a reduced cellular redox environment, combined enhancement of O2˙ˉ and H2O2 scavenging fails to improve muscle insulin action in response to HF feeding. Consistent with recently reported findings [28–30], plotting Rg obtained in the current study as a function of glutathione redox state (GSH/GSSG) in the skeletal muscle of mice from our previous study [4] reveals two distinct relationships. First, that Rg is positively correlated with insulin-stimulated Rg in chow-fed mice (Fig 5A). However, this linear relationship is incompatible in mice fed a HF diet because insulin-stimulated Rg is low when GSH/GSSG exists above or below a potentially “critical” range (Fig 5B). These results altogether support a paradigm where low rates of mitochondrial H2O2 production (JH2O2) play a role in maintaining cellular homeostasis (i.e., prevents excessive reduction of cellular redox environment) while a sustained elevation in mitochondrial JH2O2 shifts the cellular redox environment to a more oxidized state and worsens muscle insulin action [31].
Fig 5. The relationship between glutathione redox state and muscle glucose uptake in chow and HF-fed mice.
Rg determined by 2[14C]deoxyglucose during the insulin clamp plotted as a function of glutathione redox state (GSH/GSSG) in gastrocnemius of chow- (A) and HF-fed (B) mice. GSH/GSSG values were adapted from Kang et al. [4].
Conclusions
The current report demonstrates that SOD2 overexpression does not alleviate muscle insulin resistance even when combined with increased scavenging of its reaction product, H2O2. This study, combined with our earlier work using mcat tg mice [3, 4], demonstrate that drugs designed to mitigate H2O2 production and/or enhance H2O2 scavenging will have a greater benefit for the treatment of diabetes and insulin resistance than those that target O2˙ˉ.
Data Availability
All relevant data are within the paper and its Supporting Information files.
Funding Statement
This work was supported by National Institutes of Health Grants DK054902 (to D.H.W.), DK059637 (Vanderbilt-NIDDK Mouse Metabolic Phenotyping Center), DK007061 (to D.S.L.) and DK073488 (to P.D.N.). The authors would also like to acknowledge the Diabetes Research and Training Center (DK20593). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1. Houstis N, Rosen ED, Lander ES. Reactive oxygen species have a causal role in multiple forms of insulin resistance. Nature. 2006;440(7086):944–8. Epub 2006/04/14. nature04634 [pii] 10.1038/nature04634 . [DOI] [PubMed] [Google Scholar]
- 2. Hoehn KL, Salmon AB, Hohnen-Behrens C, Turner N, Hoy AJ, Maghzal GJ, et al. Insulin resistance is a cellular antioxidant defense mechanism. Proc Natl Acad Sci U S A. 2009;106(42):17787–92. Epub 2009/10/07. 0902380106 [pii] 10.1073/pnas.0902380106 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Anderson EJ, Lustig ME, Boyle KE, Woodlief TL, Kane DA, Lin C-T, et al. Mitochondrial H2O2 emission and cellular redox state link excess fat intake to insulin resistance in both rodents and humans. The Journal of Clinical Investigation. 2009;119(3):573–81. 10.1172/JCI37048 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Kang L, Lustig ME, Bonner JS, Lee-Young RS, Mayes WH, James FD, et al. Mitochondrial Anti-Oxidative Capacity Regulates Muscle Glucose Uptake in the Conscious Mouse: Effect of Exercise and Diet. J Appl Physiol. 2012. Epub 2012/06/02. japplphysiol.01344.2011 [pii] 10.1152/japplphysiol.01344.2011 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Motoori S, Majima HJ, Ebara M, Kato H, Hirai F, Kakinuma S, et al. Overexpression of mitochondrial manganese superoxide dismutase protects against radiation-induced cell death in the human hepatocellular carcinoma cell line HLE. Cancer Res. 2001;61(14):5382–8. Epub 2001/07/17. . [PubMed] [Google Scholar]
- 6. Wispe JR, Warner BB, Clark JC, Dey CR, Neuman J, Glasser SW, et al. Human Mn-superoxide dismutase in pulmonary epithelial cells of transgenic mice confers protection from oxygen injury. J Biol Chem. 1992;267(33):23937–41. Epub 1992/11/25. . [PubMed] [Google Scholar]
- 7. Ibrahim W, Lee US, Yen HC, St Clair DK, Chow CK. Antioxidant and oxidative status in tissues of manganese superoxide dismutase transgenic mice. Free Radic Biol Med. 2000;28(3):397–402. Epub 2000/03/04. . [DOI] [PubMed] [Google Scholar]
- 8. Silva JP, Shabalina IG, Dufour E, Petrovic N, Backlund EC, Hultenby K, et al. SOD2 overexpression: enhanced mitochondrial tolerance but absence of effect on UCP activity. Embo j. 2005;24(23):4061–70. Epub 2005/11/11. 10.1038/sj.emboj.7600866 ; PubMed Central PMCID: PMCPmc1356306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Kim H, You S, Kong BW, Foster LK, Farris J, Foster DN. Necrotic cell death by hydrogen peroxide in immortal DF-1 chicken embryo fibroblast cells expressing deregulated MnSOD and catalase. Biochim Biophys Acta. 2001;1540(2):137–46. Epub 2001/08/22. . [DOI] [PubMed] [Google Scholar]
- 10. Venkataraman S, Jiang X, Weydert C, Zhang Y, Zhang HJ, Goswami PC, et al. Manganese superoxide dismutase overexpression inhibits the growth of androgen-independent prostate cancer cells. Oncogene. 2005;24(1):77–89. Epub 2004/11/16. 10.1038/sj.onc.1208145 . [DOI] [PubMed] [Google Scholar]
- 11. Zhang Z, Zhang X, Hou G, Sha W, Reynolds GP. The increased activity of plasma manganese superoxide dismutase in tardive dyskinesia is unrelated to the Ala-9Val polymorphism. Journal of psychiatric research. 2002;36(5):317–24. Epub 2002/07/20. . [DOI] [PubMed] [Google Scholar]
- 12. Dasgupta J, Subbaram S, Connor KM, Rodriguez AM, Tirosh O, Beckman JS, et al. Manganese superoxide dismutase protects from TNF-alpha-induced apoptosis by increasing the steady-state production of H2O2. Antioxid Redox Signal. 2006;8(7–8):1295–305. Epub 2006/08/17. 10.1089/ars.2006.8.1295 . [DOI] [PubMed] [Google Scholar]
- 13. Schriner SE, Linford NJ, Martin GM, Treuting P, Ogburn CE, Emond M, et al. Extension of murine life span by overexpression of catalase targeted to mitochondria. Science. 2005;308(5730):1909–11. Epub 2005/05/10. 1106653 [pii] 10.1126/science.1106653 . [DOI] [PubMed] [Google Scholar]
- 14. Ayala JE, Bracy DP, McGuinness OP, Wasserman DH. Considerations in the design of hyperinsulinemic-euglycemic clamps in the conscious mouse. Diabetes. 2006;55(2):390–7. Epub 2006/01/31. 55/2/390 [pii]. . [DOI] [PubMed] [Google Scholar]
- 15. Ayala JE, Bracy DP, Malabanan C, James FD, Ansari T, Fueger PT, et al. Hyperinsulinemic-euglycemic clamps in conscious, unrestrained mice. J Vis Exp. 2011;(57). Epub 2011/12/01. 10.3791/3188 ; PubMed Central PMCID: PMCPmc3308587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Ayala JE, Samuel VT, Morton GJ, Obici S, Croniger CM, Shulman GI, et al. Standard operating procedures for describing and performing metabolic tests of glucose homeostasis in mice. Dis Model Mech. 2010;3(9–10):525–34. Epub 2010/08/18. dmm.006239 [pii] 10.1242/dmm.006239 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Altszuler N, De Bodo RC, Steele R, Wall JS. Carbohydrate metabolism of hypophysectomized dogs as studied with radioactive glucose. Am J Physiol. 1956;187(1):25–31. Epub 1956/10/01. . [DOI] [PubMed] [Google Scholar]
- 18. Kraegen EW, James DE, Jenkins AB, Chisholm DJ. Dose-response curves for in vivo insulin sensitivity in individual tissues in rats. Am J Physiol. 1985;248(3 Pt 1):E353–62. Epub 1985/03/01. . [DOI] [PubMed] [Google Scholar]
- 19. Livingstone C, Collison M. Sex steroids and insulin resistance. Clinical science (London, England: 1979). 2002;102(2):151–66. Epub 2002/02/09. . [DOI] [PubMed] [Google Scholar]
- 20. Kane DA, Lin CT, Anderson EJ, Kwak HB, Cox JH, Brophy PM, et al. Progesterone increases skeletal muscle mitochondrial H2O2 emission in nonmenopausal women. Am J Physiol Endocrinol Metab. 2011;300(3):E528–35. Epub 2010/12/30. 10.1152/ajpendo.00389.2010 ; PubMed Central PMCID: PMCPmc3064007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Liu Y, Qi W, Richardson A, Van Remmen H, Ikeno Y, Salmon AB. Oxidative damage associated with obesity is prevented by overexpression of CuZn- or Mn-superoxide dismutase. Biochem Biophys Res Commun. 2013;438(1):78–83. Epub 2013/07/23. 10.1016/j.bbrc.2013.07.029 ; PubMed Central PMCID: PMCPmc3768142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Hughey CC, Wasserman DH, Lee-Young RS, Lantier L. Approach to assessing determinants of glucose homeostasis in the conscious mouse. Mammalian genome: official journal of the International Mammalian Genome Society. 2014;25(9–10):522–38. Epub 2014/07/31. 10.1007/s00335-014-9533-z ; PubMed Central PMCID: PMCPmc4167555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Chiang YF, Shaw HM, Yang MF, Huang CY, Hsieh CH, Chao PM. Dietary oxidised frying oil causes oxidative damage of pancreatic islets and impairment of insulin secretion, effects associated with vitamin E deficiency. The British journal of nutrition. 2011;105(9):1311–9. Epub 2011/01/06. 10.1017/s0007114510005039 . [DOI] [PubMed] [Google Scholar]
- 24. Drews G, Krippeit-Drews P, Dufer M. Oxidative stress and beta-cell dysfunction. Pflugers Arch. 2010;460(4):703–18. Epub 2010/07/24. 10.1007/s00424-010-0862-9 . [DOI] [PubMed] [Google Scholar]
- 25. Kang L, Dai C, Lustig ME, Bonner JS, Mayes WH, Mokshagundam S, et al. Heterozygous SOD2 deletion impairs glucose-stimulated insulin secretion, but not insulin action, in high-fat-fed mice. Diabetes. 2014;63(11):3699–710. Epub 2014/06/21. 10.2337/db13-1845 ; PubMed Central PMCID: PMCPmc4207395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Boden MJ, Brandon AE, Tid-Ang JD, Preston E, Wilks D, Stuart E, et al. Overexpression of manganese superoxide dismutase ameliorates high-fat diet-induced insulin resistance in rat skeletal muscle. Am J Physiol Endocrinol Metab. 2012;303(6):E798–805. Epub 2012/07/26. 10.1152/ajpendo.00577.2011 ; PubMed Central PMCID: PMCPmc3468429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Higaki Y, Mikami T, Fujii N, Hirshman MF, Koyama K, Seino T, et al. Oxidative stress stimulates skeletal muscle glucose uptake through a phosphatidylinositol 3-kinase-dependent pathway. Am J Physiol Endocrinol Metab. 2008;294(5):E889–97. Epub 2008/02/28. 10.1152/ajpendo.00150.2007 ; PubMed Central PMCID: PMCPmc2882683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Maddux BA, See W, Lawrence JC Jr, Goldfine AL, Goldfine ID, Evans JL. Protection against oxidative stress-induced insulin resistance in rat L6 muscle cells by mircomolar concentrations of alpha-lipoic acid. Diabetes. 2001;50(2):404–10. Epub 2001/03/29. . [DOI] [PubMed] [Google Scholar]
- 29. Chung SS, Kim M, Youn BS, Lee NS, Park JW, Lee IK, et al. Glutathione peroxidase 3 mediates the antioxidant effect of peroxisome proliferator-activated receptor gamma in human skeletal muscle cells. Mol Cell Biol. 2009;29(1):20–30. Epub 2008/10/22. 10.1128/mcb.00544-08 ; PubMed Central PMCID: PMCPmc2612482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Archuleta TL, Lemieux AM, Saengsirisuwan V, Teachey MK, Lindborg KA, Kim JS, et al. Oxidant stress-induced loss of IRS-1 and IRS-2 proteins in rat skeletal muscle: role of p38 MAPK. Free Radic Biol Med. 2009;47(10):1486–93. Epub 2009/08/26. S0891-5849(09)00500-0 [pii] 10.1016/j.freeradbiomed.2009.08.014 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Fisher-Wellman KH, Neufer PD. Linking mitochondrial bioenergetics to insulin resistance via redox biology. Trends Endocrinol Metab. 2012;23(3):142–53. Epub 2012/02/07. S1043-2760(11)00198-6 [pii] 10.1016/j.tem.2011.12.008 . [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All relevant data are within the paper and its Supporting Information files.