Abstract
Introduction:
This paper examines the organization, services, and priorities of public health agencies and their capacity to be learning public health systems (LPHS). An LPHS uses data to measure population health and health risks and to evaluate its services and programs, and then integrates its own research with advances in scientific knowledge to innovate and improve its efficiency and effectiveness.
Public Health Agencies and Impact for LPHS:
Public health agencies’ (PHA) organizational characteristics vary across states, as does their funding per capita. Variations in organization, services provided, and expenditures per capita may reflect variations in community needs or may be associated with unmet needs. The status of legal statutes defining responsibilities and authorities and their relationships to other public and private agencies also vary. Little information is available on the efficiency and effectiveness of state and local PHAs, in part due to a lack of information infrastructure to capture uniform data on services provided. There are almost no data on the relationship of quality of services, staff performance, and resources to population health outcomes. By building a capacity to collect and analyze data on population health within and across communities, and by becoming a continuous learning PHA, the allocation of resources can more closely match population health needs and improve health outcomes. Accreditation of every PHA is an important first step toward becoming a learning PHA.
Conclusions:
Public Health Services and Systems Research (PHSSR) is beginning to shed light on some of these issues, particularly by investigating variation across PHAs. As this emerging discipline grows, there is a need to enhance the collection and use of data in support of building organized, effective, and efficient LPHSs with the PHA capacity to continually improve the public’s health.
Keywords: Public Health, PHSSR, organization
Introduction
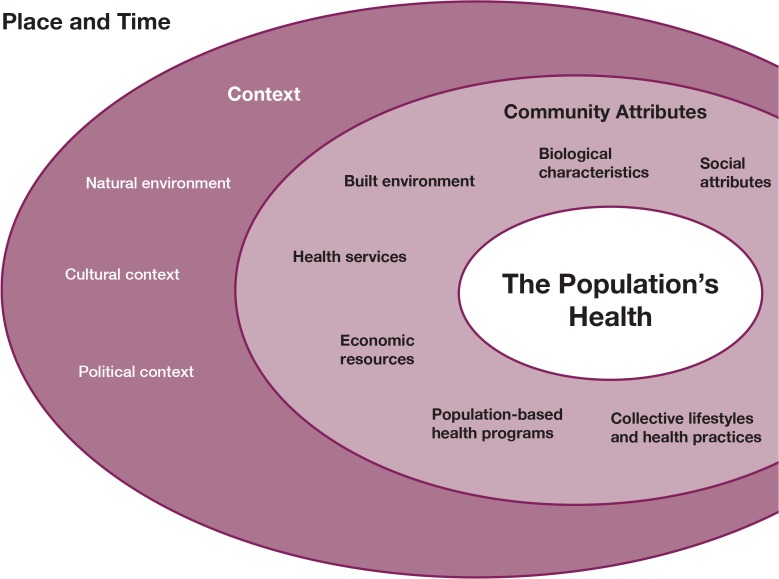
The Public Health Leadership Forum (May 2014) described its vision for 2020 of a high achieving PHA and called for new practices and skills that can address the changing circumstances. These circumstances include changing demographic and health care needs, an explosion of health information and data, and a shift in priorities to respond to the increasing prevalence of chronic diseases, “often a key to optimizing the health of the public.” Central to a high achieving PHA will be a new generation of information systems with the capacity to examine the range of factors (Figure 1) affecting population health, to identify health disparities, and to provide information needed to evaluate public health interventions. At the same time, PHAs face organizational challenges, wide variations in funding levels, and inconsistent legal statutes defining their mission and services. As a result, PHAs vary significantly in the services they provide and the health status of communities served. This paper first addresses how public health’s guiding principles align in support of an effective, efficient, and continuous learning to become learning public health systems (LPHSs). With this goal of continuous learning in mind, the paper then explores the complex interdependencies and Public Health Services and Systems Research (PHSSR) research questions that need to be addressed in key areas such as PHA agencies’ legal authority, funding, structure and organization, and performance. Major data sources, data gaps, and strategies for collecting and applying the data that are needed to address critical PHSSR questions with respect to PHA organization, quality, and efficiency are discussed.
Figure 1.
Conceptual Framework for Population Health National Committee on Vital Health Statistics58
Guiding Frameworks: Public Health Agency (PHA) Organization, Services, and Performance
Learning Public Health System Characteristics
The Institute of Medicine (IOM) published a series of reports on learning health care systems and the necessity for transformational change in health and health care.1 As interpreted by the Academic Health Department Learning Community,2 the essential characteristics of an LPHS are listed in Table 1 with examples of data sources and measures.
Table 1.
Essential Characteristics of a Learning Public Health System (LPHS)
| Science and Informatics | Essential Characteristics of Learning Public Health System | Data Sources and Measures |
|---|---|---|
| In-time access to knowledge | The LPHS reliably captures and delivers the best available evidence to guide and support decision-making to improve population health through assessment, policy development, and assurance. | American Community Survey provides social, economic, and housing characteristics data on the population annually; 10 states have systems for merging claims data from all health insurers to monitor cost and use of services. PHA relevant including measures include use of preventive services, continuity of medication treatment for chronic conditions, and rates of preventable hospitalizations. |
| Digital capture of data | The capture of data on population health indicators and the changing characteristics of communities and contextual changes provide the basis for in-time generation and application of knowledge. | Health Information Exchanges can access electronic health record data and have the potential to aggregate key indicators of health-illness in populations and to identify trends. |
| Community-PHA Relationships | ||
| Engaged and empowered communities | The LPHS is anchored on community needs and promotes community inclusion as members of the LPHS team. | Assess community health needs through surveys, analysis of health and health services data, and document disparities and high need groups. |
| Incentives | ||
| Incentives aligned for value | Incentives structured to encourage continuous improvement, minimize waste, and promote value (ratio of population health improvement divided by cost). | Collect data on incentives, changes in incentives and individuals/groups targeted for incentives. Examine the relationship of incentives to disparities, use of services, and health status indicators. |
| Full transparency | The LPHS monitors context, community characteristics, quality processes, cost, and population health outcomes and makes information available to communities, policymakers and PHA staff. | Identify the range of methods used to share information with communities, policymakers, and PHA staff and assess their effectiveness. |
| Culture | ||
| Leadership instilled culture of learning | “Leadership commitment to a culture of teamwork, collaboration, and adaptability in support of continuously learning as a core aim.”3 | Survey PHA leadership and staff to assess organizational culture including teamwork, collaboration, and adaptability. |
| Supportive system competencies | “Complex community intervention operations and support processes are “constantly being refined through team training and skill building, systems analysis and information development, and creation of the feedback loops for continuous learning and system improvement.”4 | LPHS constantly refines its data sources and analyses of community needs and services provided by the PHA; measures quality, efficiency, and population outcomes; and provides feedback to communities, policymakers and PHA staff. |
An essential LPHS characteristic is the role of agency leadership in instilling a culture of learning in the organization Management research provides insights into leadership styles and actions that support culture change and learning. Edmonson discusses how organizations can learn from failure5. The common human tendency is to assign blame and then not learn from the failure experience. She concludes that only leaders can create a culture that counteracts blame and makes people comfortable with discussing and learning from failure.
Core Functions, Essential Services, and the Role of Accreditation
The vision of an LPHS is for PHAs to have the organizational capacity to use data and evidence to drive system priorities and to support public health practice with timely information on quality, cost, and population health outcomes. A useful framework for examining organizational capacity and data gaps for PHSSR is to review the 3 core functions of public health (assessment, policy development, and assurance) and the 10 essential services needed to carry out the core functions.6,7 According to the Centers for Disease Control and Prevention (CDC), the core functions and essential services provide a foundation for any public health activity; describe public health at the state, tribal, local, and territorial levels; and provide structure for national voluntary public health accreditation.8
In an effort to strengthen PHAs, the Public Health Accreditation Board (PHAB) was established. PHAB formally accredits PHAs and requires all accredited PHAs to meet nationally accepted standards. PHAB’s vision, a high-performing governmental public health system that will make the United States a healthier nation, could be supported by the adoption of a culture of continuous learning in PHAs. Such a culture would provide the model for responding to health risks, complex social and environmental factors, and evolving scientific evidence.
PHAB requires the PHA to demonstrate its capacity to do the following: (1) perform a community health assessment, (2) develop a community health improvement plan, and (3) develop a 3–5 year strategic plan. A natural starting point for developing the capacity and the culture of an LPHS in a PHA would be to tackle these data intensive requirements and apply for accreditation.
Table 2 maps these three PHAB requirements with the essential characteristics of an LPHS and the core functions and essential services of a PHA. Also noted are the activities, associated with each essential service, that involve a major data component. The table depicts the interrelationships between these guiding frameworks, and supports the notion that governmental PHAs are organized and structured to support the development, use, and application of data.
Table 2.
Relationship of Public Health Agency (PHA) Core Functions and Essential Services to Essential Characteristics of a Learning Public Health System (LPHS) and Selected Public Health Board Accreditation (PHAB) Requirements
| Core Functions, Essentials Services, and Organizational Culture (major data components included where applicable) | Essential Characteristics of a Learning Public Health System (LPHS) | Public Health Accreditation Board (PHAB): Data Intensive Requirements for Meeting Accreditation Standards |
|---|---|---|
| I. Assessment | ||
| 1. Monitor health status to identify and solve community health problems (data Intensive and involving epidemiologic research skills). | In-time access to knowledge.9 Digital capture of data.10 |
Community Health Assessment (CHA): Learn health status of community, identify areas for health improvement, including special populations and contributing causes of health issues. |
| 2. Diagnose and investigate health problems and hazards in the community (requires data and research skills). | ||
| II. Policy Development | ||
| 3. Inform, educate, and empower people about health issues (PHA working collaboratively with the community sharing and interpreting data). | Full transparency: monitors context, community characteristics, quality processes, etc.—and makes information available to communities.11 | |
| 4. Mobilize community partnerships and action to identify and solve health problems (PHA working collaboratively with the community in data analysis and its interpretation). | Engaged and empowered communities: anchored on community needs and promoting community inclusion as part of LPHS team.12 | Community Health Improvement Plan (CHIP): Plan for working together with community to improve health of the populations, including policy changes needed to achieve objectives. |
| 5. Develop policies and plans that support individual and community health efforts. (PHA working collaboratively with the community in planning and policy analysis using data). | Supportive system competencies: complex community intervention operations are constantly being refined through team training and skill building, systems analysis and information development, and creation of feedback loops for continuous learning and system improvement.13 | Health Department Strategic Plan (HDSP) Plan for 3–5 years with strategic priorities, goals, measurable objectives, defined time frame, link to CHIP, and quality improvement (QI) plan |
| III. Assurance | ||
| 6. Enforce laws and regulations that protect health and ensure safety. | ||
| 7. Link people to personal health services and ensure the provision of health care when it is otherwise not available. | ||
| 8. Assure competent public and personal health care workforce (training of workforce). | Supportive team competencies: “team training and skill building, systems analysis, and information development.”14 | |
| 9. Evaluate effectiveness, accessibility, and quality of personal and population-based health services (data intensive with strong analytics). | Incentives aligned for value; incentives encourage continuous improvement, minimize waste, and promote value.15 | |
| 10. Research for new insights and innovative solutions for health problems (may be data intensive, and requires research skills). | ||
| Public Health Agency (PHA) Organizational Culture (leadership builds a culture of continuous learning in the public health system and PHA). | Leadership-instilled culture of learning: leadership commitment to a culture of teamwork, collaboration, and adaptability in support of continuous learning as a core aim.16 | PHA accreditation reinforces key organizational goals and builds organizational capacity to identify community health problems; work with community to develop and implement a quality improvement (QI) plan, and to evaluate the effects of QI improvement on population health outcomes. |
Public Health Coming into the 21st Century: Legal Considerations, Funding, and Local Priorities
Legal Authority
The mission, authority, and responsibility of a state PHA should be specified in state statutes. Yet a study of the status of state laws governing public health functions found great variability in the comprehensiveness of statutes: “Given the centrality of law to the mission, structure, and workforce in public health,” the authors found “state public health laws are often antiquated, fragmented, inconsistent, and incomplete.”17 This is alarming, given that “law is a critical component to each of three elements of the national public health infrastructure: (1) health data and other factual information, (2) a competent workforce, (3) systems and relationships.”18
Understanding the inadequacies of state statutes, IOM—in its 2003 report on the future of public health—recommended that states use the Turning Point Model Public Health Act (TPMPHA) to achieve public health law reform by using standard statutory language to reflect the mission and essential services of public health.19 The TPMPHA addressed the following: (1) purpose and definitions; (2) mission and function; (3) public health infrastructure; (4) collaboration and relationships with public and private partners; (5) public health authorities and powers; (6) public health emergencies; (7) declaring a state public health emergency; (8) public health information privacy; and (9) administrative procedures, civil and criminal enforcement, and immunities. After September 11th, 2001, the drafting committee took the Model State Emergency Health Powers Act and folded it into the TPMPHA with a few edits to into public health acts.20
Subsequent to the 2003 IOM recommendation, a study assessed the status of adoption of the TPMPHA,21 including defining the 10 essential public health services in statutes.22,23 Although there was progress by 2008, only 17 of the 50 states had put in place statutes covering 7 or more of the 10 essential services and, notably, only 4 states had codified statutes for all 10 essential services. Half (4–6) of the essential services were codified by 26 states, and the remaining 7 states codified 3 or fewer. States with a mission statute consistent with TPMPHA increased from 10 to 22 states. The failure of the majority of states to create statutes for all 10 essential services suggests uncertain commitment to comprehensive services.
Of the 10 essential services, 3 overlap with core aspects of the LPHS: (1) monitor health status, (2) evaluate health services, and (3) conduct research on new insights and innovative solutions to health problems. Monitoring health status was included in statutes by 2008 in 41 states. However, only 18 states had statutes for the evaluation of health services, and only 8 had statutes for research into new solutions for public health problems.24
States reported that many services were provided that were not in statutes,25 as would be expected. Nearly all states (49 of 51 including the District of Columbia) reported monitoring behavioral risk factors, infectious diseases, reportable diseases, and vital statistics. Similarly, in the essential services categories of evaluation and research, over 90 percent of the states reported analyzing and interpreting data and over 70 percent reported applying the findings to improve practice. Over half were involved in research, ranging from developing research and evaluation questions to collaborating with external researchers. On average, states participated or led 32 research or evaluation studies, varying from a high of 217 studies to a low of 2 studies. Monitoring activities focused on mortality, morbidity, and state-level behavioral risk factors and may have captured a few health indicators. The capacity of states to rigorously evaluate their own programs and to conduct research on potentially promising interventions was unclear in the Association of State and Territorial Health Officials (ASTHO) survey, and likely varied widely.26 In Table 3, research questions are proposed related to legal statute and the use of findings from PHA program evaluation studies.
Table 3.
Research Questions for Legal Status of Public Health Mission and Services
| Research Questions for Legal Status of Public Health Mission and Services | Data Sources | Next Steps |
|---|---|---|
| Has the creation of legal statutes for essential services ensured provision of services, adequate funding, and PHA accountability? Is PHA staffing and infrastructure adequate to provide the full range of essential services? | Collect data from state public health agencies including state statutes and dates of enactment, trends in PHA statistics on essential services provided, staffing, and funding levels. Examine factors associated with unmet needs and failure to provide one or more essential services. Is there a relationship between legal mandate and provision of the 10 essential services? | Select successful and less successful state public health agencies to provide interviews and data leading to publication of case studies useful to states. |
| Are program evaluation and research services being used to support a learning health system process, including QI and improved efficiency? | Review publications and reports of past and current evaluation programs including documentation of studies undertaken, focus of studies, relevance of results for quality and efficiency improvement, and evidence of use of study findings. | Interview selected state PHAs with different approaches to program evaluation to learn how the information was used to improve quality and efficiency of essential services. |
Funding
Research questions for PHSSR related to funding for public health are noted in another paper in this special issue, see Corso et al.27
Public Health Agency (PHA) Priorities
In 2013, the Institute of Medicine (IOM) report Shorter Lives, Poorer Health observed that the United States is one of the wealthiest countries in the world, but not one of the healthiest. When compared with the average of peer countries, Americans as a group fare worse in at least nine health areas, including infant mortality and low birth weight, homicides, HIV and AIDS, drug-related deaths, obesity and diabetes, heart disease, and chronic lung disease. To overcome this U.S. health disadvantage, we will need to sustain and strengthen primary prevention initiatives and focus more resources on secondary prevention (disease management) for chronic disorders. However, governmental public health agencies are stretched thin. According to the 2010 ASTHO survey,28 the priorities in state PHAs were infrastructure (40 states); quality improvement (QI) (21 states); health promotion (18 states); obesity, nutrition, and physical activity (14 states); and emergency preparedness (14 states). Only 10 states cited chronic conditions as a priority.
To be successful in tackling these complex challenges, stronger partnerships are needed between public health (population health) and medical providers (individual health), as well as with community organizations and human service organizations. A growing national movement toward upstream, multisectoral approaches to tackling health challenges is supported by the Robert Wood Johnson Foundation’s new Culture of Health strategy, the growing field of health impact assessment, and the increasing urgency to tackle health care costs. It has been suggested that PHAs become the Chief Health Strategists, or “integrators,” in communities; achieving public health accreditation and fostering an LPHS would be the first steps toward serving in those roles.29,30
Future Directions for PHSSR
Taken together—the goals of LPHS, core functions and essential services of PHA, context of legal and funding, and local priorities that have been discussed—set the stage for future directions and questions PHSSR must tackle. The following sections explore key research questions, data sources, and next steps for PHSSR with respect to PHA’s organization and data infrastructure, performance and quality measurement, and measures of organizational efficiency.
Public Health Agency (PHA) Organization and Data Infrastructure
Organizational capacity and committed PHA leadership provide the essential foundation required for an LPHS. PHA organization and reporting relationships vary widely across states.31 In 23 states the PHA is part of a large umbrella organization. Umbrella organizations are ones in which the PHA does not stand alone but has been merged with other health agencies under the same leadership. The ASTHO survey reported that, in most cases, when PHA is part of a larger umbrella organization it includes long-term care, Medicaid and public assistance, and mental-health and substance-abuse services. Among states without a large umbrella organization, some non-PHA services may be present, including services for the aging and elderly, child and family services, services for individuals with disabilities, and licensure of health professionals and facilities. The implications for PHA performance within an umbrella organization, as well as implications for PHA leadership needed to grow the culture of an LPHS, are not clear.
PHSSR on PHA organizational structures has examined three characteristics: differentiation (the different programs and activities delivered), integration (the extent to which services are provided through relationships with other organizations), and centrality (the concentration or distribution of authority at the state- or local level).32 In an analysis of PHAs with 100,000 or greater population (17 percent of all PHAs), PHAs were found to vary widely in organizational structure, yet could be clustered in seven distinct configurations. Examining organizational changes between 1998 and 2006, many PHAs were found to have migrated from one configuration to another, changing the mix of differentiation, integration, and centrality in the organization. The research base linking agency structure to PHA performance over time, and to health outcomes, is thin but growing.33 In Table 4, research questions are proposed related to organization and the performance of the PHA as an LPHS.
Table 4.
Research Questions for Organization and Data Infrastructure and Being a Learning Public Health System (LPHS)
| Organization and Data Infrastructure Research Questions | Data Sources | Next Steps |
|---|---|---|
| Does the organizational structure (e.g., umbrella organization and differentiation, integration, and centralization) facilitate or impede the sharing of public health data across organizational units? Is the information shared used to aid in coordination of services and programs? | Survey PHA leadership and staff asking questions on relationships between organizational units in the PHA and its partners who comprise the Public Health System (PHS). Do staff in different units share data and information, how is this done, and information, how is this done, and what are the benefits and costs. | If organizational characteristics are related to willingness and capacity to share data across units, is this related collaboration occurring across units in the development and implementation of health initiatives? Is there collaboration in program evaluation of services provided? |
| To what extent and how effectively are PHAs with various organizational structures partnering with medical care providers and communities to improve the prevention of chronic diseases and their management? Is chronic disease a priority for the PHA? | The prevalence of chronic diseases in communities, receipt of preventive services, and population outcomes can be estimated from health insurance claims data, except for the uninsured. Linking indicators of poor outcomes (e.g., preventable hospitalizations and ER visits) may be useful in identifying PHA service gaps and poor access to needed care. | Based on service gaps, surveys of PHS leadership and staff are needed to identify how unmet needs are being or should be addressed. This can be enriched with the availability of community- level information on coordination of care and collaboration with medical providers. In the survey, ask about perceived barriers to improving chronic disease services and outcomes. |
| To what extent do the organizational characteristics of differentiation, integration, and centralization enhance or detract from PHA capacity to provide essential services? Are these organizational characteristics associated whether or not a PHA becomes accredited and is likely to become an LPHS? | Research has shown that PHAs vary in organizational differentiation, integration, and centralization. Linking data on these organizational characteristics with data on essential services provided, quality of services, and level of efficiency can focus attention on organizational structures associated with greater effectiveness. | Assess the extent to which the PHAs are functioning as LPHS using leadership and staff surveys, and examine the relationship of LPHS to the PHA’s level of organizational differentiation, integration, and centralization in service delivery and in the collection, analysis, and interpretation of community public health data. |
| Does PHA’s control over information technology—as compared to being a user of systems controlled by others—for receiving, storing, and analyzing public health data enhance or detract from PHA’s effectiveness in monitoring, evaluation and research, and foundational components of an LPHS? | Use ASTHO survey data and initiate new surveys of PHAs nationally to identify the status of their information technology, extent of control of the technology and data by the PHA or a higher authority, and the types of information available to the PHA. | Bring PHAs together to define a minimum data set that should be available to all PHAs for monitoring and surveillance and facilitate access. Identify potential data sources to enhance the minimum data set and to support evaluations of community health interventions. |
Data Infrastructure and a Learning Public Health System
While the explosion of data and data sources over the past few decades is providing new opportunities for public health, they are significant challenges for data users seeking the best data to inform public health surveillance, policy development, and assessment (evaluation). Electronic health records (EHR) are collecting rich clinical data that are largely free-text and not easily aggregated or analyzed. Health interview surveys of the Centers for Disease Control and Prevention (CDC) National Center for Health Statistics are nationally representative and informative, but sample sizes are insufficient for small area analysis, e.g., at the county- or ZIP code levels. The Bureau of the Census’s American Community Survey has the sample size needed to describe the socioeconomic characteristics of small population groups, but safeguards to protect confidentiality require users to analyze data through government data centers. Health insurance claims data provide coded diagnoses, medical procedures, and preventive services for insured population groups—but not for the uninsured. There are other data concerns in public health. Timely data is needed to ensure early recognition of emerging health threats, but cleaning of data sets and their availability may lag by months or years. The quality of data, as well as gaps in data, may be of concern. For example, there are few sources for measuring population health status and well-being. Much more is known about disease, disability, and death than is known about population health. The importance of data in public health is in its applications for surveillance and health monitoring, for planning community QI initiatives, for intervention evaluation, and for research into innovative solutions for health problems.
The development of learning organizations has been actively promoted in public health over the last decade. Notably, the Robert Wood Johnson Foundation (RWJF) funded the Common Ground project to accelerate the transformation of information systems used in PHAs.34 The project relied on working groups drawn from participating PHAs with consultant support to address common core concerns, the standardization of data and data definitions, and key aspects of system redesign. The guiding concept was that all PHAs face common issues and have similar needs for information to respond to pandemics and bioterrorism, to intervene with chronic diseases, to establish best practices, and to develop training for public health staff. The experience was found to be positive for PHAs.35
More recently, the Academic Health Department (AHD) Learning Community was established with CDC support and open to all PHAs. “The AHD is meant to enhance public health education and training, research, and service by facilitating collaboration across the academic and practice communities.” Through this partnership, LPHSs are being developed and strengthened.36
In a parallel development under the Health Information Technology for Economic and Clinical (HITECH) act,37 17 Beacon Communities38 were funded on a competitive basis to develop models for community-level public health information systems. The Beacon focus was on using electronic medical record (EMR) data as a source of population health indicators, particularly morbidity and receipt of preventive services, which is unavailable in most communities. The program brought Beacon communities together to share their learning experiences.39
Sources of Data
The need for state- and local-level health data to inform PHA priorities and program evaluation is widely recognized. The Affordable Care Act of 2009 made funds available to expand the sample in the National Center for Health Statistics surveys, making state-level estimates feasible. Also, the Bureau of the Census’s American Community Survey (ACS) provides state- and community-level data on population characteristics. State Health Access Data Assistance Center (SHADAC), uses ACS data and other sources to make available state- and county-level data on access to care, insurance coverage, and sources of insurance.40 Comparable national data on community health status and need for services are not available. For this reason, there is increasing interest in using clinical data from EHRs to meet some of these information needs.
The volume of electronic data sent and received by PHAs is increasing.41 In a recent ASTHO survey, over 80 percent reported exchanging electronic data directly with providers, and 20 percent reported using direct data exchange through an intermediary. Almost half of PHAs reported having overall authority for information exchange and health technology. More than 90 percent of state agencies exchange information with hospitals, and over 80 percent report electronic information exchange with laboratories, providers, and local health departments. Exchange of data with Medicaid agencies is reported by over 60 percent, with community health centers by over 50 percent, and with insurers and health plans by over 40 percent.
There are recognized limitations and implementation barriers to be considered in using EMR for public health purposes. These include the following: (1) EMRs may be missing the desired data, including environmental and psychological factors, and data reliability and validity is uneven; and (2) PHAs may lack staff with necessary skill levels and may lack the resources to build a centralized system.42 Building on the lessons learned in Common Ground and Beacon Communities, the AHD is supporting a collaborative process for PHAs to learn how to access and make best use of existing and new data sources in collaboration with academic settings.
Sources of Evidence from Research for Public Health Interventions
In addition, PHAs need timely access to information based on systematic reviews of scientific evidence. In the United States, the responsibility for evidence-based reviews and evidence-based practice guidelines is widely dispersed. This is not true for preventive services where evidence-based reviews are done by the U.S. Preventive Services Taskforce.43 Complementing the evidence-based reviews is the work of the Community Preventive Services Task Force supported by the CDC. It is providing evidence-based reviews on preventive interventions for communities covering 22 major topic areas.44 Together, the two taskforces are providing critical systematic reviews of scientific evidence needed by PHAs.
In Table 4, research questions are proposed regarding the organizational and data infrastructure and implications for becoming an LPHS.
Public Health Quality Performance and Quality Measurement
The Congressionally mandated report on the National Quality Strategy states its aim as being to “Improve the health of the U.S. population by supporting proven interventions to address behavioral, social, and environmental determinants of health in addition to delivering higher quality care.”45
The 2013 IOM report, “Toward Quality Measures in Public Health”46 endorses nine aims for quality improvement in public health systems as proposed by the Public Health Quality Forum (PHQF).47 A quality public health system should be population centered, equitable, proactive, health promoting, risk reducing, vigilant, transparent, effective, and efficient (Table 5). The definition of quality in public health parallels the definition of quality for medical care: “the degree to which policies, programs, services and research for the population increase desired health outcomes and conditions in which the population can be healthy.”48
Table 5.
Quality Characteristics of Public Health Systems59
| Quality Characteristics of Public Health Systems | Description of Quality Characteristic |
|---|---|
| Population centered | Protecting and promoting healthy conditions and the health for the entire population. |
| Equitable | Working to achieve health equity. |
| Proactive | Formulating policies and sustainable practices in a timely manner, while mobilizing rapidly to address new and emerging threats and vulnerabilities. |
| Health promoting | Ensuring policies and strategies that advance safe practices by providers and the population and that increase the probability of positive health behaviors and outcomes. |
| Risk reducing | Diminishing adverse environmental and social events by implementing policies and strategies to reduce the probability of preventable injuries and illness or other negative outcomes. |
| Vigilant | Intensifying practices and enacting policies to support enhancements to surveillance activities (e.g., technology, standardization, systems thinking and modeling). |
| Transparent | Ensuring openness in the delivery of services and practices with particular emphasis on valid, reliable, accessible, timely, and meaningful data that is readily available to stakeholders, including the public. |
| Effective | Justifying investments by utilizing evidence, science, and best practices to achieve optimal results in areas of greatest need. |
| Efficient | Understanding costs and benefits of public health interventions to facilitate the optimal utilization of resources to achieve desired outcomes. |
Central to measuring quality is the measurement of desired health outcomes within population groups, data that are not generally collected. We rely on scientific studies to provide evidence on the relationship of services and specific outcomes, usually clinical outcomes. Outcomes desired by population groups will likely go beyond clinical indicators and will include well-being and functional capacity. If so, additional research will most likely be needed.
The nine public health quality aims set out by PHQF (Table 5) build on Donabedian’s quality measurement framework of structure, process, and outcome.49,50 They include the six IOM quality aims of medical care, and add quality dimensions of PHAs being proactive, health promoting, and vigilant.51
The 2013 IOM public health quality report, gives sample measures for quality in achieving United States health objectives for nutrition, physical activity and obesity.52,53 To be useful for examining population health, the measures must be amenable to distributional analysis and facilitate the identification of disparities across population subgroups.
From a systems perspective one might ask, does the quality metric need to be adapted for specific pathways or is a comprehensive measure valid, and how can these metrics be used to help understand the pathways that lead to poor nutrition, limited physical activity, and obesity? How often do poor nutrition, limited physical activity, and obesity co-occur? Are pathways different for those at greater risk of health disparities, e.g., living in poverty, diagnosed with a serious mental disorder, member of minority group, and less than a high school education? One potential advantage of pathway-specific quality measures could be the identification of pathway-specific interventions, as well as learning if specific interventions work equally well across multiple pathways.
The IOM committee on public health quality measures endorsed the use of predictive and system-based simulation models to understand health outcomes and consequences of underlying determinants of health. Modeling pathways and transition probabilities could assist in identifying priority targets for intervention, simulating the expected impact of science-based interventions, and estimating the intervention outcomes and cost. The development of simulation models will require analytic work identifying population groups, pathways, and outcomes, and how they vary with individual and community characteristics. Simulation model validation will be important. Once done, many PHAs and communities may potentially be able to use and adapt validated pathway models to assess their intervention options and expected outcomes.
The IOM committee provided criteria for selecting conditions and outcomes for public health quality measurement and intervention.54 Conditions should be reflective of a high preventable burden, and should be actionable at the appropriate level of intervention. The criteria recommended for choosing quality measures are the following: measures should be timely, usable across various populations, understandable, methodologically rigorous, and accepted and harmonized. Putting measurement in a public health framework, measures may be used for assessment at a point in time; for improvement requiring measurement over time; and for accountability to demonstrate the value of investments, effectiveness, and efficiency with healthy outcomes (e.g., self-reported well-being and quality of life, functional status, mental health, and social engagement).
Since 2010, CDC’s National Public Health Improvement Initiative (NPHII) has funded state- and local health departments to develop their capacity to undertake QI studies.55 QI relies on the application of evaluation methodologies, and organizational commitment to QI studies is a requirement for PHA accreditation by the Public Health Accreditation Board. Accreditation also requires gathering information for a community health assessment and the development of a community health improvement plan. In Table 6, research questions are proposed based on data needs to support quality measurement and assess quality performance.
Table 6.
Research Questions on Quality Performance and Quality Measurement
| Research Questions on Quality Performance and Quality Measurement | Data Sources | Next Steps |
|---|---|---|
| What are effective and efficient ways to learn about health outcomes within population groups? | Information on morbidity and mortality are available in some states (e.g., Utah and Vermont) from all insurers and from state death records. Missing from claims data are health indicators and self-reported health status. Existing state-level surveys capturing some health data are the Behavioral Health Risk Factor Survey (CDC), Health Interview Survey (National Center for Health Statistics—NCHS) and American Community Survey (Bureau of the Census). | Identify data sources that can be used to develop county- and community-level health data, e.g., merging three years of American Community Survey data by county, use of insurance claims data to measure receipt of preventive health services by county. |
| Identify medical conditions and treatments where there is evidence that desired outcomes vary across population groups. | Review medical literature and other sources to identify desired health outcomes. Examples include immunization, end of life care, mental health treatments, and religious beliefs (e.g., Christian Scientists, Jehovah’s Witnesses) | Develop quality measures for physician and patient reports of the match between desired outcomes and care offered and received. |
| What data sources and methodologies are best for modeling longitudinal health risks and outcomes and the expected impact of evidence-based interventions? | Data sources include those listed above. In addition evidence-based guidelines for common chronic conditions (Agency for Healthcare Research and Quality—AHRQ warehouse) and preventive services (United States Preventive Services Task Force—USPSTF) are required to model and simulate potential effects of changes in practice and adherence. | A partnership with academic institutions should be sought and a multidisciplinary group constituted with clinical, modeling, and other relevant expertise present. |
Public Health Data to Improve Organizational Efficiency for Social and Preventive Services
Adequacy of resources is and will continue to be a concern in achieving the objective of transforming PHAs into data and evidence-driven learning public health organizations. Per capita expenditures vary widely by state, possibly reflecting variations in the mix of urban and rural populations, the mix of public health services provided, and variation in using other organizations to provide essential services. Also, per capita expenditures may reflect variations in health disparities by state and efficiency of the PHAs.
Information systems infrastructure needs to be sufficient to support the collection, analysis, and sharing of information across the public health system, including social service agencies and health providers. For example, Alameda County Social Services Agency serves 125,000 citizens supported by an interoperable information system fed by core state systems including welfare, employment services, elderly and disabled, school districts, juvenile probation, and Oakland housing authority. Information is available to every case manager for every client, and the system can be used to identify people receiving or eligible for services across programs and geographic areas. The director, Don Edwards, stated “a primary goal…is to help management and staff to do their jobs better and more efficiently.”56
Improving efficiency requires data on staffing, services, and costs to be routinely collected and examined to understand the flow of resources and to assess the value of programs and services (value = (quality or outcomes)/cost). QI methods are useful for evaluating staffing options, technology, and work processes and making choices that improve the value of services. Sources of inefficiency may be associated with lack of adequate training of personnel, organizational silos with overlapping responsibilities, and populations served without coordination of services. For example, the coordination of services by sharing information across agencies can reduce duplication, improve follow-up, and ensure the provision of all needed services. Follow-back to service recipients and service providers can provide valuable information on the effectiveness of coordination and service quality.
There could be benefits for the PHAs to move toward a uniform set of accounts and report expenditures and income as recommended by the IOM.57 Uniform accounting reports would facilitate benchmarking costs of essential services. Uniform accounting would facilitate making comparisons across PHAs and would provide an information foundation for PHAs coming together in learning collaboratives to improve efficiency. In Table 7 research questions are proposed regarding potential efficiencies to be gained through sharing data systems and implementing uniform accounting systems.
Table 7.
Research Questions on Organizational Efficiency
| Organizational Efficiency Research Questions | Data Sources and Measures | Next Steps |
|---|---|---|
| What incentives, technical assistance, and investments are needed for PHAs, social service agencies, and health care providers to collaborate on interoperable systems to support their staff and to promote coordinated and efficient services in the community? | Routinely collect and examine data on staffing, services, and costs in order to understand the flow of resources and to assess value of programs and services. Survey public health, social services, and medical professionals to assess current level of collaboration and interest in improving care coordination. | Assess the cost of coordination of services across community providers and agencies and agencies and the benefits for experienced populations served as compared to fragmented service delivery. |
| What steps need to be taken to promote the adoption of a uniform set of accounts by PHAs? | Conduct a survey of PHAs’ attitudes toward the adoption of uniform accounting standards and national implementation. Ask what incentives would be needed to gain adoption of standards. | Provide incentives to PHAs to fully implement uniform accounting systems and compare performance to other PHAs. |
Conclusion
The organization of public health agencies, their legal mandates, levels of funding, and provision of the 10 essential services vary widely by state and by individual public health department within the state. Variation is fine if the organizational structure, leadership, staffing, and resources match the needs of the populations being served with high quality services at a reasonable cost. Variations inconsistent with population needs and unresponsive to disparities should not be acceptable. Achieving the goals of public health is to meet the needs of populations for access to housing, education, income and jobs, health insurance, medical and mental health services, and preventive services and reduction in behavioral health risks. It is likely that the variations found across PHAs are a combination of variations in levels of need as well as variations in capacity of PHAs to meeting unmet needs.
If the notion of PHA leaders as chief health strategists were embraced, public health could lead the charge toward healthier communities by enhancing the effectiveness and efficiency of PHAs; fostering innovation in data collection and use; and driving partnerships with other government agencies, community organizations, businesses, and foundations toward common goals. To be effective, public health needs to collect and analyze data, and to continually evaluate population health needs in collaboration with the community, the services provided, population health, and future priorities. Accreditation, leadership, and continuous QI can help public health agencies build and shape the skills needed to become an LPHS. By maximizing present opportunities to use new data streams and evaluate innovative new programs, PHSSR can play a major role in providing the evidence base that is needed to drive and sustain LPHS. Working with the research community, the time has come for public health agencies to engage in transformational change to improve effectiveness, efficiency, and the health of the nation.
Acknowledgments
The paper was made possible through the funding of the Robert Wood Johnson Foundation and the leadership of AcademyHealth in organizing and supporting this author and others. A national advisory group of public health experts was formed by AcademyHealth, and its members reviewed early drafts and provided valuable feedback. In addition, AcademyHealth staff provided editorial guidance and assistance in formatting.
Footnotes
Disciplines
Health Services Research | Public Health
References
- 1.Institute of Medicine . Report brief: Best care at lower cost. Washington, D C: The National Academies Press; 2012. [Google Scholar]
- 2.Academic Health Department Learning Community [Internet]. [cited 2014 January 16] Available from http://www.phf.org/programs/AHDLC/Pages/Academic_Health_Department_Learning_Community.aspx.
- 3.Institute of Medicine . Report brief: Best care at lower cost. Washington, D C: The National Academies Press; 2012. [Google Scholar]
- 4. Ibid.
- 5.Edmondson AC. Strategies for learning from failure. Harvard Business Review. 2011 Apr;:48–55. [PubMed] [Google Scholar]
- 6.Institute of Medicine . The future of public health. Washington, D C: The National Academies Press; 1988. [PubMed] [Google Scholar]
- 7.Institute of Medicine . The future of the public’s health in the 21st century. Washington, D C: The National Academies Press; 2003. [Google Scholar]
- 8.Centers for Disease Control and Prevention The 10 Essential Public Health Services: An Overview. Mar, 2014. http://www.cdc.gov/nphpsp/documents/essential-phs.pdf.
- 9.Kindig D, Gotddary G. What is population health? American Journal of Public Health. 2003;93(3):380–383. doi: 10.2105/ajph.93.3.380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.U.S. Department of Health and Human Services National committee on vital and health statistics. 60th Anniversary symposium and history, 1949–2009; Hyattsville, Maryland. February 2011. [Google Scholar]
- 11.Academic Health Department Learning Community. [Internet]. [cited 2014 January 16] Available from http://www.phf.org/programs/AHDLC/Pages/Academic_Health_Department_Learning_Community.aspx.
- 12.U.S. Department of Health and Human Services . National Committee on Vital and Health Statistics. Hyattsville, Maryland: 2002. Shaping a health statistics vision for the 21st century. [Google Scholar]
- 13.Hodge JG, Gostin LO, Gebbie K, Erickson DL. Transforming public health law: The Turning Point Model State Public Health Act. Journal of Law, Medicine, and Ethics. 2006 Spring;:77–84. doi: 10.1111/j.1748-720X.2006.00010.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Ibid.
- 15.Institute of Medicine . Report brief: Best care at lower cost. Washington, D C: The National Academies Press; 2012. [Google Scholar]
- 16.Association of State and Territorial Health Officers . ASTHO Profile of State Public Health, Volume II. Association of State and Territorial Health Officials; Arlington: 2011. [Google Scholar]
- 17. Hodge Op. Cit. 2006.
- 18. Hodge Op. Cit. 2006.
- 19. Hodge Op. Cit. 2006. [Google Scholar]
- 20.Hodge JG. The evolution of law in biopreparedness. Biosecurity and Bioterrorism. 2012;10(1):38–48. doi: 10.1089/bsp.2011.0094. [DOI] [PubMed] [Google Scholar]
- 21.Meier BM, Merrill J, Gebbie KM. Modernizing state public health enabling statutes to reflect the mission and essential services of public health. J Public Health Management Practice. 2009;15(4):284–291. doi: 10.1097/01.PHH.0000356797.01872.ae. (2009). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. IOM. Op. Cit. 1988.
- 23. IOM. Op. Cit. 2003.
- 24.Meier BM, Merrill J, Gebbie KM. Modernizing state public health enabling statutes to reflect the mission and essential services of public health. J Public Health Management Practice. 2009;15(4):284–291. doi: 10.1097/01.PHH.0000356797.01872.ae. (2009). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. ASTHO Op. Cit. 2011.
- 26. ASTHO Op. Cit. 2011.
- 27.Corso Phaedra, Ingles Justin B, Taylor Nathaniel, Desai Samir. “Linking Costs to Health Outcomes for Allocating Scarce Public Health Resources,”. eGEMs (Generating Evidence & Methods to improve patient outcomes) 2014;2(4) doi: 10.13063/2327-9214.1128. Article 2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. http://www.resolv.org/site-healthleadershipforum/files/2014/05/The-High-Achieving-Governmental-Health-Department-as-the-Chief-Health-Strategist-by-2020-Final1.pdf.
- 30. http://www.sciencedirect.com/science/article/pii/S1570677X13000920.
- 31. ASTHO. Op. Cit. 2011.
- 32.Mays GP, Scutchfield FD, Bhandari MW, Smith MA. Understanding the organization of public health delivery systems: An empirical typology. Milbank. 2010;88(1):81–111. doi: 10.1111/j.1468-0009.2010.00590.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Mays GP, McHugh MC, Shim K, Perry N, Lenaway D, Halverson PK, Moonesinghe R. Institutional and Economic Determinants of Public Health System Performance. Am J Public Health. 2006 Mar;96(3):523–531. doi: 10.2105/AJPH.2005.064253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Robert Wood Johnson Foundation . Common ground: Transforming public health information systems: Final project report. Princeton, NJ: 2012. [Google Scholar]
- 35. Ibid.
- 36.Academic Health Department Learning Community [Internet]. [cited 2014 January 16] Available from http://www.phf.org/programs/AHDLC/Pages/Academic_Health_Department_Learning_Community.aspx.
- 37.National Association of County and City Health Officers [Internet]. [cited 20 January 2014]. The Top Eight Things LHDs Should Know about the HITECH Act. Available from http://www.naccho.org/topics/infrastructure/informatics/resources/upload/top-8-with-NACCHO-letterhead-2.pdf.
- 38.Beacon Nation [Internet}. Hawai’i [cited 2014 February 15] Building Technology Capabilities to Aggregate Clinical Data and Enable Population Health Assessment. ( http://www.hibeacon.org/images/BeaconNation/Beacon_Nation_Learning_Guide_Population_Health_LG6.pdf).
- 39.Beacon Community Program [Internet] Health IT Gov [cited 2014 April 3] Health Adoption Programs ( http://www.health-it.gov/policy-researchers-implementers/beacon-community-program)
- 40.University of Minnesota [Internet] [13 March 2014]. State Health Access Data Assistance Center. Available at http://www.shadac.org.
- 41. Op. Cit. ASTHO 2011.
- 42.Tomines A, Readhead H, Readhead A, Teutsch S. Applications of electronic health information in public health: Uses, opportunities & barriers. eGEMs. 1(2) doi: 10.13063/2327-9214.1019. Article 5: 2013 Available http://repository.academyhealth.org/egems/vol1/iss2/5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. U.S. Department of Health and Human Services [Internet] [15 March 2014]. Preventive Services Taskforce, Agency for Healthcare Research and Quality.
- 44. U.S. Department of Health and Human Services. [Internet] [14 March 2014]. Community Preventive Services Taskforce. Centers for Disease Control. Available at http://www.thecommunityguide.org.
- 45. U.S. Department of Health and Human Services. [Internet]. [13 March 2014] National Quality Strategy. Available at http://www.ahrq.gov/workingforquality/about.htm.
- 46.Institute of Medicine . Toward quality measures for public health. Washington, D.C: The National Academies Press; 2013. [Google Scholar]
- 47.Public Health Forum. [Internet] [15 March 2014] Consensus statement on quality in the public health system:2008. Available at http://www.hhs.gov/ash/initiatives/quality/quality/phqf-consensus-statement.pdf.
- 48. Ibid.
- 49.Institute of Medicine . Toward quality measures for public health. Washington, D.C: The National Academies Press; 2013. [Google Scholar]
- 50.Donabedian A. Evaluating the quality of medical care. Milbank Quarterly. 2005;83(4):691–729. doi: 10.1111/j.1468-0009.2005.00397.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Institute of Medicine . Crossing the quality chasm. Washington, D.C: The National Academies Press; 2001. [Google Scholar]
- 52. IOM Op. Cit. 2013.
- 53.U.S. Department of Health and Human Services . Healthy people 2020. Washington D.C: Office of Disease Prevention and Health Promotion; .[Internet] [cited 212 January 2014] Available at http://www.healthypeople.gov/2020/faqs.aspx. [Google Scholar]
- 54. IOM. Op. Cit. 2013.
- 55.U.S. Department of Health and Human Services National Public Health Improvement Initiative. [Internet]. [cited 14 March 2014] Available at http://www:cdc.gov/stltpublichealth/nphii.
- 56.Edwards D. Alameda County social services integrated reporting system. Alameda County; California: undated. [Google Scholar]
- 57.Institute of Medicine . For the public’s health: The role of measurement in action and accountability. Washington, D C: The National Academies Press; 2011. [PubMed] [Google Scholar]
- 58.U.S. Department of Health and Human Services . National Committee on Vital and Health Statistics. Hyattsville, Maryland: 2002. Shaping a health statistics vision for the 21st century. [Google Scholar]
- 59.U.S. Department of Health and Human Services. [Internet] National Quality Strategy. [13 March 2014] Available at http://www.ahrq.gov/workingforquality/about.htm.