Abstract
Objective:
The aim of this paper was to systematically review and meta-analyse the prevalence of co-morbid psychiatric disorders (DSM-IV Axis I disorders) among treatment-seeking problem gamblers.
Methods:
A systematic search was conducted for peer-reviewed studies that provided prevalence estimates of Axis I psychiatric disorders in individuals seeking psychological or pharmacological treatment for problem gambling (including pathological gambling). Meta-analytic techniques were performed to estimate the weighted mean effect size and heterogeneity across studies.
Results:
Results from 36 studies identified high rates of co-morbid current (74.8%, 95% CI 36.5–93.9) and lifetime (75.5%, 95% CI 46.5–91.8) Axis I disorders. There were high rates of current mood disorders (23.1%, 95% CI 14.9–34.0), alcohol use disorders (21.2%, 95% CI 15.6–28.1), anxiety disorders (17.6%, 95% CI 10.8–27.3) and substance (non-alcohol) use disorders (7.0%, 95% CI 1.7–24.9). Specifically, the highest mean prevalence of current psychiatric disorders was for nicotine dependence (56.4%, 95% CI 35.7–75.2) and major depressive disorder (29.9%, 95% CI 20.5–41.3), with smaller estimates for alcohol abuse (18.2%, 95% CI 13.4–24.2), alcohol dependence (15.2%, 95% CI 10.2–22.0), social phobia (14.9%, 95% CI 2.0–59.8), generalised anxiety disorder (14.4%, 95% CI 3.9–40.8), panic disorder (13.7%, 95% CI 6.7–26.0), post-traumatic stress disorder (12.3%, 95% CI 3.4–35.7), cannabis use disorder (11.5%, 95% CI 4.8–25.0), attention-deficit hyperactivity disorder (9.3%, 95% CI 4.1–19.6), adjustment disorder (9.2%, 95% CI 4.8–17.2), bipolar disorder (8.8%, 95% CI 4.4–17.1) and obsessive-compulsive disorder (8.2%, 95% CI 3.4–18.6). There were no consistent patterns according to gambling problem severity, type of treatment facility and study jurisdiction. Although these estimates were robust to the inclusion of studies with non-representative sampling biases, they should be interpreted with caution as they were highly variable across studies.
Conclusions:
The findings highlight the need for gambling treatment services to undertake routine screening and assessment of psychiatric co-morbidity and provide treatment approaches that adequately manage these co-morbid disorders. Further research is required to explore the reasons for the variability observed in the prevalence estimates.
Keywords: Gambling, systematic review, meta-analysis, psychiatric disorders, co-morbidity
The Diagnostic and Statistical Manual of Mental Disorders (Fifth Edition) (DSM-5) (American Psychiatric Association, 2013) has reclassified pathological gambling as an addiction and related disorder along with alcohol and substance use disorders, and renamed it gambling disorder. In many jurisdictions, however, the term problem gambling is employed to describe all forms of gambling, including the more severe classification of pathological gambling, that lead to adverse consequences for the gambler, others, or the community (Neal et al., 2005). There is substantial evidence that problem gambling can result in many adverse consequences, including impaired mental and physical health, relationship and family dysfunction, financial problems, employment difficulties and legal issues (Productivity Commission, 1999). Problem gambling has also been consistently associated with a range of co-morbid psychiatric conditions formerly known as Axis I disorders in the DSM-IV, including alcohol and other substance use disorders, mood and anxiety disorders, and other impulse control disorders (Crockford and El-Guebaly, 1998; Lorains et al., 2011; Petry, 2005; Westphal and Johnson, 2007).
Internationally, the co-occurrence between problem gambling and co-morbid psychiatric conditions has been empirically examined in both epidemiological and clinical samples. By randomly sampling the general population, epidemiological studies provide results that are representative of problem gamblers in the community. They are, however, generally only able to determine the co-occurrence of problem gambling with highly prevalent co-morbid disorders because they yield very small numbers of problem gamblers (Lorains et al., 2011; Westphal and Johnson, 2007). A systematic review and meta-analysis of co-morbid disorders in population-representative samples of problem gamblers revealed high rates of psychiatric disorders, including nicotine dependence (60%), alcohol and substance use disorders (58%), mood disorders (38%) and anxiety disorders (37%) (Lorains et al., 2011).
Although these population-representative studies provide important information about the prevalence of co-morbidity in problem gamblers living in the community, caution is required in generalising results from these samples to treatment-seeking populations given emerging evidence that treatment-seeking problem gamblers display more severe gambling problems and a greater variety and intensity of co-morbid psychiatric disorders compared with their non-treatment seeking counterparts (Crockford and El-Guebaly, 1998; Slutske et al., 2001; Specker et al., 1996). Although they generally employ non-random samples, treatment-seeking studies generally comprise larger samples of problem gamblers, which allows for the investigation of lower prevalence co-morbid disorders and an investigation of how the level of gambling severity co-varies with co-morbid disorders (Westphal and Johnson, 2007).
To date, only narrative reviews of psychiatric co-morbidity in treatment-seeking problem gambling samples are available (Petry, 2005; Specker et al., 1996; Westphal and Johnson, 2007). Unfortunately, these reviews are not based on all of the available evidence, generally only explore the prevalence of high prevalence disorders, such as mood disorders, anxiety disorders and substance use disorders, and are unable to explore the degree to which prevalence estimates of co-morbidity fluctuate as a function of clinical and methodological considerations, such as gambling severity. They are also generally characterised by a lack of quality and risk of bias appraisal, a failure to identify the relative strength and reliability of the evidence for each of the psychiatric co-morbid disorders, and a lack of clarity about the generalizability of the findings to all treatment-seeking problem gamblers. It is therefore important that a systematic review of psychiatric co-morbidity in treatment-seeking problem gambling samples is conducted to redress the limitations of these narrative reviews.
The findings relating to psychiatric co-morbidity in treatment-seeking samples of problem gamblers are important in understanding individual treatment needs and outcomes (Lorains et al., 2011). There is accumulating evidence that the presence of co-morbid disorders in treatment-seeking problem gamblers is associated with an increased severity of gambling behaviour, gambling-related consequences, psychiatric symptoms, impulsivity and other psychosocial difficulties (Grall-Bronnec et al., 2011; Grant and Kim, 2003; Ibanez et al., 2001; Ledgerwood and Petry, 2006). The presence of co-morbid psychiatric conditions therefore has implications for individual case formulation, treatment planning and selection, the proposed objectives and expectations of the selected treatment, and the length of treatment. Psychiatric co-morbidity may also affect an individual’s compliance with treatment, the success of treatment, the likelihood of relapse and the number of treatment attempts (Ibanez et al., 2001; Kausch, 2003a; Kruedelbach et al., 2006; Westphal and Johnson, 2007). Although there are equivocal findings, there is some evidence that problem gamblers with co-morbid psychiatric symptoms have poorer outcomes and higher rates of drop-out for psychological interventions than those without co-morbid disorders (Echeburua et al., 2001; Hodgins and El-Guebaly, 2010; Milton et al., 2002).
The findings from both community-representative and treatment-seeking studies suggest that prevalence estimates of psychiatric co-morbidity in treatment-seeking problem gamblers vary widely. There is therefore a need to explore the methodological and clinical factors that may explain these variations in estimates. The heterogeneity in prevalence estimates may be due to differences in the characteristics of the sample or patient population, measurement factors, treatment factors or methodological considerations (Bagby et al., 2008; Blaszczynski and Steel, 1998; Echeburua and Fernandez-Montalvo, 2008; Lorains et al., 2011). There is some evidence that pathological gamblers display higher rates of co-morbidity than problem gamblers (Lorains et al., 2011) and that self-report inventories generally produce higher rates of co-morbidity than clinical interviews (Jimenez-Murcia et al., 2009; Kruedelbach et al., 2006). There is also some indication that gamblers attending residential services report higher rates of co-morbid conditions than those attending outpatient services (Battersby et al., 2006; Ladouceur et al., 2006; Petry, 2005) and that rates may be affected by region (Lorains et al., 2011; Specker et al., 1996).
Aims
The aims of the current paper are to: (1) evaluate the prevalence of current and lifetime co-morbid psychiatric disorders that are listed as Axis I diagnoses in the fourth edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-IV) (American Psychiatric Association, 2000) among problem gamblers seeking treatment using meta-analytic techniques; (2) explore the factors that explain the variability in the prevalence estimates of these co-morbid conditions using sub-group analyses; and (3) examine whether findings were robust to the quality of the study methodologies using sensitivity analyses. Prevalence estimates of co-morbid disorders that are listed as Axis II diagnoses (personality disorders) in the DSM-IV are reported in a separate article (Dowling et al., 2014a).
Method
The methodology employed in this review is compliant with the Preferred Reporting Items for Systematic reviews and Meta-Analyses (PRISMA) (Moher et al., 2009) and the guidelines for the Meta-analysis Of Observational Studies in Epidemiology (MOOSE) (Stroup et al., 2000).
Search strategy
A systematic search was conducted for studies that provided prevalence estimates of psychiatric disorders in individuals seeking psychological or pharmacological treatment for problem gambling. This search procedure comprised a number of strategies. Electronic databases, including Medline, PsycInfo, EMBASE and CINAHL, were searched. A number of specific journals that were not indexed in the electronic databases were also manually examined. These included Gambling Research (2003 onwards), International Gambling Studies (2001–2003) and Journal of Gambling Issues (2000–2006). Finally, the reference lists of all included studies and several narrative reviews were also searched manually. The search was limited to peer-reviewed published studies so as to ensure a rigorous methodological standard of included research. The search terms used incorporated a combination of keywords and wildcards relating to problem gambling and treatment. It did not include keywords relating to specific co-morbid psychiatric conditions. The search was restricted to articles published from January 1990 to August 2011, consistent with the development of the first standardised and validated assessment instrument for the identification of problem gambling in clinical settings (Lesieur and Blume, 1987). A detailed description of the search strategy is provided in Appendix A.
Inclusion criteria
Studies were considered eligible for the current review if they met the following inclusion criteria: (1) the study sample comprised adults recruited from treatment services where problem gambling was the index condition or clinical trials of gambling treatment for problem gamblers recruited from these services or the community. Gambling treatment included any treatment primarily delivered for the index condition of problem gambling, including psychological treatments (including self-help and Gamblers Anonymous) or pharmacological treatments. These treatments could be delivered in any setting, including specialist gambling services, addiction services, impulse control disorders services or mental health services. They could be delivered in any modality, including outpatient, residential, online or telephone; (2) the study provided an estimate of the prevalence of one or more psychiatric conditions that are listed as diagnoses in the DSM-IV identified using standardised and validated self-report measures with clinical cut-off scores or clinical interviews based on the DSM-IV or previous versions of the DSM; (3) the full-text report was available in English; and (4) the study was reported in a complete manuscript outlining original work published in a peer-reviewed journal from 1990 to 2011.
Studies were not eligible if they: (1) applied inclusion or exclusion criteria (for participant admission to the study) based on DSM-IV diagnostic conditions (e.g. a clinical trial that excluded participants on the basis of all current Axis I disorders). Studies that excluded participants on the basis of conditions that preclude completion of assessment measures or treatment (e.g. cognitive impairment, such as intellectual disability, delirium, dementia or amnesia; or acute/uncontrolled psychiatric disorders, such as psychotic disorder or suicidality) were included; (2) assessed clinical characteristics that are not listed as diagnostic conditions in the DSM-IV (e.g. impulsivity, suicidality, personality traits, substance use, sensation seeking); or (3) failed to provide sufficient data (e.g. providing only means or standard deviations, combining prevalence estimates for multiple co-morbid disorders, or failing to identify the measure employed). Where there were multiple articles based on the same sample: (a) only the study with the larger sample was included when a larger sample in one study subsumed a smaller sample in another study; (b) only the study with the most focus on co-morbid disorders was reported when two studies reported the same prevalence data from the same sample; and (c) both studies were included and are listed together in the table of included studies (Table 1) when two studies with the same sample reported prevalence data for different disorders. Data from each sample was included only once in any given analysis.
Table 1.
Characteristics of included studies.
| Study | Year | Country | Sample size (n) | Average age (years) | Gender (% male) | Treatment facility (outpatient, residential) | Treatment service (gambling, addictions, impulse control, mental health) | Treatment type (psychological, pharmacological, GA) | Gambling severity (pathological, problem) | Measure of problem gambling | Problematic gambling activity (mixed, EGMs) | Co-morbidity measures (interview, self-report) |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Battersby et al. | 2006 | Australia | 43 | 41.5 | 70 | Outpatient | Gambling | Psychological | Pathological | Diagnostic criteria | NR | Self-report |
| Breen and Zimmerman | 2002 | US | 44 | 46.9 | 61 | Outpatient | Gambling | Combined | Pathological | Diagnostic criteria | Mixed | Interview |
| Cavedini et al. | 2002 | Italy | 20 | 38.5 | 95 | Outpatient | Gambling | NR | Pathological | Diagnostic criteria | NR | Interview |
| Dannon et al. | 2006 | Israel | 78 | NRa | 54 | Outpatient | Gambling | NR | Pathological | Diagnostic criteria | NR | Interview |
| Echeburua et al. | 2011 | Spain | 103 | 43.1 | 51 | Outpatient | Gambling | Psychological | Pathological | Diagnostic criteria | Mixed | Interview |
| Goudriaan et al. | 2010 | Netherlands | 17 | 35.3 | 100 | NR | Addiction | NR | Problem | DIS | NR | Interview |
| Grall-Bronnec et al. | 2011 | France | 84 | 41.8 | 86 | NR | Addiction | NR | Problem | Diagnostic criteria | Mixed | Interview and self-report |
| Granero et al. | 2009 | Spain | 286 | 45.4 | 50 | NR | Gambling | NR | Pathological | DQ-PG | Mixed | Interview |
| Grant and Grosz | 2004 | US | 14 | 64.9 | 57 | Outpatient | Gambling | Combined | Pathological | Diagnostic criteria | NR | Interview |
| Grant and Kim | 2002 | US | 50 | 47.7 | 50 | Outpatient | Gambling | Combined | Pathological | Diagnostic criteria | NR | Interview |
| Grant and Kim | 2003 | US | 96 | 46.7 | 54 | Outpatient | impulse control | NR | Pathological | Diagnostic criteria | NR | Interview |
| Grant et al. | 2009 | US | 322 | 48.3 | 42 | Outpatient | Gambling | Psychological or pharmacological | Pathological | SCI-PG | Mixed | Interview |
| Grant et al. | 2008 | US | 465 | 47.6 | 46 | Outpatient | Gambling | Psychological or pharmacological | Pathological | SCI-PG | Mixed | Interview |
| Grant and Potenza | 2006 | US | 105 | 46.1 | 100 | Outpatient | Gambling | Psychological or pharmacological | Pathological | SCI-PG | NR | Interview |
| Ibanez et al. | 2001 | Spain | 69 | NR a | 68 | NR | Gambling | NR | Pathological | Diagnostic criteria | NR | Interview |
| Jimenez-Murcia et al. | 2009 | Spain | 498 | 41.5 | 88 | NR | Gambling | NR | Pathological | Diagnostic criteria | Mixed | Interview |
| Kausch / Kausch | 2003 | US | 113 | 48.9 | 91 | Residential | Gambling | NR | Pathological | Diagnostic criteria | NR | Interview |
| Kausch | 2004 | US | 135 | 51.9 | 93 | Residential | Gambling | NR | Pathological | Diagnostic criteria | Mixed | Interview |
| Kennedy et al. | 2005 | Japan | 35 | 33.2 | 74 | NR | Gambling | Psychological | Pathological | Diagnostic criteria | Mixed | Interview |
| Kerber et al. | 2008 | US | 40 | 62.0 | 63 | Outpatient | Gambling | Psych or GA | Problem | SOGS/NODS | NR | Interview |
| Korman et al. | 2008 | Canada | 42 | 47.6 | 86 | Outpatient | addiction/mental health | Psychological | Problem | PGSI | NR | Interview |
| Kroeber | 1992 | Germany | 43 | 32.2 | 98 | Either | Gambling | Psychological | Problem | Diagnostic criteria | Mixed | Interview |
| Kruedelbach et al. | 2006 | US | 162 | 46.7 | 98 | Residential | Gambling | NR | Pathological | Diagnostic criteria | Mixed | Interview |
| Ladouceur et al. | 2006 | Canada | 233 | 42.8 | 73 | Either | Gambling | Psychological | Pathological | Diagnostic criteria | NR | Interview |
| Ledgerwood and Petry | 2006 | US | 149 | 47.6 | 48 | NR | Gambling | NR | Problem | NODS | NR | Self-report |
| Lee et al./Teo et al. | 2007 | Singapore | 300 | 40.7 | 88 | Either | Gambling | Psychological | Pathological | Diagnostic criteria | Mixed | Interview |
| Maccallum and Blaszczynski | 2002 | Australia | 75 | 37.7 | 64 | Outpatient | Gambling | Psychological | Pathological | Diagnostic criteria | EGMs | Interview |
| Martins et al. | 2004 | Brazil | 156 | 42.7 | 50 | Outpatient | Gambling | Psychological | Pathological | Diagnostic criteria | NR | Interview |
| Patterson et al. | 2006 | US | 18 | 45.0 | NR a | Residential | Gambling | NR | Pathological | SOGS | NR | Interview |
| Sander and Peters | 2009 | Germany | 281 | 38.2 | 88 | Residential | Gambling | Psychological | Pathological | Diagnostic criteria | Mixed | Interview |
| Smith et al. | 2010 | Australia | 127 | 43.1 | 54 | Outpatient | Gambling | Psychological | Problem | VGS | Mixed | Self-report |
| Specker et al./Specker et al. | 1995/1996 | US | 40 | 41.1 | 63 | Outpatient | Gambling | NR | Pathological | Diagnostic criteria | Mixed | Interview |
| Stinchfield and Winters | 2001 | US | 592 | 39.0 | 59 | Outpatient | Gambling | Psychological | Pathological | Diagnostic criteria | Mixed | Interview |
| Tavares and Gentil | 2007 | Brazil | 40 | 40.5 | 50 | NR | Gambling | NR | Pathological | Diagnostic criteria | NR | Interview |
| Tavares et al. | 2003 | Brazil | 140 | 42.8 | 50 | Outpatient | Gambling | NR | Pathological | Diagnostic criteria | Mixed | Interview |
| Zimmerman et al. | 2010 | US | 210 | 39.9 | 56 | Outpatient | Gambling | NR | Problem | NR | NR | Interview |
DIS: Diagnostic Interview Schedule; DQ-PG: Diagnostic Questionnaire for Pathologic Gambling; GA: Gamblers Anonymous; NODS: NORC Diagnostic Screen for Gambling Disorders; NR: Not reported; PGSI: Problem Gambling Severity Index; SCI-PG: Structured Clinical Interview for Pathologic Gambling; SOGS: South Oaks Gambling Screen; VGS: Victorian Gambling Screen.
Search results
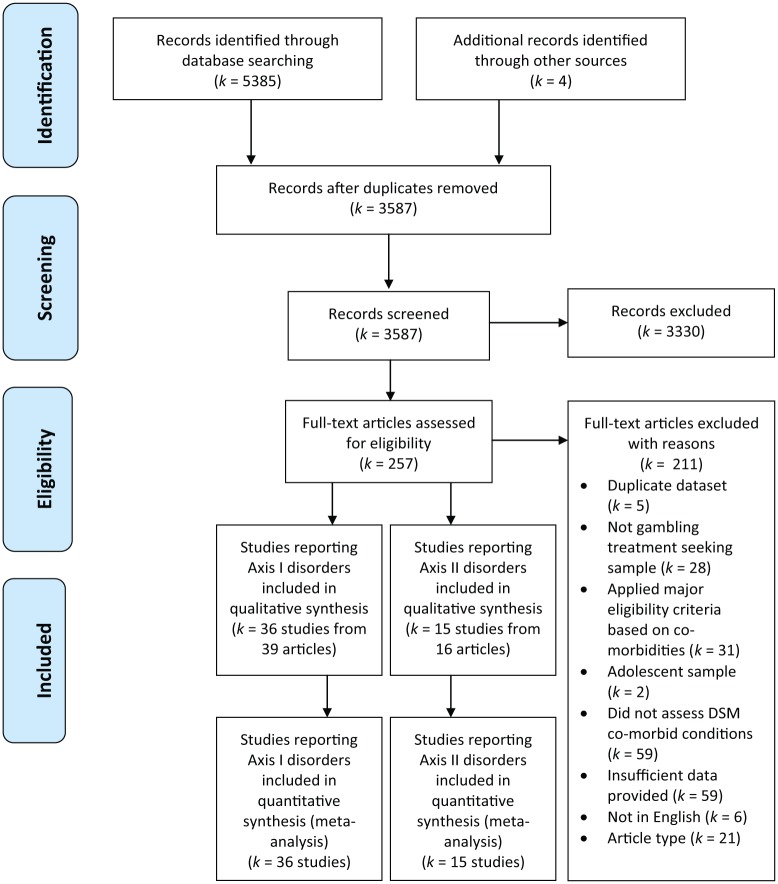
A PRISMA flow diagram of the search results is displayed in Figure 1. The search identified 3,587 articles after duplicate records were removed. The title and abstracts of these records were independently reviewed for inclusion by two separate authors. The full-texts of the 257 articles that were deemed potentially eligible were retrieved and 42 studies, published in 46 articles, met the inclusion criteria. Of these, 36 studies, published in 39 articles, provided prevalence estimates for DSM-IV Axis I disorders and are reported in this article. Fifteen studies, published in 16 articles, provided prevalence estimates for Axis II disorders (personality disorders) and are reported separately (Dowling et al., 2014a).
Figure 1.
Flow diagram of search results.
Data extraction
The first author (ND) extracted data from the included studies. In most cases, the prevalence estimate was available from the primary study. In other instances, it was necessary to combine findings reported for separate groups (e.g. men and women) to derive total sample prevalence rates. Prevalence estimates were reported for co-morbid psychiatric disorders that had three or more estimates available. To ensure the data extraction was accurate, one-third of the articles (33%; k=15) were randomly selected for double data extraction by two independent reviewers (AJ and KF). The inter-rater agreement across the multiple reviewers was 98.2%. Discrepancies were resolved through group discussion with third reviewer as arbiter.
Data analysis
Meta-analyses
Findings from primary studies were synthesised in meta-analyses using the Comprehensive Meta-Analysis (CMA) program (Version 2.0) (Borenstein et al., 2009). A series of separate meta-analyses were conducted to provide the current best prevalence estimate of each co-morbid disorder, all using a ‘random effects’ model. When differences across studies are attributed mainly to sampling error, a random-effects analysis provides an estimate of the weighted mean effect and a 95% confidence interval (CI) (that indicates the precision of this estimate). The I2 statistic indicates the amount of variation across studies due to true differences (heterogeneity) rather than chance (sampling error), and is expressed as a proportion (%) of the total observed variance. This statistic is in the range of 0–100%, whereby values of 25%, 50% and 75% are tentatively suggested to represent low, moderate and high levels of heterogeneity, respectively (Higgins et al., 2003).
Subgroup analyses
The observation of heterogeneity across studies precipitated consideration of study characteristics that could explain these between-study differences. Subgroup analyses were conducted to examine potential sources of heterogeneity for co-morbid disorders that had a sufficient number of primary studies available (10 or more). This involved the production of separate estimates of summary effect (with 95% CIs) for subgroups of studies. Significant differences were assumed when the 95% CIs did not overlap (Hunter and Schmidt, 2004). Based on previous literature, several study characteristics potentially explaining the observed variance were identified before the commencement of analysis. These were: (1) gambling problem severity (pathological gamblers compared to problem gamblers); (2) the measure of co-morbidity employed (clinician-administered interviews compared to self-report questionnaires); (3) the type of treatment facility (outpatient treatment services only compared to residential treatment services only); and (4) the jurisdiction in which the study was conducted (treatment services located in the US compared to treatment services located in Europe); other jurisdictions were not included in the subgroup analyses due to an insufficient number of studies.
Risk of bias assessment
The use of quality scoring in meta-analyses of observational studies is controversial and generally not recommended (Higgins et al., 2003; Stroup et al., 2000; Viswanathan et al., 2012) because scores constructed in an ad hoc fashion may lack demonstrated validity, and results may not be associated with quality (Jüni et al., 1999). A components approach was therefore adopted to assess risk of bias in this systematic review, whereby each study was rated on individual criteria that reflect the methodological risk of bias (Higgins et al., 2003; Viswanathan et al., 2012). These criteria explicitly evaluated risk of selection bias (use of an appropriate comparison group, volunteer/selection bias, and observation of treatment in naturalistic settings settings), performance bias (concurrent treatment restriction), detection bias (valid and reliable gambling measure) and reporting biases (industry sponsorship) (Higgins et al., 2003; Viswanathan et al., 2012). Studies that failed to consecutively or randomly recruit participants and/or were clinical trials were classified as having a non-representative sampling bias. With a view to contextualising this information, studies were also examined for the degree to which the measurement of co-morbidity was the stated purpose of the study. These criteria were reviewed by pairs of bias reviewers with a third reviewer serving as arbiter of conflicts. The inter-rater agreement across the multiple reviewers for the assessment of bias criteria was 95.1%.
Sensitivity analyses
As recommended by experts in the area of risk of bias assessment (Stroup et al., 2000; Viswanathan et al., 2012), sensitivity analyses were conducted to examine whether findings were robust to the quality of the methodological approaches of the included studies. The sensitivity analyses were sequentially limited to studies with representative samples: (1) observational studies of treatment in naturalistic settings (versus clinical trials which were excluded); and (2) random samples or recruitment of consecutive admissions (versus convenience samples comprising research participants who have volunteered to participate [self-selected samples] or studies failing to indicate the sampling strategies which were excluded). The data analytic approach employed in this study for each sensitivity analysis, whereby the meta-analysis was undertaken twice: first, including all studies and second, only including those that are definitely known to be eligible, is recommended by the Cochrane collaboration (Higgins and Green, 2011). These analyses were conducted for all types of co-morbidity, irrespective of number of studies.
Study and sample characteristics
The characteristics of the included studies reporting prevalence estimates for DSM-IV Axis I disorders are presented in Table 1. The sizes of the samples were in the range of 14–592 (M=145.1, SD=143.4, median=100). The average age of study participants was in the range of 33.2–64.9 years (M=43.0, SD=6.7, median=44) and the proportion of men in the samples was in the range of 42–100% (M=62.5%, SD=18.9, median=69). Most samples were restricted to pathological gamblers only (77.8%) measured via diagnostic criteria (69.4%) who were treated in gambling services (88.9%). Most samples were recruited from the US (44.4%) and Europe (25.0%) and most studies (94.4%) were published between 2001 and 2011. Co-morbidity measures were predominantly clinician-administered interviews (88.9%), with few studies using self-report measures (11.1%). Less commonly reported data were the problematic gambling activity (47.2% mixed, 2.8% electronic gaming machines only, 50.0% not reported), the type of treatment facility (52.8% outpatient facilities, 13.9% residential facilities, 11.1% recruitment from multiple types of facilities, 22.2% not reported), and the type of treatment delivered (33.3% psychological treatments, 8.3% combined treatments, 11.1% recruitment from multiple types of treatments, 47.2% not reported).
Approximately one-third of studies (k=11, 30.6%) indicated they excluded participants who were unable to complete assessment measures or treatment. However, with the exception of one study that excluded 23 participants on the basis of an ‘unstable mental state’ (Smith et al., 2010), these studies either failed to report the number of participants excluded on this basis (k=8) or reported that few (none or one) participants were excluded on this basis (k=2). A series of subgroup analyses revealed that there were no significant differences in prevalence estimates between studies that excluded participants on this basis and those that did not.
Results
Meta-analyses
Current DSM-IV Axis I disorders
Prevalence estimates for any current DSM-IV Axis I disorder were provided by five studies (Table 2). There was a weighted mean effect of 74.8% (95% CI 36.5–93.9) with very high between-study heterogeneity.
Table 2.
Prevalence of any current Axis I disorder in treatment-seeking problem gamblers.
| Study | Co-morbidity measure | Any current Axis I disorder |
|---|---|---|
| Grant and Potenza (2006b) | SCID (DSM-IV) | 21.0% |
| Kausch (2004) | Clinical diagnosis | 93.0% |
| Patterson et al. (2006) | MINI | 100% |
| Tavares and Gentil (2007) | SCAN | 81.0% |
| Specker et al. (1996) | SCID (DSM-III-R) | 54.0% |
| Summary effect (95% CI) | 74.8% (36.5–93.9) | |
| I2 (%) | 95.88 |
MINI: Mini International Neuropsychiatric Interview; SCAN: Schedules for Clinical Assessment in Neuropsychiatry; SCID (DSM-III-R): Structured Clinical Interview for DSM-III-R; SCID (DSM-IV): Structured Clinical Interview for DSM-IV.
Substance use disorders
Prevalence estimates for substance use disorders were provided by 26 studies (Table 3). There were weighted mean effects of 22.2% (95% CI 36.5–93.9) for any alcohol or substance use disorder, 21.2% (95% CI 5.6–28.1) for any alcohol use disorder and 7.0% (95% CI 1.7–24.9) for any substance (non-alcohol) use disorder. Specifically, the highest weighted mean effect was for nicotine dependence (56.4%, 95% CI 35.7–75.2) followed by alcohol abuse (18.2%, 95% CI 13.4–24.2), alcohol dependence (15.2%, 95% CI 10.2–22.0) and cannabis use disorder (11.5%, 95% CI 4.8–25.0). There was moderate to very high between-study heterogeneity for current substance use disorders.
Table 3.
Prevalence of co-morbid current substance use disorders in treatment-seeking problem gamblers.
| Study | Co-morbidity measure | Any alcohol or substance use disorder | Any alcohol use disorder | Alcohol abuse | Alcohol dependence | Any substance (non-alcohol) use disorder | Substance (non-alcohol) abuse | Substance (non-alcohol) dependence | Nicotine dependence | Cannabis use disorder |
|---|---|---|---|---|---|---|---|---|---|---|
| Dannon et al. (2006) | Clinical diagnosis | 11.5% | 5.1% | |||||||
| Echeburua et al. (2011) | Clinical diagnosis | 20.4% | ||||||||
| Granero et al. (2009) | Clinical diagnosis | 12.7% | 8.6% | |||||||
| Grant and Grosz (2004) | Clinical diagnosis | 0% | 0% | 0% | ||||||
| Grant and Kim (2002) | Clinical diagnosis | 14.0% | ||||||||
| Grant and Kim (2008) | SCID (DSM-IV) | 5.2% | 0% | 0% | 0% | |||||
| Grant et al. (2008) | SCID (DSM-IV) | 23.7% | 20.2% | 6.9% | ||||||
| Grant and Potenza (2006b) | SCID (DSM-IV) | 10.5% | ||||||||
| Ibanez et al. (2001) | SCID (DSM-III-R) | 23.2% | 2.9% | |||||||
| Jimenez-Murcia et al. (2009) | Clinical diagnosis (DSM-IV) | 10.7% | ||||||||
| Kausch (2003a) | Clinical diagnosis | 32.7% | ||||||||
| Kennedy et al. (2005) | Clinical diagnosis | 40.0% | ||||||||
| Kerber et al. (2008) | MINI | 32.5% | ||||||||
| Korman et al. (2008) | Clinical diagnosis | 45.2% | 38.1% | 19.0% | ||||||
| Kroeber (1992) | Clinical diagnosis (DSM-III-R) | 47.8% | 34.9% | 30.2% | 4.3% | |||||
| Ladouceur et al. (2006) | MCMI-III | 24.0% | ||||||||
| Lee et al. (2011)/Teo et al. (2007) | SCID (DSM-IV) | 10.3% | 7.3% | |||||||
| Maccallum and Blaszczynski (2002) | CIDI | 24.0% | 16.0% | 8.0% | 37.3% | 10.6% | ||||
| Martins et al. (2004) | SCAN | 10.9% | ||||||||
| Patterson et al. (2006) | MINI | 27.7% | 27.7% | 16.7% | 11.1% | 11.1% | 11.1% | 0% | ||
| Sander and Peters (2009) | Clinical diagnosis (DSM-IV/ICD-10) | 19.9% | 34.9% | 54.8% | ||||||
| Smith et al. (2010) | AUDIT | 30.7% | 16.5% | 14.2% | ||||||
| Specker et al. (1996) | SCID (DSM-III-R) | 7.5% | 7.5% | 0% | 0% | 0% | 0% | |||
| Stinchfield and Winters (2001) | Clinical diagnosis (DSM-III-R) | 16.0% | ||||||||
| Tavares and Gentil (2007) | SCAN | 20.0% | 5.0% | 62.5% | ||||||
| Tavares et al. (2003) | SCAN | 16.4% | 12.1% | 68.6% | ||||||
| Summary effect (95% CI) | 22.2% (16.1–29.8) | 21.2% (15.6–28.1) | 18.2% (13.4–24.2) | 15.2% (10.2–22.0) | 7.0% (1.7–24.9) | 6.6% (3.3–12.7) | 4.2% (1.5–11.4) | 56.4% (35.7–75.2) | 11.5% (4.8–25.0) | |
| I2 (%) | 89.68 | 86.62 | 79.02 | 61.52 | 97.53 | 72.13 | 51.21 | 89.49 | 58.02 |
AUDIT: Alcohol Use Disorders Identification Test; CIDI: Composite International Diagnostic Interview; MCMI-III: Millon Clinical Multiaxial Inventory-III; MINI: Mini International Neuropsychiatric Interview; SCAN: Schedules for Clinical Assessment in Neuropsychiatry; SCID (DSM-III-R): Structured Clinical Interview for DSM-III-R; SCID (DSM-IV): Structured Clinical Interview for DSM-IV.
Mood disorders
Prevalence estimates for mood disorders were provided by 22 studies (Table 4). There was a weighted mean effect of 23.1% (95% CI 14.9–34.0) for any mood disorder. Specifically, there were weighted mean effects of 29.9% (95% CI 20.5–41.3) for major depressive disorder, 8.8% (95% CI 4.4–17.1) for bipolar disorder and 6.7% (95% CI 4.8–9.2) for dysthymic disorder. There was high between-study heterogeneity for all current mood disorders, except dysthymic disorder, which had very low between-study heterogeneity.
Table 4.
Prevalence of co-morbid current mood disorders in treatment-seeking problem gamblers.
| Study | Co-morbidity measure | Any mood disorder | Major depressive disorder | Dysthymic disorder | Bipolar disorder |
|---|---|---|---|---|---|
| Battersby et al. (2006) | BDI | 48.8% | |||
| Dannon et al. (2006) | Clinical diagnosis | 11.5% | 3.8% | ||
| Goudriaan et al. (2010) | CIDI | 17.0% | |||
| Grant and Grosz (2004) | Clinical diagnosis | 42.9% | |||
| Grant and Kim (2002) | Clinical diagnosis | 28.0% | 6.0% | ||
| Grant and Kim (2008) | SCID (DSM-IV) | 10.4% | 4.2% | ||
| Grant et al. (2008) | SCID (DSM-IV) | 29.5% | 13.1% | 6.7% | |
| Grant and Potenza (2006b) | SCID (DSM-IV) | 4.8% | |||
| Ibanez et al. (2001) | SCID (DSM-III-R) | 8.7% | |||
| Jimenez-Murcia et al. (2009) | Clinical diagnosis (DSM-IV) | 12.1% | |||
| Kausch (2003a)/ Kausch (2003b) | Clinical diagnosis | 42.5% | 7.1% | ||
| Kennedy et al. (2005) | Clinical diagnosis | 25.7% | |||
| Kerber et al. (2008) | MINI | 82.5% | 82.5% | 20.0% | |
| Kroeber (1992) | Clinical diagnosis (DSM-III-R) | 11.6% | 4.7% | ||
| Lee et al. (2011) | SCID (DSM-IV) | 11.7% | |||
| Patterson et al. (2006) | MINI | 83.0% | 16.7% | 5.6% | 66.6% |
| Sander and Peters (2009) | Clinical diagnosis (DSM-IV/ICD-10) | 18.5% | 17.5% | ||
| Specker et al. (1996) | SCID (DSM-III-R) | 37.5% | 35.0% | 7.5% | 0% |
| Stinchfield and Winters (2001) | Clinical diagnosis (DSM-III-R) | 12.0% | |||
| Tavares and Gentil (2007) | SCAN | 45.0% | 7.5% | ||
| Tavares et al. (2003) | SCAN | 71.4% | 7.9% | ||
| Zimmerman et al. (2010) | SCID (DSM-IV) | 28.1% | |||
| Summary effect (95% CI) | 23.1% (14.9–34.0) | 29.9% (20.5–41.3) | 6.7% (4.8–9.2) | 8.8% (4.4–17.1) | |
| I2 (%) | 94.87 | 93.73 | 0.00 | 82.21 |
BDI: Beck Depression Inventory; CIDI: Composite International Diagnostic Interview; MINI: Mini International Neuropsychiatric Interview; SCAN: Schedules for Clinical Assessment in Neuropsychiatry; SCID (DSM-III-R): Structured Clinical Interview for DSM-III-R; SCID (DSM-IV): Structured Clinical Interview for DSM-IV.
Anxiety disorders
Prevalence estimates for anxiety disorders were provided by 15 studies (Table 5). There was a weighted mean effect of 17.6% (95% CI 0.8–27.3) for any anxiety disorder. The anxiety disorders with the highest weighted mean effects were social phobia (14.9%, 95% CI 2.0–59.8) and generalised anxiety disorder (GAD) (14.4%, 95% CI 3.9–40.8), followed by panic disorder (13.7%, 95% CI 6.7–26.0), post-traumatic stress disorder (PTSD) (12.3%, 95% CI 3.4–35.7) and obsessive-compulsive disorder (OCD) (8.2%, 95% CI 3.4–18.6). There was high to very high between-study heterogeneity for current anxiety disorders.
Table 5.
Prevalence of co-morbid current anxiety disorders in treatment-seeking problem gamblers.
| Study | Co-morbidity measure | Any anxiety disorder | OCD | Panic disorder | GAD | PTSD | Social phobia |
|---|---|---|---|---|---|---|---|
| Dannon et al. (2006) | Clinical diagnosis | 9.0% | 3.8% | 3.8% | |||
| Goudriaan et al.(2010) | CIDI | 17.0% | |||||
| Grant and Grosz (2004) | Clinical diagnosis | 7.1% | 7.1% | ||||
| Grant and Kim (2008) | SCID (DSM-IV) | 2.1% | |||||
| Grant et al. (2008) | SCID (DSM-IV) | 11.4% | |||||
| Grant and Potenza (2006b) | SCID (DSM-IV) | 8.6% | |||||
| Ibanez et al. (2001) | SCID (DSM-III-R) | 4.3% | |||||
| Jimenez-Murcia et al. (2009) | Clinical diagnosis (DSM-IV) | 10.1% | |||||
| Kausch (2003a)/ Kausch (2003b) | Clinical diagnosis | 7.0% | 5.3% | ||||
| Kerber et al. (2008) | MINI | 47.5% | 5.0% | 27.5% | 22.5% | ||
| Ledgerwood and Petry (2006) | PTSD Checklist – Civilian | 34.2% | |||||
| Patterson et al. (2006) | MINI | 94.4% | 50.0% | 38.9% | 50.0% | 16.7% | 50.0% |
| Specker et al. (1996) | SCID (DSM-III-R) | 22.5% | 2.5% | 10.0% | 5.0% | 5.0% | 5.0% |
| Tavares and Gentil (2007) | SCAN | 27.5% | 2.5% | ||||
| Tavares et al. (2003) | SCAN | 14.3% | 10.0% | ||||
| Summary effect (95% CI) | 17.6% (10.8–27.3) | 8.2% (3.4–18.6) | 13.7% (6.7–26.0) | 14.4% (3.9–40.8) | 12.3% (3.4–35.7) | 14.9% (2.0–59.8) | |
| I2 (%) | 88.44 | 81.86 | 77.42 | 86.98 | 90.58 | 85.61 |
CIDI: Composite International Diagnostic Interview; MINI: Mini International Neuropsychiatric Interview; PTSD Checklist – Civilian: Post-traumatic Stress Disorder Checklist – Civilian version; SCAN: Schedules for Clinical Assessment in Neuropsychiatry; SCID (DSM-III-R): Structured Clinical Interview for DSM-III-R; SCID (DSM-IV): Structured Clinical Interview for DSM-IV.
Other disorders
Prevalence estimates for other DSM-IV Axis I disorders were provided by 13 studies (Table 6). None of the primary articles employed to derive the prevalence estimate for psychotic disorder reported excluding participants on the basis of conditions that precluded completion of assessment measures or treatment. The highest weighted mean effects were for attention-deficit hyperactivity disorder (ADHD) (9.3%, 95% CI 4.1–19.6) and adjustment disorder (9.2%, 95% CI 4.8–17.2). There was low to very low between-study heterogeneity for all current other disorders, except adjustment disorder and ADHD, which had moderate to high between-study heterogeneity.
Table 6.
Prevalence of co-morbid current other Axis I disorders in treatment-seeking problem gamblers.
| Study | Co-morbidity measure | Intermittent explosive disorder | Kleptomania | Psychotic disorder | Somatoform disorder | Adjustment disorder | ADHD |
|---|---|---|---|---|---|---|---|
| Dannon et al. (2006) | Clinical diagnosis | 1.3% | |||||
| Grall-Bronnec et al. (2011) | ASRS | 10.5% | |||||
| Grant and Kim (2008) | MIDI | 2.1% | 2.1% | ||||
| Grant and Potenza (2006b) | SCID (DSM-IV) | 0% | 1.0% | 0% | |||
| Grant and Potenza (2006b) | MIDI | 4.8% | 1.9% | ||||
| Ibanez et al. (2001) | SCID (DSM-III-R) | 17.4% | |||||
| Jimenez-Murcia et al.(2009) | Clinical diagnosis (DSM-IV) | 4.2% | |||||
| Kausch (2003a)/ Kausch (2003b) | Clinical diagnosis | 5.3% | 15.9% | ||||
| Kerber et al. (2008) | MINI | 10.0% | 5.0% | 7.5% | |||
| Ladouceur et al. (2006) | MCMI-III | 6.0% | |||||
| Specker et al. (1995) | Clinical diagnosis | 20.0% | |||||
| Specker et al. (1996) | SCID (DSM-III-R) | 2.5% | 0% | ||||
| Specker et al. (1996) | MIDI | 7.5% | 5.0% | ||||
| Stinchfield and Winters (2001) | Clinical diagnosis (DSM-III-R) | 7.0% | |||||
| Tavares and Gentil (2007) | SCAN | 2.5% | |||||
| Tavares et al. (2003) | SCAN | 3.6% | |||||
| Summary effect (95% CI) | 4.6% (2.5–8.4) | 2.7% (1.2–5.9) | 4.7% (3.4–6.5) | 3.6% (1.6–8.0) | 9.2% (4.8–17.2) | 9.3% (4.1–19.6) | |
| I2 (%) | 3.22 | 0.0 | 8.81 | 39.42 | 80.27 | 65.30 |
ASRS: Adult ADHD Self-Report Scale; MCMI-III: Millon Clinical Multiaxial Inventory-III; MIDI: Minnesota Impulsive Disorders Interview; MINI: Mini International Neuropsychiatric Interview; SCAN: Schedules for Clinical Assessment in Neuropsychiatry; SCID (DSM-III-R): Structured Clinical Interview for DSM-III-R; SCID (DSM-IV): Structured Clinical Interview for DSM-IV.
Lifetime DSM-IV Axis I disorders
Prevalence estimates for lifetime DSM-IV Axis I disorders were provided by 13 studies (Table 7). There was a weighted mean effect of 75.5% (95% CI 45.6–91.8) for lifetime Axis I disorders. There were weighted mean effects of 47.0% (95% CI 31.0–63.7) for any alcohol or substance use disorder, 41.1% (95% CI 29.1–54.2) for any alcohol use disorder, 38.6% (95% CI 25.7–53.4) for any mood disorder, 23.9% (95% CI 16.3–33.8) for any anxiety disorder and 21.4% (95% CI 12.2–34.7) for any substance (non-alcohol) use disorder. There was high to very high between-study heterogeneity for lifetime Axis I disorders.
Table 7.
Prevalence of co-morbid lifetime Axis I disorders in treatment-seeking problem gamblers.
| Study | Co-morbidity measure | Any Axis I disorder | Any alcohol or substance use disorder | Any alcohol use disorder | Alcohol dependence | Any substance (non-alcohol) use disorder | Any mood disorder | Major depressive disorder | Any anxiety disorder | OCD |
|---|---|---|---|---|---|---|---|---|---|---|
| Battersby et al. (2006) | CAGE | 25.6% | ||||||||
| Breen and Zimmerman (2002) | SCID (DSM-IV) | 34.0% | 70.0% | 25.0% | ||||||
| Cavedini et al. (2002) | DIS-R | 15.0% | ||||||||
| Grall-Bronnec et al. (2011) | MINI | 41.5% | 29.3% | 42.7% | 32.9% | |||||
| Grant and Grosz (2004) | Clinical diagnosis | 35.7% | ||||||||
| Grant and Kim (2008) | SCID (DSM-IV) | 46.9% | 14.6% | 2.1% | 24.0% | 2.1% | ||||
| Grant et al. (2009) | SCID (DSM-IV) | 25.2% | 36.3% | 17.0% | ||||||
| Grant and Potenza (2006b) | SCID (DSM-IV) | 78.1% | 37.1% | 29.5% | 30.5% | |||||
| Ibanez et al. (2001) | SCID (DSM-III-R) | 34.8% | 15.8% | 7.2% | ||||||
| Kausch (2003a)/ Kausch (2003b) | SCID (DSM-IV) | 66.4% | 59.3% | 42.5% | 38.6% | |||||
| Kausch (2004) | SCID (DSM-IV) | 61.9% | 55.9% | 33.6% | ||||||
| Kruedelbach et al.(2006) | SCID (DSM-III-R) | 47.2% | ||||||||
| Specker et al. (1996) | SCID (DSM-III-R) | 92.0% | 60.0% | 50.0% | 10.0% | 77.5% | 70.0% | 37.5% | 2.5% | |
| Summary effect (95% CI) | 75.5% (45.6–91.8) | 47.0% (31.0–63.7) | 41.1% (29.1–54.2) | 40.1% (30.4–50.7) | 21.4% (12.2–34.7) | 38.6% (25.7–53.4) | 54.3% (21.9–83.4) | 23.9% (16.3–33.8) | 4.8% (1.1–18.0) | |
| I2 (%) | 93.51 | 94.13 | 87.63 | 67.08 | 86.18 | 89.30 | 94.37 | 81.80 | 65.37 |
CAGE: The CAGE Questionnaire; DIS-R: Diagnostic Interview Schedule–Revised; MINI: Mini International Neuropsychiatric Interview; SCID (DSM-III-R): Structured Clinical Interview for DSM-III; SCID (DSM-IV): Structured Clinical Interview for DSM-IV.
Subgroup analyses
The potentially relevant sources of heterogeneity identified before the commencement of analysis included: (1) gambling problem severity; (2) the measure of co-morbidity employed; (3) the type of treatment facility; and (4) the jurisdiction in which the study was conducted. Subgroup analyses were performed for the six co-morbid disorders that had sufficient (10 or more) primary studies available (any current alcohol or substance use disorder, any current alcohol use disorder, any current mood disorder, current major depressive disorder, current bipolar disorder and any current anxiety disorder).
Gambling problem severity
Only alcohol use disorder and major depressive disorder had sufficient primary studies in both gambling problem severity subgroups (pathological gamblers and problem gamblers) to conduct subgroup analyses. For alcohol use disorder, pathological gambling samples (17.3%, 95% CI 11.7–25.0) yielded statistically significantly lower point estimates relative to problem gambling samples (33.1%, 95% CI 27.1–39.7). There was no evidence of systematic variation in point estimates for major depressive disorder.
Measure of co-morbidity employed
None of the disorders had sufficient primary studies in both co-morbidity measure subgroups (clinician-administered interviews and self-report questionnaires) to conduct subgroup analyses.
Type of treatment facility
Only major depressive disorder had sufficient primary studies in both treatment facility subgroups (outpatient treatment and residential treatment) to conduct subgroup analyses. There was no evidence of systematic variation in point estimates for this disorder.
Jurisdiction
All co-morbid disorders except bipolar disorder had sufficient primary studies in both jurisdiction subgroups (US and Europe) to conduct subgroup analyses. Prevalence estimates for alcohol use disorder from studies in the US (13.6%, 95% CI 7.6–23.0) were significantly lower than those from studies conducted in Europe (31.7%, 95% CI 24.8–39.5). However, there was no evidence of systematic variation in point estimates for mood disorder, anxiety disorder, major depressive disorder, or alcohol or substance use disorder.
Risk of bias assessment
A components approach was adopted to assess risk of bias in this systematic review (Table 8). Measurement of co-morbidity was the stated purpose of the study for almost two-thirds of the included studies (61.1%). Almost all (97.2%) employed a valid and reliable gambling measure, and most studies (86.1%) reported that they did not have any sponsorship from the gambling industry. Although most (86.1%) were observational studies of treatment in naturalistic settings (i.e. not clinical trials), the representativeness of the included samples was limited by only 63.9% reporting consecutive or random recruitment of participants. Moreover, only 19.4% of studies reported employing an appropriate comparison group and few studies (5.8%) ruled out any impact from a concurrent intervention or an unintended exposure that might bias results. Just under half of the included studies (44.4%) were classified as having a non-representative sampling bias (self-selected samples and/or clinical trials).
Table 8.
Risk of bias assessment.
NR: Not reported.
Sensitivity analyses
Sensitivity analyses were conducted to determine whether findings were robust to the inclusion of studies with non-representative sampling biases, and involved sequentially limiting studies to: (1) observational studies of treatment in naturalistic settings (i.e. clinical trials were excluded); and (2) random samples or recruitment of consecutive admissions (i.e. self-selected samples or studies failing to indicate sampling strategies were excluded). Given the large number of analyses conducted, these results are available from the corresponding author.
Studies of naturalistic treatment
Across most types of co-morbidity, results based on studies of naturalistic treatment varied minimally relative to all studies including clinical trials. Where salient differences were observed, they generally indicated higher estimates in analyses of naturalistic treatment. The largest differences were observed for: (1) ‘any lifetime Axis I disorder’, whereby studies of naturalistic treatment suggested higher estimates (k=1; 92.5%, 95% CI 79.2–91.8) relative to results from all studies (k=3; 75.5%, 95% CI 45.6–0.92); and (2) ‘lifetime major depressive disorder’, whereby studies of naturalistic treatment suggested higher estimates (k=2; 70.2%, 95% CI 59.7–79.0) relative to results from all studies (k=3; 54.3%, 95% CI 21.9–83.4). In each instance, the sensitivity analyses were based on few studies and produced wide 95% CIs. Only the analyses of ‘any current impulse control disorder’ suggested lower estimates in studies of naturalistic treatment (k=3; 6.7%, 95% CI 0.5–48.4) versus all studies (k=5; 13.7%, 95% CI 4.2–36.1); however, the magnitude of the difference was small. Accordingly, it was concluded that the results of the review were robust to the inclusion of clinical trials.
Studies of random samples and consecutive admissions
Across most types of co-morbidity, results based on random samples or consecutive admissions varied minimally relative to analyses based on all studies (including self-selected samples). Where more salient differences were observed, there was no clear pattern of higher or lower estimates. The largest increase was observed for ‘lifetime major depressive disorder’, whereby studies of random / consecutive samples suggested higher estimates (k=2; 70.2%, 95% CI 59.7–79.0) relative to all studies (k=3; 54.3%, 95% CI 21.9–83.4). The largest decrease was observed for ‘current social phobia’ (equal with GAD), whereby studies of random/consecutive samples suggested lower estimates (k=2; 5.6%, 95% CI 1.8–16.1) relative to results from all studies (k=3; 14.9%, 95% CI 2.0–59.8). In each instance, the sensitivity analyses were based on few studies and produced wide 95% CIs, while the absolute magnitudes of differences were small. Accordingly, it was concluded that results of the current review were also robust to inclusion of self-selected samples.
Discussion
Prevalence rates of co-morbid psychiatric disorders
This is the first systematic review and meta-analysis to explore the prevalence rates of co-morbid psychiatric disorders in treatment-seeking problem gamblers. The findings from 36 studies indicated that approximately three-quarters of treatment-seeking problem gamblers display current and lifetime co-morbid Axis I disorders. The most common current disorders were nicotine dependence, major depressive disorder, alcohol abuse and dependence, social phobia, GAD, panic disorder, PTSD, cannabis use disorder, ADHD, adjustment disorder, bipolar disorder and OCD, while the most common lifetime disorders were major depressive disorder and alcohol and substance use disorders. Unlike previous narrative reviews, this review used robust, replicable and reliable procedures to systematically identify and synthesise all available evidence, including studies in which the investigation of co-morbidity was not the primary aim, and sheds light on the relative strength and reliability of the evidence for each co-morbid psychiatric disorder. Although the general conclusion that treatment-seeking problem gambling is associated with high rates of mood, anxiety and substance use disorders is generally consistent with those of available narrative reviews (Petry, 2005; Specker et al., 1996; Westphal and Johnson, 2007), this review adds information about the high co-occurrence of problem gambling and specific disorders with less available evidence, such as social phobia, GAD, PTSD, cannabis use disorder, ADHD, adjustment disorder and dysthymic disorder.
Interestingly, the prevalence estimates derived in this review were not consistently higher than those derived from a meta-analysis of community samples (Lorains et al., 2011). This contrasts with expectations from treatment-seeking sample selection biases (Berkson, 1946; Crockford and El-Guebaly, 1998) that treatment-seeking samples include those with the most serious gambling problems and the highest rates of co-morbid psychopathology (Crockford and El-Guebaly, 1998; Slutske et al., 2001; Specker et al., 1996). It may suggest a paradoxical effect, whereby problem gamblers with co-morbid disorders seek treatment at mental health or addiction services to manage their co-morbid psychopathology rather than at specialist gambling agencies for their gambling problems (Lorains et al., 2011; Winters and Kushner, 2003). This explanation is supported by findings that the rate of problem gambling in mental health, alcohol and drug, family violence and financial counselling services is two to 21 times higher (Dowling et al., 2014b, 2014c) than in the general population (Jackson et al., 2010). It implies that the co-morbid psychiatric condition may be of more concern than the gambling problem or that gamblers are more aware of their co-morbid symptomatology than their gambling symptomatology. Indeed, a recent population study has found that approximately half of problem gamblers do not self-perceive even a moderate gambling problem (Suurvali et al., 2012). An alternative explanation is that the social acceptability, public awareness and accessibility of mental health or addiction services may be higher than gambling services. There may therefore be a need for these services to routinely screen for problem gambling and have appropriate resources to assess and manage the gambling behaviour of problem gambling clients.
Heterogeneity in prevalence estimates of co-morbid psychiatric disorders
A strength of this systematic review over previous narrative reviews is that it was able to explore the degree to which prevalence estimates of co-morbidity fluctuate as a function of clinical and methodological considerations. A notable feature of the data was significant variability in the reported rates of many co-morbid psychiatric disorders. Unfortunately, although several potentially relevant methodological and clinical factors that may explain the variations in these estimates were explored, no consistent patterns were identified. This is consistent with a meta-analysis of community-representative samples of problem gamblers (Lorains et al., 2011).
However, there were a few specific findings from the subgroup analyses that are worth noting. The current review revealed significantly lower estimates for alcohol use disorders in pathological gamblers than problem gamblers and in US studies than European studies. These findings could suggest that pathological gamblers with co-morbid alcohol use disorders are more likely to seek assistance at alcohol treatment services than at gambling agencies (Lorains et al., 2011; Westphal and Johnson, 2007) and that problem gamblers with alcohol use disorders in the US may be more likely to seek treatment for alcohol use problems than gambling problems compared to their European counterparts. Alternatively, of course, the findings relating to jurisdictional variances could reflect differences in the provision of gambling treatment services across the US and Europe.
As more studies become available and reporting improves, future updates of this review may consider the effect of these and other sample characteristics (such as gender composition of the sample, problematic gambling activity), measurement factors (such as the method and quality of problem gambling and comorbidity measurement), treatment factors (such as type of treatment delivered) or other methodological considerations (such as sample size and year of publication). Subgroup analysis of other methodological issues considered in the risk of bias assessment could also be analysed as sources of variation that could be included in future updates of this review, such as the purposive nature of the co-morbidity measurement, the influence of sponsorship from the gambling industry, the use of a comparison group, and concurrent treatment restriction.
Limitations of the available evidence base
Several limitations of the evidence on which the review is based are noted. First, although most studies were observational studies of treatment in naturalistic settings, only two-thirds of studies reported consecutive or random recruitment of participants. Just under half of the included studies were classified as having a non-representative sampling bias as evidenced by the inclusion of self-selected samples and/or clinical trials. Although a higher degree of sample representativeness is necessary in future research, the sensitivity analyses conducted in the current systematic review suggested that the identified prevalence estimates were robust to the inclusion of clinical trials and self-selected samples.
Second, although all cross-sectional, case-control and cohort studies that examined the prevalence of psychiatric conditions in treatment-seeking problem gamblers were included, less than 20% of studies included healthy control groups. The failure to employ these groups do not allow for conclusions regarding the presence of a psychiatric co-morbidity between the problem gambling group and their non-gambling counterparts. Moreover, most studies were unable to rule out any impact from a concurrent intervention that might bias their results. Future research incorporating healthy control groups and exclusion criteria relating to concurrent interventions will enhance the rigour of future research in this area.
Third, most samples were treated in outpatient or residential facilities, with studies delivered in online or telephone settings predominantly excluded on the basis of employing non-standardised measures of psychiatric co-morbidity or clinical characteristics that are not listed as diagnostic conditions in the DSM-IV. Similarly, while studies exploring self-help treatments, Gamblers Anonymous and pharmacological treatments were not excluded from this review, very few studies administering these treatments were included. Given the increased accessibility and confidentiality provided by telephone counselling services, web-based counselling services and self-help interventions (Dowling et al., 2014b, 2014c; Rodda et al., 2013a, 2013b, 2015), it will be important for future studies to evaluate the psychiatric co-morbidity of these treatment-seeking gamblers using standardised instruments.
Fourth, the cross-sectional nature of the studies reviewed precludes an explication of the temporal or causal relationship between problem gambling and these co-morbid conditions. Future research exploring the onset and pattern of psychiatric disorders and problem gambling using prospective study designs is therefore needed (Westphal and Johnson, 2007). The prevalence estimates identified in this review must also be interpreted in the context of an emerging literature indicating that a substantial proportion of treatment-seeking problem gamblers have multiple co-morbid conditions (Ibanez et al., 2001; Kerber et al., 2008; Kruedelbach et al., 2006; Westphal and Johnson, 2007). Because failure to control for other disorders may produce inflated rates of psychiatric co-morbidity (Bagby et al., 2008), research controlling for multiple co-occurring disorders or using multi-morbidity coefficients (Batstra et al., 2002) is required.
Finally, there are several other limitations of the existing evidence base that are important in determining the direction of future research. The sample sizes of the included studies are generally small and many do not report important characteristics of the study, such as the problematic gambling activity of the participants, the type of treatment facility or the type of treatment delivered. Moreover, although the larger number of problem gamblers in treatment-seeking samples allows for the investigation of lower prevalence co-morbid disorders (Westphal and Johnson, 2007), there remain many classes of Axis I psychiatric conditions in the DSM-IV that were not explored by sufficient studies to be included in the review, such as cognitive disorders, dissociative disorders, eating disorders, factitious disorders, sexual and gender identity disorders, and sleep disorders. There were also insufficient studies investigating the prevalence of specific disorders within classes that were well-represented in the available literature, such as anxiety disorders (e.g. specific phobia, acute stress disorder), substance use disorders (e.g. opioid-related disorders, cocaine-related disorders) and impulse control disorders (e.g. pyromania, trichotillomania). Future studies using large samples and rigorous reporting protocols are required to investigate the prevalence of these less common psychiatric disorders.
Clinical implications for practice and research
Although there are some issues around the precision of the findings in the current review, it is clear that treatment-seeking problem gamblers report generally high rates of psychiatric co-morbidity. The findings of this review therefore highlight the need to undertake systematic and routine screening and comprehensive assessment of co-occurring psychiatric disorders in individuals seeking treatment for gambling problems (Dowling et al., 2014b, 2014c; Petry, 2005; Westphal and Johnson, 2007). This can be achieved through comprehensive screening for multiple psychiatric co-morbid disorders or targeted screening for prevalent psychiatric disorders such as alcohol and substance use disorders, mood disorders and anxiety disorders (Westphal and Johnson, 2007). Clients who screen positively for co-morbid problems will require more extensive diagnostic assessments, an exploration of the ways in which the comorbidity is associated with the gambling problem, and identification of therapeutic needs.
The findings of this review also underscore the need to develop individually tailored case formulations, treatment plans, treatment objectives and individualised intervention approaches for problem gamblers with co-morbid psychiatric conditions. Such recognition of psychiatric co-morbidity could serve to maximize treatment response, enhance client satisfaction, reduce attrition and lower treatment costs (Ladouceur et al., 2006). There is also a need for an appropriate clinical response by specialist gambling agencies, such as appropriate referral pathways or a workforce with adequate skills to appropriately manage these disorders (Petry, 2005; Specker et al., 1996 Westphal and Johnson, 2007). The presence of high levels of psychiatric co-morbidity suggests that a multimodal, stepped care approach to gambling treatment may be appropriate, whereby treatment intensity increases with increasing client needs. Such a stepped care approach involves a treatment network that encompasses a continuum of integrated services delivering a broad spectrum of treatment from minimally restrictive to increasingly intensive approaches (Marotta, 2003).
Despite their obvious importance, the implications of co-morbid psychiatric disorders for treatment have received little research attention. Although there is some evidence that psychiatric co-morbidity is associated with poorer outcomes and higher attrition rates (Echeburua et al., 2001; Hodgins and El-Guebaly, 2010; Milton et al., 2002), few studies have applied targeted pharmacological (Black, 2004; Grant and Potenza, 2006a; Hollander et al., 2005) or psychological (Korman et al., 2008) treatments to subgroups of problem gamblers with co-occurring psychiatric co-morbidity. Further research is required to evaluate the efficacy of interventions specifically designed for these subgroups of problem gamblers.
Supplementary Material
Acknowledgments
The authors would like to thank Azusa Umemoto for assisting in the scanning of the titles and abstracts of the retrieved articles for inclusion and Felicity Lorains for serving as the third reviewer in the arbitration of conflicts in the risk of bias assessment.
Footnotes
Funding: This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Declaration of interest: The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
References
- American Psychiatric Association (2000) Diagnostic and statistical manual of mental disorders. 4th edn. Washington, DC: American Psychiatric Association. [Google Scholar]
- American Psychiatric Association (2013) Diagnostic and statistical manual of mental disorders. 5th edn. Washington, DC: American Psychiatric Association. [Google Scholar]
- Bagby RM, Vachon DD, Bulmash E, et al. (2008) Personality disorders and pathological gambling: a review and re-examination of prevalence rates. Journal of Personality Disorders 22: 191–207. [DOI] [PubMed] [Google Scholar]
- Batstra L, Bos EH, Neeleman J. (2002) Quantifying psychiatric comorbidity—lesions from chronic disease epidemiology. Social Psychiatry and Psychiatric Epidemiology 37: 105–111. [DOI] [PubMed] [Google Scholar]
- Battersby M, Tolchard B, Scurrah M, et al. (2006) Suicide ideation and behaviour in people with pathological gambling attending a treatment service. International Journal of Mental Health and Addiction 4: 233–246. [Google Scholar]
- Berkson J. (1946) Limitations of the application of four fold table analysis to hospital data. Biomedical Bulletin 2: 4753. [PubMed] [Google Scholar]
- Black DW. (2004) An open-label trial of bupropion in the treatment of pathologic gambling. Journal of Clinical Psychopharmacology 24: 108–110. [DOI] [PubMed] [Google Scholar]
- Blaszczynski A, Steel Z. (1998) Personality disorders among pathological gamblers. Journal of Gambling Studies 14: 51–71. [DOI] [PubMed] [Google Scholar]
- Borenstein M, Hedges LV, Higgins JPT, et al. (2009) Introduction to Meta-Analysis. New York: Wiley. [Google Scholar]
- Breen RB, Zimmerman M. (2002) Rapid onset of pathological gambling in machine gamblers. Journal of Gambling Studies 18: 31–43. [DOI] [PubMed] [Google Scholar]
- Cavedini P, Riboldi G, Keller R, et al. (2002) Frontal lobe dysfunction in pathological gambling patients. Biological Psychiatry 51: 334–341. [DOI] [PubMed] [Google Scholar]
- Crockford DN, El-Guebaly N. (1998) Psychiatric comorbidity in pathological gambling: A critical review. Canadian Journal of Psychiatry 43: 43–50. [DOI] [PubMed] [Google Scholar]
- Dannon PN, Lowengrub K, Shalgi B, et al. (2006) Dual psychiatric diagnosis and substance abuse in pathological gamblers: a preliminary gender comparison study. Journal of Addictive Diseases 25: 49–54. [DOI] [PubMed] [Google Scholar]
- Dowling NA, Cowlishaw S, Jackson AC, et al. (2014a) The prevalence of comorbid personality disorders in treatment-seeking problem gamblers: A systematic review and meta-analysis. Journal of Personality Disorders September 23: 1–20. Epub ahead of print. [DOI] [PubMed] [Google Scholar]
- Dowling NA, Jackson AC, Suomi A, et al. (2014b) Problem gambling and family violence: Prevalence and patterns in help-seeking populations. Addictive Behaviors 39: 1713–1717. [DOI] [PubMed] [Google Scholar]
- Dowling NA, Rodda SN, Lubman DI, et al. (2014c) The impacts of problem gambling on concerned significant others accessing web-based counselling. Addictive Behaviors 39: 1253–1257. [DOI] [PubMed] [Google Scholar]
- Echeburua E, Fernandez-Montalvo J. (2008) Are there more personality disorders in treatment-seeking pathological gamblers than in other kind of patients? A comparative study between the IPDE and the MCMI. International Journal of Clinical and Health Psychology 8: 53–64. [Google Scholar]
- Echeburua E, Fernandez-Montalvo J, Baez C. (2001) Predictors of therapeutic failure in slot-machine pathological gamblers following behavioural treatment. Behavioural and Cognitive Psychotherapy 29: 379–383. [Google Scholar]
- Echeburua E, Gonzalez-Ortega I, de Corral P, et al. (2011) Clinical gender differences among adult pathological gamblers seeking treatment. Journal of Gambling Studies 27: 215–227. [DOI] [PubMed] [Google Scholar]
- Goudriaan AE, De Ruiter MB, Van Den Brink W, et al. (2010) Brain activation patterns associated with cue reactivity and craving in abstinent problem gamblers, heavy smokers and healthy controls: An fMRI study. Addiction Biology 15: 491–503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grall-Bronnec M, Wainstein L, Augy J, et al. (2011) Attention deficit hyperactivity disorder among pathological and at-risk gamblers seeking treatment: A hidden disorder. European Addiction Research 17: 231–240. [DOI] [PubMed] [Google Scholar]
- Granero R, Penelo E, Martinez-Gimenez R, et al. (2009) Sex differences among treatment-seeking adult pathologic gamblers. Comprehensive Psychiatry 50: 173–180. [DOI] [PubMed] [Google Scholar]
- Grant JE, Grosz R. (2004) Pharmacotherapy outcome in older pathological gamblers: A preliminary investigation. Journal of Geriatric Psychiatry and Neurology 17: 9–12. [DOI] [PubMed] [Google Scholar]
- Grant JE, Kim SW. (2002) Effectiveness of pharmacotherapy for pathological gambling: A chart review. Annals of Clinical Psychiatry 14: 155–161. [DOI] [PubMed] [Google Scholar]
- Grant JE, Kim SW. (2003) Comorbidity of impulse control disorders in pathological gamblers. Acta Psychiatrica Scandinavica 108: 203–207. [DOI] [PubMed] [Google Scholar]
- Grant JE, Kim SW, Odlaug BL, et al. (2009) Late-onset pathological gambling: Clinical correlates and gender differences. Journal of Psychiatric Research 43: 380–387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grant JE, Kim SW, Odlaug BL, et al. (2008) Daily tobacco smoking in treatment-seeking pathological gamblers: clinical correlates and co-occurring psychiatric disorders. Journal of Addiction Medicine 2: 178–184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grant JE, Potenza MN. (2006a) Escitalopram treatment of pathological gambling with co-occurring anxiety: An open-label pilot study with double-blind discontinuation. International Clinical Psychopharmacology 21: 203–209. [DOI] [PubMed] [Google Scholar]
- Grant JE, Potenza MN. (2006b) Sexual orientation of men with pathological gambling: prevalence and psychiatric comorbidity in a treatment-seeking sample. Comprehensive Psychiatry 47: 515–518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Higgins JPT, Green S. (eds). (2011). Cochrane Handbook for Systematic Reviews of Interventions. version 5.1.0 [updated March 2011]. The Cochrane Collaboration. Available at: www.cochrane-handbook.org.
- Higgins JPT, Thompson SG, Deeks JJ, et al. (2003) Measuring inconsistency in meta-analysis. British Medical Journal 327: 557–560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hodgins DC, El-Guebaly N. (2010) The influence of substance dependence and mood disorders on outcome from pathological gambling: five-year follow-up. Journal of Gambling Studies 26: 117–127. [DOI] [PubMed] [Google Scholar]
- Hollander E, Pallanti S, Allen A, et al. (2005) Does sustained-release lithium reduce impulsive gambling and affective instability versus placebo in pathological gamblers with bipolar spectrum disorders? American Journal of Psychiatry 162: 137–145. [DOI] [PubMed] [Google Scholar]
- Hunter JE, Schmidt FL. (2004) Methods of Meta-Analysis: Correcting Error and Bias in Research Findings. Thousand Oaks, CA: SAGE Publications. [Google Scholar]
- Ibanez A, Blanco C, Donahue E, et al. (2001) Psychiatric comorbidity in pathological gamblers seeking treatment. American Journal of Psychiatry 158: 1733–1735. [DOI] [PubMed] [Google Scholar]
- Jackson AC, Wynne H, Dowling N, et al. (2010) Using the CPGI to determine problem gambling prevalence in Australia: Measurement issues. International Journal of Mental Health and Addiction 8: 570–582. [Google Scholar]
- Jimenez-Murcia S, Granero Perez R, Fernandez-Aranda F, et al. (2009) Comorbidity in pathological gambling: Clinical variables, personality and treatment response. Revista de Psiquiatria y Salud Mental 2: 178–189. [DOI] [PubMed] [Google Scholar]
- Jüni P, Witschi A, Bloch R, et al. (1999) The hazards of scoring the quality of clinical trials for meta-analysis. JAMA 282: 1054–1060. [DOI] [PubMed] [Google Scholar]
- Kausch O. (2003a) Patterns of substance abuse among treatment-seeking pathological gamblers. Journal of Substance Abuse Treatment 25: 263–270. [DOI] [PubMed] [Google Scholar]
- Kausch O. (2003b) Suicide attempts among veterans seeking treatment for pathological gambling. Journal of Clinical Psychiatry 64: 1031–1038. [DOI] [PubMed] [Google Scholar]
- Kausch O. (2004) Pathological gambling among elderly veterans. Journal of Geriatric Psychiatry and Neurology 17: 13–19. [DOI] [PubMed] [Google Scholar]
- Kennedy CH, Cook JH, Poole DR, et al. (2005) Review of the first year of an overseas military gambling treatment program. Military Medicine 170: 683–687. [DOI] [PubMed] [Google Scholar]
- Kerber CS, Black DW, Buckwalter K. (2008) Comorbid psychiatric disorders among older adult recovering pathological gamblers. Issues in Mental Health Nursing 29: 1018–1028. [DOI] [PubMed] [Google Scholar]
- Korman L, Collins J, Littman-Sharp N, et al. (2008) Randomized control trial of an integrated therapy for comorbid anger and gambling. PSYCHOTHER RES 18: 454–465. [DOI] [PubMed] [Google Scholar]
- Kroeber HL. (1992) Roulette gamblers and gamblers at electronic game machines: where are the differences? Journal of Gambling Studies 8: 79–92. [DOI] [PubMed] [Google Scholar]
- Kruedelbach N, Walker H, Chapman H, et al. (2006) Comorbidity on disorders with loss of impulse-control: Pathological gambling, addictions and personality disorders. Actas Espanolas de Psiquiatria 34: 76–82. [PubMed] [Google Scholar]
- Ladouceur R, Sylvain C, Sevigny S, et al. (2006) Pathological gamblers: Inpatients’ versus outpatients’ characteristics. Journal of Gambling Studies 22: 443–450. [DOI] [PubMed] [Google Scholar]
- Ledgerwood DM, Petry NM. (2006) Posttraumatic stress disorder symptoms in treatment-seeking pathological gamblers. Journal of Traumatic Stress 19: 411–416. [DOI] [PubMed] [Google Scholar]
- Lee KM, Guo S, Manning V, et al. (2011) Are the demographic and clinical features of pathological gamblers seeking treatment in singapore changing? Singapore Medical Journal 52: 428–431. [PubMed] [Google Scholar]
- Lesieur HR, Blume SB. (1987) The South Oaks Gambling Screen (SOGS): A new instrument for the identification of Pathological gamblers. American Journal of Psychiatry 144: 1184–1188. [DOI] [PubMed] [Google Scholar]
- Lorains FK, Cowlishaw S, Thomas SA. (2011) Prevalence of comorbid disorders in problem and pathological gambling: systematic review and meta-analysis of population surveys. Addiction 106: 490–498. [DOI] [PubMed] [Google Scholar]
- Maccallum F, Blaszczynski A. (2002) Pathological gambling and comorbid substance use. Australian and New Zealand Journal of Psychiatry 36: 411–415. [DOI] [PubMed] [Google Scholar]
- Marotta JJ. (2003) Oregon’s Problem Gambling Services: Public health orientation in a stepped care approach. The Electronic Journal of Gambling Issues 9. doi: 10.4309/jgi.2003.9.15. [DOI] [Google Scholar]
- Martins SS, Tavares H, Da Silva Lobo DS, et al. (2004) Pathological gambling, gender, and risk-taking behaviors. Addictive Behaviors 29: 1231–1235. [DOI] [PubMed] [Google Scholar]
- Milton S, Crino R, Hunt C, et al. (2002) The effect of compliance-improving interventions on the cognitive-behavioural treatment of pathological gambling. Journal of Gambling Studies 18: 207–229. [DOI] [PubMed] [Google Scholar]
- Moher D, Liberati A, Tetzlaff J, et al. (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Annals of Internal Medicine 151: 264–269. [DOI] [PubMed] [Google Scholar]
- Neal P, Delfabbro P, O’Neil M. (2005) Problem gambling and harm: Towards a national definition. Melbourne: Gambling Research Australia. [Google Scholar]
- Patterson JC, Holland J, Middleton R. (2006) Neuropsychological performance, impulsivity, and comorbid psychiatric illness in patients with pathological gambling undergoing treatment at the CORE Inpatient Treatment Center. Southern Medical Journal 99: 36–43. [DOI] [PubMed] [Google Scholar]
- Petry NM. (2005) Comorbidity of disordered gambling and other psychiatric disorders. Washington, DC: American Psychological Association. [Google Scholar]
- Productivity Commission. (1999) Australia’s gambling industries, Report No. 10. Canberra AusInfo. [Google Scholar]
- Rodda S, Lubman DI, Dowling NA, et al. (2013a) Web-based counseling for problem gambling: exploring motivations and recommendations. Journal of Medical Internet Research 15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rodda SN, Lubman DI, Dowling NA, et al. (2013b) Reasons for using web-based counselling among family and friends impacted by problem gambling. Asian Journal of Gambling Issues and Public Health 3: 1–11. [Google Scholar]
- Rodda SN, Lubman DI, Cheetham A, et al. (2015) Single session web-based counselling: A thematic analysis of content from the perspective of the client. British Journal of Guidance and Counselling 43: 117–130. [Google Scholar]
- Sander W, Peters A. (2009) Pathological gambling: influence of quality of life and psychological distress on abstinence after cognitive-behavioral inpatient treatment. Journal of Gambling Studies 25: 253–262. [DOI] [PubMed] [Google Scholar]
- Slutske WS, Eisen S, Xian H, et al. (2001) A twin study of the association between pathological gambling and antisocial personality disorder. Journal of Abnormal Psychology 110: 297–308. [DOI] [PubMed] [Google Scholar]
- Smith D, Harvey P, Battersby M, et al. (2010) Treatment outcomes and predictors of drop out for problem gamblers in South Australia: a cohort study. Australian and New Zealand Journal of Psychiatry 44: 911–920. [DOI] [PubMed] [Google Scholar]
- Specker SM, Carlson GA, Christenson GA, et al. (1995) Impulse control disorders and attention deficit disorder in pathological gamblers. Annals of Clinical Psychiatry 7: 175–179. [DOI] [PubMed] [Google Scholar]
- Specker SM, Carlson GA, Edmonson KM, et al. (1996) Psychopathology in pathological gamblers seeking treatment. Journal of Gambling Studies 12: 67–81. [DOI] [PubMed] [Google Scholar]
- Stinchfield R, Winters KC. (2001) Outcome of Minnesota’s gambling treatment programs. Journal of Gambling Studies 17: 217–245. [DOI] [PubMed] [Google Scholar]
- Stroup DF, Berlin JA, Morton SC, et al. (2000) Meta-analysis of observational studies in epidemiology: a proposal for reporting. JAMA 283: 2008–2012. [DOI] [PubMed] [Google Scholar]
- Suurvali H, Hodgins DC, Toneatto T, et al. (2012) Hesitation to seek gambling-related treatment among Ontario problem gamblers. Journal of Addiction Medicine 6: 39–49. [DOI] [PubMed] [Google Scholar]
- Tavares H, Gentil V. (2007) Pathological gambling and obsessive-compulsive disorder: Towards a spectrum of disorders of volition. Revista Brasileira de Psiquiatria 29: 107–117. [DOI] [PubMed] [Google Scholar]
- Tavares H, Martins SS, Lobo DSS, et al. (2003) Factors at play in faster progression for female pathological gamblers: An exploratory analysis. Journal of Clinical Psychiatry 64: 433–438. [DOI] [PubMed] [Google Scholar]
- Teo P, Mythily S, Anantha S, et al. (2007) Demographic and clinical features of 150 pathological gamblers referred to a community addictions programme. Annals of the Academy of Medicine Singapore 36: 165–168. [PubMed] [Google Scholar]
- Viswanathan M, Ansari M, Berkman N, et al. ( 2012) Assessing the Risk of Bias of Individual Studies in Systematic Reviews of Health Care Interventions. AHRQ Publication No. 12-EHC047-EF. Rockville, MD: Agency for Healthcare Research and Quality Methods Guide for Comparative Effectiveness Reviews; Available at: www.effectivehealthcare.ahrq.gov. [PubMed] [Google Scholar]
- Westphal JR, Johnson LJ. (2007) Multiple co-occurring behaviours among gamblers in treatment: Implications and assessment. International Gambling Studies 7: 73–99. [Google Scholar]
- Winters KC, Kushner MG. (2003) Treatment issues pertaining to pathological gamblers with a comorbid disorder. Journal of Gambling Studies 19: 261–277. [DOI] [PubMed] [Google Scholar]
- Zimmerman M, Galione JN, Chelminski I, et al. (2010) A simpler definition of major depressive disorder. Psychological Medicine 40: 451–457. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.