Abstract
The Third Universal Definition of Myocardial Infarction (MI) requires cardiac myocyte necrosis with an increase and/or a decrease in a patient’s plasma of cardiac troponin (cTn) with at least one cTn measurement greater than the 99th percentile of the upper normal reference limit during: (1) symptoms of myocardial ischemia; (2) new significant electrocardiogram (ECG) ST-segment/T-wave changes or left bundle branch block; (3) the development of pathological ECG Q waves; (4) new loss of viable myocardium or regional wall motion abnormality identified by an imaging procedure; or (5) identification of intracoronary thrombus by angiography or autopsy. Myocardial infarction, when diagnosed, is now classified into five types. Detection of a rise and a fall of troponin are essential to the diagnosis of acute MI. However, high sensitivity troponin assays can increase the sensitivity but decrease the specificity of MI diagnosis. The ECG remains a cornerstone in the diagnosis of MI and should be frequently repeated, especially if the initial ECG is not diagnostic of MI.
There have been significant advances in adjunctive pharmacotherapy, procedural techniques and stent technology in the treatment of patients with MIs. The routine use of antiplatelet agents such as clopidogrel, prasugrel or ticagrelor, in addition to aspirin, reduces patient morbidity and mortality. Percutaneous coronary intervention (PCI) in a timely manner is the primary treatment of patients with acute ST segment elevation MI. Drug eluting coronary stents are safe and beneficial with primary coronary intervention. Treatment with direct thrombin inhibitors during PCI is non-inferior to unfractionated heparin and glycoprotein IIb/IIIa receptor antagonists and is associated with a significant reduction in bleeding. The intra-coronary use of a glycoprotein IIb/IIIa antagonist can reduce infarct size. Pre- and post-conditioning techniques can provide additional cardioprotection. However, the incidence and mortality due to MI continues to be high despite all these recent advances. The initial ten year experience with autologous human bone marrow mononuclear cells (BMCs) in patients with MI showed modest but significant increases in left ventricular (LV) ejection fraction, decreases in LV end-systolic volume and reductions in MI size. These studies established that the intramyocardial or intracoronary administration of stem cells is safe. However, many of these studies consisted of small numbers of patients who were not randomized to BMCs or placebo. The recent LateTime, Time, and Swiss Multicenter Trials in patients with MI did not demonstrate significant improvement in patient LV ejection fraction with BMCs in comparison with placebo. Possible explanations include the early use of PCI in these patients, heterogeneous BMC populations which died prematurely from patients with chronic ischemic disease, red blood cell contamination which decreases BMC renewal, and heparin which decreases BMC migration. In contrast, cardiac stem cells from the right atrial appendage and ventricular septum and apex in the SCIPIO and CADUCEUS Trials appear to reduce patient MI size and increase viable myocardium. Additional clinical studies with cardiac stem cells are in progress.
Keywords: Myocardial necrosis, Type 1-5 myocardial infarctions, Troponin assays, Percutaneous coronary intervention, Fibrinolytic therapy, Thienopyridines, Cardioprotection, Bone marrow stem cells, Cardiac stem cells
Core tip: The Third Universal Definition of myocardial infarction (MI) combines clinical symptoms, cardiac biomarkers and electrocardiogram (ECG) changes. Small amounts of myocardial necrosis may occur with heart failure, renal failure, myocarditis, arrhythmias, pulmonary embolism or uneventful percutaneous or surgical coronary revascularization and should be termed myocardial injury. High sensitivity troponin assays increase the sensitivity but decrease the specificity of MI diagnosis. The ECG remains a cornerstone of MI diagnosis. Primary percutaneous coronary intervention in a timely manner is the primary treatment of patients with acute ST segment elevation MI. Antiplatelet agents (clopidogrel, prasugrel or ticagrelor), in addition to aspirin, reduce patient MI morbidity and mortality. The recent LateTime, Time, and Swiss Multicenter Trials of bone marrow stem cells in MI treatment did not demonstrate significant improvement in patient LV ejection fraction in comparison with placebo. In contrast, cardiac stem cells from the right atrial appendage or ventricular septum/apex in the SCIPIO and CADUCEUS Trials reduced patient MI size and increased viable myocardium. Studies with cardiac stem cells are continuing.
DEFINITION OF MYOCARDIAL INFARCTION
The Third Universal Definition of myocardial infarction (MI) expert consensus document was published in October 2012 by the global Myocardial Infarction Task Force[1]. The definition of MI requires cardiac myocyte necrosis with an increase and/or a decrease in plasma of cardiac troponin (cTn). At least one cTn measurement should be greater than the 99th percentile normal reference limit during: (1) symptoms of myocardial ischemia; (2) new (or presumably new) significant ECG ST-segment/T-wave changes or left bundle branch block; (3) the development of pathological electrocardiographic (ECG) Q waves; (4) new loss of viable myocardium or regional wall motion abnormality identified by an imaging procedure; or (5) identification of intracoronary thrombus by angiography or autopsy.
Cardiac troponin (I or T) has high myocardial tissue specificity as well as high clinical sensitivity because cTn T and I are essential contractile components of myocardial cells and are expressed almost exclusively in the myocardium. Release of cardiac troponin from the myocardium can result from normal turnover of myocardial cells, myocyte apoptosis, myocyte release of troponin degradation products, increased myocyte wall permeability and bleb formation, or myocyte necrosis[1].
Myocardial necrosis due to myocardial ischemia is defined as myocardial infarction[2]. Detection of a rise and a fall of troponin, expressed in ng/L or pg/mL, is essential to the diagnosis of acute MI[3,4]. Blood samples for the measurement of cTn should be drawn during the initial patient assessment and repeated 3-6 h later. Subsequent additional blood samples are required if further ischemic episodes occur, or when the timing of the initial symptoms onset is unclear[5]. The demonstration of a rise and fall in troponin measurements is extremely important in the differentiation of acute from chronic elevations in cTn concentrations that can be associated with structural heart disease such as patients with left ventricular hypertrophy (LVH), renal failure and heart failure (Table 1)[6].
Table 1.
Causes of troponin elevation
| System | Causes of troponin elevation |
| Cardiovascular | Acute aortic dissection |
| Arrhythmia | |
| Medical ICU patients | |
| Hypotension | |
| Heart failure | |
| Apical ballooning syndrome | |
| Cardiac inflammation | |
| Endocarditis, myocarditis, pericarditis | |
| Hypertension | |
| Infiltrative disease | |
| Amyloidosis, sarcoidosis, hemochromatosis, scleroderma | |
| Left ventricular hypertrophy | |
| Myocardial injury | Blunt chest trauma |
| Cardiac surgeries | |
| Cardiac procedures | |
| Ablation, cardioversion, percutaneous intervention | |
| Chemotherapy | |
| Hypersensitivity drug reactions | |
| Envenomation | |
| Respiratory | Acute PE |
| ARDS | |
| Infectious/immune | Sepsis/SIRS |
| Viral illness | |
| Thrombotic thrombocytopenic purpura | |
| Gastrointestinal | Severe GI bleeding |
| Nervous system | Acute stroke |
| Ischemic stroke | |
| Hemorrhagic stroke | |
| Head trauma | |
| Renal | Chronic kidney disease |
| Endocrine | Diabetes |
| Hypothyroidism | |
| Musculoskeletal | Rhabdomyolysis |
| Integumentary | Extensive skin burns |
| Inherited | Neurofibromatosis |
| Duchenne muscular dystrophy | |
| Klippel-Feil syndrome | |
| Others | Endurance exercise |
| Environmental exposure | |
| Carbon monoxide, hydrogen sulfide |
GI: Gastrointestinal; ICU: Intensive care unit; PE: Pulmonary embolus; ARDS: Acute respiratory distress syndrome; SIRS: Systemic inflammatory response syndrome.
The ECG remains a cornerstone in the diagnosis of MI and should be acquired and interpreted within 10 min after patient presentation[7]. Since ECG changes of MI can be transient, ECGs should be acquired at 15-30 min intervals, especially if the initial ECG is equivocal. Wide spread and profound ST-T changes are associated with greater degrees of myocardial ischemia. The extent and severity of coronary stenosis, collateral coronary circulation and prior myocardial necrosis impact on the ECG manifestations of myocardial ischemia[8]. Prior ECGs, when available, should be compared with current tracings. Mimickers of ECG changes of MI such as acute pericarditis, LVH, left bundle branch block (LBBB), Brugada syndrome, stress cardiomyopathy, and early repolarization patterns should be considered in the differential diagnosis[9].
Electrocardiographic ST-T wave criteria for the diagnosis of acute myocardial ischemia is listed in Table 2. The J point is used to determine the magnitude of the ST-segment shift. “Contiguous leads” refers to lead groups such as anterior leads (V1-V6), inferior leads (II, III, aVF) or lateral/apical leads (I, aVL).
Table 2.
Electrocardiogram manifestations of acute myocardial ischemia (in absence of left ventricular hypertrophy and left bundle branch block)
| ST elevation |
| New ST elevation at the J point in two contiguous leads with the cut-points: |
| ≥ 0.1 mV in all leads other than leads V2–V3 where the following cut points apply: ≥ 0.2 mV in men ≥ 40 yr; ≥ 0.25 mV in men < 40 yr, or ≥ 0.15 mV in women |
| ST depression and T wave changes |
| New horizontal or down-sloping ST depression ≥ 0.05 mV in two contiguous |
| leads and/or T inversion ≥ 0.1 mV in two contiguous leads with prominent R wave or R/S ratio > 1 |
Supplemental leads such as V3R and V4R, in the third and fourth right intercostal spaces, indicate the electrical activity in the free wall of the right ventricle and V7-V9 indicate the electrical activity in the inferobasal left ventricular wall. In patients with inferior and right ventricular infarction, ST segments are often elevated ≥ 0.05 mV in V3R and V4R. In addition, ST elevation of ≥ 0.05 mV ST in leads V7-V9 (V7 at the left posterior axillary line, V8 at the left mid-scapular line, and V9 at the left paraspinal border), supports the diagnosis of inferobasal MI due to left circumflex coronary artery occlusion. ST depression in leads V1-V3 also may be suggestive of inferobasal myocardial ischemia (posterior infarction), especially when the terminal T wave is positive[10-12].
ST segment elevation of > 0.5 mV is observed in lead aVR in acute left main coronary artery (LMCA) obstruction and proximal left anterior descending coronary artery (LAD) obstruction proximal to the first major septal branch. The ST elevation in aVR is more pronounced than in V1 in patients with acute LMCA occlusion. This pattern occurred in 88% of the patients with acute occlusion of LMCA group in one study[10,13]. Types of MI, five types of MI are based on pathological, clinical and prognostic differences (Table 3).
Table 3.
Third universal classification of myocardial infarction
| Type 1: Spontaneous MI |
| Spontaneous MI due to atherosclerotic plaque rupture, ulceration, fissuring, erosion, or dissection with resulting intraluminal thrombus in one or more of the coronary arteries leading to decreased myocardial blood flow or distal platelet emboli with ensuing myocyte necrosis. The patient may have underlying severe CAD, non-obstructive coronary disease or no CAD |
| Type 2: MI secondary to an ischemic imbalance |
| Myocardial injury with necrosis occurs due to conditions other than CAD that contribute to an imbalance between myocardial oxygen supply and/or demand such as coronary endothelial dysfunction, coronary artery spasm, coronary embolism, tachycardia-bradycardia arrhythmias, anemia, respiratory failure, hypotension, and hypertension |
| Type 3: MI resulting in death when biomarker values are unavailable |
| Cardiac death with symptoms suggestive of myocardial ischemia and presumed new ischemic ECG changes or new LBBB, but death occurs before blood samples can be obtained, before cardiac troponins biomarkers rise, or when cardiac biomarkers were not collected |
| Type 4A: MI related to percutaneous coronary intervention |
| MI associated with PCI is defined by elevation of cTn values greater than five times the 99th percentile upper normal reference limit (URL) in patients with normal baseline values (< 99th percentile URL) or a rise of cTn values by > 20% if the baseline troponins are elevated and are stable or falling. In addition one of the following criterion are required: (1) symptoms suggestive of myocardial ischemia; (2) new ischemic ECG changes or new LBBB; (3) angiographic loss of patency of a major coronary artery or a side branch or persistent slow- or no coronary flow or coronary embolization; or (4) demonstration with imaging of a new loss of viable myocardium or new regional wall motion abnormality |
| Type 4B: MI related to stent thrombosis |
| MI associated with stent thrombosis detected by coronary angiography or autopsy in the presence of myocardial ischemia with a rise and/or fall of troponin biomarkers. One troponin measurement should be above the 99th percentile UR |
| Type 4C: MI related to restenosis |
| MI associated with restenosis defined as ≥ 50% stenosis or a complex lesion demonstrated at coronary angiography after (1) initial successful stent deployment; or (2) dilatation of a coronary artery stenosis with balloon angioplasty. These coronary angiographic changes should be associated with an increase and/or decrease of cTn values > 99th percentile URL and no other significant obstructive CAD |
| Type 5: MI related to coronary artery bypass grafting |
| MI associated with CABG is defined by elevation of cardiac troponins greater than ten times the 99th percentile URL in patients with normal baseline cTn values (< 99th percentile URL). In addition, one of the following should be present: (1) new pathological Q waves or new LBBB; or (2) angiographic documented new graft or new native coronary artery occlusion; or (3) new loss of viable myocardium or new regional wall motion abnormality as shown by an imaging modality |
Adapted from Thygesen et al[14]. MI: Myocardial infarction; CAD: Coronary artery disease; PCI: Percutaneous coronary intervention; cTn: Cardiac troponin; CABG: Coronary artery bypass grafting; LBBB: Left bundle branch block.
DIFFERENTIATING BETWEEN SPONTANEOUS TYPE 1 AND ISCHEMIC IMBALANCE TYPE 2 MYOCARDIAL INFARCTION
Differentiation between type 2 and type 1 MI is challenging and needs careful clinical assessment. It is very important that the differentiation be made whether the myocardial injury is likely to be due to plaque rupture (type 1 MI), or whether it is due to an imbalance in myocardial oxygen supply or demand (type 2 MI), because the management of these two conditions is very different. While, the treatment of type 1 MI primarily includes antithrombotic therapy and/or revascularization, as clinically appropriate, the management of type 2 MI is more varied because several different mechanisms may be responsible for pathogenesis ischemic imbalance. In critically ill patients or in patients with major (non-cardiac) surgery, biomarker elevation may be caused by the direct toxic effects of endogenous or exogenous high circulating catecholamines, coronary vasospasm and/or endothelial dysfunction or fixed coronary atherosclerosis and demand-supply mismatch (Figure 1). For example, a post-operative patient with hypotension and troponin elevation due to hypovolemia or acute blood loss, requires treatment with intravascular volume replacement, including blood transfusion. In certain instances, troponin elevation due to ischemic demand may unmask severe coronary artery disease (CAD) by increasing myocardial oxygen demand in the presence of fixed coronary stenosis. Consequently once the patient recovers from the acute illness, a stress test for inducible ischemia or coronary angiography can be helpful.
Figure 1.
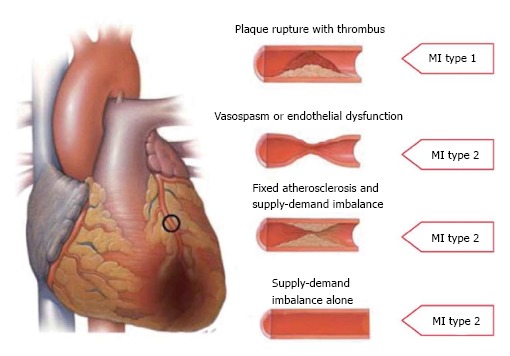
Type 1 and type 2 myocardial infarctions.
MYOCARDIAL INFARCTION DUE TO REVASCULARIZATION PROCEDURES
The 2007 universal MI definition required the presence of cardiac biomarkers greater than three times the 99th percentile of the upper normal range limit (URL) without requirements for associated ischemic changes or complications from angiographic procedures. This resulted in approximately 15% of patients undergoing PCI being diagnosed with an AMI[15,16]. In the 2012 definition of MI, there is a more strict definition of type 4a MI[1]. Percutaneous coronary intervention related MI is defined by cTn elevation greater than five times 99th percentile within 48 h after the procedure with: (1) symptoms suggestive of myocardial ischemia; or (2) new ischemic ECG changes; or (3) angiographic findings consistent with a procedural complication with loss of a major artery or side coronary artery branch, decreased coronary flow, or coronary embolization; or (4) demonstration of new loss of viable myocardium or new regional wall motion abnormality. The occurrence of procedure-related myocardial cell injury with necrosis can be detected by measurements of cardiac troponin before the procedure, 3-6 h after the procedure and, optionally, re-measurement 12 h thereafter. An increasing cTn can only be interpreted as a procedure-related myocardial injury if the pre-procedural cTn value is ≤ 99th percentile URL or if the troponin measurements are stable or falling. If the pre-procedural troponin is increased but is either stable or falling, an increase in cTn levels of > 20% is used to characterize a PCI-related MI.
The relationship between troponin increases after revascularization and mortality is controversial. The evidence for the association between biomarkers and mortality has evolved over the last 15 years. Studies have suggested a stronger association with the post-PCI MB fraction of creatine kinase (CK-MB) and subsequent cardiovascular events than with cTn elevation[15,17]. The level of CK-MB measurements varied from three to ten times the URL in these studies. When analyzed in categories of incrementally increasing biomarker elevations, most contemporary PCI studies have reported associations between peri-procedural myonecrosis and mortality only for very large patient infarctions[17]. Only pre-procedure cTn elevations are correlated with subsequent mortality[18,19]. Consequently, in patients with baseline troponin elevation prior to PCI, the diagnostic accuracy of using the definition of post-PCI MI is limited.
With the application of the 2007 universal definition of post CABG MI (type 5), 42% to 82% of cardiac surgical patients had cardiac biomarker elevation greater than five times the URL[20], but only 4% to 7% had electrocardiographic evidence required for post-CABG MI[21]. Elevation of cardiac biomarker values after CABG can occur due to myocardial trauma, with dissection of the coronary arteries, manipulation of the heart, inadequate cardiac protection, reperfusion injury, or graft failure. Any increase in cardiac biomarker values > 99th percentile URL is defined as myocardial injury. The new criteria for type 5 MI in patients with CABG requires an increase in biomarkers > 10 × 99th percentile URL from a normal baseline during the first 48 h after surgery, plus new electrocardiographic Q waves or new LBBB, angiographic documentation of new graft or new native coronary artery occlusion, or imaging evidence of new regional wall motion abnormality or new loss of viable myocardium. The 2012 global MI task force emphasized that the threshold for diagnosing MI is more robust for on-pump CABG. The existing criteria for the universal definition of myocardial infarction should be used for diagnosing MI in patients who are more than 48 h after cardiac surgery[1].
The Society for Cardiovascular Angiography and Interventions has published an expert consensus document that defines clinically relevant myocardial infarction after revascularization (Table 4)[14].
Table 4.
Proposed definition of clinically relevant myocardial infarction after both percutaneous coronary intervention and coronary artery bypass grafting procedures
| In patients with normal baseline CK-MB | The peak CK-MB measured within 48 h of the procedure rises to ≥ 10 × the local laboratory ULN, or to ≥ 5 × ULN with new pathologic Q-waves in ≥ 2 contiguous leads or new persistent LBBB, OR in the absence of CK-MB measurements and a normal baseline cTn, a cTn (I or T) level measured within 48 h of the PCI rises to ≥ 70 × the local laboratory ULN, or ≥ 35 × ULN with new pathologic Q-waves in ≥ 2 contiguous leads or new persistent LBBB |
| In patients with elevated baseline CK-MB (or cTn) in whom the biomarker levels are stable or falling | The CK-MB (or cTn) rises by an absolute increment equal to those levels recommended above from the most recent pre-procedure level |
| In patients with elevated CK-MB (or cTn) in whom the biomarker levels have not been shown to be stable or falling | The CK-MB (or cTn) rises by an absolute increment equal to those levels recommended above plus new ST-segment elevation or depression plus signs consistent with a clinically relevant MI, such as new onset or worsening heart failure or sustained hypotension |
ULN: Upper limit of normal; MI: Myocardial infarction; cTn: Cardiac troponin.
REINFARCTION/RECURRENT MI
The term “reinfarction” is used for an acute MI that occurs within 28 d of a MI. If the cTn concentration is elevated, but stable or decreasing at the time of suspected reinfarction, the diagnosis of reinfarction requires a 20% or greater increase in the cTn measurement. If the initial cTn concentration is normal at the time of suspected reinfarction, the criteria for new acute MI apply[1,22].
TROPONIN ELEVATION IN HEART FAILURE
Based on the type of assay used, a range of elevated cTn values, indicative of myocardial injury with necrosis, may be seen in patients with a heart failure (HF) syndrome[23]. In stable heart failure patients, the median concentration of hs-cTnT is 12 ng/L, which is very close to the 99th percentile URL of 14 ng/L for this assay[24]. Hence, using hs-cTn assays, cTn concentrations may be measured in nearly all patients with HF. Many HF patients exceed the 99th percentile URL, especially those patients with severe decompensated HF syndrome[25]. While type 1 MI is an important cause of acutely decompensated heart failure, other mechanism(s) leading to troponin elevation in HF syndromes such as supply-demand inequity (type 2 MI) should be considered. Non-coronary triggers, such as anemia, cellular necrosis, apoptosis, or autophagy in the context of wall stress may cause troponin release in HF, as can the toxic effects of circulating neurohormones, toxins, inflammation, and infiltrative processes. Nonetheless, in patients with HF, troponin elevation independent of its mechanism, is strongly predictive of an adverse outcome and should not be ignored[25].
HIGH SENSITIVITY TROPONIN ASSAYS
Highly sensitive assays for cTnT and cTnI are available and are widely used in many parts of the world, although they are not generally used at the present time in the United States[26]. Two criteria should be met for high sensitivity troponin assays (hs-Tn). First, the coefficient of variation at the 99th percentile value should be ≤ 10%. Second, the assay should be able to measure cTn concentrations below the 99th percentile in ≥ 95% of normal individuals[27]. Compared with standard cTn assays, the hs-cTn assays have improved sensitivity and discrimination for MI, particularly in the first 3 to 6 h after symptom onset[28]. These advantages are somewhat offset by a decrease in specificity for MI[28-30] and concerns regarding the broad application of these tests, especially in populations with a low MI prevalence.
There is controversy regarding the metrics that should be used with hs-cTn assays for the diagnosis of AMI. In this regard, attempts have been made to define in these assays the optimal value for relative change or deltas in hs-cTn concentrations. Higher deltas increase specificity while lower ones improve sensitivity. The potential for analytical interferences with hs-cTn assays is greater than with conventional assays. Examples include reductions in hs-cTnT concentrations due to hemolysis and autoantibodies or increases due to heterophilic antibodies[31]. Studies suggest that an absolute increase of hs-cTnT values, i.e., > 7 ng/L over 2 h, is superior to relative percentage changes from the baseline in the diagnosis of MI[32-34].
According to the recent guideline for the management of patients with acute coronary syndromes, blood samples for high-sensitivity cardiac troponin measurements should be obtained at presentation and 3 h after admission[35]. Measurements of hs-cTn should be repeated 6 h after admission in patients in whom the 3 h values are unchanged but in whom the clinical suspicion of MI is still high[36].
Distinguishing between type 1 and type 2 MI is challenging with high sensitivity troponin measurements. As troponin assay sensitivity increases, the frequency of possible type 2 MI increases and the distinction from type 1 MI becomes more complicated. Moreover, the diagnostic accuracy of a baseline measurement of hs-cTn for presence of AMI in patients with renal insufficiency is poor[37]. Nevertheless, elevated hs-cTns have important prognostic implications and patients require additional evaluations because a high cTnT level is associated with all-cause and cardiovascular mortality and with incident heart failure in 3 population based studies[30].
TREATMENT OF ACUTE MYOCARDIAL INFARCTION
The incidence of ST segment myocardial infarction (STEMI) has gradually declined over the past decade. However it still accounts for 25%-40% of all acute coronary syndrome related hospitalizations in the United States[37]. Moreover, the incidence of acute myocardial infarction is increasing in the developing countries[38]. Heart disease is expected to be the leading cause of death in the developing world by the year 2020. With changing dietary and personal habits, the prevalence of smoking, hypertension, diabetes, obesity and metabolic syndrome are increasing in areas of the world with large populations such as India[39], China[40] and South America[41]. Advances made in the area of medical therapy and coronary interventions have resulted in a significant decrease in the mortality rates. Current in-hospital and one year mortality are in the order of 5%-6% and 7%-18% respectively[42,43]. During the course of last three decades, there have been significant advances in our understanding of the pathophysiology and treatment of STEMI. In addition to these scientific advances, substantial progress has been made in the areas of public awareness and guideline driven clinical practice[44]. This has led to a gradual decline in STEMI related mortality and improved patient related outcomes. However, there continues to be significant difference in the 30-d mortality rates based on the geographic region[45], age[46,47], gender[48] and race[49]. In addition, individuals with diabetes and chronic renal insufficiency continue to have high rates of mortality[50-52]. In the recent INFUSE-AMI (Intracoronary Abciximab and Aspiration Thrombectomy During Primary PCI for Anterior STEMI) trial[53], diabetics compared to non-diabetics, had higher incidence of stent thrombosis at 30 d (4.3% vs 0.8%, P = 0.03) and higher rates of major cardiovascular and cerebrovascular events at 1 year (16.5% vs 8.0%, P = 0.04). It has been shown that patients with end-stage renal disease frequently do not receive guideline based therapies. In one registry, it has been shown that only 45% of eligible patients on dialysis received coronary reperfusion therapy, and only 70% of patients received aspirin on admission for coronary syndromes. In-hospital mortality rate from myocardial infarction is 21.3% in those on dialysis and 11.7% in those with renal disease but not on dialysis[54].
Approximately 7% of the eligible patients with myocardial infarctions do not receive reperfusion therapy[55]. There is evidence suggesting that reperfusion therapy offers benefit in the elderly. However, age is the strongest predictor associated with an individual not receiving reperfusion therapy[56]. Programs that focus on patient education, systematic organization of STEMI programs and standardization of clinical practice result in improved care of all groups of patients and minimize disparities[57,58].
One of the most important components of STEMI management is getting the patients in a time efficient manner to a hospital that is capable of administering reperfusion therapies such as fibrinolytic therapy and primary percutaneous coronary intervention. Although approximately 98% of the United States population is within the reach of 911 based emergency medical service systems, patients with STEMI do not routinely utilize the system[59]. System based delays have been shown to increase STEMI related morbidity and mortality[60-63]. Hence increased community awareness and preparedness is important. In addition, regional STEMI centers with organized protocols, system based time-to-treatment goals and quality improvement programs must be established. Such efforts minimize delays and lower morbidity and mortality in STEMI patients[64,65]. In a study by Sørensen et al[66], where 759 consecutive STEMI patients were divided into a group with pre-hospital diagnosis and direct referral to a primary PCI center vs a group without pre-hospital diagnosis. Pre-hospital diagnosis and direct referral resulted in shorter system delay (92 min vs 153 min, P < 0.001).
CORONARY REPERFUSION STRATEGIES
Fibrinolytic therapy (FT) and Primary Percutaneous Coronary Intervention (P-PCI) are the two currently available modalities of reperfusion therapies. Both of these options are extensively studied. P-PCI, when performed in a timely manner at a high patient volume center is superior to FT. However, P-PCI is not universally available[67]. Delays in door-to-balloon times (D2B) are associated with increased mortality[68]. Adherence to D2B goal of < 90 min lowers mortality[69,70]. Although P-PCI is superior to FT, emphasis should be placed on timely administration of some form of reperfusion therapy rather than the mode of treatment[71].
For patients who present to a P-PCI capable hospital, the door to balloon time should not exceed 90 min. When patients present to a hospital that is not capable of P-PCI, factors such as time of onset of symptoms, risk of bleeding, presence of acute heart failure or shock, risk of mechanical complications, time-to-transfer to a P-PCI capable hospital should be taken into consideration. In patients who present within less than 1-2 h of onset of symptoms, immediate FT may be advantageous even if the transfer times are short[72].
ROLE OF PRE-HOSPITAL FIBRINOLYTIC THERAPY
Multiple trials have shown the safety and efficacy of pre-hospital FT[73-76]. This approach reduces the time to treatment by approximately 60 min and decreases mortality by 17%[77]. Similar findings were also seen in the pooled analysis of two other trials[78]. The Swedish and the French (USIC) registries showed that pre-hospital FT can be administered safely and results in reduces mortality[79,80]. At this time, pre-hospital use of FT is not commonly used in the United States but is used frequently in Western Europe and England.
STEMI PATIENTS WITH OUT-OF-HOSPITAL CARDIAC ARREST
Approximately 70% of CAD related deaths present as cardiac arrest prior to presenting to a hospital[81]. Less than a quarter of patients presenting with sudden cardiac arrest have ventricular tachycardia or ventricular fibrillation that can be electrically converted to normal sinus rhythm[82]. Of the 60% patients who are resuscitated by emergency response teams, the median survival rate to hospital discharge is 7.9%[83]. In patients with STEMI who present with sudden cardiac arrest, timely defibrillation and hypothermia have been shown to increase survival. For every minute delay in defibrillation, there is 7% to 10% drop in survival[83,84]. Increasing access to and use of defibrillators in public places has resulted in an increase in the number of patients that are neurologically intact after sudden cardiac arrest[84-86]. In patients with out-of hospital cardiac arrest, hypothermia with temperatures between 32 °C to 34 °C increases survival. In a study of 77 patients[87], hypothermia (with the core body temperature reduced to 33 degrees C within 2 h after the return of spontaneous circulation and maintained at that temperature for 12 h) compared to normal temperature increased the survival rates 26% to 49% P = 0.0046. In another study, survival was shown to be improved with hypothermia[88]. In patients with out-of hospital cardiac arrest in the setting of STEMI, hypothermia should be initiated as soon as possible.
FIBRINOLYTIC THERAPY
When P-PCI is not available, FT is an alternative. It reduced mortality and morbidity when carefully administered within 12 h of symptom onset[89-94]. The usefulness of FT in patients presenting greater than 12 h from the onset of symptoms is not well established[95-98]. Fibrin specific agents such as tenecteplase, retaplase and alteplase are preferred. Tenecteplase is the most fibrin specific. None of the fibrin specific agents are antigenic. Patency rates of the infarct related artery with fibrin specific agents are approximately 85%[99-103]. Streptokinase is a non-fibrin-specific agent and can cause antigenic reactions. Infarct related artery patency rate with streptokinase is 60%-70%[104]. When the delay from first medical contact to primary PCI is > 120 min, FT is indicated if the time of onset of symptoms is < 12 h.
ADJUNCTIVE PHARMACOTHERAPY WITH FIBRINOLYTIC THERAPY
The role of Aspirin and Clopidogrel with fibrinolytic therapy is well established[105-107]. Aspirin and Clopidogrel should be given prior to the administration of fibrinolytic agent. Dual antiplatelelt therapy should be continued for at least one year[107]. The data on using newer antiplatelet agents like Prasugrel and Ticagrelor as an adjunct to thrombolytic therapy for fibrinolysis is not yet well established.
In addition to antiplatelet therapy, the use of adjunctive anticoagulants is supported when fibrinolytic agents are used for STEMI[108]. Unfractionated heparin, Enoxaparin and Fondaparinux can be used. However, low molecular weight heparins (LMWH) should be avoided in patients with impaired renal function (Creatinine Clearance < 30 mL/min)[109].
FAILED FIBRINOLYTIC THERAPY
Ongoing chest pain, lack of > 50% ST segment resolution and the absence of reperfusion arrhythmias at 60-90 min after the administration of fibrinolytics is considered failure of treatment. These parameters predict TIMI flow < 3 in the infarct artery[110]. In patients who don’t respond to (FT), “rescue” PCI has been shown to be beneficial. In the Rapid Early Action for Coronary Treatment Trail[111]. The primary components endpoint of death, reinfarction, stroke, or severe HF at 6 mo, was lower among patients randomized to rescue PCI compared to conservative care or repeat fibrinolysis (event-free survival rate: 84.6% vs 70.1% vs 68.7%, P = 0.004). This was due to reduction in reinfarction. There was no significant survival benefit. Minor bleeding was significantly higher among patients randomized to rescue PCI. However, there were no differences in major bleeding among the conservative therapy, repeat fibrinolysis or, rescue PCI groups. Similar findings of improved event free survival were reported in the Middlesbrough Early Revascularization to Limit Infarction trail. However, higher rates of stroke and periprocedural bleeding were associated with rescue PCI[112,113]. In patients with ongoing symptoms, lack of signs reperfusion, significant hypotension, severe CHF, cardiogenic shock, ECG evidence of large area of myocardium at risk, the benefit of early PCI justifies the risk of bleeding. Conservative treatment might be reasonable in a patient with improving symptoms and a limited inferior infarction despite the persistence of ST elevation.
PATIENTS PRESENTING WITH CARDIOGENIC SHOCK
In the SHOCK trial[114], 302 patient with STEMI with shock were randomized to medical stabilization (n = 150) group, which included thrombolysis (63% of patients), intra-aortic balloon counterpulsation (86%), and subsequent revascularization (25%), or to an early revascularization group (n = 152). The primary endpoint of survival at 1 year was 46.7% for patients in the early revascularization group compared with 33.6% in the initial medical stabilization group (absolute difference in survival, 13.2%; P < 0.03). In a prespecified subgroup analyses, only age (< 75 years vs ≥ 75 years) interacted significantly (P < 0.03) with treatment. The benefit was seen only in patients younger than 75 years (51.6% survival in early revascularization group vs 33.3% in initial medical stabilization group). The benefit of early revascularization was apparent across a wide time window, extending up to 54 h after MI and 18 h after shock onset. Based on this data, STEMI patients who present with acute cardiogenic shock should undergo emergency cardiac catheterization and revascularization. This is especially true for patients younger than 75 years.
ROUTINE EARLY ANGIOGRAPHY AFTER SUCCESSFUL FIBRINOLYTIC THERAPY
In the Grup de Analisis de la Cardiopatia Isquemica Aguda trial[115], 500 patients with STEMI that were treated with recombinant tissue plasminogen activator were randomly assigned to angiography and coronary intervention if indicated within 24 h of thrombolysis, or to an ischemia-guided conservative approach. The primary endpoint of combined rate of death, reinfarction, or revascularization at 12 mo occurred in 9% of the angiography and intervention group compared to 21% in the conservative group (P = 0.0008). There was a trend towards reduced rates of death or reinfarction (7% vs 12%, P = 0.07). There were no differences in major bleeding or vascular complications.
In the Trial of Routine Angioplasty and Stenting after Fibrinolysis to Enhance Reperfusion in Acute Myocardial Infarction[116], 1059 high-risk patients who had a STEMI received FT at centers not capable of performing P-PCI were randomized to either standard treatment (including rescue PCI, if required, or delayed angiography) or immediate transfer to another hospital and PCI within 6 h after fibrinolysis. At 30 d, the primary composite endpoint of death, reinfarction, recurrent ischemia, new or worsening congestive heart failure, or cardiogenic shock occurred in 11.0% of PCI and in 17.2% of the patients assigned to standard treatment (P = 0.004). There was no evidence of increased major bleeding with the early invasive strategy.
In the Norwegian Study on District Treatment of ST-Elevation Myocardial Infarction trial[117] 266 patients with acute STEMI living in rural areas, where the transfer time to P-PCI are greater than 90 min, were initially treated with the combination of tenecteplase, aspirin, enoxaparin, and clopidogrel and were randomized to immediate transfer for P-PCI or to standard management in the local hospitals with early transfer, only if indicated for rescue or clinical deterioration. The primary outcome of composite of death, reinfarction, stroke, or new ischemia at 12 mo occurred in 21% vs 27% in the early invasive group and the conservative treatment group respectively (P = 0.19). Although this study failed to demonstrate a statistically significant difference between the 2 treatment groups in the incidence of the primary composite endpoint, the incidence of death, recurrent MI, or stroke was significantly lower in the immediate-transfer group. The risk reduction was similar to that reported for high-risk patients in the Trial of Routine Angioplasty and Stenting after Fibrinolysis to Enhance Reperfusion in Acute Myocardial Infarction.
In a meta-analysis by Borgia et al[118] that included 2961 patients from 7 trials, early PCI after successful fibrinolysis reduced the rate of re-infarction (P = 0.003), the combined endpoint death/re-infarction (P = 0.004) and recurrent ischemia (P < 0.001) at 30-d. There was no evidence of an increase in patient major bleeding or stroke.
In the recent Strategic Reperfusion Early After Myocardial Infarction trial[119], 1892 patients with STEMI who presented within 3 h of symptom onset who were unable to undergo primary PCI within 1 h, were randomly assigned to undergo either primary PCI or fibrinolytic therapy with bolus tenecteplase (half dose in patients ≥ 75 years of age), clopidogrel, and enoxaparin before transport to a P-PCI capable hospital. Emergency coronary angiography was performed only if fibrinolysis failed, which occurred in 36.3% of the patients; otherwise, angiography was performed 6 to 24 h after randomization. The primary composite end point of death, shock, congestive heart failure, or reinfarction within 30 d occurred in 12.4% of the patients in the fibrinolysis group and in 14.3% in the primary PCI group (P = 0.21). In patients who did not undergo primary PCI within one hour of medical contact, pre-hospital fibrinolysis with coronary angiography with a median time = 17 h resulted in effective reperfusion. The incidence of intracranial bleeding was higher with FT when compared to PCI (1.0% vs 0.2% P = 0.04).
Based on these studies, in STEMI patient who are treated successfully with FT, cardiac catheterization can be considered as part of a routine pharmacoinvasive or ischemia-guided approach > 24 h after administration of FT. Very early cardiac catheterization and PCI within 2-3 h after the administration of (FT) increases the risk of bleeding. Very early (< 2-3 h) invasive approach should be utilized for patients who require rescue PCI.
FACILITATED PCI
Fibrinolytic agents use as adjunct to primary PCI has been studied. This approach is called facilitated PCI. Full dose or half dose of a fibrinolytic agent is administered with or without glycoprotein IIb/IIIa (GP IIb/IIIa) inhibitor prior to planned PCI. This approach is based on the assumption that pre PCI pharmacotherapy will facilitate higher and faster rates of reperfusion.
The Assessment of the Safety and Efficacy of a New Treatment Strategy for Acute Myocardial Infarction trail[120] was stopped prematurely because of an increased mortality associated with facilitated PCI. In the Facilitated Intervention with Enhanced Reperfusion Speed to Stop Events trial[121], patients were randomized to primary PCI or facilitated PCI with abciximab or facilitated PCI with half-dose reteplase and full-dose abciximab. Although the rates of death, heart failure, and ischemic outcome at 90 d for all three groups were similar, there was increased rate of major bleeding with the facilitated strategies. Because of these findings, facilitated PCI is currently not advised.
PRIMARY PCI
Timely reperfusion with primary PCI (P-PCI) by experienced operators at an experienced center is superior to FT. Compared to FT, P-PCI results in higher rates of infarct related artery patency, higher rates of TIMI 3 flow and lower rates of complications such as recurrent ischemia, reinfarction, emergency repeat revascularization procedures, intracranial hemorrhage (ICH), and death. However, P-PCI is associated with increased rates of access site bleeding complications[122]. In addition, PCI can result in the “no reflow” phenomenon where the myocardial perfusion is inadequate despite restoration of TIMI 3 epicardial flow in the infarct related artery. No reflow phenomenon is due to a combination of endothelial injury, edema, atheroembolization, vasospasm, and myocyte reperfusion injury and inflammation[123]. Occurance of no reflow is associated with with increased mortality[123]. Multiple treatment strategies that included the use of GP IIb/IIIa antagonists, nitroprusside, verapamil, adenosine, nicorandil, pexelizumab have not shown promising results[123].
The benefits of P-PCI over FT are time sensitive. Door to balloon (D2B) times greater than 90-120 min can eliminate the benefits of P-PCI over FT[124]. Over the past ten years, there has been a significant reduction in the median D2B times. Although approximately 80% of the United States population lives within one hour from a P-PCI capable hospital, the majority of patients in the rural areas do not have access to such facilities. A significant increase in the number of PCI capable hospitals from 2001 to 2006 result in minimal increase in the overall patient access to such facilities[125,126]. One of the strategies to make P-PCI more accessible is to allow hospitals without onsite cardiac surgery facilities to perform PCI procedures. The Cardiovascular Patient Outcomes Research Team trail[127] showed that primary PCI can be performed safely and rapidly at hospitals without cardiac surgery back-up. Other strategies include bypassing the non PCI hospital and transferring the patients to a primary PCI capable hospital where the care and transfer protocols are standardized. These strategies have been shown to extend P-PCI to more patients and result in better patient outcomes[127-129].
DELAYED PRESENTATION
In patients presenting more than 12 h after the onset of symptoms, cardiac catheterization and PCI should be considered in the setting of ongoing chest pain, cardiogenic shock, acute severe heart failure, or spontaneous or provoked myocardial ischemia.
In the Occluded Artery Trial[130], 2166 patients with occluded infarct related arteries who presented 3-28 d after myocardial infarction and had ejection fractions less than 50% were randomized to PCI vs conservative medical therapy. The 4-year cumulative primary event rate was 17.2% in the PCI group and 15.6% in the medical therapy group (P = 0.20). However, patients with high risk features such as New York Heart Association class III-IV, rest angina, high risk stress test, left main or three vessel diseases were excluded from the trial. The trail showed that routine PCI did not reduce the occurrence of death, reinfarction, or heart failure, and there was a trend toward excess reinfarction during 4 years of follow-up in stable patients with occlusion of the infarct-related artery 3 to 28 d after myocardial infarction. Based on this data, in patients who present more than 12 h after their symptom onset and are clinically stable, routine cardiac catheterization and PCI are not advised.
PCI OF THE NON-INFARCT RELATED ARTERY
In patients presenting with STEMI, multivessel coronary artery disease is frequently seen and is associated with poor outcomes[131]. PCI of a non-infarct related artery prior to discharge from the hospital, at a time that is separate from the index STEMI related PCI, is indicated if there is evidence of spontaneous myocardial ischemia. However, this practice is largely based on non-randomized cohort studies[132-134]. The role of fractional flow reserve (FFR) at the time of STEMI, to evaluate the functional significance of a non-infarct related artery is not well established. In a small study by Ntalianis et al[135], FFR was useful in evaluating the functional significance of a non-culprit coronary lesion.
In the recent Preventive Angioplasty in Acute Myocardial Infarction trail[136], 465 patients with acute STEMI who were undergoing primary PCI were randomly assigned to either preventive PCI defined as immediate PCI of any lesion with > 50% stenosis or no preventive PCI. The trial was stopped early by the data safety monitoring board. In an intention to treat analysis, the primary composite endpoint of death from cardiac causes, nonfatal myocardial infarction, or refractory angina occurred in 9% of the preventive PCI arm and 23% of the non-preventive PCI arm, respectively (P = 0.001). It should be noted that the trail excluded patients with concomitant disease in the left anterior descending and left circumflex arteries, patients with > 50% stenosis of the left main artery, patients with prior CABG and patient with a non-culprit artery with a chronic total occlusion.
At this time, PCI of a non-infarct related artery should be performed prior to hospital discharge if the patient has evidence of spontaneous or provocable myocardial ischemia.
PCI TECHNIQUE BASED STRATEGIES
During the past decade, we have seen significant advances in the field of interventional cardiology as it relates to the management of acute myocardial infarction. Some of the frequently debated issues include access site (radial vs femoral), routine use of aspiration thrombectomy, and bare-metal vs drug eluting stents.
Access site
Transradial PCI had gained widespread acceptance and is now used routinely for elective angioplasty. Major advantages with transradial approach include reductions in bleeding complications and length of hospitalizations and improved quality of life. Given these advantages, transradial PCI during STEMI has been extensively studied. Multiple randomized trials and a large meta-analysis showed that transradial primary PCI is associated with significant reduction in access site complications. In the Radial vs femoral access for coronary angiography and intervention in patients with acute coronary syndromes trial[137] 7021 patients with STEMI were randomly assigned to radial vs femoral access sites. The primary endpoint of death, myocardial infarction, stroke, or non-CABG-related major bleeding at 30 d occurred in 3.7% and 4.0% of the radial access and femoral access patients respectively (P = 0.5). In a pre-specified subgroup analysis, non-CABG-related major bleeding at 30 d occurred in 24 patients in the radial group compared with 33 patients in the femoral group (P = 0.23). At 30 d, 42 of 3507 patients in the radial group had large hematomas compared with 106 of 3514 in the femoral group (P < 0.0001). In the Radial vs Femoral Randomized Investigation in ST Elevation Acute Coronary Syndrome[138,139] trial, 1001 STEMI patients undergoing primary/rescue percutaneous coronary intervention were randomized to the radial or femoral approach. The primary endpoint of cardiac death, stroke, myocardial infarction, target lesion revascularization, and bleeding at 30 d occurred in 13.6% in the radial artery group and 21.0% in the femoral artery group (P = 0.003). Radial access was associated with significantly lower rates of cardiac mortality (5.2% vs 9.2%, P = 0.020), bleeding (7.8% vs 12.2%, P = 0.026), and shorter hospital stay. In the STEMI-RADIAL trail[103] 2959 patients undergoing primary PCI within 12 h of onset of symptoms were randomized to radial vs femoral approach. The primary endpoint of access site complications and bleeding occurred in 7.2% of the femoral vs 1.4% of the radial group (80% relative risk reduction, P = 0.001). Radial and femoral approaches are both safe and effective for PCI. Lower rates of local vascular complications may be a reason to use the radial access approach. There is some concern about longer D2B times and increased radiaton exposure with radial artery access. This is mostly limited to low volumes centers and operators[140,141]. Data from the randomized control trials suggests that D2B times and the cumulative radiation dose are minimally increased with radial artery catheterization. The impact of the radial artery approach on patient mortality remains unclear at this time as the reported studies are underpowered to evaluate this end-point.
Adjunctive thrombectomy
A vast majority of patients with STEMI have large thrombus burden. It seems intuitive that thrombectomy may improve epicardial coronary flow, prevent distal embolization, reduce microvascular obstruction and the no-reflow phenomenon. However, trials that have used mechanical thrombectomy have been largely negative without any improvement in myocardial blush grade, final infarct size and overall left ventricular ejection fraction[142-144]. Recently there has been renewed interest in aspiration thrombectomy. In the Thrombus Aspiration during Percutaneous coronary intervention in Acute myocardial infarction Study[145], 1071 patients were randomly assigned to the thrombus-aspiration group or the conventional-PCI group before undergoing coronary angiography. The primary end point of myocardial blush grade of 0 or 1 occurred in 17.1% of the patients in the thrombus-aspiration group and in 26.3% in the conventional-PCI group (P < 0.001). At one year follow up, cardiac death occurred in 3.6% of the patients in the thrombus aspiration group and 6.7% in the conventional PCI group (P = 0.020). In the Impact of Thrombectomy With Export Catheter in Infarct-Related Artery During Primary Percutaneous Coronary Intervention trail[146], 155 STEMI patients were randomly assigned to standard percutaneous coronary intervention PCI (n = 87) or aspiration thrombectomy guided PCI (n = 88). The primary end points of myocardial blush grade ≥ 2 and the rate of 90-min ST-segment resolution > 70% occurred more frequently in the thrombectomy guided PCI group (88% vs 60%, P = 0.001; and 64% vs 39%, P = 0.001). In a meta-analysis conducted by Bavry et al[147], total of 30 studies with 6415 patients were included, a weighted mean follow-up of 5.0 mo showed that the morality was 3.2% for the adjunctive thrombectomy group vs 3.7% for conventional PCI.
In the recently published TASTE[148] (The Thrombus Aspiration in ST-Elevation Myocardial Infarction in Scandinavia) trial, aspiration thrombectomy did not show reduction in 30 d mortality. The event rate was 2.8% in the aspiration arm vs 3.0% in the routine PCI arm (P = 0.63). The recently published TOTAL [A Trial of Routine Aspiration Thrombectomy With Percutaneous Coronary Intervention (PCI) vs PCI Alone in Patients With ST-Segment Elevation Myocardial Infarction (STEMI) Undergoing Primary PCI] trial[149] 10732 patients with ST-segment elevation myocardial infarction (STEMI) undergoing primary PCI were randomized to routine upfront manual thrombectomy versus PCI alone. Within 180 days, manual aspiration thrombectomy did not lower the rates of cardiovascular death, recurrent myocardial infarction, cardiogenic shock, or NYHA class IV heart failure. Stroke within 30 d occurred in 33 patients (0.7%) in the thrombectomy group vs 16 patients (0.3%) in the PCI-alone group (HR = 2.06; 95%CI: 1.13-3.75; P = 0.02).
The TASTE and the TOTAL Trials suggest that routine use of aspiration thrombectomy may not be beneficial in reducing patient morbidity and mortality.
TYPE OF STENTS IN THE SETTING OF PRIMARY PCI
It is now a routine practice to use coronary stents during primary PCI. Compared to balloon angioplasty, primary PCI with bare metal stents (BMS) has been shown to reduce the rates of reinfarction and target vessel revascularization. However, this does not translate into a reduction in mortality[150]. Drug eluting stents (DES) are currently being used for both elective and primary PCI. DES when compared with BMS significantly reduces restenosis rates and the need for reintervention but does not definitively reduce rates of death[151]. First generation DES such as Taxus and Cypher, when compared to BMS, can increase the risk of very late stent thrombosis[152]. Newer generation DES such as Xience, Promus and Endeavour, when compared to BMS do not increase the risk of acute or late stent thrombosis. Cobalt-chromium based everolimus eluting stents have the lowest reported rates of stent thrombosis[153]. In the Xience or Vision Stents for Management of Angina in the Elderly trail[154], second generation, everolimus eluting DES were safely used in the elderly without increasing the risk of bleeding. Patients who are taking oral anticoagulation and present with a STEMI pose a significant challenge. Triple therapy significantly increases the risk of bleeding. In the What is the Optimal antiplatelet and anticoagulant therapy in patients with oral anticoagulation and coronary stenting trial[155], the group receiving warfarin plus clopidogrel had lower bleeding complications compared with the group receiving warfarin, clopidogrel and aspirin. Although the rate of stent thrombosis was not increased, this trial was not powered to evaluate the risk of stent thrombosis.
Given the advantages of marked reduction in the rates of restenosis, target vessel and target lesion revascularization and very low rates of late stent thrombosis, second generation DES should be the preferred choice during primary PCI. However, that decision should be made on a case to case basis. Factors such as bleeding risk, other indications for systemic oral anticoagulants, socioeconomic status, compliance, need for surgical procedures during the following one year should be considered. If these factors are a concern, DES implantation should be avoided. There still remain gaps in our understanding of routine use of DES in the elderly and patients who are on oral anticoagulants. Further research is need in these areas.
ADJUNCTIVE PHARMACOTHERAPY BASED STRATEGIES
In recent years, there has been extensive research done in the area of adjunctive pharmaco-therapy. As a result, we now have multiple antithrombotic and anti-platelet agents that have been shown to reduce major adverse cardiac events in the setting of STEMI.
Unfractionated heparin (UFH) is time tested and the most familiar of all the agents. It is used frequently. When titrated to appropriate activated clotting times of 250-300 s, it is an acceptable strategy. Low molecular weight heparins (LMWN) such as Enoxaparin and Fondaparinux are not well studied in the setting of STEMI. In the STEMI Treated With Primary Angioplasty and Intravenous Lovenox or Unfractionated Heparin trial[156] 901 patients were randomized to treatment with enoxaparin (n = 450) or unfractionated heparin (n = 460). The composite primary endpoint of 30-d incidence of death, complication of myocardial infarction, procedure failure, or major bleeding occurred in 126 (28%) patients after anticoagulation with enoxaparin vs 155 (34%) patients on unfractionated heparin (P = 0.06). Data from this trail suggests that enoxaparin can be safely and effectively used in patients with STEMI. In the OASIS-6 trial[157] death or reinfarction at 30 d was significantly reduced from 11.2% in the control group to 9.7% patients in the fondaparinux group (P = 0.008). However, fondaparinux was associated with higher rates of catheter thrombosis. At this time, fondaparinux in not used as an anticoagulant in the setting of primary PCI.
The role of Bivalirduin in the setting of STEMI treated with primary PCI was tested in the Harmonizing Outcomes with Revascularization and Stents in Acute Myocardial Infarction trial[158]. Three thousand six hundred and two patients with ST-segment elevation myocardial infarction presenting within 12 h after the onset of symptoms and were undergoing primary PCI, were randomly assigned to treatment with heparin plus a glycoprotein IIb/IIIa inhibitor or to treatment with bivalirudin alone. Primary end points of major bleeding and combined adverse clinical events, including death, reinfarction, target-vessel revascularization for ischemia, and stroke within 30 d occurred in 22% of the heparin plus glycoprotein IIb/IIIa inhibitor group vs 9.2% in the bivalirudin group (P = 0.005). The risk of acute stent thrombosis within 24 h in the bivalirudin group increased, but no significant increase was present by 30 d. This was most likely secondary to a combination of adenosine diphosphate–induced platelet activation before maximal thienopyridine blockade of the platelet P2Y12 receptor or by residual thrombin activity after the discontinuation of bivalirudin. Based on the results from the HORIZONS-AMI trail, it is a reasonable approach to use bivalurudin in patients with STEMI who are undergoing primary PCI. This approach may provide long term survival benefit by lowering the rate of bleeding complications.
ADJUNCTIVE ANTIPLATELET THERAPY
Aspirin
An initial single dose of 325 mg of Aspirin should be administered as early as possible. This should be followed by a maintenance dose of 81 mg once daily. Higher doses of Aspirin for maintenance therapy have shown to increase the risk of bleeding. In the Committee members of the Clopidogrel and Aspirin Optimal Dose Usage to Reduce Recurrent Events-Seventh Organization to Assess Strategies in Ischemic Syndromes trial[159] 25086 patients with an acute coronary syndrome who underwent cardiac catheterizatoin were randomized to either double-dose clopidogrel (a 600-mg loading dose on day 1, followed by 150 mg daily for 6 d and 75 mg daily thereafter) or standard-dose clopidogrel (a 300-mg loading dose and 75 mg daily thereafter) and either higher-dose aspirin (300 to 325 mg daily) or lower-dose aspirin (75 to 100 mg daily). The primary outcome of cardiovascular death, myocardial infarction, or stroke at 30 d was not different between higher-dose and lower-dose aspirin (4.2% vs 4.4%, P = 0.61) or major bleeding (2.3% vs 2.3%, P = 0.90).
Clopidogrel
The importance of at least 12 mo of dual antiplatelet therapy with aspirin and clopidogrel in the setting of ACS with and without PCI has been well established based on the data from the Clopidogrel in Unstable Angina to Prevent Recurrent Event (CURE)[160] and PCI-CURE[161] trials. A 600 mg loading dose of clopidogrel offers rapid platelet inhibition compared to 300 mg dose[162]. In the CURRENT-OASIS 7 trail[159] the primary outcome of cardiovascular death, myocardial infarction, or stroke at 30 d occurred in 4.2% of the double-dose clopidogrel group vs 4.4% in the standard-dose clopidogrel (P = 0.30). Major bleeding occurred in 2.5% of the double-dose group and in 2.0% in the standard-dose group patients (P = 0.01). Rates of stent thrombosis was lower in the double dose group (1.6% vs 2.3% P = 0.001). Incidence of major bleeding was 2.5% in the double dose group vs 2.1% in the standard dose group (P = 0.001). Clopidogrel 600 mg loading dose followed by 75 mg once daily for at least one year should be considered for all patients with acute coronary syndromes.
One common clinical concern with the use of clopidogrel is the variable therapeutic response. This is secondary to multiple factors such as diabetes, obesity, polymorphisms in enteric ABCB 1 and hepatic cytochrome P450 (CYP450) enzymes (CYP2C19*2) and drug interaction that interferes with the metabolism of clopidogrel. Nearly 30% of patients have a reduced functional allele of CYP2C19*2. This has been shown to be associated with decreased levels of the active metabolite of clopidogrel, suboptimal platelet inhibition and increased rates of major adverse cardiac events and stent thrombosis[162-165]. Based on this data, the United States Food and Drug Administration made changes to clopidogrel’s prescribing information noting the potential impact of CYP2C19 genotype on clopidogrel’s bioavailability and clinical response. However, in a study by Mega et al[166] homozygotes and heterozygotes for loss of functional allele had similar rates of primary efficacy outcomes. At this time routine testing for CYP2C19*2 polymorphisms is not indicated. Further studies are needed to fully understand the clinical risk associated with these polymorphisms and to develop effective treatment strategies.
Proton-pump inhibitors, such as omeprazole, have been shown to interfere with clopidogrel metabolism resulting in decreased antiplatelet effect[167]. However, this does not lead to worse clinical outcomes[168]. At this time there is no strong evidence to avoid concomitant use of PPIs, when clinically indicated, in patients receiving clopidogrel.
Prasugrel
Prasugrel is a thienopyridine class of drug that competiviely antagonizes the P2Y12 receptor. Similar to Clopidogrel, it is also a pro drug that requires biologic conversion to an active metabolites. In the Trial to Assess Improvement in Therapeutic Outcomes by Optimizing Platelet Inhibition with Prasugrel trial[169] 13608 patients with moderate-to-high-risk acute coronary syndromes treated with early invasive approach were randomly assigned to prasugrel, with a 60-mg loading dose and a 10-mg daily maintenance dose, or clopidogrel, with a 300-mg loading dose and a 75-mg daily maintenance dose, for 6 to 15 mo. The primary efficacy end-point of death from cardiovascular causes, nonfatal myocardial infarction, or nonfatal stroke occurred in 12.1% of patients receiving clopidogrel and 9.9% of patients receiving prasugrel (P < 0.001). There was significant reductions in the rates of myocardial infarction (9.7% for clopidogrel vs 7.4% for prasugrel; P < 0.001), urgent target-vessel revascularization (3.7% vs 2.5%; P < 0.001), and stent thrombosis (2.4% vs 1.1%; P < 0.001). Major bleeding was increased with prasugrel 2.4% in comparison with 1.8% of patients with clopidogrel (P = 0.03). The prasugrel group had higher rates of life-threatening bleeding (1.4% vs 0.9%; P = 0.01), including nonfatal bleeding (P = 0.23) and fatal bleeding (0.4% vs 0.1%; P = 0.002). While prasugrel significantly reduced the rates of ischemic events and stent thrombosis, it increased the risk of major bleeding and did not reduce mortality. The benefits of prasugrel must be carefully weighed against the increased risk of bleeding. Prasugrel may be a preferred agent in younger, high risk acute coronary syndrome patients with large area of myocardium at risk and low bleeding risk. Prasugrel should not be used in patients with history of prior stroke, transient ischemic attacks, age greater than or equal 75, or body weight less than 60 kg. A lower dose of prasugrel 5 mg once daily has been suggested in patients who are at higher risk for bleeding. However, prasugrel 5 mg/d has not been prospectively studied.
Ticagrelor
Ticagrelor is a cyclopentyl triazolo pyrimidine that acts on the platelet P2Y12 receptor as an antagonist. It does not require conversion to active metabolite and is a reversible agent. In The Study of Platelet Inhibition and Patient Outcomes trail[170] 18624 patients with acute coronary syndromes, were randomized to ticagrelor (180-mg loading dose, followed by 90 mg twice daily) or clopidogrel (300-to-600-mg loading dose, followed by 75 mg daily). Thirty-five percent of the patients had STEMI. Overall, at 12 mo, the composite end-point of death from vascular causes, myocardial infarction, or stroke occurred in 9.8% of patients receiving ticagrelor vs 11.7% of patients receiving clopidogrel (P < 0.001). The rate of death from any cause was also reduced with ticagrelor (4.5% vs 5.9%, P < 0.001). In addition, there were reductions in the rates of myocardial infarction (5.8% in the ticagrelor group vs 6.9% in the clopidogrel group, P = 0.005) and death from vascular causes (4.0% vs 5.1%, P = 0.001). There was no difference in the frequency of stroke alone (1.5% vs 1.3%, P = 0.22) or the rates of major bleeding (11.6% and 11.2%, P = 0.43). However, ticagrelor was associated with a higher rate of major non CABG related bleeding (4.5% vs 3.8%, P = 0.03), including more instances of fatal intracranial bleeding.
In a pre-specified subgroup analysis of the Study of Platelet Inhibition and Patient Outcomes trail, the net benefit of ticagrelor was smaller in the North American cohort. This was attributed to chance alone or alternatively to the frequent use of higher dose of aspirin for maintenance therapy. Based on this observation, the dose of aspirin when used in combination with ticagrelor for maintenance therapy should not exceed 100 mg a day.
When considering adding a second drug to aspirin for dual antiplatelet therapy (DAPT), the decision should be individualized. The anti-ischemic benefits should be carefully weighed against patient comorbidities, risk of bleeding, need for long term treatment with an oral anticoagulant, cost, compliance, and the possibility of surgical procedures during the following year.
DURATION OF ANTIPLATELET THERAPY
Current guidelines[171] support uninterrupted use of dual antiplatelet therapy for at least one year in post ACS patients regardless of invasive or conservative treatment or the type of stent (BMS vs DES). Recently, there has been significant data supporting the discontinuation of dual antiplatelet therapy 3 to 6 mo after a PCI in the setting of acute coronary syndrome.
In the Efficacy of Xience/Promus vs Cypher in Reducing Late Loss after Stenting trail[172] 1443 patients undergoing implantation of drug-eluting stents were randomized to receive 6- or 12-mo DAPT. The primary end point of target vessel failure at 12 mo was 4.8% in the 6-mo DAPT group and 4.3% in the 12-mo DAPT group (P = 0.001 for non-inferiority). This study was underpowered for evaluation of death and MI.
In the Prolonging dual antiplatelet treatment after grading stent-induced intimal hyperplasia trial[173] 2013 patients were randomly assigned to receive bare-metal, zotarolimus-eluting, paclitaxel-eluting, or everolimus-eluting stent implantation. At 30 d, patients in each stent group were randomly allocated to receive up to 6 or 24 mo of clopidogrel therapy in addition to aspirin. The primary composite endpoint of death from any cause, myocardial infarction, or cerebrovascular accident at 24 mo was similar.
In the Real Safety and Efficacy of a 3-mo dual antiplatelet Therapy following E-ZES Implantation trail[174], 2117 patients with coronary artery stenosis were randomized to 2 groups according to DAPT duration and stent type: 3-mo DAPT following zotarolimus-eluting stent (E-ZES) implantation vs 12-mo DAPT following the other (sirolimus, everolimus DES implantation). The primary composite endpoint of cardiovascular death, myocardial infarction, stent thrombosis, target vessel revascularization, or bleeding at 1 year occurred in 4.7% patients assigned to E-ZES + 3-mo DAPT compared with 4.7% patients assigned to the standard therapy (P = 0.001 for noninferiority).
In the recently published Optimized Duration of Clopidogrel Therapy Following Treatment With the Endeavor Zotarolimus - Eluting Stent in the Real World Clinical Practice trail[175], 3119 patients undergoing PCI using zotarolimus DES were randomly assigned to 3 mo vs 12 mo of dual antiplatelet therapy. The primary composite end point of all-cause death, myocardial infarction, stroke, or major bleeding occurred in 6.0% vs 5.8%, respectively P = 0.002 for noninferiority.
Although the data from these trials is reassuring and supports the discontinuation of dual anti-platelet therapy at the end of 6 mo, it is important to note that these trial included patients with stable coronary disease and low risk acute coronary syndrome. Caution should be used in extrapolating this data to patients with STEMI. At this time, dual anti-platelet therapy should be continued for at least one year without interruption when tolerated in patients with ACS.
Role of glycoprotein IIb/IIIa receptor antagonists
Role of glycoprotein IIb/IIIa (GP IIb/IIIa) receptor antagonists in the setting of STEMI was extensively studied prior to routine use of dual antiplatelet therapy. Addition of a GP IIb/IIIa receptor antagonist to combination of DAPT plus unfractionated heparin or bivalirudin failed to show benefit[176-178]. However, in a meta-analysis by De Luca[179] where 722 patients with STEMI from seven randomized trials were included, early administration of abciximab compared to late/peri-procedural administration was associated with reduction in mortality (20% vs 24.6% P = 0.02), improvement in pre-procedural (TIMI) 3 flow (21.6% vs 10.1%, P < 0.0001), post-procedural TIMI 3 flow (90% vs 84.8%, P = 0.04), post-procedural myocardial blush grade (52.0% vs 43.2%, P = 0.03), ST-segment resolution (58.4% vs 43.5%, P < 0.0001) and distal embolization (10.1% vs 16.2%, P = 0.02). There was no difference in the rates of major bleeding complications between early and late abciximab administration (3.3% vs 2.3%, P = 0.4). Adjunctive use of GP IIb/IIIa inhibitors can be considered at the time P-PCI if there is evidence of large thrombus or inadequate response to a P2Y12 antagonist[179,180]. Based on the data from the HORIZONS-AMI[158] and CICERO[181] trials, a GP IIb/IIIa receptor antagonist can be used as adjunct to bivalirudin in the presence of large thrombus or for “bail-out use” for procedure related dissection. Similar findings were also confirmed in a recent meta-analysis by Shimada et al[182]. In a recent MI trail[183], intra-coronary infusion of abciximab reduced infarct size at 30 d. This approach should be considered on an individual patient basis[182,183].
ROLE OF CARDIOPROTECTION IN STEMI
Despite significant improvements in every area of STEMI management, adverse event rates continue to be high. Although, reperfusion therapy and the adjunctive pharmacotherapy help reestablish coronary flow, restoration of coronary blood flow can cause further injury to cardiac myocytes. This type of injury is called lethal reperfusion injury. In animal models, close to 50% of the final infarct size is due to lethal reperfusion injury[184]. This injury results from oxidative stress[185,186], calcium overload[187,188], inflammation[189] and rapid restoration of pH[189]. Understanding these mechanisms at a cellular level has led to renewed interest in designing treatment strategies that target pathways that mediate lethal reperfusion injury. These strategies mediate their cardioprotective effect by multiple signaling pathways such as reperfusion injury salvage kinase (RISK) group of protective kinases. The cardioprotective signaling pathways inhibit the mitochondrial permeability transition pore and multiple other molecules[190].
PRECONDITIONING
Repeated, brief episodes of coronary occlusion with myocardial ischemia alternating with coronary reperfusion before a prolonged episode of ischemia, is a powerful way to limit infarct size. This is known as ischemic pre-conditioning[191]. However due to the fact that the brief episodes of ischemia need to be applied prior to an ischemic event, this approach has limited value in the setting of STEMI.
POST CONDITIONING
Applying the principles of preconditioning after the ischemic event has been shown to be beneficial in animal models[192,193]. In a small randomized control trial, Staat et al[194] showed that post-conditioning by 4 cycles of 1-min coronary angioplasty balloon inflations followed by 1 min of balloon deflation within 1 min of coronary reflow after deployment of a coronary stent reduced infarct size and improved myocardial blush grades. Similar findings have also been noted in other small studies that used different balloon inflation and deflation protocols[195]. A significant limitation of catheter/balloon based post-conditioning is that it is limited to cardiac catheterization laboratories at the time of P-PCI.
Post conditioning by cyclosporine
Cyclosporine has been shown to be cardioprotective by inhibiting the mitochondrial permeability transition pore[196]. In a small randomized study of 58 patients, single bolus of 2.5 milligrams of intravenous cyclosporine, compared to placebo reduced infarct size by 40% as quantified by the degree of plasma creatine-kinase elevation[197]. The cardioprotective effect of cyclosporine appears to be promising.
REMOTE ISCHEMIC CONDITIONING
Transient, repeated episodes of ischemia when applied to an organ distant from the heart have been shown to reduce infarct size[198]. This is called remote ischemic conditioning. One proposed mechanism is the release of a chemical by the distant organ that promotes cardiac conditioning. Another possibility is afferent neural pathway stimulation. In a study by Bøtker et al[199], 333 patients with a suspected first STEMI were randomly assigned in a 1:1 ratio to receive P-PCI with or without remote conditioning that consisted of intermittent arm ischemia through four cycles of 5-min inflation and 5-min deflation of a blood-pressure cuff. The patients received remote conditioning during transport to hospital, and P-PCI in hospital. The primary endpoint of myocardial salvage index at 30 d, measured by myocardial perfusion imaging, was significantly improved in the preconditioning group (0.75 in the remote conditioning group vs 0.55 in the control group, P = 0.0333). Given the ease of use and potential universal applicability of this approach, large-scale trials are underway to study this treatment.
ROLE OF ADENOSINE
Adenosine, by mediating its effects via A1 and A3 receptors appears to play a key role in promoting a cardioprotective a state. Although the mechanisms are complex, inhibition of the formation of mitochondrial permeability transition pores appears to be a primary mechanism[200]. Intravenous infusion of adenosine in patients with STEMI was tested in the Acute Myocardial Infarction Study of Adenosine I trail[201]. Although there was 33% relative reduction in the infarct size, this was mostly limited to individuals with large anterior wall MI. Based on this study, the Acute Myocardial Infarction Study of Adenosine II trail[202] randomized 2118 patients to 3-h intravenous infusion of low-dose adenosine (50 μg/kg per minute), high-dose adenosine (70 μg/kg per minute), or placebo before PCI or within 15 min of the initiation of fibrinolysis. There was no difference in the composite endpoint of death, new-onset congestive heart failure, or rehospitalization for congestive heart failure within 6 mo. However, subsequent post-hoc and subgroup analyses showed that there was significant reduction in the infarct size in those who received the high dose and those who received adenosine within 3 h of onset of symptoms[203]. Although the routine use of adenosine is currently not supported, early administration of high dose adenosine may reduce infarct size in patients with anterior wall STEMI with large areas of myocardium at risk.
ROLE OF BETA BLOCKERS
Most of the data on the role of routine use of beta blockers in STEMI either predates or involves thrombolytic therapy. There is very limited data on the cardioprotective benefits of beta blockers in the setting of PPCI. In the recently published Effect of Metoprolol in Cardioprotection during an Acute Myocardial Infarction trail[204], 270 patients with STEMI (Killip Class 2 or less) presenting within 6 h of onset of symptoms were randomized to receive intravenous metoprolol or no metoprolol. The primary endpoint of infarct size by magnetic resonance imaging was smaller after intravenous metoprolol compared with control (25.6 ± 15.3 gm vs 32.0 ± 22.2 gm, P = 0.012). This trail illustrates that a commonly used inexpensive medication may play a significant role in cardioprotection in the setting of reperfusion by P-PCI for STEMI. Larger clinical trials that are powered to analyze hard clinical endpoints are needed to definitively understand the role of intravenous beta blockers in the setting of P-PCI.
The ideal duration of treatment with beta blockers after a STEMI is not well established. At the present time most patients are treated indefinitely with beta blockers after a STEMI. This is mostly based on evidence from a large meta-analysis that included 50000 patients and showed a 23% reduction in mortality at a mean follow up of 1.4 years[205]. Lower rates of reperfusion, suboptimal utilization of medical therapy, and short duration of follow up limit this data.
In a recent meta-analysis by Bangalore et al[206], that included 21000 patients with mean follow up of 44 mo, the primary composite outcome of cardiovascular death, nonfatal MI, or nonfatal stroke in post myocardial infarction patients were not significantly different the group that was treated with β-blockers compared with those who were not. (16.93% vs 18.60% respectively, P = 0.14). At the present time, the data on duration of therapy with beta blockers after an MI in inconclusive. In patients with preserved left ventricular ejection fraction and without any evidence of arrhythmias and ischemia, beta blockers can most likely be stopped after one year.
ROLE OF ATRIAL NATRIURETIC PEPTIDES
The cardioptotective effects of atrial natriuretic peptides (ANP) was tested in the Human Atrial Natriuretic Peptide and Nicorandil as Adjunts to Reperfusion Treatment trail[207]. Following reperfusion by either PCI or fibrinolytic therapy, 569 patients with STEMI were randomized to receive a continuous infusion of ANP or placebo for 3 d. Compared to placebo, there was 14.7% reduction in infarct size by area under the curve for total creatine kinase. ANP infusion was also associated improved ejection fraction at 6 to 12 mo compared with controls (44.7% vs 42.5%). Over a median follow-up time of 2.7 years, cardiac death and rates of hospitalization were also reduced in the ANP group. Further large-scale studies are needed to fully understand the cardioprotective role of ANP.
ROLE OF HYPOTHERMIA
In animal models, moderate hypothermia (28 °C-32 °C) offers cardioprotection by altering signaling pathways[208]. The Cooling as an Adjunctive Therapy to Percutaneous Intervention in Patients With Acute Myocardial Infarction trail[209] failed to show overall statistically significant reduction in infarct size. However, in patients with large anterior STEMI who were cooled to temperatures of less than 35 °C prior to reperfusion there was a reduction in the infarct size (9.3% in treated patients vs 18.2% in controls; P = 0.05).
The Rapid Cooling by Cold Saline and Endovascular Cooling before Reperfusion in patients with ST-elevation Myocardial Infarction trail[210] randomized 20 patients with STEMI undergoing P-PCI to rapid hypothermia by an endovascular catheter or standard therapy. Temperatures < 35 °C were obtained in all hypothermia patients prior to reperfusion. The primary end point of infarct size by cardiac MRI was reduced by 38% in the hypothermia group.
However, in the CHILL-MI[211] trail, hypothermia resulted in only a trend towards reduction in infarct size in patients who presented within 4 h of symptoms onset and were cooled to 33 °C large scale randomized trials are needed to determine if hypothermia during or immediately prior to P-PCI will result in significant reductions in infarct size and clinical endpoints.
STEM CELLS IN THE TREATMENT OF ACUTE MYOCARDIAL INFARCTION
Because atherosclerotic coronary vascular disease is the major cause of death in the United States and has recently become a major cause of death throughout the world, stem cell therapy is being investigated in patients with acute myocardial infarction (AMI) to limit myocardial damage and possibly regenerate myocardium[212-214]. Two populations of stem cells have been examined in patients with myocardial infarctions and/or ischemic cardiomyopathies: adult bone marrow mononuclear cells and cardiac stem cells. Adult bone marrow mononuclear cells from bone marrow aspirates contain approximately 0.5%-3% hematopoietic and mesenchymal “progenitor” cells that secrete growth factors and cytokines that can limit myocardial inflammation and infarct size. These cells have limited ability to replicate, do not transdifferentiate into myocytes, but can chemoattract endogenous patient stem cells for repair of cardiac injury. Cardiac stem cells are specific undifferentiated progenitor cells found in the right atrial appendage and the ventricular apices of the heart that have paracrine effects, can chemoattract patient stem cells, and may transdifferentiate into myocytes for cardiac repair.
The initial ten year experience with autologous human bone marrow mononuclear cells (BMCs) in the treatment of patients with AMIs showed significant approximately 2%-3% (range 1.9%-5.4%) increases in left ventricular ejection fraction (LVEF), decreases in left ventricular end-systolic volume of -4.8 mL (range -1.4 to -8.2 mL) and reductions in myocardial infarction size of approximately 5.5% (-1.9% to -9.1%)[213,214]. These studies established that the direct intramyocardial or intracoronary administration of bone marrow mononuclear cells was safe and that significant side effects did not occur with administration of these cells[213-214], see Tables 5 and 6[215-237]. However many of the initial clinical bone marrow cell studies consisted of small numbers of patients and not all the studies randomized patients to treatment with either bone marrow mononuclear cells or placebo (Tables 5 and 6)[215-237].
Table 5.
Bone marrow and circulating progenitor cells in coronary artery disease patients
| Ref. | n | Randomize | Time post PCI and/or MI | Cell dose | Injection route | Baseline LVEF | LVEF change | Duration | Other findings |
| Assmus et al[215] | 92 | Yes | 2348-2470 d | 22 ± 106 CPC 205 ± 110 × 106 BMC | IC | CPC 39% ± 10% BMC: 41% ± 11% | CPC -0.4% BMC 2.90% | 3 mo | Pts with previous MI; ↑ LVEF in BMC but not CPC |
| Bartunek et al[216] | 35 | Cohort | 10 d | 12.6 ± 2.2 × 106 | IC | 45% ± 2.5% | 7% | 4 mo | ↑ LV regional function, perfusion; restenosis ↑ |
| Chen et al[217] | 69 | Yes | 18.4 ± 0.5 d | 8-10 × 109 | IC | 49% ± 9% | 18% | 6 mo | ↑ LVEF by ventriculogram ↑ perfusion; ↓ ESV |
| Erbs et al[218] | 26 | Yes | 225 ± 87 d | 69 ± 14 × 106 | IC | 51.7% ± 3.7% | 7.20% | 3 mo | Pts with chronic CAD occlusion Rxed with CPC; ↓ EF by MRI; infarct size 16% |
| Ge et al[219] | 20 | Yes | 1 d | 39 ± 22 × 106 | IC | 53.8% ± 9.2% | 4.80% | 6 mo | ↑ Perfusion by SPECT |
| Hendrikx et al[220] | 20 | Yes | 217 ± 162 d | 60 ± 31 × 106 IM | IM | 42.9% ± 10.3% | 5% | 4 mo | CABG in Pts with previous CAD ↑ Regional but not global LV function; 6/9 with induced ventricular tachycardia |
| Janssens et al [221] | 67 | Yes | 1 d | 172 × 106 | IC | 48.5 ± 7.2 | 3.30% | 4 mo | ↓ Infarct size |
| Kang et al[222] | 96 | Yes | < 14 d AMI; > 14 d OMI | 1-2 × 109 | IC | 52.0 ± 9.9 | 5.10% AMI | 6 mo | G-CSF for 3 d; ↓ ESV and infarct size in AMI; = EF, ESV and infarct size in OMI |
| Katritsis et al[223] | 22 | Cohort | 224 ± 464 d | 2-4 × 106 | IC | 39.7% ± 9.3% | 1.60% | 4 mo | ↑ Regional but not global LV function |
| Lunde et al[224,225] | 100 | Yes | 6 ± 1.3 d | 68 × 106 (median) 54-130 × 106 | IC | 41.3 ± 11.0 | = | 6-12 mo | ↑ LVEF in treated and controls; = EDV and infarct size |
| Meyer et al[226] | 60 | Yes | 4.8 ± 1.3 | 24.6 ± 9.4 × 108 | IC | 50 ± 10 | 5.90% | 18 ± 6 mo | ↑ LVEF by MRI significant at 6 but not 18 mo |
| Mocini et al[227] | 36 | Cohort | AMI < 6 mo | 292 ± 232 × 106 IM | IM | 46% ± 6% | 5% | 3-12 mo | CABG in all; troponin increased |
| Perin et al[228] | 20 | Cohort | ICM | 25.5 ± 6.3 × 106 | IM Trans-Endo-cardial | 30% ± 6% | 5.10% | 12 mo | LVEF = Controls; ↑ LV perfusion ↑ Exercise |
| Ruan et al[229] | 20 | Yes | Approximately 1 d | NR | IC | 53.5% ± 5.8% | 5.80% | 6 mo | ↑ LV segmental contraction |
| Schächinger et al[230,231] | 204 | Yes | 3-8 d | 2.4 × 108 | IC | 48.3% ± 9.2% | 6%-7% | 4-12 mo | ↑ EF when Rx > 4 d post MI and when EF ↑ ≤ 48.9; LV perfusion |
| Strauer et al[232] | 20 | Cohort | 5-9 d | 2.8 ± 2.2 × 107 IM | IC | 57% ± 8% | 5% | 3 mo | ↑ Regional but not global LVEF; ↓ ESV and ↓ Infarct size |
| Li et al[234] | 70 | Yes | 7 ± 5 d | 7.3 ± 7.3 × 107 | IC | 50% ± 8.2% | 7% | 6 mo | G-CSF for 5 d; ↓ LV ESV, ↓ LV wall motion score |
NR: Not recorded or equals no change; CPC: Circulating progenitor cells; BMC: Bone marrow cells; ICM: Ischemic cardiomyopathy; IC: Intracoronary injection; IM: Intramyocardial injection; AMI: Acute myocardial infarction; OMI: Old myocardial infarction; G-CSF: Granulocyte colony stimulating factor; ESV: LV end-systolic volume; SPECT: Single photon emission computer tomography. Adapted from Henning[213].
Table 6.
Stem cells in the treatment of patients with acute myocardial infarction
| Ref. | n | Random-ized | Time post MI | Cell dose | Baseline | LVEF | Duration | Other findings |
| Strauer et al[232] | 20 | Cohort | 8 d | 2.8 ± 2.2 × 107 | 57% ± 8% | 5% | 3 mo | ↑ Regional but not global LVEF ↓ LV ESV and infarct size |
| Bartunek et al[216] | 35 | Cohort | 10 d | 12.6 ± 2.2 × 106 | 45% ± 2.5% | 7% | 4 mo | ↑ LV regional function, ↑ perfusion; ↑↑ restenosis |
| Li et al[234] | 70 | Yes | 6 d | 7.3 ± 7.3 × 107 | 50 ± 8.2 | 7% | 6 mo | ↓ LV ESV, LV wall motion score |
| Janssens et al[221] | 67 | Yes | 1 d | 172 × 106 | 48.5 ± 7.2 | 3.30% | 4 mo | ↓ Infarct size |
| Meyer et al[226] and Wollert et al[237] | 60 | Yes | 4.8 d | 24.6 × 108 | 50.0 ± 10.0 | = | 6-18 mo | ↑ LVEF at 6 but not at 18 mo |
| Kang et al[222] | 96 | Yes | 4 d | 1-2 × 109 | 52.0 ± 9.9 | 5.1% AMI | 6 mo | ↓ LV ESV and infarction in acute MI; = ESV and = old MI |
| Lunde et al[224,225] | 100 | Yes | 6 d | 68 × 106 | 41.3 ± 11.0 | = | 6-12 mo | LVEF ↑ in treated and controls; = EDV and infarct size |
| Ge et al[219] | 20 | Yes | 1 d | 4 × 107 | 53.8 ± 9.2 | 4.80% | 6 mo | ↑ LV regional wall perfusion by SPECT |
| Meluzín et al[235,236] | 66 | Yes | 5-9 d | 107-108 | 42 ± 0.0 | 3-5 | 3-12 mo | ↑ LVEF 3% @107 ↑ LVEF 5%-7% @ 108 3-12 mo |
| Schächinger et al[230,231] | 204 | Yes | 3-8 d | 2.4 × 108 | 48.3 ± 9.2 | 6-7 | 4-12 mo | ↑ EF when Rx > 4 d post MI and when EF < 48.9%; ↑ LV perfusion |
Adapted from Henning[213]. MI: Myocardial infarctions; LVEF: Left ventricular ejection fraction.
Since the initial treatment of patients with AMIs with BMCs, major questions have persisted about the use of these cells: what is the optimal cell for AMI treatment; when is the optimal time to inject cells for treatment; what is the viability of the stem cells prior to injection into patients; what is the best parameter to monitor cardiac patients after stem cell treatment. The LateTIME, the TIME, and the Swiss Myocardial Infarction Trials were multi-center trials that addressed the questions whether adult BMCs limit myocardial damage in comparison with patients treated with placebo and what is the optimal time of cell administration after AMIs.
LATETIME TRIAL
The LateTIME trial was a randomized double blind, placebo-controlled trial designed to determine if delivery of adult BMCs two to 3 wk after primarily anterior wall myocardial infarction would be safe and effective in limiting infarct size and improving left ventricular (LV) function[238]. All patients in this study were successfully treated initially with primary percutaneous coronary intervention (PCI) within a median time of 4 h after the onset of chest pain. Bone marrow mononuclear cells were isolated from bone marrow aspirates in each center with a closed, automated system (Sepax, Biosafe). The Infarct volume and LV global and regional LV function were measured by magnetic resonance imaging (MRI) with gadolinium prior to intracoronary injection and 6 mo after injection. The LVEF prior to intracoronary infusion of cells or placebo in 87 AMI patients averaged 48.7% in the bone marrow cell (BMC) group and 45.3% in the placebo group. 150 × 106 autologous BMCs or placebo were infused in 87 patients. The changes between baseline and 6 mo in the BMC group for infarct volume, LVEF, wall motion in the infarct zone, and wall motion in the border zone of the infarction were not statistically different from the placebo group[238].
TIME TRIAL
The TIME Trial was a double-blind, placebo controlled trial that investigated the intracoronary administration of autologous BMCs or placebo in 120 patients three or seven days after primarily anterior AMI[239]. The TIME Trial was based on the REPAIR AMI trial that reported that delivery of BMCs to patients 5 to 7 d after AMI resulted in a 5.1% absolute increase in LVEF[239,240].
All patients had successful coronary reperfusion with coronary angioplasty within a median time of 3-4 h of the onset of ischemic symptoms. The mean LVEF in these patients was ≤ 45% by echocardiography. The mean time from PCI to bone marrow aspiration and cell processing was 3.3 d in the day 3 group and 7.4 d in the day 7 group. Bone marrow mononuclear cells were isolated in each center with a closed, automated system (Sepax, Biosafe) and the cells or placebo were infused into the coronary arteries within 12 h of aspiration and cell processing. The BMC contained 2.3% CD34 and 1.1% CD34 plus CD131 hematopoietic cells. All patients had baseline cardiac MRIs with gadolinium at day 3 or at day 7 after AMI and the MRIs were repeated at 6 mo after the AMI.
Forty-three patients received BMCs on day 3 and 36 patients received bone marrow cells on day 7 after AMI. Each patient received approximately 147 × 106 BMCs within 12 h of aspiration and cell processing. Forty-one patients received a placebo. The median time from bone marrow aspiration to infusion directly into the infarct related coronary artery was 8.3 h. In addition, all patients received heparin during the procedure as well as aspirin and clopidogrel.
The differences between the BMC treatment and the placebo treatment in the 3 d group and in the 7 d group were not significant. When both BMC groups were combined (n = 75) to include patients with MRI measurements at baseline and 6 mo and compared with the combined placebo group (n = 37), LVEF in the BMC group increased from 45.2% at baseline to 48.3% at 6 mo while in the combined placebo group the LVEF increased from 44.5% to 47.8% (P = NS). Moreover, there was no significant difference between the changes in regional wall motion in the infarct zone and the border zone between BMC and placebo groups. Infarct volumes uniformly decreased in both groups but the differences between groups were not statistically significant. No difference was observed in global or regional function in patients stratified by myocardial ischemic time.
SWISS MULTICENTER INTRACORONARY STEM CELL STUDY IN ACUTE MYOCARDIAL INFARCTION TRIAL
The Swiss Study[241] randomized patients with AMIs with LVEF < 45% as measured by ventriculography or echocardiography, who had been successfully treated with PCI of the infarct related artery within a median of 5 h of onset of chest pain, to either the intracoronary administration of 140-160 million autologous BMCs at a median of 6 d after AMI (early group, n = 58) or at a median of 24 d after AMI (late group, n = 49) or to a placebo group (n = 60). Ninety-two percent of the patients had anterior wall infarctions. Bone marrow aspirates were performed only in patients assigned to the BMC treatment. Each 10 mL aspirate was treated with 1000 IU Heparin to prevent clot formation. The BMCs were isolated by density gradient centrifugation at a centralized processing facility and contained 1% to 1.3% CD34+ hematopoietic cells. However, the median percentage of mononuclear cells that exhibit migration capacity was only 29%[241].
Cardiac magnetic resonance imaging with gadolinium was performed on patients at baseline prior to cell infusion and at 4 mo after the injection of BMCs into the infarct-related coronary artery and were compared with MRIs of control patients treated with best medical care. At 4 mo after coronary infusion, there were no significant differences in infarct scar size or LV myocardial wall thickening in patients treated with BMCs at either 5-7 d or 3-4 wk after AMI in comparison with control patients. Moreover, LV function did not significantly improve at 4 mo after the intracoronary infusion of autologous BMCs in either the early or late treated groups in comparison with the placebo group. However, patients with NT-proBNP levels at baseline above 1437 ng/L experienced a greater increase in LVEF of 7.1% in the early group and 9% for the late BMC group. In all cell and placebo treatment groups, LV scar as determined by late gadolinium enhancement on MRI decreased by more than 10 g with a 4%-5% decrease in the ratio of myocardial scar to myocardial mass.
ASSESSMENT OF LATETIME, TIME, AND SWISS TRIALS
Several variables in these studies contributed to the lack of significant improvement of AMI patients treated with BMCs in comparison with placebo treated patients.
Early percutaneous coronary intervention
Patients with AMIs in the LateTIME, TIME, and Swiss Multicenter Trials were treated with PCI within a median of 4 to 5 h of the onset of chest pain. Thereafter, the patients were treated with American and European Heart Association guided best medical therapy. Consequently, AMI sizes and the extent of LV remodeling in the different trial patients were significantly limited and the differences between BMC treated patients and placebo treated patients were small. Although the initial qualifying LV ejection fractions by echocardiography after PCI in the LateTIME and TIME trial patients were ≤ 45%, the LVEFs by MRI at the time of BMC injection were greater than 45%. Bone marrow mononuclear cells are much less effective in patients with small myocardial infarctions with near normal LVEFs. In addition, placebo treated patients continue to improve with best medical therapy after AMIs as demonstrated by the control patients in the Bone Marrow Transfer to Enhance ST-elevation Infarct Regeneration (BOOST) trial in which the LVEFs equaled or exceeded the increases in the LVEFs in the BMC treated patients at 18 mo after AMI[242]. In addition, the Valsartan in Acute Myocardial infarction Trial and trials of neuro-hormonal blockade of patients with AMIs have demonstrated that optimal medical therapy can increase LVEF by a mean of 2.7% at 20 mo[243]. Consequently much larger numbers of patients will be required in clinical trials to demonstrate statistically significant differences between BMC treated patients and placebo treated patients who receive PCI early after the onset of AMI and guideline directed optimal medical therapy.
Heterogeneous bone marrow cell populations
Unfractionated adult BMCs contain less than 3% CD34+ and 1% CD34+/CD133+ hematopoietic progenitor cells and ≤ 1% CD105+ mesenchymal stem cells in healthy subjects when marrow cells are separated by Ficoll density gradient-based separation. However, both CD34+ endothelial colony number and the mesenchymal cell colony number were significantly decreased amongst subjects that participated in the LateTime and Time Trials[244]. In addition, the marrow aspirates in the LateTIME and TIME Trials were separated by an automated cell process system (Sepax, Biosafe), which recovered only 23.6% of the total nucleated cells[245]. Consequently, the BMCs delivered in the LateTIME and TIME trials contained smaller numbers of CD34+ and CD105+ cells than earlier BMC studies. Moreover, stem cell motility can decline by as much as 68% 72 h after harvest from the bone marrow[246]. In addition, 140-150 × 106 unfractionated BMCs may not be the most optimal dose of BMCs for stem cell treatment of patients with AMI. In this regard, BMCs from patients with advanced age and patients with chronic diseases, such as ischemic heart disease or diabetes mellitus, are often functionally impaired, propagate poorly, and have a shortened life span[246-248]. Consequently, BMC colony forming units and cell migration capability must be determined in addition to bone marrow cell number and viability prior to use in the treatment of AMI. Furthermore, BMCs produced only a modest increase in the LVEF of approximately 2%-3% in earlier analyses of stem cell trials of patients with AMIs or ischemic cardiomyopathies[213,214]. Despite well conducted clinical trials, unfractionated BMCs selectively infused into an infarct related coronary artery have a small therapeutic effect and may not be the most optimal cells for the treatment of patients with AMIs.
Red blood cell contamination of stem cells
Red blood cell contamination of bone marrow mononuclear cells can significantly decrease the migration ability and the efficacy of BMCs. Large numbers of red blood cells in the cell preparations cause reduced BMC viability, decreased colony forming capacity, and are associated with reduced recovery of LVEF in patients with AMIs[249]. In patients in the REPAIR-AMI Trial, contamination of the bone marrow cells with red blood cells prior to infusion into patients with AMI independently predicted reduced recovery of LVEF[249]. Moreover, the addition of red blood cells to BMCs dose-dependently decreased neovascularization in ischemic hind-limbs compared to treatment with BMCs without red blood cells[249]. The mechanism by which red blood cells interfere with bone marrow cell propagation, migration and neovascularization involves a dose-dependent reduction of BMC mitochondrial membrane potential and a decrease in BMC mitochondrial adenosine triphosphate (ATP) production[249]. As a consequence of decreased mitochondrial metabolism and function, stem cell self-renewal and differentiation are decreased.
Heparin decreases stem cell migration
Heparin can bind to the chemoattractant stromal derived factor-1 (SDF-1), which is released from ischemic myocardium, and also bind to its receptor CXCR4 on stem cells and thereby block CXCR4 signaling and stem cell migration to injured myocardium[250]. Heparin, in a dose-dependent manner, can inhibit SDF-1 induced BMC migration and homing of BMCs to areas of myocardial ischemia[250-253]. Incubation of BMCs with 20 U/mL of heparin for 30 min abrogates SDF-1 BMC migration by 84% in-vitro and significantly reduces the homing of injected BMCs to injured and infarcted myocardium by 50% in research animals[250]. Decreased migratory capacity of BMCs also correlates with reduced neovascularization and decreased functional capacity in subjects with limb ischemia[251]. In addition, heparin decreases the concentration of vascular endothelial growth factor (VEGF) in ischemic tissue and thereby decreases neovascularization[252]. Heparin also interferes with activation of the cell survival factor Akt (Protein Kinase B) by SDF-1-CXCR4 signaling and in this manner interferes with cell survival and growth. In contrast, the thrombin inhibitor bivalirudin does not interfere with BMC homing or SDF-1/CXCR4 signaling and does not decrease VEGF[252].
Stem cell expulsion from myocardium
Ninety to 97% of unfractionated BMCs leave the myocardium in less than 2 h after injection directly into the myocardium or into the coronary arteries[254,255]. Most of the cells are ejected out of the myocardium through the myocardial injection sites or through the coronary veins and lymphatics into the right heart due to the massaging action of the contracting myocardium. The cells are ultimately lodged in the lungs, liver, spleen and kidneys. In addition, approximately 12% of BMCs are retained in the catheter delivery system after injection[255]. With the intravenous injection of BMCs or other cells for cardiac repair the majority of the cells become entrapped in the lungs. Consequently, fourfold greater numbers of cells are required above that required for intramyocardial or intracoronary injection for repair of myocardial infarctions[256].
Future bone marrow cell studies
The BAMI Trial (The effect of intracoronary reinfusion of bone marrow derived mononuclear cells on all-cause mortality in acute myocardial infarction) is recruiting 3000 patients with LVEFs ≤ 45% within 7 d of AMIs, who have undergone successful coronary reperfusion therapy, for randomization into treatment with either intracoronary autologous unfractionated bone marrow mononuclear cells or placebo[257]. Hopefully the BAMI Trial will avoid the important variables that have been described in this paper and will provide definitive answers to the questions whether BMCs can significantly decrease patient mortality due to myocardial infarction, substantially reduce infarct size and increase LVEF over three years in comparison with patients treated with best medical therapy.
CARDIAC STEM CELLS
Cardiovascular investigators have sought alternatives to BMCs for cardiac repair in patients with ischemic heart disease. Cardiac stem cells, which are multipotent progenitor cells, are present in niches in the heart and contribute to the physiological turnover of myocytes and vascular endothelial cells in the heart. The number of cardiac stem cells in the heart is estimated at one cardiac stem cell per 10000 cardiac myocytes[258]. Consequently, endogenous cardiac stem cells are not normally able to reverse heart damage due to myocardial infarctions. The turnover of cardiac myocytes occurs at rates estimated to be 1% to as much as 22% per year and is dependent on the age, sex, and the health of the individual[259,260]. Two major types of autologous cardiac stem cells have been investigated in patients with injured and infarcted myocardium in the SCIPIO and CADUCEUS clinical trials: C-kit + lineage negative cardiac stem cells isolated from right atrial appendages and cardiosphere derived cells (CDCs) grown from right ventricular cardiac muscle biopsies.
C-KIT + STEM CELLS
C-kit is a receptor for stem cell factor, which is released from the ischemic myocardium, and is important in the chemoattraction of stem cells to apoptotic, injured and necrotic myocardium. C-kit + stem cells have the capacity for self-renewal, clonogenicity and multi-potency[261,262]. These stem cells can express the cardiac transcription factors GATA-4, Nkx2.5 and MEF2 and can differentiate into myogenic, vascular endothelial and smooth muscles cells in-vitro[261,262]. In research animals with AMIs, cardiac stem cells can form new myocardium[262].
Autologous C-kit cardiac stem cells from right atrial appendages have recently been used for the treatment of patients with myocardial infarctions and ischemic cardiomyopathies in the open labeled Cardiac Stem Cell Infusion in Patients with Ischemic Cardiomyopathy (SCIPIO) Trial[263-265]. In this trial C-kit positive stem cells were isolated during coronary artery bypass surgery from the right atrial appendages of patients with LVEFs < 40%. The cells were then propagated in the laboratory. Four mo later, a maximum of one million cardiac stem cells were injected directly into the patient’s saphenous vein grafts and coronary arteries supplying infarcted myocardium. The two year results of this trial have been presented at the American Heart Association Scientific Sessions in November of 2012 and 2013. In the SCIPIO trial the LVEF, measured by three-dimensional echocardiography and by MRI with gadolinium in patients who received cardiac stem cells, increased in 12 patients in absolute units by 11.9% at 2 years[265]. Left ventricular scar, determined by MRI, decreased by as much as 20.4 g at 2 years (n = 6) and was associated with an increase in viable myocardium of 17.9 g (n = 6) at 2 years[265]. New York Heart Association Functional Class score decreased in these patients by 0.77 at 2 years (n = 13). A left internal mammary graft dissection occurred in one treated patient, which was treated with a graft stent, and a peri-procedural myocardial infarction occurred in a second treated patient[264]. In this study, C-kit cardiac stem cells were proposed to chemoattract patients’ native stem cells to areas of myocardial injury and also to transdifferentiate to myocytes for cardiac repair. A Phase 2 trial of safety and efficacy of C-kit cardiac stem cells in a larger group of patients is currently being planned.
CARDIOSPHERE DERIVED CELLS
Percutaneous endomyocardial biopsy specimens of the right ventricular septal wall and apex in patients, when grown in culture, can yield spherical multicellular clusters termed “cardiospheres”. Cardiospheres are a mixture of stromal, mesenchymal and hematopoietic progenitor cells that contain cells that express CD 105 (commonly associated with mesenchymal stem cells) and partially express C-kit[266,267]. Cardiosphere derived cells (CDCs), when injected into the border of myocardial infarctions in mice, engraft and increase viable myocardium[268]. The functional benefit of CDCs is predominantly due to the secretion of growth factors and the recruitment of endogenous stem cells to injured and infarcted myocardium for myocyte generation. In this regard, cardiospheres and CDCs secrete the growth factors angiopoietin-2, basic fibroblastic growth factor, hepatocyte growth factor, insulin-like growth factor 1, stromal derived factor-1 and vascular endothelial growth factor which are beneficial in repair of injured myocardium[267,268].
Autologous CDCs have been investigated in the open labeled Cardiosphere-derived Autologous Stem Cells to Reverse Ventricular Dysfunction (CADUCEUS) Trial[269,270]. In this trial, 17 patients, post myocardial infarction with LVEFs of 25%-45%, underwent endomyocardial biopsies of the right ventricular septum. Cardiosphere derived cells were obtain from cultures of the endomyocardial biopsies and the cells were propagated. In this trial, between 12.5 and 25 million CDCs were then given directly into the infarct related coronary artery of each of the 17 patients 1.5 to 3 mo after their myocardial infarctions. The one year followup of 12 of the 17 patients treated with autologous CDCs and 8 control patients have been reported[270]. Left ventricular scar by MRI significantly decreased by a mean of 11.9 g in CDC-treated patients and by 1.7 g in control patients. Left ventricular viable mass increased by a mean of 22.6 g in treated patients in comparison with 1.8 g in control patients. Left ventricular ejection fractions did not significantly increase but the regional wall function of infarcted segments did increase and correlated with the decrease in LV myocardial scar size[269,270]. Covariate statistical analysis demonstrated that the lower percentage of infused CD90+ cells caused the greatest reductions in scar size in patients with large infarctions. A Phase 2 study of CDCs (ALLSTAR Trial) is currently in progress that involves allogeneic CDCs for the treatment of patients after myocardial infarction.
ASSESSMENT OF THE SCIPIO AND CADUCEUS TRIALS
In the SCIPIO trial 1545 patients were evaluated. Two hundred thirteen patients had LVEFs < 40% and 20 patients were treated with C-kit + stem cells. Twelve of 20 patients had MRI determinations of left ventricular function whereas the control patients did not have MRI determinations of left ventricular function. In the CADUCEUS Trial 436 patients were evaluated and 17 patients received CDCs. Consequently, these trials report a highly selected patient population and the results of these trials cannot be applied to all patients with myocardial infarctions and ischemic cardiomyopathies. Much larger trials are necessary of each of these cell types in patients with myocardial infarctions.
In each of these studies, LV infarction was defined by MRI of delayed enhancement of myocardium in the region of coronary artery occlusion/reperfusion due to gadolinium that leaked from myocardial capillaries and pooled in the myocardial interstitial spaces and intracellular spaces. In these patients the gadolinium volume of distribution was increased and washout from the myocardium was reduced. However, cardiac stem cells can incorporate into damaged blood vessels, chemoattract endogenous stem cells that can form entirely new blood vessels, and can also secrete angiogenic growth factors that stimulate new blood vessels from preexisting vessels. Consequently, the blood vessels in the damaged myocardium of patients treated with these stem cells were less permeable to gadolinium[271]. Infarct scars can potentially appear smaller on MRI due to less gadolinium leak as well as contracture of the myocardial infarction. Moreover inter-scan variability and intra- and inter-observer variability in infarct measurements and interpreting MRI scans can account for some myocardial changes between pre- and post-stem cell infusion[272]. Rebuttals to these arguments against the use of contrast enhanced MRI in estimating infarct size and myocardial regeneration after stem cell treatment have been published[273]. The rebuttal is based on a porcine myocardial infarction study in which allogeneic CDCs decreased infarct scar size and led to cardiomyocyte hyperplasia on MRI and also on histological examination[273]. Nevertheless, anatomical and histological examinations of myocardial biopsies of infarcted hearts of patients or myocardial autopsy examinations of patients treated with these stem cells are necessary to determine if infarct fibrosis is significantly decreased and if substantial generation of new myocytes occurs. Trials of larger numbers of patients treated with C-kit + cardiac stem cells and cardiosphere derived cells for longer times are warranted to determine the precise mechanisms of action of these stem cells and their clinical benefit.
FUTURE DIRECTIONS
The LateTIME, TIME, Swiss, SCIPO and CAUDUCEUS Trials demonstrate that stem cells can be safely administered to patients with acute myocardial infarctions and ischemic cardiomyopathies and do not have significant adverse effects. Specific bone marrow cell subsets, such as unconditioned or conditioned mesenchymal cells or CD34+ hematopoietic cells, may prove to be more efficacious in myocardial infarction repair than unfractionated BMCs[274,275]. In this regard, bone marrow mesenchymal stem cells or mesenchymal stem cells conditioned with cardiogenic growth factors have been reported to be beneficial in increasing LV function and functional capacity in patients with ischemic cardiomyopathies[275]. In addition, mesenchymal stem cells may enhance the beneficial effects of C-kit cardiac stem cells when these cells are administered together[276]. The large size of mesenchymal stem cells, however, requires that these cells be most safely delivered into the heart by direct myocardial injection rather than intracoronary injection in order to avoid problems of cell clumping and coronary occlusion. Mesenchymal stem cells and also umbilical cord stem cells are reported to be “immunoprivileged” and lack Class II human leukocyte antigens[277,278]. If allogeneic stem cells prove to be safe and effective in limiting myocardial damage and LV remodeling after myocardial infarction in patients, then these cells might become an “off the shelf” product that surpasses the significant limitations of inter-patient variability of unfractionated bone marrow mononuclear cells. Since the functional benefit of stem cells appears to be predominantly due to the secretion of biologically active factors, the ultimate rejection of allogeneic stem cells may not be of major concern if the rejection is delayed long enough to allow these cells to exert their paracrine effects. Nevertheless, stem cell trials must be performed in patients with large myocardial infarctions and LVEFs by MRI less than 40% at the time of stem cell administration because stem cells may not be efficacious in patients with small infarctions and near normal or normal LVEFs. In these studies, substantial stem cell viability, colony forming and migration capabilities must be established prior to infusion in patients.
A major problem with all stem cell trials is the short term engraftment and survival of stem cells in injured and infarcted myocardium. The cells that remain in the myocardium do not survive due to ischemia, inflammation, or anoikis or migrate from the myocardium in one to two weeks[254,255]. Consequently, stem engraftment in the heart must be increased in order to significantly enhance their beneficial effects. Possible treatment options include “conditioning” of the myocardium prior to stem cell delivery or co-delivery of stem cells directly into the myocardium with extracellular matrix molecules, nanofibers, hydrogels, or fibrin glues[213,214,279]. Co-delivery of stem cells with other molecules will require direct intramyocardial cell injection at the time of cardiac surgery or cardiac catheterization which appears to produce the greatest functional benefit[280]. Alternatively, stem cells can be administered in patches that are applied directly to the epicardial surface of the damaged myocardium at the time of cardiac surgery[213,214]. Direct stem cell to myocyte contact and interactions may be crucial in eliciting beneficial myocyte functional effects. In addition, genetic engineering of stem cells must be developed that facilitate the homing of stem cells to ischemic myocardium and the retention of the stem cells within the myocardium after intracoronary or intravenous injection.
A major mechanism of action of stem cells studied to date in myocardial repair is the secretion of growth factors, chemokines, anti-inflammatory cytokines and exosomes or microparticles, which contain proteins, messenger ribonucleic acids and micro-ribonucleic acids. Hypoxic stress appears to increase the paracrine effects of stem cells[281,282]. Biologically active factors from stem cells can suppress inflammatory cytokines and inflammatory cells in the injured myocardium, improve myocardial metabolism, promote angiogenesis, inhibit myocyte and endothelial cell apoptosis, recruit endogenous progenitor cells to injured myocardium, and possibly stimulate surviving myocytes to re-enter the cell cycle and proliferate. The most efficacious stem cell biologically active factors must be identified, purified, and the pharmacologic effects established in research animals and ultimately in patients with injured myocardium.
ACKNOWLEDGMENTS
The information presented in this manuscript does not necessarily represent the views of the Department of Veterans Affairs or the United States Government. The section on “Stem Cells in the Treatment of Acute Myocardial Infarction” was adapted from Henning RJ. Stem Cells in Cardiac Repair: Problems and Possibilities. Future Cardiology 2013; 9(6), 875-884
Footnotes
P- Reviewer: Gao GF S- Editor: Wen LL L- Editor: A E- Editor: Lu YJ
Supported by Research facilities at the James A Haley VA Hospital and, in part; Grants from the Florida King Biomedical Research Program, the Muscular Dystrophy Association, the Robert O Law Foundation and the Cornelius Foundation.
Conflict-of-interest: The authors declare no conflicts of interest regarding this manuscript.
Open-Access: This article is an open-access article which was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/
Peer-review started: February 26, 2014
First decision: March 26, 2014
Article in press: March 9, 2015
References
- 1.Thygesen K, Alpert JS, Jaffe AS, Simoons ML, Chaitman BR, White HD. Third universal definition of myocardial infarction. Nat Rev Cardiol. 2012;9:620–633. doi: 10.1038/nrcardio.2012.122. [DOI] [PubMed] [Google Scholar]
- 2.White HD, Thygesen K, Alpert JS, Jaffe AS. Clinical implications of the Third Universal Definition of Myocardial Infarction. Heart. 2014;100:424–432. doi: 10.1136/heartjnl-2012-302976. [DOI] [PubMed] [Google Scholar]
- 3.Jaffe AS. Chasing troponin: how low can you go if you can see the rise? J Am Coll Cardiol. 2006;48:1763–1764. doi: 10.1016/j.jacc.2006.08.006. [DOI] [PubMed] [Google Scholar]
- 4.Apple FS, Wu AH, Jaffe AS, Panteghini M, Christenson RH, Cannon CP, Francis G, Jesse RL, Morrow DA, Newby LK, et al. National Academy of Clinical Biochemistry and IFCC Committee for Standardization of Markers of Cardiac Damage Laboratory Medicine practice guidelines: Analytical issues for biomarkers of heart failure. Circulation. 2007;116:e95–e98. doi: 10.1161/CIRCULATIONAHA.107.185266. [DOI] [PubMed] [Google Scholar]
- 5.Taylor J. Third universal definition of myocardial infarction. Eur Heart J. 2012;33:2506–2507. doi: 10.1093/eurheartj/ehs296. [DOI] [PubMed] [Google Scholar]
- 6.Thygesen K, Mair J, Katus H, Plebani M, Venge P, Collinson P, Lindahl B, Giannitsis E, Hasin Y, Galvani M, et al. Recommendations for the use of cardiac troponin measurement in acute cardiac care. Eur Heart J. 2010;31:2197–2204. doi: 10.1093/eurheartj/ehq251. [DOI] [PubMed] [Google Scholar]
- 7.Thygesen K, Alpert JS, White HD. Universal definition of myocardial infarction. Eur Heart J. 2007;28:2525–2538. doi: 10.1093/eurheartj/ehm355. [DOI] [PubMed] [Google Scholar]
- 8.Zimetbaum PJ, Josephson ME. Use of the electrocardiogram in acute myocardial infarction. N Engl J Med. 2003;348:933–940. doi: 10.1056/NEJMra022700. [DOI] [PubMed] [Google Scholar]
- 9.Wang K, Asinger RW, Marriott HJ. ST-segment elevation in conditions other than acute myocardial infarction. N Engl J Med. 2003;349:2128–2135. doi: 10.1056/NEJMra022580. [DOI] [PubMed] [Google Scholar]
- 10.Engelen DJ, Gorgels AP, Cheriex EC, De Muinck ED, Ophuis AJ, Dassen WR, Vainer J, van Ommen VG, Wellens HJ. Value of the electrocardiogram in localizing the occlusion site in the left anterior descending coronary artery in acute anterior myocardial infarction. J Am Coll Cardiol. 1999;34:389–395. doi: 10.1016/s0735-1097(99)00197-7. [DOI] [PubMed] [Google Scholar]
- 11.Matetzky S, Freimark D, Feinberg MS, Novikov I, Rath S, Rabinowitz B, Kaplinsky E, Hod H. Acute myocardial infarction with isolated ST-segment elevation in posterior chest leads V7-9: “hidden” ST-segment elevations revealing acute posterior infarction. J Am Coll Cardiol. 1999;34:748–753. doi: 10.1016/s0735-1097(99)00249-1. [DOI] [PubMed] [Google Scholar]
- 12.Lopez-Sendon J, Coma-Canella I, Alcasena S, Seoane J, Gamallo C. Electrocardiographic findings in acute right ventricular infarction: sensitivity and specificity of electrocardiographic alterations in right precordial leads V4R, V3R, V1, V2, and V3. J Am Coll Cardiol. 1985;6:1273–1279. doi: 10.1016/s0735-1097(85)80213-8. [DOI] [PubMed] [Google Scholar]
- 13.Yamaji H, Iwasaki K, Kusachi S, Murakami T, Hirami R, Hamamoto H, Hina K, Kita T, Sakakibara N, Tsuji T. Prediction of acute left main coronary artery obstruction by 12-lead electrocardiography. ST segment elevation in lead aVR with less ST segment elevation in lead V(1) J Am Coll Cardiol. 2001;38:1348–1354. doi: 10.1016/s0735-1097(01)01563-7. [DOI] [PubMed] [Google Scholar]
- 14.Thygesen K, Alpert JS, Jaffe AS, Simoons ML, Chaitman BR, White HD, Thygesen K, Alpert JS, White HD, Jaffe AS, et al. Third universal definition of myocardial infarction. Eur Heart J. 2012;33:2551–2567. doi: 10.1093/eurheartj/ehs184. [DOI] [PubMed] [Google Scholar]
- 15.White HD. The prequel: defining prognostically important criteria in the periprocedural PCI troponin saga. Circ Cardiovasc Interv. 2012;5:142–145. doi: 10.1161/CIRCINTERVENTIONS.112.969113. [DOI] [PubMed] [Google Scholar]
- 16.Herrmann J. Peri-procedural myocardial injury: 2005 update. Eur Heart J. 2005;26:2493–2519. doi: 10.1093/eurheartj/ehi455. [DOI] [PubMed] [Google Scholar]
- 17.Moussa ID, Klein LW, Shah B, Mehran R, Mack MJ, Brilakis ES, Reilly JP, Zoghbi G, Holper E, Stone GW. Consideration of a new definition of clinically relevant myocardial infarction after coronary revascularization: an expert consensus document from the Society for Cardiovascular Angiography and Interventions (SCAI) J Am Coll Cardiol. 2013;62:1563–1570. doi: 10.1016/j.jacc.2013.08.720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Jaffe AS, Apple FS, Lindahl B, Mueller C, Katus HA. Why all the struggle about CK-MB and PCI? Eur Heart J. 2012;33:1046–1048. doi: 10.1093/eurheartj/ehr502. [DOI] [PubMed] [Google Scholar]
- 19.Miller WL, Garratt KN, Burritt MF, Lennon RJ, Reeder GS, Jaffe AS. Baseline troponin level: key to understanding the importance of post-PCI troponin elevations. Eur Heart J. 2006;27:1061–1069. doi: 10.1093/eurheartj/ehi760. [DOI] [PubMed] [Google Scholar]
- 20.Eigel P, van Ingen G, Wagenpfeil S. Predictive value of perioperative cardiac troponin I for adverse outcome in coronary artery bypass surgery. Eur J Cardiothorac Surg. 2001;20:544–549. doi: 10.1016/s1010-7940(01)00825-9. [DOI] [PubMed] [Google Scholar]
- 21.Nesher N, Alghamdi AA, Singh SK, Sever JY, Christakis GT, Goldman BS, Cohen GN, Moussa F, Fremes SE. Troponin after cardiac surgery: a predictor or a phenomenon? Ann Thorac Surg. 2008;85:1348–1354. doi: 10.1016/j.athoracsur.2007.12.077. [DOI] [PubMed] [Google Scholar]
- 22.Mendis S, Thygesen K, Kuulasmaa K, Giampaoli S, Mähönen M, Ngu Blackett K, Lisheng L. World Health Organization definition of myocardial infarction: 2008-09 revision. Int J Epidemiol. 2011;40:139–146. doi: 10.1093/ije/dyq165. [DOI] [PubMed] [Google Scholar]
- 23.Kociol RD, Pang PS, Gheorghiade M, Fonarow GC, O’Connor CM, Felker GM. Troponin elevation in heart failure prevalence, mechanisms, and clinical implications. J Am Coll Cardiol. 2010;56:1071–1078. doi: 10.1016/j.jacc.2010.06.016. [DOI] [PubMed] [Google Scholar]
- 24.Latini R, Masson S, Anand IS, Missov E, Carlson M, Vago T, Angelici L, Barlera S, Parrinello G, Maggioni AP, et al. Prognostic value of very low plasma concentrations of troponin T in patients with stable chronic heart failure. Circulation. 2007;116:1242–1249. doi: 10.1161/CIRCULATIONAHA.106.655076. [DOI] [PubMed] [Google Scholar]
- 25.Januzzi JL, Filippatos G, Nieminen M, Gheorghiade M. Troponin elevation in patients with heart failure: on behalf of the third Universal Definition of Myocardial Infarction Global Task Force: Heart Failure Section. Eur Heart J. 2012;33:2265–2271. doi: 10.1093/eurheartj/ehs191. [DOI] [PubMed] [Google Scholar]
- 26.Apple FS, Collinson PO. Analytical characteristics of high-sensitivity cardiac troponin assays. Clin Chem. 2012;58:54–61. doi: 10.1373/clinchem.2011.165795. [DOI] [PubMed] [Google Scholar]
- 27.Apple FS. A new season for cardiac troponin assays: it’s time to keep a scorecard. Clin Chem. 2009;55:1303–1306. doi: 10.1373/clinchem.2009.128363. [DOI] [PubMed] [Google Scholar]
- 28.Reichlin T, Hochholzer W, Bassetti S, Steuer S, Stelzig C, Hartwiger S, Biedert S, Schaub N, Buerge C, Potocki M, et al. Early diagnosis of myocardial infarction with sensitive cardiac troponin assays. N Engl J Med. 2009;361:858–867. doi: 10.1056/NEJMoa0900428. [DOI] [PubMed] [Google Scholar]
- 29.Keller T, Zeller T, Ojeda F, Tzikas S, Lillpopp L, Sinning C, Wild P, Genth-Zotz S, Warnholtz A, Giannitsis E, et al. Serial changes in highly sensitive troponin I assay and early diagnosis of myocardial infarction. JAMA. 2011;306:2684–2693. doi: 10.1001/jama.2011.1896. [DOI] [PubMed] [Google Scholar]
- 30.de Lemos JA. Increasingly sensitive assays for cardiac troponins: a review. JAMA. 2013;309:2262–2269. doi: 10.1001/jama.2013.5809. [DOI] [PubMed] [Google Scholar]
- 31.Thygesen K, Mair J, Giannitsis E, Mueller C, Lindahl B, Blankenberg S, Huber K, Plebani M, Biasucci LM, Tubaro M, et al. How to use high-sensitivity cardiac troponins in acute cardiac care. Eur Heart J. 2012;33:2252–2257. doi: 10.1093/eurheartj/ehs154. [DOI] [PubMed] [Google Scholar]
- 32.Gamble JH, Carlton EW, Orr WP, Greaves K. High-sensitivity cardiac troponins: no more ‘negatives’. Expert Rev Cardiovasc Ther. 2013;11:1129–1139. doi: 10.1586/14779072.2013.828978. [DOI] [PubMed] [Google Scholar]
- 33.Reichlin T, Irfan A, Twerenbold R, Reiter M, Hochholzer W, Burkhalter H, Bassetti S, Steuer S, Winkler K, Peter F, et al. Utility of absolute and relative changes in cardiac troponin concentrations in the early diagnosis of acute myocardial infarction. Circulation. 2011;124:136–145. doi: 10.1161/CIRCULATIONAHA.111.023937. [DOI] [PubMed] [Google Scholar]
- 34.Mueller M, Biener M, Vafaie M, Doerr S, Keller T, Blankenberg S, Katus HA, Giannitsis E. Absolute and relative kinetic changes of high-sensitivity cardiac troponin T in acute coronary syndrome and in patients with increased troponin in the absence of acute coronary syndrome. Clin Chem. 2012;58:209–218. doi: 10.1373/clinchem.2011.171827. [DOI] [PubMed] [Google Scholar]
- 35.Hamm CW, Bassand JP, Agewall S, Bax J, Boersma E, Bueno H, Caso P, Dudek D, Gielen S, Huber K, et al. ESC Guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation: The Task Force for the management of acute coronary syndromes (ACS) in patients presenting without persistent ST-segment elevation of the European Society of Cardiology (ESC) Eur Heart J. 2011;32:2999–3054. doi: 10.1093/eurheartj/ehr236. [DOI] [PubMed] [Google Scholar]
- 36.Pfortmueller CA, Funk GC, Marti G, Leichtle AB, Fiedler GM, Schwarz C, Exadaktylos AK, Lindner G. Diagnostic performance of high-sensitive troponin T in patients with renal insufficiency. Am J Cardiol. 2013;112:1968–1972. doi: 10.1016/j.amjcard.2013.08.028. [DOI] [PubMed] [Google Scholar]
- 37.Yeh RW, Sidney S, Chandra M, Sorel M, Selby JV, Go AS. Population trends in the incidence and outcomes of acute myocardial infarction. N Engl J Med. 2010;362:2155–2165. doi: 10.1056/NEJMoa0908610. [DOI] [PubMed] [Google Scholar]
- 38.Yusuf S, Reddy S, Ounpuu S, Anand S. Global burden of cardiovascular diseases: Part II: variations in cardiovascular disease by specific ethnic groups and geographic regions and prevention strategies. Circulation. 2001;104:2855–2864. doi: 10.1161/hc4701.099488. [DOI] [PubMed] [Google Scholar]
- 39.Goyal A, Yusuf S. The burden of cardiovascular disease in the Indian subcontinent. Indian J Med Res. 2006;124:235–244. [PubMed] [Google Scholar]
- 40.Critchley J, Liu J, Zhao D, Wei W, Capewell S. Explaining the increase in coronary heart disease mortality in Beijing between 1984 and 1999. Circulation. 2004;110:1236–1244. doi: 10.1161/01.CIR.0000140668.91896.AE. [DOI] [PubMed] [Google Scholar]
- 41.Beaglehole R, Reddy S, Leeder SR. Poverty and human development: the global implications of cardiovascular disease. Circulation. 2007;116:1871–1873. doi: 10.1161/CIRCULATIONAHA.107.736926. [DOI] [PubMed] [Google Scholar]
- 42.Steinberg BA, Moghbeli N, Buros J, Ruda M, Parkhomenko A, Raju BS, García-Castillo A, Janion M, Nicolau JC, Fox KA, et al. Global outcomes of ST-elevation myocardial infarction: comparisons of the Enoxaparin and Thrombolysis Reperfusion for Acute Myocardial Infarction Treatment-Thrombolysis In Myocardial Infarction study 25 (ExTRACT-TIMI 25) registry and trial. Am Heart J. 2007;154:54–61. doi: 10.1016/j.ahj.2007.03.047. [DOI] [PubMed] [Google Scholar]
- 43.Jernberg T, Johanson P, Held C, Svennblad B, Lindbäck J, Wallentin L. Association between adoption of evidence-based treatment and survival for patients with ST-elevation myocardial infarction. JAMA. 2011;305:1677–1684. doi: 10.1001/jama.2011.522. [DOI] [PubMed] [Google Scholar]
- 44.Mehta RH, Roe MT, Chen AY, Lytle BL, Pollack CV, Brindis RG, Smith SC, Harrington RA, Fintel D, Fraulo ES, et al. Recent trends in the care of patients with non-ST-segment elevation acute coronary syndromes: insights from the CRUSADE initiative. Arch Intern Med. 2006;166:2027–2034. doi: 10.1001/archinte.166.18.2027. [DOI] [PubMed] [Google Scholar]
- 45.Krumholz HM, Merrill AR, Schone EM, Schreiner GC, Chen J, Bradley EH, Wang Y, Wang Y, Lin Z, Straube BM, et al. Patterns of hospital performance in acute myocardial infarction and heart failure 30-day mortality and readmission. Circ Cardiovasc Qual Outcomes. 2009;2:407–413. doi: 10.1161/CIRCOUTCOMES.109.883256. [DOI] [PubMed] [Google Scholar]
- 46.Alexander KP, Newby LK, Cannon CP, Armstrong PW, Gibler WB, Rich MW, Van de Werf F, White HD, Weaver WD, Naylor MD, et al. Acute coronary care in the elderly, part I: Non-ST-segment-elevation acute coronary syndromes: a scientific statement for healthcare professionals from the American Heart Association Council on Clinical Cardiology: in collaboration with the Society of Geriatric Cardiology. Circulation. 2007;115:2549–2569. doi: 10.1161/CIRCULATIONAHA.107.182615. [DOI] [PubMed] [Google Scholar]
- 47.Alexander KP, Newby LK, Armstrong PW, Cannon CP, Gibler WB, Rich MW, Van de Werf F, White HD, Weaver WD, Naylor MD, et al. Acute coronary care in the elderly, part II: ST-segment-elevation myocardial infarction: a scientific statement for healthcare professionals from the American Heart Association Council on Clinical Cardiology: in collaboration with the Society of Geriatric Cardiology. Circulation. 2007;115:2570–2589. doi: 10.1161/CIRCULATIONAHA.107.182616. [DOI] [PubMed] [Google Scholar]
- 48.Lee PY, Alexander KP, Hammill BG, Pasquali SK, Peterson ED. Representation of elderly persons and women in published randomized trials of acute coronary syndromes. JAMA. 2001;286:708–713. doi: 10.1001/jama.286.6.708. [DOI] [PubMed] [Google Scholar]
- 49.Roe MT, Messenger JC, Weintraub WS, Cannon CP, Fonarow GC, Dai D, Chen AY, Klein LW, Masoudi FA, McKay C, et al. Treatments, trends, and outcomes of acute myocardial infarction and percutaneous coronary intervention. J Am Coll Cardiol. 2010;56:254–263. doi: 10.1016/j.jacc.2010.05.008. [DOI] [PubMed] [Google Scholar]
- 50.De Luca G, Gibson CM, Bellandi F, Noc M, Dudek D, Zeymer U, Arntz HR, Cutlip D, Maioli M, Zorman S, et al. Diabetes mellitus is associated with distal embolization, impaired myocardial perfusion, and higher mortality in patients with ST-segment elevation myocardial infarction treated with primary angioplasty and glycoprotein IIb-IIIa inhibitors. Atherosclerosis. 2009;207:181–185. doi: 10.1016/j.atherosclerosis.2009.03.042. [DOI] [PubMed] [Google Scholar]
- 51.Svensson AM, McGuire DK, Abrahamsson P, Dellborg M. Association between hyper- and hypoglycaemia and 2 year all-cause mortality risk in diabetic patients with acute coronary events. Eur Heart J. 2005;26:1255–1261. doi: 10.1093/eurheartj/ehi230. [DOI] [PubMed] [Google Scholar]
- 52.Herzog CA. Acute myocardial infarction in patients with end-stage renal disease. Kidney Int Suppl. 1999;71:S130–S133. doi: 10.1046/j.1523-1755.1999.07132.x. [DOI] [PubMed] [Google Scholar]
- 53.Sanidas EA, Brener SJ, Maehara A, Généreux P, Witzenbichler B, El-Omar M, Fahy M, Mehran R, Gibson CM, Stone GW. Outcomes in diabetic patients undergoing primary percutaneous coronary intervention for acute anterior myocardial infarction: results from the INFUSE-AMI study. Catheter Cardiovasc Interv. 2014;83:704–710. doi: 10.1002/ccd.25203. [DOI] [PubMed] [Google Scholar]
- 54.Herzog CA, Littrell K, Arko C, Frederick PD, Blaney M. Clinical characteristics of dialysis patients with acute myocardial infarction in the United States: a collaborative project of the United States Renal Data System and the National Registry of Myocardial Infarction. Circulation. 2007;116:1465–1472. doi: 10.1161/CIRCULATIONAHA.107.696765. [DOI] [PubMed] [Google Scholar]
- 55.Medi C, Montalescot G, Budaj A, Fox KA, López-Sendón J, FitzGerald G, Brieger DB. Reperfusion in patients with renal dysfunction after presentation with ST-segment elevation or left bundle branch block: GRACE (Global Registry of Acute Coronary Events) JACC Cardiovasc Interv. 2009;2:26–33. doi: 10.1016/j.jcin.2008.09.010. [DOI] [PubMed] [Google Scholar]
- 56.Gharacholou SM, Alexander KP, Chen AY, Wang TY, Melloni C, Gibler WB, Pollack CV, Ohman EM, Peterson ED, Roe MT. Implications and reasons for the lack of use of reperfusion therapy in patients with ST-segment elevation myocardial infarction: findings from the CRUSADE initiative. Am Heart J. 2010;159:757–763. doi: 10.1016/j.ahj.2010.02.009. [DOI] [PubMed] [Google Scholar]
- 57.Shah P, Najafi AH, Panza JA, Cooper HA. Outcomes and quality of life in patients greater than or equal to 85 years of age with ST-elevation myocardial infarction. Am J Cardiol. 2009;103:170–174. doi: 10.1016/j.amjcard.2008.08.051. [DOI] [PubMed] [Google Scholar]
- 58.Glickman SW, Granger CB, Ou FS, O’Brien S, Lytle BL, Cairns CB, Mears G, Hoekstra JW, Garvey JL, Peterson ED, et al. Impact of a statewide ST-segment-elevation myocardial infarction regionalization program on treatment times for women, minorities, and the elderly. Circ Cardiovasc Qual Outcomes. 2010;3:514–521. doi: 10.1161/CIRCOUTCOMES.109.917112. [DOI] [PubMed] [Google Scholar]
- 59.Lewis WR, Ellrodt AG, Peterson E, Hernandez AF, LaBresh KA, Cannon CP, Pan W, Fonarow GC. Trends in the use of evidence-based treatments for coronary artery disease among women and the elderly: findings from the get with the guidelines quality-improvement program. Circ Cardiovasc Qual Outcomes. 2009;2:633–641. doi: 10.1161/CIRCOUTCOMES.108.824763. [DOI] [PubMed] [Google Scholar]
- 60.Mathews R, Peterson ED, Li S, Roe MT, Glickman SW, Wiviott SD, Saucedo JF, Antman EM, Jacobs AK, Wang TY. Use of emergency medical service transport among patients with ST-segment-elevation myocardial infarction: findings from the National Cardiovascular Data Registry Acute Coronary Treatment Intervention Outcomes Network Registry-Get With The Guidelines. Circulation. 2011;124:154–163. doi: 10.1161/CIRCULATIONAHA.110.002345. [DOI] [PubMed] [Google Scholar]
- 61.Faxon D, Lenfant C. Timing is everything: motivating patients to call 9-1-1 at onset of acute myocardial infarction. Circulation. 2001;104:1210–1211. [PubMed] [Google Scholar]
- 62.De Luca G, Suryapranata H, Ottervanger JP, Antman EM. Time delay to treatment and mortality in primary angioplasty for acute myocardial infarction: every minute of delay counts. Circulation. 2004;109:1223–1225. doi: 10.1161/01.CIR.0000121424.76486.20. [DOI] [PubMed] [Google Scholar]
- 63.Terkelsen CJ, Sørensen JT, Maeng M, Jensen LO, Tilsted HH, Trautner S, Vach W, Johnsen SP, Thuesen L, Lassen JF. System delay and mortality among patients with STEMI treated with primary percutaneous coronary intervention. JAMA. 2010;304:763–771. doi: 10.1001/jama.2010.1139. [DOI] [PubMed] [Google Scholar]
- 64.Jacobs AK, Antman EM, Faxon DP, Gregory T, Solis P. Development of systems of care for ST-elevation myocardial infarction patients: executive summary. Circulation. 2007;116:217–230. doi: 10.1161/CIRCULATIONAHA.107.184043. [DOI] [PubMed] [Google Scholar]
- 65.Trivedi K, Schuur JD, Cone DC. Can paramedics read ST-segment elevation myocardial infarction on prehospital 12-lead electrocardiograms? Prehosp Emerg Care. 2009;13:207–214. doi: 10.1080/10903120802706153. [DOI] [PubMed] [Google Scholar]
- 66.Sørensen JT, Terkelsen CJ, Nørgaard BL, Trautner S, Hansen TM, Bøtker HE, Lassen JF, Andersen HR. Urban and rural implementation of pre-hospital diagnosis and direct referral for primary percutaneous coronary intervention in patients with acute ST-elevation myocardial infarction. Eur Heart J. 2011;32:430–436. doi: 10.1093/eurheartj/ehq437. [DOI] [PubMed] [Google Scholar]
- 67.Antman EM. Time is muscle: translation into practice. J Am Coll Cardiol. 2008;52:1216–1221. doi: 10.1016/j.jacc.2008.07.011. [DOI] [PubMed] [Google Scholar]
- 68.Bates ER, Nallamothu BK. Commentary: the role of percutaneous coronary intervention in ST-segment-elevation myocardial infarction. Circulation. 2008;118:567–573. doi: 10.1161/CIRCULATIONAHA.108.788620. [DOI] [PubMed] [Google Scholar]
- 69.Rathore SS, Curtis JP, Chen J, Wang Y, Nallamothu BK, Epstein AJ, Krumholz HM. Association of door-to-balloon time and mortality in patients admitted to hospital with ST elevation myocardial infarction: national cohort study. BMJ. 2009;338:b1807. doi: 10.1136/bmj.b1807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Bradley EH, Nallamothu BK, Stern AF, Cherlin EJ, Wang Y, Byrd JR, Linnander EL, Nazem AG, Brush JE, Krumholz HM. The door-to-balloon alliance for quality: who joins national collaborative efforts and why? Jt Comm J Qual Patient Saf. 2009;35:93–99. doi: 10.1016/s1553-7250(09)35012-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Antman EM, Anbe DT, Armstrong PW. ACC/AHA guidelines for the management of patients with ST-elevation myocardial infarction: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee to Revise the 1999 Guidelines for the Management of Patients With Acute Myocardial Infarction) J Am Coll Cardiol. 2004;44:e1–e212. doi: 10.1016/j.jacc.2004.07.014. [DOI] [PubMed] [Google Scholar]
- 72.Bonnefoy E, Steg PG, Boutitie F, Dubien PY, Lapostolle F, Roncalli J, Dissait F, Vanzetto G, Leizorowicz A, Kirkorian G, et al. Comparison of primary angioplasty and pre-hospital fibrinolysis in acute myocardial infarction (CAPTIM) trial: a 5-year follow-up. Eur Heart J. 2009;30:1598–1606. doi: 10.1093/eurheartj/ehp156. [DOI] [PubMed] [Google Scholar]
- 73.Bonnefoy E, Lapostolle F, Leizorovicz A, Steg G, McFadden EP, Dubien PY, Cattan S, Boullenger E, Machecourt J, Lacroute JM, et al. Primary angioplasty versus prehospital fibrinolysis in acute myocardial infarction: a randomised study. Lancet. 2002;360:825–829. doi: 10.1016/S0140-6736(02)09963-4. [DOI] [PubMed] [Google Scholar]
- 74.Boersma E, Maas AC, Deckers JW, Simoons ML. Early thrombolytic treatment in acute myocardial infarction: reappraisal of the golden hour. Lancet. 1996;348:771–775. doi: 10.1016/S0140-6736(96)02514-7. [DOI] [PubMed] [Google Scholar]
- 75.Morrow DA, Antman EM, Sayah A, Schuhwerk KC, Giugliano RP, deLemos JA, Waller M, Cohen SA, Rosenberg DG, Cutler SS, et al. Evaluation of the time saved by prehospital initiation of reteplase for ST-elevation myocardial infarction: results of The Early Retavase-Thrombolysis in Myocardial Infarction (ER-TIMI) 19 trial. J Am Coll Cardiol. 2002;40:71–77. doi: 10.1016/s0735-1097(02)01936-8. [DOI] [PubMed] [Google Scholar]
- 76.Pedley DK, Bissett K, Connolly EM, Goodman CG, Golding I, Pringle TH, McNeill GP, Pringle SD, Jones MC. Prospective observational cohort study of time saved by prehospital thrombolysis for ST elevation myocardial infarction delivered by paramedics. BMJ. 2003;327:22–26. doi: 10.1136/bmj.327.7405.22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Morrison LJ, Verbeek PR, McDonald AC, Sawadsky BV, Cook DJ. Mortality and prehospital thrombolysis for acute myocardial infarction: A meta-analysis. JAMA. 2000;283:2686–2692. doi: 10.1001/jama.283.20.2686. [DOI] [PubMed] [Google Scholar]
- 78.Westerhout CM, Bonnefoy E, Welsh RC, Steg PG, Boutitie F, Armstrong PW. The influence of time from symptom onset and reperfusion strategy on 1-year survival in ST-elevation myocardial infarction: a pooled analysis of an early fibrinolytic strategy versus primary percutaneous coronary intervention from CAPTIM and WEST. Am Heart J. 2011;161:283–290. doi: 10.1016/j.ahj.2010.10.033. [DOI] [PubMed] [Google Scholar]
- 79.Björklund E, Stenestrand U, Lindbäck J, Svensson L, Wallentin L, Lindahl B. Pre-hospital thrombolysis delivered by paramedics is associated with reduced time delay and mortality in ambulance-transported real-life patients with ST-elevation myocardial infarction. Eur Heart J. 2006;27:1146–1152. doi: 10.1093/eurheartj/ehi886. [DOI] [PubMed] [Google Scholar]
- 80.Danchin N, Blanchard D, Steg PG, Sauval P, Hanania G, Goldstein P, Cambou JP, Guéret P, Vaur L, Boutalbi Y, et al. Impact of prehospital thrombolysis for acute myocardial infarction on 1-year outcome: results from the French Nationwide USIC 2000 Registry. Circulation. 2004;110:1909–1915. doi: 10.1161/01.CIR.0000143144.82338.36. [DOI] [PubMed] [Google Scholar]
- 81.Lloyd-Jones D, Adams RJ, Brown TM, Carnethon M, Dai S, De Simone G, Ferguson TB, Ford E, Furie K, Gillespie C, et al. Heart disease and stroke statistics--2010 update: a report from the American Heart Association. Circulation. 2010;121:e46–e215. doi: 10.1161/CIRCULATIONAHA.109.192667. [DOI] [PubMed] [Google Scholar]
- 82.Valenzuela TD, Roe DJ, Nichol G, Clark LL, Spaite DW, Hardman RG. Outcomes of rapid defibrillation by security officers after cardiac arrest in casinos. N Engl J Med. 2000;343:1206–1209. doi: 10.1056/NEJM200010263431701. [DOI] [PubMed] [Google Scholar]
- 83.Larsen MP, Eisenberg MS, Cummins RO, Hallstrom AP. Predicting survival from out-of-hospital cardiac arrest: a graphic model. Ann Emerg Med. 1993;22:1652–1658. doi: 10.1016/s0196-0644(05)81302-2. [DOI] [PubMed] [Google Scholar]
- 84.Ornato JP, McBurnie MA, Nichol G, Salive M, Weisfeldt M, Riegel B, Christenson J, Terndrup T, Daya M. The Public Access Defibrillation (PAD) trial: study design and rationale. Resuscitation. 2003;56:135–147. doi: 10.1016/s0300-9572(02)00442-2. [DOI] [PubMed] [Google Scholar]
- 85.Caffrey SL, Willoughby PJ, Pepe PE, Becker LB. Public use of automated external defibrillators. N Engl J Med. 2002;347:1242–1247. doi: 10.1056/NEJMoa020932. [DOI] [PubMed] [Google Scholar]
- 86.Myerburg RJ, Fenster J, Velez M, Rosenberg D, Lai S, Kurlansky P, Newton S, Knox M, Castellanos A. Impact of community-wide police car deployment of automated external defibrillators on survival from out-of-hospital cardiac arrest. Circulation. 2002;106:1058–1064. doi: 10.1161/01.cir.0000028147.92190.a7. [DOI] [PubMed] [Google Scholar]
- 87.Bernard SA, Gray TW, Buist MD, Jones BM, Silvester W, Gutteridge G, Smith K. Treatment of comatose survivors of out-of-hospital cardiac arrest with induced hypothermia. N Engl J Med. 2002;346:557–563. doi: 10.1056/NEJMoa003289. [DOI] [PubMed] [Google Scholar]
- 88.Hypothermia after Cardiac Arrest Study Group. Mild therapeutic hypothermia to improve the neurologic outcome after cardiac arrest. N Engl J Med. 2002;346:549–556. doi: 10.1056/NEJMoa012689. [DOI] [PubMed] [Google Scholar]
- 89.The I. S.A.M. Study Group. A prospective trial of intravenous streptokinase in acute myocardial infarction (I.S.A.M.). Mortality, morbidity, and infarct size at 21 days. N Engl J Med. 1986;314:1465–1471. doi: 10.1056/NEJM198606053142301. [DOI] [PubMed] [Google Scholar]
- 90.Randomised trial of intravenous streptokinase, oral aspirin, both, or neither among 17,187 cases of suspected acute myocardial infarction: ISIS-2. ISIS-2 (Second International Study of Infarct Survival) Collaborative Group. Lancet. 1988;2:349–360. [PubMed] [Google Scholar]
- 91.Rossi P, Bolognese L. Comparison of intravenous urokinase plus heparin versus heparin alone in acute myocardial infarction. Urochinasi per via Sistemica nell’Infarto Miocardico (USIM) Collaborative Group. Am J Cardiol. 1991;68:585–592. doi: 10.1016/0002-9149(91)90348-o. [DOI] [PubMed] [Google Scholar]
- 92.Randomised trial of late thrombolysis in patients with suspected acute myocardial infarction. EMERAS (Estudio Multicéntrico Estreptoquinasa Repúblicas de América del Sur) Collaborative Group. Lancet. 1993;342:767–772. [PubMed] [Google Scholar]
- 93.Late Assessment of Thrombolytic Efficacy (LATE) study with alteplase 6-24 hours after onset of acute myocardial infarction. Lancet. 1993;342:759–766. [PubMed] [Google Scholar]
- 94.Indications for fibrinolytic therapy in suspected acute myocardial infarction: collaborative overview of early mortality and major morbidity results from all randomised trials of more than 1000 patients. Fibrinolytic Therapy Trialists’ (FTT) Collaborative Group. Lancet. 1994;343:311–322. [PubMed] [Google Scholar]
- 95.Langer A, Goodman SG, Topol EJ, Charlesworth A, Skene AM, Wilcox RG, Armstrong PW. Late assessment of thrombolytic efficacy (LATE) study: prognosis in patients with non-Q wave myocardial infarction. (LATE Study Investigators) J Am Coll Cardiol. 1996;27:1327–1332. doi: 10.1016/0735-1097(96)00012-5. [DOI] [PubMed] [Google Scholar]
- 96.Van de Werf F, Bax J, Betriu A, Blomstrom-Lundqvist C, Crea F, Falk V, Filippatos G, Fox K, Huber K, Kastrati A, et al. Management of acute myocardial infarction in patients presenting with persistent ST-segment elevation: the Task Force on the Management of ST-Segment Elevation Acute Myocardial Infarction of the European Society of Cardiology. Eur Heart J. 2008;29:2909–2945. doi: 10.1093/eurheartj/ehn416. [DOI] [PubMed] [Google Scholar]
- 97.Bode C, Smalling RW, Berg G, Burnett C, Lorch G, Kalbfleisch JM, Chernoff R, Christie LG, Feldman RL, Seals AA, et al. Randomized comparison of coronary thrombolysis achieved with double-bolus reteplase (recombinant plasminogen activator) and front-loaded, accelerated alteplase (recombinant tissue plasminogen activator) in patients with acute myocardial infarction. The RAPID II Investigators. Circulation. 1996;94:891–898. doi: 10.1161/01.cir.94.5.891. [DOI] [PubMed] [Google Scholar]
- 98.Cannon CP, McCabe CH, Gibson CM, Ghali M, Sequeira RF, McKendall GR, Breed J, Modi NB, Fox NL, Tracy RP, et al. TNK-tissue plasminogen activator in acute myocardial infarction. Results of the Thrombolysis in Myocardial Infarction (TIMI) 10A dose-ranging trial. Circulation. 1997;95:351–356. doi: 10.1161/01.cir.95.2.351. [DOI] [PubMed] [Google Scholar]
- 99.Martin GV, Sheehan FH, Stadius M, Maynard C, Davis KB, Ritchie JL, Kennedy JW. Intravenous streptokinase for acute myocardial infarction. Effects on global and regional systolic function. Circulation. 1988;78:258–266. doi: 10.1161/01.cir.78.2.258. [DOI] [PubMed] [Google Scholar]
- 100.The effects of tissue plasminogen activator, streptokinase, or both on coronary-artery patency, ventricular function, and survival after acute myocardial infarction. The GUSTO Angiographic Investigators. N Engl J Med. 1993;329:1615–1622. doi: 10.1056/NEJM199311253292204. [DOI] [PubMed] [Google Scholar]
- 101.Collaborative meta-analysis of randomised trials of antiplatelet therapy for prevention of death, myocardial infarction, and stroke in high risk patients. BMJ. 2002;324:71–86. doi: 10.1136/bmj.324.7329.71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Effect of intravenous APSAC on mortality after acute myocardial infarction: preliminary report of a placebo-controlled clinical trial. AIMS Trial Study Group. Lancet. 1988;1:545–549. [PubMed] [Google Scholar]
- 103.Cannon C, McCabe C, Gibson C, Adgey A, Ghali M, Sequeira R, McKendall G, Breed J, Modi N, Fox N, et al. TNK-tissue plasminogen activator in acute myocardial infarction. Results of Thrombolysis in Myocardial Infarction (TIMI) 10A dose ranging trial. Circulation. 1997;95:351–356. doi: 10.1161/01.cir.95.2.351. [DOI] [PubMed] [Google Scholar]
- 104.Lundergan CF, Reiner JS, McCarthy WF, Coyne KS, Califf RM, Ross AM. Clinical predictors of early infarct-related artery patency following thrombolytic therapy: importance of body weight, smoking history, infarct-related artery and choice of thrombolytic regimen: the GUSTO-I experience. Global Utilization of Streptokinase and t-PA for Occluded Coronary Arteries. J Am Coll Cardiol. 1998;32:641–647. doi: 10.1016/s0735-1097(98)00278-2. [DOI] [PubMed] [Google Scholar]
- 105.Serebruany VL, Steinhubl SR, Berger PB, Malinin AI, Baggish JS, Bhatt DL, Topol EJ. Analysis of risk of bleeding complications after different doses of aspirin in 192,036 patients enrolled in 31 randomized controlled trials. Am J Cardiol. 2005;95:1218–1222. doi: 10.1016/j.amjcard.2005.01.049. [DOI] [PubMed] [Google Scholar]
- 106.Steinhubl SR, Bhatt DL, Brennan DM, Montalescot G, Hankey GJ, Eikelboom JW, Berger PB, Topol EJ. Aspirin to prevent cardiovascular disease: the association of aspirin dose and clopidogrel with thrombosis and bleeding. Ann Intern Med. 2009;150:379–386. doi: 10.7326/0003-4819-150-6-200903170-00006. [DOI] [PubMed] [Google Scholar]
- 107.Chen ZM, Jiang LX, Chen YP, Xie JX, Pan HC, Peto R, Collins R, Liu LS. Addition of clopidogrel to aspirin in 45,852 patients with acute myocardial infarction: randomised placebo-controlled trial. Lancet. 2005;366:1607–1621. doi: 10.1016/S0140-6736(05)67660-X. [DOI] [PubMed] [Google Scholar]
- 108.Eisenberg PR. Role of heparin in coronary thrombolysis. Chest. 1992;101:131S–139S. doi: 10.1378/chest.101.4_supplement.131s. [DOI] [PubMed] [Google Scholar]
- 109.Nutescu EA, Spinler SA, Wittkowsky A, Dager WE. Low-molecular-weight heparins in renal impairment and obesity: available evidence and clinical practice recommendations across medical and surgical settings. Ann Pharmacother. 2009;43:1064–1083. doi: 10.1345/aph.1L194. [DOI] [PubMed] [Google Scholar]
- 110.Sutton AG, Campbell PG, Price DJ, Grech ED, Hall JA, Davies A, Stewart MJ, de Belder MA. Failure of thrombolysis by streptokinase: detection with a simple electrocardiographic method. Heart. 2000;84:149–156. doi: 10.1136/heart.84.2.149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Gershlick AH, Stephens-Lloyd A, Hughes S, Abrams KR, Stevens SE, Uren NG, de Belder A, Davis J, Pitt M, Banning A, et al. Rescue angioplasty after failed thrombolytic therapy for acute myocardial infarction. N Engl J Med. 2005;353:2758–2768. doi: 10.1056/NEJMoa050849. [DOI] [PubMed] [Google Scholar]
- 112.Sutton AG, Campbell PG, Graham R, Price DJ, Gray JC, Grech ED, Hall JA, Harcombe AA, Wright RA, Smith RH, et al. A randomized trial of rescue angioplasty versus a conservative approach for failed fibrinolysis in ST-segment elevation myocardial infarction: the Middlesbrough Early Revascularization to Limit INfarction (MERLIN) trial. J Am Coll Cardiol. 2004;44:287–296. doi: 10.1016/j.jacc.2003.12.059. [DOI] [PubMed] [Google Scholar]
- 113.Wijeysundera HC, Vijayaraghavan R, Nallamothu BK, Foody JM, Krumholz HM, Phillips CO, Kashani A, You JJ, Tu JV, Ko DT. Rescue angioplasty or repeat fibrinolysis after failed fibrinolytic therapy for ST-segment myocardial infarction: a meta-analysis of randomized trials. J Am Coll Cardiol. 2007;49:422–430. doi: 10.1016/j.jacc.2006.09.033. [DOI] [PubMed] [Google Scholar]
- 114.Hochman JS, Sleeper LA, White HD, Dzavik V, Wong SC, Menon V, Webb JG, Steingart R, Picard MH, Menegus MA, et al. One-year survival following early revascularization for cardiogenic shock. JAMA. 2001;285:190–192. doi: 10.1001/jama.285.2.190. [DOI] [PubMed] [Google Scholar]
- 115.Fernandez-Avilés F, Alonso JJ, Castro-Beiras A, Vázquez N, Blanco J, Alonso-Briales J, López-Mesa J, Fernández-Vazquez F, Calvo I, Martínez-Elbal L, et al. Routine invasive strategy within 24 hours of thrombolysis versus ischaemia-guided conservative approach for acute myocardial infarction with ST-segment elevation (GRACIA-1): a randomised controlled trial. Lancet. 2004;364:1045–1053. doi: 10.1016/S0140-6736(04)17059-1. [DOI] [PubMed] [Google Scholar]
- 116.Cantor WJ, Fitchett D, Borgundvaag B, Ducas J, Heffernan M, Cohen EA, Morrison LJ, Langer A, Dzavik V, Mehta SR, et al. Routine early angioplasty after fibrinolysis for acute myocardial infarction. N Engl J Med. 2009;360:2705–2718. doi: 10.1056/NEJMoa0808276. [DOI] [PubMed] [Google Scholar]
- 117.Bøhmer E, Hoffmann P, Abdelnoor M, Arnesen H, Halvorsen S. Efficacy and safety of immediate angioplasty versus ischemia-guided management after thrombolysis in acute myocardial infarction in areas with very long transfer distances results of the NORDISTEMI (NORwegian study on DIstrict treatment of ST-elevation myocardial infarction) J Am Coll Cardiol. 2010;55:102–110. doi: 10.1016/j.jacc.2009.08.007. [DOI] [PubMed] [Google Scholar]
- 118.Borgia F, Goodman SG, Halvorsen S, Cantor WJ, Piscione F, Le May MR, Fernández-Avilés F, Sánchez PL, Dimopoulos K, Scheller B, et al. Early routine percutaneous coronary intervention after fibrinolysis vs. standard therapy in ST-segment elevation myocardial infarction: a meta-analysis. Eur Heart J. 2010;31:2156–2169. doi: 10.1093/eurheartj/ehq204. [DOI] [PubMed] [Google Scholar]
- 119.Armstrong PW, Gershlick AH, Goldstein P, Wilcox R, Danays T, Lambert Y, Sulimov V, Rosell Ortiz F, Ostojic M, Welsh RC, et al. Fibrinolysis or primary PCI in ST-segment elevation myocardial infarction. N Engl J Med. 2013;368:1379–1387. doi: 10.1056/NEJMoa1301092. [DOI] [PubMed] [Google Scholar]
- 120.Primary versus tenecteplase-facilitated percutaneous coronary intervention in patients with ST-segment elevation acute myocardial infarction (ASSENT-4 PCI): randomised trial. Lancet. 2006;367:569–578. doi: 10.1016/S0140-6736(06)68147-6. [DOI] [PubMed] [Google Scholar]
- 121.Ellis SG, Tendera M, de Belder MA, van Boven AJ, Widimsky P, Janssens L, Andersen HR, Betriu A, Savonitto S, Adamus J, et al. Facilitated PCI in patients with ST-elevation myocardial infarction. N Engl J Med. 2008;358:2205–2217. doi: 10.1056/NEJMoa0706816. [DOI] [PubMed] [Google Scholar]
- 122.Keeley EC, Boura JA, Grines CL. Primary angioplasty versus intravenous thrombolytic therapy for acute myocardial infarction: a quantitative review of 23 randomised trials. Lancet. 2003;361:13–20. doi: 10.1016/S0140-6736(03)12113-7. [DOI] [PubMed] [Google Scholar]
- 123.Niccoli G, Burzotta F, Galiuto L, Crea F. Myocardial no-reflow in humans. J Am Coll Cardiol. 2009;54:281–292. doi: 10.1016/j.jacc.2009.03.054. [DOI] [PubMed] [Google Scholar]
- 124.Pinto DS, Frederick PD, Chakrabarti AK, Kirtane AJ, Ullman E, Dejam A, Miller DP, Henry TD, Gibson CM. Benefit of transferring ST-segment-elevation myocardial infarction patients for percutaneous coronary intervention compared with administration of onsite fibrinolytic declines as delays increase. Circulation. 2011;124:2512–2521. doi: 10.1161/CIRCULATIONAHA.111.018549. [DOI] [PubMed] [Google Scholar]
- 125.Concannon TW, Nelson J, Goetz J, Griffith JL. A percutaneous coronary intervention lab in every hospital? Circ Cardiovasc Qual Outcomes. 2012;5:14–20. doi: 10.1161/CIRCOUTCOMES.111.963868. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Concannon TW, Kent DM, Normand SL, Newhouse JP, Griffith JL, Cohen J, Beshansky JR, Wong JB, Aversano T, Selker HP. Comparative effectiveness of ST-segment-elevation myocardial infarction regionalization strategies. Circ Cardiovasc Qual Outcomes. 2010;3:506–513. doi: 10.1161/CIRCOUTCOMES.109.908541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Aversano T, Aversano LT, Passamani E, Knatterud GL, Terrin ML, Williams DO, Forman SA. Thrombolytic therapy vs primary percutaneous coronary intervention for myocardial infarction in patients presenting to hospitals without on-site cardiac surgery: a randomized controlled trial. JAMA. 2002;287:1943–1951. doi: 10.1001/jama.287.15.1943. [DOI] [PubMed] [Google Scholar]
- 128.Henry TD, Sharkey SW, Burke MN, Chavez IJ, Graham KJ, Henry CR, Lips DL, Madison JD, Menssen KM, Mooney MR, et al. A regional system to provide timely access to percutaneous coronary intervention for ST-elevation myocardial infarction. Circulation. 2007;116:721–728. doi: 10.1161/CIRCULATIONAHA.107.694141. [DOI] [PubMed] [Google Scholar]
- 129.Aguirre FV, Varghese JJ, Kelley MP, Lam W, Lucore CL, Gill JB, Page L, Turner L, Davis C, Mikell FL. Rural interhospital transfer of ST-elevation myocardial infarction patients for percutaneous coronary revascularization: the Stat Heart Program. Circulation. 2008;117:1145–1152. doi: 10.1161/CIRCULATIONAHA.107.728519. [DOI] [PubMed] [Google Scholar]
- 130.Hochman JS, Reynolds HR, Dzavík V, Buller CE, Ruzyllo W, Sadowski ZP, Maggioni AP, Carvalho AC, Rankin JM, White HD, et al. Long-term effects of percutaneous coronary intervention of the totally occluded infarct-related artery in the subacute phase after myocardial infarction. Circulation. 2011;124:2320–2328. doi: 10.1161/CIRCULATIONAHA.111.041749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Corpus RA, House JA, Marso SP, Grantham JA, Huber KC, Laster SB, Johnson WL, Daniels WC, Barth CW, Giorgi LV, et al. Multivessel percutaneous coronary intervention in patients with multivessel disease and acute myocardial infarction. Am Heart J. 2004;148:493–500. doi: 10.1016/j.ahj.2004.03.051. [DOI] [PubMed] [Google Scholar]
- 132.Kong JA, Chou ET, Minutello RM, Wong SC, Hong MK. Safety of single versus multi-vessel angioplasty for patients with acute myocardial infarction and multi-vessel coronary artery disease: report from the New York State Angioplasty Registry. Coron Artery Dis. 2006;17:71–75. doi: 10.1097/00019501-200602000-00012. [DOI] [PubMed] [Google Scholar]
- 133.Vlaar PJ, Mahmoud KD, Holmes DR, van Valkenhoef G, Hillege HL, van der Horst IC, Zijlstra F, de Smet BJ. Culprit vessel only versus multivessel and staged percutaneous coronary intervention for multivessel disease in patients presenting with ST-segment elevation myocardial infarction: a pairwise and network meta-analysis. J Am Coll Cardiol. 2011;58:692–703. doi: 10.1016/j.jacc.2011.03.046. [DOI] [PubMed] [Google Scholar]
- 134.Hannan EL, Samadashvili Z, Walford G, Holmes DR, Jacobs AK, Stamato NJ, Venditti FJ, Sharma S, King SB. Culprit vessel percutaneous coronary intervention versus multivessel and staged percutaneous coronary intervention for ST-segment elevation myocardial infarction patients with multivessel disease. JACC Cardiovasc Interv. 2010;3:22–31. doi: 10.1016/j.jcin.2009.10.017. [DOI] [PubMed] [Google Scholar]
- 135.Ntalianis A, Sels JW, Davidavicius G, Tanaka N, Muller O, Trana C, Barbato E, Hamilos M, Mangiacapra F, Heyndrickx GR, et al. Fractional flow reserve for the assessment of nonculprit coronary artery stenoses in patients with acute myocardial infarction. JACC Cardiovasc Interv. 2010;3:1274–1281. doi: 10.1016/j.jcin.2010.08.025. [DOI] [PubMed] [Google Scholar]
- 136.Wald DS, Morris JK, Wald NJ, Chase AJ, Edwards RJ, Hughes LO, Berry C, Oldroyd KG. Randomized trial of preventive angioplasty in myocardial infarction. N Engl J Med. 2013;369:1115–1123. doi: 10.1056/NEJMoa1305520. [DOI] [PubMed] [Google Scholar]
- 137.Jolly SS, Yusuf S, Cairns J, Niemelä K, Xavier D, Widimsky P, Budaj A, Niemelä M, Valentin V, Lewis BS, et al. Radial versus femoral access for coronary angiography and intervention in patients with acute coronary syndromes (RIVAL): a randomised, parallel group, multicentre trial. Lancet. 2011;377:1409–1420. doi: 10.1016/S0140-6736(11)60404-2. [DOI] [PubMed] [Google Scholar]
- 138.Romagnoli E, Biondi-Zoccai G, Sciahbasi A, Politi L, Rigattieri S, Pendenza G, Summaria F, Patrizi R, Borghi A, Di Russo C, et al. Radial versus femoral randomized investigation in ST-segment elevation acute coronary syndrome: the RIFLE-STEACS (Radial Versus Femoral Randomized Investigation in ST-Elevation Acute Coronary Syndrome) study. J Am Coll Cardiol. 2012;60:2481–2489. doi: 10.1016/j.jacc.2012.06.017. [DOI] [PubMed] [Google Scholar]
- 139.Lee MS, Wolfe M, Stone GW. Transradial versus transfemoral percutaneous coronary intervention in acute coronary syndromes: re-evaluation of the current body of evidence. J Am Coll Cardiol Intv. 2013;6:1149–1150. doi: 10.1016/j.jcin.2013.08.003. [DOI] [PubMed] [Google Scholar]
- 140.Jolly SS, Cairns J, Niemela K, Steg PG, Natarajan MK, Cheema AN, Rao SV, Cantor WJ, Džavík V, Budaj A, et al. Effect of radial versus femoral access on radiation dose and the importance of procedural volume: a substudy of the multicenter randomized RIVAL trial. JACC Cardiovasc Interv. 2013;6:258–266. doi: 10.1016/j.jcin.2012.10.016. [DOI] [PubMed] [Google Scholar]
- 141.Pancholy S, Patel T, Sanghvi K, Thomas M, Patel T. Comparison of door-to-balloon times for primary PCI using transradial versus transfemoral approach. Catheter Cardiovasc Interv. 2010;75:991–995. doi: 10.1002/ccd.22425. [DOI] [PubMed] [Google Scholar]
- 142.Burzotta F, De Vita M, Gu YL, Isshiki T, Lefèvre T, Kaltoft A, Dudek D, Sardella G, Orrego PS, Antoniucci D, et al. Clinical impact of thrombectomy in acute ST-elevation myocardial infarction: an individual patient-data pooled analysis of 11 trials. Eur Heart J. 2009;30:2193–2203. doi: 10.1093/eurheartj/ehp348. [DOI] [PubMed] [Google Scholar]
- 143.Ali A, Cox D, Dib N, Brodie B, Berman D, Gupta N, Browne K, Iwaoka R, Azrin M, Stapleton D, et al. Rheolytic thrombectomy with percutaneous coronary intervention for infarct size reduction in acute myocardial infarction: 30-day results from a multicenter randomized study. J Am Coll Cardiol. 2006;48:244–252. doi: 10.1016/j.jacc.2006.03.044. [DOI] [PubMed] [Google Scholar]
- 144.Antoniucci D, Valenti R, Migliorini A, Parodi G, Memisha G, Santoro GM, Sciagrà R. Comparison of rheolytic thrombectomy before direct infarct artery stenting versus direct stenting alone in patients undergoing percutaneous coronary intervention for acute myocardial infarction. Am J Cardiol. 2004;93:1033–1035. doi: 10.1016/j.amjcard.2004.01.011. [DOI] [PubMed] [Google Scholar]
- 145.Vlaar PJ, Svilaas T, van der Horst IC, Diercks GF, Fokkema ML, de Smet BJ, van den Heuvel AF, Anthonio RL, Jessurun GA, Tan ES, et al. Cardiac death and reinfarction after 1 year in the Thrombus Aspiration during Percutaneous coronary intervention in Acute myocardial infarction Study (TAPAS): a 1-year follow-up study. Lancet. 2008;371:1915–1920. doi: 10.1016/S0140-6736(08)60833-8. [DOI] [PubMed] [Google Scholar]
- 146.Sardella G, Mancone M, Canali E, Di Roma A, Benedetti G, Stio R, Badagliacca R, Lucisano L, Agati L, Fedele F. Impact of thrombectomy with EXPort Catheter in Infarct-Related Artery during Primary Percutaneous Coronary Intervention (EXPIRA Trial) on cardiac death. Am J Cardiol. 2010;106:624–629. doi: 10.1016/j.amjcard.2010.04.014. [DOI] [PubMed] [Google Scholar]
- 147.Bavry AA, Kumbhani DJ, Bhatt DL. Role of adjunctive thrombectomy and embolic protection devices in acute myocardial infarction: a comprehensive meta-analysis of randomized trials. Eur Heart J. 2008;29:2989–3001. doi: 10.1093/eurheartj/ehn421. [DOI] [PubMed] [Google Scholar]
- 148.Kumbhani DJ, Bavry AA, Desai MY, Bangalore S, Bhatt DL. Role of aspiration and mechanical thrombectomy in patients with acute myocardial infarction undergoing primary angioplasty: an updated meta-analysis of randomized trials. J Am Coll Cardiol. 2013;62:1409–1418. doi: 10.1016/j.jacc.2013.04.025. [DOI] [PubMed] [Google Scholar]
- 149.Jolly S, Cairns J, Yusuf S, Meeks B, Pogue J, Rokoss M, Kedev S, Thabane L, Stankovic G, Niemela K, et al. Randomized trial of primary PCI with or without routine manual thrombectomy. New England Journal Medicine. 2015;372:1389–1398. doi: 10.1056/NEJMoa1415098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Nordmann AJ, Hengstler P, Harr T, Young J, Bucher HC. Clinical outcomes of primary stenting versus balloon angioplasty in patients with myocardial infarction: a meta-analysis of randomized controlled trials. Am J Med. 2004;116:253–262. doi: 10.1016/j.amjmed.2003.08.035. [DOI] [PubMed] [Google Scholar]
- 151.Kastrati A, Dibra A, Spaulding C, Laarman GJ, Menichelli M, Valgimigli M, Di Lorenzo E, Kaiser C, Tierala I, Mehilli J, et al. Meta-analysis of randomized trials on drug-eluting stents vs. bare-metal stents in patients with acute myocardial infarction. Eur Heart J. 2007;28:2706–2713. doi: 10.1093/eurheartj/ehm402. [DOI] [PubMed] [Google Scholar]
- 152.Räber L, Wohlwend L, Wigger M, Togni M, Wandel S, Wenaweser P, Cook S, Moschovitis A, Vogel R, Kalesan B, et al. Five-year clinical and angiographic outcomes of a randomized comparison of sirolimus-eluting and paclitaxel-eluting stents: results of the Sirolimus-Eluting Versus Paclitaxel-Eluting Stents for Coronary Revascularization LATE trial. Circulation. 2011;123:2819–2828, 6 p following 2828. doi: 10.1161/CIRCULATIONAHA.110.004762. [DOI] [PubMed] [Google Scholar]
- 153.Sabate M, Cequier A, Iñiguez A, Serra A, Hernandez-Antolin R, Mainar V, Valgimigli M, Tespili M, den Heijer P, Bethencourt A, et al. Everolimus-eluting stent versus bare-metal stent in ST-segment elevation myocardial infarction (EXAMINATION): 1 year results of a randomised controlled trial. Lancet. 2012;380:1482–1490. doi: 10.1016/S0140-6736(12)61223-9. [DOI] [PubMed] [Google Scholar]
- 154.de Belder A, de la Torre Hernandez JM, Lopez-Palop R, O’Kane P, Hernandez Hernandez F, Strange J, Gimeno F, Cotton J, Diaz Fernandez JF, Carrillo Saez P, et al. A prospective randomized trial of everolimus-eluting stents versus bare-metal stents in octogenarians: the XIMA Trial (Xience or Vision Stents for the Management of Angina in the Elderly) J Am Coll Cardiol. 2014;63:1371–1375. doi: 10.1016/j.jacc.2013.10.053. [DOI] [PubMed] [Google Scholar]
- 155.Dewilde WJ, Oirbans T, Verheugt FW, Kelder JC, De Smet BJ, Herrman JP, Adriaenssens T, Vrolix M, Heestermans AA, Vis MM, et al. Use of clopidogrel with or without aspirin in patients taking oral anticoagulant therapy and undergoing percutaneous coronary intervention: an open-label, randomised, controlled trial. Lancet. 2013;381:1107–1115. doi: 10.1016/S0140-6736(12)62177-1. [DOI] [PubMed] [Google Scholar]
- 156.Montalescot G, Zeymer U, Silvain J, Boulanger B, Cohen M, Goldstein P, Ecollan P, Combes X, Huber K, Pollack C, et al. Intravenous enoxaparin or unfractionated heparin in primary percutaneous coronary intervention for ST-elevation myocardial infarction: the international randomised open-label ATOLL trial. Lancet. 2011;378:693–703. doi: 10.1016/S0140-6736(11)60876-3. [DOI] [PubMed] [Google Scholar]
- 157.Yusuf S, Mehta SR, Chrolavicius S, Afzal R, Pogue J, Granger CB, Budaj A, Peters RJ, Bassand JP, Wallentin L, et al. Effects of fondaparinux on mortality and reinfarction in patients with acute ST-segment elevation myocardial infarction: the OASIS-6 randomized trial. JAMA. 2006;295:1519–1530. doi: 10.1001/jama.295.13.joc60038. [DOI] [PubMed] [Google Scholar]
- 158.Stone G, Mehran R, Goldstein P, Witzenbichler B, van’t Hof A, Guagliumi G, Hamm C, Genereux P, Clemmensen P, Pocock S, et al. Bivalirudin versus heparin with or without glycoprotein IIb, IIa inhibition in patients with STEM. J Am Coll Cardiol. 2015;65:27–38. doi: 10.1016/j.jacc.2014.10.029. [DOI] [PubMed] [Google Scholar]
- 159.Mehta SR, Bassand JP, Chrolavicius S, Diaz R, Eikelboom JW, Fox KA, Granger CB, Jolly S, Joyner CD, Rupprecht HJ, et al. Dose comparisons of clopidogrel and aspirin in acute coronary syndromes. N Engl J Med. 2010;363:930–942. doi: 10.1056/NEJMoa0909475. [DOI] [PubMed] [Google Scholar]
- 160.Yusuf S, Zhao F, Mehta SR, Chrolavicius S, Tognoni G, Fox KK. Effects of clopidogrel in addition to aspirin in patients with acute coronary syndromes without ST-segment elevation. N Engl J Med. 2001;345:494–502. doi: 10.1056/NEJMoa010746. [DOI] [PubMed] [Google Scholar]
- 161.Mehta SR, Yusuf S, Peters RJ, Bertrand ME, Lewis BS, Natarajan MK, Malmberg K, Rupprecht H, Zhao F, Chrolavicius S, et al. Effects of pretreatment with clopidogrel and aspirin followed by long-term therapy in patients undergoing percutaneous coronary intervention: the PCI-CURE study. Lancet. 2001;358:527–533. doi: 10.1016/s0140-6736(01)05701-4. [DOI] [PubMed] [Google Scholar]
- 162.Di Sciascio G, Patti G, Pasceri V, Gatto L, Colonna G, Montinaro A. Effectiveness of in-laboratory high-dose clopidogrel loading versus routine pre-load in patients undergoing percutaneous coronary intervention: results of the ARMYDA-5 PRELOAD (Antiplatelet therapy for Reduction of MYocardial Damage during Angioplasty) randomized trial. J Am Coll Cardiol. 2010;56:550–557. doi: 10.1016/j.jacc.2010.01.067. [DOI] [PubMed] [Google Scholar]
- 163.Giusti B, Gori AM, Marcucci R, Saracini C, Sestini I, Paniccia R, Buonamici P, Antoniucci D, Abbate R, Gensini GF. Relation of cytochrome P450 2C19 loss-of-function polymorphism to occurrence of drug-eluting coronary stent thrombosis. Am J Cardiol. 2009;103:806–811. doi: 10.1016/j.amjcard.2008.11.048. [DOI] [PubMed] [Google Scholar]
- 164.Collet JP, Hulot JS, Pena A, Villard E, Esteve JB, Silvain J, Payot L, Brugier D, Cayla G, Beygui F, et al. Cytochrome P450 2C19 polymorphism in young patients treated with clopidogrel after myocardial infarction: a cohort study. Lancet. 2009;373:309–317. doi: 10.1016/S0140-6736(08)61845-0. [DOI] [PubMed] [Google Scholar]
- 165.Sibbing D, Stegherr J, Latz W, Koch W, Mehilli J, Dörrler K, Morath T, Schömig A, Kastrati A, von Beckerath N. Cytochrome P450 2C19 loss-of-function polymorphism and stent thrombosis following percutaneous coronary intervention. Eur Heart J. 2009;30:916–922. doi: 10.1093/eurheartj/ehp041. [DOI] [PubMed] [Google Scholar]
- 166.Mega JL, Close SL, Wiviott SD, Shen L, Hockett RD, Brandt JT, Walker JR, Antman EM, Macias W, Braunwald E, et al. Cytochrome p-450 polymorphisms and response to clopidogrel. N Engl J Med. 2009;360:354–362. doi: 10.1056/NEJMoa0809171. [DOI] [PubMed] [Google Scholar]
- 167.Paré G, Mehta SR, Yusuf S, Anand SS, Connolly SJ, Hirsh J, Simonsen K, Bhatt DL, Fox KA, Eikelboom JW. Effects of CYP2C19 genotype on outcomes of clopidogrel treatment. N Engl J Med. 2010;363:1704–1714. doi: 10.1056/NEJMoa1008410. [DOI] [PubMed] [Google Scholar]
- 168.Bhatt DL, Cryer BL, Contant CF, Cohen M, Lanas A, Schnitzer TJ, Shook TL, Lapuerta P, Goldsmith MA, Laine L, et al. Clopidogrel with or without omeprazole in coronary artery disease. N Engl J Med. 2010;363:1909–1917. doi: 10.1056/NEJMoa1007964. [DOI] [PubMed] [Google Scholar]
- 169.Wiviott SD, Braunwald E, McCabe CH, Montalescot G, Ruzyllo W, Gottlieb S, Neumann FJ, Ardissino D, De Servi S, Murphy SA, et al. Prasugrel versus clopidogrel in patients with acute coronary syndromes. N Engl J Med. 2007;357:2001–2015. doi: 10.1056/NEJMoa0706482. [DOI] [PubMed] [Google Scholar]
- 170.Wallentin L, Becker RC, Budaj A, Cannon CP, Emanuelsson H, Held C, Horrow J, Husted S, James S, Katus H, et al. Ticagrelor versus clopidogrel in patients with acute coronary syndromes. N Engl J Med. 2009;361:1045–1057. doi: 10.1056/NEJMoa0904327. [DOI] [PubMed] [Google Scholar]
- 171.ACC/AHA 2013 STEMI Guidelines. J Am Coll Cardiol. 2013;61:e78–e140. doi: 10.1016/j.jacc.2012.11.019. [DOI] [PubMed] [Google Scholar]
- 172.Gwon HC, Hahn JY, Park KW, Song YB, Chae IH, Lim DS, Han KR, Choi JH, Choi SH, Kang HJ, et al. Six-month versus 12-month dual antiplatelet therapy after implantation of drug-eluting stents: the Efficacy of Xience/Promus Versus Cypher to Reduce Late Loss After Stenting (EXCELLENT) randomized, multicenter study. Circulation. 2012;125:505–513. doi: 10.1161/CIRCULATIONAHA.111.059022. [DOI] [PubMed] [Google Scholar]
- 173.Valgimigli M, Campo G, Monti M, Vranckx P, Percoco G, Tumscitz C, Castriota F, Colombo F, Tebaldi M, Fucà G, et al. Short- versus long-term duration of dual-antiplatelet therapy after coronary stenting: a randomized multicenter trial. Circulation. 2012;125:2015–2026. doi: 10.1161/CIRCULATIONAHA.111.071589. [DOI] [PubMed] [Google Scholar]
- 174.Kim BK, Hong MK, Shin DH, Nam CM, Kim JS, Ko YG, Choi D, Kang TS, Park BE, Kang WC, et al. A new strategy for discontinuation of dual antiplatelet therapy: the RESET Trial (REal Safety and Efficacy of 3-month dual antiplatelet Therapy following Endeavor zotarolimus-eluting stent implantation) J Am Coll Cardiol. 2012;60:1340–1348. doi: 10.1016/j.jacc.2012.06.043. [DOI] [PubMed] [Google Scholar]
- 175.The OPTIMZE Trial Group. Three versus Twelve Months of Dual Antiplatelet Therapy After Zotarolimus Eluting Stents. The OPTIMIZE Randomized Trial: JAMA; 2013. [DOI] [PubMed] [Google Scholar]
- 176.ten Berg JM, van ‘t Hof AW, Dill T, Heestermans T, van Werkum JW, Mosterd A, van Houwelingen G, Koopmans PC, Stella PR, Boersma E, et al. Effect of early, pre-hospital initiation of high bolus dose tirofiban in patients with ST-segment elevation myocardial infarction on short- and long-term clinical outcome. J Am Coll Cardiol. 2010;55:2446–2455. doi: 10.1016/j.jacc.2009.11.091. [DOI] [PubMed] [Google Scholar]
- 177.El Khoury C, Dubien PY, Mercier C, Belle L, Debaty G, Capel O, Perret T, Savary D, Serre P, Bonnefoy E. Prehospital high-dose tirofiban in patients undergoing primary percutaneous intervention. The AGIR-2 study. Arch Cardiovasc Dis. 2010;103:285–292. doi: 10.1016/j.acvd.2010.04.005. [DOI] [PubMed] [Google Scholar]
- 178.Van’t Hof AW, Ten Berg J, Heestermans T, Dill T, Funck RC, van Werkum W, Dambrink JH, Suryapranata H, van Houwelingen G, Ottervanger JP, et al. Prehospital initiation of tirofiban in patients with ST-elevation myocardial infarction undergoing primary angioplasty (On-TIME 2): a multicentre, double-blind, randomised controlled trial. Lancet. 2008;372:537–546. doi: 10.1016/S0140-6736(08)61235-0. [DOI] [PubMed] [Google Scholar]
- 179.DeLuca G, Bellandi F, Huber K, Noc M, Petronio AS, Arntz HR, Maioli M, Gabriel HM, Zorman S, DE Carlo M, et al. Early glycoprotein IIb-IIIa inhibitors in primary angioplasty-abciximab long-term results (EGYPT-ALT) cooperation: individual patient’s data meta-analysis. J Thromb Haemost. 2011;9:2361–2370. doi: 10.1111/j.1538-7836.2011.04513.x. [DOI] [PubMed] [Google Scholar]
- 180.Akerblom A, James SK, Koutouzis M, Lagerqvist B, Stenestrand U, Svennblad B, Oldgren J. Eptifibatide is noninferior to abciximab in primary percutaneous coronary intervention: results from the SCAAR (Swedish Coronary Angiography and Angioplasty Registry) J Am Coll Cardiol. 2010;56:470–475. doi: 10.1016/j.jacc.2009.10.093. [DOI] [PubMed] [Google Scholar]
- 181.Gu YL, Kampinga MA, Wieringa WG, Fokkema ML, Nijsten MW, Hillege HL, van den Heuvel AF, Tan ES, Pundziute G, van der Werf R, et al. Intracoronary versus intravenous administration of abciximab in patients with ST-segment elevation myocardial infarction undergoing primary percutaneous coronary intervention with thrombus aspiration: the comparison of intracoronary versus intravenous abciximab administration during emergency reperfusion of ST-segment elevation myocardial infarction (CICERO) trial. Circulation. 2010;122:2709–2717. doi: 10.1161/CIRCULATIONAHA.110.002741. [DOI] [PubMed] [Google Scholar]
- 182.Shimada YJ, Nakra NC, Fox JT, Kanei Y. Meta-analysis of prospective randomized controlled trials comparing intracoronary versus intravenous abciximab in patients with ST-elevation myocardial infarction undergoing primary percutaneous coronary intervention. Am J Cardiol. 2012;109:624–628. doi: 10.1016/j.amjcard.2011.10.016. [DOI] [PubMed] [Google Scholar]
- 183.Bertrand OF, Rodés-Cabau J, Larose E, Rinfret S, Gaudreault V, Proulx G, Barbeau G, Déry JP, Gleeton O, Manh-Nguyen C, Noël B, Roy L, Costerousse O, De Larochellière R. Intracoronary compared to intravenous Abciximab and high-dose bolus compared to standard dose in patients with ST-segment elevation myocardial infarction undergoing transradial primary percutaneous coronary intervention: a two-by-two factorial placebo-controlled randomized study. Am J Cardiol. 2010;105:1520–1527. doi: 10.1016/j.amjcard.2010.01.006. [DOI] [PubMed] [Google Scholar]
- 184.Bolli R, Becker L, Gross G, Mentzer R, Balshaw D, Lathrop DA. Myocardial protection at a crossroads: the need for translation into clinical therapy. Circ Res. 2004;95:125–134. doi: 10.1161/01.RES.0000137171.97172.d7. [DOI] [PubMed] [Google Scholar]
- 185.Zweier JL. Measurement of superoxide-derived free radicals in the reperfused heart. Evidence for a free radical mechanism of reperfusion injury. J Biol Chem. 1988;263:1353–1357. [PubMed] [Google Scholar]
- 186.Downey JM. Free radicals and their involvement during long-term myocardial ischemia and reperfusion. Annu Rev Physiol. 1990;52:487–504. doi: 10.1146/annurev.ph.52.030190.002415. [DOI] [PubMed] [Google Scholar]
- 187.Piper HM, García-Dorado D, Ovize M. A fresh look at reperfusion injury. Cardiovasc Res. 1998;38:291–300. doi: 10.1016/s0008-6363(98)00033-9. [DOI] [PubMed] [Google Scholar]
- 188.Vinten-Johansen J. Involvement of neutrophils in the pathogenesis of lethal myocardial reperfusion injury. Cardiovasc Res. 2004;61:481–497. doi: 10.1016/j.cardiores.2003.10.011. [DOI] [PubMed] [Google Scholar]
- 189.Kim JS, Jin Y, Lemasters JJ. Reactive oxygen species, but not Ca2+ overloading, trigger pH- and mitochondrial permeability transition-dependent death of adult rat myocytes after ischemia-reperfusion. Am J Physiol Heart Circ Physiol. 2006;290:H2024–H2034. doi: 10.1152/ajpheart.00683.2005. [DOI] [PubMed] [Google Scholar]
- 190.Downey JM, Davis AM, Cohen MV. Signaling pathways in ischemic preconditioning. Heart Fail Rev. 2007;12:181–188. doi: 10.1007/s10741-007-9025-2. [DOI] [PubMed] [Google Scholar]
- 191.Yellon DM, Downey JM. Preconditioning the myocardium: from cellular physiology to clinical cardiology. Physiol Rev. 2003;83:1113–1151. doi: 10.1152/physrev.00009.2003. [DOI] [PubMed] [Google Scholar]
- 192.Murry CE, Jennings RB, Reimer KA. Preconditioning with ischemia: a delay of lethal cell injury in ischemic myocardium. Circulation. 1986;74:1124–1136. doi: 10.1161/01.cir.74.5.1124. [DOI] [PubMed] [Google Scholar]
- 193.Zhao ZQ, Corvera JS, Halkos ME, Kerendi F, Wang NP, Guyton RA, Vinten-Johansen J. Inhibition of myocardial injury by ischemic postconditioning during reperfusion: comparison with ischemic preconditioning. Am J Physiol Heart Circ Physiol. 2003;285:H579–H588. doi: 10.1152/ajpheart.01064.2002. [DOI] [PubMed] [Google Scholar]
- 194.Staat P, Rioufol G, Piot C, Cottin Y, Cung TT, L’Huillier I, Aupetit JF, Bonnefoy E, Finet G, André-Fouët X, et al. Postconditioning the human heart. Circulation. 2005;112:2143–2148. doi: 10.1161/CIRCULATIONAHA.105.558122. [DOI] [PubMed] [Google Scholar]
- 195.Laskey WK, Yoon S, Calzada N, Ricciardi MJ. Concordant improvements in coronary flow reserve and ST-segment resolution during percutaneous coronary intervention for acute myocardial infarction: a benefit of postconditioning. Catheter Cardiovasc Interv. 2008;72:212–220. doi: 10.1002/ccd.21583. [DOI] [PubMed] [Google Scholar]
- 196.Griffiths EJ, Halestrap AP. Mitochondrial non-specific pores remain closed during cardiac ischaemia, but open upon reperfusion. Biochem J. 1995;307(Pt 1):93–98. doi: 10.1042/bj3070093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 197.Piot C, Croisille P, Staat P, Thibault H, Rioufol G, Mewton N, Elbelghiti R, Cung TT, Bonnefoy E, Angoulvant D, et al. Effect of cyclosporine on reperfusion injury in acute myocardial infarction. N Engl J Med. 2008;359:473–481. doi: 10.1056/NEJMoa071142. [DOI] [PubMed] [Google Scholar]
- 198.Andreka G, Vertesaljai M, Szantho G, Font G, Piroth Z, Fontos G, Juhasz ED, Szekely L, Szelid Z, Turner MS, et al. Remote ischaemic postconditioning protects the heart during acute myocardial infarction in pigs. Heart. 2007;93:749–752. doi: 10.1136/hrt.2006.114504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 199.Bøtker HE, Kharbanda R, Schmidt MR, Bøttcher M, Kaltoft AK, Terkelsen CJ, Munk K, Andersen NH, Hansen TM, Trautner S, et al. Remote ischaemic conditioning before hospital admission, as a complement to angioplasty, and effect on myocardial salvage in patients with acute myocardial infarction: a randomised trial. Lancet. 2010;375:727–734. doi: 10.1016/S0140-6736(09)62001-8. [DOI] [PubMed] [Google Scholar]
- 200.Cohen MV, Downey JM. Adenosine: trigger and mediator of cardioprotection. Basic Res Cardiol. 2008;103:203–215. doi: 10.1007/s00395-007-0687-7. [DOI] [PubMed] [Google Scholar]
- 201.Mahaffey KW, Puma JA, Barbagelata NA, DiCarli MF, Leesar MA, Browne KF, Eisenberg PR, Bolli R, Casas AC, Molina-Viamonte V, et al. Adenosine as an adjunct to thrombolytic therapy for acute myocardial infarction: results of a multicenter, randomized, placebo-controlled trial: the Acute Myocardial Infarction Study of ADenosine (AMISTAD) trial. J Am Coll Cardiol. 1999;34:1711–1720. doi: 10.1016/s0735-1097(99)00418-0. [DOI] [PubMed] [Google Scholar]
- 202.Ross AM, Gibbons RJ, Stone GW, Kloner RA, Alexander RW. A randomized, double-blinded, placebo-controlled multicenter trial of adenosine as an adjunct to reperfusion in the treatment of acute myocardial infarction (AMISTAD-II) J Am Coll Cardiol. 2005;45:1775–1780. doi: 10.1016/j.jacc.2005.02.061. [DOI] [PubMed] [Google Scholar]
- 203.Kloner RA, Forman MB, Gibbons RJ, Ross AM, Alexander RW, Stone GW. Impact of time to therapy and reperfusion modality on the efficacy of adenosine in acute myocardial infarction: the AMISTAD-2 trial. Eur Heart J. 2006;27:2400–2405. doi: 10.1093/eurheartj/ehl094. [DOI] [PubMed] [Google Scholar]
- 204.Ibanez B, Macaya C, Sánchez-Brunete V, Pizarro G, Fernández-Friera L, Mateos A, Fernández-Ortiz A, García-Ruiz JM, García-Álvarez A, Iñiguez A, et al. Effect of early metoprolol on infarct size in ST-segment-elevation myocardial infarction patients undergoing primary percutaneous coronary intervention: the Effect of Metoprolol in Cardioprotection During an Acute Myocardial Infarction (METOCARD-CNIC) trial. Circulation. 2013;128:1495–1503. doi: 10.1161/CIRCULATIONAHA.113.003653. [DOI] [PubMed] [Google Scholar]
- 205.Freemantle N, Cleland J, Young P, Mason J, Harrison J. Beta blockade after myocardial infarction: systematic review and meta regression analysis. BMJ. 1999;318:1730–1737. doi: 10.1136/bmj.318.7200.1730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 206.Bangalore S, Steg G, Deedwania P, Crowley K, Eagle KA, Goto S, Ohman EM, Cannon CP, Smith SC, Zeymer U, et al. β-Blocker use and clinical outcomes in stable outpatients with and without coronary artery disease. JAMA. 2012;308:1340–1349. doi: 10.1001/jama.2012.12559. [DOI] [PubMed] [Google Scholar]
- 207.Kitakaze M, Asakura M, Kim J, Shintani Y, Asanuma H, Hamasaki T, Seguchi O, Myoishi M, Minamino T, Ohara T, et al. Human atrial natriuretic peptide and nicorandil as adjuncts to reperfusion treatment for acute myocardial infarction (J-WIND): two randomised trials. Lancet. 2007;370:1483–1493. doi: 10.1016/S0140-6736(07)61634-1. [DOI] [PubMed] [Google Scholar]
- 208.Tissier R, Chenoune M, Ghaleh B, Cohen MV, Downey JM, Berdeaux A. The small chill: mild hypothermia for cardioprotection? Cardiovasc Res. 2010;88:406–414. doi: 10.1093/cvr/cvq227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 209.O’Neill WW. Cooling as an Adjunctive Therapy to Percutaneous Intervention in Patients with Acute Myocardial Infarction (COOL-MI) Presented at: Transcatheter Cardiovascular Therapeutics Session;; 2003. pp. Sep 15–19; Washington, DC. [Google Scholar]
- 210.Götberg M, Olivecrona GK, Koul S, Carlsson M, Engblom H, Ugander M, van der Pals J, Algotsson L, Arheden H, Erlinge D. A pilot study of rapid cooling by cold saline and endovascular cooling before reperfusion in patients with ST-elevation myocardial infarction. Circ Cardiovasc Interv. 2010;3:400–407. doi: 10.1161/CIRCINTERVENTIONS.110.957902. [DOI] [PubMed] [Google Scholar]
- 211.Erlinge D. The Transcatheter Cardiovascular Therapeutics Meeting; 2013 Oct 30; San Francisco, CA. 2013. [Google Scholar]
- 212.Henning RJ. Stem cells in cardiac repair: Problems and Possibilities. Future Cardiol. 2013;9:875–884. doi: 10.2217/fca.13.78. [DOI] [PubMed] [Google Scholar]
- 213.Henning RJ. Stem cells in cardiac repair. Future Cardiol. 2011;7:99–117. doi: 10.2217/fca.10.109. [DOI] [PubMed] [Google Scholar]
- 214.Henning RJ. Stem cells in cardiac repair-Recent Developments and Future Directions. Interv Cardiol. 2012;7:10–13. [Google Scholar]
- 215.Assmus B, Honold J, Schächinger V, Britten MB, Fischer-Rasokat U, Lehmann R, Teupe C, Pistorius K, Martin H, Abolmaali ND, et al. Transcoronary transplantation of progenitor cells after myocardial infarction. N Engl J Med. 2006;355:1222–1232. doi: 10.1056/NEJMoa051779. [DOI] [PubMed] [Google Scholar]
- 216.Bartunek J, Vanderheyden M, Vandekerckhove B, Mansour S, De Bruyne B, De Bondt P, Van Haute I, Lootens N, Heyndrickx G, Wijns W. Intracoronary injection of CD133-positive enriched bone marrow progenitor cells promotes cardiac recovery after recent myocardial infarction: feasibility and safety. Circulation. 2005;112:I178–I183. doi: 10.1161/CIRCULATIONAHA.104.522292. [DOI] [PubMed] [Google Scholar]
- 217.Chen SL, Fang WW, Ye F, Liu YH, Qian J, Shan SJ, Zhang JJ, Chunhua RZ, Liao LM, Lin S, et al. Effect on left ventricular function of intracoronary transplantation of autologous bone marrow mesenchymal stem cells in patients with acute myocardial infarction. Am J Cardiol. 2004;94:92–95. doi: 10.1016/j.amjcard.2004.03.034. [DOI] [PubMed] [Google Scholar]
- 218.Erbs S, Linke A, Adams V, Lenk K, Thiele H, Diederich KW, Emmrich F, Kluge R, Kendziorra K, Sabri O, et al. Transplantation of blood-derived progenitor cells after recanalization of chronic coronary artery occlusion: first randomized and placebo-controlled study. Circ Res. 2005;97:756–762. doi: 10.1161/01.RES.0000185811.71306.8b. [DOI] [PubMed] [Google Scholar]
- 219.Ge J, Li Y, Qian J, Shi J, Wang Q, Niu Y, Fan B, Liu X, Zhang S, Sun A, et al. Efficacy of emergent transcatheter transplantation of stem cells for treatment of acute myocardial infarction (TCT-STAMI) Heart. 2006;92:1764–1767. doi: 10.1136/hrt.2005.085431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 220.Hendrikx M, Hensen K, Clijsters C, Jongen H, Koninckx R, Bijnens E, Ingels M, Jacobs A, Geukens R, Dendale P, et al. Recovery of regional but not global contractile function by the direct intramyocardial autologous bone marrow transplantation: results from a randomized controlled clinical trial. Circulation. 2006;114:I101–I107. doi: 10.1161/CIRCULATIONAHA.105.000505. [DOI] [PubMed] [Google Scholar]
- 221.Janssens S, Dubois C, Bogaert J, Theunissen K, Deroose C, Desmet W, Kalantzi M, Herbots L, Sinnaeve P, Dens J, et al. Autologous bone marrow-derived stem-cell transfer in patients with ST-segment elevation myocardial infarction: double-blind, randomised controlled trial. Lancet. 2006;367:113–121. doi: 10.1016/S0140-6736(05)67861-0. [DOI] [PubMed] [Google Scholar]
- 222.Kang HJ, Lee HY, Na SH, Chang SA, Park KW, Kim HK, Kim SY, Chang HJ, Lee W, Kang WJ, et al. Differential effect of intracoronary infusion of mobilized peripheral blood stem cells by granulocyte colony-stimulating factor on left ventricular function and remodeling in patients with acute myocardial infarction versus old myocardial infarction: the MAGIC Cell-3-DES randomized, controlled trial. Circulation. 2006;114:I145–I151. doi: 10.1161/CIRCULATIONAHA.105.001107. [DOI] [PubMed] [Google Scholar]
- 223.Katritsis DG, Sotiropoulou PA, Karvouni E, Karabinos I, Korovesis S, Perez SA, Voridis EM, Papamichail M. Transcoronary transplantation of autologous mesenchymal stem cells and endothelial progenitors into infarcted human myocardium. Catheter Cardiovasc Interv. 2005;65:321–329. doi: 10.1002/ccd.20406. [DOI] [PubMed] [Google Scholar]
- 224.Lunde K, Solheim S, Aakhus S, Arnesen H, Abdelnoor M, Egeland T, Endresen K, Ilebekk A, Mangschau A, Fjeld JG, et al. Intracoronary injection of mononuclear bone marrow cells in acute myocardial infarction. N Engl J Med. 2006;355:1199–1209. doi: 10.1056/NEJMoa055706. [DOI] [PubMed] [Google Scholar]
- 225.Lunde K, Solheim S, Forfang K, Arnesen H, Brinch L, Bjørnerheim R, Ragnarsson A, Egeland T, Endresen K, Ilebekk A, et al. Anterior myocardial infarction with acute percutaneous coronary intervention and intracoronary injection of autologous mononuclear bone marrow cells: safety, clinical outcome, and serial changes in left ventricular function during 12-months’ follow-up. J Am Coll Cardiol. 2008;51:674–676. doi: 10.1016/j.jacc.2007.10.032. [DOI] [PubMed] [Google Scholar]
- 226.Meyer GP, Wollert KC, Lotz J, Steffens J, Lippolt P, Fichtner S, Hecker H, Schaefer A, Arseniev L, Hertenstein B, et al. Intracoronary bone marrow cell transfer after myocardial infarction: eighteen months’ follow-up data from the randomized, controlled BOOST (BOne marrOw transfer to enhance ST-elevation infarct regeneration) trial. Circulation. 2006;113:1287–1294. doi: 10.1161/CIRCULATIONAHA.105.575118. [DOI] [PubMed] [Google Scholar]
- 227.Mocini D, Staibano M, Mele L, Giannantoni P, Menichella G, Colivicchi F, Sordini P, Salera P, Tubaro M, Santini M. Autologous bone marrow mononuclear cell transplantation in patients undergoing coronary artery bypass grafting. Am Heart J. 2006;151:192–197. doi: 10.1016/j.ahj.2005.02.001. [DOI] [PubMed] [Google Scholar]
- 228.Perin EC, Dohmann HF, Borojevic R, Silva SA, Sousa AL, Silva GV, Mesquita CT, Belém L, Vaughn WK, Rangel FO, et al. Improved exercise capacity and ischemia 6 and 12 months after transendocardial injection of autologous bone marrow mononuclear cells for ischemic cardiomyopathy. Circulation. 2004;110:II213–II218. doi: 10.1161/01.CIR.0000138398.77550.62. [DOI] [PubMed] [Google Scholar]
- 229.Ruan W, Pan CZ, Huang GQ, Li YL, Ge JB, Shu XH. Assessment of left ventricular segmental function after autologous bone marrow stem cells transplantation in patients with acute myocardial infarction by tissue tracking and strain imaging. Chin Med J (Engl) 2005;118:1175–1181. [PubMed] [Google Scholar]
- 230.Schächinger V, Erbs S, Elsässer A, Haberbosch W, Hambrecht R, Hölschermann H, Yu J, Corti R, Mathey DG, Hamm CW, et al. Intracoronary bone marrow-derived progenitor cells in acute myocardial infarction. N Engl J Med. 2006;355:1210–1221. doi: 10.1056/NEJMoa060186. [DOI] [PubMed] [Google Scholar]
- 231.Dill T, Schächinger V, Rolf A, Möllmann S, Thiele H, Tillmanns H, Assmus B, Dimmeler S, Zeiher AM, Hamm C. Intracoronary administration of bone marrow-derived progenitor cells improves left ventricular function in patients at risk for adverse remodeling after acute ST-segment elevation myocardial infarction: results of the Reinfusion of Enriched Progenitor cells And Infarct Remodeling in Acute Myocardial Infarction study (REPAIR-AMI) cardiac magnetic resonance imaging substudy. Am Heart J. 2009;157:541–547. doi: 10.1016/j.ahj.2008.11.011. [DOI] [PubMed] [Google Scholar]
- 232.Strauer BE, Brehm M, Zeus T, Köstering M, Hernandez A, Sorg RV, Kögler G, Wernet P. Repair of infarcted myocardium by autologous intracoronary mononuclear bone marrow cell transplantation in humans. Circulation. 2002;106:1913–1918. doi: 10.1161/01.cir.0000034046.87607.1c. [DOI] [PubMed] [Google Scholar]
- 233.Strauer BE, Brehm M, Zeus T, Bartsch T, Schannwell C, Antke C, Sorg RV, Kögler G, Wernet P, Müller HW, et al. Regeneration of human infarcted heart muscle by intracoronary autologous bone marrow cell transplantation in chronic coronary artery disease: the IACT Study. J Am Coll Cardiol. 2005;46:1651–1658. doi: 10.1016/j.jacc.2005.01.069. [DOI] [PubMed] [Google Scholar]
- 234.Li ZQ, Zhang M, Jing YZ, Zhang WW, Liu Y, Cui LJ, Yuan L, Liu XZ, Yu X, Hu TS. The clinical study of autologous peripheral blood stem cell transplantation by intracoronary infusion in patients with acute myocardial infarction (AMI) Int J Cardiol. 2007;115:52–56. doi: 10.1016/j.ijcard.2006.04.005. [DOI] [PubMed] [Google Scholar]
- 235.Meluzín J, Mayer J, Groch L, Janousek S, Hornácek I, Hlinomaz O, Kala P, Panovský R, Prásek J, Kamínek M, et al. Autologous transplantation of mononuclear bone marrow cells in patients with acute myocardial infarction: the effect of the dose of transplanted cells on myocardial function. Am Heart J. 2006;152:975.e9–975.15. doi: 10.1016/j.ahj.2006.08.004. [DOI] [PubMed] [Google Scholar]
- 236.Meluzín J, Janousek S, Mayer J, Groch L, Hornácek I, Hlinomaz O, Kala P, Panovský R, Prásek J, Kamínek M, et al. Three-, 6-, and 12-month results of autologous transplantation of mononuclear bone marrow cells in patients with acute myocardial infarction. Int J Cardiol. 2008;128:185–192. doi: 10.1016/j.ijcard.2007.04.098. [DOI] [PubMed] [Google Scholar]
- 237.Wollert KC, Meyer GP, Lotz J, Ringes-Lichtenberg S, Lippolt P, Breidenbach C, Fichtner S, Korte T, Hornig B, Messinger D, et al. Intracoronary autologous bone-marrow cell transfer after myocardial infarction: the BOOST randomised controlled clinical trial. Lancet. 2004;364:141–148. doi: 10.1016/S0140-6736(04)16626-9. [DOI] [PubMed] [Google Scholar]
- 238.Traverse JH, Henry TD, Ellis SG, Pepine CJ, Willerson JT, Zhao DX, Forder JR, Byrne BJ, Hatzopoulos AK, Penn MS, et al. Effect of intracoronary delivery of autologous bone marrow mononuclear cells 2 to 3 weeks following acute myocardial infarction on left ventricular function: the LateTIME randomized trial. JAMA. 2011;306:2110–2119. doi: 10.1001/jama.2011.1670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 239.Traverse JH, Henry TD, Pepine CJ, Willerson JT, Zhao DX, Ellis SG, Forder JR, Anderson RD, Hatzopoulos AK, Penn MS, et al. Effect of the use and timing of bone marrow mononuclear cell delivery on left ventricular function after acute myocardial infarction: the TIME randomized trial. JAMA. 2012;308:2380–2389. doi: 10.1001/jama.2012.28726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 240.Schächinger V, Erbs S, Elsässer A, Haberbosch W, Hambrecht R, Hölschermann H, Yu J, Corti R, Mathey DG, Hamm CW, et al. Improved clinical outcome after intracoronary administration of bone-marrow-derived progenitor cells in acute myocardial infarction: final 1-year results of the REPAIR-AMI trial. Eur Heart J. 2006;27:2775–2783. doi: 10.1093/eurheartj/ehl388. [DOI] [PubMed] [Google Scholar]
- 241.Sürder D, Manka R, Lo Cicero V, Moccetti T, Rufibach K, Soncin S, Turchetto L, Radrizzani M, Astori G, Schwitter J, et al. Intracoronary injection of bone marrow-derived mononuclear cells early or late after acute myocardial infarction: effects on global left ventricular function. Circulation. 2013;127:1968–1979. doi: 10.1161/CIRCULATIONAHA.112.001035. [DOI] [PubMed] [Google Scholar]
- 242.Meyer GP, Wollert KC, Lotz J, Pirr J, Rager U, Lippolt P, Hahn A, Fichtner S, Schaefer A, Arseniev L, et al. Intracoronary bone marrow cell transfer after myocardial infarction: 5-year follow-up from the randomized-controlled BOOST trial. Eur Heart J. 2009;30:2978–2984. doi: 10.1093/eurheartj/ehp374. [DOI] [PubMed] [Google Scholar]
- 243.Solomon SD, Skali H, Anavekar NS, Bourgoun M, Barvik S, Ghali JK, Warnica JW, Khrakovskaya M, Arnold JM, Schwartz Y, et al. Changes in ventricular size and function in patients treated with valsartan, captopril, or both after myocardial infarction. Circulation. 2005;111:3411–3419. doi: 10.1161/CIRCULATIONAHA.104.508093. [DOI] [PubMed] [Google Scholar]
- 244.Cogle C, Wise E. Meacham A, Traverse J, Henry T, Perin E. Variable and decreased clonogenic activity of autologous bone marrow in cell therapy patients with ischemic heart disease, and CD34 as a biomarker for clinical outcomes: results from the cardiovascular cell therapy research network (CCTRN) Present at the American Heart Association Scientific Sessions;; 2013. p. Nov 18; American. [Google Scholar]
- 245.Richman S, Gee AP, McKenna DH, Traverse JH, Henry TD, Fisk D, Pepine CJ, Bloom J, Willerson JT, Prater K, et al. Factors affecting the turnaround time for manufacturing, testing, and release of cellular therapy products prepared at multiple sites in support of multicenter cardiovascular regenerative medicine protocols: a Cardiovascular Cell Therapy Research Network (CCTRN) study. Transfusion. 2012;52:2225–2233. doi: 10.1111/j.1537-2995.2011.03543.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 246.Kissel CK, Lehmann R, Assmus B, Aicher A, Honold J, Fischer-Rasokat U, Heeschen C, Spyridopoulos I, Dimmeler S, Zeiher AM. Selective functional exhaustion of hematopoietic progenitor cells in the bone marrow of patients with postinfarction heart failure. J Am Coll Cardiol. 2007;49:2341–2349. doi: 10.1016/j.jacc.2007.01.095. [DOI] [PubMed] [Google Scholar]
- 247.Fadini GP, Boscaro E, de Kreutzenberg S, Agostini C, Seeger F, Dimmeler S, Zeiher A, Tiengo A, Avogaro A. Time course and mechanisms of circulating progenitor cell reduction in the natural history of type 2 diabetes. Diabetes Care. 2010;33:1097–1102. doi: 10.2337/dc09-1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 248.Orlandi A, Chavakis E, Seeger F, Tjwa M, Zeiher A, Dimmeler S. Long-term diabetes impairs repopulation of hematopoietic progenitor cells and dysregulates the cytokine expression in the bone marrow microenvironment in mice. Basic Res Cardiol. 2010;105:703–712. doi: 10.1007/s00395-010-0109-0. [DOI] [PubMed] [Google Scholar]
- 249.Assmus B, Tonn T, Seeger FH, Yoon CH, Leistner D, Klotsche J, Schächinger V, Seifried E, Zeiher AM, Dimmeler S. Red blood cell contamination of the final cell product impairs the efficacy of autologous bone marrow mononuclear cell therapy. J Am Coll Cardiol. 2010;55:1385–1394. doi: 10.1016/j.jacc.2009.10.059. [DOI] [PubMed] [Google Scholar]
- 250.Seeger FH, Rasper T, Fischer A, Muhly-Reinholz M, Hergenreider E, Leistner DM, Sommer K, Manavski Y, Henschler R, Chavakis E, et al. Heparin disrupts the CXCR4/SDF-1 axis and impairs the functional capacity of bone marrow-derived mononuclear cells used for cardiovascular repair. Circ Res. 2012;111:854–862. doi: 10.1161/CIRCRESAHA.112.265678. [DOI] [PubMed] [Google Scholar]
- 251.Heeschen C, Lehmann R, Honold J, Assmus B, Aicher A, Walter DH, Martin H, Zeiher AM, Dimmeler S. Profoundly reduced neovascularization capacity of bone marrow mononuclear cells derived from patients with chronic ischemic heart disease. Circulation. 2004;109:1615–1622. doi: 10.1161/01.CIR.0000124476.32871.E3. [DOI] [PubMed] [Google Scholar]
- 252.Murphy JW, Cho Y, Sachpatzidis A, Fan C, Hodsdon ME, Lolis E. Structural and functional basis of CXCL12 (stromal cell-derived factor-1 alpha) binding to heparin. J Biol Chem. 2007;282:10018–10027. doi: 10.1074/jbc.M608796200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 253.Seeger FH, Tonn T, Krzossok N, Zeiher AM, Dimmeler S. Cell isolation procedures matter: a comparison of different isolation protocols of bone marrow mononuclear cells used for cell therapy in patients with acute myocardial infarction. Eur Heart J. 2007;28:766–772. doi: 10.1093/eurheartj/ehl509. [DOI] [PubMed] [Google Scholar]
- 254.Hofmann M, Wollert KC, Meyer GP, Menke A, Arseniev L, Hertenstein B, Ganser A, Knapp WH, Drexler H. Monitoring of bone marrow cell homing into the infarcted human myocardium. Circulation. 2005;111:2198–2202. doi: 10.1161/01.CIR.0000163546.27639.AA. [DOI] [PubMed] [Google Scholar]
- 255.Hou D, Youssef EA, Brinton TJ, Zhang P, Rogers P, Price ET, Yeung AC, Johnstone BH, Yock PG, March KL. Radiolabeled cell distribution after intramyocardial, intracoronary, and interstitial retrograde coronary venous delivery: implications for current clinical trials. Circulation. 2005;112:I150–I156. doi: 10.1161/CIRCULATIONAHA.104.526749. [DOI] [PubMed] [Google Scholar]
- 256.Henning RJ, Burgos JD, Vasko M, Alvarado F, Sanberg CD, Sanberg PR, Morgan MB. Human cord blood cells and myocardial infarction: effect of dose and route of administration on infarct size. Cell Transplant. 2007;16:907–917. doi: 10.3727/096368907783338299. [DOI] [PubMed] [Google Scholar]
- 257.Mathur A. The Effect of Intracoronary Reinfusion of Bone Marrow-derived Mononuclear Cells (BM-MNC) on All Cause Mortality in Acute Myocardial Infarction. Available from: http://www.ClinicalTrials.Gov.
- 258.Beltrami AP, Barlucchi L, Torella D, Baker M, Limana F, Chimenti S, Kasahara H, Rota M, Musso E, Urbanek K, et al. Adult cardiac stem cells are multipotent and support myocardial regeneration. Cell. 2003;114:763–776. doi: 10.1016/s0092-8674(03)00687-1. [DOI] [PubMed] [Google Scholar]
- 259.Kikuchi K, Poss KD. Cardiac regenerative capacity and mechanisms. Annu Rev Cell Dev Biol. 2012;28:719–741. doi: 10.1146/annurev-cellbio-101011-155739. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 260.Kajstura J, Gurusamy N, Ogórek B, Goichberg P, Clavo-Rondon C, Hosoda T, D’Amario D, Bardelli S, Beltrami AP, Cesselli D, et al. Myocyte turnover in the aging human heart. Circ Res. 2010;107:1374–1386. doi: 10.1161/CIRCRESAHA.110.231498. [DOI] [PubMed] [Google Scholar]
- 261.Bearzi C, Rota M, Hosoda T, Tillmanns J, Nascimbene A, De Angelis A, Yasuzawa-Amano S, Trofimova I, Siggins RW, LecapitaineN , et al. Human cardiac stem cells. Proc Natl Acad Sci USA. 2007;104:14066–14073. doi: 10.1073/pnas.0706760104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 262.Anversa P, Kajstura J, Rota M, Leri A. Regenerating new heart with stem cells. J Clin Invest. 2013;123:62–70. doi: 10.1172/JCI63068. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 263.Bolli R, Chugh AR, D’Amario D, Loughran JH, Stoddard MF, Ikram S, Beache GM, Wagner SG, Leri A, Hosoda T, et al. Cardiac stem cells in patients with ischaemic cardiomyopathy (SCIPIO): initial results of a randomised phase 1 trial. Lancet. 2011;378:1847–1857. doi: 10.1016/S0140-6736(11)61590-0. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 264.Chugh AR, Beache GM, Loughran JH, Mewton N, Elmore JB, Kajstura J, Pappas P, Tatooles A, Stoddard MF, Lima JA, et al. Administration of cardiac stem cells in patients with ischemic cardiomyopathy: the SCIPIO trial: surgical aspects and interim analysis of myocardial function and viability by magnetic resonance. Circulation. 2012;126:S54–S64. doi: 10.1161/CIRCULATIONAHA.112.092627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 265.Bolli R. Effect of cardiac stem cells in patients with ischemic cardiomyopathy: Interim Results of the SCIPIO Trial up to 2 years after therapy. Los Angeles, California: Presented at the American Heart Association Scientific Sessions; 2012. [Google Scholar]
- 266.Smith RR, Barile L, Cho HC, Leppo MK, Hare JM, Messina E, Giacomello A, Abraham MR, Marbán E. Regenerative potential of cardiosphere-derived cells expanded from percutaneous endomyocardial biopsy specimens. Circulation. 2007;115:896–908. doi: 10.1161/CIRCULATIONAHA.106.655209. [DOI] [PubMed] [Google Scholar]
- 267.Li TS, Cheng K, Malliaras K, Smith RR, Zhang Y, Sun B, Matsushita N, Blusztajn A, Terrovitis J, Kusuoka H, et al. Direct comparison of different stem cell types and subpopulations reveals superior paracrine potency and myocardial repair efficacy with cardiosphere-derived cells. J Am Coll Cardiol. 2012;59:942–953. doi: 10.1016/j.jacc.2011.11.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 268.Chimenti I, Smith RR, Li TS, Gerstenblith G, Messina E, Giacomello A, Marbán E. Relative roles of direct regeneration versus paracrine effects of human cardiosphere-derived cells transplanted into infarcted mice. Circ Res. 2010;106:971–980. doi: 10.1161/CIRCRESAHA.109.210682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 269.Makkar RR, Smith RR, Cheng K, Malliaras K, Thomson LE, Berman D, Czer LS, Marbán L, Mendizabal A, Johnston PV, et al. Intracoronary cardiosphere-derived cells for heart regeneration after myocardial infarction (CADUCEUS): a prospective, randomised phase 1 trial. Lancet. 2012;379:895–904. doi: 10.1016/S0140-6736(12)60195-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 270.Malliaras K, Makkar RR, Smith RR, Cheng K, Wu E, Bonow RO, Marbán L, Mendizabal A, Cingolani E, Johnston PV, et al. Intracoronary cardiosphere-derived cells after myocardial infarction: evidence of therapeutic regeneration in the final 1-year results of the CADUCEUS trial (CArdiosphere-Derived aUtologous stem CElls to reverse ventricUlar dySfunction) J Am Coll Cardiol. 2014;63:110–122. doi: 10.1016/j.jacc.2013.08.724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 271.Chin MT, Murry CE. Is it possible to transform cardiac scar tissue into beating heart muscle in humans? Regen Med. 2012;7:623–625. doi: 10.2217/rme.12.54. [DOI] [PubMed] [Google Scholar]
- 272.Kwong RY, Farzaneh-Far A. Measuring myocardial scar by CMR. JACC Cardiovasc Imaging. 2011;4:157–160. doi: 10.1016/j.jcmg.2010.12.004. [DOI] [PubMed] [Google Scholar]
- 273.Malliaras K, Smith RR, Kanazawa H, Yee K, Seinfeld J, Tseliou E, Dawkins JF, Kreke M, Cheng K, Luthringer D, et al. Validation of contrast-enhanced magnetic resonance imaging to monitor regenerative efficacy after cell therapy in a porcine model of convalescent myocardial infarction. Circulation. 2013;128:2764–2775. doi: 10.1161/CIRCULATIONAHA.113.002863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 274.Heldman A, DiFede D, Fishman J, Zambrano J, Trachtenberg B, Karantalis V, Mushtaq M, Williams A, Suncion V, McNiece I, et al. Transendocardial mesenchymal stem cells and mononuclear bone marrow cells for ischemic cardiomyopathy. The TAC-HFT Randomized Trial. JAMA. 2014;311:62–73. doi: 10.1001/jama.2013.282909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 275.Bartunek J, Behfar A, Dolatabadi D, Vanderheyden M, Ostojic M, Dens J, El Nakadi B, Banovic M, Beleslin B, Vrolix M, et al. Cardiopoietic stem cell therapy in heart failure: the C-CURE (Cardiopoietic stem Cell therapy in heart failURE) multicenter randomized trial with lineage-specified biologics. J Am Coll Cardiol. 2013;61:2329–2338. doi: 10.1016/j.jacc.2013.02.071. [DOI] [PubMed] [Google Scholar]
- 276.Williams AR, Hatzistergos KE, Addicott B, McCall F, Carvalho D, Suncion V, Morales AR, Da Silva J, Sussman MA, Heldman AW, et al. Enhanced effect of combining human cardiac stem cells and bone marrow mesenchymal stem cells to reduce infarct size and to restore cardiac function after myocardial infarction. Circulation. 2013;127:213–223. doi: 10.1161/CIRCULATIONAHA.112.131110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 277.Di Nicola M, Carlo-Stella C, Magni M, Milanesi M, Longoni PD, Matteucci P, Grisanti S, Gianni AM. Human bone marrow stromal cells suppress T-lymphocyte proliferation induced by cellular or nonspecific mitogenic stimuli. Blood. 2002;99:3838–3843. doi: 10.1182/blood.v99.10.3838. [DOI] [PubMed] [Google Scholar]
- 278.Broxmeyer HE. Cellular Characteristics of Cord Blood and Cord Blood Transplantation. Bethesda, Maryland: AABB Press; 1998. pp. 1–227. [Google Scholar]
- 279.Assmus B, Walter DH, Seeger FH, Leistner DM, Steiner J, Ziegler I, Lutz A, Khaled W, Klotsche J, Tonn T, et al. Effect of shock wave-facilitated intracoronary cell therapy on LVEF in patients with chronic heart failure: the CELLWAVE randomized clinical trial. JAMA. 2013;309:1622–1631. doi: 10.1001/jama.2013.3527. [DOI] [PubMed] [Google Scholar]
- 280.Henning RJ, Burgos JD, Vasko M, Alvarado F, Sanberg C, Sanberg P, Morgan MB. Human Cord Blood Cells and Myocardial Infarction: Effect of Dose and Route of Administration on Infarct Size. Cell Transplant. 2007;16:907–917. doi: 10.3727/096368907783338299. [DOI] [PubMed] [Google Scholar]
- 281.Henning RJ, Dennis S, Sawmiller D, Hunter L, Sanberg P, Miller L. Human umbilical cord blood mononuclear cells activate the survival protein Akt in cardiac myocytes and endothelial cells that limits apoptosis and necrosis during hypoxia. Transl Res. 2012;159:497–506. doi: 10.1016/j.trsl.2012.02.004. [DOI] [PubMed] [Google Scholar]
- 282.Jin H, Sanberg PR, Henning RJ. Human umbilical cord blood mononuclear cell-conditioned media inhibits hypoxic-induced apoptosis in human coronary artery endothelial cells and cardiac myocytes by activation of the survival protein Akt. Cell Transplant. 2013;22:1637–1650. doi: 10.3727/096368912X661427. [DOI] [PubMed] [Google Scholar]


