ABSTRACT
Early growth is an important indicator of health and wellbeing of children and a good predictor of adult health. The objective of this study was to examine trends and determinants of overweight and stunting among infants aged 0 to 23 month(s) over the past decade (1999-2011) in Uruguay. Data were used from four large representative samples of 11,056 infants aged 0-23 month(s), who attended public and private health services in 1999, 2003, 2007, and 2011, using a similar methodology. Linear regression analysis was used for assessing trends in early growth indices and binary logistic regression to estimate the probability of being stunted and overweight. Although prevalence of overweight fell from 12.5% (1999) to 9.5% (2011) and stunting from 13.6% to 10.9% respectively, both rates remained higher than expected. Low birthweight (LBW) was the main predictor of stunting [OR 6.5 (5.6-7.6)] and macrosomia of overweight [6.7 (5.3-8.3)]. We did not observe changes in LBW (7.8-8.8%) or macrosomia (5.9-6.7%) over the last decade. Boys showed increased chance of being overweight [OR 1.2 (1.04-1.3)]. Being stunted doubles the chances of being overweight [OR 2.5 (2.2-3.0)]. Overweight [OR 7.1 (6.1-8.3)], LBW [OR 13.2 (11.0-15.9)], and non-breastfed infants [OR 1.9 (1.7-2.1)] showed rapid weight gain. Uruguay has taken positive steps to decline the prevalence of stunting and overweight but both remain excessively high.
Key words: Breastfeeding, Low birthweight, Overweight, Rapid weight gain, Stunting, Uruguay
INTRODUCTION
The last two decades experienced an accumulation of evidence, suggesting that the roots of the inequalities are embedded in early infancy. Conceptional period and the first years of life are determinants of health and wellbeing over the lifecycle. Infant's body-size and growth velocity during the early years of life are important indicators of wellbeing of children and are good predictors of health in adulthood (1). Optimal nutrition in infancy is essential for healthy growth and mental development. Evidence also highlights the role of foetal nutrition and early growth in the programming of disease management (2,3-8). Linear growth during infancy has been considered the best indicator of infants’ health (9). Stunted children have less learning capacity, less lean body mass, and they are at higher risk of being overweight (10-13). Low birthweight, followed by rapid weight gain during infancy, affects several components of the metabolic syndrome, increasing the risk of high blood pressure, altered glucose tolerance, overweight, central fat distribution as well as later obesity (14-17).
The objective of this study was to examine trends and determinants of overweight and stunting among infants aged 0 to 23 month(s) over the past decade (1999-2011) in Uruguay. During this period, the economy contracted and, after a few years, began to grow. As a consequence of the major financial crisis between 1999 and 2002, the country saw an increased population living under poverty conditions. While economic stability returned, renewed emphasis on social issues triggered a healthcare reform and the creation of the Ministry for Social Development. Efforts to promote breastfeeding and “good practices in nutrition” have been undertaken through the health services (18-20). Several years of strong economic growth reduced poverty from 39,6% (2004) to 13,7% (2011) and extreme poverty from 4.2% to 0.8%. The knowledge produced by this study can be useful to understand trends of overweight and stunting during different social and economic periods in Uruguay.
MATERIALS AND METHODS
Data from four large representative samples of infants aged 0-23 month(s) in Uruguay were analyzed to address the objective of this study. The surveys were organized and ethically authorized by the Ministry of Public Health (MSP) and carried out by RUANDI with the support of UNICEF in 1999 (N=2,571), 2003 (N=2,783), 2007 (N=3,003), and 2011 (N=2,994). All surveys used a similar methodology. Only cross-sectional information was obtained. The survey results have been published by UNICEF (18-19).
Four probabilistic, multistage samples were selected, which were representative of the national and regional (capital and other provinces) levels. For each survey, a probabilistic sample was designed, which included the selection of provinces, health services, and children aged 0 to 23 month(s). The study was conducted in 58 health facilities located in the capital and 12 in 18 provinces of the country. Families were invited to participate in the study and asked to sign an informed consent prior to collection of data.
Sex, birthweight, and gestational age were taken from health records. Date of birth was also collected, and age was calculated. Information on infant-feeding practices was collected through a structured interview following recent WHO recommendations. Current anthropometric data were collected by appropriately-trained nutritionists. Children were weighed and measured without clothing or diapers, according to standardized techniques. Weight was measured by a scale with a precision of 0.1 kg. Horizontal length was measured with an infantometer with precision of 0.1 cm.
Using the WHO Child Growth Standards (2006), we estimated z-scores of current measures: length-for-age (LAZ), body mass index-for-age (BAZ), and weight-for-age (WAZ). Birthweight was also expressed as WAZ. WHO Anthro (version 3.2.2) was used in processing anthropometric data; 1.2% of measurements were excluded from the analyses, after being flagged as outliers according to the valid ranges accepted by WHO (WAZ <−6 or >5; LAZ <−6 or >6; BAZ <−5 or >5 z-scores) (WHO Anthro manual).
Infants with length-for-age <−2 SD (LAZ) below WHO reference population were classified as stunted and <−3 SD (LAZ) as severely stunted. Those with body mass index-for-age z-score (BAZ) >2 SD above WHO reference population were classified as overweight and >3 SD (BAZ) as obese.
Changes in SD scores between birth and current age were calculated for weight-for-age (WAZ at current age minus WAZ at birth). We considered indicating significant rapid weight gain when the difference from birth was greater than 0.67 z-scores (current WAZ minus WAZ at birth >0.67) (15,16).
Statistical analysis
Descriptive statistics: mean, standard deviation (SD), median, minimum and maximum values were calculated. We used analysis of variance to test differences in z-scores over time and chi-square for categorical variables.
Trends in LAZ and BAZ over the years were assessed by linear regression analysis.
We included overweight and stunting as dependent variables. The year of the study was included as an independent variable. Binary logistic regression was carried out to estimate the probability of being stunted and overweight, controlling for birthweight, age, gender, breastfeeding duration, and socioeconomic level. The association of each explanatory variable was expressed as adjusted odds ratio (OR) with upper and lower bounds of 95% confidence interval.
Statistical significance level was defined by a p value (α) of <0.05. Management and analysis of data were performed using SPSS (version 15.0).
RESULTS
We studied 5,710 (50.3%) boys and 5,641 (49.7%) girls aged less than 24 months (<6 months=2,898; 6-11 months=2,852; 12-17 months=2,790, and 18-23 months=2,811). We observed a high prevalence of overweight [11.3% (10.7-11.9%)] and stunting [13.3% (12.7-13.9%)] over the last decade in Uruguay (Table 1).
Table 1.
Prevalence of low birthweight (LBW)†, macrosomia†, overweight (OW)§, and stunting‡ in boys and girls aged 0 to 23 month(s) in Uruguay in 1999, 2003, 2007, and 2011
| LBW† | LBW n (%)* | 95% CI* | Boys n (%) | Girls n (%) | p value | |
|---|---|---|---|---|---|---|
| 1999 | 199 (7.7) | 6.7-8.7 | 104 (7.9) | 95 (7.6) | 0.41 | |
| 2003 | 223 (8.1) | 7.3-9.3 | 224 (8.3) | 112 (8.6) | 0.33 | |
| 2007 | 248 (8.3) | 7.3-9.3 | 111 (7.2) | 138 (9.5) | 0.01 | |
| 2011 | 260 (8.7) | 7.3-9.7 | 126 (8.3) | 134 (9.1) | 0.23 | |
| Total | 930 (8.3) | 7.8-8.8 | 452 (7.8) | 478 (8.7) | 0.04 | |
| Macrosomia† | n (%)* | 95% CI* | Boys n (%) | Girls n (%) | p value | |
| 1999 | 169 (6.6) | 5.6-7.6 | 114 (8.7) | 155 (4.4) | <0.001 | |
| 2003 | 176 (6.5) | 5.6-7.4 | 131 (9.4) | 45 (3.4) | <0.001 | |
| 2007 | 181 (6.0) | 5.2-7.0 | 120 (7.8) | 61 (4.2) | <0.001 | |
| 2011 | 181 (6.1) | 5.2-7.0 | 99 (6.5) | 82 (5.6) | 0.16 | |
| Total | 708 (6.3) | 5.9-6.7 | 464 (8.0) | 244 (4.5) | <0.001 | |
| OW§ | n (%)* | 95% CI* | Boys n (%) | Girls n (%) | p value | Obesity§ n (%) |
| 1999 | 318 (12.5) | 11.2-13.8 | 183 (14.1) | 135 (10.9) | 0.01 | 98 (3.9) |
| 2003 | 382 (14.1) | 12.8-15.4 | 219 (15.8) | 163 (12.4) | 0.01 | 96 (3.6) |
| 2007 | 279 (9.3) | 8.3-10.3 | 161 (10.4) | 118 (8.2) | 0.02 | 53 (1.8) |
| 2011 | 279 (9.5) | 8.4-10.6 | 145 (9.7) | 134 (9.2) | 0.33 | 45 (1.5) |
| Total | 1,258 (11.3) | 10.7-11.9 | 708 (12.4) | 550 (10.1) | <0.001 | 292 (2.6) |
| Stunting‡ | n (%)* | 95% CI* | Boys n (%) | Girls n (%) | p value | Severe stunting‡ n (%) |
| 1999 | 368 (13.6) | 12.3-14.9 | 236 (18.5) | 132 (10.6) | <0.001 | 130 (5.2) |
| 2003 | 459 (16.4) | 15.0-17.8 | 279 (20.0) | 180 (13.8) | <0.001 | 154 (5.7) |
| 2007 | 338 (11.3) | 10.2-12.4 | 201 (13.0) | 137 (9.5) | <0.001 | 97 (3.2) |
| 2011 | 320 (10.9) | 9.8-12.0 | 177 (11.9) | 142 (9.8) | 0.04 | 78 (2.7) |
| Total | 1,485 (13.3) | 12.7-13.9 | 893 (15.7) | 591 (10.9) | <0.001 | 459 (4.1) |
*Number of cases observed; percent valid cases; 95% confidence interval; p=Level of significance according to χ2;
†LBW=Birthweight <2,500 g;
†Macrosomia birthweight ≥4,000 g;
§OW=Overweight >2 BAZ; Obesity >3 BAZ;
‡Stunting <−2 HAZ; Severe stunting <−3 HAZ
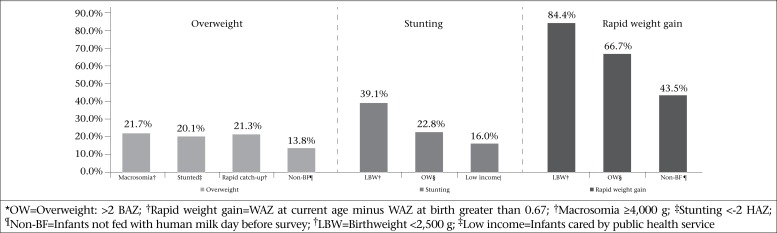
Low birthweight (LBW) was the main predictor of being stunted [OR 6.5 (5.6-7.6)] and macrosomia of being overweight [OR 6.7 (5.3-8.3)] (Table 2 and Figure 1). During the study period, we did not observe changes in low birthweight (7.8-8.8%) or in macrosomia (5.9-6.7%) (Table 1).
Table 2.
Relative predictors of overweight§, stunting‡, and rapid weight-gain†† in 1999, 2003, 2007, and 2011 in Uruguay
| Overweight§ 1,258 (11.3%) | n (%)* | p value | OR (95% CI) |
|---|---|---|---|
| Year 2003 | 385 (14.3) | <0.001 | 1.4 (1.2-1.7) |
| Year 1999 | 327 (12.6) | 0.020 | 1.2 (1.04-1.5) |
| Rapid weight gain†† | 799 (21.3) | <0.001 | 7.1 (6.1-8.3) |
| Macrosomia† | 151 (21.7) | <0.001 | 6.7 (5.3-8.3) |
| Stunting‡ | 270 (20.1) | <0.001 | 3.1 (2.6-3.6) |
| 6 to 23 months | 686 (14.5) | <0.001 | 2.4 (1.9-3.0) |
| Non-BF¶ | 644 (13.8) | 0.024 | 1.2 (1.02-1.3) |
| Boys | 684 (12.6) | 0.010 | 1.2 (1.04-1.3) |
| Stunting‡ 1,485 (13.3%) | n (%)* | p value | OR (95% CI) |
| Year 2003 | 461 (17.1) | <0.001 | 1.5 (1.2-1.7) |
| Year 1999 | 370 (14.7) | 0.006 | 1.3 (1.1-1.5) |
| LBW† | 337 (39.1) | <0.001 | 6.5 (5.6-7.6) |
| OW§ | 270 (22.8) | <0.001 | 2.5 (2.2-3.0) |
| Low income‡ | 990 (16.2) | <0.001 | 2.1 (1.8-2.4) |
| Boys | 834 (15.4) | <0.001 | 1.6 (1.4-1.8) |
| <6 months | 396 (14.7) | <0.001 | 1.3 (1.1-1.6) |
| Rapid weight gain†† 3,764 (34,3%) | n (%)* | p value | OR (95% CI) |
| LBW† | 726 (84.4) | <0.001 | 13.2 (11.0-15.9) |
| OW§ | 799 (66.7) | <0.001 | 5.5 (4.8-6.3) |
| Non-BF¶ | 2,072 (43.5) | <0.001 | 1.9 (1.7-2.1) |
*Number of cases observed; percent valid cases;
**p=Level of significance; OR=Odds ratios obtained from logistic regression, adjusted models=EXP (β). 95% confidence interval for EXP (β);
§OW=Overweight >2 BAZ;
†Macrosomia ≥4,000 g;
‡Stunting <−2 HAZ;
††Rapid weight gain WAZ at current age minus WAZ at birth greater than 0.67 z-scores;
¶Non-BF=Infants not fed with human milk day before survey;
†LBW=Birthweight <2,500 g;
‡Low income=Infants cared by public health service
Figure 1.
Higher rates of overweight*, stunting‡ and rapid weight-gain† in infants aged less than 24 months
Both overweight and stunting were significantly higher in boys than girls; boys showed an increased chance of being overweight [OR 1.2 (1.04-1.3)] as well as being stunted [OR 1.6 (1.4-1.8)] (Table 1 and 2).
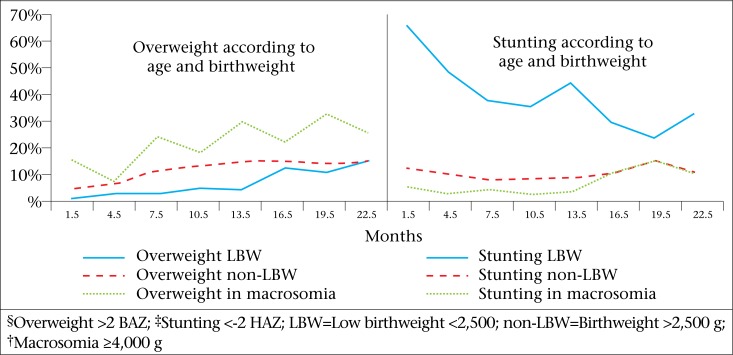
Infants aged <6 months were three times more likely to be stunted than infants aged 6 to 23 months. On the other hand, the risk of being overweight increased with age, doubling when children were aged >6 months [OR 2.4 (1.9-3.0)] (Table 2 and Figure 2).
Figure 2.
Overweight§ and stunting‡ in low-birthweight (LBW) infants non-low-birthweight (non-LBW) infants and macrosomia
When the infants showed rapid weight gain (current WAZ minus WAZ at birth >0.67), they increased probability of being overweight [OR 7.1 (6.1-8.3)]. We observed the highest risk of rapid weight gain among LBW [OR 13.2 (11.0-15.9)] and non-breastfed [OR 1.9 (1.7-2.1)] infants. LBW infants showed so rapid postnatal weight gain that they reached the overweight prevalence of non-LBW after 20 months of age as can be seen in Figure 2.
Stunting and overweight were closely associated. Being stunted doubled the chance of being overweight [OR 2.5 (2.2-3.0)] (Table 2 and Figure 1).
Table 3 shows the trends in body mass index-for-age (BAZ) and length-for-age (LAZ) over the last decade. Mean LAZ increased by +0.016 z-score, and mean BAZ decreased by −0.018 per year studied.
Table 3.
Body mass index-for-age (BAZ) and length-for-age (LAZ) trends over years among infants aged 0 to 23 month(s) in Uruguay, 1999, 2003, 2007, and 2011
| Parameter | Mean±SD | Regression coefficient* | 95% CI | p value |
|---|---|---|---|---|
| BAZ | 0.56±1.22 | -0.018 | -0.023 to −0.013 | <0.001 |
| HAZ | -0.59±1.36 | 0.016 | 0.01 to 0.022 | <0.001 |
*Regression coefficients represent the amount of dependent variable and changes when the corresponding independent variable changes by 1 unit
Prevalence of overweight fell from 12.5% in 1999 to 9.5% in 2011 and stunting from 13.6% to 10.9%. Particularly noticeable was the change in obesity (3.9% to 1.5%) and severe stunting (5.2% to 2.7%). In 2003, we observed a rise in the prevalence of stunting from 13.6% to 16.4% and overweight from 12.5% to 14.1% compared to 1999 (Table 1).
DISCUSSION
In spite of having a strong commitment to democracy, with the most equitable distribution of income in Latin America, the results of this study suggest that Uruguay needs to rethink new strategies to improving physical growth in early infancy for optimal health and wellbeing through the course of life.
We confirm that underweight was not a problem but stunting and overweight rates remained higher than expected in the context of Uruguay. Despite robust income growths and important decreases in poverty, low birthweight (LBW) rate did not reduce, and prevalence of stunting fell only 2.7% over the last decade. LBW rate and prevalence of stunting in 2011 were higher than in Costa Rica, Cuba, and Chile (21-23). An increase in the prevalence of stunting in 2003 was consistent with the worst socioeconomic and financial crisis in Uruguay in the past century.
As has been reported by other authors, our results showed that boys were more vulnerable to poor growth compared to girls (21,24-25). Male students in public school system in Uruguay are those with the highest prevalence of stunting (20) and the poorest educational performance (39).
In the present study, the probability of being overweight among stunted infants doubled, indicating the recognized association between poverty and obesity as well as the double burden in the social, economic, and healthcare systems (12,13,27-28)
Prevalence of overweight, despite showing positive steps towards decline, is still too high in Uruguay (2011: 8.4-10.6%). Special attention should be given to avoid fast catch-up weight gain in low-birthweight infants (5,6,8,10,17,37,38). In the present study, non-breastfed infants showed an increased risk of being overweight and especially increased chance of fast catch-up weight gain (33,34).
To improve linear growth and, at the same time, to address measures to avoid excessive weight gain, Uruguay should continue encouraging exclusive breastfeeding, particularly to LBW infants as well as improving complementary food practices that provide an adequate micronutrient supply after 6 months of age (21,25,30,32-37).
Strengths and limitations
The main limitation of this study is the fact that we analyzed cross-sectional data with only one measure per child; so, we only could describe association and could not establish causal relationship. The strength of this study is the robust sample-sizes analyzed as well as that children included in the analysis were from different socioeconomic families. On the other hand, there was little information about Uruguayan early growth indices before this study.
Conclusions
Uruguay has taken positive steps to decline the prevalence of stunting and overweight. Nevertheless, both remain excessively high and, according to our results, new strategies need to be thought of.
ACKNOWLEDGEMENTS
The four surveys were financed by UNICEF of Uruguay. This analysis is part of the first author´s thesis to fulfill the requirements for a doctorate, and it was supported by Monesia Group, Granada University.
We would like to acknowledge Alvaro Arroyo for his constant help; Cristina Lustemberg, Ximena Moratorio, Mara Castro, Jorge Quian, Cecilia Muxi for trust, diffusion, and providing logistics to carry out these surveys; Valentina Muxi for excellent field work supervision; Walter Álvarez for sample selection; Graciela Romano, Monica Márquez and Jacqueline Lucas for their assistance in interviewers’ training. We thank UNICEF and the participating families for making these studies possible.
Competing interests: The authors declare no conflict of interest.
REFERENCES
- 1.Dewey KG, Begum K. Long-term consequences of stunting in early life. Matern Child Nutr. 2011;7(Suppl 3):5–18. doi: 10.1111/j.1740-8709.2011.00349.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Dickerson JW. Some aspects of the public health importance of measurement of growth. J R Soc Promot Health. 2003;123:165–8. doi: 10.1177/146642400312300313. [DOI] [PubMed] [Google Scholar]
- 3.Thornburg KL, Shannon J, Thuillier P, Turker MS. In utero life and epigenetic predisposition for disease. Adv Genet. 2010;71:57–78. doi: 10.1016/B978-0-12-380864-6.00003-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lawlor DA, Andersen AM, Batty GD. Birth cohort studies: past, present and future. Int J Epidemiol. 2009;38:897–902. doi: 10.1093/ije/dyp240. [DOI] [PubMed] [Google Scholar]
- 5.Langley-Evans SC, McMullen S. Developmental origins of adult disease. Med Princ Pract. 2010;19:87–98. doi: 10.1159/000273066. [DOI] [PubMed] [Google Scholar]
- 6.Gluckman PD, Hanson MA, Cooper C, Thornburg KL. Effect of in utero and early-life conditions on adult health and disease. N Engl J Med. 2008;359:61–73. doi: 10.1056/NEJMra0708473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Fisher D, Baird J, Payne L, Lucas P, Kleijnen J, Roberts H, et al. Are infant size and growth related to burden of disease in adulthood? A systematic review of literature. Int J Epidemiol. 2006;35:1196–210. doi: 10.1093/ije/dyl130. [DOI] [PubMed] [Google Scholar]
- 8.Gluckman PD, Hanson MA, Bateson P, Beedle AS, Law CM, Bhutta ZA, et al. Towards a new developmental synthesis: adaptive developmental plasticity and human disease. Lancet. 2009;373:1654–7. doi: 10.1016/S0140-6736(09)60234-8. [DOI] [PubMed] [Google Scholar]
- 9.de Onis M, Blössner M, Borghi E, Frongillo EA, Morris R. Estimates of global prevalence of childhood underweight in 1990 and 2015. JAMA. 2004;291:2600–6. doi: 10.1001/jama.291.21.2600. [DOI] [PubMed] [Google Scholar]
- 10.Barker DJ, Bergmann RL, Ogra PL. Concluding remarks. The window of opportunity: pre-pregnancy to 24 months of age. Nestle Nutr Workshop Ser Pediatr Program. 2008;61:255–60. doi: 10.1159/000113499. [DOI] [PubMed] [Google Scholar]
- 11.Corvalán C, Kain J, Weisstaub G, Uauy R. Impact of growth patterns and early diet on obesity and cardiovascular risk factors in young children from developing countries. Proc Nutr Soc. 2009;68:327–37. doi: 10.1017/S002966510900130X. [DOI] [PubMed] [Google Scholar]
- 12.Sawaya AL, Roberts S. Stunting and future risk of obesity: principal physiological mechanisms. Cad Saude Publica. 2003;19(Suppl 1):S21–8. doi: 10.1590/s0102-311x2003000700003. [DOI] [PubMed] [Google Scholar]
- 13.Martins PA, Hoffman DJ, Fernandes MTB, Nascimento CR, Roberts SB, Sesso R, et al. Stunted children gain less lean body mass and more fat mass than their non-stunted counterparts: a prospective study. Br J Nutr. 2004;92:819–25. doi: 10.1079/bjn20041274. [DOI] [PubMed] [Google Scholar]
- 14.Baird J, Fisher D, Lucas P, Kleijnen J, Roberts H, Law C. Being big or growing fast: systematic review of size and growth in infancy and later obesity. BMJ. 2005;22:331–929. doi: 10.1136/bmj.38586.411273.E0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ong KK, Ahmed ML, Emmett PM, Preece MA, Dunger DB. Association between postnatal catch-up growth and obesity in childhood: prospective cohort study. BMJ. 2000;320:967–71. doi: 10.1136/bmj.320.7240.967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ekelund U, Ong K, Linné Y, Neovius M, Brage S, Dunger DB, et al. Upward weight percentile crossing in infancy and early childhood independently predicts fat mass in young adults: the Stockholm Weight Development Study (SWEDES) Am J Clin Nutr. 2006;83:324–30. doi: 10.1093/ajcn/83.2.324. [DOI] [PubMed] [Google Scholar]
- 17.Ong KK, Loos RJ. Rapid infancy weight gain and subsequent obesity: systematic reviews and hopeful suggestions. Acta Paediatr. 2006;95:904–8. doi: 10.1080/08035250600719754. [DOI] [PubMed] [Google Scholar]
- 18.Bove MI, Cerruti F. Montevideo: United Nations Children's Fund; 2007. Encuesta de lactancia, estado nutricional y alimentación complementaria: en niños y niñas menores de 24 meses; p. 71. [Spanish] [Google Scholar]
- 19.Bove MI, Cerruti F. Montevideo: Fondo de las Naciones Unidas para la Infancia; 2011. Encuesta nacional sobre estado nutricional, prácticas de alimentación y anemia; p. 76. [Google Scholar]
- 20.Amarante V, Arim R, Severi C, Vigorito A, Aldabe I. Montevideo: United Nations Development Programme, Uruguay; 2007. El estado nutricional de los niños/as y las políticas alimentarias; p. 109. [Spanish] [Google Scholar]
- 21.Uauy R, Albala C, Kain J. Obesity trends in Latin America: transiting from under- to overweight. J Nutr. 2001;131:893S–9S. doi: 10.1093/jn/131.3.893S. [DOI] [PubMed] [Google Scholar]
- 22.de Onis M, Blössner M, Borghi E. Prevalence and trends of stunting among pre-school children, 1990-2020. Public Health Nutr. 2012;15:142–8. doi: 10.1017/S1368980011001315. [DOI] [PubMed] [Google Scholar]
- 23.Lutter CK, Chaparro CM, Muñoz S. Progress towards Millennium Development Goal 1 in Latin America and the Caribbean: the importance of the choice of indicator for undernutrition. Bull World Health Organ. 2011;89:22–30. doi: 10.2471/BLT.10.078618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Uauy R, Kain J, Corvalan C. How can the Developmental Origins of Health and Disease (DOHaD) hypothesis contribute to improving health in developing countries? Am J Clin Nutr. 2011;94(Suppl 6):1759S–64S. doi: 10.3945/ajcn.110.000562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Uauy R, Rojas J, Corvalan C, Lera L, Kain J. Prevention and control of obesity in preschool children: importance of normative standards. J Pediatr Gastroenterol Nutr. 2006;43(Suppl 3):S26–37. doi: 10.1097/01.mpg.0000255848.84658.52. [DOI] [PubMed] [Google Scholar]
- 26.Caballero B. A nutrition paradox—underweight and obesity in developing countries. N Engl J Med. 2005;352:1514–6. doi: 10.1056/NEJMp048310. [DOI] [PubMed] [Google Scholar]
- 27.Duran P, Caballero B, de Onis M. The association between stunting and overweight in Latin American and Caribbean preschool children. Food Nutr Bull. 2006;27:300–5. doi: 10.1177/156482650602700403. [DOI] [PubMed] [Google Scholar]
- 28.Popkin BM, Gordon-Larsen P. The nutrition transition: worldwide obesity dynamics and their determinants. Int J Obes Relat Metab Disord. 2004;28(Suppl 3):S2–9. doi: 10.1038/sj.ijo.0802804. [DOI] [PubMed] [Google Scholar]
- 29.Leary SD, Smith GD, Rogers IS, Reilly JJ, Wells JCK, Ness AR. Smoking during pregnancy and offspring fat and lean mass in childhood. Obesity (Silver Spring) 2006;14:2284–93. doi: 10.1038/oby.2006.268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Horta BL, Gigante DP, Osmond C, Barros FC, Victora CG. Intergenerational effect of weight gain in childhood on offspring birthweight. Int J Epidemiol. 2009;38:724–32. doi: 10.1093/ije/dyp168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Monteiro PO, Victora CG, Barros FC, Monteiro LM. Birth size, early childhood growth, and adolescent obesity in a Brazilian birth cohort. Int J Obes Relat Metab Disord. 2003;27:1274–82. doi: 10.1038/sj.ijo.0802409. [DOI] [PubMed] [Google Scholar]
- 32.Victora CG, Adair L, Fall C, Hallal PC, Martorell R, Richter L, et al. Maternal and Child Undernutrition Study Group, Maternal and child undernutrition: consequences for adult health and human capital. Lancet. 2008;26(371):340–57. doi: 10.1016/S0140-6736(07)61692-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Singhal A, Lanigan J. Breastfeeding, early growth and later obesity. Obes Rev. 2007;8(Suppl 1):51–4. doi: 10.1111/j.1467-789X.2007.00318.x. [DOI] [PubMed] [Google Scholar]
- 34.Dewey KG. Growth patterns of breastfed infants and the current status of growth charts for infants. J Hum Lact. 1998;14:89–92. doi: 10.1177/089033449801400202. [DOI] [PubMed] [Google Scholar]
- 35.Victora CG, Barros FC, Horta BL, Martorell R. Short-term benefits of catch-up growth for small-for-gestational-age infants. Int J Epidemiol. 2001;30:1325–30. doi: 10.1093/ije/30.6.1325. [DOI] [PubMed] [Google Scholar]
- 36.Ashworth A, Shrimpton R, Jamil K. Growth monitoring and promotion: review of evidence of impact. Matern Child Nutr. 2008;4(Suppl 1):86–117. doi: 10.1111/j.1740-8709.2007.00125.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Péneau S, Rouchaud A, Rolland-Cachera M-F, Arnault N, Hercberg S, Castetbon K. Body size and growth from birth to 2 years and risk of overweight at 7-9 years. Int J Pediatr Obes. 2011;6:e162–9. doi: 10.3109/17477166.2010.518241. [DOI] [PubMed] [Google Scholar]
- 38.Ong KK, Dunger DB. Birth weight, infant growth and insulin resistance. Eur J Endocrinol. 2004;151(Suppl 3):U131–9. doi: 10.1530/eje.0.151u131. [DOI] [PubMed] [Google Scholar]
- 39.Kaztman R, Filgueira F. Montevideo: Programa de Investigación sobre Integración, Pobreza y Exclusión Social (IPES) de la Facultad de Ciencias Sociales y Comunicación. Universidad Católica del Uruguay Universidad Católica del Uruguay; 2006. Panorama de la infancia y la familia en Uruguay; pp. 110–5. [Spanish] [Google Scholar]