Abstract
Collapsing focal segmental glomerulosclerosis (FSGS), or collapsing glomerulopathy (CG), responds poorly to commonly employed therapies, with a high proportion of patients progressing to end-stage renal disease. We report an adult in a nephrotic state, diagnosed with minimal-change disease on biopsy, who failed to respond to steroids, calcineurin inhibitors (CNIs), mycophenolate mofetil and cyclophosphamide. Repeat biopsy showed CG. Treatment with 4 weekly doses of rituximab led to sustained remission of his nephrotic state. This is the first report of adult-onset CG that has responded favourably to rituximab. Rituximab could be a treatment option for patients with this difficult-to-treat condition.
Keywords: collapsing glomerulopathy, focal segmental glomerulosclerosis, rituximab
Background
Collapsing focal segmental glomerulosclerosis (FSGS), also known as collapsing glomerulopathy (CG), was first described in association with HIV infection [1]. Subsequently, this condition has been recognized in non-HIV-infected patients. The clinical course of CG is characterized by rapid progression to end-stage renal disease and a dismal response to medical therapy. A survey of observational studies reported complete and partial remission rates of 9.6 and 15.2%, respectively, despite multiple therapies that included steroids, calcineurin inhibitors (CNIs) and cyclophosphamide [1]. There have been two reports suggesting a favourable response to rituximab in children with CG [2, 3]. However, there is no such report with regard to adults.
Case report
A 19-year-old-male presented in May 2007 with swelling of the lower limbs and periorbital puffiness of 2 months’ duration. Evaluation at his primary health centre had revealed albuminuria on dipstick analysis, prompting referral to our institution. He gave no history of recent infections, arthralgia, oral ulcers, cough or haemoptysis. On examination, he had bilateral leg oedema extending up to his knees. The blood pressure was 110/70 mmHg, pulse rate was 90 b.p.m. and respiratory rate 14/min. The cardiovascular, abdomen, chest and nervous system examinations were within normal limits. Urinalysis showed 4+ proteinuria, but no erythrocytes or leucocytes. The 24-h urine protein excretion was 6.3 g. The serum creatinine was 71 μmol/L (0.8 mg/dL); serum total protein and albumin were 55 and 17 g/L (5.5 and 1.7 g/dL), respectively, and aspartate and alanine aminotransferases were 12 and 14 IU/L, respectively. Serum cholesterol was 10.4 mmol/L (400 mg/dL), triglyceride 2.8 mmol/L (250 mg/dL), low-density lipoprotein 7.2 mmol/L (280 mg/dL) and high-density lipoprotein 1.3 mmol/L (50 mg/dL). He tested negative for hepatitis B surface antigen, anti-HCV antibody and human immunodeficiency virus I/II. The antinuclear antibody test was negative.
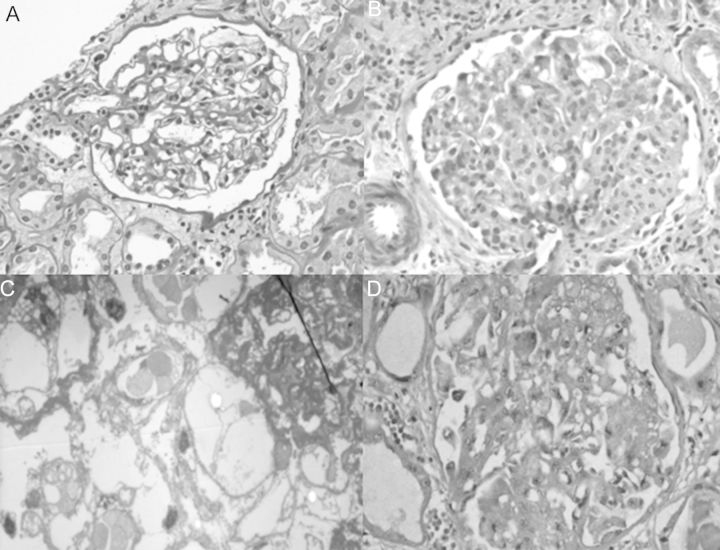
Kidney biopsy (Figure 1A) revealed 10 glomeruli, which were normal on light microscopy (LM), as were the tubulointerstitial and vascular compartments. Immunofluorescence did not reveal any immune deposits and electron microscopy (EM) showed diffuse foot process effacement.
Fig. 1.
Photomicrograph showing (A) normal glomeruli by LM (PAS, ×40), and complete foot process effacement by EM (not shown), consistent with minimal-change disease; (B) Segmental collapse with overlying proliferation of visceral epithelial cells consistent with collapsing glomerulopathy (Masson's trichrome, ×40), (C) electron microscrograph shows hypertrophied podocytes with vacuoles over a collapsed glomerular tuft (uranyl acetate, ×62 000) and (D) proliferating visceral epithelial cells stained with Ki67 (IHC, ×40)
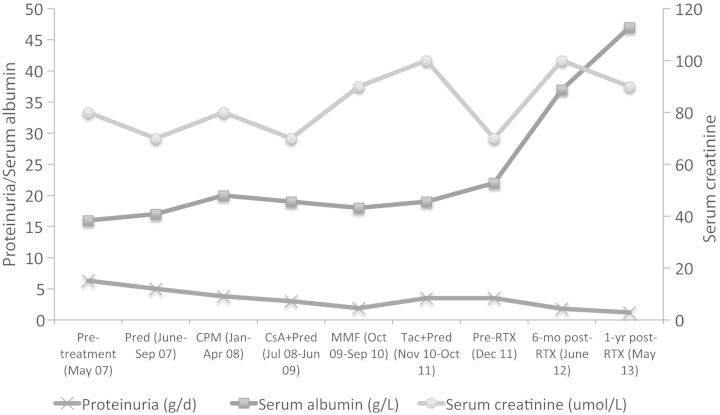
A diagnosis of minimal-change disease (MCD) was made and the patient was started on oral prednisolone at 1 mg/kg/day. However, the proteinuria did not show any reduction. At the end of 4 months, the daily urinary protein excretion remained at 5 g. He was deemed to be steroid resistant and treated first with oral cyclophosphamide at 2 mg/kg for 3 months, followed by oral cyclosporine (4 mg/kg/day, average C0 120 ng/mL) and oral prednisolone (0.1 mg/kg/day) for 6 months, mycophenolate mofetil 2 g/day for 6 months and finally a combination of tacrolimus (0.1 mg/kg/day, average Tac C0 7 ng/mL) and oral prednisolone (0.1 mg/kg/day). The nephrotic state persisted throughout this period, with serum albumin <20 g/L (2.0 g/dL) and the serum creatinine 62–80 μmol/L (0.7–0.9 mg/dL) (Figure 2). During the entire course of his illness, he was continued on supportive therapy with torsemide 10–20 mg twice daily, atorvastatin 20 mg/day and losartan 150 mg/day.
Fig. 2.
Temporal evolution of the clinical and laboratory parameters.
At this time, the kidney biopsy was repeated. LM revealed 13 glomeruli, 2 of which showed segmental collapse of the capillary tuft with an overlying crown of podocytes along with synechiae formation, 2 showed segmental endocapillary cellularity with foam cells, 2 were globally sclerosed and the remaining 7 did not show any significant abnormality (Figure 1B). Tubules showed abundant protein absorption droplets along with patchy tubular atrophy occupying 20% of the biopsy area. Tubules close to the medulla showed marked nucleomegaly along with nuclear smudging associated with tubular necrosis, interstitial oedema and mild-to-moderate patchy plasma cell-rich interstitial inflammation occupying 10% of the biopsy area. Blood vessels were within normal limits. Immunofluorescence was negative for all immunoglobulins, C1q and light chains. EM showed segmental sclerosis with evidence of collapse (Figure 1C). There was diffuse and extensive foot process effacement, and no reticular aggregates were seen. Ki 67 immunostain showed nuclear positivity in the podocytes of glomeruli showing collapse (Figure 1D). CD 20 staining was negative. A final diagnosis of CG was made. The patient's serum tested negative by polymerase chain reaction for cytomegalovirus and parvovirus B-19.
In view of his resistance to the above therapies and a persistently severe nephrotic state with the biopsy showing many plasma cells, the patient was treated with 4 weekly injections of rituximab (375 mg/m2/dose). His oedema subsided and he stopped requiring the diuretic 3 months after the last dose. Six months after the last dose of rituximab, the 24-h urine protein was 1.8 g with a serum albumin of 37 g/L (3.7 g/dL). The patient has now been followed up for 18 months and remains asymptomatic. On his last follow-up, his 24-h urine protein is 1.2 g, serum creatinine 80 μmol/L (0.9 mg/dL) and serum albumin 47 g/L (4.7 g/dL). Figure 2 shows the evolution of his clinical and laboratory parameters during the course of the treatment.
Discussion
We report the first case of adult-onset collapsing FSGS successfully treated with rituximab. CG constitutes ∼11–23.7% of FSGS [4, 5]. Most of the CG is idiopathic or HIV associated. The prognosis of CG not associated with HIV infection has been uniformly dismal [6–8]. Based upon a survey of the observational studies that have reported the response to treatment of collapsing FSGS, the rates of durable complete and partial remission were 9.6 and 15.2%, respectively. Valeri et al. had reported steroid resistance in all of the 26 (100%) CG patients treated with steroids. One out of six (17%) of the patients with steroid-resistant CG treated with cyclophosphamide achieved partial remission and two out three patients with steroid-resistant CG treated with cyclosporine achieved remission (one complete and one partial) [7]. Even though the evidence base is weak, aggressive treatment seems to be associated with higher remission rates, especially in patients with serum creatinine <177 μmol/L (<2 mg/dL) and <20% interstitial fibrosis on kidney biopsy [9, 10].
Rituximab has been successfully used in the management of several glomerular diseases including idiopathic membranous glomerulonephritis, steroid-dependent and -resistant childhood nephrotic syndrome (MCD and FSGS) and vasculitides. The efficacy of rituximab in idiopathic CG was shown in two case reports in the paediatric age group. Kaito et al. [2] described a 2-year-old boy with steroid- and cyclosporine-resistant CG who went into complete remission with four doses of rituximab. However, the child had a relapse after 4 months and required re-treatment with methyl prednisolone to achieve remission. Bitzan et al. [3] reported a favourable response to rituximab in a young patient with CG with dominant C1q containing mesangial immune deposits and CD 20+ interstitial infiltrates, who was initially resistant to steroids.
Other interesting aspects of our case were that the initial kidney biopsy showed features of MCD, failure to respond to steroids, cyclophosphamide, CNIs and mycophenolate mofetil, and the disease being found to have evolved into CG. He tested negative for parvovirus B19, which has been implicated in some cases of CG. MCD is steroid responsive in ∼75% of cases [11]. The lack of response suggests the possibility of FSGS. In a series of 11 patients with steroid-resistant MCD in whom a repeat biopsy was performed, FSGS was present in 54% [11]. This could be explained as the evolution of MCD to FSGS over time. Another possibility is of unsampled FSGS reported as MCD in the first biopsy, which had 10 glomeruli, whereas ideally 25 glomeruli should be evaluated to avoid missing this focal disease.
Rituximab, tried in view of a persistent severe nephrotic state, led to partial remission, which has now been sustained for 18 months. Importantly, Kaito et al. [2] had used CNIs in combination with rituximab. A less than complete response is not surprising in view of the histological changes on biopsy. Compared with the report of the successful use of rituximab in C1q nephropathy with CG by Bitzan et al. [3], our patient lacked CD 20+ infiltrates in the interstitium, but still responded to rituximab.
The exact mechanism by which rituximab induces remission is not clear. Recently, it has become clear that B cells display a variety of functions other than antibody production, which could contribute to autoimmunity. Rituximab depletes B-lymphocytes and blocks T-cell activation by B-lymphocytes and other B-cell-derived factors [12]. Our case is unique by the fact that it is the first case of adult-onset collapsing FSGS that has responded favourably to rituximab after failing all other treatments.
In conclusion, we show a favourable effect of rituximab in an adult with CG, a difficult-to-treat condition. This possibly beneficial role needs to be tested in larger studies.
Conflict of interest statement. We declare that the results presented in this paper have not been published previously in whole or in part, except in abstract format.
References
- 1.Albaqumi M, Soos TJ, Barisoni L, Nelson PJ. Collapsing glomerulopathy. J Am Soc Nephrol. 2006;17:2854–2863. doi: 10.1681/ASN.2006030225. doi:10.1681/ASN.2006030225. [DOI] [PubMed] [Google Scholar]
- 2.Kaito H, Kamei K, Kikuchi E, et al. Successful treatment of collapsing focal segmental glomerulosclerosis with a combination of rituximab, steroids and ciclosporin. Pediatr Nephrol. 2010;25:957–959. doi: 10.1007/s00467-009-1410-8. doi:10.1007/s00467-009-1410-8. [DOI] [PubMed] [Google Scholar]
- 3.Bitzan M, Ouahed JD, Krishnamoorthy P, Bernard C. Rituximab treatment of collapsing C1q glomerulopathy: clinical and histopathological evolution. Pediatr Nephrol. 2008;23:1355–1361. doi: 10.1007/s00467-008-0781-6. doi:10.1007/s00467-008-0781-6. [DOI] [PubMed] [Google Scholar]
- 4.Thomas DB, Franceschini N, Hogan SL, et al. Clinical and pathologic characteristics of focal segmental glomerulosclerosis pathologic variants. Kidney Int. 2006;69:920–926. doi: 10.1038/sj.ki.5000160. doi:10.1038/sj.ki.5000160. [DOI] [PubMed] [Google Scholar]
- 5.Stokes MB, Valeri AM, Markowitz GS, D'Agati VD. Cellular focal segmental glomerulosclerosis: clinical and pathologic features. Kidney Int. 2006;70:1783–1792. doi: 10.1038/sj.ki.5001903. doi:10.1038/sj.ki.5001903. [DOI] [PubMed] [Google Scholar]
- 6.Detwiler RK, Falk RJ, Hogan SL, Jennette JC. Collapsing glomerulopathy: a clinically and pathologically distinct variant of focal segmental glomerulosclerosis. Kidney Int. 1994;45:1416. doi: 10.1038/ki.1994.185. doi:10.1038/ki.1994.185. [DOI] [PubMed] [Google Scholar]
- 7.Valeri A, Barisoni L, Appel GB, Seigle R, D'Agati V. Idiopathic collapsing focal segmental glomerulosclerosis: a clinicopathologic study. Kidney Int. 1996;50:1734–1746. doi: 10.1038/ki.1996.493. doi:10.1038/ki.1996.493. [DOI] [PubMed] [Google Scholar]
- 8.Grcevska L, Polenakovik M. Collapsing glomerulopathy: clinical characteristics and follow-up. Am J Kidney Dis. 1999;33:652–657. doi: 10.1016/s0272-6386(99)70215-5. doi:10.1016/S0272-6386(99)70215-5. [DOI] [PubMed] [Google Scholar]
- 9.Schwimmer JA, Markowitz GS, Valeri A, Appel GB. Collapsing glomerulopathy. Semin Nephrol. 2003;23:209–218. doi: 10.1053/snep.2003.50019. doi:10.1053/snep.2003.50019. [DOI] [PubMed] [Google Scholar]
- 10.Laurinavicius A, Hurwitz S, Rennke HG. Collapsing glomerulopathy in HIV and non-HIV patients: a clinicopathological and follow-up study. Kidney Int. 1999;56:2203–2213. doi: 10.1046/j.1523-1755.1999.00769.x. doi:10.1046/j.1523-1755.1999.00769.x. [DOI] [PubMed] [Google Scholar]
- 11.Waldman M, Crew RJ, Valeri A, et al. Adult minimal-change disease: clinical characteristics, treatment, and outcomes. Clin J Am Soc Nephrol. 2007;2:445–453. doi: 10.2215/CJN.03531006. doi:10.2215/CJN.03531006. [DOI] [PubMed] [Google Scholar]
- 12.Porakishvili N, Mageed R, Jamin C, et al. Recent progress in the understanding of B-cell functions in autoimmunity. Scand J Immunol. 2001;54:30–38. doi: 10.1046/j.1365-3083.2001.00950.x. doi:10.1046/j.1365-3083.2001.00950.x. [DOI] [PubMed] [Google Scholar]