ABSTRACT
Studies on diet quality among individuals with type 2 diabetes mellitus (T2DM) are scarce. This cross-sectional study aimed to assess the diet quality and to determine its associated factors among individuals with T2DM at the Medical Outpatients Department, Serdang Hospital, Selangor, Malaysia, from July 2010 to March 2011. Subjects were interviewed for sociodemographic data. Diabetes history was retrieved from the hospital's e-database. Usual dietary intake was measured using a food frequency questionnaire, from which a dietary diversity score was obtained with two measures: Food Group Score and Serving Score were constructed based on the Malaysian Dietary Guidelines. Food Group Score was computed from the number of food groups consumed from five major food groups (grains, vegetables, fruits, meat, and dairy products) whereas Serving Score was computed from the number of servings consumed from the various food groups. Anthropometric measures, including weight, height, waist- and hip-circumference were examined. For data analyses, descriptive statistics, simple and multiple linear regression were conducted using IBM SPSS Statistics 20.0. A total of 113 subjects (50.4% female), with mean±SD age of 54.05±10.30 years and duration of diabetes of 11.25±9.05 years were studied. The mean Food Group Score and Serving Score were 4.12±0.79 and 12.75±3.50 respectively. Slightly more than one-third of the subjects achieved five food groups a day while less than 2% consumed a desirable number of servings from all food groups. Among the five food groups, dairy, and fruits were the least-frequently consumed foods. Lower education, lower personal income, working, non-insulin, overweight and obese subjects had significantly lower Food Group Score than their counterparts [F (6,106)=4.924, p<0.0001] whereas lower education, lower waist-to-hip ratio, overweight and obese subjects had significantly lower Serving Score than their counterparts [F (4,108)=7.520, p<0.0001]. There was a high proportion of individuals with T2DM, who failed to adhere to the national dietary guidelines. The importance of taking a well-balanced diet in accordance with the guidelines should be emphasized, especially among those with lower educational level through a simple and easy-to-understand approach.
Key words: Cross-sectional studies, Dietary diversity, Diet quality, Type 2 diabetes mellitus, Malaysia
INTRODUCTION
Diabetes mellitus remains a major cause of mortality and morbidity worldwide. Factors associated with the continuous upward trend include population growth, ageing, urbanization, increasing prevalence of obesity as well as physical inactivity (1). The prevalence of diabetes worldwide is projected to increase from 8.3% in 2011 to 9.9% in 2030 (2). Among 80 most-populated countries in the world, Malaysia appears to have the highest prevalence of diabetes in the Western Pacific region (3). International Diabetes Federation predicted that the prevalence of diabetes in Malaysia is projected to reach 13.3% in 2030 (3). However, the worrying fact is that the prevalence of diabetes in Malaysia increases even faster than the projection, which recorded 11.6% in 2006 (4) and 15.2% in 2011 (5). It was ranked in the top 10 total burden of disease in Malaysia in terms of premature mortality (6). Individuals with diabetes are at higher risk of suffering from diabetes complications as it frequently co-exists with a constellation of cardiovascular (CVD) risk factors and metabolic syndrome (7,8).
Dietary management is crucial for preventing diabetes, managing existing condition, and preventing the development of diabetes complications (9). Assessing diet quality among individuals with diabetes may be beneficial for the development of diabetes management intervention, particularly for secondary and tertiary prevention to reduce the burden of disease. Diet quality was found to have a protective effect towards health outcomes, including a reduction of 17-42% for all-cause mortality, 18-53% for CVD mortality, and 14-28% for CVD risk (10). Dietary diversity score (DDS), as one of the diet quality indicator (11,12), was found to be inversely associated with CVD risk (13) and metabolic syndrome (14). Although dietary management is crucial for individuals with diabetes, the studies on diet quality among them are scarce (10,15). Type 2 diabetes mellitus (T2DM) is the most common type of diabetes, and it accounted for 90-95% of all diabetes cases (8). Therefore, this study aims to assess the diet quality as measured using DDS and to determine the factors associated with DDS among individuals with T2DM.
MATERIALS AND METHODS
Subjects
This cross-sectional study was conducted among 113 Malaysian men and women who were aged above 18 years, diagnosed with T2DM, with poor glycaemic control as defined by HbA1c ≥8.0%, and attended the Medical Outpatient Department of Serdang Hospital, a government-funded multispecialty hospital located in the district of Sepang in the state of Selangor, Malaysia, during July 2010-March 2011. The exclusion criteria included those who were severely impaired in vision, hearing, or speech and who were unable to communicate in English, Malay, Mandarin, or Cantonese. In addition, pregnant or lactating women and individuals who were diagnosed with cardiac failure, severe renal disease, gastrointestinal diseases, mental disorientation or other chronic medical conditions that required specific dietary restriction were excluded.
The sample-size was calculated based on Torheim and colleagues’ study (12) who found that about 22% of the variance for DDS was explained by sociodemographic characteristics. The effect-size was obtained using the formula as follows (16):
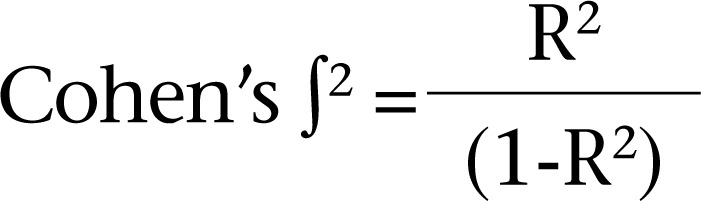
where R2 is the expected coefficient of determination.
The minimum sample-size comprised 92 subjects based on G*Power version 3.1.7 (Franz Faul, University of Kiel, Kiel, Germany) (17), with an expected medium effect-size of 0.282, power of 0.90, alpha (α) value of 0.05 for a multiple linear regression model with 13 predictors. The final sample-size was further increased to 108 after considering an estimated 15% non-response rate.
Ethical clearance
Ethical approval for the study was obtained from the Medical Research and Ethics Committee of the Faculty of Medicine and Health Sciences, Universiti Putra Malaysia and the Ministry of Health Malaysia. The nature of the study was explained, and an informed consent was given by individuals to participate in the study.
Instruments
All subjects were interviewed using a structured questionnaire pre-tested with face validity and content clarity. Diabetes history of subjects was retrieved through the hospital's electronic medical record database. Anthropometric measures, including weight, height, waist-circumference (WC), and hip-circumference were recorded using standardized procedures. Body mass index (BMI) was calculated as weight in kg divided by height in metre squared. The BMI classification was based on the WHO criteria (2004) (18), specifically for the Asian population as follows: BMI <18.5 kg/m2 underweight; 18.5-22.9 kg/m2 normal range; 23.0-27.4 kg/m2 overweight; 27.5-32.4 kg/m2 pre-obese; 32.5-37.4 kg/m2 obese Class I; and ≥37.5 kg/m2 obese Class II. Waist-to-hip ratio (WHR) was calculated as WC in cm divided by hip-circumference in cm. The classifications of WC and WHR were based on the WHO/IASO/IOTF criteria (2000) (19) and WHO criteria (1998) (20) respectively.
Usual dietary intake of subjects was assessed using a food frequency questionnaire which consisted of 28 food groups that were commonly consumed in Malaysia. Subjects were asked to recall the frequency and portion-size of foods and beverages that they consumed over the past month on a daily, weekly or monthly basis with the aid of household measurement tools. The reported frequency was converted to daily intake while the reported portion-size was converted to number of servings based on the serving-size recommended by the Malaysian Dietary Guidelines (MDG) (21) to generate DDS for subjects. Measures of DDS, namely Food Group Score (FGS) and Serving Score (SS) were modified from Kant et al. (22). The FGS reflected the number of food groups consumed daily from a total of five food groups—grains (cereals, tubers, and grains), fruits, vegetables, meat (fish, poultry, meat, eggs, and legumes), and dairy (milk and dairy products). The minimum amount to be credited as consumed for each food group was at least one-half serving per day based on the serving-size recommended in the MDG (21) (Table 1). One point was given for each food group consumed daily and added up to a maximum of five if all food groups were consumed daily. Meanwhile, the SS reflected the presence of achieving the minimum recommended number of servings for the five food groups—four servings daily for grains and two servings daily each of fruits, vegetables, meat, and dairy. Subjects who consumed below the minimum amount, which was less than one-half serving, were treated as having zero serving; intakes above the minimum amount but below the recommended serving-size were credited with one serving; intakes which were 1.5 times of the recommended serving-size were credited with 1.5 servings, and so on. One or two point(s) were awarded for the consumption of each serving of grains and other food groups respectively. The maximum score for each food group was four points while the maximum score for total SS was 20 points. Perfect score of 5 for FGS indicated consumption of all the 5 food groups daily whereas perfect score of 20 for SS indicated that the individuals were taking at least the minimum number of servings from all food groups as recommended in the MDG (21).
Table 1.
Number of servings according to food groups recommended by the Malaysian Dietary Guidelines (21)
| Food group | Recommended number of servings/day* |
|---|---|
| Cereals, tubers, and grains† | 4-8 |
| Fruits‡ | 2 |
| Vegetables | 3 |
| Fish, poultry, meat, eggs, and legumes | |
|
|
| Milk and dairy products§ | 1-3 |
*Based on 1,500-2,500 kcal/day, with calories from fat and sugars included;
†Based on 30 g carbohydrate per serving;
‡Based on 15 g carbohydrate per serving;
¶Based on 14 g protein per serving;
§Based on 7 g protein per serving
Statistical analyses
The IBM SPSS Statistics 20.0 (SPSS Inc., Chicago, IL, USA) was used in all statistical analyses. Univariate analysis was conducted to describe the data. A series of simple linear regression models were applied. Variables that had p<0.25 in the simple linear regression models were chosen for backward stepwise multiple linear regression analysis to further examine the factors associated with DDS among the subjects. Statistical significance was indicated by p<0.05.
RESULTS
A total of 113 subjects (50.4% female), with mean age of 54.05±10.30 years, comprising various ethnic groups (46.0% Malay, 28.3% Chinese, 23.0% Indian, and 2.7% other ethnicities) participated in the present study (Table 2). Majority of the study subjects were married (84.1%). Approximately one-third of the subjects had attained primary education (32.7%); more than one-third (37.2%) had monthly personal income of less than 500 MYR (Malaysian Ringgit) (US$ 158), and almost half (46.9%) had monthly household income of less than 3,000 MYR (US$ 950). On average, the subjects were diagnosed with T2DM for 11.25±9.05 years, and more than half (57.5%) were on insulin regimen. Most were overweight, pre-obese or obese (93.8%), and more than two-thirds (74.3-87.6%) were found to have abdominal obesity.
Table 2.
Sociodemographics, diabetes history, and anthropometric characteristics of subjects
| Characteristics | n (%) | Mean±SD |
|---|---|---|
| Gender | ||
|
|
|
| Age (years) | ||
|
|
54.05±10.30 |
| Ethnicity | ||
|
|
|
| Marital status | ||
|
|
|
| Educational level | ||
|
|
9.23±4.38 |
| Working status | ||
|
|
|
| Personal income (MYR)* | ||
|
|
|
| Household income (MYR)* | ||
|
|
|
| Duration of diabetes (years) | ||
|
|
11.25±9.05 |
| Type of medication | ||
|
|
|
| Weight (kg) | 76.35±17.70 | |
| Height (cm) | 159.52±9.40 | |
| Body mass index (kg/m2) | ||
|
|
29.82±5.45 |
| Waist-circumference (cm) | 98.49±13.34 | |
|
|
|
| Hip-circumference (cm) | 104.26±10.69 | |
| Waist-to-hip ratio | ||
|
|
0.94±0.07 |
*1.00 MYR was equivalent to US$ 0.32 at the time of study; SD=Standard deviation; MYR=Malaysian Ringgit
Table 3 presents the distribution of subjects by DDS. The mean FGS and SS were 4.12±0.79 and 12.75±3.50 points respectively. Slightly more than one-third of the subjects (34.5%) scored a perfect point of 5 for FGS while only a handful (1.8%) scored a perfect point of 20 for SS. Grains group was consumed daily by all subjects; however, only about half (54.0%) of them consumed four servings of cereals and grains. This was followed by meat (97.3%) and vegetable (95.6%) consumption. It is worth noting that only 38.9% and 51.3% of the subjects took at least 2 servings daily each of the meat and vegetable groups respectively. Although approximately three-quarters of the subjects (76.1%) consumed fruits daily, less than one-third of the subjects (29.2%) met the recommended number of servings of fruits, which were 2 servings per day. Dairy products were the least-frequently consumed foods. Less than half of the subjects (43.4%) consumed milk and dairy products on a daily basis, with a majority (89.4%) failing to achieve two servings of milk and dairy products.
Table 3.
Distribution of subjects according to dietary diversity score
| Food group | Dietary diversity score | |||
|---|---|---|---|---|
| Food group Score* | Serving score† | |||
| n (%) | Mean±SD | n (%) | Mean±SD | |
|
|
|
||
*Food Group Score (FGS) counts the number of food groups consumed daily from a total of five groups, namely grains, fruits, vegetables, meat, and dairy. One point was given for each food group;
†Serving Score (SS) evaluates the presence of achieving the minimum recommended number of servings for the various food groups—four servings daily from grains group and two servings for each of the remaining groups. One point was given for each serving of grains and two points for other food groups;
‡Proportion of subjects consuming the food group daily;
¶Proportion of subjects achieving the recommended number of servings of the food group daily;
§Perfect score for Food Group Score was 5 and, for Serving Score, it was 20
Table 4 displays the strength of the associations between FGS and characteristics of the subjects in simple and multiple linear regression models. Among the eight variables that were selected (p<0.25) to be entered into the final model, only five were found to predict significantly the number of food group intake as measured by FGS [F (6,106)=4.924, p<0.0001]. Educational level was positively associated with FGS, with every one year increase in education contributing to 0.05 unit increase in FGS (p=0.005). Among individuals with T2DM, those who were not working, had high personal income, on insulin regimen, and of normal weight were found to have more diversified diet than their counterparts, ranging from 0.3-0.7 food group more each day (p<0.05).
Table 4.
Associations between Food Group Score (FGS) and characteristics of sociodemographic, diabetes history, and anthropometric measures in simple and multiple regression models
| Characteristics | Simple regression† | Multiple regression‡ | ||
|---|---|---|---|---|
| β (95% CI) | p value | β (95% CI) | p value | |
| Sociodemographic characteristics | ||||
|
|
|
|
|
| Diabetes history | ||||
|
|
|
|
|
| Anthropometric measures | ||||
|
|
|
|
|
Variables that had a p<0.25 in the simple linear regression models are shown in bold and were chosen for backward stepwise multiple linear regression analysis.
†Simple linear regression: association is significant at *p<0.004 (Bonferroni adjustment);
‡Backward stepwise multiple linear regression: association is significant at *p<0.05, **p<0.01, R=0.467, R2=0.218, Adjusted R2=0.174, F (6,106)=4.924, p<0.0001, Durbin-Watson=1.943; β=Coefficient; BMI=Body mass index; CI=Confidence interval
On the other hand, only three out of eight variables were found to predict significantly the presence of achieving the minimum recommended number of servings of various food groups as measured by SS [F (4,108)=7.520, p<0.0001] (Table 5). Educational level was positively associated with SS, with each year increase in education contributing to 0.29 unit increase in SS (p<0.0001). Subjects who were of normal weight were found to have approximately 4 units higher in SS than their overweight, pre-obese or obese counterparts (p<0.05). On the other hand, WHR was positively associated with SS, with one unit increase in WHR contributing to 9.58 units increase in SS (p=0.025). The final models explained about 21.8% of the variance in the scores for FGS and SS. The Durbin-Watson coefficients were found to be approaching 2, indicating the data were independent, and there was no autocorrelation in the sample.
Table 5.
Associations between Serving Score (SS) and sociodemographics, diabetes history, and anthropometric measures in simple and multiple regression models
| Characteristics | Simple regression† | Multiple regression‡ | ||
|---|---|---|---|---|
| β (95% CI) | p value | β (95% CI) | p value | |
| Sociodemographic characteristics | ||||
|
|
|
0.29 (0.15, 0.43) | 0.000*** |
| Diabetes history | ||||
|
|
|
||
| Anthropometric measures | ||||
|
|
|
|
|
Variables that had a p<0.25 in the simple linear regression models are shown in bold and were chosen for backward stepwise multiple linear regression analysis.
†Simple linear regression, association is significant at *p<0.004 (Bonferroni adjustment);
‡Backward stepwise multiple linear regression, association is significant at *p<0.05, **p<0.01, ***p<0.001, R=0.467, R2=0.218, Adjusted R2=0.189, F (4,108)=7.520, p<0.0001, Durbin-Watson=2.164; β=Coefficient; BMI=Body mass index; CI=Confidence interval
DISCUSSION
This study demonstrates that a high proportion of subjects with T2DM failed to adhere to the national dietary guidelines. Nearly two-thirds of the study subjects with T2DM did not consume all five major food groups daily. Only about half of the subjects fulfilled the minimum recommended number of servings of each food group. In contrast to earlier findings from studies conducted among free-living community-based Malaysians, which reported that only dairy consumption was below the suggested intake (23), our findings were consistent with other studies done in European countries among individuals with diabetes (24,25). This suggests that, although diet is acknowledged as a very critical component in the overall treatment for T2DM, poor adherence is highly expected.
A possible explanation for non-adherence to national dietary guideline might be that individuals with T2DM were looking for ‘diabetic diet’. In this study, dairy and fruits are the least-frequently consumed food groups. Some respondents reported that they tried to avoid these foods because they perceived dairy is potentially fattening (16.7%) and fruit is ‘too sweet’ (19.0%) for people with diabetes. In fact, nutritional recommendations for individuals with T2DM resemble the ‘healthy pattern of diet’ for the general population as shown in the national dietary guidelines. A well-balanced meal is equally important for preventing and controlling diabetes for both individuals with or without diabetes (9,26). A healthy and well-balanced diet should meet the national dietary guidelines that encourage people to eat a variety of foods that include carbohydrate from fruits, vegetables, whole grains, legumes, and low-fat milk; to monitor portion-sizes; to eat a variety of fibre-containing foods; to consume protein in moderation; and to reduce intakes of energy, saturated and trans-fatty acids, cholesterol as well as sodium (9). Studies have shown that consuming a diet with fruits, vegetables, whole grains, low-fat dairy, lean meats, and alternatives was not only associated with a lower risk of all-cause mortality (27), it also had considerable merit for improving health outcome (28).
Dairy products are frequently perceived as fattening and should be avoided to prevent obesity. In fact, a review done by Zemel (29) found evidence for the presence of an anti-obesity effect of dairy foods. Dairy foods were also found to be inversely associated with the development of intra-abdominal adipose tissues (30). Besides the anti-obesity effects, dairy intake was found to be inversely associated with the development of abnormal glucose homeostasis, elevated blood pressure, and dyslipidaemia among overweight adults (31). All these components are particularly crucial for preventing diabetes complications among individuals with T2DM (9).
The present study shows a direct association between level of education and DDS. This finding was consistent with other studies (32-34) which found that lower education was associated with less diversified and poor diet quality. These results may be explained by the fact that certain literacy level is required to comprehend the available health information. Less-educated subjects may find it hard to make use of written materials, like newspaper articles and leaflets, to gain nutritional and health-related knowledge (35). Understanding the information regarding diet-disease links can be complex and challenging for these vulnerable subjects and, hence, limit their ability to implement the nutritional and health-related knowledge in daily life (35). Norimah et al. (36) demonstrated that the key words and key messages in the newly-updated MDG are poorly understood by less-educated Malaysians, especially those with only primary education. Although the importance of taking well-balanced diet with various food groups to prevent diet-related chronic diseases has existed for more than a decade in Malaysia (37), such messages fail to reach their target audience, especially to those with lower educational level. As higher prevalence of T2DM was documented amongst lower-educated subjects, there is an urgent need to promote nutritional awareness with messages that are tailor-made for this group. In this context, the USDA's newest visual tool—MyPlate—might serve as one of the options as many new users perceived it as simple, visually appealing, and could be personalized to fit their diet (38).
Our data are in agreement with the findings reported in a review paper by Darmon and Drewnowski (39) that showed better-quality diets are mainly consumed by better-educated and more-affluent people and suggested that the observed socioeconomic status gradient in diet quality may be mediated by prices of food and costs of diet. Prices of food could be a very important determinant of food choices and diet quality as low-income group spend a relatively higher proportion of their income on food than higher-income group does (40). Individuals with low educational level and limited income were more likely to perceive food price as very important, which could further influence their food-purchasing decisions and, consequently, impact on their diet quality (41). Bowman (41) found that those who perceived food price as very important were more likely to eat a low amount of relatively high-price foods and consume more energy-dense poor-nutrient diets.
Our data reveal that working diabetics are more likely to eat a less diversified diet. This finding may be particularly true as working subjects may have more workloads and working demands than do their non-working counterparts. They may be more likely to experience feelings of time scarcity and lack of energy which may further alter their food choices, such as eating out, eating on the run, eating junk foods, or skipping meals. Lin et al. (42) found that eating out or consuming foods away from home was associated with poorer nutritional quality, which typically contained more in fat and saturated fat and less in calcium, fibre and iron compared to home-made foods. These were probably true in the present study, where the number of food groups consumed was found to be strongly and positively associated with nutritional quality (11). Devine et al. (43) suggested that many workers may have sufficient information about healthy dietary choices but, due to work constraint, they perceive that they cannot put food choice ideals into practice. As a result, convenience seems to be the most important factor above personal health for working subjects when dealing with food choices in lunch (44). These may explain why this group of people had poorer diet quality, and nutrition intervention should include specific strategies to addressing the problems.
Type of medication is also found to predict the dietary quality significantly in the present study. Subjects with T2DM, who were on insulin regimen, tended to eat more food groups compared to their counterparts not on insulin regimen. The possible explanations for the differences are that those on insulin regimen might be more likely to feel better and to have less symptoms of dizziness, depression, fatigue, thirst and dry mouth, polyuria, and nocturia than their non-insulin counterparts (45,46). This better general wellbeing may lead to better appetite and feeling safe to include various food groups into their diet. In contrast, non-insulin group may be more cautious to take certain type of food groups which they perceived as forbidden, especially during poorly-controlled conditions; therefore, consuming less number of food groups than their insulin counterparts. To the best of our knowledge, there are inadequate studies on diet quality and type of medication used among individuals with T2DM. Diet therapy is one of the most important interventions for diabetes for those newly-diagnosed with T2DM. Thus, it is important for healthcare providers to reinforce the healthy eating concept for better diabetes management.
It is somewhat surprising that our data show contradictory results between the two anthropometric measures, namely BMI and WHR in predicting DDS. BMI seemed to be negatively associated while WHR was positively associated with DDS. Subjects with normal weight consumed significantly higher number of food groups and higher number of servings in all food groups, which indicated a better diet quality. On the other hand, subjects with higher WHR consumed significantly higher number of servings in all food groups and, in turn, had better diet quality. Inconsistent findings were found in the literature regarding the association between diet quality, obesity, and abdominal adiposity. Better diet quality or specifically more diversified and varied diets were often found to be associated with higher energy intake and, hence, obesity (47-50). However, such association may be affected by the nutrient contents of the diet or the distribution of the energy across various food groups. In a study by Azadbakht et al. (51), although subjects with higher DDS had significantly higher energy intake, such increase in energy intakes was attributed by the increased intake of healthy food groups and low-energy food groups and, hence, were inversely related to obesity and abdominal adiposity. This double-edged diversity may, hence, make the potential associations between diet quality and nutritional status difficult to reveal (52).
Limitations
This study has several limitations. First, the cross-sectional design did not allow us to rule out the direction of the associations, especially the association between diet quality and nutritional status. Second, the study subjects were individuals with T2DM, who had undergone routine check-ups and, hence, dietary changes among them were very likely. To address this shortcoming, food frequency questionnaire, instead of 24-hour dietary recall, was used for determining dietary diversity based on their usual dietary intake. Third, like other DDS studies (13,14,22), the definition of FGS and SS were limited to setting the minimum levels but not the upper limits, which restricted us from capturing those who had over-consumed. It is noteworthy that, although DDS is a relatively simple index that does not require any quantitative estimation of serving-size, this index was a positive predictor of dietary biomarkers (53) and nutrient adequacy (11,12), a negative predictor of CVD risk (13), and metabolic syndrome (14). However, a review of DDS suggested that this index might be improved by applying a minimum portion-size (54). As little as 10 g of cutoff was found to improve the sensitivity and specificity of the index and improve the ability to predict nutrient adequacy (55). Acknowledgeing the limitations of this study, the present study, nevertheless, is pertinent to other researchers and individuals with T2DM as research on diet quality is scarce. Diet is one of the most important treatments for individuals with T2DM where proper dietary intake could help them get rid of or to delay the development of diabetes complications.
Conclusions
The findings of this study demonstrate that high proportion of individuals with T2DM failed to adhere to the national dietary guidelines. Those with lower education, working, had low personal income, currently not on insulin regimen, being overweight or obese, and those with lower WHR were found to have a significantly poorer dietary diversity. The importance of taking a well-balanced diet in accordance with the national dietary guidelines should be emphasized among individuals with T2DM, especially those with lower education through a simple and easy-to-understand approach.
ACKNOWLEDGEMENTS
This research received no specific grant from any funding agency in the public, commercial or not-for-profit sectors. The authors are grateful to SW Food International (M) Pte Ltd. and Fonterra Brands (Malaysia) Pte Ltd. for their kind support as well as to all the participants from Serdang Hospital and the University Health Clinic of UPM for their enthusiastic cooperation.
Conflict of interest: The authors have no conflict of interest.
REFERENCES
- 1.Wild S, Roglic G, Green A, Sicree R, King H. Global prevalence of diabetes: estimates for the year 2000 and projections for 2030. Diabetes Care. 2004;27:1047–53. doi: 10.2337/diacare.27.5.1047. [DOI] [PubMed] [Google Scholar]
- 2.International Diabetes Federation . 5th ed. Brussels: International Diabetes Federation; 2011. IDF diabetes atlas; p. 25. [PubMed] [Google Scholar]
- 3.Whiting DR, Guariguata L, Weil C, Shaw J. IDF diabetes atlas: global estimates of the prevalence of diabetes for 2011 and 2030. Diabetes Res Clin Pract. 2011;94:311–21. doi: 10.1016/j.diabres.2011.10.029. [DOI] [PubMed] [Google Scholar]
- 4.Malaysia . Ministry of Health Malaysia. The third national health and morbidity survey 2006. V. II. Kuala Lumpur: Institute for Public Health, Ministry of Health Malaysia; 2008. p. 253. [Google Scholar]
- 5.Malaysia . Ministry of Health Malaysia. National health and morbidity survey 2011. Non-communicable diseases. V. II. Kuala Lumpur: Institute for Public Health, Ministry of Health Malaysia; 2011. p. 2. [Google Scholar]
- 6.Ummi Nadiah Y, Diana M, Azahadi O, Teh CH, Norzawati Y, Riyanti S. Burden of premature mortality in Malaysia. Int J Public Health Res. 2013;3:249–56. [Google Scholar]
- 7.Air EL, Kissela BM. Diabetes, the metabolic syndrome, and ischemic stroke: epidemiology and possible mechanisms. Diabetes Care. 2007;30:3131–40. doi: 10.2337/dc06-1537. [DOI] [PubMed] [Google Scholar]
- 8.American Diabetes Association Diagnosis and classification of diabetes mellitus. Diabetes Care. 2013;36(Suppl 1):S67–74. doi: 10.2337/dc13-S067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bantle JP, Wylie-Rosett J, Albright AL, Apovian CM, Clark NG, Franz MJ, et al. American Diabetes Association. Nutrition recommendations and interventions for diabetes: a position statement of the American Diabetes Association. Diabetes Care. 2008;31(Suppl 1):S61–78. doi: 10.2337/dc08-S061. [DOI] [PubMed] [Google Scholar]
- 10.Wirt A, Collins CE. Diet quality—what is it and does it matter? Public Health Nutr. 2009;12:2473–92. doi: 10.1017/S136898000900531X. [DOI] [PubMed] [Google Scholar]
- 11.Hatløy A, Torheim LE, Oshaug A. Food variety—a good indicator of nutritional adequacy of the diet? A case study from an urban area in Mali, West Africa. Eur J Clin Nutr. 1998;52:891–8. doi: 10.1038/sj.ejcn.1600662. [DOI] [PubMed] [Google Scholar]
- 12.Torheim LE, Ouattara F, Diarra MM, Thiam FD, Barikmo I, Hatløy A, et al. Nutrient adequacy and dietary diversity in rural Mali: association and determinants. Eur J Clin Nutr. 2004;58:594–604. doi: 10.1038/sj.ejcn.1601853. [DOI] [PubMed] [Google Scholar]
- 13.Azadbakht L, Mirmiran P, Esmaillzadeh A, Azizi F. Dietary diversity score and cardiovascular risk factors in Tehranian adults. Public Health Nutr. 2006;9:728–36. doi: 10.1079/phn2005887. [DOI] [PubMed] [Google Scholar]
- 14.Azadbakht L, Mirmiran P, Azizi F. Dietary diversity score is favorably associated with the metabolic syndrome in Tehranian adults. Int J Obes (Lond) 2005;29:1361–7. doi: 10.1038/sj.ijo.0803029. [DOI] [PubMed] [Google Scholar]
- 15.Waijers PMCM, Feskens EJM, Ocké MC. A critical review of predefined diet quality scores. Br J Nutr. 2007;97:219–31. doi: 10.1017/S0007114507250421. [DOI] [PubMed] [Google Scholar]
- 16.Cohen J. 2nd ed. Hillsdale, NJ: Lawrence Earlbaum Associates; 1988. Statistical power analysis for the behavioral sciences; p. 412. [Google Scholar]
- 17.Faul F, Erdfelder E, Lang A-G, Buchner A. G*Power 3: a flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav Res Methods. 2007;39:175–91. doi: 10.3758/bf03193146. [DOI] [PubMed] [Google Scholar]
- 18.WHO Expert Consultation Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies. Lancet. 2004;363:157–63. doi: 10.1016/S0140-6736(03)15268-3. [DOI] [PubMed] [Google Scholar]
- 19.World Health Organization . Melbourne: Health Communication Australia; 2000. The Asia-Pacific perspective: redefining obesity and its treatment; p. 55. [Google Scholar]
- 20.World Health Organization Obesity: prevention and managing the global epidemic. Report of the WHO consultation. World Health Organ Tech Rep Ser. 2000;894:i–xii. 1–253. [PubMed] [Google Scholar]
- 21.National Coordinating Committee on Food and Nutrition . Putrajaya: Ministry of Health Malaysia; 2010. Malaysian dietary guidelines; p. 6. [Google Scholar]
- 22.Kant AK, Block G, Schatzkin A, Ziegler RG, Nestle M. Dietary diversity in the US population, NHANES II, 1976-1980. J Am Diet Assoc. 1991;91:1526–31. [PubMed] [Google Scholar]
- 23.Norimah AK, Safiah MY, Zuhaida H, Fatimah S, Rohida SH, Siti Haslinda MD, et al. Putrajaya: Nutrition Section, Family Health Development Division, Ministry of Health Malaysia; 2008. Malaysian Adult Nutrition Survey 2003. Habitual food intake of adults aged 18 to 59 years. V. 7; p. 58. [Google Scholar]
- 24.Toeller M, Klischan A, Heitkamp G, Schumacher W, Milne R, Buyken A, et al. Nutritional intake of 2868 IDDM patients from 30 centres in Europe. EURODIAB IDDM Complications Study Group. Diabetologia. 1996;39:929–39. doi: 10.1007/BF00403912. [DOI] [PubMed] [Google Scholar]
- 25.Thanopoulou A, Karamanos B, Angelico F, Assaad-Khalil S, Barbato A, Del Ben M, et al. Multi-Centre Study of the Mediterranean Group for the Study of Diabetes (MGSD). Nutritional habits of subjects with Type 2 diabetes mellitus in the Mediterranean Basin: comparison with the non-diabetic population and the dietary recommendations. Multi-Centre Study of the Mediterranean Group for the Study of Diabetes (MGSD) Diabetologia. 2004;47:367–76. doi: 10.1007/s00125-003-1316-0. [DOI] [PubMed] [Google Scholar]
- 26.Gehling E. Medical nutrition therapy: an individualized approach to treating diabetes. Lippincotts Case Manag. 2001;6:2–12. [PubMed] [Google Scholar]
- 27.Kant AK, Leitzmann MF, Park Y, Hollenbeck A, Schatzkin A. Patterns of recommended dietary behaviors predict subsequent risk of mortality in a large cohort of men and women in the United States. J Nutr. 2009;139:1374–80. doi: 10.3945/jn.109.104505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kant AK, Graubard BI, Schatzkin A. Dietary patterns predict mortality in a national cohort: the National Health Interview Surveys, 1987 and 1992. J Nutr. 2004;134:1793–9. doi: 10.1093/jn/134.7.1793. [DOI] [PubMed] [Google Scholar]
- 29.Zemel MB. The role of dairy foods in weight management. J Am Coll Nutr. 2005;24(Suppl 6):537S–46S. doi: 10.1080/07315724.2005.10719502. [DOI] [PubMed] [Google Scholar]
- 30.Bush NC, Alvarez JA, Choquette SS, Hunter GR, Oster RA, Darnell BE, et al. Dietary calcium intake is associated with less gain in intra-abdominal adipose tissue over 1 year. Obesity (Silver Spring) 2010;18:2101–4. doi: 10.1038/oby.2010.39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Pereira MA, Jacobs DR, Jr, Van Horn L, Slattery ML, Kartashov AI, Ludwig DS. Dairy consumption, obesity, and the insulin resistance syndrome in young adults: the CARDIA Study. JAMA. 2002;287:2081–9. doi: 10.1001/jama.287.16.2081. [DOI] [PubMed] [Google Scholar]
- 32.McNaughton SA, Dunstan DW, Ball K, Shaw J, Crawford D. Dietary quality is associated with diabetes and cardio-metabolic risk factors. J Nutr. 2009;139:734–42. doi: 10.3945/jn.108.096784. [DOI] [PubMed] [Google Scholar]
- 33.McCabe-Sellers BJ, Bowman S, Stuff JE, Champagne CM, Simpson PM, Bogle ML. Assessment of the diet quality of US adults in the Lower Mississippi Delta. Am J Clin Nutr. 2007;86:697–706. doi: 10.1093/ajcn/86.3.697. [DOI] [PubMed] [Google Scholar]
- 34.Harrington J, Fitzgerald AP, Layte R, Lutomski J, Molcho M, Perry IJ. Sociodemographic, health and lifestyle predictors of poor diets. Public Health Nutr. 2011;14:2166–75. doi: 10.1017/S136898001100098X. [DOI] [PubMed] [Google Scholar]
- 35.Parmenter K, Waller J, Wardle J. Demographic variation in nutrition knowledge in England. Health Educ Res. 2000;15:163–74. doi: 10.1093/her/15.2.163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Norimah AK, Jr, Hwong CS, Liew WC, Ruzita AT, Siti Sa'adiah HN, Ismail MN. Messages of the newly proposed Malaysian Dietary Guidelines (MDG): do adults in Kuala Lumpur understand them? Malays J Nutr. 2010;16:113–23. [PubMed] [Google Scholar]
- 37.National Coordinating Committee on Food and Nutrition . Kuala Lumpur: Ministry of Health Malaysia; 1999. Malaysian dietary guidelines; p. 50. [Google Scholar]
- 38.Quinlan JJ, Lee L, Mangroo A, Vierow K. Evaluation of MyPlate as a dietary learning tool among young adults. J Acad Nutr Diet. 2012;112:A85. [Google Scholar]
- 39.Darmon N, Drewnowski A. Does social class predict diet quality? Am J Clin Nutr. 2008;87:1107–17. doi: 10.1093/ajcn/87.5.1107. [DOI] [PubMed] [Google Scholar]
- 40.Blaylock J, Smallwood D, Kassel K, Variyam J, Aldrich L. Economics, food choices, and nutrition. Food Policy. 1999;24:269–86. [Google Scholar]
- 41.Bowman SA. A comparison of the socioeconomic characteristics, dietary practices, and health status of women food shoppers with different food price attitudes. Nutr Res. 2006;26:318–24. [Google Scholar]
- 42.Lin B-H, Frazão E, Guthrie J. Away-from-home foods increasingly important to quality of American diet. Agricul Info Bull. 1999;749:22. [Google Scholar]
- 43.Devine CM, Connors MM, Sobal J, Bisogni CA. Sandwiching it in: spillover of work onto food choices and family roles in low- and moderate-income urban households. Soc Sci Med. 2003;56:617–30. doi: 10.1016/s0277-9536(02)00058-8. [DOI] [PubMed] [Google Scholar]
- 44.Blanck HM, Yaroch AL, Atienza AA, Yi SL, Zhang J, Mâsse LC. Factors influencing lunchtime food choices among working Americans. Health Educ Behav. 2009;36:289–301. doi: 10.1177/1090198107303308. [DOI] [PubMed] [Google Scholar]
- 45.Barnett AH. Tablet and insulin therapy in type 2 diabetes in the elderly. J R Soc Med. 1994;87:612–4. [PMC free article] [PubMed] [Google Scholar]
- 46.Johansen J, Claudi T, Holtedahl K. Insulin treatment for poorly regulated diabetic patients in general practice. Better regulation and symptom relief? Scand J Prim Health Care. 1999;17:244–9. doi: 10.1080/028134399750002485. [DOI] [PubMed] [Google Scholar]
- 47.Foote JA, Murphy SP, Wilkens LR, Basiotis PP, Carlson A. Dietary variety increases the probability of nutrient adequacy among adults. J Nutr. 2004;134:1779–85. doi: 10.1093/jn/134.7.1779. [DOI] [PubMed] [Google Scholar]
- 48.Kennedy E. Dietary diversity, diet quality, and body weight regulation. Nutr Rev. 2004;62(7 Pt. 2):S78–81. doi: 10.1111/j.1753-4887.2004.tb00093.x. [DOI] [PubMed] [Google Scholar]
- 49.Raynor HA, Epstein LH. Dietary variety, energy regulation, and obesity. Psychol Bull. 2001;127:325–41. doi: 10.1037/0033-2909.127.3.325. [DOI] [PubMed] [Google Scholar]
- 50.Jayawardena R, Byrne NM, Soares MJ, Katulanda P, Yadav B, Hills AP. High dietary diversity is associated with obesity in Sri Lankan adults: an evaluation of three dietary scores. BMC Public Health. 2013;13:314. doi: 10.1186/1471-2458-13-314. doi: 10.1186/1471-2458-13-314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Azadbakht L, Esmaillzadeh A. Dietary diversity score is related to obesity and abdominal adiposity among Iranian female youth. Public Health Nutr. 2010;14:62–9. doi: 10.1017/S1368980010000522. [DOI] [PubMed] [Google Scholar]
- 52.Savy M, Martin-Prével Y, Danel P, Traissac P, Dabiré H, Delpeuch F. Are dietary diversity scores related to the socio-economic and anthropometric status of women living in an urban area in Burkina Faso? Public Health Nutr. 2008;11:132–41. doi: 10.1017/S1368980007000043. [DOI] [PubMed] [Google Scholar]
- 53.Kant AK, Graubard BI. A comparison of three dietary pattern indexes for predicting biomarkers of diet and disease. J Am Coll Nutr. 2005;24:294–303. doi: 10.1080/07315724.2005.10719477. [DOI] [PubMed] [Google Scholar]
- 54.Ruel MT. Operationalizing dietary diversity: a review of measurement issues and research priorities. J Nutr. 2003;133((11 Suppl 2)):3911S–26S. doi: 10.1093/jn/133.11.3911S. [DOI] [PubMed] [Google Scholar]
- 55.Daniels MC, Adair LS, Popkin BM, Truong YK. Dietary diversity scores can be improved through the use of portion requirements: an analysis in young Filipino children. Eur J Clin Nutr. 2007;63:199–208. doi: 10.1038/sj.ejcn.1602927. [DOI] [PubMed] [Google Scholar]


