Abstract
Objective
Frequent self-weighing is linked with weight management success but concern has been raised about its possible association with unhealthy practices. We examined the association of self-weighing with other weight control behaviors in a sample for whom frequent weighing might be questioned—namely normal weight or overweight (BMI of 21–29.9) young adults (age 18–35).
Design and Methods
Participants (N=583; mean [SD] age= 27.7 [4.4]; BMI=25.4 [2.6]) entering the Study of Novel Approaches to Weight Gain Prevention (SNAP) completed objective measures of weight and physical activity and self-reported weight history, use of healthy and unhealthy weight control strategies, depressive symptoms, and dietary intake.
Results
Daily self-weighing was reported by 11% of participants and 23% weighed several times per week. Frequent weighing was not associated with current BMI, gender or age, but was associated with being further below one’s highest weight, history of dieting, and perceived difficulty maintaining weight. Frequent weighing was associated with number of healthy weight management strategies but not with unhealthy practices or depressive symptoms.
Conclusions
In this sample, frequent self-weighing appears to be part of a constellation of healthy weight control behaviors used to counteract a perceived tendency toward weight gain. SNAP follow-up will determine whether frequent self-weighing helps prevent weight gain.
Keywords: Self-weighing, Young adults, Weight gain prevention
Frequent self-weighing (daily or weekly) is consistently linked with weight management success but concerns persist about its potential association with unhealthy weight control practices. Although a number of studies have found evidence that frequent self-weighing is associated with better initial weight loss and prevention of weight gain or regain with no deleterious effects,(1–6) its use as a weight management strategy particularly among young adults is still viewed with caution. Whether this caution is justified is an important question that has not been adequately addressed.
Concerns about frequent self-weighing have been primarily raised by those who study normal weight adolescents. Project EAT (7) followed a cohort of middle school and high school students and found that females who reported frequent weighing at baseline, compared to those who did not, were more likely to report binge eating and unhealthy weight control behaviors 5 years later. Frequent self-weighing has also been associated with depression and body dissatisfaction in studies with college age or young adults. (8–10) Conversely, studies of successful weight losers suggest that frequent self-weighing is part of a constellation of healthy weight control behaviors.(11) The National Weight Control Registry, a study of adults who have lost an average of 70 lb and kept it off 6 years, has identified frequent self-weighing as one of the key behaviors associated with initial weight loss success and long-term weight loss maintenance.(12, 13) Other behaviors in this constellation include consuming a low calorie, low fat diet, maintaining high levels of physical activity, regular consumption of breakfast, and exerting conscious control to maintain body weight. (14) Similarly, in adolescents who were successful at weight loss, Alm, et al. (15) found that frequent self-weighers (weekly or more often) reported using more healthy behavioral strategies, including decreasing calories, high fat foods, and junk foods and engaged in more strenuous activity and less video game play than those who weighed less often; they were not more prone to engage in unhealthy weight control behaviors.(16)
To date, little has been published on the frequency of self-weighing in young adults age 18–35 and it is unclear whether frequent self-weighing is part of a constellation of healthy weight control behaviors or a potential marker of other unhealthy and disordered habits. The young adult population is of interest because they are at risk of major weight gain and the behaviors established during this critical developmental period are likely to persist into later adulthood. (17) We therefore determined the self-reported frequency of self-weighing in a cohort of almost 600 young adults at entry into a weight gain prevention study and examined the association of frequent self-weighing with a constellation of both healthy and unhealthy weight control behaviors.
Methods
Participants
We studied the participants in the Study of Novel Approaches to Prevent Weight Gain (SNAP) at trial entry.(18) To be eligible for SNAP, participants had to be between the ages of 18 and 35 and have a BMI between 21 and 30. The target was to recruit 600 participants between two sites (Providence, RI and Chapel Hill, NC), with 25% males and 25% racial or ethnic minorities. Individuals were excluded if they reported bariatric surgery or a recent weight loss of >10 pounds, a health problem that could affect the safety of physical activity or weight loss, a past diagnosis or treatment for anorexia or bulimia nervosa or for alcohol or substance abuse, or a current or recent pregnancy. The full list of inclusion and exclusion criteria has been published previously. (18)
SNAP trial
SNAP is a randomized clinical trial examining two novel approaches to weight gain prevention in young adults compared to a minimal treatment control. The interventions are based on self-regulation and focus on either small consistent changes in eating and exercise or larger, periodic changes to buffer against expected weight gains. All measures reported in this paper were collected prior to randomization, either during two screening visits which were conducted within 1 to 2 weeks of each other.
Assessments
All measures were completed online via a secure server between these two visits, except for the measures of weight and height, depression and physical activity (which are described below),
Self-weighing frequency
Participants were asked to report how frequently they weighed themselves over the prior 4 months. Choices included never, <1 /month, <1/week, once/week, several times/week, once a day and several times per day. We grouped together those reporting never (N=74) or <1 month (N=85). Since only 15 participants (2.5%) reported weighing more than once daily, this small group was excluded from the analyses. In addition, one participant did not provide a response to this question.
Demographic and weight history questionnaire
Participants were asked to provide basic demographic information and to answer several questions about their weight history, including information about their highest weight ever and the degree of effort required to maintain their weight.
Restraint and disinhibition
All participants completed the Restraint and Disinhibition subscales of The Eating Inventory (TFEQ), assessing the degree of conscious control over eating behaviors and the susceptibility to loss of control over eating, respectively.(19) In addition we included the items suggested by Westenhoefer et al. (20) to assess rigid and flexible control of eating behavior. In their validation study of these concepts, the authors noted that rigid control was associated with higher scores on disinhibition, higher BMI, and more frequent binge eating episodes. Flexible restraint was associated in the opposite direction with each of these variables and with weight loss success over a yearlong weight loss program. In addition the Rigid and Flexible control scores are related to each other, with a correlation of .77 reported in a study of 639 college students. (21)
Weight Management Strategies
SNAP assessed the frequency with which participants reported each of 45 weight management strategies. The items were derived primarily from an earlier weight gain prevention trial,(22) with additional items reflecting the small or large change strategies that would be taught later in the SNAP trial and were used in a pilot study in preparation for SNAP.(23) Participants reported the frequency of use of 45 strategies over the prior 4 months using the following 5 categories: Never or Hardly Ever, Some of the Time, About Half of the Time, Much of the Time, or Always or Almost Always. To address use of unhealthy weight control strategies, participants completed a questionnaire used in Look AHEAD (24) (an adapted version of the Questionnaire on Eating and Weight Patterns – Revised(25)) that assesses the frequency of binge eating episodes accompanied by loss of control and the frequency of compensatory behaviors.
Dietary Intake
The Block Food Frequency, a semi-quantitative food frequency questionnaire that has been used in a number of weight loss trials, was completed by participants online.(26) Participants also reported on other eating behaviors, including their frequency of meals and snacks and eating at fast food restaurants as part of a battery developed for the EARLY trials.(27)
Weight/height
Weight was measured at the clinic at Screening Visit 1 with participants in light clothes, without shoes, on a calibrated scale; height was determined using a wall-mounted stadiometer. These measures were used to compute body mass index (BMI; kg/m2).
Physical Activity
All participants wore the SenseWear armband (Body Media, Pittsburgh, Pa) for a week between Screening visits 1 and 2 to provide an objective assessment of physical activity.(28) They completed the Paffenbarger Activity Questionnaire,(29) which was administered by interview at Screening Visit 2.
Depression
The Center for Epidemiologic Studies Depression Scale (CES-D) was completed in the clinic at Screening Visit 1 and used to assess depressive symptoms.(30) Higher scores on this scale reflect greater depressive symptomatology.
Statistical Analyses
Analyses compared the 5 self-weighing categories using logistic regression for categorical variables and linear regression for continuous variables. When significant differences were observed among the 5 groups, trend tests were conducted. Interactions between BMI category (normal weight/overweight) and self-weighing frequency were also conducted to determine whether the relationship between frequency of self-weighing and healthy/unhealthy weight strategies differed across BMI categories.
Results
A total of 583 participants (97.3% of the full cohort) were included in our analyses (457 females; 126 males), including 300 recruited in Chapel Hill, NC and 283 in Providence, RI. On average (SD) participants were 27.7 (4.4) years of age, and weighed 71.3 (10.7 kg) with a BMI of 25.4 (2.6). Approximately half were normal weight (BMI of 21–25) and the others were overweight (BMI of 25–30). Twenty three percent were from ethnic/racial minority groups.
Table 1 shows the number and percent of participants who reported each category of self-weighing frequency. As shown in Table 1, 27% reported weighing themselves never or less than once a month, whereas 11% reported weighing themselves once a day, and an additional 23% weighed themselves several times per week (34% weighed at least several times per week). Demographic characteristics, including gender, age, BMI, ethnicity and proportion of students (vs employed), did not differ across self-weighing categories. However, those who weighed themselves more frequently reported a larger difference between their current weight and their highest weight ever (p=.04),with those who weighed daily reporting that they were currently 13.5 pounds below their highest weight and those weighing never or <1 month were 9.2 pounds below their highest weight. Frequent weighers were also more likely to report having tried previously to lose weight. Whereas 89.1% of those who weighed daily had tried previously to lose weight, only 73.4% of those who weighed never or <1 month and 72.2% of those who weighed <1 week had previously tried to lose weight (p<0.001).
Table 1.
Demographic characteristics and weight history of participants according to their self-weighing frequency: Mean (SD) or N (%)
| Self-weighing frequency | ||||||
|---|---|---|---|---|---|---|
| Never or < 1/mo |
< 1/week | Once/week | Several /week | Once/day | P-value | |
| Number of subjects | 159 (27.2%) | 122 (20.9%) | 105 (18.0%) | 133 (22.8%) | 64 (11.0%) | |
| Gender (% Female) | 125 (78.6%) | 97 (79.5%) | 84 (80.0%) | 105 (79.0%) | 46 (71.9%) | 0.76 |
| Age | 27.5 (4.6) | 27.3 (4.5) | 27.4 (4.0) | 28.1 (4.1) | 28.8 (4.8) | 0.12 |
| BMI | 25.4 (2.5) | 25.2 (2.6) | 25.3 (2.7) | 25.5 (2.6) | 25.9 (2.4) | 0.52 |
| Ethnicity (%) | ||||||
| African American | 25 (%) | 11 (9.0%) | 10 (9.5%) | 21 (15.8%) | 9 (14.1%) | |
| White | 113 (71.1%) | 102 (83.6%) | 83 (79.0%) | 102 (76.7%) | 49 (76.6%) | 0.32 |
| Other | 21 (13.2%) | 9 (7.4%) | 12 (11.4%) | 10 (7.5%) | 6 (9.4%) | |
| Current student (%) | 48 (30.2%) | 30(34.6%) | 27 (25.7%) | 29 (21.8%) | 13 (20.3%) | 0.44 |
| Difference (lbs) between highest and current weight | 9.2 (0.9) | 10.3 (1.1) | 9.1 (1.2) | 12.1 (1.0) | 13.5 (1.5) | 0.04 |
| Previously tried to lose weight (%) | 117 (73.4%) | 88 (72.2%) | 93 (88.5%) | 118 (88.6%) | 57 (89.1%) | <0.001 |
Restraint and Disinhibition
Self-weighing groups differed on several measures of dietary restraint and on disinhibition and the trend analysis for each of these measures was significant (Table 2). Scores on the rigid and flexible restraint scales were correlated with each other (r=.43, p<.001), and those who weighed frequently reported higher scores on both the scales than those who weighed less often. The groups also differed on disinhibition but the only pairwise significant differences were between those who weighed less than once a week and those who weighed either once/week or several times per week. The interactions between BMI and self-weighing frequency were not significant for any of the restraint or disinhibition scales.
Table 2.
Restraint and disinhibition scores [mean (SE)] by self-weighing frequency with adjustment for gender, age, baseline BMI, and clinic site. Shared superscripts are used to denote pairwise group differences that are not statistically significant (p>0.05) based on a Scheffe multiple comparisons test.
| Self-weighing frequency | ||||||
|---|---|---|---|---|---|---|
| Never or < 1/mo | < 1/week | Once/week | Several /week | Once/day | P-value1 | |
| Restraint | 10.39 (0.15)a,b | 10.18 (0.17)a | 10.49 (0.18)a,b | 10.54 (0.16)a,b | 11.20 (0.24)b | 0.049 |
| Disinhibition | 9.02 (0.19)a,b | 8.78 (0.22)a | 9.79 (0.24)b | 9.74 (0.21)b | 9.33 (0.30)a,b | 0.003 |
| Flexible Control | 6.06 (0.18)a | 6.02 (0.21)a | 6.58 (0.22)a,b | 6.85 (0.20)a,b | 7.48 (0.28)b | <0.001 |
| Rigid Control | 6.09 (0.22)a | 6.40 (0.26)a,b | 7.51 (0.27)b,c | 7.53 (0.24)c | 8.44 (0.35),c | <0.001 |
test for trend from logistic regression was significant for all variables
Pairwise comparisons of categories of self-weighing (e.g. 1 = Never or < 1/mo and 5 = Once/day) (Scheffe method: p<0.05):
Restraint: 2 vs 5
Disinhibition: 2 vs 3 and 2 vs 4
Flexible Control: 1 vs 5; 2 vs 5
Rigid Control: 1 vs 3, 4, and 5; 2 vs 4,5
Depressive symptoms, Eating Disorder Assessment, and Attention to weight and shape
The self-weighing groups did not differ significantly on CES-D scores (with mean scores for all groups below 4.5). Similarly there were no significant differences between self-weighing groups in the proportion who reported episodes of binge eating or use of any compensatory behaviors; of note, the number of participants reporting these behaviors was very low across all groups. For example, 5 (3%) participants in the lowest self-weighing group and 3 (4.6%) of those who weighed daily reported having more than one binge eating episode per week (described as eating a large amount within short time and feeling a loss of control). Vomiting to lose weight was reported by 2 individuals in the lowest self-weighing category and 1 in the most frequent self-weighing group.
The EDA also asked about how much weight and shape mattered to the individual. The proportion of individuals who reported that weight and shape were “pretty” or “very” important to how the person felt about themselves increased from 49% in those who weighed never or less than once a month to 55% in those who weighed <1 week, 61% in those who weighed once per week and 67% in both those who weighed several times per week or once per day (p=.01). This finding was confirmed by other questionnaire items showing that those who weighed more frequently reported higher scores on the amount of effort required to maintain their weight, on the importance of maintaining their weight and on the amount of time they spent thinking about controlling weight (Table 4).
Table 4.
Self-reported effort to maintain current weight [mean (SE)] with adjustment for age, BMI, sex and clinic. Shared superscripts are used to denote pairwise group differences that are not statistically significant (p>0.05) based on a Scheffe multiple comparisons test.
| Never or <1/month (N=159) |
<1/week (N=122) |
Once/week (N=105) |
Several times/week (N=133) |
1+/day (N=64) | P-value | |
|---|---|---|---|---|---|---|
| Effort to Maintain Weight | 4.69 (0.12)a,b | 4.51 (0.14)a | 4.77 (0.15)a,b | 4.98 (0.13)b | 5.25 (0.19)a,b | 0.02 |
| Importance of Maintaining Weight | 6.65 (0.10)a | 6.81 (0.11)a,b | 7.15 (0.12)b | 7.21 (0.11)b | 7.23 (0.16)b | <0.001 |
| How Easy to Control your Weight | 4.57 (0.11)a | 4.61 (0.13)a | 4.67 (0.14)a | 4.90 (0.12)a | 5.18 (0.18)a | 0.03 |
| How often do you think about controlling your weight | 5.54 (0.14)a | 5.66 (0.16)a,b | 6.08 (0.17)a,b,c | 6.35 (0.15)c | 6.65 (0.22)c | <0.001 |
Pairwise comparisons of categories of self-weighing (e.g. 1 = Never or < 1/mo and 5 = Once/day) (Scheffe method: p<0.05):
Effort maintaining: 2 vs 4
Importance of maintaining: 1 vs 2,3,4
Frequency of thinking about controlling weight: 1 vs 4 ,5; 2 vs 4, 5
Weight Management Strategies
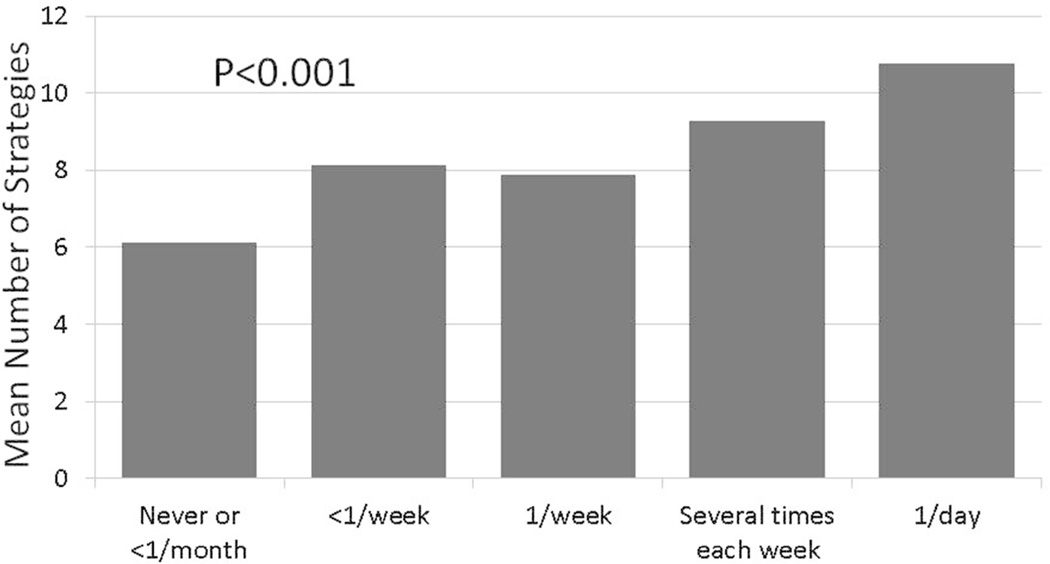
In keeping with the perceived effort required to maintain weight, there were marked differences in the number of weight management strategies endorsed by each self-weighing group. We compared the number of strategies that participants in each self-weighing category reported using “always or almost” or “much of the time”. Figure 1 shows that those who reported weighing most frequently used nearly twice as many strategies as those who weighed <1 per month. The interaction between BMI and self-weighing categories was not significant. Chi square analyses examined the proportion of participants in each self-weighing category who reported that they had used a specific weight management strategy “much of the time” or “always or almost always” over the past 4 months to manage their weight. Table 3 shows only those strategies where use differed (i.e. nominal p<0.05) across the self-weighing categories, and where the greatest use was in the daily weighing category. As expected participants who reported weighing daily on the self-weighing questionnaire also reported that they used daily weighing as a specific weight control strategy on the Weight Management Strategies Questionnaire; in addition, they were more likely to report recording their weight. Daily self-weighers also were more likely to use some strategies that were endorsed commonly by a relatively large percentage of the SNAP participants, such as decreasing desserts, decreasing junk foods, and reducing portion sizes. Likewise, they endorsed greater use of other strategies that were used relatively infrequently, such as using home exercise equipment, following a structured meal plan and reducing intake by 500–1000 kcal /day. Only one item on this questionnaire asked about an unhealthy strategy (skipping meals) as a strategy for weight management. This strategy was used by 2.5% of those who reported never weighing and 3.1% of those who weighed daily, with a non-significant chi-square across the 5 self-weighing categories. (p>.10).
Figure 1.
Mean number of strategies used much, almost all, or all of the time by participants in each self-weighing category report, with adjustment for gender, age, body mass index, and clinic site
Table 3.
Percent of participants using strategy much or all of the time
| Self-weighing frequency | ||||||
|---|---|---|---|---|---|---|
| Never or < 1/mo | < 1/week | Once/week | Several /week | Once/day | P-value1 | |
| Weigh daily | 0 | 1.6 | 0.95 | 34.6 | 85.9 | <0.0001 |
| Decrease dessert | 24.5 | 28.7 | 38.1 | 36.1 | 43.8 | 0.02 |
| Reduce junk food | 21.4 | 36.1 | 35.2 | 30.1 | 39.1 | 0.02 |
| Reduce portion size | 15.1 | 18.8 | 14.3 | 26.3 | 28.1 | 0.03 |
| Record weight | 1.9 | 4.1 | 7.6 | 11.3 | 26.6 | <0.0001 |
| Use home exercise equip | 5.7 | 8.2 | 3.8 | 10.5 | 15.6 | 0.04 |
| Make small dietary changes | 4.4 | 12.3 | 5.7 | 11.3 | 14.1 | 0.04 |
| Follow structured meal plan | 3.8 | 4.9 | 1.9 | 6.0 | 12.5 | 0.04 |
| Reduce intake by 500–1000/day | 1.9 | 5.7 | 1.9 | 8.3 | 9.4 | 0.03 |
test for trend from logistic regression was significant for all strategies, except make small dietary changes where p=0.08.
Eating and Physical Activity
Although those who weighed daily reported using more weight management strategies, there was no association between frequency of self-weighing and total number of calories consumed (ranging from 1598 to 1744 across the 5 self-weighing categories) or percent of calories from fat (ranging from 34.5–35.5 across the categories). Fast foods were consumed 1.5 times per week on average, again with no difference between groups. However, eating 5+meals/snacks per day was reported by 66% of those who reported weighing themselves daily, decreasing by frequency of self-weighing to 54%, 47% and 49% and 42% in those who weighed several times per week, weekly, less than once per week, and less than once a month, respectively. This difference resulted in part from a non-significant tendency for a greater proportion of those who weighed most often to eat breakfast every day (55% vs 45% of those weighing less than once a month) and a significant difference for eating lunch every day (80% vs 58.5%, p=.04). There was also no association between frequency of self-weighing and physical activity as reported on the Paffenbarger Questionnaire or the amount of time spent in sedentary or moderate-vigorous activity as measured objectively by the armband.
Discussion
To date there have been few studies of self-weighing frequency in young adults and it is not known whether this behavior is part of a constellation of healthy weight management behaviors or conversely, is associated with disordered eating behaviors. SNAP provided a unique cohort to address this question because all participants in the trial were young adults who had expressed interest in trying to prevent weight gain and approximately half of the participants were normal weight. We found that 11% of our participants weighed themselves daily, and over one-third of the participants self-weighed at least several times a week. Frequent self-weighing was not associated with current BMI but it was associated with being further below one’s highest ever weight and with greater importance of maintaining one’s weight, greater perceived effort involved in managing one’s weight, and greater use of healthy weight control strategies. Importantly, frequent self-weighing was not associated with greater use of unhealthy weight control practices or disordered eating behaviors, and findings did not appear to vary as a function of BMI status. Thus, our data suggest that self-weighing is an important aspect of a healthy and vigilant approach used to counteract a perceived tendency toward weight gain.
The prevalence of frequent self-weighing in SNAP exceeds that usually reported with young adults. For example in a study of 268 undergraduates,(31) 2 reported weighing several times a day, 12 reported weighing once a day, and 37 weighed several times per week (omitting those who weighed several times a day, 18% of the participants weighed several times per week or more). In the EAT-III follow-up (conducted when the study group had a mean age of 25), 18% of women and 12% of the men reported self-weighing a few times per week or more.(10) The higher frequency of self-weighing in this study relative to other reports may reflect the fact that participants in the present study were all choosing to enter a trial to help them prevent gaining weight and thus may have been more concerned about future weight gain than the general population of young adults.
There have been a number of recent randomized trials using frequent self-weighing as part of interventions to produce weight loss(5, 23, 32)or to prevent weight gain, (6) or weight regain.(1) Although the effect of self-weighing cannot always be examined independent of other aspects of the self-regulation intervention, these studies have shown positive effects on weight change, with little evidence of untoward reactions.(33, 34) Moreover, a meta-analysis of this literature supports the beneficial effects of frequent weighing.(35)
Although we found no evidence that frequency of self-weighing was associated with a lower BMI, frequent self-weighing was associated with maintaining a current weight that is below the individuals’ highest weight ever, with greater importance and difficulty of maintaining current weight and with greater use of weight control strategies. While frequent self-weighers reported working harder to maintain their weight, they did not differ from others in self-reported caloric intake or activity or objectively measured physical activity. What appeared to differ was the perceived effort that was required to maintain this level of caloric intake. Despite similar caloric intake, those who weighed daily more frequently endorsed strategies such as making small changes to diet each day, leaving a few bites of food on the plate and following a structured meal plan. Similarly, while objective activity levels did not differ, those who weighed more often also reported using home exercise equipment more, and using stairs instead of elevators. Thus, it appears that the frequency of self-weighing reflects success at maintaining a body weight that is, perhaps, lower than their biological set-point. There was no evidence that frequency of self-weighing was associated with depression or eating disordered behaviors and thus these efforts do not appear to be having significant negative effects.
Participants who reported frequent self-weighing reported higher levels of both flexible and rigid restraint compared to those who weighed less often. These two constructs, measured with items from the original Three Factor Eating Questionnaire restraint scale combined with other additional items, were developed to distinguish between rigid control which is characterized by dichotomous thinking and an all-or-nothing approach and flexible control which is characterized by a more graduated approach (e.g. where fattening foods can be eaten in limited quantities without guilt.) However, in validation studies, a high correlation between the two has been noted and the two scores were also significantly related to each other in the present sample. Thus, self-weighing was associated with greater cognitive control over eating, including both rigid and flexible control. We also observed a significant association between self-weighing frequency and disinhibition. However, pair-wise comparisons indicated that the levels of disinhibition only differed between those who weighed less than once a week versus those who weighed once or several times a week. The level of disinhibition in those who weighed daily did not differ significantly from that seen in any of the other self-weighing categories. We also found no significant interactions between self-weighing frequency and BMI category (overweight or normal weight) on these measures of restraint or disinhibition, suggesting that the association of weighing frequency and restraint/disinhibition did not differ in those who were overweight compared to those who were normal weight.
The study has several strengths and limitations that should be noted. The strengths include a large sample of healthy young adults, equal proportions of overweight and normal weight individuals, objectively measured height and weight, and a large battery of measures to understand both behavioral and psychological associations with frequent weighing. The primary limitations of the study are the cross-sectional design and the characteristics of the study sample. Our participants included a limited number of men and racial / ethnic minorities and all were between age 18 and 35; we excluded individuals who reported prior treatment for or current experience of an eating disorder, but only 2 individuals were screened out due to this eligibility criterion. Given the cross-sectional design, we cannot assess the effects of increases or decreases in weighing frequency. The SNAP study will continue to follow these participants over time and we will thus be able to examine prospectively whether changes in the frequency of weighing are associated with changes in other weight-related behaviors, psychological outcomes, and future weight change trajectories.
In conclusion, we find that in the absence of a weight-focused intervention frequent self-weighing is part of a cluster of behaviors that suggest the person is working harder to maintain the same body weight as those who weigh less often. However, daily self-weighing does not seem to be associated with greater psychological distress or unhealthy eating behaviors. An important question to be addressed in future work is whether this frequent self-weighing and increased effort to maintain body weight is successful in decreasing the risk of future weight gain.
What is already known about this subject
Frequent self-weighing is associated with better outcomes in weight loss programs and with success at weight loss maintenance.
Frequent self-weighing is of concern in certain populations, such as normal weight adolescents, because of its association with unhealthy weight control practices.
What this study adds
This study provides novel data on frequent self-weighing in normal weight and overweight young adults who were entering a weight gain prevention trial and its association with healthy and unhealthy weight control behaviors
We show that frequent self-weighing was not associated with current BMI but was associated with being further below one’s highest prior weight, reported difficulty in maintaining weight, and use of healthy weight control strategies. Frequent self-weighing was not associated with depressive symptoms or binge eating.
Acknowledgments
NIH Grant Number: 5U01 HL090864
Footnotes
ClinicalTrials.gov Identifier: NCT 01183689
Contributor Information
Deborah Tate, Email: dtate@unc.edu.
Jessica Gokee LaRose, Email: jlarose@vcu.edu.
Amy A. Gorin, Email: amy.gorin@uconn.edu.
Karen Erickson, Email: keericks@email.unc.edu.
Erica Ferguson Robichaud, Email: eferguson@lifespan.org.
Letitia Perdue, Email: lperdue@wakehealth.edu.
Judy Bahnson, Email: jbahnson@wakehealth.edu.
Mark A. Espeland, Email: mespelan@wakehealth.edu.
References
- 1.Wing RR, Tate DF, Gorin AA, Raynor HA, Fava JL. A self-regulation program for maintenance of weight loss. N Engl J Med. 2006;355(15):1563–1571. doi: 10.1056/NEJMoa061883. [DOI] [PubMed] [Google Scholar]
- 2.Wing RR, Tate DF, Gorin AA, Raynor HA, Fava JL, Machan J. "STOP regain": Are there negative effects of daily weighing? J Consult Clin Psychol. 2007;75(4):652–656. doi: 10.1037/0022-006X.75.4.652. [DOI] [PubMed] [Google Scholar]
- 3.Jeffery RW, Bjornson-Benson WM, Rosenthal BS, Lindquist RA, Kurth CL, Johnson SL. Correlates of weight loss and its maintenance over two years of follow-up among middle-aged men. Preventive Medicine. 1984;13:155–168. doi: 10.1016/0091-7435(84)90048-3. [DOI] [PubMed] [Google Scholar]
- 4.Linde JA, Jeffery RW, French SA, Pronk NP, Boyle RG. Self-weighing in weight gain prevention and weight loss trials. Annals of Behavioral Medicine. 2005;30(3):210–216. doi: 10.1207/s15324796abm3003_5. [DOI] [PubMed] [Google Scholar]
- 5.Gokee-Larose J, Gorin AA, Wing RR. Behavioral self-regulation for weight loss in young adults: a randomized controlled trial. Int J Behav Nutr Phys Act. 2009;6:10. doi: 10.1186/1479-5868-6-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Levitsky DA, Garay J, Nausbaum M, Neighbors L, Dellavalle DM. Monitoring weight daily blocks the freshman weight gain: a model for combating the epidemic of obesity. Int J Obes (Lond) 2006;30(6):1003–1010. doi: 10.1038/sj.ijo.0803221. [DOI] [PubMed] [Google Scholar]
- 7.Neumark-Sztainer D, van den Berg P, Hannan PJ, Story M. Self-weighing in adolescents: helpful or harmful? Longitudinal associations with body weight changes and disordered eating. J Adolesc Health. 2006;39(6):811–818. doi: 10.1016/j.jadohealth.2006.07.002. [DOI] [PubMed] [Google Scholar]
- 8.Ogden J, Whyman C. The effects of repeated weighing on psychological state. Eur Eating Dis Rev. 1997;5:121–130. [Google Scholar]
- 9.Mecurio A, Rima B. Watching my weight: Self-weighing, body surveillance, and body dissatisfaction. Sex Roles. 2011;65:47–55. [Google Scholar]
- 10.Quick V, Larson N, Eisenberg ME, Hannan PJ, Neumark-Sztainer D. Self-weighing behaviors in young adults: tipping the scale toward unhealthy eating behaviors? J Adolesc Health. 2012;51(5):468–474. doi: 10.1016/j.jadohealth.2012.02.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.McGuire M, Wing R, Hill J. The prevalence of weight loss maintenance among American adults. International Journal of Obesity. 1999;23:1314–1319. doi: 10.1038/sj.ijo.0801075. [DOI] [PubMed] [Google Scholar]
- 12.Butryn ML, Phelan S, Hill JO, Wing RR. Consistent self-monitoring of weight: a key component of successful weight loss maintenance. Obesity (Silver Spring) 2007;15(12):3091–3096. doi: 10.1038/oby.2007.368. [DOI] [PubMed] [Google Scholar]
- 13.Thomas JG, Bond DS, Phelan S, Hill JO, Wing RR. Weight-loss maintenance for 10 years in the National Weight Control Registry. Am J Prev Med. 2014;46(1):17–23. doi: 10.1016/j.amepre.2013.08.019. [DOI] [PubMed] [Google Scholar]
- 14.Wing R, Phelan S. Long-term weight loss maintainence. American Journal of Clinical Nutrition. 2005;82(1 Suppl):222S–225S. doi: 10.1093/ajcn/82.1.222S. [DOI] [PubMed] [Google Scholar]
- 15.Alm ME, Neumark-Sztainer D, Story M, Boutelle KN. Self-weighing and weight control behaviors among adolescents with a history of overweight. J Adolesc Health. 2009;44(5):424–430. doi: 10.1016/j.jadohealth.2008.08.016. [DOI] [PubMed] [Google Scholar]
- 16.Boutelle KN, Libbey H, Neumark-Sztainer D, Story M. Weight control strategies of overweight adolescents who successfully lost weight. J Am Diet Assoc. 2009;109(12):2029–2035. doi: 10.1016/j.jada.2009.09.012. [DOI] [PubMed] [Google Scholar]
- 17.Nelson MC, Story M, Larson NI, Neumark-Sztainer D, Lytle LA. Emerging adulthood and college-aged youth: an overlooked age for weight-related behavior change. Obesity (Silver Spring) 2008;16(10):2205–2211. doi: 10.1038/oby.2008.365. [DOI] [PubMed] [Google Scholar]
- 18.Wing RR, Tate D, Espeland M, Gorin A, Larose J, Ferguson Robichaud E, et al. Weight gain prevention in young adults: design of the study of novel approaches to weight gain prevention (SNAP) randomized controlled trial. BMC Public Health. 2013;13(1):300. doi: 10.1186/1471-2458-13-300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Stunkard AJ, Messick S. Eating Inventory Manual. New York: Psychological Corporation; 1988. [Google Scholar]
- 20.Westenhoefer J, Stunkard AJ, Pudel V. Validation of the Flexible and Rigid Control dimensions of dietary restraint. International Journal of Eating Disorders. 1999;26:53–64. doi: 10.1002/(sici)1098-108x(199907)26:1<53::aid-eat7>3.0.co;2-n. [DOI] [PubMed] [Google Scholar]
- 21.Timko CA, Perone J. Rigid and flexible control of eating behavior in a college population. Eat Behav. 2005;6(2):119–125. doi: 10.1016/j.eatbeh.2004.09.002. [DOI] [PubMed] [Google Scholar]
- 22.Jeffery R, French S. Preventing weight gain in adults: the pound of prevention study. American Journal of Public Health. 1999;89(5):747–751. doi: 10.2105/ajph.89.5.747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Gokee LaRose J, Tate DF, Gorin AA, Wing RR. Preventing weight gain in young adults: a randomized controlled pilot study. Am J Prev Med. 2010;39(1):63–68. doi: 10.1016/j.amepre.2010.03.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Look AHEAD Research Group. Look AHEAD: Action for Health in Diabetes: Design and methods for a clinical trial of weight loss for the prevention of cardiovascular disease in type 2 diabetes. Controlled Clinical Trials. 2003;24:610–628. doi: 10.1016/s0197-2456(03)00064-3. [DOI] [PubMed] [Google Scholar]
- 25.Spitzer RL, Yanovski JA, Marcus MD. The questionnaire on eating and weight patterns-revised (QEPD-R) 1993. [Google Scholar]
- 26.Block G, Hartman AM, Dresser CM, Carroll MD, Gannon J, Gardner L. A data-based approach to diet questionnaire design and testing. American Journal of Epidemiology. 1986;124:453–469. doi: 10.1093/oxfordjournals.aje.a114416. [DOI] [PubMed] [Google Scholar]
- 27.Lytle LA, Svetkey LP, Patrick K, Belle SH, Fernandez ID, Jakicic JM, et al. The EARLY trials: a consortium of studies targeting weight control in young adults. Transl Behav Med. 2014;4(3):304–313. doi: 10.1007/s13142-014-0252-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Jakicic JM, Marcus M, Gallagher KI, Randall C, Thomas E, Goss FL, et al. Evaluation of the SenseWear Pro Armband to assess energy expenditure during exercise. Med Sci Sports Exerc. 2004;36(5):897–904. doi: 10.1249/01.mss.0000126805.32659.43. [DOI] [PubMed] [Google Scholar]
- 29.Paffenbarger RS, Wing AL, Hyde RT. Physical activity as an index of heart attack risk in college alumni. American Journal of Epidemiology. 1978;108:161–175. doi: 10.1093/oxfordjournals.aje.a112608. [DOI] [PubMed] [Google Scholar]
- 30.Turvey CL, Wallace RB, Herzog R. A revised CES-D measure of depressive symptoms and a DSM-based measure of major depressive episodes in the elderly. Int Psychogeriatr. 1999;11(2):139–148. doi: 10.1017/s1041610299005694. [DOI] [PubMed] [Google Scholar]
- 31.Klos LA, Esser VE, Kessler MM. To weigh or not to weigh: the relationship between self-weighing behavior and body image among adults. Body Image. 2012;9(4):551–554. doi: 10.1016/j.bodyim.2012.07.004. [DOI] [PubMed] [Google Scholar]
- 32.Steinberg DM, Tate DF, Bennett GG, Ennett S, Samuel-Hodge C, Ward DS. The efficacy of a daily self-weighing weight loss intervention using smart scales and e-mail. Obesity (Silver Spring) 2013;21(9):1789–1797. doi: 10.1002/oby.20396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Steinberg DM, Tate DF, Bennett GG, Ennett S, Samuel-Hodge C, Ward DS. Daily self-weighing and adverse psychological outcomes: a randomized controlled trial. Am J Prev Med. 2014;46(1):24–29. doi: 10.1016/j.amepre.2013.08.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.LaRose JG, Fava JL, Steeves EA, Hecht J, Wing RR, Raynor HA. Daily self-weighing within a lifestyle intervention: impact on disordered eating symptoms. Health Psychol. 2014;33(3):297–300. doi: 10.1037/a0034218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Vanwormer JJ, French SA, Pereira MA, Welsh EM. The impact of regular self-weighing on weight management: a systematic literature review. Int J Behav Nutr Phys Act. 2008;5:54. doi: 10.1186/1479-5868-5-54. [DOI] [PMC free article] [PubMed] [Google Scholar]