Introduction
Infection has been well documented to cause glomerulonephritis (GN), with Streptococcus being the most common pathogen. However, the pattern of the disease has changed over recent decades [1–3]. The bacterial flora now comprises Staphylococcus and Gram-negative strains, and the focus of infection is wider than the throat and the skin [1]. GN secondary to osteomyelitis has rarely been reported.
We report a case of immune complex-mediated diffuse proliferative GN with acute on chronic renal failure, superimposed on diabetic nephropathy due to osteomyelitis caused by Enterobacter cloacae.
Case report
A 42-year-old woman with diabetes mellitus for 12 years, hypertensive for 6 years, hypothyroidism on treatment, with diabetic nephropathy and a baseline serum creatinine of 141.4 µmol/L (2.5 mg/dL) presented with a non-healing chronic trophic ulcer of the right sole. Blood pressure was 160/95 mmHg. There was a 5 × 5-cm ulcer over the sole of her right foot with bilateral deep pedal oedema and peripheral neuropathy. She had diabetic retinopathy. Renal ultrasonography showed normal-sized kidneys.
Blood count showed a white blood cell (WBC) of 11.8 × 109/L, neutrophils 86.3%, lymphocytes 7.6%, monocytes 3.9%, eosinophils 2.1%, basophils 0.1% and platelets 175 × 109/L. Blood chemistry showed blood urea nitrogen of 23 mmol/L, serum creatinine 221 µmol/L (2.5 mg/dL), sodium 140 mmol/L, potassium 5.8 mmol/L, bicarbonate 20 mmol/L, HbA1c 5.3%, serum total protein 67 g/L (6.7 g/dL) and serum albumin 24 g/L (2.4 g/dL).
Urinalysis revealed protein ++, with numerous red blood cells and 3–5 WBCs/high-power field in the urinary sediment. Twenty-four-hour urinary protein was 7.25 g. Blood and urine cultures were negative. Serum complement C3 was 1.06 (0.9–1.8) g/L, and C4 0.30 (0.16–0.38) g/L. Echocardiography showed concentric left ventricular hypertrophy and good biventricular function with no vegetation. Free T4 was 16.4 pmol/L and thyroid stimulating harmone was 3.86 mU/L.
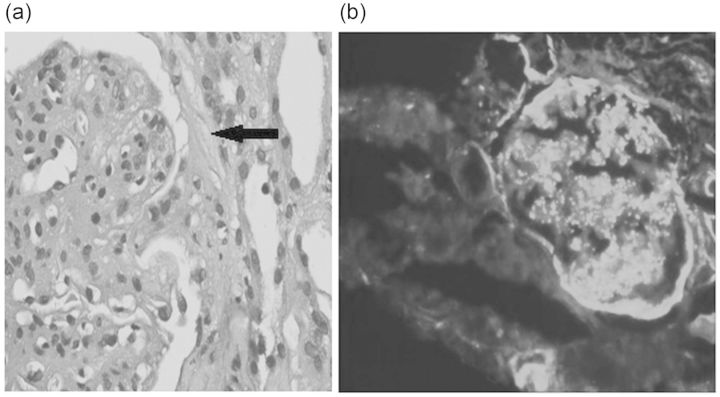
She was commenced on haemodialysis for progressively worsening renal function. A kidney biopsy yielded 17 glomeruli; 10 were globally sclerotic. Diffuse endocapillary proliferation and mesangial expansion were seen in all glomeruli. Crescent formation was noted in two glomeruli (Figure 1a).
Fig. 1.
(a) Kidney biopsy—endocapillary proliferative GN with cellular crescents (arrow). (b) Immunofluorescence showing C3(+3).
Immunofluorescence revealed IgM (+1), C3 (+3) and IgA (+1), which gave a coarse granular positivity over the capillary walls and mesangium. Antisera for IgG and C1q were negative (Figure 1b). Post-infectious GN (PIGN) superimposed on diabetic nephropathy.
Tc-99m methylene diphosphonate bone scan showed active inflammation in the tarsal bones of the left foot, left ankle joints, metatarsophalangeal joints of the right foot and in the tarsal bones of the right foot (Figure 2). One hundred and twenty-eight-slice positron emission tomography – computed tomography (PET/CT) scan showed erosions and sclerosis at the right calcaneum associated with soft tissue collection and defect with subcutaneous inflammatory fatty changes of osteomyelitis (Figure 3). Right leg arterial Doppler was normal.
Fig. 2.
Tc-99m methylene diphosphonate bone scan showing active inflammation of metatarsophalangeal joints of the right foot and in the tarsal bones of the right foot (arrow).
Fig. 3.
One hundred and twenty-eight-slice positron emission tomography – computed tomography (PET/CT) scan showing erosions and sclerosis at the right calcaneum ( ) associated with soft tissue collection and defect with subcutaneous inflammatory fat changes (
) associated with soft tissue collection and defect with subcutaneous inflammatory fat changes ( ).
).
Culture of the ulcer pus grew E. cloacae, which was treated with levofloxacin 500 mg for 24 days and antibiotic impregnated dressing. The patient did not recover renal function and continues on thrice weekly dialysis 5 months after the kidney biopsy. The ulcer is resolving and is scheduled for a skin graft.
Discussion
GN related to osteomyelitis is rare [2] and Staphylococcus aureus is the most common causative organism [1, 3]. Our patient had an E. cloacae osteomyelitis causing crescenteric GN.
Unlike previous reports of PIGN with acute kidney injury associated with osteomyelitis in which there was an improvement in renal function with treatment of the infected bone [2], our patient had rapidly progressing renal failure despite adequate systemic antibiotics and remained dialysis dependent.
Hypocomplementaemia is not always a ‘sine qua non’ feature of PIGN [1, 4] as seen in our case.
The most common histologic lesion in PIGN is diffuse endocapillary proliferative GN, sometimes with membranoproliferative features [3]. Glomerular deposits consist mainly of IgG and C3. Our patient had endocapillary proliferative GN, IgA on immunofluorescence and cellular crescents consistent with PIGN on a background of diabetic nephropathy. Nasr et al. [5] reported a novel immunopathological phenotype of IgA-dominant acute post-staphylococcal GN occurring in patients with underlying diabetic nephropathy, with irreversible renal failure in four of five cases. Our patient had diabetes with progressive renal failure due to infection with E. cloacae causing PIGN. The presence of crescents on kidney biopsy was predictive of a poor renal survival [1]
Diabetics with peripheral neuropathy and poor foot care, especially those who walk bare foot, develop ulcers and infection that go uncontrolled, as in our case, and may lead to PIGN. In developing countries, where early detection of diabetes mellitus and diabetic nephropathy are met with challenges, appropriate foot care and prevention of neuropathic foot are important measures for preventing PIGN super imposed on diabetic nephropathy.
Conflict of interest statement. None declared.
References
- 1.Montseny JJ, Meyrier A, Kleinknecht D, et al. The current spectrum of infectious glomerulonephritis: experience with 76 patients and review of the literature. Medicine (Baltimore) 1995;74:63–73. doi: 10.1097/00005792-199503000-00001. [DOI] [PubMed] [Google Scholar]
- 2.Chang-I Ho, Yao-Ko Wen, Mei-Ling Chen. Glomerulonephritis with acute renal failure related to osteomyelitis. J Chin Med Assoc. 2008;71:315–317. doi: 10.1016/S1726-4901(08)70129-1. [DOI] [PubMed] [Google Scholar]
- 3.Griffin MD, Björnsson J, Erickson SB. Diffuse proliferative glomerulonephritis and acute renal failure associated with acute staphylococcal osteomyelitis. J Am Soc Nephrol. 1997;8:1633–1639. doi: 10.1681/ASN.V8101633. [DOI] [PubMed] [Google Scholar]
- 4.Beaufils M, Morel-Maroger L, Sraer JD, et al. Acute renal failure of glomerular origin during visceral abscesses. N Engl J Med. 1976;295:185–189. doi: 10.1056/NEJM197607222950402. [DOI] [PubMed] [Google Scholar]
- 5.Nasr SH, Markowitz GS, Whelan JD, et al. IgA-dominant acute poststaphylococcal glomerulonephritis complicating diabetic nephropathy. Hum Pathol. 2003;34:1235–1241. doi: 10.1016/s0046-8177(03)00424-6. [DOI] [PubMed] [Google Scholar]