Abstract
Background. In the United States, measles, mumps, rubella, and varicella immunity is now primarily achieved through vaccination. Monitoring population immunity is necessary.
Methods. We evaluated seroprevalence of antibodies to measles, mumps, rubella, and varicella using the National Health and Nutrition Examination Survey during 2009–2010.
Results. Measles, mumps, rubella, and varicella seroprevalence was 92.0% (95% confidence interval [CI], 90.9%−93.0%), 87.6% (CI, 85.8%−89.2%), 95.3% (CI, 94.3%−96.2%), and 97.8% (CI, 97.1%−98.3%), respectively. United States (US)-born persons had lower mumps seroprevalence and higher varicella seroprevalence than non-US born persons.
Conclusions. Seroprevalence was high (88%–98%) for all 4 viruses in the US population during 2009−2010.
Keywords: antibodies, chickenpox, measles, mumps, NHANES, rubella, seroepidemiologic studies.
Measles, mumps, rubella, and varicella are acute viral diseases that are preventable by vaccination. In the United States (US), routine measles, rubella, and mumps vaccination of children was initiated in 1963, 1969, and 1977, respectively. The Advisory Committee on Immunization Practices (ACIP) recommended routine use of the combination measles, mumps and rubella (MMR) vaccine in 1977 and a 2-dose schedule at ages 12–15 months and 4–6 years in 1989 [1]. As a result of high MMR vaccination coverage (≥90% in children aged 19–35 months), incidence declined; endemic transmission of measles was declared eliminated in 2000 and documented for rubella and congenital rubella syndrome (CRS) in 2004 [2, 3]. However, import-associated cases continue to occur in the US, because measles and rubella remain endemic in other countries. Reported mumps cases also declined to an average of <300 cases annually by the early 2000s, with outbreaks occurring in limited settings [1, 4, 5].
The varicella vaccination program was implemented in 1996 as a 1-dose program. By the end of the first decade of the program, vaccination coverage reached 90% among children aged 19–35 months and incidence declined by 90% [6]. However, outbreaks continued to occur among highly vaccinated populations [7]. In 2006, ACIP recommended implementation of a routine 2-dose program, with vaccination at the same ages as MMR vaccine [6]. Further reductions in incidence and outbreaks have been reported since 2006 [8].
To sustain these achievements, high population immunity is needed. Reported antibody seroprevalence from the National Health and Nutrition Examination Survey (NHANES) from 1999 to 2004 was 96%, 90%, and 91% for MMR respectively [9–11]. Varicella seroprevalence among those aged 6–19 and 20–49 years was 94% and 98%, respectively [12]. Monitoring population seroprevalence remains important to potentially identify subgroups with higher susceptibility and guide national immunization policies. We assessed seroprevalence of measles, mumps, rubella, and varicella antibodies in the US civilian noninstitutionalized population aged 6–49 years using samples from NHANES 2009–2010.
METHODS
The NHANES is conducted by the National Center for Health Statistics (NCHS), Centers for Disease Control and Prevention (CDC), to assess the health and nutritional status of the US population. The survey uses a stratified, multistage, probability-cluster design, to provide a sample representative of the civilian noninstitutionalized US population. Survey participants undergo household interviews, standardized physical examinations, and provide biological samples for testing. Non-Hispanic blacks and Hispanics were oversampled to provide stable estimates for these groups. Informed consent was obtained from all participants, and the Institutional Review Board of NCHS, CDC approved the protocol.
Serum samples from NHANES participants aged 6–49 years during 2009–2010 were tested for immunoglobulin G (IgG) antibodies of interest. Commercially available indirect enzyme-linked immunosorbent IgG assays (IgG ELISA II; Wampole Laboratories) were used for the detection and qualitative determination of IgG antibody to MMR viruses. IgG antibodies to measles and mumps viruses were categorized based on index standard ratio (ISR) values as follows: seronegative, ISR of ≤0.90; indeterminate, ISR of 0.91–1.09; and seropositive, ISR of ≥1.10. For rubella, values of ≥10 IU were considered seropositive. Seronegative and indeterminate samples were retested with an equal number of randomly selected seropositive samples. Samples that initially tested indeterminate then positive on retesting were categorized as seropositive; negative or indeterminate samples were categorized as negative for this study. Discordant results were reconciled by 1 additional test; the final result was used. For quality assurance, a 10% random-sample repeat of the entire specimen collection set was performed. For varicella, the CDC in-house varicella whole-cell enzyme immunoassay (W-EIA) was used; IgG antibodies were categorized based on optical density (OD). Samples with OD of ≥0.250 were considered seropositive. Samples testing W-EIA negative (OD of <0.170) or indeterminate (OD of 0.170–0.249) were retested using a more sensitive glycoprotein antigen-based EIA (gpELISA) appropriate for detection of vaccine-induced antibodies [12]. Samples were considered seropositive if gpELISA-adjusted OD was ≥0.200 and considered seronegative if <0.200.
Procedures used in previous analysis of NHANES measles, mumps, rubella, and varicella data were used here [9–12]. Participants were grouped by birth year (1957–1966, 1967–1976, 1977–1986, 1987–1998, and 1999–2004) and age (6–11 years, 12–19 years, 20–29 years, 30–39 years, and 40–49 years) [9–12]. Race and Hispanic origin were based on the respondent's self-assessment and categorized as non-Hispanic white, non-Hispanic black, Mexican American, and other (subjects who did not self-select into the previous groups or reported multiple races). Separate estimates were not reported for the other race/ethnic group, but these individuals were included in all other estimates. Birthplace was coded as US and non-US. Estimates were weighted to represent the total civilian noninstitutionalized US household population and account for oversampling and nonresponse [13]. Standard errors were calculated accounting for the complex sample design using SUDAAN software (version 11.0.1). Estimates were considered unstable if the relative standard error around the percent seronegative participants was >30% or if based on <10 seronegative persons. The exact binomial method was used to calculate 95% confidence intervals (CIs) [14]. The t tests were used to assess differences between groups; P values < .05 were considered significant. No adjustments for multiple comparisons were made.
RESULTS
Response Rates
Of 6981 persons aged 6–49 years sampled for NHANES 2009–2010, 5785 (83%) were interviewed and 5652 (81%) were examined. Of those examined, 5054 (89%) had serum samples available for testing. The percent of participants with tested samples varied by age (6–11 years, 79%; 12–49 years, ≥90%), race/Hispanic origin (Mexican American, 92%; non-Hispanic white, 89%; non-Hispanic black, 86%; P < .05), and birthplace (US, 88%; non-US, 94%; P < .05), but not sex.
Seroprevalence of Measles, Mumps, and Rubella Antibody
During 2009–2010, among the US population aged 6–49 years, MMR seroprevalence was 92.0% (95% CI, 90.9%–93.0%), 87.6% (95% CI, 85.8%–89.2%), and 95.3% (95% CI, 94.3%–96.2%), respectively. Measles and mumps seroprevalence was higher among those aged 6–11 years compared to all other age groups (P < .05) (Table 1). Rubella seroprevalence was also highest among those aged 6–11 years, but this estimate was unstable (based on <10 negative persons with a relative standard error of >40%). Seroprevalence was lowest among those aged 30–39 years compared to each other age group for all 3 outcomes, but these differences only reached statistical significance for measles. Rubella seroprevalence was higher in females than males (97.2% vs 93.5%; P < .001), but no gender differences were observed for measles and mumps.
Table 1.
Seroprevalence of Measles, Mumps, Rubella and Varicella Antibodies by Demographic Characteristics: National Health and Nutrition Examination Survey, 2009–2010.
| n | Measles |
Mumps |
Rubella |
Varicella |
|||||
|---|---|---|---|---|---|---|---|---|---|
| % (95% CI) | P Value | % (95% CI) | P Value | % (95% CI) | P Value | % (95% CI) | P Value | ||
| Overall | 5054 | 92.0 (90.9–93.0) | 87.6 (85.8–89.2) | 95.3 (94.3–96.2) | 97.8 (97.1–98.3) | ||||
| Age | |||||||||
| 6–11 years (ref) | 960 | 96.8 (94.5–98.4) | 91.9 (89.3–94.1) | 99.1 (97.9–99.7)a | 98.0 (96.0–99.1)b | ||||
| 12–19 years | 1172 | 93.2 (89.8–95.7) | <.05 | 86.9 (83.2–90.1) | <.05 | 97.0 (95.5–98.2) | <.01 | 97.1 (95.7–98.2) | NS |
| 20–29 years | 950 | 93.3 (90.9–95.3) | <.05 | 87.7 (84.8–90.3) | <.05 | 95.8 (94.2–97.0) | <.001 | 97.6 (96.0–98.7) | NS |
| 30–39 years | 937 | 87.9 (84.8–90.6) | <.001 | 85.6 (81.5–89.2) | <.01 | 93.4 (90.9–95.3) | <.001 | 97.0 (94.6–98.5) | NS |
| 40–49 years | 1035 | 91.2 (89.0–93.2) | <.001 | 87.8 (84.9–90.2) | <.05 | 93.8 (91.8–95.4) | <.001 | 98.9 (97.8–99.6)b | NS |
| Sex | |||||||||
| Male | 2483 | 91.5 (89.2–93.5) | NS | 86.8 (84.8–88.7) | NS | 93.5 (92.2–94.6) | <.001 | 97.6 (96.8–98.3) | NS |
| Female | 2571 | 92.4 (91.0–93.7) | 88.4 (86.3–90.2) | 97.2 (96.1–98.0) | 97.9 (97.2–98.4) | ||||
| Race/Ethnicity | |||||||||
| Non-Hispanic white (ref) | 1971 | 91.3 (89.5–92.9) | 85.8 (83.1–88.1) | 95.0 (93.6–96.2) | 98.5 (97.9–99.0) | ||||
| Non-Hispanic black | 928 | 96.2 (94.9–97.2) | <.001 | 92.0 (89.1–94.3) | <.001 | 97.2 (95.9–98.2) | <.01 | 96.3 (95.0–97.4) | <.01 |
| Mexican American | 1232 | 87.0 (84.9–88.9) | <.01 | 89.0 (87.3–90.6) | <.05 | 94.2 (92.0–95.9) | NS | 97.8 (96.6–98.7) | NS |
| Birthplace | |||||||||
| Non-US | 1099 | 92.2 (89.6–94.3) | NS | 92.3 (89.9–94.2) | <.001 | 95.8 (94.1–97.2) | NS | 95.6 (93.7–97.1) | <.01 |
| US | 3951 | 91.9 (90.5–93.2) | 86.6 (84.7–88.4) | 95.2 (94.0–96.2) | 98.2 (97.6–98.7) | ||||
Abbreviations: CI, confidence interval; NS, not significant (P > .05); ref, reference group.
a Estimates unstable based on <10 negative sample persons and relative standard error >40%.
b Estimates unstable relative standard error >30%.
Seroprevalence was significantly higher among non-Hispanic blacks than non-Hispanic whites for all 3 outcomes (P < .01) (Table 1) and among non-Hispanic blacks than Mexican Americans for measles and rubella (P < .001 and P < .05, respectively). Non-Hispanic whites had higher measles seroprevalence than Mexican Americans but lower mumps seroprevalence (P < .001 and P < .05, respectively). There was no difference in rubella seroprevalence between non-Hispanic whites and Mexican Americans. US-born persons had lower mumps seroprevalence compared to non-US born persons (86.6% vs 92.3%; P < .001), but no differences were observed for measles and rubella.
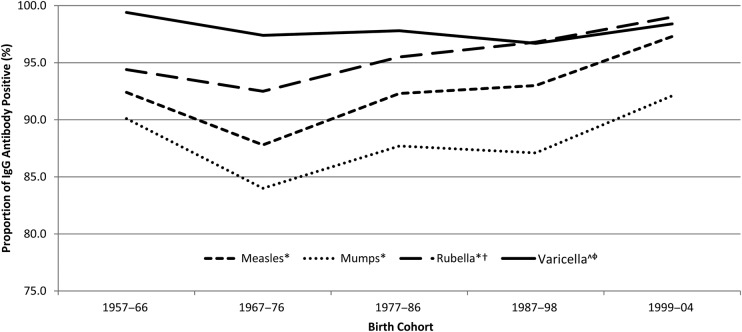
Trends by birth cohorts were similar for measles, mumps, and rubella, with the highest seroprevalence among those born during 1999–2004 and lowest among those born during 1967–1976 (Figure 1). There was a significant linear increase in all 3 outcomes from the 1967–1976 to the 1999–2004 birth cohort (P < .001). However, the 1999–2004 birth cohort rubella seroprevalence estimate was unstable.
Figure 1.
Seroprevalence of measles, mumps, rubella (MMR) and varicella antibodies by birth cohorts: National Health and Nutrition Examination Survey, 2009–2010. *For MMR: P < .001 for the test for linear trend from the 1967–1976 birth cohort to the 1999–2004 birth cohort; †Estimate for Rubella seroprevalence for birth cohort 1999–2004 may be unstable. Relative standard error = 51% and it is based on 6 seronegative samples; ^Estimate for Varicella seroprevalence for birth cohort 1957–1966 may be unstable. Relative standard error = 43% and it is based on 5 seronegative samples; ϕEstimate for Varicella seroprevalence for birth cohort 1999–2004 may be unstable. Relative standard error = 50%.
Seroprevalence of Varicella Antibody
Varicella seroprevalence was 97.8% (95% CI, 97.1%–98.3%) and consistently high across all age groups. Seroprevalence was lower among non-Hispanic blacks than non-Hispanic whites (P < .01) and Mexican Americans (P = .05) (96.3%, 98.5%, and 97.8%, respectively). Seroprevalence was higher in US-born than non-US born persons (98.2% vs 95.6%; P < .01). There was little variability across birth cohorts (Figure 1). However, estimates for the 1957–1966 and 1999–2004 birth cohorts were unstable.
DISCUSSION
Overall seroprevalence remains high for measles, mumps, rubella, and varicella antibodies in the US population aged 6–49 years during 2009–2010. Seroprevalence was highest among those aged 6–11 years, a group likely to have been vaccinated recently. Lower estimates in older age groups (birth cohort 1967–1976) for MMR is consistent with findings from previous NHANES and could be a result of lower vaccination levels, changes in vaccine policy, and declining disease prevalence, and immunosenescence [9, 10]. US-born persons had lower mumps and higher varicella seroprevalence than non-US born persons. Lower seroprevalence among some subgroups may indicate populations at increased risk for transmission and outbreaks of these vaccine-preventable diseases.
High measles seroprevalence reflects high vaccine coverage nationally; however, 8% of persons aged 6–49 years were found to be susceptible. Susceptibility is likely to be even higher if we considered children aged <12 months. Susceptible persons remain at risk for measles in the US, primarily due to importation. During 2001–2011, 88% of the 911 reported measles cases were import-associated [15]. As long as measles remains endemic in other countries, importations will continue with the risk for sustained outbreaks among unvaccinated populations.
Seroprevalence was lower for mumps than measles and rubella. Lower seroprevalence may be explained by the lower effectiveness of the mumps component of the MMR vaccine estimated at 88% (range, 66–95%) compared with 97% (range, 67%–100%) for measles and 97% (range, 94%–100%) for rubella [1]. However, although antibody measurements are often used as surrogate measures of immunity, no serologic tests that reliably predict immunity are available for mumps. Although recent mumps outbreaks occurred in populations with high 2-dose coverage, they were limited to intense exposure settings, with limited spread outside these settings [4, 5]. To maintain control of mumps, it remains important to ensure appropriate MMR vaccination among children and persons in settings with the potential for intense exposure and transmission of mumps (eg, schools, colleges, correctional facilities, congregate living facilities, or healthcare settings) [1].
Rubella seroprevalence was high (>93%) in all subgroups. As a result, few rubella and only 4 CRS cases have been reported through national surveillance during 2005–2011 [1, 15]. The higher rubella seroprevalence during 2009–2010 in women than men likely reflects continued efforts to vaccinate susceptible women of child-bearing age as part of the efforts to maintain CRS elimination.
During 2009–2010, varicella seroprevalence was high across all age groups. Age group-specific estimates were similar to estimates from NHANES 1999–2004, except children aged 6–11 years, where seroprevalence increased from 88.9% to 98.0% [12]. Considering the low varicella incidence among children in the last decade, this increase could be directly attributed to the successful implementation of routine varicella vaccination in the US starting in 1996. By 2008, 1-dose varicella vaccination coverage among children aged 19–35 months reached 91% [16]. Fewer children will enter adolescence and adulthood susceptible to varicella and at risk of severe disease. Similar to previous studies, seroprevalence was lower in those born outside compared with inside the US [12]. Providers should continue to assess evidence of immunity for all non-US born adults, irrespective of age.
This study has several limitations. Sample sizes for subgroup estimates were limited or unstable because data was only available for 2 survey years. Hence, results for these subgroups should be interpreted with caution. Second, ELISA testing methods for measles and rubella differed from NHANES 1999–2004; therefore, the 2 survey periods were not directly comparable. Finally, NHANES does not collect disease or vaccination history so we were unable to distinguish between seropositivity due to infection versus vaccination.
CONCLUSIONS
Results from NHANES 2009–2010 indicate high seroprevalence to measles, mumps, rubella, and varicella in the civilian non-institutionalized US population aged 6–49 years and provides evidence to support sustained maintenance of elimination of measles, rubella, and CRS, and low mumps and varicella incidence in the US. Measles and rubella remain endemic in much of the world with ongoing risk for importation to the US. Monitoring seroprevalence is an important component of understanding risks for these diseases in the US.
Acknowledgments
We acknowledge the laboratory staff at the Measles, Mumps, Rubella, and Herpersviruses Laboratory Branch, Division of Viral Diseases, US Centers for Disease Control and Prevention (CDC), for performing serology testing.
Financial support. This work was supported by the CDC (Atlanta, Georgia).
Potential conflicts of interest. All authors: No reported conflicts.
All authors have submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest.
References
- 1.McLean HQ, Fiebelkorn AP, Temte JL, et al. Prevention of measles, rubella, congenital rubella syndrome, and mumps, 2013: summary recommendations of the Advisory Committee on Immunization Practices (ACIP) MMWR Recomm Rep. 2013;62:1–34. [PubMed] [Google Scholar]
- 2.Katz SL, Hinman AR. Summary and conclusions: measles elimination meeting, 16–17 March 2000. J Infect Dis. 2004;189(Suppl 1):S43–7. doi: 10.1086/377696. [DOI] [PubMed] [Google Scholar]
- 3.Reef SE, Cochi SL. The evidence for the elimination of rubella and congenital rubella syndrome in the United States: a public health achievement. Clin Infect Dis. 2006;43(Suppl 3):S123–5. doi: 10.1086/505943. [DOI] [PubMed] [Google Scholar]
- 4.Dayan GH, Quinlisk MP, Parker AA, et al. Recent resurgence of mumps in the United States. N Engl J Med. 2008;358:1580–9. doi: 10.1056/NEJMoa0706589. [DOI] [PubMed] [Google Scholar]
- 5.Barskey AE, Schulte C, Rosen JB, et al. Mumps outbreak in Orthodox Jewish communities in the United States. N Engl J Med. 2012;367:1704–13. doi: 10.1056/NEJMoa1202865. [DOI] [PubMed] [Google Scholar]
- 6.Marin M, Guris D, Chaves SS, et al. Prevention of varicella: recommendations of the Advisory Committee on Immunization Practices (ACIP) MMWR Recomm Rep. 2007;56:1–40. [PubMed] [Google Scholar]
- 7.Guris D, Jumaan AO, Mascola L, et al. Changing varicella epidemiology in active surveillance sites--United States, 1995–2005. J Infect Dis. 2008;197(Suppl 2):S71–5. doi: 10.1086/522156. [DOI] [PubMed] [Google Scholar]
- 8.Bialek SR, Perella D, Zhang J, et al. Impact of a routine two-dose varicella vaccination program on varicella epidemiology. Pediatrics. 2013;132:e1134–40. doi: 10.1542/peds.2013-0863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.McQuillan GM, Kruszon-Moran D, Hyde TB, et al. Seroprevalence of measles antibody in the US population, 1999–2004. J Infect Dis. 2007;196:1459–64. doi: 10.1086/522866. [DOI] [PubMed] [Google Scholar]
- 10.Kutty PK, Kruszon-Moran DM, Dayan GH, et al. Seroprevalence of antibody to mumps virus in the US population, 1999–2004. J Infect Dis. 2010;202:667–74. doi: 10.1086/655394. [DOI] [PubMed] [Google Scholar]
- 11.Hyde TB, Kruszon-Moran D, McQuillan GM, et al. Rubella immunity levels in the United States population: has the threshold of viral elimination been reached? Clin Infect Dis. 2006;43(Suppl 3):S146–50. doi: 10.1086/505947. [DOI] [PubMed] [Google Scholar]
- 12.Reynolds MA, Kruszon-Moran D, Jumaan A, et al. Varicella seroprevalence in the U.S.: data from the National Health and Nutrition Examination Survey, 1999–2004. Public Health Rep. 2010;125:860–9. doi: 10.1177/003335491012500613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Johnson CL, Paulose-Ram R, Ogden CL, et al. National health and nutrition examination survey: analytic guidelines, 1999–2010. Vital Health Stat. 2013. pp. 1–24. [PubMed]
- 14.Korn LK, Graubard BI. Confidence intervals for proportions with small expected number of positive counts estimated form survey data. Surv Methodol. 1998;24:193–201. [Google Scholar]
- 15.Papania MJ, Wallace GS, Rota PA, et al. Elimination of endemic measles, rubella, and congenital rubella syndrome from the Western hemisphere: the US experience. JAMA Pediatr. 2014;168:148–55. doi: 10.1001/jamapediatrics.2013.4342. [DOI] [PubMed] [Google Scholar]
- 16.Centers for Disease Control and Prevention. National, state, and local area vaccination coverage among children aged 19–35 months - United States, 2008. MMWR Morb Mortal Wkly Rep. 2009;58:921–6. [PubMed] [Google Scholar]