Abstract
Volumetric studies suggest smaller amygdalae in subjects with schizophrenia (SZ) than with bipolar disorder (BP). We use morphometry to identify subregions of amygdala differentially affected in SZ and psychotic BP. Based on template centered population analysis, the shape of the amygdala in psychotic BP differs from SZ (pleft=0.044, pright=0.042). Using a high-field 7T atlas, the bilateral basolateral, basomedial and centromedial subregions and the right lateral subregion were significantly atrophied in SZ compared to psychotic BP (p<0.02). These results suggest that change in shape of amygdala may represent a morphologic feature distinguishing SZ from psychotic BP.
Keywords: psychotic bipolar disorder, schizophrenia, amygdala, morphometry
1. INTRODUCTION
Epidemiologic, genetic and neuroimaging studies suggest both shared and unique susceptibility factors for bipolar disorder (BP) and schizophrenia (SZ) (Craddock and Owen, 2010). One potentially informative distinction can be made between subtypes of BP presenting with and without psychosis (Potash, 2006) and it has been suggested that neuroanatomical features of psychotic BP, rather than BP without psychosis, may be more similar to what is seen in SZ (Strasser et al., 2005). However, volumes of amygdala have been reported to be smaller in SZ than in psychotic BP (Frazier et al., 2008; Mahon et al., 2012; Velakoulis et al., 2006).
The amygdalae are comprised of many functionally different nuclei. Assessing the surface of the amygdala may provide additional information about specific nuclei or pathways affected, which might then correlate with clinical features. We are aware of only two studies examining shape of amygdala in both SZ and BP (Mamah et al., 2010; Qiu et al., 2013). These studies reported discrepant findings, with one observing atrophy in SZ and the other not. Evidence for differential involvement of amygdalar subregions in SZ and BP also comes from resting state functional connectivity and postmortem studies (Liu et al., 2014; Varea et al., 2012).
We previously reported smaller amygdala volume in SZ compared to psychotic BP (Mahon et al., 2012). Here, we extend that study by utilizing morphometry to examine neuroanatomic features of amygdala in the same sample. Specifically, we examine amygdala for differences in surface shape and utilize a high-field 7T parcellation of amygdala to map features across coordinate systems and examine differences in four subregions.
2. METHODS
2.1 Subjects
This sample has been described in detail previously (Mahon et al., 2012; Ratnanather et al., 2013). All subjects provided informed consent prior to participating in the study. Briefly, right-handed subjects were selected from SZ and BP studies at Johns Hopkins University School of Medicine. Consensus diagnosis of BP or SZ was determined using a semi-structured interview and two instruments, either the DIGS and MINI or SCAN and CIDI-SF. All BP patients had at least one episode of psychotic symptoms. Healthy comparison (HC) subjects were screened for mental illness using the same instruments. All affected participants had a history of medication use. No SZ subjects were on lithium. Distributions of age and sex of subjects were similar across the diagnostic groups (Table 1).
Table 1.
Demographic and clinical characteristics
| Psychotic Bipolar Disorder (n=36) | Schizophrenia (n=31) | Healthy Comparison (n=27) | Statistical Test, p-value | |
|---|---|---|---|---|
| Age, years | 39.9(11.1) | 41.4(9.5) | 44.0(15.6) | F=0.93, p=0.400 |
| Males (%) | 52.8 | 54.8 | 44.4 | χ2=0.69, p=0.707 |
| Education level, years | 14.6(2.5) | 12.5(2.2) | 13.7(2.6) | F=5.61, p=0.005 |
| Socioeconomic status | 3.2(1.0) | 3.9(1.2) | 3.8(1.0) | F=4.10, p=0.020 |
| Duration of illness, years | 17.6(12.7) | 19.3(11.0) | NA | t59=0.54, p=0.593 |
2.2 MRI
T1 weighted 3D volumes were acquired using a 1.5 T Philip MR system and MPRAGE sequence (TR = 13.40 ms, TE = 4.6 ms, flip angle = 20, FOV 256 × 256), with 1-mm3 isotropic resolution across the entire cranium. Skullstripping was performed in Freesurfer 3.0.5 (Ségonne et al., 2004). Semi-automated segmentation of amygdala was performed in MRIStudio software (Jiang et al., 2006), utilizing the LDDMM algorithm (Oishi et al., 2009) and the JHU-MNI-SS Type II atlas (www.mristudio.org). Segmentations were blind to diagnosis, were visually inspected and manually edited where necessary. Segmentations were converted into triangulated surfaces using isosurface polygonization.
2.3 Amygdala Subregion Parcellation
A T1 weighted 3D volume for a 42 year old healthy male volunteer was acquired using a 7.0T Philips Achieva scanner. The subject was scanned using a standard MPRAGE protocol with 0.8mm isotropic resolution (TR =4.3 ms, TE=1.95ms, flip angle = 7, FOV = 220x220x180). Based on The Atlas of the Human Brain (Mai et al., 2007), the amygdala was partitioned into four subregions: lateral, basolateral, basomedial and centromedial (http://caportal.cis.jhu.edu/wiki/tutorials/amygdala/amygdala.html).
2.4 Shape Analysis via Surface-Based Morphometry
2.4.1 Vertex Marker
These methods have been described in detail previously (Miller et al., 2014; Younes et al., 2014). Briefly, all 1.5T amygdalar surfaces were rigidly aligned. A population template, a common coordinate system of all surfaces, was generated using the aligned volumes and a generative shape model. The population template was mapped to each subject’s structure, and a deformation marker measuring the expansion/atrophy at each vertex for each subject was calculated. The log-Jacobian is a measure of the local expansion/atrophy of the surface around a particular vertex. To a first approximation, it is the % increase or decrease in surface area around a particular vertex. The vertex marker has 796 dimensions, associated with the number of vertices.
2.4.2 High-field Markers
We also computed four high-field subregion markers, defined from the 7T image described above and mapped onto the population template using LDDMM surface matching. This transports the labeled high-field template to the population template allowing the labeling of the vertices (Miller et al., 2014).
2.5 Statistical Analysis
Generalized linear models were used to compare the shape markers for group differences. Age and gender were included as covariates. Education and socioeconomic status did not contribute significantly (LRT≥0.12) and were not included in the final model. For the vertex markers, statistics were computed at each vertex of the template surface and permutation tests were utilized to account for multiple comparisons. For the high-field markers, statistics were computed for each of the four subregions and a threshold for significance was determined based on permutation testing.
3. RESULTS
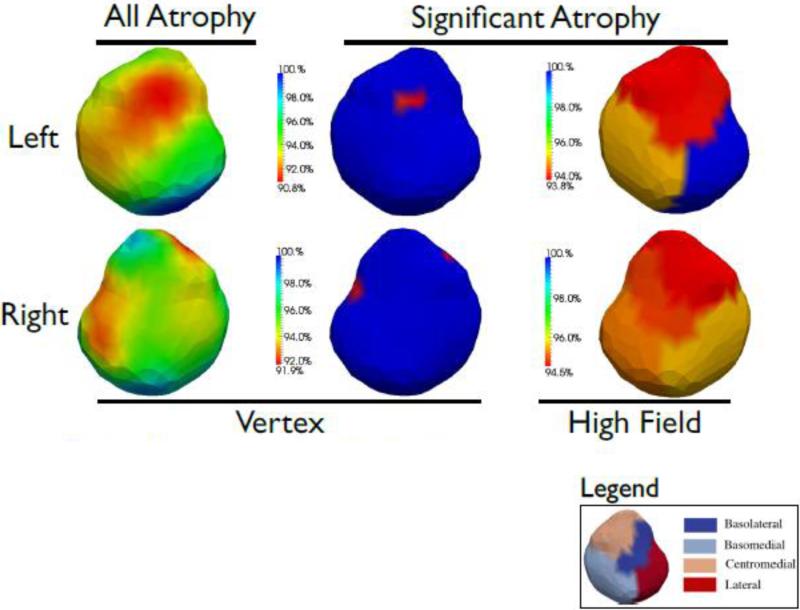
The vertex marker and high-field marker results indicate bilateral atrophy in SZ as compared to psychotic BP (Table 2 and Figure). Specifically, left basolateral and centromedial subregions show the largest proportion of atrophy in SZ as compared to psychotic BP with 6% atrophy in both regions. There was also 5% atrophy in the left basomedial subregion in SZ. The left lateral subregion was similar between SZ and psychotic BP. For right amygdala, all subregions were significantly atrophied in SZ as compared to psychotic BP (4-5% atrophy). Trends toward atrophy in SZ (pvertex=0.09) and expansion in BP (pvertex=0.075) as compared to HC were observed in right amygdala (Table 2).
Table 2.
Group differences in amygdala shapea
| Vertex Marker | High Field Markers | |||||
|---|---|---|---|---|---|---|
| Basolateral | Basomedial | Centromedial | Lateral | |||
| SZ v. BP | Left | 0.044 | 0.004 | 0.008 | 0.002 | 0.443 |
| Right | 0.042 | 0.014 | 0.019 | 0.012 | 0.019 | |
| SZ v. HC | Left | 0.456 | 0.110 | 0.293 | 0.104 | 0.984 |
| Right | 0.09 | 0.012 | 0.040 | 0.076 | 0.278 | |
| BP v. HC | Left | 0.344 | 0.265 | 0.149 | 0.218 | 0.521 |
| Right | 0.075 | 0.840 | 0.856 | 0.572 | 0.125 | |
Shown are the p-values from permutation testing at 5% familywise error rate. Columns list the p-values from the vertex (796 dimensions per structure) and the four high-field regions (1 dimension per structure). Thresholds determined by permutation with p-values shown in bold significant. SZ=schizophrenia, BP=psychotic bipolar disorder, HC=healthy comparison
Figure. Results modeling SZ as compared to psychotic BP.
Top and bottom rows portray left and right amygdala respectively. The left column shows the vertex marker and all % atrophy, regardless of significance. Note that the relative % surface atrophy is shown, with 100% meaning no difference. The middle column shows the vertex maker with regions of statistically significant atrophy shown in red, the blue implies no statistically significant atrophy (determinant Jacobian=1). The right column shows the four high field markers, with 7T subfields transferred to the 1.5T population template. Where there is statistically significant reduction, the relative % atrophy is shown in warm hues (yellow to red), with red indicating the largest % atrophy, the blue implies no statistically significant atrophy (determinant Jacobian=1). The legend shows the segmentations of the four subregions in the left amygdala.
4. DISCUSSION
This study expands upon our previous work comparing volume of amygdala in patients with psychotic BP and SZ, where we reported a significantly smaller volume of amygdala in SZ than in psychotic BP. Here, we examined surface shape of amygdala in the same sample and observed similar left lateral amygdala in the SZ and psychotic BP groups. All other subregions showed significant atrophy in SZ as compared to psychotic BP.
To our knowledge, only two previous studies have directly compared shape of amygdala in SZ and BP. Mamah et al (2010) were unable to detect morphometric differences using 10 principal components representing variation in surface shape in their sample of 11 SZ subjects and 12 BP subjects. Similar to our findings, a second larger study with 28 participants in each group found that subjects with first episode SZ displayed atrophy in the right amygdala, as compared to subjects with first-episode mania based on a log-Jacobian marker (Qiu et al., 2013). Using a vertex marker, we identified a similar small region of atrophy in SZ versus psychotic BP, although we observed atrophy bilaterally. Two potentially important differences between our study and both previous studies is our focus on the phenotype of psychotic BP and the different shape markers utilized. Interestingly, atrophy in the basolateral subregion of amygdala has been reported in familial pediatric BP, paralleling findings of reduced volume of amygdala in pediatric BP (Kelley et al., 2013).
The amygdala, or amygdaloid complex, is comprised of many different nuclei and is involved in a variety of functions including memory, perception, attention and fear conditioning. In functional neuroimaging studies, bilateral amygdala hyperactivation to facial affect processing has been found in patients with BP and hypoactivation in patients with SZ (Anticevic et al., 2012; Chen et al., 2011; Delvecchio et al., 2013; Li et al., 2010; Taylor et al., 2012). Different patterns of functional connectivity between amygdala subregions and frontal regions have been identified in BP and SZ (Liu et al., 2014). In postmortem studies, synaptic and plasticity-related markers have also been shown to differ between BP and SZ in specific amygdala nuclei (Varea et al., 2012).
Our high-field marker results suggest that the left lateral subregion is similar in SZ and psychotic BP, but not the right. The lateral nucleus of the amygdala receives projections from the sensory neocortex and thalamus and acts as the primary sensory interface for the amygdala . Our finding of different subregions affected in left and right amygdala may reflect on the lateralization of amygdala function reported for various facets in emotion perception studies (Costafreda et al., 2008; Fusar-Poli et al., 2009; Murphy et al., 2003; Sergerie et al., 2008; Wager et al., 2003).
A limitation of the current study is that we do not have available a sample with non-psychotic BP for comparison. Also, this study was not designed to assess the potential confounding effects of medication. For example, pre-clinical studies suggest that lithium may have a neuroprotective effect in the amygdala (Johnson et al., 2009). Thus, it is possible that our observed differences might be attributable to medication use.
These results suggest that change in shape of amygdala may represent a morphologic feature distinguishing psychotic BP from SZ. While the nature of abnormalities of the amygdala in BP and SZ differ, this brain region might still be the locus of a partially shared pathophysiology between these disorders.
ACKNOWLEDGEMENTS
We thank all participants for generously helping us with this research.
ROLE OF THE FUNDING SOURCE
This work was supported by grants from the Johns Hopkins Medicine Brain Science Institute and the National Institute of Health (K01 MH093870, R01 MH064838, R01 EB000975, P41 EB015909, R01 EB008171).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
CONTRIBUTORS
P.B.M. contributed to the study design, analysis, interpretation and manuscript writing; D.S.L., D.T., H.T. contributed to the analysis and interpretation; L.Y. contributed to the study design, analysis and interpretation; M.I.M., P.B., contributed to the study design and interpretation; J.T.R. contributed to the study design, interpretation and manuscript writing. All authors contributed to and have approved the final manuscript.
CONFLICT OF INTEREST
All authors declare that they have no conflicts of interest.
REFERENCES
- Anticevic A, Van Snellenberg JX, Cohen RE, Repovs G, Dowd EC, Barch DM. Amygdala recruitment in schizophrenia in response to aversive emotional material: a meta-analysis of neuroimaging studies. Schizophr. Bull. 2012;38:608–21. doi: 10.1093/schbul/sbq131. doi:10.1093/schbul/sbq131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen C-H, Suckling J, Lennox BR, Ooi C, Bullmore ET. A quantitative meta-analysis of fMRI studies in bipolar disorder. Bipolar Disord. 2011;13:1–15. doi: 10.1111/j.1399-5618.2011.00893.x. doi:10.1111/j.1399-5618.2011.00893.x. [DOI] [PubMed] [Google Scholar]
- Costafreda SG, Brammer MJ, David AS, Fu CHY. Predictors of amygdala activation during the processing of emotional stimuli: a meta-analysis of 385 PET and fMRI studies. Brain Res. Rev. 2008;58:57–70. doi: 10.1016/j.brainresrev.2007.10.012. doi:10.1016/j.brainresrev.2007.10.012. [DOI] [PubMed] [Google Scholar]
- Craddock N, Owen MJ. The Kraepelinian dichotomy - going, going... but still not gone. Br. J. Psychiatry. 2010;196:92–5. doi: 10.1192/bjp.bp.109.073429. doi:10.1192/bjp.bp.109.073429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Delvecchio G, Sugranyes G, Frangou S. Evidence of diagnostic specificity in the neural correlates of facial affect processing in bipolar disorder and schizophrenia: a meta-analysis of functional imaging studies. Psychol. Med. 2013;43:553–69. doi: 10.1017/S0033291712001432. doi:10.1017/S0033291712001432. [DOI] [PubMed] [Google Scholar]
- Frazier JA, Hodge SM, Breeze JL, Giuliano AJ, Terry JE, Moore CM, Kennedy DN, Lopez-Larson MP, Caviness VS, Seidman LJ, Zablotsky B, Makris N. Diagnostic and sex effects on limbic volumes in early-onset bipolar disorder and schizophrenia. Schizophr. Bull. 2008;34:37–46. doi: 10.1093/schbul/sbm120. doi:10.1093/schbul/sbm120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fusar-Poli P, Placentino A, Carletti F, Allen P, Landi P, Abbamonte M, Barale F, Perez J, McGuire P, Politi PL. Laterality effect on emotional faces processing: ALE meta-analysis of evidence. Neurosci. Lett. 2009;452:262–7. doi: 10.1016/j.neulet.2009.01.065. doi:10.1016/j.neulet.2009.01.065. [DOI] [PubMed] [Google Scholar]
- Jiang H, van Zijl PCM, Kim J, Pearlson GD, Mori S. DtiStudio: resource program for diffusion tensor computation and fiber bundle tracking. Comput. Methods Programs Biomed. 2006;81:106–16. doi: 10.1016/j.cmpb.2005.08.004. doi:10.1016/j.cmpb.2005.08.004. [DOI] [PubMed] [Google Scholar]
- Johnson SA, Wang J-F, Sun X, McEwen BS, Chattarji S, Young LT. Lithium treatment prevents stress-induced dendritic remodeling in the rodent amygdala. Neuroscience. 2009;163:34–9. doi: 10.1016/j.neuroscience.2009.06.005. doi:10.1016/j.neuroscience.2009.06.005. [DOI] [PubMed] [Google Scholar]
- Kelley R, Chang KD, Garrett A, Alegría D, Thompson P, Howe M, L Reiss A. Deformations of amygdala morphology in familial pediatric bipolar disorder. Bipolar Disord. 2013;15:795–802. doi: 10.1111/bdi.12114. doi:10.1111/bdi.12114. [DOI] [PubMed] [Google Scholar]
- Li H, Chan RCK, McAlonan GM, Gong Q. Facial emotion processing in schizophrenia: a meta-analysis of functional neuroimaging data. Schizophr. Bull. 2010;36:1029–39. doi: 10.1093/schbul/sbn190. doi:10.1093/schbul/sbn190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu H, Tang Y, Womer F, Fan G, Lu T, Driesen N, Ren L, Wang Y, He Y, Blumberg HP, Xu K, Wang F. Differentiating patterns of amygdala-frontal functional connectivity in schizophrenia and bipolar disorder. Schizophr. Bull. 2014;40:469–77. doi: 10.1093/schbul/sbt044. doi:10.1093/schbul/sbt044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mahon PB, Eldridge H, Crocker B, Notes L, Gindes H, Postell E, King S, Potash JB, Ratnanather JT, Barta PE. An MRI study of amygdala in schizophrenia and psychotic bipolar disorder. Schizophr. Res. 2012;138:188–91. doi: 10.1016/j.schres.2012.04.005. doi:10.1016/j.schres.2012.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mai J, Paxinos G, Voss T. Atlas of the Human Brain. 3rd ed. Academic Press; 2007. [Google Scholar]
- Mamah D, Wang L, Csernansky JG, Rice JP, Smith M, Barch DM. Morphometry of the hippocampus and amygdala in bipolar disorder and schizophrenia. Bipolar Disord. 2010;12:341–3. doi: 10.1111/j.1399-5618.2010.00802.x. doi:10.1111/j.1399-5618.2010.00802.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller M, Younes L, Ratnanather J, Brown T, Trinh H, Lee D, Tward D, Mahon P, Mori S, Albert M, The BIOCARD Research Team Amygdalar atrophy in symptomatic AD based on diffeomorphometry: The BIOCARD cohort. Neurobiol. 2014 doi: 10.1016/j.neurobiolaging.2014.06.032. Aging in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murphy FC, Nimmo-Smith I, Lawrence AD. Functional neuroanatomy of emotions: a meta-analysis. Cogn. Affect. Behav. Neurosci. 2003;3:207–33. doi: 10.3758/cabn.3.3.207. [DOI] [PubMed] [Google Scholar]
- Oishi K, Faria A, Jiang H, Li X, Akhter K, Zhang J, Hsu JT, Miller MI, van Zijl PCM, Albert M, Lyketsos CG, Woods R, Toga AW, Pike GB, Rosa-Neto P, Evans A, Mazziotta J, Mori S. Atlas-based whole brain white matter analysis using large deformation diffeomorphic metric mapping: application to normal elderly and Alzheimer's disease participants. Neuroimage. 2009;46:486–99. doi: 10.1016/j.neuroimage.2009.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Potash JB. Carving chaos: genetics and the classification of mood and psychotic syndromes. Harv. Rev. Psychiatry. 2006;14:47–63. doi: 10.1080/10673220600655780. doi:10.1080/10673220600655780. [DOI] [PubMed] [Google Scholar]
- Qiu A, Gan SC, Wang Y, Sim K. Amygdala-hippocampal shape and cortical thickness abnormalities in first-episode schizophrenia and mania. Psychol. Med. 2013;43:1353–63. doi: 10.1017/S0033291712002218. doi:10.1017/S0033291712002218. [DOI] [PubMed] [Google Scholar]
- Ratnanather JT, Poynton CB, Pisano DV, Crocker B, Postell E, Cebron S, Ceyhan E, Honeycutt NA, Mahon PB, Barta PE. Morphometry of superior temporal gyrus and planum temporale in schizophrenia and psychotic bipolar disorder. Schizophr. Res. 2013;150:476–83. doi: 10.1016/j.schres.2013.08.014. doi:10.1016/j.schres.2013.08.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ségonne F, Dale AM, Busa E, Glessner M, Salat D, Hahn HK, Fischl B. A hybrid approach to the skull stripping problem in MRI. Neuroimage. 2004;22:1060–75. doi: 10.1016/j.neuroimage.2004.03.032. doi:10.1016/j.neuroimage.2004.03.032. [DOI] [PubMed] [Google Scholar]
- Sergerie K, Chochol C, Armony JL. The role of the amygdala in emotional processing: a quantitative meta-analysis of functional neuroimaging studies. Neurosci. Biobehav. Rev. 2008;32:811–30. doi: 10.1016/j.neubiorev.2007.12.002. doi:10.1016/j.neubiorev.2007.12.002. [DOI] [PubMed] [Google Scholar]
- Strasser HC, Lilyestrom J, Ashby ER, Honeycutt NA, Schretlen DJ, Pulver AE, Hopkins RO, Depaulo JR, Potash JB, Schweizer B, Yates KO, Kurian E, Barta PE, Pearlson GD. Hippocampal and ventricular volumes in psychotic and nonpsychotic bipolar patients compared with schizophrenia patients and community control subjects: a pilot study. Biol. Psychiatry. 2005;57:633–9. doi: 10.1016/j.biopsych.2004.12.009. doi:10.1016/j.biopsych.2004.12.009. [DOI] [PubMed] [Google Scholar]
- Taylor SF, Kang J, Brege IS, Tso IF, Hosanagar A, Johnson TD. Meta-analysis of functional neuroimaging studies of emotion perception and experience in schizophrenia. Biol. Psychiatry. 2012;71:136–45. doi: 10.1016/j.biopsych.2011.09.007. doi:10.1016/j.biopsych.2011.09.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Varea E, Guirado R, Gilabert-Juan J, Martí U, Castillo-Gomez E, Blasco-Ibáñez JM, Crespo C, Nacher J. Expression of PSA-NCAM and synaptic proteins in the amygdala of psychiatric disorder patients. J. Psychiatr. Res. 2012;46:189–97. doi: 10.1016/j.jpsychires.2011.10.011. doi:10.1016/j.jpsychires.2011.10.011. [DOI] [PubMed] [Google Scholar]
- Velakoulis D, Wood SJ, Wong MTH, McGorry PD, Yung A, Phillips L, Smith D, Brewer W, Proffitt T, Desmond P, Pantelis C. Hippocampal and amygdala volumes according to psychosis stage and diagnosis: a magnetic resonance imaging study of chronic schizophrenia, first-episode psychosis, and ultra-high-risk individuals. Arch. Gen. Psychiatry. 2006;63:139–49. doi: 10.1001/archpsyc.63.2.139. doi:10.1001/archpsyc.63.2.139. [DOI] [PubMed] [Google Scholar]
- Wager TD, Phan KL, Liberzon I, Taylor SF. Valence, gender, and lateralization of functional brain anatomy in emotion: a meta-analysis of findings from neuroimaging. Neuroimage. 2003;19:513–31. doi: 10.1016/s1053-8119(03)00078-8. [DOI] [PubMed] [Google Scholar]
- Younes L, Ratnanather JT, Brown T, Aylward E, Nopoulos P, Johnson H, Magnotta VA, Paulsen JS, Margolis RL, Albin RL, Miller MI, Ross CA. Regionally selective atrophy of subcortical structures in prodromal HD as revealed by statistical shape analysis. Hum. Brain Mapp. 2014;35:792–809. doi: 10.1002/hbm.22214. doi:10.1002/hbm.22214. [DOI] [PMC free article] [PubMed] [Google Scholar]