Abstract
Background
Diabetic retinopathy is a common complication of diabetes and a leading cause of visual impairment and blindness. Research has established the importance of blood glucose control to prevent development and progression of the ocular complications of diabetes. Simultaneous blood pressure control has been advocated for the same purpose, but findings reported from individual studies have supported varying conclusions regarding the ocular benefit of interventions on blood pressure.
Objectives
The primary aim of this review was to summarize the existing evidence regarding the effect of interventions to control or reduce blood pressure levels among diabetics on incidence and progression of diabetic retinopathy, preservation of visual acuity, adverse events, quality of life, and costs. A secondary aim was to compare classes of anti-hypertensive medications with respect to the same outcomes.
Search methods
We searched a number of electronic databases including CENTRAL as well as ongoing trial registries. We last searched the electronic databases on 25 April 2014. We also reviewed reference lists of review articles and trial reports selected for inclusion. In addition, we contacted investigators of trials with potentially pertinent data.
Selection criteria
We included in this review randomized controlled trials (RCTs) in which either type 1 or type 2 diabetic participants, with or without hypertension, were assigned randomly to intense versus less intense blood pressure control, to blood pressure control versus usual care or no intervention on blood pressure, or to different classes of anti-hypertensive agents versus placebo.
Data collection and analysis
Pairs of review authors independently reviewed titles and abstracts from electronic and manual searches and the full text of any document that appeared to be relevant. We assessed included trials independently for risk of bias with respect to outcomes reported in this review. We extracted data regarding trial characteristics, incidence and progression of retinopathy, visual acuity, quality of life, and cost-effectiveness at annual intervals after study entry whenever provided in published reports and other documents available from included trials.
Main results
We included 15 RCTs, conducted primarily in North America and Europe, that had enrolled 4157 type 1 and 9512 type 2 diabetic participants, ranging from 16 to 2130 participants in individual trials. In 10 of the 15 RCTs, one group of participants was assigned to one or more anti-hypertensive agents and the control group received placebo. In three trials, intense blood pressure control was compared to less intense blood pressure control. In the remaining two trials, blood pressure control was compared with usual care. Five of the 15 trials enrolled type 1 diabetics, and 10 trials enrolled type 2 diabetics. Six trials were sponsored entirely by pharmaceutical companies, seven trials received partial support from pharmaceutical companies, and two studies received support from government-sponsored grants and institutional support.
Study designs, populations, interventions, and lengths of follow-up (range one to nine years) varied among the included trials. Overall, the quality of the evidence for individual outcomes was low to moderate. For the primary outcomes, incidence and progression of retinopathy, the quality of evidence was downgraded due to inconsistency and imprecision of estimates from individual studies and differing characteristics of participants.
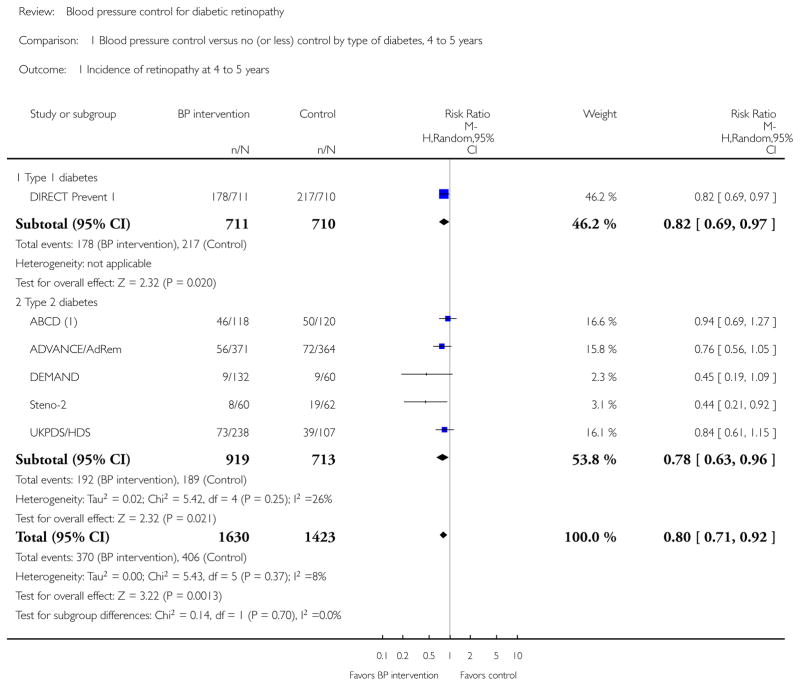
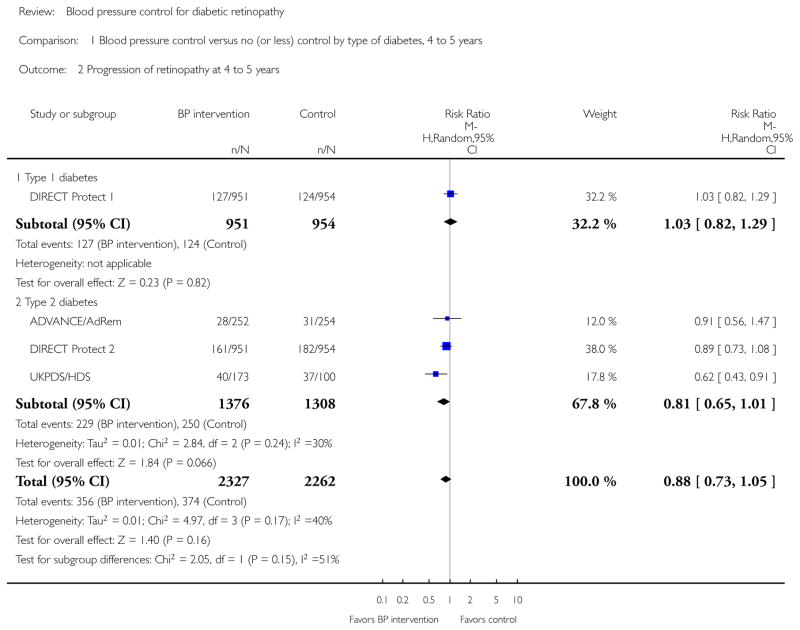
For primary outcomes among type 1 diabetics, one of the five trials reported incidence of retinopathy and one trial reported progression of retinopathy after 4 to 5 years of treatment and follow-up; four of the five trials reported a combined outcome of incidence and progression over the same time interval. Among type 2 diabetics, 5 of the 10 trials reported incidence of diabetic retinopathy and 3 trials reported progression of retinopathy; one of the 10 trials reported a combined outcome of incidence and progression during a 4-to 5-year follow-up period. One trial in which type 2 diabetics participated had reported no primary (or secondary) outcome targeted for this review.
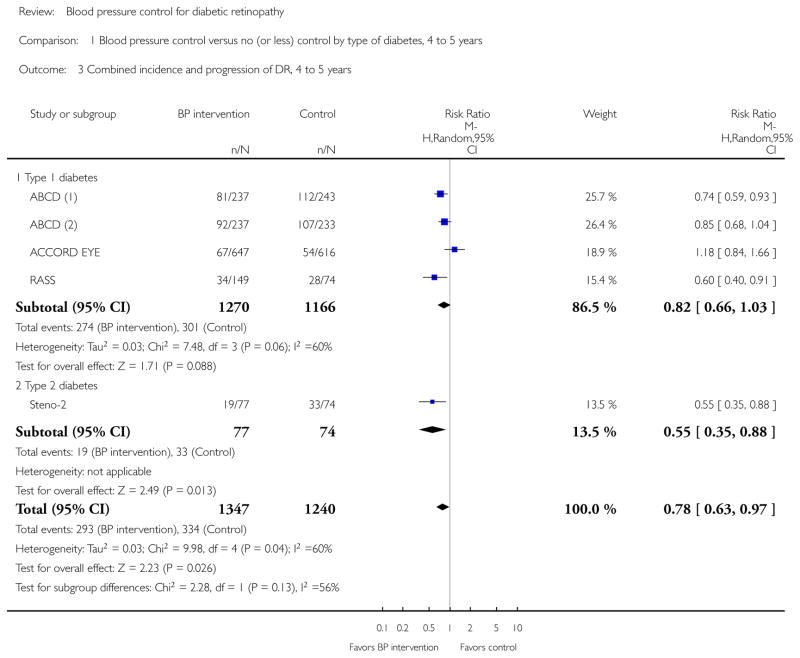
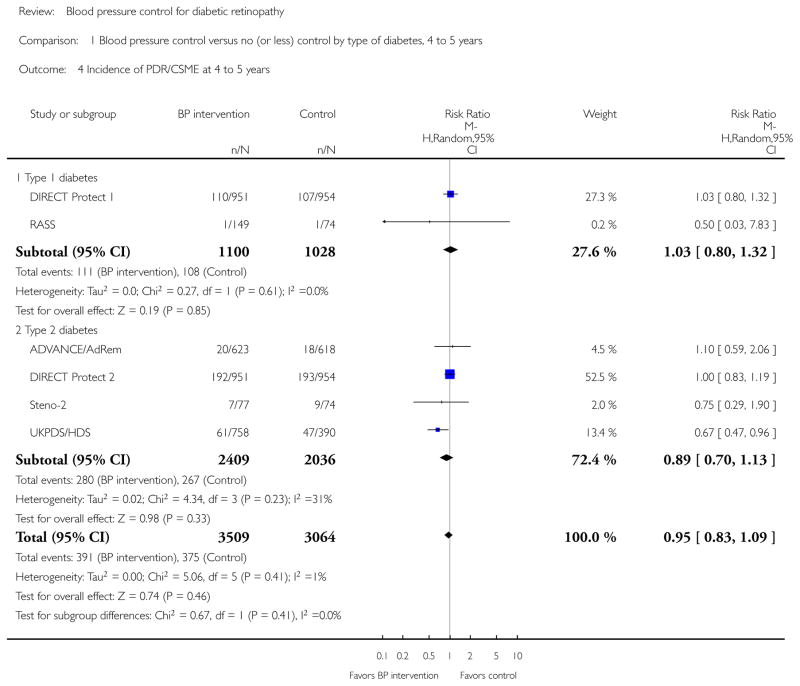
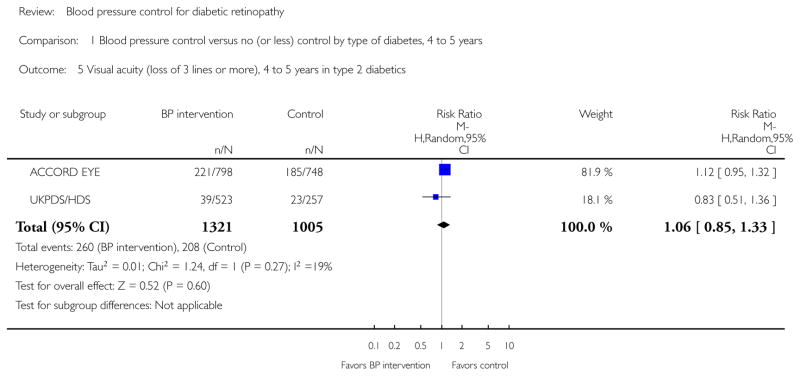
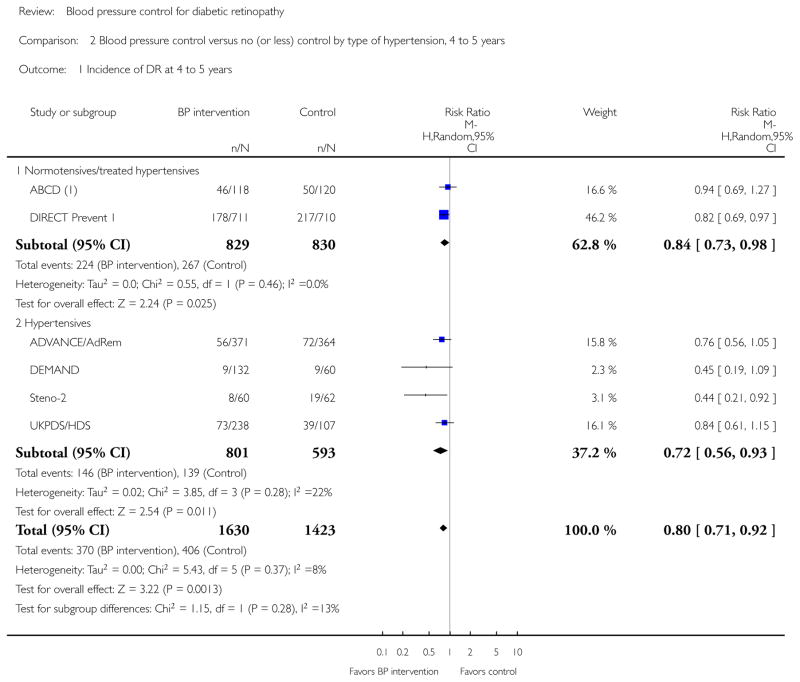
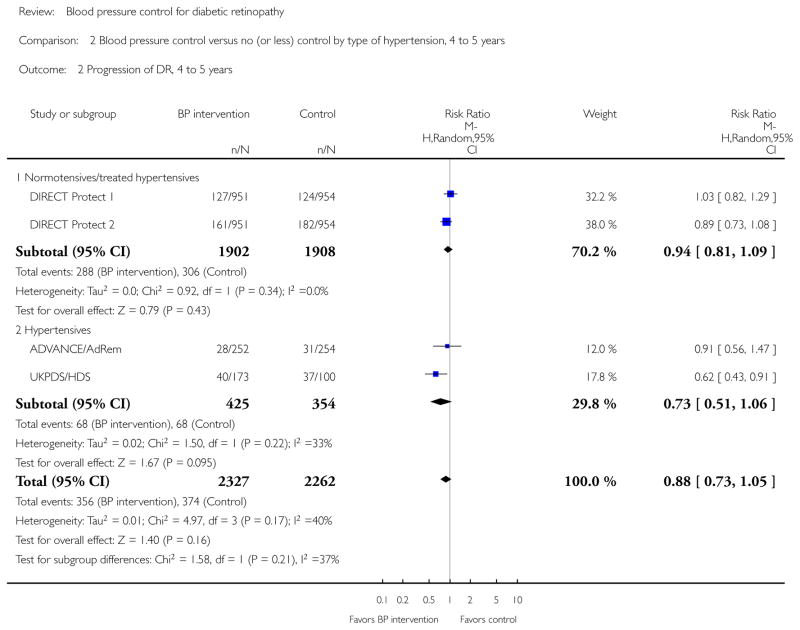
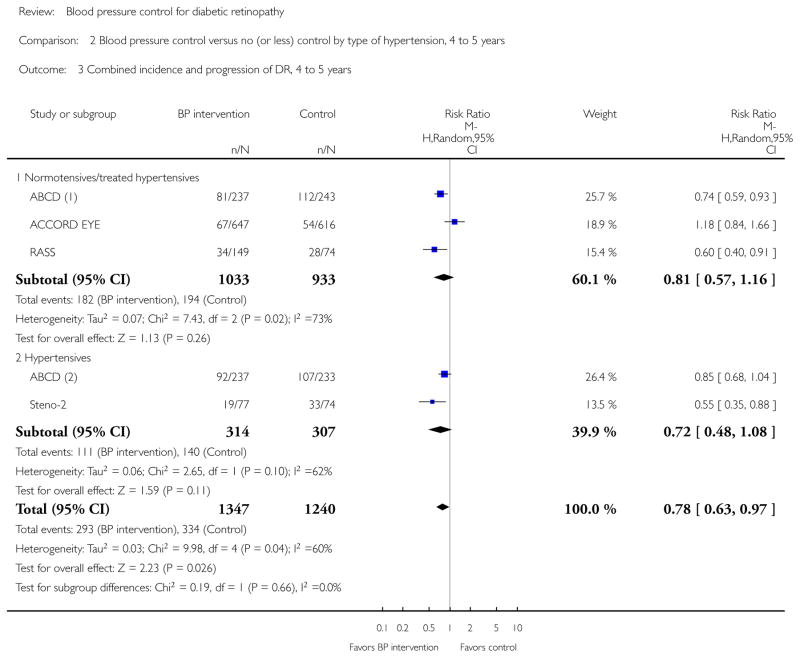
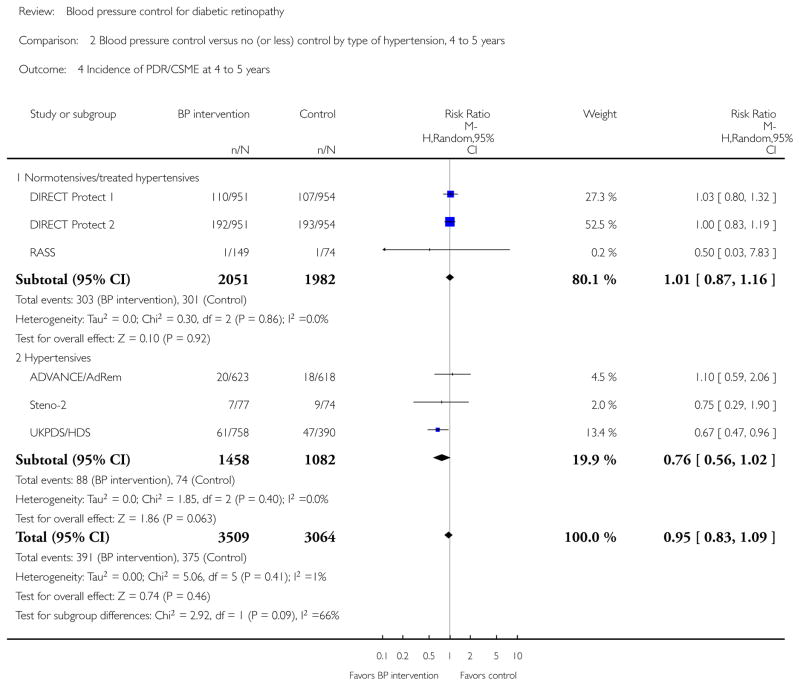
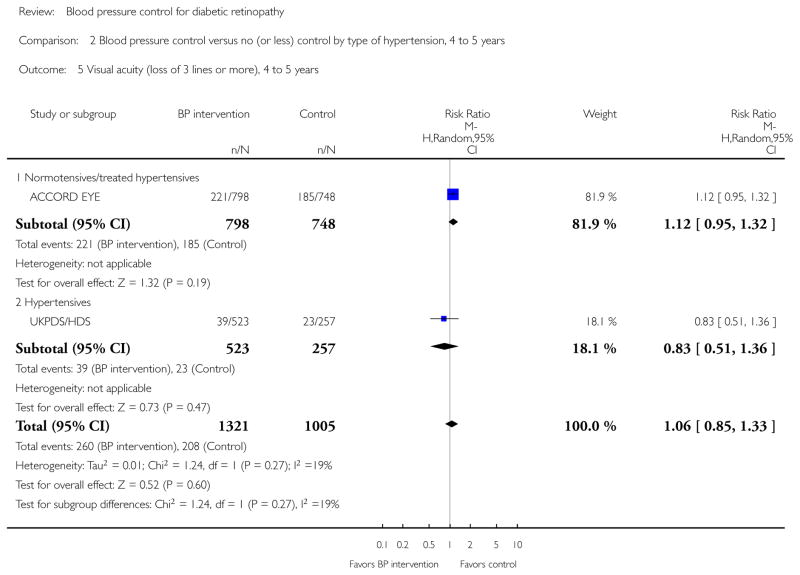
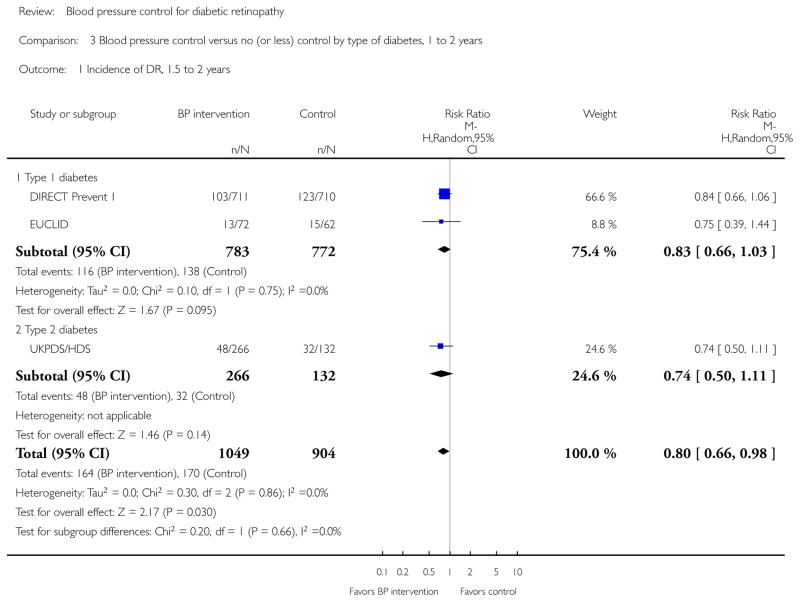
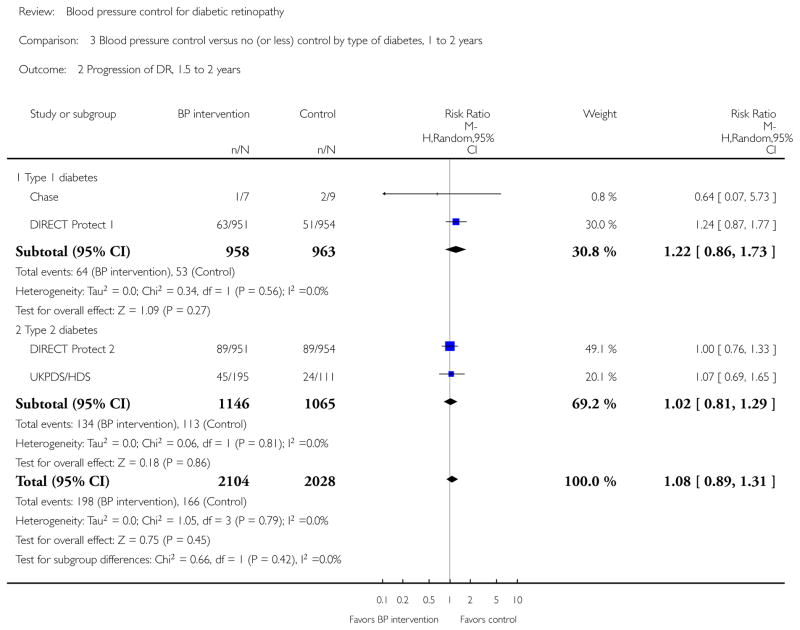
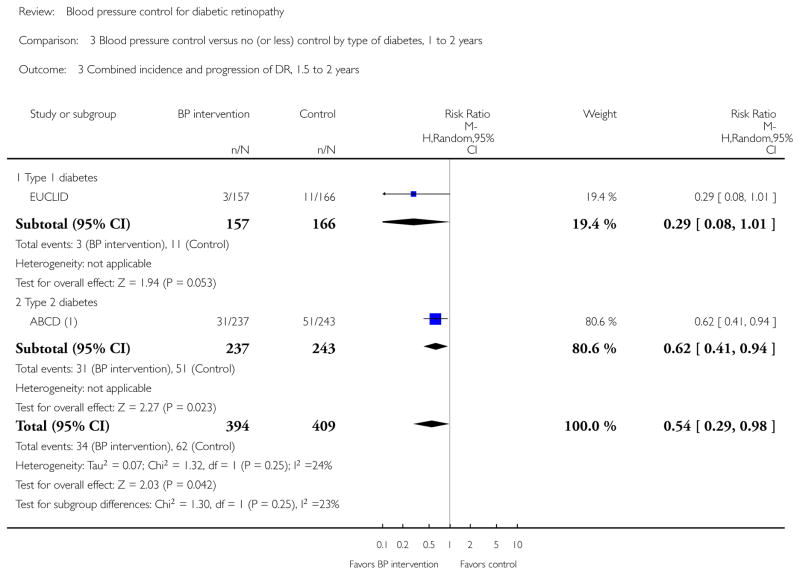
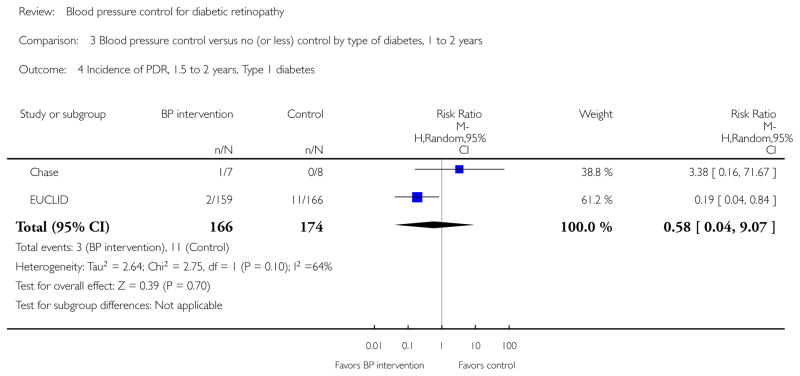
The evidence from these trials supported a benefit of more intensive blood pressure control intervention with respect to 4- to 5-year incidence of diabetic retinopathy (estimated risk ratio (RR) 0.80; 95% confidence interval (CI) 0.71 to 0.92) and the combined outcome of incidence and progression (estimated RR 0.78; 95% CI 0.63 to 0.97). The available evidence provided less support for a benefit with respect to 4- to 5-year progression of diabetic retinopathy (point estimate was closer to 1 than point estimates for incidence and combined incidence and progression, and the CI overlapped 1; estimated RR 0.88; 95% CI 0.73 to 1.05). The available evidence regarding progression to proliferative diabetic retinopathy or clinically significant macular edema or moderate to severe loss of best-corrected visual acuity did not support a benefit of intervention on blood pressure: estimated RRs and 95% CIs 0.95 (0.83 to 1.09) and 1.06 (0.85 to 1.33), respectively, after 4 to 5 years of follow-up. Findings within subgroups of trial participants (type 1 and type 2 diabetics; participants with normal blood pressure levels at baseline and those with elevated levels) were similar to overall findings.
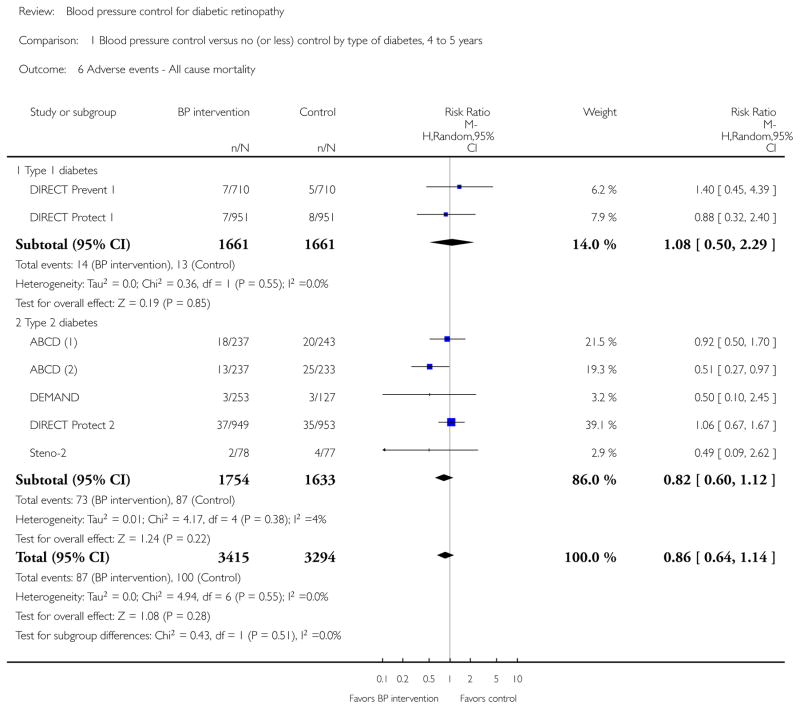
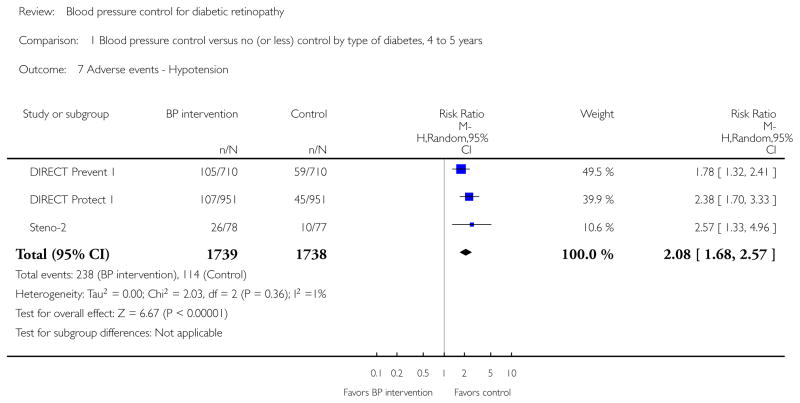
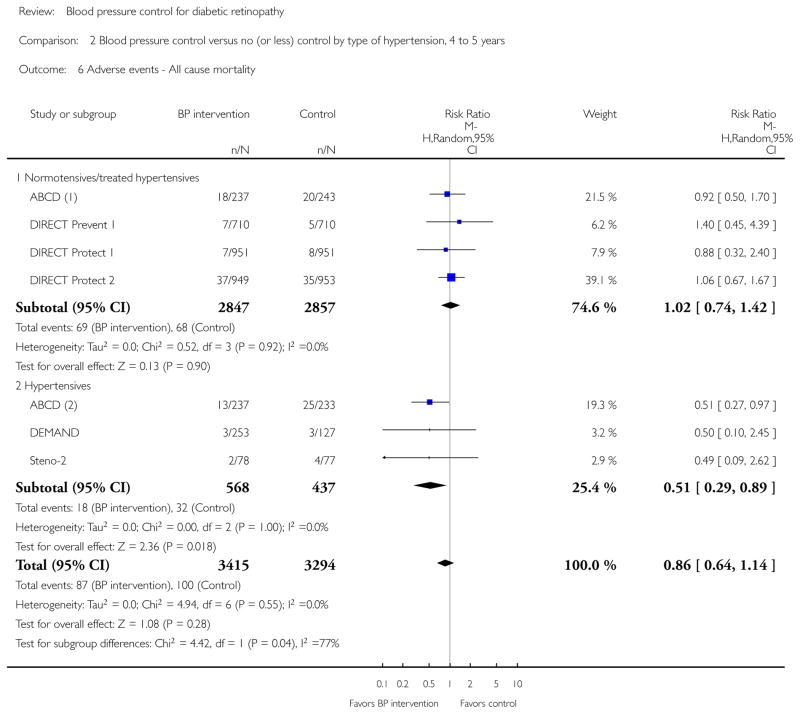
The adverse event reported most often (7 of 15 trials) was death, yielding an estimated RR 0.86 (95% CI 0.64 to 1.14). Hypotension was reported from three trials; the estimated RR was 2.08 (95% CI 1.68 to 2.57). Other adverse ocular events were reported from single trials.
Authors’ conclusions
Hypertension is a well-known risk factor for several chronic conditions in which lowering blood pressure has proven to be beneficial. The available evidence supports a beneficial effect of intervention to reduce blood pressure with respect to preventing diabetic retinopathy for up to 4 to 5 years. However, the lack of evidence to support such intervention to slow progression of diabetic retinopathy or to prevent other outcomes considered in this review, along with the relatively modest support for the beneficial effect on incidence, weakens the conclusion regarding an overall benefit of intervening on blood pressure solely to prevent diabetic retinopathy.
PLAIN LANGUAGE SUMMARY
Blood pressure control for diabetic retinopathy
Review question
We reviewed the evidence about the effect of blood pressure control to prevent diabetic retinopathy and/or to slow progression of diabetic retinopathy.
Background
Diabetes is characterized by high levels of blood glucose (sugar circulating in the blood) and is classified as either type 1 or type 2, depending on the underlying cause of increased blood glucose. A common complication in people with diabetes is diabetic retinopathy, often called ’diabetic eye disease,’ which affects the blood vessels in the back of the eye. Diabetic retinopathy is a major cause of poor vision and blindness worldwide among adults of working age. Research has shown that control of blood glucose reduces the risk of diabetic retinopathy and prevents worsening of the condition once it develops. However, the current diabetes epidemic suggests that the rates of new and worsening diabetic retinopathy will increase without effective means of prevention and treatment in addition to blood glucose control. Simultaneous treatment to reduce blood pressure among diabetics has been suggested as one approach.
Study characteristics
We found 15 randomized controlled trials, conducted primarily in North America and Europe, to investigate the effects of methods to lower blood pressure (drug-based in 14 trials; lifestyle change in 1 trial) in 4157 type 1 and 9512 type 2 diabetics, ranging from 16 to 2130 participants in individual trials. The follow-up period ranged from one to nine years for included trials. Of the 15 trials, six were funded in full by one or more drug companies. Seven more studies received drug company support, usually in the form of study medications. The remaining two studies were conducted with support from government-sponsored grants and institutional support. The evidence is current to April 2014.
Key results
Overall, the included trials provided modest support for lowering blood pressure to prevent diabetic retinopathy, regardless of diabetes type or baseline blood pressure level. However, the evidence did not indicate that lowering blood pressure kept diabetic retinopathy from worsening once it had developed or that it prevented advanced stages of diabetic retinopathy that required laser or other treatment of affected eyes. Treatment to reduce the blood pressure of people with diabetes is warranted for other health reasons, but the available evidence does not justify reduction of blood pressure solely to prevent or slow diabetic retinopathy.
Quality of the evidence
Overall, the quality of the evidence was low to moderate based on the reported information. The quality was downgraded mainly because some studies did not report outcomes for all or most participants at follow-up time points, and results from different studies were not highly consistent.
SUMMARY OF FINDINGS FOR THE MAIN COMPARISON [Explanation]
Table 10.
| Blood pressure intervention/intensive blood pressure intervention compared with placebo/standard intensive blood pressure intervention for diabetic retinopathy | ||||||
|---|---|---|---|---|---|---|
| Patient or population: type 1 or type 2 diabetics Settings: diabetes and ophthalmology clinics Intervention: blood pressure intervention/intensive blood pressure intervention (anti-hypertensive medication or intense anti-hypertensive medication, or intense lifestyle intervention and medication) Comparison: placebo/standard blood pressure intervention (anti-hypertensive medication) | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | No. of participants (trials) | Quality of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | |||||
| Placebo/standard blood pressure intervention | Blood pressure intervention/intensive blood pressure intervention | |||||
| Incidence of retinopathy at 4 to 5 years | 285 per 1000 | 228 per 1000 (202 to 262) | RR 0.80 (0.71 to 0.92) | 3053 (6 trials) | ⊕⊕⊕○ moderate1,3 |
- |
| Progression of retinopathy at 4 to 5 years | 185 per 1000 | 163 per 1000 (135 to 194) | RR 0.88 (0.73 to 1.05) | 4105 (4 trials) | ⊕⊕⊕○ moderate1,3 |
- |
| Combined incidence and progression of diabetic retinopathy, 4 to 5 years | 269 per 1000 | 210 per 1000 (169 to 261) | RR 0.78 (0.63 to 0.97) | 2587 (5 trials) | ⊕⊕○○ low1,2,3 |
- |
| Incidence of PDR/CSME at 4 to 5 years | 133 per 1000 | 126 per 1000 (110 to 144) | RR 0.95 (0.83 to 1.08) | 6089 (6 trials) | ⊕⊕⊕○ moderate1,3 |
- |
| Visual acuity at 4 to 5 years | 207 per 1000 | 219 per 1000 (176 to 275) | RR 1.06 (0.85 to 1.33) | 2326 (2 trials) | ⊕⊕⊕○ moderate2,3 |
- |
| Adverse events - All-cause mortality | 30 per 1000 | 26 per 1000 (19 to 34) | RR 0.86 (0.64 to 1.14) | 6709 (7 trials) | ⊕⊕⊕○ moderate1,3 |
- |
| Adverse events - Hypotension | 66 per 1000 | 137 per 1000 (111 to 170) | RR 2.08 (1.68 to 2.57) | 3477 (3 trials) | ⊕⊕⊕○ moderate1,3 |
- |
The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI).
CI: confidence interval; CSME: clinically significant macular edema; RR: risk ratio; PDR: proliferative diabetic retinopathy
| GRADE (Grades of Recommendation, Assessment, Development, and Evaluation) Working Group grades of evidence High quality: Further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: We are very uncertain about the estimate. |
Downgraded for risk of bias (−1) because of considerable numbers of participants lost to follow-up in some trials.
Downgraded for inconsistency (−1) I2 > 50%.
The studies had different comparisons including intensive blood pressure control versus moderate blood pressure control for hypertensives and blood pressure control intervention versus placebo for normotensives.
BACKGROUND
Description of the condition
Introduction and epidemiology
Diabetic retinopathy is a complex disorder of the retinal vasculature that is characterized by increased vascular permeability, retinal ischemia and edema, and new blood vessel formation. The National Eye Institute reports age-related macular degeneration, cataracts, glaucoma, and diabetic retinopathy to be the leading causes of visual impairment and blindness among Americans older than 40 years (EDPRG 2004a). Similar findings have been reported for older Americans over the age of 75 years (Desai 2001) and from other epidemiologic studies from Western Europe (Buch 2004; Grey 1989; Krumpaszky 1999; Rosenberg 1996).
Globally, diabetes mellitus is a significant public health problem. Some estimates predict that the worldwide prevalence of diabetes will exceed 366 million people by 2030 (Wild 2004). Diabetic retinopathy is a common complication among individuals with diabetes and an important cause of loss of vision (Sivaprasad 2012). A diabetic individual has a three-fold increased risk of blindness compared with the general population (Hayward 2002). The US Centers for Disease Control and Prevention estimates that 25.8 million people in the US were living with diabetes in 2010 (CDC 2011). In the US alone, it is estimated that 4.1 million adults over the age of 40 have diabetic retinopathy (any level of severity) and that 899,000 adults have vision-threatening diabetic retinopathy (EDPRG 2004b). Among Americans with type 1 diabetes, the prevalence of diabetic retinopathy of any severity is 74.9% and 82.3% in black and white persons respectively; the prevalence of vision-threatening (severe non-proliferative and proliferative) retinopathy is 30% and 32.2% (EDPRG 2004c). The prevalence of diabetic retinopathy among type 1 and type 2 diabetics in Wales recently was reported to be 56% and 30.3%, respectively (Thomas 2014). People with impaired visual acuity or legal blindness secondary to diabetic retinopathy face enormous challenges in pursuing activities of daily life. Visual impairment is defined as best-corrected visual acuity worse than 20/40 in the better-seeing eye; blindness is defined as best-corrected visual acuity of 20/200 or worse in the better-seeing eye as measured on the original Bailey-Lovie or modified Bailey-Lovie (also known as the Early Treatment Diabetic Retinopathy Study (ETDRS)) visual acuity chart or other charts that use a logMAR scale.
The duration of diabetes and the severity of hyperglycemia are major risk factors associated with the development (incidence) and progression of diabetic retinopathy (DCCT 1993; DRS10 1985; ETDRS18 1998; Harris 1998; Klein 1984a; Klein 1984b; Klein 1988; Krakoff 2003; Kullberg 2002; Leske 2003; Porta 2001; UKPDS33 1998; van Leiden 2003; Zhang 2001). After retinopathy develops, persistent hyperglycemia has been reported to be a more important factor than duration of diabetes for progression of the disease (ETDRS18 1998; Giuffre 2004).
The Diabetes Control and Complications Trial (DCCT) and the United Kingdom Prospective Diabetes Study (UKPDS) demonstrated lower incidence and slower progression of diabetic retinopathy with tight blood glucose control (DCCT 1993; UKPDS33 1998). The Diabetic Retinopathy Study (DRS2 1978; DRS5 1981; DRS8 1981) and the ETDRS (ETDRS1 1985; ETDRS9 1991) demonstrated a decrease in the progression of proliferative diabetic retinopathy and diabetic macular edema with more than 1200 applications of ’pan-retinal’ (for proliferative retinopathy) or with ’focal’ (for macular edema) laser photocoagulation. However, the prevalence of diabetic retinopathy observed in recent epidemiologic studies (EDPRG 2004b; EDPRG 2004c) conducted after the DCCT and UKPDS continued to be high. Recently, investigators participating in trials conducted by the Diabetic Retinopathy Clinical Research Network (DRCRnet) have reported that other treatments, either alone or combined with laser treatment, can slow progression of diabetic retinopathy (DRCR.net 2010). These studies strongly support treatment of diabetic retinopathy to reduce loss of vision. Nevertheless, findings from all studies reinforce the need to evaluate the role of other risk factors and to intervene on those that are modifiable in order to decrease the prevalence of diabetic retinopathy.
Risk factors for diabetic retinopathy include hypertension (Klein 1989a; Klein 1989b; Leske 2003; Tapp 2003; UKPDS38 1998), hypercholesterolemia (Chew 1996; Klein 2002b; van Leiden 2002), abdominal obesity and elevated body mass index (van Leiden 2002; van Leiden 2003; Zhang 2001), alcohol intake (Giuffre 2004), younger age at onset (Krakoff 2003; Kullberg 2002; Porta 2001), smoking, and ancestry (Keen 2001; Moss 1996). Age and ancestry are not modifiable, but other risk factors suggest possible interventions.
Presentation and diagnosis
Diabetic retinopathy progresses sequentially from a mild non-proliferative stage to a severe proliferative disorder. Increased retinal vascular permeability occurs early, at the stage of mild non-proliferative diabetic retinopathy (NPDR). Moderate and severe NPDR are characterized by vascular closure, which results in impaired retinal perfusion (ischemia).
Diabetic retinopathy typically is diagnosed during ophthalmoscopy. Fundus photographs and fluorescein angiograms may be used to monitor progression. Signs of NPDR include microaneurysms, intraretinal hemorrhages, and occasional ’cotton wool spots’ caused by closure of small retinal arterioles, resulting in localized ischemia and edema, with consequent damage to nerve fibers leading to reduced axonal transport. Signs of increasing ischemia include extensive intraretinal hemorrhages, venous abnormalities such as wide variations in caliber (’beading’) and looping (’reduplication’), capillary non-perfusion, and intraretinal microvascular abnormalities. Severe NPDR, also known as pre-proliferative retinopathy, is diagnosed when these changes progress to pre-defined thresholds.
Proliferative diabetic retinopathy (PDR) is characterized by neo-vascularization, which is the growth of abnormal blood vessels in response to severe ischemia. The new vessels grow into the vitreous and often are seen at the optic disc (NVD) and elsewhere in the retina (NVE); they are prone to bleeding, which results in vitreous hemorrhage and vision loss. Furthermore, these vessels may undergo fibrosis and contraction and, along with other fibrous proliferation, may lead to epiretinal membrane formation, vitreoretinal traction bands, retinal tears, and either tractional or rhegmatogenous retinal detachments (that is, those due to a retinal hole or tear). It is said that proliferative diabetic retinopathy is at the high-risk stage when NVE that occupy a total area of 0.5 optic disc area or more in size throughout the retina are accompanied by pre-retinal or vitreous hemorrhage, or when NVD occupy an area greater than or equal to about one-third disc area, even in the absence of vitreous hemorrhage, or when NVD of any size are accompanied by vitreous hemorrhage. People in the ’high risk’ stage of PDR who do not receive prompt pan-retinal laser treatment have a 30% to 50% probability of progressing to severe visual acuity loss and blindness (less than 5/200 best-corrected visual acuity) in three years (DRS8 1981; ETDRS10 1991; ETDRS12 1991). Increased retinal vascular permeability, which can occur at any stage of diabetic retinopathy, may result in retinal thickening (edema) and lipid deposits (hard exudates). Retinal thickening, hard exudates, or both that occur at or within 500 microns (approximately one-third an optic disc diameter) of the center of the macula, and which therefore threaten, or actually cause, loss of central visual acuity, are referred to as clinically significant macular edema.
The major reasons for vision loss in diabetic retinopathy include macular edema, macular capillary non-perfusion (which can be demonstrated by fluorescein angiography), vitreous hemorrhage, distortion or tractional detachment of the retina (PPP 2012), and neovascular glaucoma (new blood vessels in the iris), which usually is associated with very late-stage PDR (Fong 2004).
Pathogenesis
Several biochemical pathways have been investigated for the pathogenesis of diabetic retinopathy. Apart from the well-documented role of chronic hyperglycemia, none of the other biochemical pathways has been shown conclusively to be relevant (Frank 2004). Although the exact mechanism for the pathogenesis of hypertensive damage in eyes with diabetic retinopathy is unknown, scientists have hypothesized that an increase in blood pressure damages the retinal capillary endothelial cells (Klein 2002a). In eyes with diabetic retinopathy, chronic hyperglycemia leads to endothelial cell damage, pericyte loss, and breakdown of the blood-retinal barrier. Such changes to the structure of the microvasculature lead to dysregulation of retinal perfusion, thereby making eyes with diabetic retinopathy more susceptible to hyperperfusion damage from hypertension (Gillow 1999).
Description of the intervention
The current standard of care for the prevention and treatment of diabetic retinopathy consists of strict glycemic control and regular ophthalmologic screening for diabetic retinopathy among diabetics, the use of focal laser treatment or intravitreal anti-vascular endothelial growth factor injections for diabetic macular edema, and the use of pan-retinal scatter laser photocoagulation for proliferative diabetic retinopathy (Smith 2011; Virgili 2014). Strict blood pressure control has been recommended as part of the standard of care for diabetics, primarily because of its known beneficial effect on the prevention of cardiovascular events, stroke, and nephropathy, rather than for its effect on diabetic retinopathy (Hansson 1998; HOPESI 2000).
How the intervention might work
Blood pressure control may be beneficial in preventing the development or slowing the progression of diabetic retinopathy by reducing the damage to endothelial cells, blood vessels, and surrounding tissues from hyperperfusion. Diabetic retinopathy leads to endothelial cell dysfunction, loss of pericytes, and breakdown of the blood-retinal barrier. Hypertension may cause additional vascular damage because of shearing that occurs with hyperperfusion. Blood pressure control may prevent hyperperfusion and decrease the likelihood of shearing damage to the blood vessels from hypertension.
Why it is important to do this review
Diabetic retinopathy remains an important cause of vision loss even with good blood glucose control (ADA 1998; Ferris 1993). At the end of the DCCT, with participant follow-up of 6.5 ± 1.6 years (mean ± standard error), 10% of type 1 diabetic patients in the intensive glycemic control group had developed diabetic retinopathy despite strict glycemic control (Zhang 2001). Similarly, in the UKPDS, tight blood glucose control decreased but did not eliminate the risk of diabetic retinopathy (UKPDS33 1998). Diabetic retinopathy is a substantial public health problem (Zhang 2010). Because studies of retinal physiology suggest a role for blood pressure in pathological changes in diabetic retinopathy (Sjølie 2011), a systematic review of the effectiveness of blood pressure control with respect to diabetic retinopathy is warranted (Sleilati 2009).
OBJECTIVES
The primary aim of this review was to summarize the existing evidence regarding the effect of interventions to control or reduce blood pressure levels among diabetics on incidence and progression of diabetic retinopathy, preservation of visual acuity, adverse events, quality of life, and costs. A secondary aim was to compare classes of anti-hypertensive medications with respect to the same outcomes.
METHODS
Criteria for considering studies for this review
Types of studies
We included only randomized controlled trials (RCTs).
Types of participants
We included RCTs in which participants had a diagnosis of either type 1 or type 2 diabetes, irrespective of age, gender, ethnicity, ancestry, status regarding blood pressure or its treatment, or diabetic retinopathy status.
Types of interventions
We included trials in which:
Participants assigned to strict blood pressure control, alone or in combination with other interventions, were compared with participants assigned to less strict blood pressure control;
Participants assigned to blood pressure control were compared with participants assigned to no intervention (placebo);
Participants assigned to treatment with one class of anti-hypertensive agents were compared with participants assigned to another class of anti-hypertensive agents.
Types of outcome measures
Primary outcomes
Incidence of retinopathy, defined as mild non-proliferative or more severe diabetic retinopathy, that is score on the Early Treatment Diabetic Retinopathy Study (ETDRS) final scale of 35 or greater, based on evaluation of stereoscopic color fundus photographs of eyes of participants who did not have retinopathy at baseline (ETDRS10 1991).
Progression of retinopathy, defined as a two-step or greater progression from baseline on the ETDRS final scale based on evaluation of stereoscopic color fundus photographs of eyes of participants who had diabetic retinopathy at baseline (ETDRS10 1991).
Post hoc, we added a composite outcome of incidence or progression of retinopathy as reported by several included studies. For trials that used scales other than the ETDRS to define retinopathy and its progression, we assessed comparability of the scale with the ETDRS scale.
Although 5 years was specified as the primary outcome time of interest in the protocol for this review, few trials reported outcomes for this interval. We thus analyzed the primary outcomes reported for 4 to 5 years after enrollment. We also analyzed the primary outcomes at 1.5 to 2 years reported from a few trials.
Secondary outcomes
We assessed the secondary outcomes at follow-up times as reported above.
Decrease in visual acuity by three or more lines in both eyes on a logMAR chart. A three-line decrease corresponds to a doubling of the minimum angle of resolution.
Post hoc: incidence of proliferative diabetic retinopathy (PDR) or clinically significant macular edema (CSME) using criteria described in the included trials.
Adverse effects
We summarized adverse effects related to blood pressure control as reported from the included studies, with particular attention to death, hypotension, and adverse ocular events. We did not conduct an additional search for adverse events reported in RCTs that did not report retinopathy outcomes or in non-randomized studies (not included in this review).
Quality of life
We summarized vision-related quality-of-life data as reported from the included studies, for example, scores from the National Eye Institute Visual Functioning Questionnaire 25 (Mangione 2001) or another vision-related scale, when available. For future updates of the review, when sufficient data are available, we expect to compare the differences in scores between treatment groups using either means and standard errors when scores follow a normal or nearly normal distribution or using non-parametric methods when scores are not normally distributed.
Economic data
We summarized any cost or cost-effectiveness data reported from the included trials. For future updates of the review, when sufficient data are available, we expect to compare the cost differences between treatment strategies that yield similar benefits with respect to retinopathy outcomes.
Follow-up
We placed no restrictions on study selection based on the length of follow-up of participants for primary or secondary outcomes. However, we judged follow-up for less than one year to be inadequate for the outcomes relevant to this review because of the rate of development and progression of diabetic retinopathy and the time required for anti-hypertensive agents to affect the microvasculature. Five years was specified a priori as the primary outcome time for analyses.
Search methods for identification of studies
Electronic searches
We searched CENTRAL (which contains the Cochrane Eyes and Vision Group Trials Register) (2014, Issue 4), Ovid MEDLINE, Ovid MEDLINE In-Process and Other Non-Indexed Citations, Ovid MEDLINE Daily, Ovid OLDMEDLINE (January 1946 to April 2014), EMBASE (January 1980 to April 2014), Latin American and Caribbean Health Sciences Literature Database (LILACS) (January 1982 to April 2014), the metaRegister of Controlled Trials (mRCT) (www.controlled-trials.com), ClinicalTri-als.gov (www.clinicaltrials.gov) and the World Health Organization (WHO) International Clinical Trials Registry Platform (IC-TRP) (www.who.int/ictrp/search/en). We did not use any date or language restrictions in the electronic searches for trials. We last searched the electronic databases on 25 April 2014.
See: Appendices for details of search strategies for CENTRAL (Appendix 1), MEDLINE (Appendix 2), EMBASE (Appendix 3), LILACS (Appendix 4), mRCT (Appendix 5), ClinicalTrials.gov (Appendix 6), and the ICTRP (Appendix 7).
Searching other resources
We searched reference lists of reports from included trials and related reviews to find additional potentially eligible studies. We did not conduct manual searches of conference abstracts for this review.
Data collection and analysis
Selection of studies
Pairs of review authors independently assessed titles and abstracts of all records identified by the electronic and manual searches. We classified each record as ’definitely relevant,’ ’possibly relevant,’ or ’definitely not relevant.’ We obtained full-text reports corresponding to records classified as ’definitely relevant’ or ’possibly relevant’ by at least one review author. Two review authors independently classified studies described in full-text reports as ’include,’ ’exclude,’ ’uncertain,’ or ’ongoing.’ We resolved disagreements through discussion. For reports classified as ’uncertain’ or ’ongoing,’ that is those with unclear or insufficient information in reports, we contacted trial investigators for additional information or clarification. We documented studies labeled as ’exclude’ and the reasons for exclusion in the Characteristics of excluded studies table. We documented studies labeled as ’ongoing’ in the Characteristics of ongoing studies table. We documented studies with insufficient publicly available information in the Characteristics of studies awaiting classification table. For reports in languages not read by the review authors, we consulted with translators to assist with screening for eligibility; no full-text translations were required.
Table 7.
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Araki 2012 | No data on diabetic retinopathy were available; RCT of 1173 participants with type 2 diabetes randomized to intensive or conservative treatment |
| Auyanet 2010 | Not an RCT; case-control study to evaluate whether people with diabetic retinopathy who had or had not received photocoagulation had been treated with carvedilol |
| CALM-II | No data on diabetic retinopathy were available; the investigator’s response to our query indicated that retinopathy data from this trial had not been analyzed; RCT of 75 participants with type 1 or type 2 diabetes randomized to lisinopril alone or dual-blockade treatment with candesartan and lisinopril |
| Chang 2011 | Not an RCT; commentary on an included trial, no new trial data |
| DCCT | Not an RCT of blood pressure control; RCT of 1441 participants with insulin-dependent diabetes randomized to intensive or conservative glycemic control treatment |
| Durruty 2000 | No data on diabetic retinopathy were available; we did not receive a response to multiple requests for information regarding outcomes on diabetic retinopathy; RCT of 57 participants with type 2 diabetes and normal blood pressure randomized to enalapril or placebo |
| Faguer de Moustier 1989 | No data on diabetic retinopathy were available; RCT of 20 participants with type 2 diabetes and slight hypertension randomized to nicardipine or placebo |
| Harrold 1969 | Not an RCT of blood pressure control; RCT of 56 participants with diabetic retinopathy randomized to clofibrate (a lipid-lowering agent) or placebo |
| Jackson 1992 | Not an RCT; retrospective cohort study evaluating people with diabetic retinopathy and use of angiotensin- converting enzyme (ACE) inhibitors |
| JDCS 2011 | Not an RCT of blood pressure control; RCT of 2205 participants with type 2 diabetes randomized to intensive lifestyle intervention or conventional diabetes treatment; data on diabetic retinopathy outcomes were reported for the entire RCT cohort and not by treatment group |
| Larsen 1990 | No data on diabetic retinopathy were available; RCT of 20 participants with insulin-dependent diabetes and normal blood pressure randomized to captopril or control |
| Lehsten 1996 | Not an RCT; case-control study to compare prevalence of hypertension in people with or without diabetic retinopathy |
| Malik 1998 | No data on diabetic retinopathy were available; we did not receive a response to our request for information regarding outcomes for diabetic retinopathy; RCT of 41 participants with type 1 or type 2 diabetes and normal blood pressure randomized to trandolapril or placebo |
| MCSG 1995 | Not an RCT of blood pressure control; RCT of 70 participants with insulin-dependent diabetes randomized to intensive or conventional diabetes treatment |
| Mehlsen 2011 | No data on diabetic retinopathy were available; cross-over RCT of 25 participants with type 1 diabetes, mild retinopathy, and normal blood pressure randomized to amlodipine followed by lisinopril, or vice versa |
| Newsom 1991 | No data on diabetic retinopathy were available; RCT of 8 participants with insulin-dependent diabetes and normal blood pressure randomized to propanolol, dilevalol, salbutamol, or placebo |
| Patel 1998 | No data on diabetic retinopathy were available; RCT of 45 participants with type 1 or type 2 diabetes and hypertension randomized to perindopril or atenolol |
| Porush 2000 | Not an RCT; narrative review of multiple RCTs of blood pressure control in diabetic participants with or without diabetic retinopathy; most of the RCTs discussed focused on renal and cardiovascular outcomes and were not included in this review |
| Rachmani 2000 | No data on diabetic retinopathy were available; RCT of 250 participants with type 2 diabetes and normal blood pressure randomized to enalapril or placebo |
| Rachmani 2002 | Not an RCT of blood pressure control; RCT of 165 participants with type 2 diabetes and hypertension randomized to a patient participation program or standard annual consultation |
| Rassam 1997 | No data on diabetic retinopathy were available; RCT of 42 participants with mild diabetic retinopathy and normal blood pressure randomized to perindopril or placebo |
| Schwartz 1998 | No data on diabetic retinopathy were available; RCT of 1715 participants with type 2 diabetes and hypertension randomized to irbesartan or amlodipine |
| Wang 2012 | No data on diabetic retinopathy were available; RCT of 317 participants with type 2 diabetes randomized to captopril or placebo |
RCT: randomized controlled trial
Table 9.
Characteristics of ongoing studies [ordered by study ID]
| AdDIT | |
| Trial name or title | Adolescent type 1 Diabetes cardio-renal Intervention Trial (AdDIT) |
| Methods |
Study design: Multicenter RCT; 2×2 factorial design; randomization with minimization with primary intent-to-treat analysis and secondary ‘as treated’ analysis Unit of randomization and analysis: individual Number randomized - Total: not reported Per group: not reported Sample size calculation: Yes; “This sample size is informed by the ORPS cohort study (477 participants in the correct age range of recruitment with a mean of 3.5 observations over time)” |
| Participants |
Country: United Kingdom, Australia, and Canada Study period: not reported Age: not reported Gender: not reported Race/ethnicity: not reported Inclusion criteria: type 1 diabetics 11 to 16 years of age with albumin/creatinine ratio measured twice from average of 3 early-morning samples; adjusted for gender, age, and duration of diabetes; eligible whenever “subject’s residual lies above log 1.2” (i.e. higher side); < 1 year since diagnosis or C-peptide negative Exclusion criteria: “the presence of any of the following will prevent patient inclusion: 1) Non T1D, i.e. type 2 diabetes, insulin dependent diabetes related to monogenic disease, secondary diabetes; 2) ACR based on six early morning urines deemed to be at low risk for subsequent development of CVD or DN; 3) Pregnancy or unwillingness to comply with contraceptive advice and regular testing throughout trial; 4) Breast feeding; 5) Severe hyperlipidaemia and family history data to support diagnosis of familial hypercholesterolaemia; 6) Established hypertension unrelated to DN; 7) Prior exposure to the investigational products; 8) Unwillingness/inability to comply with the study protocol; 9) Other co-morbidities considered unsuitable by the investigator (excluding treated hypothyroidism and celiac disease); 10) Proliferative retinopathy.” Type of diabetes: type 1 HbA1c categories/levels: not reported Retinopathy status: not reported |
| Interventions |
Intervention 1: ACE inhibitor Intervention 2: statin Intervention 3: combination of ACE inhibitor and statin Intervention 4: placebo Length of follow-up: Planned: 5 to 10 years Actual: not reported |
| Outcomes |
Primary study outcome: reduction in albumin/creatinine ratio (30% assumed; 25% advantage) using the area under the curve of the log albumin/creatinine ratio standardized for gender, age, and duration of diabetes Secondary study outcomes: changes in 1) carotid intima-media thickness, fibromuscular dysplasia, endothelial dysfunction, and pulse wave velocity; 2) arterial blood pressure, lipids, and other lipoproteins, cardiovascular disease risk markers (high-sensitivity C-reactive protein and asymmetric dimethylarginine); 3) measure of glomerular filtration rate (plasma symmetric dimethyl arginine, creatinine, and cystatin C); 4) retinopathy scores and retinal microvascular structure; 5) quality of life and health economics Intervals at which outcomes were assessed: every 3 months Eyes examined for outcome: not reported Cost of interventions: not reported Quality of life: not reported |
| Starting date | Registered in 2007 and publication expected in 2009 |
| Contact information | The Adolescent type 1 Diabetes cardio-renal Intervention Trial Research Group (dbd25@cam.ac.uk) |
| Notes |
Source of funding: Juvenile Diabetes Research Foundation, British Heart Foundation, and Diabetes UK. Study drugs are supplied by Pfizer UK Ltd. The study is also funded in Canada by the Canadian Diabetes Association and the Heart and Stroke Foundation of Canada Declaration of interest: “The author declares that they have no competing interests” Target sample size: 500 For retinopathy, expect > 90% power to detect 25% difference in “retinopathy prevalence” using retinal photographs EudraCT number: 2007-001039-72 Trial Registration Number: ISRCTN91419926 |
| NCT00134160 | |
| Trial name or title | The Study Comparing the Incidence of Cardiovascular Events Between High-Dose ARB Monotherapy and Combination Therapy With ARB and Calcium Channel Blocker in Japanese Elderly Hypertensive Patients at High Cardiovascular Risk |
| Methods |
Study design: Parallel group RCT Unit of randomization and analysis: individual Number randomized - Total: not reported Per group: not reported Sample size calculation: not reported |
| Participants |
Country: Japan Study period: not reported Age: not reported Gender: not reported Race/ethnicity: not reported Inclusion criteria: individuals aged 65 to 85 years on anti-hypertensive therapy (SBP ≥ 140 mmHg or DBP ≥ 90 mmHg) with either type 2 diabetes, cardiovascular risk factors, elevated serum creatinine, or proteinuria Exclusion criteria: “Secondary hypertension or malignant hypertension; Heart failure (NYHA functional classification III or IV); Required treatment for malignant tumor; Serious liver or renal dysfunction (serum creatinine > 2.5 mg/dL or with dialysis treatment); Not appropriate for change to the test drugs from current therapy for hypertension or coronary diseases (i.e. calcium channel blockers, β-blockers, thiazide diuretics, etc.); History of serious adverse drug reactions to angiotensin II receptor blockers or calcium channel blockers; Patients with other serious reasons (i.e. illness, significant abnormalities, etc.) that investigators judge inappropriate for the study” Type of diabetes: type 2 HbA1c categories/levels: not reported Retinopathy status: not reported |
| Interventions |
Intervention 1: ARB therapy: olmesartan medoxomil 40 mg/day Intervention 2: Combination therapy: ARB and calcium channel blocker (olmesartan medoxomil 20 mg/day and either amlodipine or azelnidipine) Length of follow-up: Planned: 36 months Actual: not reported |
| Outcomes |
Primary study outcome: composite fatal and nonfatal cardiovascular events; coronary events; heart failure; vascular events; diabetic complications (nephropathy, retinopathy, neuropathy); renal dysfunction; all-cause mortality Secondary study outcomes: change in blood pressure; serious adverse events not including primary outcomes Intervals at which outcomes were assessed: not reported Eyes examined for outcome: not reported Cost of interventions: not reported Quality of life: not reported |
| Starting date | August 2005 |
| Contact information | Kikuo Arakawa, MD Emeritus Professor, Fukuoka University Fukuoka, Japan |
| Notes | ClinicalTrials.gov identifier: NCT00134160 |
| NCT00300976 | |
| Trial name or title | Japan Diabetes Optimal Integrated Treatment Study for 3 Major Risk Factors of Cardiovascular Diseases (J-DOIT3) |
| Methods |
Study design: Parallel group RCT Unit of randomization and analysis: individual Number randomized - Total: not reported Per group: not reported Sample size calculation: not reported |
| Participants |
Country: Japan Study period: not reported Age: not reported Gender: not reported Race/ethnicity: not reported Inclusion criteria: Individuals aged 45 to 70 years with type 2 diabetes with 1 of the following: 1) HbA1c ≥ 6.9% despite therapy and lifestyle interventions; 2) SBP ≥ 140 mmHg or DBP ≥ 90 mmHg when not on anti-hypertensive therapy or SBP of 130 mmHg or DBP of 80 mmHg on ACE inhibitors, ARBs, and/or long-acting calcium channel blockers; 3) abnormalities in lipid metabolism Exclusion criteria: “1. Those with poorly controlled hypertension despite pharmacological therapy (systolic BP 200 mmHg or diastolic BP 120 mmHg) 2. Those on insulin therapy 3. Those with non-diabetic renal disease 4. Those in whom type 1 and other diabetes due to pathogenic mechanisms other than those associated with type 2 diabetes is strongly suspected 5. Those who tested anti-GAD antibody*-positive 6. Those with LDL-cholesterol 200 mg/dL 7. Those suspected of having secondary hypertension other than renal parenchymal hypertension 8. Those suspected of having hereditary lipid disorder with a strong family history of lipid metabolic disorder 9. Those who were receiving antihypertensive agents other than ARB, ACEI, long-acting CCB, except where they were receiving these agents for other purposes than blood pressure lowering 10. Those who were receiving 3 or more antihypertensive agents (i.e., ARB, ACEI, and long-acting CCB), except where they were receiving these agents for other purposes than blood pressure lowering 11. Those with more serious retinopathy than proliferative retinopathy 12. Renal failure (serum Cr: 2.0 mg/dL in men; 1.5 mg/dL in women) 13. Those with a history of cardiac failure or those with cardiac failure 14. Those who were pregnant or potentially pregnant 15. Those who met any of the following criteria and who had BNP 100 pg/mL, Myocardial infarction, Angina pectoris (or a history of disease), History of coronary artery bypass graft (CABG), History of percutaneous coronary angioplasty (PTCA), Other cardiac disease, ECG findings of left ventricular hyperplasia, Abnormal ECG findings (excluding isolated extrasystole or right bundle branch block (RBBB)) 16. Those judged by the physician in charge to be ineligible for study entry” Type of diabetes: type 2 HbA1c categories/levels: not reported Retinopathy status: not reported |
| Interventions |
Intervention 1: Intensive therapy: weight control, diet, and exercise through lifestyle consultation; and drug therapy to achieve HbA1c < 6.2%, SBP/DBP < 120/75 mmHg, high-density lipoprotein cholesterol of 40 mg/dL, low-density lipoprotein cholesterol < 80 mg/dL, triglycerides < 120 mg/dL Intervention 2: Conventional therapy: weight control, diet, and exercise according to standard guidelines Length of follow-up: Planned: not reported; follow up every 6 or 12 months Actual: not reported |
| Outcomes |
Primary study outcome: incidence of cardiovascular events Secondary study outcomes: incidence or progression of nephropathy, retinopathy, incidence of peripheral vascular events Intervals at which outcomes were assessed: every 6 or 12 months Eyes examined for outcome: not reported Cost of interventions: not reported Quality of life: not reported |
| Starting date | May 2006 |
| Contact information | Takashi Kadowaki University of Tokyo |
| Notes | ClinicalTrials.gov identifier: NCT00300976 |
ACE: angiotensin-converting enzyme ARBs: angiotensin II receptor blockers DBP: diastolic blood pressure HbA1c: glycated hemoglobin mg/dL: milligram per deciliter mmHg: millimeter of mercury ORPS: Oxford Regional Prospective Study RCT: randomized controlled trial SBP: systolic blood pressure
Table 8.
Characteristics of studies awaiting assessment [ordered by study ID]
| ABCD-2V | |
| Methods |
Study design: randomized controlled trial, single center Unit of randomization and analysis: individual Number randomized - Total: 129 Per group: 66 allocated to intensive treatment; 63 allocated to moderate treatment Sample size calculation: not reported |
| Participants |
Country: USA Study period: not reported Age: mean (SD) 56.7 (7.7) years in intensive treatment group and 55.5 (7.7) in moderate treatment group Gender: 33.3% in intensive treatment group and 31.7% in moderate treatment group were women Race/ethnicity: 71.2% white, 19.7% Hispanic, 9.1%African-American in intensive treatment group; 76.2% white, 11.1% Hispanic, 6.4% African-American, and 3.2% Asian in moderate treatment group Inclusion criteria: type 2 diabetes, 40 to 81 years of age, with a SBP < 140 mmHg, a DBP between 80 and 90 mmHg, and without evidence of overt albuminuria (< 200 μg/min) Exclusion criteria: “pregnant or lactating women, need for any antihypertensive medications, documented myocardial infarction or cerebrovascular accident within the past 6 months, severe peripheral vascular disease, history of bilateral renal artery stenosis or stenosis in a solitary kidney, evidence of severe liver disease, hyperkalemia, or history of active cancer” Type of diabetes: type 2 HbA1c categories/levels: not reported Retinopathy status: both non-proliferative and proliferative |
| Interventions |
Intervention 1: intensive treatment Intervention 2: moderate treatment Length of follow-up: Planned: 5 years Actual: mean follow-up was 1.9 ± 1.0 years; ranging from < 1 year to 4 years, with 12 participants having 4 years of follow-up |
| Outcomes |
Primary outcomes for this review: progression of diabetic retinopathy Secondary outcomes for this review: none mentioned Other diabetic retinopathy outcomes: regression of diabetic retinopathy Other outcomes: change in creatinine clearance from baseline, proportion with doubling of serum creatinine, and change in log urinary albumin excretion from baseline; progression/regression of neuropathy; incidence of cardiovascular events Intervals at which outcomes were assessed: every 6 months Eyes examined for outcome: not reported Cost of interventions: not reported Quality of life: not reported |
| Notes |
Source of funding: Novartis Pharmaceutical Company Declaration of interest: not reported |
| ADDITION 2014 | |
| Methods |
Study design: cluster randomized controlled trial Unit of randomization and analysis: individual Number randomized - Total: 3057 Per group: 1678 allocated to intensive care; 1379 allocated to routine care Sample size calculation: Yes; “We calculated that a patient-level randomised trial would have required enrolment of 2700 individuals (1350 per treatment group) to detect a 30% reduction in the risk of the primary endpoint at a 5% significance level, and with 90% power. This calculation allowed for 10% loss to follow-up and assumed an event rate in the routine care group of 3% per year, on the basis of the results of the UK Prospective Diabetes Study Group (UKPDS). We expected a minimum effect of clustering within general practice, with the estimated within-cluster correlation coefficient being 0·01. We assumed that the average number of participants per general practice would be 10 and, therefore, the design effect was 1·09. Thus, we inflated the estimated sample size for this cluster trial to 3000 patients in total.” |
| Participants |
Country: Denmark, United Kingdom, the Netherlands Study period: September 2008 to the end of December 2009 Age: not reported Gender: not reported Race/ethnicity: not reported Inclusion criteria: newly diagnosed type 2 diabetes Exclusion criteria: patients had “contraindications to the proposed study medication, an illness with a life expectancy of 12 months, or psychological or psychiatric problems that were likely to invalidate informed consent” Type of diabetes: type 2 HbA1c categories/levels: not reported Retinopathy status: not reported |
| Interventions |
Intervention 1: intensive treatment Intervention 2: routine care Length of follow-up: Planned: 5 years Actual: mean (SD) follow-up period of 5.3 (1.6) years |
| Outcomes |
Primary outcomes for this review: combined incidence and progression of diabetic retinopathy Secondary outcomes for this review: none mentioned Other outcomes: neuropathy Intervals at which outcomes were assessed: not reported Eyes examined for outcome: both eyes, but whether average of two eyes were analyzed or whether two eyes were analyzed separately not stated Cost of interventions: not reported Quality of life: not reported |
| Notes |
Source of funding: multiple sources from government agencies, foundations, etc Declaration of interest: multiple sources including receiving grants, speaking and travel expenses, advisory board members, etc Author’s contact information: Annelli Sandbæk, annelli.sandbaek@alm.au.dk |
| ROADMAP | |
| Methods |
Study design: randomized, double-blind, placebo-controlled, parallel-group, multicenter, phase III Unit of randomization and analysis: individual Number randomized - Total: not reported Per group: not reported Sample size calculation: Yes; The study can “detect a 30% reduction in the risk of microalbuminuria (hazard ratio of 1.433) with 90% power at the 5% significance level … Thus, at least 2043 subjects are needed in each treatment arm and 328 events of microalbuminuria are expected to be observed. To compensate for withdrawals, 2200 patients are being recruited and randomized to each of the two treatment arms of the study.” |
| Participants |
Country: European countries including Austria, Belgium, Bulgaria, Czech Republic, Estonia, France, Germany, Hungary, Italy, Latvia, Lithuania, Poland, Romania, Russia, Slovak Republic, Spain, the Netherlands, the United Kingdom, and Ukraine Study period: not reported Age: not reported Gender: not reported Race/ethnicity: not reported Inclusion criteria: Type 2 diabetics free of signs of urinary albumin excretion who have one additional cardiovascular risk factor; if hypertensive, not taking ACE inhibitors or ARBs; 18 to 75 years of age; HbA1c ≥ 6.5% or are on treatment; hypertensive (SBP ≥ 130 mmHg and/or DBP ≥ 80 mmHg) Exclusion criteria: renal and/or renal-vascular disease (including malignant or severe renal disease); a history of nephrectomy and/or renal transplantation, or if they require dialysis; a recent history (within 6 months of starting the study) of myocardial infarction, stroke, transient ischaemic attack, myocardial revascularization or reperfusion; recent use of (within 6 months of starting the study) ARBs or ACE inhibitors or if they have severe hypertension, defined as SBP > 200 mmHg and/or DBP > 110 mmHg; severe uncontrolled hyperlipidaemia, severe heart failure, bradycardia (< 50 beats/minute at rest), a significant narrowing of the aortic bicuspid valve, a severe obstruction of cardiac outflow (hypertrophic cardiomyopathy, New York Heart Association (NYHA) stage 3–4) Type of diabetes: type 2 HbA1c categories/levels: not reported Retinopathy status: not reported |
| Interventions |
Intervention 1: 40 mg olmesartan twice daily with water before breakfast Intervention 2: placebo tablet twice daily with water before breakfast Length of follow-up: Planned: 5 years Actual: not reported |
| Outcomes |
Primary outcome for this review: incidence and progression of retinopathy Secondary outcomes for this review: none mentioned Other outcomes: time to albuminuria, cardiovascular mortality, stroke, cardiovascular morbidity, serum creatinine, hospitalization for various bad outcomes (end-stage renal disease, worsening glomerular filtration rate) Intervals at which outcomes were assessed: week 4, week 12, and month 6 (visits 2, 3, and 4, respectively) and thereafter every 6 months until the end of the study Eyes examined for outcome: not reported Cost of interventions: not reported Quality of life: not reported |
| Notes |
Source of funding: Sankyo Declaration of interest: “All steering committee members are consultants for Sankyo for the ROADMAP study.” |
Data extraction and management
Two review authors independently extracted data necessary to describe study characteristics, judge risk of bias, and describe outcomes from included trials and recorded them onto paper data collection forms developed by the Cochrane Eyes and Vision Group. We extracted details of study methods, participants, interventions, outcomes, cost, and quality-of-life data. We resolved discrepancies through discussion or consultation with a third author when members of a pair disagreed. We contacted primary investigators in an effort to obtain outcome data not reported. One review author entered data into Review Manager 5.3 (RevMan 2014); a second review author verified the entries.
One review author made a final check of the review in June 2014 to confirm that all extracted data had been entered into Review Manager 5.3 and that entries agreed with full-text reports and supplemental information provided by study investigators. During that process, we found additional data regarding outcomes for a few studies. The reviewing author extracted the newly found data; a second author confirmed all data extracted, entered the data into Review Manager 5.3, and updated the analyses with the added data included.
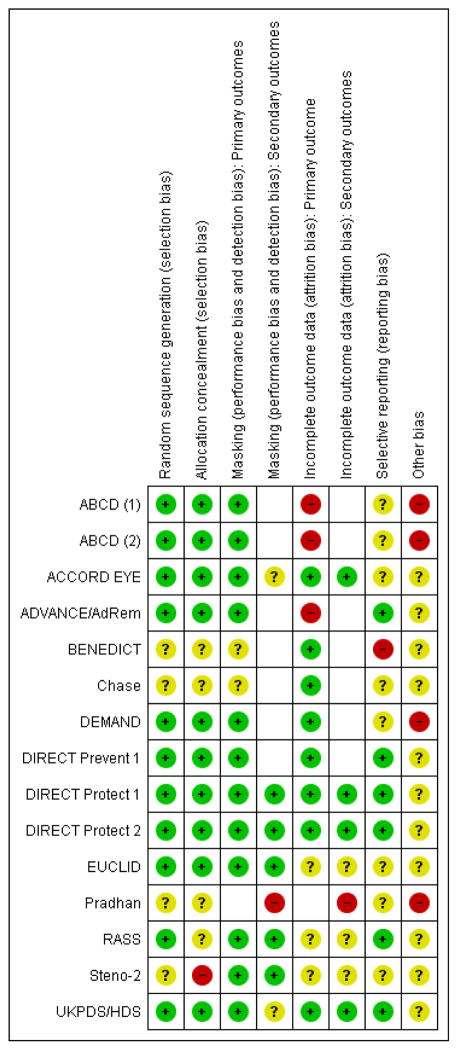
Assessment of risk of bias in included studies
Pairs of review authors independently assessed the included trials for risk of bias according to methods described in Chapter 8 of the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011). We assessed the risk of bias for the following domains: (a) generation of allocation sequence, (b) allocation concealment before randomization, (c) masking of caregivers, participants, and outcome assessors, (d) methods used to address incomplete or missing outcome data, (e) selective outcome reporting, and (f) other sources of bias. We classified each trial as having ’low,’ ’high,’ or ’unclear’ risk of bias with respect to each domain.
We contacted trial investigators for clarification whenever information relevant to domains of potential bias was reported unclearly or was missing from the published reports. We attempted to assess evidence of reporting bias by comparing protocols and publications on trial design, where available, with publications of results. We were able to access protocols for only a few trials included in the review. For trials without a publicly available protocol, we assessed reporting bias by comparing the Results section and the Methods section of the published trial reports. Again, we resolved disagreements through discussion.
We adopted the following conventions to assess other sources of bias, with specific attention paid to funding source: 1. High risk of bias: total industry support and other source(s) of potential bias identified 2. Unclear risk of bias: i) Total industry support but no other source of potential bias identified ii) Partial industry support and other source(s) of potential bias iii) No industry support but other source(s) of potential bias judged not to be classifiable as ’high risk’ 3. Low risk of bias: i) Industry support limited to donations of drugs or materials and no other source of potential bias identified ii) No industry support reported and no other source of potential bias identified
Measures of treatment effect
Because all outcomes considered for this review were dichotomous, we estimated and reported risk ratios (RRs) with 95% confidence intervals (CIs) for primary and secondary outcomes (incidence of retinopathy, progression of retinopathy, combined incident and progressed retinopathy, visual acuity decrease of greater than or equal to three lines, and progression to PDR or CSME) and for adverse events. Whenever the 95% CI for a RR did not include 1, we interpreted the comparison as yielding a statistically significant result despite the many comparisons reported in this review. We did not estimate treatment effects for quality-of-life outcomes or costs; rather we summarized these data by study and treatment group as reported by the trial investigators.
Unit of analysis issues
The unit of analysis was the person.
Dealing with missing data
We contacted study investigators when information we sought was missing or reported unclearly. When there was no response, we used the available data. We did not include studies that reported no data for diabetic retinopathy outcomes. We did not impute data for the purposes of this review.
Assessment of heterogeneity
We assessed clinical and methodological heterogeneity across included trials using participant characteristics, details of interventions, duration of follow-up, risk of bias, and definitions of outcomes. We examined statistical heterogeneity using the Chi2 test and I2 values; we considered an I2 greater than 50% to indicate substantial statistical heterogeneity.
Assessment of reporting biases
For selective outcome reporting, we compared the protocols of studies, when available, with the primary published report. We compared the outcomes specified in the Methods section and the outcomes reported in the Results section of published reports when a protocol was not available. We planned to use asymmetry of funnel plots as an indicator of potential publication bias, but too few studies reported individual outcomes for this approach to be useful. In future updates when a meta-analysis includes 10 or more studies, we expect to assess potential publication bias by examining funnel plots.
Data synthesis
We planned to employ a fixed-effect model to conduct meta-analyses using data from trials with no or minimal clinical or methodological heterogeneity. Due to methodological, clinical, and statistical heterogeneity among included trials, we used a random-effects model in meta-analyses of 4- to 5-year outcomes. We based meta-analyses of outcomes between 1.5 and 2 years on a fixed-effect model.
Subgroup analysis and investigation of heterogeneity
We planned to conduct subgroup analyses according to baseline level of metabolic control, as determined using glycated hemoglobin (HbA1c), and severity of diabetic retinopathy whenever sufficient data were available. However, none of the publications from the trials reported outcomes by baseline HbA1c levels. Post hoc, but before retrieval of full-text reports of studies identified as ’include’ or ’uncertain,’ we agreed to present outcomes separately for trials that enrolled type 1 and type 2 diabetics because of the different etiologies and characteristics of the conditions. We also decided to present outcomes separately for participants who were hypertensive at baseline for comparison with those who were normotensive or whose hypertension was controlled by treatment at baseline because of potential differences in benefits versus risks of intervention on blood pressure in these subgroups.
Sensitivity analysis
We planned to conduct sensitivity analyses to determine the impact of exclusion of studies with high risk of attrition bias, unpublished studies, and industry-funded studies. We did not conduct any of the pre-specified sensitivity analyses as it was not possible to assess attrition in all included studies; most studies had industry support; and we did not include data from any unpublished study.
RESULTS
Description of studies
Results of the search
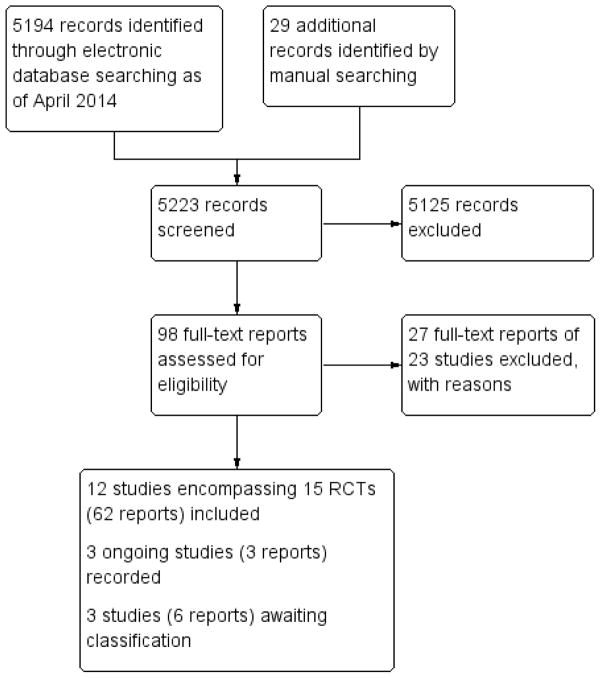
We screened a total of 5157 records retrieved from bibliographic database searches and 37 records retrieved from clinical trial registers as of 25 April 2014 (Figure 1). We also retrieved three full-text reports identified from reference lists in the screened citations and two additional citations for ongoing studies. To facilitate data extraction, we retrieved an additional 24 full-text articles for the included studies. From 5223 total records screened, we retrieved full-text reports for 98 records assessed as potentially relevant for this review. We excluded 27 full-text reports from 23 studies described in the Characteristics of excluded studies table. We included 62 full-text reports from 12 studies (15 randomized trials). Three studies based on six reports are awaiting final assessment pending receipt of additional information regarding study characteristics (ABCD-2V; ADDITION 2014; ROADMAP); we will consider them when we update this review (see Characteristics of studies awaiting classification table). Finally, we identified three ongoing trials (AdDIT; NCT00134160; NCT00300976), which are described in the Characteristics of ongoing studies table.
Figure 1.
Results of searching for studies for inclusion in the review
Included studies
A detailed description of the individual included trials is provided in the Characteristics of included studies table. The study characteristics are summarized in the following sections.
Table 6.
Characteristics of included studies [ordered by study ID]
| ABCD (1) | ||
| Methods |
Study design: 1 of 2 parallel group RCTs conducted within ABCD Unit of randomization and analysis: individual Number randomized - Total: 950 Per group: 480 normotensive patients: 237 to intensive therapy and 243 to moderate therapy Sample size calculation: sample size calculation was based on glomerular filtration rate; power was not reported |
|
| Participants |
Country: USA Study period: accrual: March 1991 to May 1993; follow-up planned for 5 to 7 years after March 1991 Age: mean (SD) was 58.5 (9.2) years in intensive therapy group and 59.1 (7.8) in moderate therapy group Gender: 47% in intensive therapy group and 44% in moderate therapy group were women Race/ethnicity: 74.1% non-Hispanic white; 7% African-American; 16.6% Hispanic; 0.8% Asian; 1.2% other Inclusion criteria: patients with type 2 diabetes diagnosed by WHO criteria aged 40 to 74 years at study enrollment, willing to participate in study, and likely to complete 5 to 7 years of study Exclusion criteria: pregnant or lactating women, allergies to study medications, heart disease including uncorrected heart block, myocardial infarction, angina or heart failure, malignant hypertension, peripheral vascular disease, aortic dissection, on dialysis or other kidney disease, liver disease Participants’ status at baseline: Blood pressure control: mean (SD) SBP was 135.6 (12.3) mmHg, DBP was 84.4 (3. 1) mmHg in intensive therapy group; SBP was 137.2 (14.0) mmHg, DBP was 84.4 (3. 1) mmHg in moderate therapy group Type of diabetes: type 2 HbA1c categories/levels: mean (SD) was 11.5 (3.1) in intensive therapy group and 11. 6 (3.1) in moderate therapy group Severity of retinopathy: 47.9% no retinopathy; 44% NPDR; 4% PDR; 4% ungradable |
|
| Interventions |
Intervention 1: intensive blood pressure control Goal DBP 10 mmHg below baseline Participants were randomized to either nisoldipine 10 mg/day, titrated to 20, 40, and then 60 mg/day (plus placebo for enalapril), or enalapril 5 mg/day titrated to 10, 20, and then 40 mg/day (plus placebo for nisoldipine) as the initial anti-hypertensive medication. Additional anti-hypertensive medications were added in an open-label fashion in a step-wise manner initially with metoprolol, then hydrochlorothiazide, and then until the target blood pressure was achieved. Addition of medications was at the discretion of the medical director, but the additional medications could not include calcium channel blockers or ACE inhibitors Intervention 2: moderate blood pressure control Goal DBP 80 to 89 mmHg; randomized to nisoldipine or enalapril if DBP ≤ 90 mmHg Length of follow-up: Planned: 5 to 7 years Actual: 4.7 years mean |
|
| Outcomes |
Primary outcome, as specified for this review: retinopathy: using modified Airlie House classification as adapted from DCCT at 2 and 5 years follow-up, graded by the Wisconsin Retinal Reading Center; overall retinopathy according to ETDRS interim scale--23 steps to represent overall extent of retinopathy in both eyes; progression of retinopathy defined as a 2-step worsening from baseline based on 7-field stereoscopic fundus photographs. Progression was not reported separately from incidence for nor-motensives or hypertensives; incidence was not reported for hypertensives Secondary outcomes, as specified for this review: visual acuity and incidence of CSME not reported Eye examined for the outcome: both eyes Intervals at which outcomes were assessed: retinal photographs taken at 2- and 5-years follow-up Cost of interventions: not reported Quality of life: not reported Other outcomes reported from the study: glomerular filtration rate, urinary albumin excretion, left ventricular hypertrophy, neuropathy, and cardiovascular events |
|
| Notes |
Source of funding: industry and government Declaration of interest: not reported Run-in length: 7 to 11 weeks on placebo Class(es) of anti-hypertensive agents: calcium channel blocker, ACE inhibitor Degrees of blood pressure control: intensive therapy and moderate therapy had goals described above in the interventions section; however, both groups achieved blood pressure control targets for intensive control group |
|
| Risk of bias | ||
| Bias | Authors’ judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | “Randomization using permuted block randomization within strata was used to ensure equal sample sizes within all arms of the study.” |
| Allocation concealment (selection bias) | Low risk | “The random assignment to intensive versus moderate treatment with either active nisoldipine coat-core or enalapril medication was made by telephone by the Data Coordinating Center and the Clinical Co-ordinating Center.” |
| Masking (performance bias and detection bias) Primary outcomes |
Low risk | “The drugs and placebos were administered in a double-blind manner. If the single study medication assigned did not achieve the target blood pressure, then open-label antihypertensive medications were added in a stepwise fashion until the target blood pressure was achieved.” “All retinal films are interpreted and staged at the Wisconsin Retinal Reading Center without knowledge of the group to which the patient has been randomized.” |
| Incomplete outcome data (attrition bias) Primary outcome |
High risk | No specific information on withdrawals, exclusions, or losses to follow-up were reported. However, figures in each report of outcomes show numbers of participants at each examination through 5 years that suggest ~40% of those enrolled were lost to follow-up sometime during the 5-year period. No analysis to account for attrition |
| Selective reporting (reporting bias) | Unclear risk | Unclear with available information. Percentages reported without explicit denominators for outcomes over 5 years |
| Other bias | High risk | “Financial support was provided by Bayer Pharmaceutical Company.” “Supported by the Bayer Pharmaceutical Company and by a grant (DK50298-02) from the National Institute of Diabetes and Digestive and Kidney Diseases.” “We are indebted to the members of the Data and Safety Monitoring Committee for their guidance: Paul W. Whelton, M.D., Tulane University, New Orleans;… and Kevin Higgins, M.D., Bayer Pharmaceuticals, West Haven, Conn.” |
| ABCD (2) | ||
| Methods |
Study design: 1 of 2 parallel group RCTs conducted within ABCD Unit of randomization and analysis: individual Number randomized - Total: 950 Per group: 470 hypertensive participants; 237 to intensive therapy and 233 to moderate therapy Sample size calculation: sample size calculation was based on glomerular filtration rate; power was not reported |
|
| Participants |
Country: USA Study period: accrual: March 1991 to May 1993; follow-up planned for 5 to 7 years after March 1991 Age: mean (SD) was 58.0 (8.4) years in intensive therapy group and 57.7 (8.3) years in moderate therapy group Gender: 33% in intensive therapy group and 32% in moderate therapy group were women Race/ethnicity: 66.3% non-Hispanic white; 17% African-American; 13.4% Hispanic; 1.9% Asian; 1% other Inclusion criteria: patients with type 2 diabetes diagnosed by WHO criteria aged 40 to 74 years at study enrollment, willing to participate in study, and likely to complete 5 to 7 years of study Exclusion criteria: pregnant or lactating women, allergies to study medications, heart disease including uncorrected heart block, myocardial infarction, angina or heart failure, malignant hypertension, peripheral vascular disease, aortic dissection, on dialysis or other kidney disease, liver disease Participants’ status at baseline: Blood pressure control: mean (SD) SBP was 156 (16.1) mmHg, DBP was 98 (6.4) mmHg in intensive therapy group; SBP 154 (16.9) mmHg and DBP 98 (6.4) mmHg in moderate therapy group Type of diabetes: type 2 HbA1c categories/levels: mean (SD) was 11.6 (3.2) in intensive therapy group and 11. 5 (3.5) in moderate therapy group Severity of retinopathy: 38.5% no retinopathy; 52.5% NPDR; 4.5% PDR; 4.5% ungradable |
|
| Interventions |
Intervention 1: intensive blood pressure control Goal DBP 75 mmHg Participants were randomized to either nisoldipine 10 mg/day, titrated to 20, 40, and then 60 mg/day (plus placebo for enalapril), or enalapril 5 mg/day titrated to 10, 20, and then 40 mg/day (plus placebo for nisoldipine) as the initial anti-hypertensive medication. Additional anti-hypertensive medications were added in an open-label fashion in a step-wise manner initially with metoprolol, then hydrochlorothiazide, and then until the target blood pressure was achieved. Addition of medications was at the discretion of the medical director, but the additional medications could not include calcium channel blockers or ACE inhibitors Intervention 2: moderate blood pressure control Goal DBP 89 mmHg Length of follow-up: Planned: 5 to 7 years Actual: 4.7 years mean |
|
| Outcomes |
Primary outcome, as specified for this review: retinopathy: using modified Airlie House classification as adapted from DCCT at 2 and 5 years follow-up, graded by the Wisconsin Retinal Reading Center; overall retinopathy according to ETDRS interim scale--23 steps to represent overall extent of retinopathy in both eyes; progression of retinopathy defined as a 2-step worsening from baseline based on 7-field stereoscopic fundus photographs. Progression was not reported separately from incidence for nor-motensives or hypertensives; incidence was not reported for hypertensives Secondary outcomes, as specified for this review: visual acuity and incidence of PDR or CSME not reported Eye examined for the outcome: both eyes Intervals at which outcomes were assessed: retinal photographs taken at 2- and 5-years follow-up Cost of interventions: not reported Quality of life: not reported Other outcomes reported from the study: glomerular filtration rate, urinary albumin excretion, left ventricular hypertrophy, neuropathy, and cardiovascular events |
|
| Notes |
Source of funding: industry and government Declaration of interest: not reported Run-in length: 7 to 11 weeks on placebo Class(es) of anti-hypertensive agents: calcium channel blocker, ACE inhibitor Degrees of blood pressure control: intensive therapy and moderate therapy had goals described above in the interventions section; however, both groups achieved blood pressure control targets for intensive control group |
|
| Risk of bias | ||
| Bias | Authors’ judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | “Randomization using permuted block randomization within strata was used to ensure equal sample sizes within all arms of the study.” |
| Allocation concealment (selection bias) | Low risk | “The random assignment to intensive versus moderate treatment with either active nisoldipine coat-core or enalapril medication was made by telephone by the Data Coordinating Center and the Clinical Co-ordinating Center.” |
| Masking (performance bias and detection bias) Primary outcomes |
Low risk | “The drugs and placebos were administered in a double-blind manner. If the single study medication assigned did not achieve the target blood pressure, then open-label antihypertensive medications were added in a stepwise fashion until the target blood pressure was achieved.” “All retinal films are interpreted and staged at the Wisconsin Retinal Reading Center without knowledge of the group to which the patient has been randomized.” |
| Incomplete outcome data (attrition bias) Primary outcome |
High risk | No specific information on withdrawals, exclusions, or losses to follow-up were reported. However, figures in each report of outcomes show numbers of participants at each examination through 5 years that suggest ~40% of those enrolled were lost to follow-up sometime during the 5-year period. No analysis to account for attrition |
| Selective reporting (reporting bias) | Unclear risk | Unclear with available information. Percentages reported without explicit denominators for outcomes over 5 years |
| Other bias | High risk | “Financial support was provided by Bayer Pharmaceutical Company.” “Supported by the Bayer Pharmaceutical Company and by a grant (DK50298-02) from the National Institute of Diabetes and Digestive and Kidney Diseases.” “We are indebted to the members of the Data and Safety Monitoring Committee for their guidance: Paul W. Whelton, M.D, Tulane University, New Orleans; … and Kevin Higgins, M.D., Bayer Pharmaceuticals, West Haven, Conn.” |
| ACCORD EYE | ||
| Methods |
Study design: substudy of ACCORD - a 2×2 factorial RCT Unit of randomization and analysis: individual Number randomized - Total: 10,251 in ACCORD; 3537 enrolled in the ACCORD EYE study and 1590 in the ACCORD EYE blood pressure trial; 1263 participants in the blood pressure trial with 4-year follow-up data were analyzed for diabetic retinopathy outcomes in ACCORD EYE Per group: blood pressure trial (n = 1263): 647 (intensive) and 616 (standard) analyzed for diabetic retinopathy outcomes. Visual acuity outcomes analyzed for 1546 participants: 798 (intensive) and 748 (standard) Sample size calculation: target of 4065, which would have given 80% power to detect a 20% relative reduction with intensive blood pressure control as compared with standard blood-pressure control (power of 77% for the blood pressure question for ACCORD EYE with 1263 enrolled participants, per ad hoc calculation) |
|
| Participants |
Country: USA and Canada Study period: protocol developed October 1999; randomization in ACCORD began January 2001 (for Vanguard centers) and restarted February 2003; accrual ended October 2005; follow-up completed June 2009 Age: mean (SD) was 61.3 ± 6.1 (intensive) and 61.5 ± 6.6 (standard) ACCORD EYE blood pressure trial Gender: 48% in intensive therapy group and 45% in standard therapy group were women Race/ethnicity: 31.4% non-white participants in intensive group and 32.6% non-white participants in standard group of the ACCORD EYE blood pressure trial Inclusion criteria: type 2 diabetes (> 3 months); HbA1c level of ≥ 7.5%; and high risk for cardiovascular disease (established cardiovascular disease or had known risk factors) Exclusion criteria: history of proliferative diabetic retinopathy that had been treated with laser photocoagulation or vitrectomy Participants’ status at baseline: Blood pressure control: mean 138 ± 17/76 ± 10 (intensive), 139 ± 15/77 ± 10 (standard) Type of diabetes: type 2 HbA1c categories/levels: 8.4 ± 1.1 (intensive) and 8.2 ± 1.0 (standard) Severity of retinopathy: intensive group: 50.9% none; 16.3% mild; 30.2% moderate NPDR; 0.5% severe NPDR; 2.2% PDR Standard group: 47.9% none; 19.0% mild; 32.1% moderate NPDR; 0.2% severe NPDR; 0.8% PDR |
|
| Interventions |
Intervention 1: intensive blood pressure control (intervention) arm targeted SBP < 120 mmHg. The recommendation was to start with a combination of a diuretic and either an ACE inhibitor or a beta-blocker at randomization. Drug doses were increased or additional anti-hypertensive medications were added, or both, at each subsequent visit in the intensive group until goal was reached Intervention 2: the standard blood pressure control arm targeted SBP < 140 mmHg. Medication dose titration or the addition of another drug was indicated whenever SBP was ≥ 160 mmHg at a single visit or ≥ 140 mmHg at 2 successive visits Both the intensive and standard treatment groups in the blood pressure trial were factorial with intensive glycemic control (maintain an HbA1c level < 6.0%) and standard (targets an HbA1c range of 7.0% to 7.9%) Length of follow-up in ACCORD EYE: Planned: 4 years Actual: 4 years |
|
| Outcomes |
Primary outcome, as specified for this review: progression of diabetic retinopathy by at least 3 steps on the ETDRS severity scale. Incidence and progression reported in combination, not separately Secondary outcomes, as specified for this review: development of proliferative diabetic retinopathy necessitating photocoagulation therapy or vitrectomy; development or progression of macular edema; change in visual acuity at 4 years compared with baseline: moderate vision loss (i.e. loss of ≥ 3 lines on the logMAR visual acuity charts) Other diabetic retinopathy outcomes: legal blindness (20/160 or worse), severe vision loss (5/200) Eye examined for the outcome: average of both eyes Intervals at which outcomes were assessed: visual acuity assessment at baseline, years 2, 4, 6, and 8 or at the study closeout visit; retinopathy assessed at 4 years Cost of the intervention: not reported Quality of life: not reported |
|
| Notes |
Sources of funding: government and industry-donated study medications, equipment, and supplies Declaration of interest: several authors declared interests related to pharmaceutical companies Class(es) of anti-hypertensive agents compared: not specified Degree of blood pressure control: intensive: median < 120 mmHg (115 to 120); standard: median < 140 mmHg (135 to 140) Concomitant treatment: participants were also randomized to intensive (maintenance of HbA1c < 6.0%) or standard (HbA1c 7.0% to 7.9%) glycemic control |
|
| Risk of bias | ||
| Bias | Authors’ judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | “An Internet-based, web browser randomization procedure will be employed in ACCORD” (protocol). Algorithm used to generate random sequence was not clearly described |
| Allocation concealment (selection bias) | Low risk | “Randomization was performed centrally on the study’s web site with the use of permuted blocks to maintain concealment of future study-group assignments” |
| Masking (performance bias and detection bias) Primary outcomes |
Low risk | The blood pressure component of ACCORD was an unmasked, open-label randomized trial “The fundus photographs were evaluated by trained graders, who were unaware of the treatment assignments …” |
| Masking (performance bias and detection bias) Secondary outcomes |
Unclear risk | Did not report whether visual acuity assessors and ophthalmologists were masked to interventions |
| Incomplete outcome data (attrition bias) Primary outcome |
Low risk | 291 of 1263 participants (23%) in the ACCORD EYE blood pressure trial: 155 (intensive blood pressure) and 136 (standard blood pressure) “there was no evidence of significant differences regarding the amount of missing data, and the results of sensitivity analyses supported those of the primary analyses.” Used logistic regression methods for multiple imputation |
| Incomplete outcome data (attrition bias) Secondary outcomes |
Low risk | see above |
| Selective reporting (reporting bias) | Unclear risk | Progression to PDR and/or CSME not reported. |
| Other bias | Unclear risk | 65 of 3537 (1.8%) of randomized participants enrolled in ACCORD EYE were subsequently excluded from the trial due to detection of exclusion criteria after randomization. “… baseline fundus photographs could not be obtained within four months of randomization.” Conflicts of interests for the Data and Safety Monitoring Board members are unclear “For the Eye Substudy (in a subset of 4065 participants), the baseline eye exam/fundus photography can be performed up to 2 months post-randomization.” (protocol) |
| ADVANCE/AdRem | ||
| Methods |
Study design: substudy of ADVANCE - a 2×2 factorial RCT Unit of randomization and analysis: individual Number randomized - Total: 11,140 in ADVANCE; 2130 enrolled in ADVANCE/AdRem; 1982 had baseline photographs received, but only 1602 had valid baseline photographs; 1241 with gradeable baseline and final photographs were included in the AdRem analysis Per group: 623 to perindopril-indapamide; 618 to placebo Sample size calculation: target of 2000 was estimated to provide 85% power to detect an absolute reduction of 6.2% in the primary outcome event rate, assuming an event rate 27.8% over 6 years and a type I error of 0.05. “The main limitation of this study is the lower than planned sample size.” |
|
| Participants |
Country: 14 countries in Asia, Australia, Europe, and North America Study period: baseline photographs: August 2002 to January 2004 Age: mean (SD) was 65.6 (5.8) years in the perindopril-indapamide group and 65.6 (5. 9) years in the placebo group; 65.6 (5.8) overall Gender: 38.7% overall were women; 40.3% in the perindopril-indapamide group and 37.1% in the placebo group Race/ethnicity: perindopril-indapamide group: 48.5% white, 37.9% Chinese, 8.5% South Asian; placebo group: 47% white, 38.3% Chinese, 9.6% South Asian Inclusion criteria: all participants in ADVANCE (55 years or older at recruitment; diagnosed with type 2 diabetes at age 30 years or older; history of at least one of the following conditions: major cardiovascular disease, risk factors including history of major microvascular disease, current cigarette smoking, elevated total cholesterol (> 6.0 mmol/L), low HDL cholesterol (< 1.0 mmol/L), microalbuminuria, diagnosed with type 2 diabetes 10 years or more preceding entry into the study or age 65 years or older at recruitment; an indication for an ACE inhibitor) who enrolled at centers with retinal cameras were eligible to participate in ADVANCE/AdRem Exclusion criteria: for ADVANCE: definite indication or contraindication for the active study treatments or a definite indication for a HbA1c target of ≤ 6.5%, long-term insulin therapy at study entry, or participating in a different clinical trial; in addition for AdRem: previous ophthalmological intervention or inability to obtain good quality photographs due to either severe cataract or inadequate pupil dilation (< 4 mm) Participants’ status at baseline: Blood pressure control: mean (SD): perindopril-indapamide group 142.3/79.2 (22.0/11.2) mmHg; placebo 143.1/79.5 (21.4/10.5) mmHg; overall 142.7/79.3 (21.7/10.8) Type of diabetes: type 2 HbA1c categories/levels: mean (SD): perindopril-indapamide group 7.5 (1.5); placebo 7.3 (1.4); overall 7.4 (1.5) Severity of diabetic retinopathy: 40.9% in placebo group and 39.3% in perindopril-indapamide group for ETDRS grade ≥ 20 (microaneurysms only; mild, moderate, moderately severe, or severe non-proliferative diabetic retinopathy; or proliferative diabetic retinopathy) |
|
| Interventions |
Intervention 1: perindopril (2 mg) plus indapamide (0.625 mg) daily at randomization and doubled to perindopril (4 mg) plus indapamide (1.25 mg) after 3 months Intervention 2: placebo Length of follow-up: Planned: 5.5 years Actual: 4.1 years (median) |
|
| Outcomes |
Primary outcome, as specified for this review: progression of diabetic retinopathy ≥ 2 steps in ETDRS classification Secondary outcome, as specified for this review: visual acuity and progression to PDR or CSME not reported Other diabetic retinopathy outcomes: ≥ 1 and ≥ 3 steps of progression and individual diabetic retinopathy lesion development Eye examined for outcome: participant’s worse eye Intervals at which outcomes were assessed: within 3 months after randomization (photographs taken within 3 months following ADVANCE randomization were considered “baseline” photographs), at 2 years, and at final follow-up examination; retinal photographs taken at 2-year follow-up were used when photographs at final follow-up were not available Cost of the interventions: not reported Quality of life: not reported |
|
| Notes |
Source of funding: institutional and government support Declaration of interest: two authors declared interests related to pharmaceutical companies Run-in length: 6 weeks on “active blood pressure lowering treatment and usual glucose lowering treatment” Class(es) of anti-hypertensive agents compared: ACE inhibitor plus diuretic Degree of blood pressure control: drug treatment yielded mean decrease of 6.1 mmHg in SBP and 2.3 mmHg in DBP Concomitant treatment: standard and intensive glucose therapy as randomized |
|
| Risk of bias | ||
| Bias | Authors’ judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | “Randomisation was stratified by study centre, history of macrovascular disease, and background use of perindopril at base-line.” “A central computer-based randomization service will assign patients to treatments …” |
| Allocation concealment (selection bias) | Low risk | “Study treatments were allocated using a central, computer-based randomization service accessible by internet, telephone, and facsimile.” |
| Masking (performance bias and detection bias) Primary outcomes |
Low risk | “The two main effects comparisons were a double-blind comparison of blood pressure-lowering vs placebo … blinded end-point evaluation design.” |
| Incomplete outcome data (attrition bias) Primary outcome |
High risk | “All analyses were based on the intention-to-treat principle (1,241 patients with gradeable baseline and final photographs).” Participants with missing retinal photographs at baseline or follow-up were excluded from the analyses |
| Selective reporting (reporting bias) | Low risk | Outcomes in published results consistent with outcomes pre-specified in design paper |
| Other bias | Unclear risk | Baseline photographs were taken after the randomization visit, “preferably within 3 months after”; median of 2 months (IQR 1 to 6 months) |
| BENEDICT | ||
| Methods |
Study design: parallel group RCT Unit of randomization and analysis: individual Number randomized - Total: 550 with available fundus photographs at baseline (of 1209 total number of people randomized in BENEDICT) Per group: number of participants was not reported for the four individual treatment groups; 279 assigned to non-ACE inhibitor; 271 assigned to ACE inhibitor Sample size calculation: none; authors stated “at the time the present analyses were planned, no data were available on the regression of retinopathy in hypertensive patients with type 2 diabetes on intensified BP and metabolic control ….” For the BENEDICT trial, based on time to persistent albuminuria at 3-years follow-up with evidence of 9. 5% in the placebo group and 3.1% in the treatment group, estimated 225 per group to provide 80% power at 2-sided alpha = 0.05; adjusted for attrition to 300 per group |
|
| Participants |
Country: Italy Study period: not reported; design and number enrolled published in 2003. Age: mean (SD): 61.6 (8.1) years in the trandolapril group; 62.5 (8.2) years in the verapamil group; 62.7 (7.7) years in the VeraTran group; and 62.6 (8.2) years in the placebo group Retina subgroup (n = 550): 62.0 (7.8) years overall Gender: 48% in trandolapril group; 46% in verapamil group; 45% in combination (VeraTran) group; and 50% in placebo group were women Retina subgroup (n = 550): 256 (46%) were women Race/ethnicity: 99.8% white in BENEDICT overall Inclusion criteria: hypertensive type 2 diabetics < 25 years duration; urinary albumin excretion rate < 20 μg/min in 2 of 3 overnight urine collections; serum creatinine < 1.5 mg/dL; hypertension defined as previous anti-hypertensive therapy or SBP/DBP > 130/85 mmHg; for retina subgroup fundus exam/photos at baseline Exclusion criteria: concomitant nondiabetic renal disease; HbA1c > 11%; specific indications or contraindications for study drugs Participants’ status at baseline: Blood pressure control: retina subgroup (n = 550): SBP 151.6 ± 14.3 mmHg; DBP 88.8 ± 8.3 mmHg Type of diabetes: type 2 HbA1c categories/levels: retina subgroup (n = 550): mean (SD): 5.9 (1.5) Severity of diabetic retinopathy: 82 of 90 with retinopathy (out of 550) had pre-proliferative retinopathy at baseline (microaneurysms, hemorrhage, vitreous coagulation, hard exudates, CWS, IRMA) and 8 had PDR (NV, glial proliferation (i.e. sheathing), preretinal hemorrhage, vitreous hemorrhage, photocoagulation scars, and/or RD) |
|
| Interventions |
Intervention 1: non-dihydropyridine CCB verapamil SR, 240 mg/day Intervention 2: ACE inhibitor: trandolapril 2 mg/day Intervention 3: fixed-dose combination of verapamil SR, 180 mg/day, plus trandolapril 2 mg/day (VeraTran) Intervention 4: placebo Length of follow-up: Planned: 3 years Actual: median 3.6 years (IQR: 1.3 to 4.3); 35.9 months (IQR: 12.4 to 60.7) |
|
| Outcomes |
Primary outcome, as specified for this review: pre-specified in BENEDICT protocol to be new-onset retinopathy in participants free of retinopathy at baseline Secondary outcomes, as specified for this review: visual acuity and progression to PDR or CSME not reported Other diabetic retinopathy outcomes: regression of retinopathy; regression of retinal changes in participants with baseline retinopathy defined as “a persistent (up to the final visit) change in the stage of retinal involvement from proliferative to pre-proliferative retinopathy, or from pre-proliferative retinopathy to no retinal involvement”; “pre-proliferative retinopathy was defined by the presence of microaneurysms, hemorrhages, hard exudates, venous congestion, cotton wool spots, or intraretinal microvascular abnormalities”; “proliferative retinopathy was diagnosed when new vessels, glial proliferation, preretinal hemorrhage, vitreous hemorrhage, scars of photocoagulation (known to have been directed at new vessels), and/or retinal detachment were found” Eye examined for the outcome: both eyes were examined and the eye with the more severe involvement was used to categorize retinal involvement Intervals at which outcomes were assessed: baseline; yearly thereafter; and at the final visit Cost of the interventions: not reported Quality of life: not reported Other outcomes reported from the study: progression to micro- and macroabuminuria, increase in albuminuria, rate of glomerular filtration rate decline, incidence of major cardiovascular events, overall and cardiovascular mortality |
|
| Notes |
Source of funding: partial support from industry Declaration of interest: not reported Run-in length: “At the first visit of the study, patients on ACE inhibitor and conventional antihypertensive treatment withdraw previous antihypertensive medications and are randomized after at least 6- and 3-week washout, respectively.” Classes of anti-hypertensive agents compared: 1) ACE inhibitors to no ACE inhibitors; 2) non-dihydropyridine CCB to no non-dihydropyridine CCB Degree of blood pressure control: not reported for the retina subgroup; in BENEDICT, similar for all arms at 3 years, SBP/DBP about 135/75 Concomitant treatment: “Other antihypertensive drugs (with the exception of RAS inhibitors and ndCCBs different from the study drugs) could be used to achieve and maintain target BP according to predefined guidelines.” |
|
| Risk of bias | ||
| Bias | Authors’ judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | “The unblinded data centre receives the randomization code from the sponsor.” |
| Allocation concealment (selection bias) | Unclear risk | No description provided. |
| Masking (performance bias and detection bias) Primary outcomes |
Unclear risk | Inadequate information provided for incident diabetic retinopathy |
| Incomplete outcome data (attrition bias) Primary outcome |
Low risk | “Of the 1209 patients randomized in the original BENEDICT cohort, 583 patients were referred to the two centers involved in the present study. Five hundred-fifty patients had a baseline funduscopy evaluation” 1209 randomized while 1204 were analyzed in parent study: 4 never took study medication; 1 ineligible |
| Selective reporting (reporting bias) | High risk | The protocol states: “The retinopathy grading score used makes it possible to quantify the progression of the retinal changes. Worsening of the disease is defined as progression from a less-severe to a more-severe class during follow-up.” However, the results were reported as: “...regression of retinopathy...”. Progression cannot be derived from regression without data regarding stabilization |
| Other bias | Unclear risk | Support in part by Abbott (pharmaceutical company) where Abbott representatives “reviewed the paper” [BENEDICT paper]. No mention of such support/review was made in the article describing retinopathy outcomes |
| Chase | ||
| Methods |
Study design: parallel group RCT Unit of randomization and analysis: individual Number randomized - Total: 16 Per group: 7 to captopril; 9 to placebo Sample size calculation: none reported |
|
| Participants |
Country: USA Age: mean (SD): 22 (8.4) years in the captopril group and 19.9 (4.4) years in the placebo group Gender: none in captopril group and 4 (44%) in placebo group were women Race/ethnicity: not reported Inclusion criteria: insulin-dependent type 1 diabetes, with an albumin excretion rate of 20 to 200 μg/min on 3 of 4 overnight urine collections Exclusion criteria: not otherwise reported Participants’ status at baseline: Blood pressure control: captopril: 118/78 mmHg (10.2/6.1); placebo: 113/78 mmHg (10.2/7.2) Type of diabetes: type 1 HbA1c categories/levels: mean (SD): 8.8 (1.6) captopril; 8.0 (1.1) placebo Severity of diabetic retinopathy: based on modified Airlie House system--1 (no microaneurysm or other diabetic retinopathy lesion) to 6 (PDR); captopril group: 0 with grade 1; 1 with grade 2; 2 with grade 3; 3 with grade 4 Placebo group: 3 with grade 1; 3 with grade 2; 1 with grade 3; 1 with grade 4, and 1 with grade 6 |
|
| Interventions |
Intervention 1: captopril 50 mg twice a day for 2 years Intervention 2: placebo for 2 years Length of follow-up: Planned: 2 years Actual: 2 years |
|
| Outcomes |
Primary outcome, as defined for this review: worsening of diabetic retinopathy defined as any change from baseline to 2 years by 1 or more grades using the modified Airlie House classification based on 7-field color photographs Secondary outcomes, as specified for this review: visual acuity and progression to CSME not reported; grade 6 represented PDR Other diabetic retinopathy outcomes: improvement of diabetic retinopathy by 1 or more grades Eye examined for the outcome: participant’s worse eye Intervals at which outcomes were assessed: 6- to 12-month intervals Cost of the interventions: not reported Quality of life: not reported Other outcomes reported from the study: albumin excretion rate and creatinine clearance rate |
|
| Notes |
Sources of funding: partial support from industry, foundation, and government Declaration of interest: not reported Class(es) of anti-hypertensive agents compared: ACE inhibitor only Degree of blood pressure control: no target blood pressure reported; 2-year follow-up blood pressure was similar to baseline blood pressure |
|
| Risk of bias | ||
| Bias | Authors’ judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | “The subjects were randomized in a double-blind study design.” |
| Allocation concealment (selection bias) | Unclear risk | Not mentioned. |
| Masking (performance bias and detection bias) Primary outcomes |
Unclear risk | “double-blind study design” |
| Incomplete outcome data (attrition bias) Primary outcome |
Low risk | Data reported for all 16 participants. |
| Selective reporting (reporting bias) | Unclear risk | Unclear with available information. |
| Other bias | Unclear risk | “Supported in part by Bristol-Myers Squibb Company.” Too little information reported regarding methods to classify as “low risk.” |
| DEMAND | ||
| Methods |
Study design: parallel group RCT Unit of randomization and analysis: individual Number randomized - Total: 380; 258 consented to central funduscopy Per group: 90 to manidipine + delapril; 81 to delapril; and 87 to placebo Sample size calculation: target of 342 which would give 80% power with 20% “nonassessable” |
|
| Participants |
Country: Italy and Slovenia Study period: May 2002 to June 2005 Age: mean (SD): 60.2 (7.8) years in the manidipine + delapril group; 61.9 (7.8) years in the delapril group; and 60.4 (7.5) years in the placebo group Gender: 38% in the manidipine + delapril group; 35% in the delapril group; and 31% in the placebo group were women Race/ethnicity: not reported Inclusion criteria: > 40 years of age with hypertension and known history of type 2 diabetes (WHO criteria); < 25 years of duration, with urinary albumin excretion < 200 μg/min in > 2 of 3 consecutive, sterile overnight samples, and serum creatinine < 1.5 mg/dL; hypertension was defined as untreated SBP/DBP >130/85 mmHg or concomitant anti-hypertensive therapy Exclusion criteria: HbA1c > 11%, ischemic kidney disease, urinary tract obstruction, or urinary abnormalities suggestive for primary glomerular disease, or specific indications or contraindications to ACE inhibitor or calcium channel blocker therapy Participants’ status at baseline: Blood pressure control: Target: SBP/DBP < 120/80 mmHg Manidipine + delapril: 148 ± 15/87 ± 9 mmHg Delapril: 147 ± 14/87 ± 8 mmHg Placebo: 147 ± 14/88 ± 10 mmHg Type of diabetes: type 2 HbA1c categories/levels: 6.2 to 6.3 (1.7) Severity of diabetic retinopathy: 208 without diabetic retinopathy at baseline who also had fundoscopy follow-up |
|
| Interventions |
Intervention 1: manidipine (10 mg/day) + delapril (30 mg/day) Intervention 2: delapril (30 mg/day) Intervention 3: placebo Length of follow-up: Planned: 3 years (last randomized patient followed for 3 years) Actual: 3.8 years (median) (IQR: 3.1 to 4.7 years) |
|
| Outcomes |
Primary outcome, as specified for this review: new onset or progression of retinopathy: retinal involvement was graded from no apparent retinopathy to mild, moderate, or severe pre-proliferative retinopathy and to PDR; new-onset retinopathy was diagnosed when any grade of retinopathy was observed in 2 consecutive evaluations in eyes with no retinopathy at baseline. Only the combined outcome of new onset or progression of retinopathy was reported as a hazard ratio Secondary outcome, as specified for this review: visual acuity and progression to PDR or CSME not reported Other diabetic retinopathy outcomes: regression of retinopathy, both arms combined; regression was diagnosed when no retinal changes were observed in 2 consecutive evaluations in eyes with retinopathy at baseline Eye examined for the outcome: eye with the higher retinopathy grade was considered for analysis Intervals at which outcomes were assessed: retinal changes were assessed at baseline and every year after randomization Cost of the interventions: not reported Quality of life: not reported Other outcomes reported from the study: rate of glomerular filtration rate decline, composite end point of all-cause and cardiovascular mortality, and nonfatal myocardial infarction or stroke, coronary revascularization, amputation, or vascular surgery for peripheral atherosclerotic artery disease, new onset, progression, or regression of peripheral neuropathy |
|
| Notes |
Source of funding: partial support from industry: “Chiesi Farmaceutici SpA (Parma, Italy) funded the study and provided the experimental drugs but had no involvement in the study conduct and data handling, analyses, and reporting.” Declaration of interest: authors declared that they had nothing to disclose Classes of anti-hypertensive agents compared: combination of calcium channel blocker (manidipine) and ACE inhibitor (delapril) vs. ACE inhibitor alone Degree of blood pressure control: means during study 137.2 ± 10/80.5 ± 6 mmHg Concomitant treatment: additional anti-hypertensive drugs were allowed to achieve target blood pressure in the following steps: 1) hydrochlorothiazide, indapamide, or furosemide; 2) beta- or alpha-blockers; 3) doxazosis, prazosin, clonidine hydrochloride, or alpha-methyldopa |
|
| Risk of bias | ||
| Bias | Authors’ judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | “The Chiesi Farmaceutici Statistical Unit created a computer generated randomization list with a block of 6 patients assigned to each therapy with a 1:1:1 ratio.” |
| Allocation concealment (selection bias) | Low risk | “Randomization numbers were blindly assigned by the treatment assignment secretariat at the Mario Negri Institute (Ranica, Italy)…. Individual sealed envelopes containing the randomized treatment code were provided to each centre and could be broken for safety reasons after discussion with the study coordinator.” |
| Masking (performance bias and detection bias) Primary outcomes |
Low risk | “Study treatments were externally nondistinguishable orange, rounded tablets containing either delapril 15 mg plus manidipine 5 mg, delapril 15 mg, or placebo … Patients and investigators were all blinded throughout the study.” “All of the end points were adjudicated at the blind review by a clinical end point committee unaware of the treatment assignments.” |
| Incomplete outcome data (attrition bias) Primary outcome |
Low risk | “Among the 192 subjects [out of 208] without retinopathy at inclusion and with fundoscopy available on follow-up …” |
| Selective reporting (reporting bias) | Unclear risk | Incidence and progression not reported separately. |
| Other bias | High risk | Participants who discontinued medication were excluded from the final analysis; pharmaceutical company sponsor |
| DIRECT Prevent 1 | ||
| Methods |
Study design: parallel group RCT conducted as part of DIRECT Unit of randomization and analysis: individual Number randomized - Total: 1421 Per group: 711 to candesartan; 710 to placebo Sample size calculation: target of 1300 which would give 80% power to detect a 5% significance for treatment effect of 23% |
|
| Participants |
Country: 30 countries: Australia, Austria, Belgium, Bulgaria, Canada, Croatia, Czech Republic, Denmark, Estonia, France, Georgia, Germany, Greece, Hungary, Ireland, Israel, Italy, Latvia, Lithuania, Luxembourg, New Zealand, Poland, Portugal, Romania, Russian Federation, South Africa, Spain, Sweden, Turkey, United Kingdom Study period: August 2001 to February 2004 (end of randomization) with follow-up through March 2008 Age: 29.6 years in candesartan group; 29.9 years in placebo group Gender: 42% in candesartan group and 45% in placebo group were women Race/ethnicity: 97% white Inclusion criteria: type 1 diabetics without retinopathy: age 18 to 50 years, no restriction on gender, younger than 36 years of age at diagnosis of diabetes, 5 to 15 years duration, continuous insulin use within a year of diagnosis, no microalbuminuria, SBP ≤ 130 mmHg and DBP ≤ 85 mmHg and a retinal grading level of 10/10 on the ETDRS scale with 7-field stereo retinal photographs Exclusion criteria: eye conditions precluding capture of gradable retinal photographs (open-angle glaucoma, cataracts obscuring view of retina); valvular stenosis; history of heart attack or stroke; pregnant or lactating women; renal impairment defined as serum creatinine ≥ 110 μmol/L for women and ≥ 130 μmol/L for men Participants’ status at baseline: Blood pressure control: normotensive patients (≤ 130/≤ 85 mmHg) SBP at baseline: mean (SD): 116 (9.5) mmHg in candesartan group and 116 (9.6) mmHg in placebo group DBP at baseline: mean (SD): 72 (6.9) mmHg in candesartan group and 72 (7.3) mmHg in placebo group Type of diabetes: type 1 HbA1c categories/levels: mean (SD): 8.0 (1.7) in candesartan group; 8.2 (1.7) in placebo group Severity of diabetic retinopathy: all participants had ETDRS grade 10/10 (no retinopathy present) |
|
| Interventions |
Intervention 1: candesartan cilexetil 16 mg (ARB); increased in dose up to 32 mg once a day after one month based on tolerability Intervention 2: placebo Length of follow-up: Planned: 3 years Actual: 4.7 years (median; IQR 4.2 to 5.2 years) |
|
| Outcomes |
Primary outcome, as specified for this review: incidence of retinopathy defined as “a two-step progression from 10/10 on the ETDRS scale”; “two steps are defined as either a 1-step change in each eye or as a 2-step change in one eye only” Secondary outcomes, as specified for this review: PDR, CSME, and visual acuity not mentioned or reported Eye examined for the outcome: both eyes; see primary outcome description above Intervals at which outcomes were assessed: 6 months and then yearly until at least 4 years for diabetic retinopathy outcomes Cost of the interventions: not reported Quality of life: not reported Other outcomes reported from the study: change in albumin excretion rate, serum total and HDL cholesterol, and glycemic control |
|
| Notes |
Source of funding: industry Declaration of interest: all authors declared interests related to pharmaceutical companies Class(es) of anti-hypertensive agents compared: angiotensin receptor antagonist only Degree of blood pressure control: no target blood pressure levels mentioned |
|
| Risk of bias | ||
| Bias | Authors’ judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | “Randomisation is performed centrally by a computerized system.” |
| Allocation concealment (selection bias) | Low risk | “Random assignment was done centrally, using an interactive voice-response system. Both investigators and participants were unaware of the treatment allocation status.” |
| Masking (performance bias and detection bias) Primary outcomes |
Low risk | “Participants were initially assigned to candesartan 16 mg once a day or matching placebo.” “Two independent observers, a primary and secondary grader, constituting a team, were assigned to each patient for the duration of the study at the Retinopathy Grading Centre, Imperial College, London, UK. The team assessed the photographs for diabetic retinopathy and clinically significant macular oedema; they were unaware of the treatment the patients were assigned to.” |
| Incomplete outcome data (attrition bias) Primary outcome |
Low risk | Intention-to-treat analysis for all participants randomized. Reasons and percent discontinued similar in both treatment groups. Imputation used from previous photographs when photographs missed |
| Selective reporting (reporting bias) | Low risk | Low risk for retinopathy outcomes. |
| Other bias | Unclear risk | “This study was jointly funded by AstraZeneca and Takeda.” ”The sponsors did the statistical analysis, with validation by an independent statistician.” No further details on independent validation |
| DIRECT Protect 1 | ||
| Methods |
Study design: parallel group RCT conducted as part of DIRECT Unit of randomization and analysis: individual Number randomized - Total: 1905 Per group: 951 to candesartan and 954 to placebo Sample size calculation: target of 1850 which would give 80% power to detect a 5% significance for treatment effect of 25% |
|
| Participants |
Country: 30 countries; Australia, Austria, Belgium, Bulgaria, Canada, Croatia, Czech Republic, Denmark, Estonia, France, Georgia, Germany, Greece, Hungary, Ireland, Israel, Italy, Latvia, Lithuania, Luxembourg, New Zealand, Poland, Portugal, Romania, Russian Federation, South Africa, Spain, Sweden, Turkey, United Kingdom Study period: August 2001 to February 2004 (end of randomization) with follow-up through March 2008 Age: 31.5 years in candesartan group and 31.9 years in placebo group Gender: 43% in candesartan group and 42% in placebo group were women Race/ethnicity: 98% white Inclusion criteria: age 18 to 55 years, no restriction on gender, younger than 36 years of age when type 1 diabetes diagnosed, duration of 1 to 20 years, continuously used insulin within a year of diagnosis, no microalbuminuria, SBP ≤ 130 mmHg and DBP ≤ 85 mmHg and a diabetic retinopathy grading ≥ 20/10 (mild, non-proliferative), up to ≤ 47/47 (moderately severe non-proliferative) on the ETDRS scale based on 7-field stereo retinal photographs Exclusion criteria: eye conditions precluding capture of gradable retinal photographs (open-angle glaucoma, cataracts obscuring view of retina), patients with valvular stenosis, history of heart attack or stroke, pregnant or lactating women, patients with renal impairment defined as serum creatinine ≥ 110 μmol/L for women and ≥ 130 μmol/L for men, Participants’ status at baseline: Blood pressure control: normotensive patients (< 130/< 85 mmHg) SBP at baseline: mean (SD): 117 (9.6) mmHg in candesartan group and 117 (9.8) mmHg in placebo group DBP at baseline: mean (SD): 74 (6.5) mmHg in candesartan group and 73 (6.9) mmHg in placebo group Type of diabetes at baseline: type 1 HbA1c categories/levels: mean (SD) was 8.5 (1.6) in candesartan group and placebo group Severity of diabetic retinopathy (worse eye): in the candesartan group 49% with ETDRS grade of 20 (microaneurysms only), 41% with grade of 35 (mild NPDR), and 10% with grade > 35 to 47 (moderate, moderately severe, or severe NPDR); in the placebo group 49% with grade of 20, 43% with grade > 35 to 47, and 8% had grades > 35 |
|
| Interventions |
Intervention 1: candesartan cilexetil 16 mg (ARB); increased in dose up to 32 mg once a day after one month based on tolerability Intervention 2: placebo Length of follow-up: Planned: 3 years Actual: 4.8 years (median; IQR 4.4 to 5.3 years) |
|
| Outcomes |
Primary outcome, as specified for this review: progression of retinopathy defined as a 3-step change or more in ETDRS levels, e.g. at least 2 steps in 1 eye and 1 step in the other or at least 3 steps in 1 eye Secondary outcomes, as specified for this review: incidence of CSME and/or PDR per the ETDRS protocol Eye examined for the outcome: both eyes; see primary outcome description above Intervals at which outcomes were assessed: 6 months and yearly thereafter for at least 4 years for retinopathy outcomes Cost of the interventions: not reported Quality of life: not reported Other outcomes reported from the study: change in albumin excretion rate, serum total and HDL cholesterol, and glycemic control |
|
| Notes |
Sources of funding: industry Declaration of interest: all authors declared interests related to pharmaceutical companies Class(es) of anti-hypertensive agents compared: angiotensin receptor antagonist only Degree of blood pressure control: no target blood pressure levels mentioned |
|
| Risk of bias | ||
| Bias | Authors’ judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | “Randomisation is performed centrally by a computerized system.” |
| Allocation concealment (selection bias) | Low risk | “Random assignment was done centrally, using an interactive voice-response system. Both investigators and participants were unaware of the treatment allocation status.” |
| Masking (performance bias and detection bias) Primary outcomes |
Low risk | “Participants were initially assigned to candesartan 16 mg once a day or matching placebo.” “Two independent observers, a primary and secondary grader, constituting a team, were assigned to each patient for the duration of the study at the Retinopathy Grading Centre, Imperial College, London, UK. The team assessed the photographs for diabetic retinopathy and clinically significant macular oedema; they were unaware of the treatment the patients were assigned to.” |
| Masking (performance bias and detection bias) Secondary outcomes |
Low risk | Same as above. |
| Incomplete outcome data (attrition bias) Primary outcome |
Low risk | Intention-to-treat analysis reported for all participants randomized. Reasons and percent discontinued similar in both treatment groups. Imputation for missed photographs based on previous photograph |
| Incomplete outcome data (attrition bias) Secondary outcomes |
Low risk | Intention-to-treat analysis with imputation for all participants randomized. Reasons and percent discontinued similar in both treatment groups |
| Selective reporting (reporting bias) | Low risk | “Low risk” for retinopathy outcomes. |
| Other bias | Unclear risk | “This study was jointly funded by AstraZeneca and Takeda.” “The sponsors did the statistical analysis, with validation by an independent statistician.” No further details on independent validation |
| DIRECT Protect 2 | ||
| Methods |
Study design: parallel group RCT Unit of randomization and analysis: individual Number randomized - Total: 1905 Per group: 951 to candesartan; 954 to placebo Sample size calculation: target of 1700 followed at least 3 years which would give 80% power to detect a 5% significance for treatment effect of 27% for 3-step or more progression |
|
| Participants |
Country: 30 countries: Australia, Austria, Belgium, Bulgaria, Canada, Croatia, Czech Republic, Denmark, Estonia, France, Georgia, Germany, Greece, Hungary, Ireland, Israel, Italy, Latvia, Lithuania, Luxembourg, New Zealand, Poland, Portugal, Romania, Russian Federation, South Africa, Spain, Sweden, Turkey, United Kingdom Study period: August 2001 to February 2004 (end of randomization) and March 2008 (end of follow-up) Age: mean was 56.9 years in candesartan group; 56.8 years in placebo group Gender: 51% in candesartan group and 49% in placebo group were women Race/ethnicity: 96% white Inclusion criteria: age 37 to 75 years, no restriction on gender, onset at 36 years of age or older, type 2 diabetes for 1 to 20 years, no microalbuminuria, SBP ≤ 130 mmHg and DBP ≤ 85 mmHg or treated for hypertension with SBP ≤ 160 mmHg and DBP ≤ 90 mmHg, and a retinopathy grading level from ≥ 20/10 (mild non-proliferative) up to ≤ 47/47 (moderately severe non-proliferative) on the ETDRS scale based on 7-field stereo retinal photographs Exclusion criteria: eye conditions precluding capture of gradable retinal photographs (angle closure glaucoma, dense cataracts), valvular stenosis, recent heart attack or stroke, pregnant or lactating women, renal impairment (serum creatinine ≥ 110 μmol/L for women and ≥ 130 μmol/L for men, or taking renin angiotensin system inhibitors) Participants’ status at baseline: Blood pressure control: Normotensive patients: SBP at baseline: mean (SD): 123 (8.7) mmHg in candesartan group and 123 (9.0) mmHg in placebo group DBP at baseline: mean (SD): 75 (6.4) mmHg in candesartan group and 76 (6.5) mmHg in placebo group Treated hypertensive patients: SBP at baseline: mean (SD): 139 (12.7) mmHg in candesartan group and 139 (12.0) mmHg in placebo group DBP at baseline: mean (SD): 79 (6.9) mmHg in candesartan group and 80 (7.1) mmHg in placebo group Type of diabetes: type 2 HbA1c categories/levels: mean (SD) was 8.2 (1.6) overall Severity of diabetic retinopathy: ETDRS scale (overall %): diabetic retinopathy absent, 10 (0.3); microaneurysms only, 20 (25.6); mild NPDR, 35 (54.3); mild, moderate, moderately severe NPDR, > 35 to 47 (16.9) |
|
| Interventions |
Intervention 1: candesartan cilexetil 16 mg (ARB) increased in dose up to 32 mg once a day after one month based on tolerability Intervention 2: placebo Length of follow-up: Planned: 3 or more years Actual: 4.7 years (median) |
|
| Outcomes |
Primary outcome, as specified for this review: progression of retinopathy defined as a 3-step change or more in ETDRS levels, e.g. at least 2 steps in 1 eye and 1 step in the other or at least 3 steps in 1 eye; overall change in retinopathy levels from baseline to final visit Secondary outcomes, as specified for this review: incidence of CSME and/or PDR per the ETDRS protocol; visual acuity not reported Eye examined for the outcome: both eyes; see primary outcome description above Intervals at which outcomes were assessed: retinal photographs at 6 months, 1 year, and every year thereafter Cost of interventions: not reported Quality of life: not reported Other outcomes reported from the study: change in albumin excretion rate, serum total and HDL cholesterol, and glycemic control |
|
| Notes |
Sources of funding: industry Declaration of interest: all authors declared interests related to pharmaceutical companies Class(es) of anti-hypertensive agents compared: angiotensin receptor antagonist only Degree of blood pressure control: reduction in blood pressure in both groups; mean changes were 4.3/2.5 mmHg in the candesartan group and 2.9/1.3 mmHg in the placebo group |
|
| Risk of bias | ||
| Bias | Authors’ judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | “Randomisation is performed centrally by a computerized system.” |
| Allocation concealment (selection bias) | Low risk | “Random assignment was done centrally, using an interactive voice-response system. Both investigators and participants were unaware of the treatment allocation status.” |
| Masking (performance bias and detection bias) Primary outcomes |
Low risk | “Participants were initially assigned to candesartan 16 mg once a day or matching placebo.” “Two grading teams of independent observers, each consisting of a primary and a secondary grader, were assigned to each patient for the duration of the study at the Retinopathy Grading Centre, Imperial College London, UK. Graders, who were unaware of treatment allocation, assessed all photographs for retinopathy.” |
| Masking (performance bias and detection bias) Secondary outcomes |
Low risk | Same as for primary outcome. |
| Incomplete outcome data (attrition bias) Primary outcome |
Low risk | Intent-to-treat analysis for all randomized participants. Reasons for discontinuation and percent discontinued were similar in the two groups. Time-to-event analysis. Missed photograph grades imputed from previous photograph grades |
| Incomplete outcome data (attrition bias) Secondary outcomes |
Low risk | Intent-to-treat analysis done on all randomized patients. Reasons for discontinuation and percent discontinued seem similar in the two groups. Time-to-event analysis. Imputation for retinopathy outcomes |
| Selective reporting (reporting bias) | Low risk | Low risk for retinopathy outcomes. |
| Other bias | Unclear risk | ”This study was jointly funded by AstraZeneca and Takeda.” “The sponsors did the statistical analysis, with validation by an independent statistician.” The authors had full access to all data and were free to interpret data and draw conclusions |
| EUCLID | ||
| Methods |
Study design: parallel group RCT Unit of randomization and analysis: individual Number randomized - Total: 530; 409 had gradable baseline photographs; 354 had baseline and follow-up retinal photographs Per group: 265 to each group (lisinopril and placebo); for retinopathy outcomes: 202 lisinopril, 207 placebo, in which 175 in the lisinopril group and 179 in the placebo group were analyzed Sample size calculation: target of 580 (500 with follow-up) which would give 80% power to detect a 28% reduction in retinopathy progression |
|
| Participants |
Countries: Austria, Belgium, Croatia, Finland, Greece, Hungary, Ireland, Italy, Luxembourg, Poland, Romania, United Kingdom Study period: not reported Age: mean (SD) of 34 (9) years in lisinopril group, 35 (8) years in placebo group Gender: 36.7% in lisinopril group and 33% in placebo group were women Race/ethnicity: not reported Inclusion criteria: men and women (on contraception or postmenopausal) aged 20 to 59 years, IDDM defined as diagnosis before 36 years of age and continuous insulin required within 1 year of diagnosis, resting DBP 75 to 90 mmHg, SBP ≤ 155 mmHg Exclusion criteria: renal artery stenosis, cardiac valve obstruction, accelerated hypertension, recent myocardial infarction, CABG, stroke, CHF, abnormal renal function (creatinine > 1.8 mg/dL), postural hypotension, or idiosyncratic reactions to ACE inhibitors Participants’ status at baseline: Blood pressure control: mean (SD): SBP 123 (10) mmHg in lisinopril group, 123 (11) mmHg in placebo group; DBP 81 (5) mmHg in both lisinopril and placebo groups Type of diabetes: type 1 HbA1c categories/levels: median (IQR): 6.9 (1.9) for lisinopril and 7.3 (1.9) for placebo group |
|
| Interventions |
Intervention 1: 10 mg/day lisinopril, which could be increased to 20 mg/day at 3 months and at subsequent visits to achieve a target DBP < 75 mmHg Intervention 2: placebo Length of follow-up: Planned: 2 years Actual: 2 years for those analyzed |
|
| Outcomes |
Primary outcome, as specified for this review: incidence of retinopathy and retinopathy progression by at least 2 levels; retinal photographs at baseline and 24 months; classification was on a 5-level scale, using the EURODIAB diabetic retinopathy classification from photos Secondary outcomes, as specified for this review: progression to PDR; CSME and visual acuity not reported Other diabetic retinopathy outcomes: retinopathy progression by 1 level Eyes examined for the outcome: both eyes, but whether average of two eyes was analyzed or whether two eyes were analyzed separately was unclear Intervals at which outcomes were assessed: retinal photographs taken at baseline and at 24 months; unclear whether photographs were taken at other follow-up visits Cost of interventions: not reported Quality of life: not reported Other outcomes reported from the study: change in albumin excretion rate and HbA1c |
|
| Notes |
Sources of funding: industry Declaration of interest: not reported Run-in length: 1 month run-in on placebo; 70% adherence required for eligibility Class(es) of anti-hypertensive agents compared: ACE inhibitor only Degree of blood pressure control: mean DBP near target in lisinopril group |
|
| Risk of bias | ||
| Bias | Authors’ judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | “Randomisation was stratified by centre and albuminuric status.” “Patients were randomly assigned to lisinopril or placebo with a block size of four. Separate schemes were created for each stratum (microalbuminuric and normoalbuminuric), with a FORTRAN computer program validated against the SAS RANUNI random-number generator. This scheme was generated by Zeneca Pharmaceuticals, so that both the coordinating centre and the local investigators were unaware of the allocation.” |
| Allocation concealment (selection bias) | Low risk | “Local investigators telephoned the coordinating centre with the provisional albuminuric status, and were given an identification number that matched numbers on pill boxes.” “This scheme was generated by Zeneca Pharmaceuticals, so that both the coordinating centre and the local investigators were unaware of the allocation. Sealed envelopes were supplied to each centre and the coordinating centre so that the code could be broken in an emergency.” |
| Masking (performance bias and detection bias) Primary outcomes |
Low risk | “AKS assessed all photographs according to the EURODIAB protocol, based on the modified Airlie House classification. She had no access to information about patients, except study number.” |
| Masking (performance bias and detection bias) Secondary outcomes |
Low risk | Same as above. |
| Incomplete outcome data (attrition bias) Primary outcome |
Unclear risk | Analysis based on 325 participants who had 2-year photographs of 409 randomized participants. Reasons for missed photographs were similar in 2 groups |
| Incomplete outcome data (attrition bias) Secondary outcomes |
Unclear risk | Same as above. |
| Selective reporting (reporting bias) | Unclear risk | Unclear with available information. |
| Other bias | Unclear risk | “This study was supported by a grant from Zeneca Pharmaceuticals, who also provided the lisinopril and placebo tablets.” Also, the company generated the randomization scheme |
| Pradhan | ||
| Methods |
Study design: parallel group RCT Unit of randomization and analysis: individual Number randomized - Total: 40 (35 included in the analysis) Per group: 18 to enalapril; 17 to multivitamin Sample size calculation: not reported |
|
| Participants |
Country: USA Study period: April 1997 through June 1998 Age: mean: 49.3 years in enalapril group; 53.4 years in multivitamin group Gender: 50% in enalapril group and 58.8% in placebo group were women Race/ethnicity: not reported Inclusion criteria: type 2 diabetes, normotensive (< 140/90 mmHg), not on any ACE inhibitors or anti-hypertensive agents, moderate or severe NPDR identified and graded as ≥ 40 to 50 level of modified Airlie House classification (ETDRS), 7-field stereoscopic photos to confirm diabetic retinopathy severity Exclusion criteria: abnormal serum creatinine, visual acuity < 20/50, dipstick proteinuria more than trace, treatment with ACE inhibitors or other anti-hypertensive medications Participants’ status at baseline: Blood pressure control: all were < 140/90; mean arterial pressures were 91.3 in enalapril group and 89.1 in multivitamin group Type of diabetes: type 2 HbA1c categories/levels: mean was 10.6 for both groups Retinopathy status: all had moderate or severe NPDR |
|
| Interventions |
Intervention 1: 5 mg enalapril daily Intervention 2: multivitamin placebo daily Length of follow-up: Planned: 2 years Actual: 7.1 months (mean; range: 3 to 15 months) |
|
| Outcomes |
Primary outcome, as specified for this review: neither incidence nor progression of diabetic retinopathy reported Secondary outcomes, as specified for this review: progression to PDR or macular edema requiring laser treatment based on slit-lamp examination; PDR, when detected ophthalmoscopically, was documented by 7-field photos; visual acuity measured but not reported Intervals at which outcomes were assessed: all participants had retinal photographs taken at 1 and 2 years; slit-lamp assessment every 3 months Eyes examined for outcome: both eyes, but whether average of two eyes was analyzed or whether two eyes were analyzed separately not stated Cost of interventions: not reported Quality of life: not reported |
|
| Notes |
Source of funding: government agency Declaration of interest: not reported Class(es) of anti-hypertensive agents compared: ACE inhibitors only Degree of blood pressure control: not reported Other: terminated with mean follow-up less than 1 year for “unlikelihood” of demonstrating a significant difference between ACE inhibitor and placebo in the study cohort |
|
| Risk of bias | ||
| Bias | Authors’ judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | “After randomization to either a multivitamin (MVI) placebo or an ACE-I …”; details of sequence generation not reported |
| Allocation concealment (selection bias) | Unclear risk | Not reported. |
| Masking (performance bias and detection bias) Secondary outcomes |
High risk | PDR and CSME reported at 3-month intervals based on slit-lamp examination by ophthalmologist for whom masking was not mentioned |
| Incomplete outcome data (attrition bias) Secondary outcomes |
High risk | “One woman had an allergic reaction and was dropped from the study. Four patients did not return for the 3-month evaluation and were also dropped from the study since they could not be contacted.” Treatment arm not specified for dropouts. Also, study terminated early for futility |
| Selective reporting (reporting bias) | Unclear risk | Unclear from available information, but visual acuity measured at 3-month intervals and not reported |
| Other bias | High risk | Terminated prematurely for futility; less than 1-year follow-up inadequate to assess diabetic retinopathy outcomes in so few participants |
| RASS | ||
| Methods |
Study design: parallel group RCT Unit of randomization and analysis: individual Number randomized - Total: 285 in the trial; 223 analyzed for retinopathy outcome Per group: 94 to enalapril, 96 to losartan, 95 to placebo; 77 enalapril, 72 losartan, 74 placebo analyzed for retinopathy Sample size calculation: target of 95 participants per each of 3 arms which would give 80% power to detect a two-sided 5% significance for treatment effect of 50% decrease in rate of change in mesangial fractional volume per glomerulus with 10% dropout; “RASS trial may not have adequate statistical power to detect small effects of RAS blockade on DR” |
|
| Participants |
Country: Canada and the USA Study period: not reported; design published in 2002 Age: mean (SD): 30.6 (10) years in enalapril group; 29.3 (10.2) years in losartan group; 29.1 (9.1) years in placebo group Gender: 52% in enalapril group; 54% in losartan group; 55% in placebo group were women Race/ethnicity: 98% white Inclusion criteria: age 18 years or older; type 1 diabetes defined as onset before the patient’s 45th birthday; BMI < 26 kg/m2 along with a positive glutamate decarboxylase or islet cell antibody test at time of diagnosis if between 31 and 40 years of age; no evidence of renal disease; participants who did not have PDR at baseline and who had fundus photographs at both baseline (defined as within 1 year after randomization) were included in analyses for diabetic retinopathy Exclusion criteria: evidence of renal disease; blood pressure > 135/85 mmHg or requiring anti-hypertensive medications; albumin excretion rate > 20 μg/min; pregnancy; failure to take at least 85% of placebo pills during a 2-week run-in period; and glomerular filtration rate < 90 mL/min/1.73 m2 of body surface area Participants’ status at baseline: Blood pressure control: Mean (SD) of SBP at baseline: 120 (13) mmHg in enalapril group; 120 (11) mmHg in losartan group; 119 (11) mmHg in placebo group Mean (SD) of DBP at baseline: 71 (8) mmHg in enalapril group; 70 (8) mmHg in losartan group; 70 (8) mmHg in placebo group Type of diabetes: type 1 HbA1c categories/levels: mean (SD): 8.6 (1.6) in enalapril group; 8.7 (1.7) in losartan group; 8.3 (1.4) in placebo group Severity of retinopathy (worse eye): no retinopathy (10): 34%; minimal NPDR (21): 40%; early NPDR (31–37): 18%; moderate/severe NPDR (43–53): 9% |
|
| Interventions |
Intervention 1: enalapril (ACE inhibitor) 10 mg + ‘losartan’ placebo daily Intervention 2: losartan (ARB) 50 mg + ‘enalapril’ placebo daily Intervention 3: ‘enalapril’ and ‘losartan’ placebos daily 40 months after first randomization, doses for the interventions were doubled owing to evidence suggesting that the reduction in proteinuria was greater with higher doses of study treatments; the treatments were increased to 20 mg enalapril and 100 mg losartan by doubling the number of pills taken each day Length of follow-up: Planned: 5 years Actual: 5 years |
|
| Outcomes |
Primary outcome, as specified for this review: retinopathy progression by 2 steps; diabetic retinopathy grade “derived by concatenating the grades of the two eyes in which the eye with the higher grade given greater weight”; only the combined outcome of incidence and progression reported Secondary outcomes, as specified for this review: as above for PDR and CSME; visual acuity not reported Other diabetic retinopathy outcomes: incidence of diabetic retinopathy by 3 steps Eye examined for outcome: participant’s worse eye Intervals at which outcomes were assessed: retinal photographs taken at baseline, midpoint, and conclusion of the study Cost of interventions: not reported Quality of life: not reported Other outcomes reported from the study: change in mesangial fractional volume, albumin excretion rate, and glomerular filtration rate |
|
| Notes |
Sources of funding: industry and government Declaration of interest: several authors declared interests related to pharmaceutical companies Run-in length: 2 weeks on placebo Class(es) of anti-hypertensive agents compared: ACE inhibitor and ARB Degree of blood pressure control: < 120/80 during follow-up Other: only 223 participants were analyzed for retinopathy outcomes; 28 with no base-line photographs, 4 with baseline PDR, 30 with no 5-year photographs were excluded from analysis for retinopathy outcomes |
|
| Risk of bias | ||
| Bias | Authors’ judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | “Patients were randomly assigned to one of three groups with the use of computer-generated blocks of six and stratified according to centre and sex …” |
| Allocation concealment (selection bias) | Unclear risk | Not reported. |
| Masking (performance bias and detection bias) Primary outcomes |
Low risk | “These [stereoscopic fundus photographs] were graded by observers, unaware of the study-drug assignments, at the University of Wisconsin Ocular Epidemiology Reading Center who used the modified Airlie House …” |
| Masking (performance bias and detection bias) Secondary outcomes |
Low risk | Same as above. |
| Incomplete outcome data (attrition bias) Primary outcome |
Unclear risk | “… use of multiple imputation techniques to assess effects of patients excluded for not having both the baseline and 5-year … diabetic retinopathy grades, respectively.” Patients without baseline photographs were excluded from the analyses |
| Incomplete outcome data (attrition bias) Secondary outcomes |
Unclear risk | See above for details of multiple imputation for missing retinal photographs at 5-year follow-up |
| Selective reporting (reporting bias) | Low risk | Unclear from available information. Retinopathy assessment is the only pertinent outcome described in Mauer 2002 paper |
| Other bias | Unclear risk | Partially supported by industry. Baseline retinal photographs were taken after randomization for 45.3% of the participants (mean time to baseline photographs was 4.8 ± 4.8 months after randomization for these participants). 32 participants were excluded: 4 with baseline PDR and 28 (of 285) without baseline photographs within 1 year after randomization. Not stated, but 30 more not analyzed for retinopathy, presumably because follow-up photographs not taken |
| Steno-2 | ||
| Methods |
Study design: parallel group RCT Unit of randomization and analysis: individual Number randomized - Total: 160 Per group: 80 per group Sample size calculation: target of 128 which would give 90% power to detect a 5% significance for treatment effect of 23% difference in urinary albumin excretion rate |
|
| Participants |
Country: Denmark Study period: enrollment 1992 to 1993; total study period 1992 to 1997 Age: mean (SD) 54.9 (7.2) years in intensive therapy and 55.2 (7.2) years in standard therapy Gender: 21% in intensive therapy and 30% in standard therapy were women Race/ethnicity: not reported Inclusion criteria: albumin excretion rate 30 mg to 300 mg in 4 of 6 24-hour overnight samples, type 2 diabetes diagnosed by 1985 WHO criteria, age between 40 and 65 years Exclusion criteria: simulated serum C peptide concentration < 600 pmol/L 6 minutes after 1 m IV glucagon injection, pancreatic insufficiency, diabetes secondary to pancreatitis, alcohol abuse, non-diabetic kidney disease, malignancy or life-threatening disease probable within 4 years Participants’ status at baseline: Blood pressure control: mean (SD): SBP 146 (20) mmHg in intensive therapy and 149 (19) mmHg in standard therapy; DBP 85 (10) mmHg in intensive therapy and 86 (11) mmHg in standard therapy Type of diabetes: type 2 HbA1c categories/levels at baseline: mean (SD) 8.4 (1.6) intensive therapy and 8.8 (1. 7) standard therapy Severity of retinopathy: NPDR: 22% intensive therapy and 20% in standard therapy PDR/photocoagulation: 4% intensive therapy and 8% standard therapy |
|
| Interventions |
Intervention 1: multifactorial; all participants in intensive therapy group received ACE inhibitor equivalent to 50 mg two times a day captopril irrespective of blood pressure with additional intensive therapy for hypertension for a goal SBP < 140 and DBP < 85; vitamin C 250 mg/day for nonsmokers and 1250 mg/day for smokers; vitamin E 100 mg/day for nonsmokers and 500 mg/day for smokers; aspirin 150 mg/day; instructions to limit daily fat intake to < 30% and saturated fat intake to < 10%; light to moderate exercise for 30 minutes, 5 times a week; smoking cessation; metformin 1 g twice a day if BMI > 25; NPH insulin if HbA1c > 7%. Anti-hypertensive therapy was initiated in a stepwise fashion starting with ACE inhibitors, progressing to AT-2 blockers, thiazides, calcium antagonists, and beta-blockers as needed Intervention 2: standard treatment by participants’ medical practitioners based on 1998 Danish guidelines with goal SBP < 160 mmHg and DBP < 95 mmHg Length of follow-up: Planned: 4 years Actual: 3.8 years mean (SD = 0.3 year) |
|
| Outcomes |
Primary outcome, as specified for this review: incidence of retinopathy; progression of retinopathy defined as at least 1 level in either eye; retinal photographs of 2 45° to 50° fields (macula-temporal and disc-nasal) of each eye with pupils dilated and graded according to EURODIAB 6-level grading scale Secondary outcomes, as specified for this review: progression to PDR or maculopathy Other diabetic retinopathy outcomes: blindness in 1 eye by WHO criteria or worse than 6/60 Eye examined for outcome: both eyes, but whether average of two eyes was analyzed or whether two eyes were analyzed separately was not stated Intervals at which outcomes were assessed: retinopathy assessed at baseline and every 2 years Cost of interventions: EUR2538 per quality adjusted life expectancy with multifactorial intensive treatment Quality of life: not reported Other outcomes reported from the study: urinary albumin excretion |
|
| Notes |
Sources of funding: unclear; the cost-effectiveness analysis was supported by the Steno Diabetes Center and Novo Nordisk A/S Declaration of interest: not reported Class(es) of anti-hypertensive agents compared: not applicable Degree of blood pressure control: blood pressure in intensive therapy group dropped by 14 (2)/12 (2)mmHg by “end of study” compared with 3 (3)/8 (2)mmHg in conventional therapy group Other: denominators for retinopathy analysis unclear given some PDR and photocoagulation at baseline |
|
| Risk of bias | ||
| Bias | Authors’ judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | “Concealed randomisation was done in groups of four with two in each treatment arm and thus allowed a maximum difference of two patients per group per stratum. ” |
| Allocation concealment (selection bias) | High risk | “Concealed randomisation …,” but treatments not masked so some assignments in each block of 4 could be known |
| Masking (performance bias and detection bias) Primary outcomes |
Low risk | Interventions compared in the trial do not allow masking of participants and personnel; however, the “photographs were graded by two independent ophthalmologists, masked to treatment allocation …” |
| Masking (performance bias and detection bias) Secondary outcomes |
Low risk | “The photographs were graded by two independent ophthalmologists, masked to treatment allocation …” |
| Incomplete outcome data (attrition bias) Primary outcome |
Unclear risk | Analyzed as randomized but withdrawals and deaths excluded from analyses. No imputation or accounting for censoring |
| Incomplete outcome data (attrition bias) Secondary outcomes |
Unclear risk | Analyzed as randomized but withdrawals and deaths excluded from analyses. No imputation or accounting for censoring |
| Selective reporting (reporting bias) | Unclear risk | Unclear with available information. |
| Other bias | Unclear risk | Sources of funding not reported. |
| UKPDS/HDS | ||
| Methods |
Study design: parallel group RCT Unit of randomization and analysis: individual Number randomized - Total: 1148 for TBP control policy versus LTBP control policy Per group: 758 to TBP control policy (400 to captopril and 358 to atenolol as main therapy), 390 to LTBP control policy Sample size calculation: none found in more than 50 study publications for TBP control versus LTBP control or captopril versus atenolol |
|
| Participants |
Country: United Kingdom Study period: enrollment 1987 to 1991 Age: mean (SD) of 56.4 (8.1) years in TBP control group and 56.5 (8.1) in LTBP control group; mean (SD) of 56.3 (8.1) years in captopril group and 56 (8.2) years in atenolol group Gender: 46%in TBP control group and 42%in LTBP control group were women; 49% in captopril group and 43% in atenolol group were women Race/ethnicity: 87% white; 5% Asian; 8% Afro-Carribean Inclusion criteria: type 2 diabetes and participating in the UKPDS with the mean of blood pressure readings from 3 consecutive visits > 160 mmHg SBP and/or a DBP > 90 mmHg when not receiving treatment for hypertension or an SBP > 150 mmHg and/or a DBP > 85 mmHg when already receiving treatment for hypertension; participants with SBP ≥ 200 mmHg and/or DBP ≥ 105 mmHg on any single occasion were eligible for randomization; the mean of subsequent 3 consecutive readings after discarding the first was used Exclusion criteria: requirement for strict blood pressure control due to a previous stroke, accelerated hypertension, ketonuria > 3 mmol/L; cardiac or renal failure; those who required beta-blockade (myocardial infarction in the previous year or current angina); severe vascular disease with more than one major vascular episode; contraindication to beta-blockade (with conditions such as asthma, intermittent claudication, foot ulcers or amputations); and severe concurrent illness Participants’ status at baseline: Blood pressure control: TBP control vs. LTBP control (UKPDS 38): mean SBP and DBP similar in both groups; treated stratum blood pressure ≥ 150/85; untreated stratum blood pressure ≥ 160/90 ACE inhibitor vs. beta-blocker (UKPDS 39): mean SBP and DBP similar in both groups; a similar proportion of patients were on anti-hypertensive therapy before randomization Type of diabetes: type 2 HbA1c categories/levels at baseline: no categories reported, mean levels similar in both groups Severity of retinopathy: in TBP group 23% with 20 or worse (microaneurysms only; mild, moderate, moderately severe, or severe NPDR; or PDR) and 7% with 35 or worse (severe NPDR or PDR); in LTBP group 29% with 20 or worse and 10% with 35 or worse |
|
| Interventions |
TBP control vs. LTBP control Intervention 1: TBP control policy aiming for blood pressure < 150/85 mmHg with a random allocation to either an ACE inhibitor or a beta-blocker
|
|
| Outcomes |
Primary outcome, as specified for this review: progression of retinopathy defined as a 2-step or greater change in ETDRS grading (both eyes 1 step or 1 eye 2 steps) with a worse eye/better eye Secondary outcomes, as specified for this review: visual loss defined as the best vision in either eye, deteriorating by 3 lines or more on the ETDRS chart (clinical records); retinopathy grading scale included retinal photocoagulation or vitreous hemorrhage (for PDR) as the most serious grade Other diabetic retinopathy outcomes: incidence of retinopathy defined as 1 or more microaneurysms in 1 eye or worse (changed to 5 or more microaneurysms after UKPDS 50 analysis); vitreous hemorrhage; blindness in 1 eye Eye examined for outcome: both eyes; see primary outcome description above Intervals at which outcomes were assessed: baseline data from retinal photographs taken up to 3 years prior to randomization within the hypertension study component of UKPDS; analyses reported at mean intervals of 1.5, 4.5, and 7.5 years from randomization Cost of interventions: reported in UKPDS 40 and UKPDS 54 publications Quality of life: UKPDS 37: cross-sectional comparison of TBP control with LTBP control Other outcomes reported from the study: occurrence of 1) first clinical end point related to diabetes (sudden death, death from hyper- or hypoglycemia, fatal or nonfatal myocardial infarction, angina, heart failure, stroke, renal failure, amputation, vitreous hemorrhage, retinal photocoagulation, blindness in 1 eye, or cataract extraction, 2) death related to diabetes due to myocardial infarction, sudden death, stroke, peripheral vascular disease, renal disease, hyper- or hypoglycemia, (3) death from all causes |
|
| Notes |
Sources of funding: government agencies, industry, and foundations Declaration of interest: not reported Class(es) of anti-hypertensive agents compared: ACE inhibitor (captopril) vs. beta-blocker (atenolol) Degree of blood pressure control: TBP control resulted in mean blood pressure decrease 140/80 mmHg compared to LTBP 150/90 mmHg Concomitant treatments: all participants also participating in UKPDS RCT of control of blood glucose levels |
|
| Risk of bias | ||
| Bias | Authors’ judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Cited UKPDS 33, in which randomization was described as follows: “Randomisation was by means of centrally produced, computer-generated therapy allocations in sealed, opaque envelopes which were opened in sequence.” “The trial was open once patients were randomised.” “The randomization was stratified for those with or without previous therapy for hypertension.” |
| Allocation concealment (selection bias) | Low risk | “Sealed opaque envelopes were used and checked as described for the UK Prospective Diabetes Study.” The reference was to UKPDS 33 in which randomization was described as above |
| Masking (performance bias and detection bias) Primary outcomes |
Low risk | “Retinal photographs, masked for all patient-identifying details and assigned a unique identification number, were assessed initially by two independent, experienced readers for quality and adherence to protocol as well as the presence of any diabetic retinal lesions.” “Retinopathy requiring photocoagulation or vitreous hemorrhage was independently assessed and recorded throughout the study” UKPDS 69 |
| Masking (performance bias and detection bias) Secondary outcomes |
Unclear risk | As above for PDR and CSME. Unclear from report for UKPDS 69 and UKPDS VIII whether visual acuity examiners were masked |
| Incomplete outcome data (attrition bias) Primary outcome |
Low risk | “Survival function estimates were calculated using the product limit (Kaplan-Meier) method.” Participants were kept in assigned group but outcomes reported only for available cases |
| Incomplete outcome data (attrition bias) Secondary outcomes |
Low risk | Same as above |
| Selective reporting (reporting bias) | Low risk | None for retinopathy outcomes. |
| Other bias | Unclear risk | “To form the baseline data set, we used the retinal photograph taken up to 3 years prior to hypertension randomization.” Partial industry support |
ABCD (1) Appropriate Blood Pressure Control in Diabetes Trial (2 RCTs)
ACCORD EYE: Action to Control Cardiovascular Risk in Diabetes - Eye Study
ACE inhibitors: angiotensin-converting enzyme inhibitors
ADVANCE/AdRem: Action in Diabetes and Vascular Disease Retinal Measurements Study
ARB: angiotensin receptor blocker
BENEDICT: BErgamo NEphrologic DIabetes Complications Trial
BMI: body mass index
CABG: coronary artery bypass graft surgery
CCB: calcium channel blocker
CHF: congestive heart failure
CSME: clinically significant macular edema
CWS: cotton-wool spots
DBP: diastolic blood pressure
DCCT: Diabetes Control and Complications Trial
DEMAND: Delapril and Manidipine for Nephroprotection in Diabetes
DIRECT: Diabetic Retinopathy Candesartan Trials Programme Prevent 1, Protect 1, Protect 2
ETDRS: Early Treatment Diabetic Retinopathy Study
EUCLID: EURODIAB Controlled Trial of Lisinopril in Insulin-Dependent Diabetes Mellitus study
HbA1c: glycated hemoglobin
HDL: high-density lipoprotein
IDDM: insulin-dependent diabetes mellitus
IQR: interquartile range
IRMA: intraretinal microvascular abnormalities
logMAR: logarithm of the minimum angle of resolution
LTBP: less tight blood pressure
mmHg: millimeter of mercury
NPDR: non-proliferative diabetic retinopathy
NV: neovascularization
PDR: proliferative diabetic retinopathy
RASS: Renin-Angiotensin System Study
RCT: randomized controlled trial
RD: retinal detachment
SBP: systolic blood pressure
SD: standard deviation
TBP: tight blood pressure
UKPDS/HDS: United Kingdom Prospective Diabetes Study/Hypertension in Diabetes Study
WHO: World Health Organization
Declaration of interest information was sought from the primary reference of each study. For UKPDS, we did not specify any one article as the primary reference. We used information from UKPDS 33 and UKPDS 40 because we extracted most of the numbers we used in our analyses from these reports.
Study design and sample size
A majority of included trials were multicenter, with participants enrolled in North America, Europe, Asia, and Australia. Trials varied in size; the largest trial randomized 2130 participants (ADVANCE/AdRem); the smallest randomized 16 participants (Chase). In total, 4157 type 1 and 9512 type 2 diabetics were randomized in the included trials. Among the trial participants, 4036 type 1 and 8251 type 2 diabetics had baseline ophthalmic evaluations (Table 1; Table 2; Table 3). Most trials reported diabetic retinopathy outcomes only for participants who had both baseline and follow-up photographs. Two trials reported findings from randomized participants at a subset of participating centers where baseline and follow-up retinal examinations were performed (BENEDICT; DEMAND); another two trials analyzed a subset of participants randomized in a larger parent study who agreed to participate in additional retinal examinations (ACCORD EYE; ADVANCE/AdRem). Two trials were conducted within the Appropriate Blood Pressure Control in Diabetes Trial (ABCD), one for initially normotensive participants and one for hypertensive participants. For the purposes of this review, we have labeled the two trials ABCD (1) and ABCD (2), respectively. Although conducted within one parent study, DIRECT Prevent 1, DIRECT Protect 1, and DIRECT Protect 2 were designed, published, and analyzed as three RCTs.
Table 1.
Baseline characteristics of Type 1 diabetics in included studies
| Characteristic | DIRECT | EUCLID | RASS | Chase | |
|---|---|---|---|---|---|
| Prevent-1 | Protect-1 | ||||
| Number enrolled | 1421 | 1905 | 530 | 285 | 16 |
| Number analyzed | 1421 | 1905 | 354 | 223 | 16 |
| Age, years (mean) | 30 | 32 | 34 | 30 | 21 |
| Men, %1 | 57 | 58 | 65 | 47 | 75 |
| White, %1 | 97 | 98 | - | 98 | - |
| Diabetes duration, years (mean) | 6.7 | 11.0 | 14.5 | 11.2 | 12.9 |
| Current smoker, %1 | 26 | 26 | 30 | - | - |
| Systolic blood pressure (mean) | 116 | 117 | 123 | 120 | 115 |
| Diastolic blood pressure (mean) | 72 | 74 | 81 | 70 | 78 |
| Body-mass index (kg/m2; mean) | 24.0 | 24.6 | 24.7 | 25.7 | - |
| HbA1c (mean) | 8.1 | 8.5 | 7.1 | 8.5 | 8.4 |
| Retinopathy, worse eye, %2 | |||||
| Number of participants with gradeable baseline photographs | 1421 | 1905 | 354 | 223 | 16 |
| ETDRS ≤ 20: None or microaneurysms only | 100 | 49 | 38 | 34 | 44 |
| ETDRS 31 to 37: Mild non-proliferative | 0 | 42 | 41 | 56 | 25 |
| ETDRS 41 to 53: Moderate or severe non-proliferative | 0 | 9 | 12 | 9 | 25 |
| ETDRS > 53: Proliferative or panretinal photocoagulation | 0 | 0 | 8 | 0 | 6 |
Percentages based on number of participants enrolled.
Percentages based on number of participants with gradeable photographs.
- Indicates no data were available in the study publications found.
Data shown for RASS includes the number of participants analyzed for retinopathy outcomes.
Table 2.
Baseline characteristics of normotensive or treated hypertensive Type 2 diabetics in included studies
| Characteristic | DIRECT Protect 2 | ACCORD EYE | ABCD (1) | Pradhan |
|---|---|---|---|---|
| Number enrolled | 1905 | 1590 | 480 | 40 |
| Number analyzed | 1905 | 1263 | 480 | 35 |
| Age, years (mean) | 57 | 61 | 59 | 51 |
| Men, %1 | 50 | 54 | 54 | 46 |
| White, %1 | 96 | 70 | 74 | - |
| Diabetes duration, years (mean) | 8.8 | 10 | 9 | 11 |
| Current smoker, %1 | 15 | 13 | 13 | - |
| Systolic blood pressure (mean) | 133 | 138 | 136 | - |
| Diastolic blood pressure (mean) | 78 | 76 | 84 | - |
| Body-mass index (kg/m2; mean) | 29.4 | 32.4 | 31.5 | 26.9 |
| HbA1c (mean) | 8.2 | 8.3 | 11.6 | 10.6 |
| Previous myocardial infarction, %1 | 5.2 | 123 | 24 | - |
| Previous stroke, %1 | 1.4 | 3.5 | - | |
| Retinopathy, worse eye, %2 | ||||
| Number of participants with gradeable baseline photographs | 1905 | 1261 | 463 | 40 |
| ETDRS ≤ 20: None or microaneurysms only | 28 | 49 | 50 | 0 |
| ETDRS 31 to 37: Mild non-proliferative | 54 | 18 | 46 | 0 |
| ETDRS 41 to 53: Moderate or severe non-proliferative | 17 | 36 | 100 | |
| ETDRS > 53: Proliferative or pan-retinal photocoagulation | 0 | 2 | 4 | 0 |
Percentages based on number of participants enrolled.
Percentages based on number of participants with gradeable photographs.
ACCORD EYE data based number of participants in the blood pressure trial.
History of cardiovascular event.
- Indicates that specific data were not reported in the publications from the trial.
Table 3.
Baseline characteristics of hypertensive Type 2 diabetics in included studies
| Characteristic | ADVANCE/AdRem | UKPDS/HDS | BENEDICT | ABCD (2) | DEMAND | Steno-2 |
|---|---|---|---|---|---|---|
| Number enrolled | 2130 | 1148 | 1209 | 470 | 380 | 160 |
| Number analyzed | 1241 | 1148 | 550 | 470 | 258 | 149 |
| Age, years (mean) | 66 | 56 | 62 | 58 | 61 | 55 |
| Men, %1 | 61 | 55 | 54 | 68 | 65 | 74 |
| White, %1 | 48 | 87 | 99 | 66 | - | - |
| Diabetes duration, years (mean) | 6.0 | 2.6 | 7.9 | 8.6 | 6 | 5.83 |
| Current smoker, %1 | 14 | 22 | 10 | 14 | 13 | 30 |
| Systolic blood pressure (mean) | 143 | 160 | 152 | 155 | 147 | 148 |
| Diastolic blood pressure (mean) | 79 | 94 | 89 | 98 | 88 | 86 |
| Body-mass index (kg/m2; mean) | 27.7 | 29.6 | 28.7 | 31.8 | 29.6 | 29.9 |
| HbA1c (mean) | 7.4 | 6.9 | 5.9 | 11.6 | 6.2 | 8.6 |
| Previous myocardial infarction, %1 | - | - | - | - | - | - |
| Previous stroke, %1 | - | - | - | - | 3 | |
| Retinopathy, worse eye, %2 | ||||||
| Number of participants with gradeable baseline photographs | 1602 | 929 | 550 | 431 | 237 | 160 |
| ETDRS ≤ 20: None or microaneurysms only | 82 | 67 | 84 | 40 | 81 | 79 |
| ETDRS 31 to 37: Mild non-proliferative | 8 | 25 | 15 | 55 | 19 | 17 |
| ETDRS 41 to 53: Moderate or severe non-proliferative | 8 | |||||
| ET- DRS > 53: Proliferative or panretinal photocoagulation | 1 | 8 | 1 | 4 | 4 |
Percentages based on number of participants enrolled.
Percentages based on number of participants with gradeable photographs.
Median, estimated from median values of treatment arms.
- indicates that specific data were not reported in the publications from the trial.
Study participants
Type 1 diabetes
Five trials reported data for 4036 type 1 diabetics (Chase; DIRECT Prevent 1; DIRECT Protect 1; EUCLID; RASS). Participants in these trials were young (average age about 30 years) and had blood pressure in the normal range at baseline (normotensive). The majority of participants had either no retinopathy, microaneurysms only, or mild non-proliferative retinopathy at baseline. Two trials (Chase; RASS) enrolled a few participants with more severe forms of retinopathy at baseline (Table 1). Participants in EUCLID had a lower HbA1c than those in the other four trials (Table 1).
Type 2 diabetes
Ten trials reported data for 8251 type 2 diabetics. The average age of participants in these trials ranged from 51 to 66 years. Four trials reported findings for 3683 type 2 diabetics who were either normotensive or hypertensive with adequately controlled blood pressures at baseline (Table 2) (ABCD (1); ACCORD EYE; DIRECT Protect 2; Pradhan). Six trials reported findings for 4568 type 2 diabetics with hypertension at baseline (Table 3) (ABCD (2); ADVANCE/AdRem; BENEDICT; DEMAND; Steno-2; UKPDS/HDS). In addition to differences in blood pressure, other variations with respect to baseline retinopathy status, history of cardiovascular disease, and other participant characteristics were observed between normotensive or treated hypertensive and hypertensive type 2 diabetics (Table 2; Table 3).
Study interventions
Ten trials compared anti-hypertensive medication to placebo or no treatment (ADVANCE/AdRem; BENEDICT; Chase; DEMAND; DIRECT Prevent 1; DIRECT Protect 1; DIRECT Protect 2; EUCLID; Pradhan; RASS). One trial incorporated lifestyle modification in addition to anti-hypertensive medications (Steno-2). Different anti-hypertensive interventions and different anti-hypertensive agents were evaluated within included trials. In three trials (ABCD (1); ABCD (2); UKPDS/HDS), the same anti-hypertensive medications were administered to each treatment arm, but different blood pressure targets were specified for each arm. In three trials (ACCORD EYE; ADVANCE/AdRem; UKPDS/HDS), participants were randomized to different blood glucose control strategies in addition to blood pressure control strategies. In five trials, outcomes following assignment to an angiotensin-converting enzyme inhibitor (ACEi) were compared with outcomes following assignment to calcium channel blockers, angiotensin receptor blockers, beta-blockers, or a combination of an agent with an ACEi (ABCD (1); ABCD (2); BENEDICT; DEMAND; RASS; UKPDS/HDS).
Five trials reported additional variation in the trial interventions, such as anti-hypertensive medications that could be added at the discretion of the treating clinicians (ABCD (1); ADVANCE/AdRem; BENEDICT; DEMAND; Steno-2). Flexible dosing schedules for anti-hypertensive medications were permitted in two trials (ABCD (1); EUCLID).
Study outcomes
Incidence and progression of diabetic retinopathy
Of the 15 included RCTs, nine trials used either the Early Treatment Diabetic Retinopathy Study (ETDRS) final 11-step scale or a modification of it in which the most severe levels of retinopathy were combined into a single category to create an 8- or 6-step scale to describe diabetic retinopathy. Two trials used the EURODIAB 5-step scale. Two trials used a condensed version of the ETDRS final scale. The remaining trials did not specify the grading scale used (DEMAND, Pradhan).
The investigators of four trials reported the incidence of diabetic retinopathy as a 2-step or greater progression on the ETDRS scale from no retinopathy or microaneurysms only at baseline (ABCD (1); ADVANCE/AdRem; DIRECT Prevent 1; UKPDS/HDS). One trial defined incidence as a 1-step progression on the EU-RODIAB scale (Steno-2) and another as a 2-step progression on the same scale (EUCLID). In all six trials, the definition of incidence equated to development of mild non-proliferative (or more severe) diabetic retinopathy. One trial (DEMAND) did not describe criteria for incident diabetic retinopathy. Among the four trials that used the ETDRS scale to evaluate progression of diabetic retinopathy, the investigators of two trials reported a 3-step change (DIRECT Protect 1; DIRECT Protect 2); the investigators of the other two trials reported a 2-step change (ADVANCE/AdRem; UKPDS/HDS). Chase reported individual participant data from which changes of 1 to 6 steps could be derived.
The ABCD (1), ABCD (2), ACCORD EYE, EUCLID, RASS, and Steno-2 investigators reported only a composite end-point of incidence and progression of retinopathy.
The protocol for the BENEDICT trial described progression of retinopathy as the outcome of interest, but the publication of trial findings omitted that protocol-specified outcome and instead introduced a new outcome, regression of retinopathy.
Visual acuity
Only two included trials reported change of visual acuity from baseline as an outcome (ACCORD EYE; UKPDS/HDS). Both trials reported change as three or more logMAR units (lines on a logMAR visual acuity chart). Steno-2 reported incident blindness. UKPDS/HDS investigators reported blindness as an adverse event.
Incidence of proliferative diabetic retinopathy (PDR) or clinically significant macular edema (CSME)
The investigators of six trials reported the incidence of PDR or CSME (ADVANCE/AdRem; DIRECT Protect 1; DIRECT Protect 2; RASS; Steno-2; UKPDS/HDS). Investigators of two trials reported only progression to PDR (Chase; EUCLID).
Other outcomes
Other outcomes, including quality of life, cost-effectiveness data, and adverse events, are described in detail in the Effects of interventions section.
Sources of funding
Six trials were sponsored entirely by pharmaceutical companies (BENEDICT; DEMAND; DIRECT Prevent 1; DIRECT Protect 1; DIRECT Protect 2; EUCLID). Seven trials were conducted with partial support from industry and additional support from governmental agencies and foundations (ABCD (1); ABCD (2); ACCORD EYE; Chase; RASS;Steno-2; UKPDS/HDS). Partial support from industry was either in the form of study drugs and supplies, support for conducting specific analyses, or unspecified. Two trials were conducted with support from governmental agencies and institutions with which the investigators were affiliated (ADVANCE/AdRem; Pradhan). Although the main trial for ADVANCE/AdRem was sponsored by a pharmaceutical company, the substudy of ocular outcomes was reported to have been investigator-initiated and supported by the investigator-affiliated institution and a government agency.
Excluded studies
We provide the primary reasons for excluding each of the 23 studies selected during initial screening in the Characteristics of excluded studies table. We excluded 13 RCTs of blood pressure control in 3788 people with diabetes because no data were available for diabetic retinopathy outcomes. We contacted trial investigators who were first authors of primary reports from the 13 trials to ascertain whether retinopathy outcomes were available. None of the 11 respondents provided data because diabetic retinopathy outcomes had not been evaluated in the trials; investigators of two studies did not respond. We excluded five studies because they were not RCTs or because they did not investigate interventions of blood pressure control.
Risk of bias in included studies
Figure 2 provides an overall summary of the risk of bias assessments of the included trials with respect to this review. We present details for each individual study in the ’Risk of bias’ section of the Characteristics of included studies table.
Figure 2.
Risk of bias summary: review authors’ judgements about each risk of bias item for each included study. Missing cells indicate that study did not measure corresponding review outcomes.
Allocation
We judged 11 trials to be at low risk of bias from sequence generation (ABCD (1); ABCD (2); ACCORD EYE; ADVANCE/AdRem; DEMAND; DIRECT Prevent 1; DIRECT Protect 1; DIRECT Protect 2; EUCLID; RASS; UKPDS/HDS), as they all reported using an appropriate randomization method. We assessed the remaining four trials as having unclear risk of bias because we did not find sufficient descriptions of random sequence generation in the trial reports (BENEDICT; Chase; Pradhan; Steno-2). We judged allocation concealment methods to provide low risk of bias for 10 trials that employed methods such as assignments made by a central coordinating center; unclear risk of bias for four trials that did not report random allocation method (BENEDICT; Chase; Pradhan; RASS); and high risk of bias for one trial that did not describe an allocation concealment method and did not mask treatments (Steno-2). Block size in this last trial was also fixed so that later assignments in each block of four could have been known to the investigators.
Masking (performance bias and detection bias)
The descriptions of 12 of the 14 trials in which the primary outcome for this review was reported indicated that the diabetic retinopathy outcome assessors were masked to the assigned treatment. We judged these 12 trials to be at low risk and the other two trials to be at unclear risk of performance and detection biases for retinopathy outcomes (Figure 2). Of the eight trials that reported information about secondary outcomes, we judged five trials to have low risk of performance and detection biases based on proper methods of masking (DIRECT Protect 1; DIRECT Protect 2; EUCLID; RASS; Steno-2); one trial to have high risk due to lack of masking for visual acuity assessment (Pradhan); and the remaining two trials to have unclear risk of bias (ACCORD EYE; UKPDS/HDS).
Incomplete outcome data
We judged three trials to have been at high risk of bias due to incomplete primary outcome data: missing data for roughly 40% of randomized participants in two trials (ABCD (1) and ABCD (2)) and excluding participants with missing baseline retinal photographs in one trial (ADVANCE/AdRem). Investigators of three trials did not provide sufficient information regarding completeness of follow-up; we thus judged those trials as being at unclear risk of attrition bias (EUCLID; RASS; Steno-2). We found the remaining eight trials to have a low risk of attrition bias for primary outcome data. Secondary outcomes for this review were reported less frequently than primary outcomes; for seven trials, no secondary outcome was reported so that risk of attrition bias was not applicable for secondary outcomes in those instances.
Selective reporting
We assessed one trial to be at high risk of selective outcome reporting because a protocol-specified outcome (progression of retinopathy) was omitted from the published report, and a new outcome (regression of retinopathy) was introduced in the trial publication (BENEDICT). Progression and regression are not complementary outcomes because stable retinopathy is not part of either outcome definition. We judged two trials to be at unclear risk of reporting bias, as percentages of participants with outcomes were reported without sufficient information to determine numbers of participants in each group (ABCD (1); ABCD (2)). We judged another six trials to have been at unclear risk of bias, as insufficient information was available from trial reports to make a judgement of low risk (ACCORD EYE; Chase; DEMAND; EUCLID; Pradhan; Steno-2). We judged the remaining six trials to have been at low risk of reporting bias.
Other potential sources of bias
Due to the presence of either partial or complete industry support, we considered nine trials to have an unclear risk of other potential biases. We judged another two trials to have an unclear risk of bias due to post-randomization exclusions (ACCORD EYE) and considering retinal photographs taken three months after randomization as reflecting the baseline status of the participants’ eyes (ADVANCE/AdRem). We judged the remaining four trials to have a high risk of bias. One trial without a data monitoring committee was terminated early for futility (Pradhan), another excluded participants from the analyses who discontinued study medication (DEMAND), and two had members of the data and safety monitoring committee who represented the pharmaceutical company funding the trial (ABCD (1); ABCD (2)).
Effects of interventions
See: Summary of findings for the main comparison
Subsets of included trials reported each of the outcomes specified for this review; no single outcome was reported by all 15 included trials. We provide a summary of data comparing intensive versus less intensive control of blood pressure (including blood pressure control versus placebo), which we refer to as blood pressure intervention versus control. We present overall findings and findings within subgroups of participants defined by type of diabetes (type 1 and type 2) and baseline hypertension status of trial participants (hypertensive and normotensive or treated hypertensive).
Although different scales were used to assess incidence and progression of retinopathy in the included trials, they were all derived from the Airlie House classification (ETDRS10 1991). For the purpose of summarizing evidence in this systematic review, we have considered a change on one retinopathy scale to represent an approximately equal change on another scale. We also present the available data comparing outcomes between classes of anti-hypertensive agents.
Intensive or strict blood pressure control versus less strict blood pressure control
Incidence of retinopathy
Data regarding 4- to 5-year incidence of retinopathy were available from one trial (DIRECT Prevent 1) conducted among 1421 type 1 diabetics and from five trials conducted among 1632 type 2 diabetics (ABCD (1); ADVANCE/AdRem; DEMAND; Steno-2; UKPDS/HDS). The estimated risk ratio (RR) and 95% confidence interval (CI) for intervention on blood pressure compared to less or no intervention based on data from these 3053 trial participants was 0.80; 95% CI 0.71 to 0.92, supporting a 20% reduction in the incidence of any retinopathy as a result of blood pressure intervention during a 4- to 5-year period (Analysis 1.1). Three trials provided data on the effect of blood pressure control over a shorter intervention and follow-up period (1.5 to 2 years): DIRECT Prevent 1 and EUCLID for 1555 type 1 diabetics and UKPDS/HDS for 398 type 2 diabetics. The estimated RR for incident diabetic retinopathy during this shorter period was also 0.80 (95% CI 0.66 to 0.98), consistent with the 4- to 5-year estimate.
The estimated effect of blood pressure intervention on the incidence of diabetic retinopathy was similar among type 1 and type 2 diabetics for both the 4- to 5-year period (Analysis 1.1: estimated RR 0.82 (95% CI 0.69 to 0.97) for type 1 diabetics and 0.78 (0.63 to 0.96) for type 2 diabetics) and the 1.5- to 2-year period (Analysis 3.1: 0.83 (0.66 to 1.03) for type 1 diabetics, 0.74 (0.50 to 1.11) for type 2 diabetics). Similarly, the estimated effects for the 1659 trial participants who were normotensive or under treatment for hypertension at the time of enrollment and the 1394 trial participants who were hypertensive, all of whom were type 2 diabetics, are consistent with the overall estimates for the 4- to 5-year period (Analysis 2.1: 0.84 (0.73 to 0.98) for normotensives/treated hypertensives and 0.72 (0.56 to 0.93) for hypertensives).
Progression of retinopathy
Four trials reported progression of retinopathy among patients in whom retinopathy already was present at time of trial enrollment among 1905 type 1 diabetics (DIRECT Protect 1) and among 2684 type 2 diabetics (ADVANCE/AdRem; DIRECT Protect 2; UKPDS/HDS). The estimated overall RR for progression during this period was 0.88 (95% CI 0.73 to 1.05), suggesting a possible 12% reduction in progression as a result of intervention on blood pressure (Analysis 1.2). However, the CI on the estimated overall RR and for the RRs estimated for three of the four trials are consistent with no effect on progression of diabetic retinopathy as a result of blood pressure intervention. Four trials reported data for this outcome during 1.5 to 2 years: Chase, DIRECT Protect 1, DIRECT Protect 2, and UKPDS/HDS. The estimated RR was 1.08 (95% CI 0.89 to 1.31), indicating no benefit of blood pressure intervention on the risk of progression during this shorter period (Analysis 3.2).
A beneficial effect of blood pressure intervention on progression of diabetic retinopathy was suggested only for type 2 diabetics (estimated RR 0.81 (95% CI 0.65 to 1.01)) who accounted for more than two-thirds of the total number of trial participants for whom this outcome was reported at 4 to 5 years (Analysis 1.2). However, the upper limit of the CI is consistent with no benefit of blood pressure intervention among type 2 diabetics. Among trial participants for whom progression was reported for 1.5 to 2 years (Analysis 3.2), blood pressure intervention was not beneficial in either type 1 or type 2 diabetics during this shorter period (Analysis 3.2). The findings for subgroups defined by blood pressure at baseline were consistent with overall findings (Analysis 2.2); a beneficial effect of blood pressure intervention was not supported for either participants who were normotensive or treated hypertensives at baseline (estimated RR 0.94 (95% CI 0.81 to 1.09)) or who were hypertensive (estimated RR 0.73 (95% CI 0.51 to 1.06)) because both CIs include 1.
Combined incidence and progression of retinopathy
Reports from six RCTs contained data regarding 4- to 5-year rates of combined incidence and progression of diabetic retinopathy from baseline (ABCD (1), ABCD (2), ACCORD EYE, DEMAND, RASS, Steno-2); however, only five of the trials reported data in a form that could be used in a meta-analysis. The effect of intervention on blood pressure for this combined outcome (Analysis 1.3) has an estimated RR of 0.78 (95% CI 0.63 to 0.97), supporting a reduction of 22% with blood pressure intervention despite heterogeneity among the trials. The estimated effect from ACCORD EYE favors less intensive intervention on blood pressure, but the evidence from the remaining trials supports more intensive intervention. Investigators from two trials (ABCD (1), EUCLID) reported this outcome for participants treated and followed for 1.5 to 2 years; the estimated RR was 0.54 (95% CI 0.29 to 0.98) during this shorter period (Analysis 3.3). The DEMAND investigators reported a hazard ratio of 0.27 (95% CI 0.07 to 0.99) over 4 years for this outcome.
Findings from trials for type 1 diabetics were statistically heterogeneous, with an I2 value of 60%, largely due to the difference between the effect estimated for ACCORD EYE compared with the other three trials. As a result, the CI on the summary RR estimated for type 1 diabetics included 1 (estimated RR 0.82 (95% CI 0.66 to 1.03)). For subgroups based on blood pressure status at baseline, the evidence did not support a beneficial effect of blood pressure among either baseline hypertensives (estimated RR 0.72 (95% CI 0.48 to 1.08)) or baseline normotensives or hypertensives controlled by treatment (estimated RR 0.81 (95% CI 0.57 to 1.16)), although the effect estimates for both subgroups favored blood pressure control (Analysis 2.3). Findings were heterogeneous in both subgroups, with I2 values of 73% and 62% for the subgroups and 60% for the overall estimate. As noted, the estimated effect from ACCORD EYE differed from the effect estimated from the other trials.
Incidence of PDR and CSME
Data regarding the incidence of PDR or CSME during a 4- to 5-year period were available from six trials (ADVANCE/AdRem; DIRECT Protect 1; DIRECT Protect 2; RASS; Steno-2; UKPDS/HDS). These outcomes typically were reported together because the presence of either one indicated the need for laser photocoagulation or some other treatment. There was no evidence of a beneficial effect of blood pressure intervention on this outcome: estimated RR 0.95 (95% CI 0.83 to 1.09). During 1.5- to 2-year treatment and follow-up of baseline normotensive or treated hypertensive type 1 diabetics enrolled in Chase and EUCLID, the evidence favored blood pressure intervention to reduce the incidence of PDR, but the CI was wide and included 1: estimated RR 0.58 (95% CI 0.04 to 9.07). Furthermore, the direction of the effect differed in the two studies, as noted by I2 = 64%. These two studies did not report the incidence of CSME.
Blood pressure intervention was not beneficial for reducing 4- to 5-year incidence of PDR and CSME among either type 1 or type 2 diabetics (Analysis 1.4) or for participants who were normotensive at baseline or whose hypertension was controlled at baseline (Analysis 2.4); all CIs included 1. There was a suggestion of benefit among baseline hypertensives: estimated RR 0.76 (95% CI 0.56 to 1.02); the estimated effect differed from that for normotensives/treated hypertensives: estimated RR 1.01 (95% CI 0.87 to 1.16) (Analysis 2.4. The available evidence thus supports no benefit to intervention on blood pressure with respect to incidence of PDR or CSME during a 4- to 5-year period of treatment and follow-up, except possibly among hypertensive type 2 diabetics (Table 4).
Table 4.
Comparison of outcomes within participant subgroups: type 1 normotensive diabetics, type 2 normotensive or treated hypertensive diabetics, and type 2 hypertensive diabetics
| Outcomes | Type 1 normotensives | Type 2 normotensives or treated hypertensives | Type 2 hypertensives | |
|---|---|---|---|---|
| Incidence of retinopathy | Direction of effect | favors BP intervention over placebo | favors BP intervention over placebo | favors intensive BP intervention over standard BP intervention |
| RR [95% CI] | 0.82 [0.69 to 0.97] | 0.94 [0.69 to 1.27] | 0.72 [0.56 to 0.93] | |
| # trials (participants) | 1 (1421) | 1 (238) | 4 (1394) | |
| Progression of retinopathy | Direction of effect | favors placebo over BP intervention | favors BP intervention over placebo | favors intensive BP intervention over standard BP intervention |
| RR [95% CI] | 1.03 [0.82 to 1.29] | 0.89 [0.73 to 1.08] | 0.73 [0.51 to 1.06] | |
| # trials (participants) | 1 (1905) | 1 (1905) | 2 (779) | |
| Combined incidence and progression of retinopathy | Direction of effect | favors BP intervention over placebo | - | favors intensive BP intervention over standard BP intervention |
| RR [95% CI] | 0.82 [0.66 to 1.03] | - | 0.55 [0.35 to 0.88] | |
| # trials (participants) | 4 (2436) | 0 | 1 (151) | |
| Incidence of PDR/CSME | Direction of effect | favors placebo over BP intervention | neither | favors intensive BP intervention over standard BP intervention |
| RR [95% CI] | 1.03 [0.80 to 1.32] | 1.00 [0.83 to 1.19] | 0.76 [0.56 to 1.02] | |
| # trials (participants) | 2 (2128) | 1 (1905) | 3 (2540) | |
| Adverse events: all-cause mortality | Direction of effect | favors placebo over BP intervention | favors placebo over BP intervention | favors intensive BP intervention over standard BP intervention |
| RR [95% CI] | 1.08 [0.50 to 2.29] | 1.01 [0.70 to 1.45] | 0.51 [0.29 to 0.89] | |
| # trials (participants) | 2 (3322) | 2 (2382) | 3 (1005) | |
BP: blood pressure
CI: confidence interval
CSME: clinically significant macular edema
PDR: proliferative diabetic retinopathy
RR: risk ratio
Visual acuity loss of 3 or more lines
Two trials, ACCORD EYE and UKPDS/HDS, reported visual acuity loss of 3 or more lines from baseline levels during 4 to 5 years of blood pressure intervention; participants in both trials had type 2 diabetes. The estimated RR was 1.06 and the 95% CI was 0.85 to 1.33. No evidence of a beneficial effect of the intervention was found in either trial with respect to prevention of moderate or severe loss of visual acuity, defined as loss of 3 or more lines on a chart with a logMAR scale.
Summary
Available evidence from randomized trials for both short-term (1.5 to 2 years) and long-term (4 to 5 years) intervention on blood pressure support a beneficial effect on incidence of diabetic retinopathy in comparison to no or less intervention on blood pressure, with an estimated reduction in incidence of 20%. This effect was consistent across type 1 and type 2 diabetics and among both trial participants who were hypertensive and those who were normotensive or whose hypertension was controlled by treatment at time of trial enrollment.
Overall findings for 4 to 5 years suggest a possible 12% reduction in the risk of progression of diabetic retinopathy with blood pressure control among RCT participants with retinopathy at baseline, but we did not observe a benefit early or among type 1 diabetics, all of whom were normotensives at baseline, nor among all participants who were normotensives or controlled hypertensives initially.
The RRs estimated for the combined outcome of incidence and progression of diabetic retinopathy are similar to those for incidence during 4 to 5 years, both overall and among type 1 diabetics and trial participants who were normotensive or under treatment for hypertension initially, consistent with a reduction in the risk of this outcome with blood pressure intervention of about 20%. A larger benefit was estimated for hypertensive participants, all of whom were type 2 diabetics (Analysis 2.3).
We did not find a benefit for intervention on blood pressure with respect to incidence of PDR or CSME or for moderate or more severe loss of visual acuity, either overall or within any major subgroup of participants examined.
In order to examine further the possible small benefit of more intensive blood pressure intervention among type 2 diabetics, we analyzed outcomes by whether these participants were normotensives/treated hypertensives at baseline or were hypertensives. As shown in Table 4, only among hypertensive type 2 diabetics did the estimated RRs favor intensive blood pressure control on both incidence and progression of diabetic retinopathy, whether considered as individual outcomes or in combination. Furthermore, the evidence was also consistent with a benefit of intensive blood pressure control on progression to PDR or CSME and death from all causes among participants in this subgroup (Table 4).
Quality of life (QOL)
The UKPDS/HDS investigators reported a cross-sectional QOL assessment conducted at eight centers (UKPDS/HDS report 37). A subset of participants completed a “domain specific” questionnaire (n = 636) and/or the EQ-5D questionnaire (n = 747) at mean times since randomization to tight or less tight blood pressure control of 5 and 8 years, respectively.. Of the specific measures (work satisfaction, mood state, symptoms, cognitive mistakes), median scores for the tight blood pressure control group differed from those of the less tight control group by 1 or 2 points for anger, symptoms, and both patient- and relative-reported cognitive mistakes; however, interquartile ranges were similar. Total scores on the mood state scale differed by 3.5 points, with the tight control group having better score. However, the authors reported that the difference was not statistically significant; this statement was supported by substantial overlap of the confidence intervals. With respect to the EQ-5D scale, scores in the two groups were similar except for the anxiety dimension, for which respondents in the tight blood pressure control group had worse scores (P < 0.05). Within the tight blood glucose control arm, scores for respondents assigned to an angiotensin-converting enzyme inhibitor (ACEi) were compared to scores of those assigned to a beta-blocker. The authors stated that “a lower proportion of patients who were allocated to β-blockers reported anxiety, on the generic questionnaire, than those allocated to ACE inhibitors (28% vs. 40%, Fisher’s exact test, P = 0.010).”
The ACCORD Study Group reported the rationale and design of health-related QOL and cost-effectiveness components, but we did not find any published data after an intensive search and queries to ACCORD EYE investigators.
Cost-effectiveness
The UKPDS/HDS investigators evaluated the cost-effectiveness of tight blood pressure control in participants with hypertension and type 2 diabetes (UKPDS/HDS reports 40 and 63). The trial investigators performed an incremental cost-effectiveness analysis in which they calculated the net costs and net effectiveness of tight control versus less tight control based on outcome data from their trial. Costs included treatment fees for blood pressure control, visits to doctors at diabetes centers, tests obtained at medical visits, and the costs of treating diabetic complications. Investigators estimated that the total costs for less tight blood pressure control was GBP6145 per patient over an 8.4-year period compared to GBP6381 per patient with tight control, which represented a difference of GBP237. Although there was a higher cost of anti-hypertensive treatment in the tight blood pressure control group than in the less tight control group, the analysis based on UKPDS/HDS data indicated that this increment was offset by reduced complication costs, longer survival, and greater interval without complications in the tight blood pressure control group than in the less tight blood pressure control group. The value of this finding is limited by the outdated definitions of hypertension and its control that were used by the UKPDS investigators.
The UKPDS investigators also compared the cost-effectiveness of an ACE inhibitor (captopril) to a beta-blocker (atenolol) (UKPDS/HDS 54). Although the two agents used to treat hypertensive type 2 diabetics were found to have similar effects, atenolol was associated with lower overall costs due to lower drug costs and fewer and shorter hospitalizations.
Data from the Steno-2 study were used to evaluate the cost-effectiveness of intensive versus conventional multifactorial interventions in type 2 diabetics. However, the cost of photography, ophthalmologic examinations, or other clinical procedures were not considered part of the “annual cost of consultation” (Steno-2). Similarly, blindness or impaired visual acuity were not included under complications, and neither photocoagulation, vitrectomy, nor other interventions for diabetic retinopathy were included in the model.
Adverse events
Reporting of adverse events associated with blood pressure control was inconsistent in the included trials. The most frequently reported adverse event for participants in the included trials was death from all causes, reported from seven trials (ABCD (1); ABCD (2); DEMAND; DIRECT Prevent 1; DIRECT Protect 1; DIRECT Protect 2; Steno-2). As shown in Analysis 1.6, the estimated RR for this adverse outcome was 0.86 (95% CI 0.64 to 1.14), indicating no important difference due to intervention on blood pressure. The effect of blood pressure intervention on deaths from all causes was similar among type 1 diabetics (estimated RR 1.08 (95% CI 0.50 to 2.29)) and type 2 diabetics (estimated RR 0.82 (95% CI 0.60 to 1.12)); Analysis 1.6). However, the effect for trial participants who were hypertensive at baseline is consistent with a substantial reduction in mortality: estimated RR 0.51 (95% CI 0.29 to 0.89).
Three trials reported hypotension (DIRECT Prevent 1; DIRECT Protect 1; Steno-2). As expected and shown in Analysis 1.7, significantly more hypotension was reported among participants in the trial arm in which there was more intense intervention on blood pressure: estimated RR 2.08 (95% CI 1.68 to 2.57). The findings were similar among type 1 diabetics (DIRECT Prevent 1; DIRECT Protect 1) and type 2 diabetics (Steno-2).
The UKPDS/HDS and Steno-2 investigators reported the only ocular complications we could find for the included trials. The UKPDS/HDS investigators reported blindness among 18 of 758 versus 12 of 390; vitreous hemorrhage among 3 of 758 versus 2 of 390; and cataract surgery among 36 of 758 versus 14 of 390 participants in the tight blood pressure control arm and less tight control arm, respectively. Steno-2 investigators reported blindness, defined as Snellen chart visual acuity of 6/60 or worse by the World Health Organization criteria, in one eye for 1 of 80 participants in the intensive group and 7 of 80 participants in the standard group (estimated RR 0.14 (95% CI 0.02 to 1.13)).
A major difficulty we encountered in our efforts to identify adverse events of blood pressure intervention was attributable to the fact that many of the included trials were ancillary to a larger parent study (ACCORD EYE; ADVANCE/AdRem; RASS; UKPDS/HDS), and that the adverse events reported were the cardiovascular or renal events that were the outcomes of the parent trial. Another difficulty was that participants in several trials were also randomized to concurrent intervention, primarily on blood glucose as in ACCORD EYE and UKPDS/HDS, but also on lipids as in RASS.
Comparison of outcomes following treatment with different classes of anti-hypertensive medications
A secondary goal of the authors of this review was to compare outcomes for different classes of anti-hypertensive agents with the goal of identifying the most effective. In six trials (ABCD (1); ABCD (2); BENEDICT; DEMAND; RASS; UKPDS/HDS), different classes of anti-hypertensive agents or combinations were compared to an ACEi. The trial identifiers, test anti-hypertensive medication compared to an ACEi, outcome for which the medications were compared, and the relative effectiveness of the test medication are shown in Table 5. Another class of anti-hypertensive agent was compared to an ACEi within more than one trial for only one outcome, combined incidence and progression of diabetic retinopathy over 4 to 5 years. In comparison to an ACEi, no other class of anti-hypertensive agent, alone or in combination with an ACEi, was clearly superior to an ACEi based on the data reported from the included trials.
Table 5.
Comparison of ACEi drugs with other classes of anti-hypertensives
| Outcome | Trial identifier | Comparator class | RR (95% CI) |
|---|---|---|---|
| Incidence of DR | DEMAND | ACEi + CCB | 0.48 (0.13, 1.86) |
| Progression of DR | UKPDS/HDS | beta-blocker | 1.01 (0.75, 1.35) |
| Combined incidence and progression of DR | ABCD (1) | CCB | 1.33 (0.93, 1.92) |
| ABCD (2) | CCB | 0.93 (0.71, 1.21) | |
| RASS | ARB | 0.89 (0.49, 1.63) | |
| Regression of DR | BENEDICT | non-ACEi | 0.44 (0.22, 0.87) |
| All-cause mortality | UKPDS/HDS | beta-blocker | 0.88 (0.64, 1.20) |
ACEi: angiotensin-converting enzyme inhibitor
ARB: angiotensin receptor blocker
CCB: calcium channel blocker
DR: diabetic retinopathy
RR: risk ratio
CI: confidence interval
DISCUSSION
Summary of main results
We found 15 randomized controlled trials that had evaluated the use of blood pressure-lowering interventions in participants with either type 1 or type 2 diabetes and that reported diabetic retinopathy outcomes. There was considerable variability among the trials with respect to sample size, interventions evaluated, eligibility criteria, diabetic retinopathy outcomes reported, and length of follow-up of participants. Among the six trials that reported the incidence of diabetic retinopathy among 3053 participants, findings supported intensive blood pressure intervention among both type 1 diabetics (one trial) and type 2 diabetics (five trials). The evidence yielded an estimated 20% reduction in the risk of incident retinopathy with intensive intervention compared to no or less intense intervention on blood pressure. Data regarding progression of retinopathy were reported from four trials in which 4195 diabetics had participated. Although some statistical heterogeneity, as well as clinical and methodologic heterogeneity, was observed among the findings from the four trials, overall the evidence indicated no benefit, or at best a small benefit, of more intense intervention on blood pressure with respect to progression of diabetic retinopathy. Findings from the five trials that reported only combined incidence and progression of retinopathy were similar to those for incidence alone: approximately a 20% reduction in risk with more intense intervention on blood pressure. However, there was substantial statistical heterogeneity among the effect estimated from individual trials that reported this outcome. Six trials with a total of 6573 participants reported data regarding incidence of proliferative diabetic retinopathy or clinically significant macular edema, or both, and two trials (2326 total participants) reported moderate to severe loss of visual acuity. Neither the findings for incidence of proliferative diabetic retinopathy nor for clinically significant macular edema favored intense blood pressure intervention; the findings were consistent within subgroups of participants defined by type of diabetes and by blood pressure status at time of trial enrollment.
Although evidence from four trials supports intensive control of blood pressure to reduce the risk of incident diabetic retinopathy, and evidence from five trials that reported only a combined outcome for incidence and progression provide similar support, only among the 3816 type 2 diabetics who were hypertensive at baseline and participated in the included trials does the evidence provide consistent support for a benefit of intensive blood pressure control with respect to progression, including progression to retinopathy that requires laser photocoagulation or another intervention. The evidence favoring tight blood pressure control may thus not be sufficient to convince all diabetic patients and their physicians of the beneficial effect of blood pressure control on retinopathy outcomes.
The investigators of the clinical trials included in this review did not report systematically on adverse events related to tight blood pressure control. Therefore, the incidence of serious adverse events, both systemic and ocular, associated with the use of anti-hypertensive medications in the diabetic population, cannot be estimated reliably from the data provided by the included trials.
Overall completeness and applicability of evidence
Although we limited this review to consideration of findings reported from RCTs, the included trials differed from one another in several important respects. In recognition of these differences, we must consider a number of points when interpreting the available evidence.
Baseline laboratory data differed in the participant cohorts that participated in the various trials (Table 1; Table 2; Table 3). In particular, in both the ABCD (1) trial and the Pradhan trial, baseline glycated hemoglobin (HbA1c) values were quite high, approximately 11% in the intensively treated and control groups. In the other studies, HbA1c values were approximately 8% or lower (Table 1; Table 2; Table 3). Although the target of intervention in these studies was blood pressure, the separate influence of blood glucose, which differed in the various studies, may have had a greater effect on the retinopathy outcome.
Clinical centers in these trials were established in numerous geographic locations. For example, ADVANCE/AdRem was carried out in 20 countries, and the Diabetic Retinopathy Candesartan Trials (DIRECT) program had centers in 30 countries. While this dispersion surely resulted in considerable ethnic and genetic variation among the participants, specific racial or ethnic distribution was not reported in the description of any of the study cohorts. Centers in India and China participated in ADVANCE/AdRem, and centers in South Africa participated in the DIRECT trials. Although ADVANCE/AdRem reported a comparison of retinal lesions at baseline among white and Asian participants, none of the trials provided data to suggest that diabetic individuals from different racial or ethnic groups differed in their responses to blood pressure control with respect to the development or progression of retinopathy or to adverse events.
Trials varied widely in size, from as few as 16 participants (Chase) to more than 2000 (ADVANCE/AdRem). The data reporting thus ranged from a listing of individual participant data to outcome rates estimated using statistical models. Not surprisingly, rates of incidence and progression of diabetic retinopathy sometimes were not reported in a form amenable to the methods of analysis suitable for a systematic review using grouped data.
Although most trials used the Early Treatment Diabetic Retinopathy Study (ETDRS) or the EURODIAB scale for grading retinopathy, the different trials had different definitions for progression of diabetic retinopathy (from one to three steps on a scale, counting progression in one or both eyes). Only 5 of the 15 trials clearly distinguished participants without retinopathy at baseline, in whom incidence could be assessed, from those with retinopathy detected at baseline. It is possible that the effect of hypertension or its control varies with the level of severity of retinopathy initially present or that is being considered as the end point.
The blood pressure goals of several of the trials included in this review do not reflect current practice. For example, in UKPDS/HDS, the tight blood pressure control group aimed for a blood pressure less than 150/85 mm Hg, with the less tight control group aiming for a blood pressure of 180/105 mm Hg or less. However, in the ACCORD blood pressure intervention trial (Cushman 2007), the goal for the less intensive control group was a systolic blood pressure less than 140 mm Hg, and for the intensive control group the goal was less than 120 mm Hg.
Quality of the evidence
1. Most studies evaluated the presence and severity of retinopathy using standard photographic protocols that provided objective documentation of the status of the retina, evaluation by observers masked to treatment status of participants, and reproducible evaluation by separate graders when necessary. In EUCLID, there was only a single grader, thus providing no mechanism to check for consistency or reproducibility of the grading.
The UKPDS/HDS and RASS did not have a true baseline for assessing diabetic retinopathy. In these studies, “baseline” retinal photographs could have been taken as much as three years before (UKPDS/HDS) or one year after (RASS) randomization to the study arm.
Several studies embedded in parent studies with different goals restricted analysis and reporting of retinopathy data to participants who had both baseline and follow-up assessments of retinopathy, without any attempt to impute data for missing assessments or to account for missing data otherwise, so as to provide or estimate outcomes for the full participant population studied. Missing follow-up assessments are common in trials with clinical outcomes, particularly those conducted among participants who are elderly or who have multiple medical problems. No totally satisfactory method has been identified to account for missing clinical outcome data due to deaths of trial participants.
Included studies did not employ the same time points for assessment of retinal photographs for retinopathy status. In most studies, photographs were taken only at baseline and a single follow-up time or when needed to document retinal status before treatment.
The trials used various strategies for intervening on blood pressure. For this review, we have pooled the data from the more intense strategy in each trial for comparison with the less intense strategy.
Attrition was an issue in some trials. Denominators for percentages often were not reported. When we could find sufficient information about deaths and other losses to follow-up, we calculated denominators based on the number of participants enrolled; otherwise, we estimated rates based on the total number randomized. A summary of quality of evidence is in the Summary of findings for the main comparison.
Potential biases in the review process
The protocol for this review did not specify subgroup analyses for participants with type 1 and type 2 diabetes and for participants characterized by blood pressure levels at baseline (Sleilati 2009). The decision to examine findings in these subgroups was made after we began screening the results of electronic searches. Our familiarity with diabetic retinopathy and randomized trials for this condition suggested that it would be inappropriate to conduct analyses specified in the protocol without considering effects of blood pressure intervention in these different subgroups of participants. Although we examined the available data for these subgroups, subgroup findings usually were consistent with overall findings.
We searched extensively for all trials that evaluated blood pressure control for diabetic retinopathy in individuals with and without retinopathy at baseline. We included trials where the effect of blood pressure control on diabetic retinopathy was evaluated in a subset of all patients randomized into the study, for example ACCORD EYE, ADVANCE/AdRem, and RASS. We excluded 13 trials of blood pressure control in people with diabetes because data regarding diabetic retinopathy outcomes were not available. We designed our searches to identify all trials of blood pressure control in people with diabetes; we screened the resulting listings for any mention of diabetic retinopathy or other ocular findings. In addition, we contacted the authors of reports from trials that suggested that data regarding ocular outcomes might have been available.
Of the 13 trials that reported either incidence or progression (or a combination of incidence and progression) (ABCD (1); ABCD (2); ACCORD EYE; ADVANCE/AdRem; Chase; DEMAND; DIRECT Prevent 1; DIRECT Protect 1; DIRECT Protect 2; EUCLID; RASS; Steno-2; UKPDS/HDS), six trials reported data for 2-step changes from baseline on the ETDRS final scale or a modification of it that provided comparable data. Three trials reported 3-step changes as progression; in the absence of data for 2-step changes, we analyzed these data together with 2-step changes. Similarly, for the three trials that used more condensed scales for grading diabetic retinopathy, we used the data as reported, that is 1-step or 2-step changes. One trial reported incidence of diabetic retinopathy only as change from no retinopathy to any retinopathy. We elected to pool the available data, reasoning that the same definition was used in trial arms compared within individual RCTs and that the goal was to estimate relative effects of blood pressure intervention rather than absolute risks. Furthermore, some 1-step changes on the condensed grading scales undoubtedly were equivalent to 2-step changes on the more detailed ETDRS scale. We could not obtain sufficient data from all included trials to incorporate their findings into all our meta-analyses, particularly those for adverse events and complications. Although some large parent studies of which some included RCTs were part have reported adverse events, we usually were not able to identify events among participants in the trials of blood pressure intervention or in the subgroup participating in the retinopathy substudy..
Agreements and disagreements with other studies or reviews
A previous qualitative review of current therapy for prevention and treatment of diabetic retinopathy reached many of the same conclusions as the present report (Mohamed 2007). However, this earlier review did not include results of the ADVANCE/AdRem, DIRECT Prevent 1, DIRECT Protect 1, DIRECT Protect 2, RASS, Steno-2, and ACCORD EYE trials, which were still in progress at the time of publication of that review. No quantitative synthesis was described in Mohamed 2007; data from included trials were reported without distinction between outcomes at different follow-up times and between incidence and progression of diabetic retinopathy.
AUTHORS’ CONCLUSIONS
Implications for practice
Among the outcomes examined for benefit of tight or intensive blood pressure control, only incidence of diabetic retinopathy, reported alone or in combination with progression, has been demonstrated by our analysis of the available evidence to provide benefit regarding retinopathy in either type 1 or type 2 diabetics, irrespective of whether normotensive or hypertensive at baseline based on the classification used by the trial investigators. Available evidence indicates that administration of anti-hypertensive agents does not decrease progression of retinopathy. Furthermore, the evidence regarding the reduction in incidence estimated for intervention on blood pressure is relatively modest. Insufficient evidence is available regarding the adverse effects of interventions to achieve current blood pressure targets to permit comparison of benefits and risks. Some physicians use angiotensin-converting enzyme inhibitors to prevent or delay the development or to slow progression of diabetic nephropathy and anticipate benefit regarding diabetic retinopathy. Physicians should be aware that data on adverse events related to tight blood pressure control in diabetics are sparse; patients on these medications require close monitoring because they may be at risk for serious adverse events.
Our findings should not be interpreted to preclude treatment of hypertension in diabetics; such treatment has been demonstrated to have substantial benefit on survival and other outcomes. However, the currently available evidence does not support blood pressure control for the sole purpose of slowing progression of diabetic retinopathy or for avoiding the need for treatment for advanced stages of diabetic retinopathy.
Implications for research
Additional randomized controlled trials are needed to define subgroups of type 1 and type 2 diabetics likely to benefit from the use of current anti-hypertensive medications to achieve current blood pressure targets with respect to reduced incidence and progression of retinopathy. If future trials are undertaken, the designers should specify not only the type of diabetics they wish to enroll (type 1 or type 2), but also whether the goal is prevention of diabetic retinopathy (that is only diabetics without retinopathy eligible for enrollment) or slowing progression of existing retinopathy; the blood pressure status of diabetics eligible to participate (normotensive without treatment, hypertensives with blood pressure controlled with treatment, untreated hypertensives); the blood pressure goals of each trial arm; and vision outcomes, which were rarely reported in the current trials. Furthermore, target sample sizes should be large enough to provide precise estimates of outcomes. Although we found data regarding hypotension in reports from only 3 of the 15 included trials, designers of future trials may wish to consider restricting enrollment to diabetics with hypertension to achieve a more favorable benefit-risk comparison in the more intensely treated arm.
The evidence from 15 randomized controlled trials conducted among thousands of diabetics may be interpreted to mean that additional trials designed to address this issue may not be justifiable. It may be more cost-effective to focus on research to explain why blood pressure control affected incidence of retinopathy but not progression, for example, by analyzing individual participant data from completed trials. In the absence of more consistent and convincing data regarding the subgroup of diabetics likely to benefit from intervention on blood pressure, it may be more useful to conduct trials that focus on interventions for other modifiable risk factors for diabetic retinopathy.
Acknowledgments
SOURCES OF SUPPORT
Internal sources
Brown University, USA.
Johns Hopkins University, USA.
External sources
The Cochrane Eyes and Vision Group US Project, which is funded by Grant 1 U01 EY020522, National Eye Institute, National Institutes of Health, USA.
An unrestricted research grant to the Wilmer Eye Institute from Research to Prevent Blindness, New York, NY, USA.
Retina Research Fund, the Wilmer Eye Institute, the Johns Hopkins School of Medicine, Baltimore, MD, USA.
National Institute for Health Research (NIHR), UK.
Richard Wormald, Coordinating Editor for the Cochrane Eyes and Vision Group (CEVG) acknowledges financial support for his CEVG research sessions from the Department of Health through the award made by the National Institute for Health Research to Moorfields Eye Hospital NHS Foundation Trust and UCL Institute of Ophthalmology for a Specialist Biomedical Research Centre for Ophthalmology.
The NIHR also funds the CEVG Editorial Base in London.
The views expressed in this publication are those of the authors and not necessarily those of the NIHR, NHS, or the Department of Health.
We thank Karen Blackhall and Iris Gordon at Cochrane Eyes and Vision Group for devising and running the search strategies for the electronic searches. We thank Bernd Richter, Catey Bunce, and Zbys Fedorowicz for their comments on the protocol; Brian VanderBeek, Danny Cheung, Tianjing Li, and Sandra Forman for commenting on early versions of the review; and Kristina Lindsley, Kay Dickersin, and Jenny Evans for suggestions that resulted in the current version of the review. We acknowledge the assistance of the Cochrane Eyes and Vision Group editorial team for their advice and assistance during the preparation of this protocol and review. Milan Mathew contributed to the conception and early development of the protocol for this review.
APPENDICES
Appendix 1. CENTRAL search strategy
-
#1
MeSH descriptor: [Diabetic Retinopathy] explode all trees
-
#2
diabet* near retinopath*
-
#3
proliferat* near retinopath*
-
#4
vitre* near detach*
-
#5
retina* near detach*
-
#6
diabet* near maculopath*
-
#7
#1 or #2 or #3 or #4 or #5 or #6
-
#8
MeSH descriptor: [Blood Pressure] explode all trees
-
#9
MeSH descriptor: [Blood Glucose] explode all trees
-
#10
MeSH descriptor: [Hypertension] explode all trees
-
#11
(pressure or glucose or glycem*) near/3 blood*
-
#12
hypertens*
-
#13
#8 or #9 or #9 or #10 or #11 or #12
-
#14
MeSH descriptor: [Antihypertensive Agents] explode all trees
-
#15
MeSH descriptor: [Angiotensin-Converting Enzyme Inhibitors] explode all trees
-
#16
ACE next inhibitor*
-
#17
antihypertensive near agent* or drug* or medicat*
-
#18
MeSH descriptor: [Calcium Channel Blockers] explode all trees
-
#19
calcium next channel next blocker*
-
#20
calcium next channel next antagonist*
-
#21
MeSH descriptor: [Diuretics] explode all trees
-
#22
diuretic*
-
#23
MeSH descriptor: [Adrenergic beta-Agonists] explode all trees
-
#24
adrenergic next beta next antagonist*
-
#25
beta next blocker*
-
#26
MeSH descriptor: [Adrenergic alpha-Agonists] explode all trees
-
#27
adrenergic next alpha next antagonist*
-
#28
MeSH descriptor: [Vasodilator Agents] explode all trees
-
#29
MeSH descriptor: [Angiotensin II Type 1 Receptor Blockers] explode all trees
-
#30
angiotensin near blocker*
-
#31
MeSH descriptor: [Acebutolol] explode all trees
-
#32
acebutolol
-
#33
MeSH descriptor: [Amiloride] explode all trees
-
#34
amiloride
-
#35
MeSH descriptor: [Amlodipine] explode all trees
-
#36
amlodipine
-
#37
atorvastin
-
#38
benazepril
-
#39
MeSH descriptor: [Atenolol] explode all trees
-
#40
atenolol
-
#41
MeSH descriptor: [Bendroflumethiazide] explode all trees
-
#42
bendroflumethiazide
-
#43
MeSH descriptor: [Nadolol] explode all trees
-
#44
nadolol
-
#45
MeSH descriptor: [Betaxolol] explode all trees
-
#46
betaxolol
-
#47
MeSH descriptor: [Bisoprolol] explode all trees
-
#48
bisoprolol
-
#49
bosentan
-
#50
bucindolol
-
#51
MeSH descriptor: [Bumetanide] explode all trees
-
#52
bumetanide
-
#53
candesartan
-
#54
MeSH descriptor: [Captopril] explode all trees
-
#55
captopril
-
#56
MeSH descriptor: [Carteolol] explode all trees
-
#57
carteolol
-
#58
carvedilol
-
#59
MeSH descriptor: [Chlorothiazide] explode all trees
-
#60
chlorothiazide
-
#61
MeSH descriptor: [Chlorthalidone] explode all trees
-
#62
chlorthalidone
-
#63
MeSH descriptor: [Clonidine] explode all trees
-
#64
clonidine
-
#65
MeSH descriptor: [Diazoxide] explode all trees
-
#66
diazoxide
-
#67
MeSH descriptor: [Diltiazem] explode all trees
-
#68
diltiazem
-
#69
MeSH descriptor: [Doxazosin] explode all trees
-
#70
doxazosin
-
#71
MeSH descriptor: [Enalapril] explode all trees
-
#72
MeSH descriptor: [Felodipine] explode all trees
-
#73
felodipine
-
#74
eperenone
-
#75
MeSH descriptor: [Epoprostenol] explode all trees
-
#76
epoprostenol
-
#77
eprosartan
-
#78
esmolol
-
#79
MeSH descriptor: [Ethacrynic Acid] explode all trees
-
#80
ethacrynic next acid
-
#81
MeSH descriptor: [Fenoldopam] explode all trees
-
#82
fenoldopam
-
#83
MeSH descriptor: [Fosinopril] explode all trees
-
#84
fosinopril
-
#85
MeSH descriptor: [Furosemide] explode all trees
-
#86
furosemide
-
#87
MeSH descriptor: [Guanabenz] explode all trees
-
#88
guanabenz
-
#89
guanadrel
-
#90
MeSH descriptor: [Guanfacine] explode all trees
-
#91
guanfacine
-
#92
MeSH descriptor: [Hydralazine] explode all trees
-
#93
hydralazine
-
#94
irbesartan
-
#95
MeSH descriptor: [Lisinopril] explode all trees
-
#96
lisinopril
-
#97
MeSH descriptor: [Losartan] explode all trees
-
#98
losartan
-
#99
methyldopa
-
#100
MeSH descriptor: [Metoprolol] explode all trees
-
#101
metoprolol
-
#102
moexipril
-
#103
olmesartan
-
#104
MeSH descriptor: [Propranolol] explode all trees
-
#105
propranolol
-
#106
quinapril
-
#107
MeSH descriptor: [Spironolactone] explode all trees
-
#108
spironlactone
-
#109
telmisartan
-
#110
MeSH descriptor: [Timolol] explode all trees
-
#111
timolol
-
#112
MeSH descriptor: [Triamterene] explode all trees
-
#113
triamterene
-
#114
valsartan
-
#115
MeSH descriptor: [Hydrochlorothiazide] explode all trees
-
#116
hydrochlorothiazide
-
#117
MeSH descriptor: [Iloprost] explode all trees
-
#118
iloprost
-
#119
MeSH descriptor: [Indapamide] explode all trees
-
#120
indapamide
-
#121
isoxsurpine
-
#122
MeSH descriptor: [Isradipine] explode all trees
-
#123
isradipine
-
#124
MeSH descriptor: [Labetalol] explode all trees
-
#125
labetalol
-
#126
lercanidipine
-
#127
MeSH descriptor: [Mecamylamine] explode all trees
-
#128
mecamylamine
-
#129
MeSH descriptor: [Methyclothiazide] explode all trees
-
#130
methyclothiazide
-
#131
MeSH descriptor: [Metolazone] explode all trees
-
#132
metolazone
-
#133
MeSH descriptor: [Mibefradil] explode all trees
-
#134
mibefradil
-
#135
MeSH descriptor: [Minoxidil] explode all trees
-
#136
minoxidil
-
#137
MeSH descriptor: [Nicardipine] explode all trees
-
#138
nicardipine
-
#139
MeSH descriptor: [Nifedipine] explode all trees
-
#140
nifedipine
-
#141
MeSH descriptor: [Nisoldipine] explode all trees
-
#142
nisoldipine
-
#143
MeSH descriptor: [Nitric Oxide] explode all trees
-
#144
MeSH descriptor: [Nitroprusside] explode all trees
-
#145
nitroprusside
-
#146
omapatrilat
-
#147
MeSH descriptor: [Penbutolol] explode all trees
-
#148
penbutolol
-
#149
MeSH descriptor: [Perindopril] explode all trees
-
#150
perindopril
-
#151
MeSH descriptor: [Phenylbutazone] explode all trees
-
#152
phenylbutazone
-
#153
MeSH descriptor: [Phenoxybenzamine] explode all trees
-
#154
phenoxybenzamine
-
#155
MeSH descriptor: [Phentolamine] explode all trees
-
#156
phentolamine
-
#157
MeSH descriptor: [Pindolol] explode all trees
-
#158
pindolol
-
#159
pindolol
-
#160
MeSH descriptor: [Polythiazide] explode all trees
-
#161
polythiazide
-
#162
MeSH descriptor: [Prazosin] explode all trees
-
#163
prazosin
-
#164
prostacyclin
-
#165
MeSH descriptor: [Ramipril] explode all trees
-
#166
ramipril
-
#167
MeSH descriptor: [Reserpine] explode all trees
-
#168
reserpine
-
#169
sildenafil
-
#170
spirapril
-
#171
terazosin
-
#172
torsemide
-
#173
trandolapril
-
#174
MeSH descriptor: [Verapamil] explode all trees
-
#175
verapamil
-
#176
trepostinil
-
#177
MeSH descriptor: [Triamterene] explode all trees
-
#178
triamterene
-
#179
MeSH descriptor: [Trichlormethiazide] explode all trees
-
#180
trichlormethiazide
-
#181
#14 or #15 or #16 or #17 or #18 or #19 or #20 or #21 or #22 or #23 or #24 or #25 or #30 or #31 or #32 or #33 or #34 or #35 or #36 or #37 or #38 or #39 or #40
-
#182
#41 or #42 or (#43 and or#44) or #45 or #46 or #47 or #48 or #49 or #50 or #51 or #52 or #53 or #54 or #55 or #56 or #57 or #58 or #59 or #60 or #61 or #62 or #63 or #64 or #65 or #66 or #67 or #68 or #69 or #70
-
#183
#71 or #72 or #73 or #74 or #75 or #76 or #77 or #78 or #79 or #80 or #81 or #82 or #83 or #84 or #85 or #86 or #87 or #88 or #89 or #90 or #91 or #92 or #93 or #94 or #95 or #96 or #97 or #98 or #99 or #100 or #101 or #102 or #103 or #104 or #105 or #106 or #107 or #108 or #109 or #110
-
#184
#111 or #112 or #113 or #114 or #115 or #116 or #117 or #118 or #119 or #120 or #121 or #122 or #123 or #124 or #125 or #126 or #127 or #128 or #129 or #130 or #131 or #132 or #133 or #134 or #135 or #136 or #137 or #138 or #139 or #140
-
#18
#141 or #142 or #143 or #144 or #145 or #146 or #147 or #148 or #149 or #150 or #151 or #152 or #153 or #154 or #155 or #156 or #157 or #158 or #159 or #160 or #161 or #162 or #163 or #164 or #165 or #166 or #167 or #168 or #169 or #170 or #171 or #172 or #173 or #174 or #175 or #176 or #177 or #178 or #179 or #180
-
#18
#181 or #182 or #183 or #184 or #185
-
#187
#7 and #13
-
#188
#7 and #186
-
#189
#187 or #188
Appendix 2. MEDLINE (OvidSP) search strategy
randomized controlled trial.pt.
(randomized or randomised).ab,ti.
placebo.ab,ti.
dt.fs.
randomly.ab,ti.
trial.ab,ti.
groups.ab,ti.
or/1–7
exp animals/
exp humans/
9 not (9 and 10)
8 not 11
exp diabetic retinopathy/
retinopath$.tw.
(vitre$ adj3 detach$).tw.
(retina$ adj3 detach$).tw.
(diabet$ adj3 maculopath$).tw.
or/13–17
exp blood pressure/
exp blood glucose/
exp hypertension/
((pressure or glucose or glycem$) adj3 blood$).tw.
hypertens$.tw.
or/19–23
exp antihypertensive agents/
exp angiotensin converting enzyme inhibitors/
(ACE adj1 inhibitor$).tw.
(antihypertensive adj2 (agent$ or drug$ or medicat$)).tw.
exp calcium channel blockers/
(calcium adj1 channel adj1 blocker$).tw.
(calcium adj1 channel adj1 antagonist$).tw.
exp diuretics/
diuretic$.tw.
exp adrenergic beta antagonists/
(adrenergic adj1 beta adj1 antagonist$).tw.
(beta adj1 blocker$).tw.
exp adrenergic alpha antagonist/
(adrenergic adj1 alpha adj1 antagonist$).tw.
exp vasodilator agents/
exp angiotensin II type 1 receptor blockers/
(angiotensin adj3 blocker$).tw.
acebutolol.tw.
amiloride.tw.
amlodipine.tw.
atorvastin.tw.
benazepril.tw.
atenolol.tw.
bendroflumethiazide.tw.
nadolol.tw.
betaxolol.tw.
bisoprolol.tw.
bosentan.tw.
bucindolol.tw.
bumetanide.tw.
candesartan.tw.
captopril.tw.
carteolol.tw.
carvedilol.tw.
chlorothiazide.tw.
chlorthalidone.tw.
clonidine.tw.
diazoxide.tw.
diltiazem.tw.
diltiazem.tw.
doxazosin.tw.
enalapril.tw.
enalapril$.tw.
felodipine.tw.
eplerenone.tw.
epoprostenol.tw.
eprosartan.tw.
esmolol.tw.
(ethacrynic adj1 acid).tw.
fenoldopam.tw.
fosinopril.tw.
furosemide.tw.
guanabenz.tw.
guanadrel.tw.
guanfacine.tw.
hydralazine.tw.
irbesartan.tw.
lisinopril.tw.
losartan.tw.
methyldopa.tw.
metoprolol.tw.
moexipril.tw.
olmesartan.tw.
propranolol.tw.
quinapril.tw.
spironolactone.tw.
telmisartan.tw.
timolol.tw.
triamterene.tw.
valsartan.tw.
hydrochlorothiazide.tw.
iloprost.tw.
indapamide.tw.
isoxsuprine.tw.
isradipine.tw.
labetalol.tw.
lercanidipine.tw.
mecamylamine.tw.
methyclothiazide.tw.
metolazone.tw.
mibefradil.tw.
minoxidil.tw.
nicardipine.tw.
nifedipine.tw.
nisoldipine.tw.
exp nitric oxide/
exp nitroprusside/
nitroprusside.tw.
omapatrilat.tw.
penbutolol.tw.
perindopril.tw.
phenylbutazone.tw.
phenoxybenzamine.tw.
phentolamine.tw.
pindolol.tw.
polythiazide.tw.
prazosin.tw.
prostacyclin.tw.
ramipril.tw.
reserpine.tw.
sildenafil.tw.
spirapril.tw.
terazosin.tw.
torsemide.tw.
trandolapril.tw.
verapamil.tw.
trepostinil.tw.
triamterene.tw.
trichlormethiazide.tw.
or/25–133
18 and 24 and 12
18 and 134 and 12
135 or 136
The search filter for trials at the beginning of the MEDLINE strategy is from the published paper by Glanville (Glanville 2006).
Appendix 3. EMBASE (OvidSP) search strategy
exp randomized controlled trial/
exp randomization/
exp double blind procedure/
exp single blind procedure/
random$.tw.
or/1–5
(animal or animal experiment).sh.
human.sh.
7 and 8
7 not 9
6 not 10
exp clinical trial/
(clin$ adj3 trial$).tw.
((singl$ or doubl$ or trebl$ or tripl$) adj3 (blind$ or mask$)).tw.
exp placebo/
placebo$tw.
random$.tw.
exp experimental design/
exp crossover procedure/
exp control group/
exp latin square design/
or/12–21
22 not 10
23 not 11
exp comparative study/
exp evaluation/
exp prospective study/
(control$ or prospectiv$ or volunteer$).tw.
or/25–28
29 not 10
30 not (11 or 23)
11 or 24 or 31
diabetic retinopathy/
retinopath$.tw.
(vitre$ adj3 detach$).tw.
(retina$ adj3 detach$).tw.
(diabet$ adj3 maculopath$).tw.
or/33–37
exp blood pressure/
glucose blood level/
exp hypertension/
((pressure or glucose or glycem$) adj3 blood$).tw.
hypertens$.tw.
or/39–43
exp antihypertensive agent/
exp dipeptidyl carboxypeptidase inhibitor/
(ACE adj1 inhibitor$).tw.
(antihypertensive adj2 (agent$ or drug$ or medicat$)).tw.
exp calcium channel blocking agent/
(calcium adj1 channel adj1 blocker$).tw.
(calcium adj1 channel adj1 antagonist$).tw.
exp diuretic agent/
diuretic$.tw.
exp beta adrenergic receptor blocking agent/
(adrenergic adj1 beta adj1 antagonist$).tw.
(beta adj1 blocker$).tw.
exp alpha adrenergic receptor blocking agent/
(adrenergic adj1 alpha adj1 antagonist$).tw.
exp vasodilator agent/
exp angiotensin 1 receptor antagonist/
(angiotensin adj3 blocker$).tw.
acebutolol.tw.
amiloride.tw.
amlodipine.tw.
atorvastin.tw.
benazepril.tw.
atenolol.tw.
bendroflumethiazide.tw.
nadolol.tw.
betaxolol.tw.
bisoprolol.tw.
bosentan.tw.
bucindolol.tw.
bumetanide.tw.
candesartan.tw.
captopril.tw.
carteolol.tw.
carvedilol.tw.
chlorothiazide.tw.
chlorthalidone.tw.
clonidine.tw.
diazoxide.tw.
diltiazem.tw.
diltiazem.tw.
doxazosin.tw.
enalapril.tw.
enalapril$.tw.
felodipine.tw.
eplerenone.tw.
epoprostenol.tw.
eprosartan.tw.
esmolol.tw.
(ethacrynic adj1 acid).tw.
fenoldopam.tw.
fosinopril.tw.
furosemide.tw.
guanabenz.tw.
guanadrel.tw.
guanfacine.tw.
hydralazine.tw.
irbesartan.tw.
lisinopril.tw.
losartan.tw.
methyldopa.tw.
metoprolol.tw.
moexipril.tw.
olmesartan.tw.
propranolol.tw.
quinapril.tw.
spironolactone.tw.
telmisartan.tw.
timolol.tw.
triamterene.tw.
valsartan.tw.
hydrochlorothiazide.tw.
iloprost.tw.
indapamide.tw.
isoxsuprine.tw.
isradipine.tw.
labetalol.tw.
lercanidipine.tw.
mecamylamine.tw.
methyclothiazide.tw.
metolazone.tw.
mibefradil.tw.
minoxidil.tw.
nicardipine.tw.
nifedipine.tw.
nisoldipine.tw.
exp nitric oxide/
nitroprusside sodium/
nitroprusside.tw.
omapatrilat.tw.
penbutolol.tw.
perindopril.tw.
phenylbutazone.tw.
phenoxybenzamine.tw.
phentolamine.tw.
pindolol.tw.
polythiazide.tw.
prazosin.tw.
prostacyclin.tw.
ramipril.tw.
reserpine.tw.
sildenafil.tw.
spirapril.tw.
terazosin.tw.
torsemide.tw.
trandolapril.tw.
verapamil.tw.
trepostinil.tw.
triamterene.tw.
trichlormethiazide.tw.
or/45–153
38 and 44
38 and 154
or/155–156
32 and 157
Appendix 4. LILACS search strategy
retinopath$ and blood pressure$ or antihypertensive or angiotensin$ or ACE
Appendix 5. metaRegister of Controlled Trials search strategy
(Diabetic Retinopathy) AND (Blood Pressure OR Antihypertensive OR Angiotensin OR ACE)
Appendix 6. ClinicalTrials.gov search strategy
Diabetic Retinopathy AND (Blood Pressure OR Antihypertensive OR Angiotensin OR ACE)
Appendix 7. ICTRP search strategy
Diabetic Retinopathy AND Blood Pressure
DATA AND ANALYSES
Comparison 1. Blood pressure control versus no (or less) control by type of diabetes, 4 to 5 years
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Incidence of retinopathy at 4 to 5 years | 6 | 3053 | Risk Ratio (M-H, Random, 95% CI) | 0.80 [0.71, 0.92] |
| 1.1 Type 1 diabetes | 1 | 1421 | Risk Ratio (M-H, Random, 95% CI) | 0.82 [0.69, 0.97] |
| 1.2 Type 2 diabetes | 5 | 1632 | Risk Ratio (M-H, Random, 95% CI) | 0.78 [0.63, 0.96] |
| 2 Progression of retinopathy at 4 to 5 years | 4 | 4589 | Risk Ratio (M-H, Random, 95% CI) | 0.88 [0.73, 1.05] |
| 2.1 Type 1 diabetes | 1 | 1905 | Risk Ratio (M-H, Random, 95% CI) | 1.03 [0.82, 1.29] |
| 2.2 Type 2 diabetes | 3 | 2684 | Risk Ratio (M-H, Random, 95% CI) | 0.81 [0.65, 1.01] |
| 3 Combined incidence and progression of DR, 4 to 5 years | 5 | 2587 | Risk Ratio (M-H, Random, 95% CI) | 0.78 [0.63, 0.97] |
| 3.1 Type 1 diabetes | 4 | 2436 | Risk Ratio (M-H, Random, 95% CI) | 0.82 [0.66, 1.03] |
| 3.2 Type 2 diabetes | 1 | 151 | Risk Ratio (M-H, Random, 95% CI) | 0.55 [0.35, 0.88] |
| 4 Incidence of PDR/CSME at 4 to 5 years | 6 | 6573 | Risk Ratio (M-H, Random, 95% CI) | 0.95 [0.83, 1.09] |
| 4.1 Type 1 diabetes | 2 | 2128 | Risk Ratio (M-H, Random, 95% CI) | 1.03 [0.80, 1.32] |
| 4.2 Type 2 diabetes | 4 | 4445 | Risk Ratio (M-H, Random, 95% CI) | 0.89 [0.70, 1.13] |
| 5 Visual acuity (loss of 3 lines or more), 4 to 5 years in type 2 diabetics | 2 | 2326 | Risk Ratio (M-H, Random, 95% CI) | 1.06 [0.85, 1.33] |
| 6 Adverse events - All cause mortality | 7 | 6709 | Risk Ratio (M-H, Random, 95% CI) | 0.86 [0.64, 1.14] |
| 6.1 Type 1 diabetes | 2 | 3322 | Risk Ratio (M-H, Random, 95% CI) | 1.08 [0.50, 2.29] |
| 6.2 Type 2 diabetes | 5 | 3387 | Risk Ratio (M-H, Random, 95% CI) | 0.82 [0.60, 1.12] |
| 7 Adverse events - Hypotension | 3 | 3477 | Risk Ratio (M-H, Random, 95% CI) | 2.08 [1.68, 2.57] |
Comparison 2. Blood pressure control versus no (or less) control by type of hypertension, 4 to 5 years
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Incidence of DR at 4 to 5 years | 6 | 3053 | Risk Ratio (M-H, Random, 95% CI) | 0.80 [0.71, 0.92] |
| 1.1 Normotensives/treated hypertensives | 2 | 1659 | Risk Ratio (M-H, Random, 95% CI) | 0.84 [0.73, 0.98] |
| 1.2 Hypertensives | 4 | 1394 | Risk Ratio (M-H, Random, 95% CI) | 0.72 [0.56, 0.93] |
| 2 Progression of DR, 4 to 5 years | 4 | 4589 | Risk Ratio (M-H, Random, 95% CI) | 0.88 [0.73, 1.05] |
| 2.1 Normotensives/treated hypertensives | 2 | 3810 | Risk Ratio (M-H, Random, 95% CI) | 0.94 [0.81, 1.09] |
| 2.2 Hypertensives | 2 | 779 | Risk Ratio (M-H, Random, 95% CI) | 0.73 [0.51, 1.06] |
| 3 Combined incidence and progression of DR, 4 to 5 years | 5 | 2587 | Risk Ratio (M-H, Random, 95% CI) | 0.78 [0.63, 0.97] |
| 3.1 Normotensives/treated hypertensives | 3 | 1966 | Risk Ratio (M-H, Random, 95% CI) | 0.81 [0.57, 1.16] |
| 3.2 Hypertensives | 2 | 621 | Risk Ratio (M-H, Random, 95% CI) | 0.72 [0.48, 1.08] |
| 4 Incidence of PDR/CSME at 4 to 5 years | 6 | 6573 | Risk Ratio (M-H, Random, 95% CI) | 0.95 [0.83, 1.09] |
| 4.1 Normotensives/treated hypertensives | 3 | 4033 | Risk Ratio (M-H, Random, 95% CI) | 1.01 [0.87, 1.16] |
| 4.2 Hypertensives | 3 | 2540 | Risk Ratio (M-H, Random, 95% CI) | 0.76 [0.56, 1.02] |
| 5 Visual acuity (loss of 3 lines or more), 4 to 5 years | 2 | 2326 | Risk Ratio (M-H, Random, 95% CI) | 1.06 [0.85, 1.33] |
| 5.1 Normotensives/treated hypertensives | 1 | 1546 | Risk Ratio (M-H, Random, 95% CI) | 1.12 [0.95, 1.32] |
| 5.2 Hypertensives | 1 | 780 | Risk Ratio (M-H, Random, 95% CI) | 0.83 [0.51, 1.36] |
| 6 Adverse events - All cause mortality | 7 | 6709 | Risk Ratio (M-H, Random, 95% CI) | 0.86 [0.64, 1.14] |
| 6.1 Normotensives/treated hypertensives | 4 | 5704 | Risk Ratio (M-H, Random, 95% CI) | 1.02 [0.74, 1.42] |
| 6.2 Hypertensives | 3 | 1005 | Risk Ratio (M-H, Random, 95% CI) | 0.51 [0.29, 0.89] |
Comparison 3. Blood pressure control versus no (or less) control by type of diabetes, 1 to 2 years
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Incidence of DR, 1.5 to 2 years | 3 | 1953 | Risk Ratio (M-H, Random, 95% CI) | 0.80 [0.66, 0.98] |
| 1.1 Type 1 diabetes | 2 | 1555 | Risk Ratio (M-H, Random, 95% CI) | 0.83 [0.66, 1.03] |
| 1.2 Type 2 diabetes | 1 | 398 | Risk Ratio (M-H, Random, 95% CI) | 0.74 [0.50, 1.11] |
| 2 Progression of DR, 1.5 to 2 years | 4 | 4132 | Risk Ratio (M-H, Random, 95% CI) | 1.08 [0.89, 1.31] |
| 2.1 Type 1 diabetes | 2 | 1921 | Risk Ratio (M-H, Random, 95% CI) | 1.22 [0.86, 1.73] |
| 2.2 Type 2 diabetes | 2 | 2211 | Risk Ratio (M-H, Random, 95% CI) | 1.02 [0.81, 1.29] |
| 3 Combined incidence and progression of DR, 1.5 to 2 years | 2 | 803 | Risk Ratio (M-H, Random, 95% CI) | 0.54 [0.29, 0.98] |
| 3.1 Type 1 diabetes | 1 | 323 | Risk Ratio (M-H, Random, 95% CI) | 0.29 [0.08, 1.01] |
| 3.2 Type 2 diabetes | 1 | 480 | Risk Ratio (M-H, Random, 95% CI) | 0.62 [0.41, 0.94] |
| 4 Incidence of PDR, 1.5 to 2 years, Type 1 diabetes | 2 | 340 | Risk Ratio (M-H, Random, 95% CI) | 0.58 [0.04, 9.07] |
Analysis 1.1.
Comparison 1 Blood pressure control versus no (or less) control by type of diabetes, 4 to 5 years, Outcome 1 Incidence of retinopathy at 4 to 5 years.
Analysis 1.2.
Comparison 1 Blood pressure control versus no (or less) control by type of diabetes, 4 to 5 years, Outcome 2 Progression of retinopathy at 4 to 5 years.
Analysis 1.3.
Comparison 1 Blood pressure control versus no (or less) control by type of diabetes, 4 to 5 years, Outcome 3 Combined incidence and progression of DR, 4 to 5 years.
Analysis 1.4.
Comparison 1 Blood pressure control versus no (or less) control by type of diabetes, 4 to 5 years, Outcome 4 Incidence of PDR/CSME at 4 to 5 years.
Analysis 1.5.
Comparison 1 Blood pressure control versus no (or less) control by type of diabetes, 4 to 5 years, Outcome 5 Visual acuity (loss of 3 lines or more), 4 to 5 years in type 2 diabetics.
Analysis 1.6.
Comparison 1 Blood pressure control versus no (or less) control by type of diabetes, 4 to 5 years, Outcome 6 Adverse events - All cause mortality.
Analysis 1.7.
Comparison 1 Blood pressure control versus no (or less) control by type of diabetes, 4 to 5 years, Outcome 7 Adverse events - Hypotension.
Analysis 2.1.
Comparison 2 Blood pressure control versus no (or less) control by type of hypertension, 4 to 5 years, Outcome 1 Incidence of DR at 4 to 5 years.
Analysis 2.2.
Comparison 2 Blood pressure control versus no (or less) control by type of hypertension, 4 to 5 years, Outcome 2 Progression of DR, 4 to 5 years.
Analysis 2.3.
Comparison 2 Blood pressure control versus no (or less) control by type of hypertension, 4 to 5 years, Outcome 3 Combined incidence and progression of DR, 4 to 5 years.
Analysis 2.4.
Comparison 2 Blood pressure control versus no (or less) control by type of hypertension, 4 to 5 years, Outcome 4 Incidence of PDR/CSME at 4 to 5 years.
Analysis 2.5.
Comparison 2 Blood pressure control versus no (or less) control by type of hypertension, 4 to 5 years, Outcome 5 Visual acuity (loss of 3 lines or more), 4 to 5 years.
Analysis 2.6.
Comparison 2 Blood pressure control versus no (or less) control by type of hypertension, 4 to 5 years, Outcome 6 Adverse events - All cause mortality.
Analysis 3.1.
Comparison 3 Blood pressure control versus no (or less) control by type of diabetes, 1 to 2 years, Outcome 1 Incidence of DR, 1.5 to 2 years.
Analysis 3.2.
Comparison 3 Blood pressure control versus no (or less) control by type of diabetes, 1 to 2 years, Outcome 2 Progression of DR, 1.5 to 2 years.
Analysis 3.3.
Comparison 3 Blood pressure control versus no (or less) control by type of diabetes, 1 to 2 years, Outcome 3 Combined incidence and progression of DR, 1.5 to 2 years.
Analysis 3.4.
Comparison 3 Blood pressure control versus no (or less) control by type of diabetes, 1 to 2 years, Outcome 4 Incidence of PDR, 1.5 to 2 years, Type 1 diabetes.
Footnotes
CONTRIBUTIONS OF AUTHORS
Conceiving the review: GGS
Designing the review: GGS, SV, RNF
Coordinating the review: SV, MM, XW
Undertaking manual searches: SV
Screening search results: SV, DVD, BSH, XW
Organizing retrieval of papers: SV, MM, XW
Screening retrieved papers against inclusion criteria: SV, DVD, BSH, MM, XW
Appraising quality of papers: SV, DVD, BSH, MM, XW
Abstracting data from papers: SV, DVD, BSH, MM
Writing to authors of papers for additional information: SV, BSH
Obtaining and screening data on unpublished studies: SV, MM
Data management for the review: SV, MM, XW
Entering data into RevMan: SV, MM, XW
Interpretation of data: SV, DVD, BSH, GGS, RNF, XW
Writing the review: DVD, SV, BSH, GGS, RNF, MM
Performing previous work that was the foundation of current study: DVD, GGS, RNF
Guarantor of the review: BSH
DECLARATIONS OF INTEREST
The authors have no conflicts to declare.
DIFFERENCES BETWEEN PROTOCOL AND REVIEW
We added a post hoc secondary outcome (that is incidence of proliferative retinopathy or clinically significant macular edema) and included a combined outcome of incidence or progression of diabetic retinopathy, which was not specified in the protocol. We reported findings from included trials separately for participants with type 1 and type 2 diabetes and by baseline hypertension status (hypertensive or normotensive), although we did not anticipate this approach when we developed the protocol for the review and decided on it post hoc.
References
* Indicates the major publication for the study
References to studies included in this review
- ABCD (1) {published data only}.Schrier RW, Estacio RO, Esler A, Mehler P. Effects of aggressive blood pressure control z in normotensive type 2 diabetic patients on albuminuria, retinopathy and strokes. Kidney International. 2002;61(3):1086–97. doi: 10.1046/j.1523-1755.2002.00213.x. [DOI] [PubMed] [Google Scholar]; * Schrier RW, Estacio RO, Jeffers B. Appropriate Blood Pressure Control in NIDDM (ABCD) Trial. Diabetologia. 1996;39(12):1646–54. doi: 10.1007/s001250050629. [DOI] [PubMed] [Google Scholar]; Schrier RW, Savage S. Appropriate Blood Pressure Control in Type II Diabetes (ABCD Trial): implications for complications. American Journal of Kidney Diseases. 1992;20(6):653–7. doi: 10.1016/s0272-6386(12)70236-6. [DOI] [PubMed] [Google Scholar]
- ABCD (2) {published data only}.Estacio RO, Jeffers BW, Gifford N, Schrier RW. Effect of blood pressure control on diabetic microvascular complications in patients with hypertension and type 2 diabetes. Diabetes Care. 2000;23(Suppl 2):B54–64. [PubMed] [Google Scholar]; Estacio RO, Jeffers BW, Hiatt WR, Biggerstaff SL, Gifford N, Schrier RW. The effect of nisoldipine as compared with enalapril on cardiovascular outcomes in patients with non-insulin dependent diabetes and hypertension. The New England Journal of Medicine. 1998;338(10):645–52. doi: 10.1056/NEJM199803053381003. [DOI] [PubMed] [Google Scholar]; Savage S, Nagel NJ, Estacio RO, Feig PU, MacCarthy EP, Lukken NJ, et al. The ABCD (Appropriate Blood Pressure Control in Diabetes) Trial. Rationale and design of a trial of hypertension control (moderate or intensive) in type II diabetes. Online Journal of Current Clinical Trials. 1993 Nov 24; Doc No 104. [PubMed] [Google Scholar]
- ACCORD EYE {published data only}.Ambrosius WT, Danis RP, Goff DC, Jr, Greven CM, Gerstein HC, Cohen RM, et al. Lack of association between thiazolidinediones and macular edema in type 2 diabetes: the ACCORD eye substudy. Archives of Ophthalmology. 2010;128(3):312–8. doi: 10.1001/archophthalmol.2009.310. [DOI] [PMC free article] [PubMed] [Google Scholar]; Buse JB, Bigger JT, Byington RP, Cooper LS, Cushman WC, Friedewald WT, et al. Action to Control Cardiovascular Risk in Diabetes (ACCORD) Trial: design and methods. American Journal of Cardiology. 2007;99(12A):21i–33i. doi: 10.1016/j.amjcard.2007.03.003. [DOI] [PubMed] [Google Scholar]; Chew EY, Ambrosius WT. Update of the ACCORD Eye Study. The New England Journal of Medicine. 2011;364(2):188–9. doi: 10.1056/NEJMc1011499. [DOI] [PubMed] [Google Scholar]; Chew EY, Ambrosius WT, Davis MD, Danis RP, Gangaputra S, Greven CM, et al. Effects of medical therapies on retinopathy progression in type 2 diabetes. The New England Journal of Medicine. 2010;363(3):233–44. doi: 10.1056/NEJMoa1001288. [DOI] [PMC free article] [PubMed] [Google Scholar]; * Chew EY, Ambrosius WT, Howard LT, Greven CM, Johnson S, Danis RP, et al. Rationale, design, and methods of the Action to Control Cardiovascular Risk in Diabetes Eye Study (ACCORD-EYE) American Journal of Cardiology. 2007;99(12A):103i–11i. doi: 10.1016/j.amjcard.2007.03.028. [DOI] [PubMed] [Google Scholar]; Cushman WC, Grimm RH, Cutler JA, Evan GW, Capes S, Corson MA. Rationale and design for the blood pressure intervention of the Action to Control Cardiovascular Risk in Diabetes (ACCORD) trial. American Journal of Cardiology. 2007;99(12A):44i–55i. doi: 10.1016/j.amjcard.2007.03.005. [DOI] [PubMed] [Google Scholar]; Ismail-Beigi F, Craven T, Banerji MA, Basile J, Calles J, Cohen RM, et al. Effect of intensive treatment of hyperglycaemia on microvascular outcomes in type 2 diabetes: an analysis of the ACCORD randomised trial. Lancet. 2010;376(9739):419–30. doi: 10.1016/S0140-6736(10)60576-4. [DOI] [PMC free article] [PubMed] [Google Scholar]; Ismail-Beigi F, Craven TE, O’Connor PJ, Karl D, Calles-Escandon J, Hramiak I, et al. Combined intensive blood pressure and glycemic control does not produce an additive benefit on microvascular outcomes in type 2 diabetic patients. Kidney International. 2012;81(6):586–94. doi: 10.1038/ki.2011.415. [DOI] [PMC free article] [PubMed] [Google Scholar]; Sullivan MD, Anderson RT, Aron D, Atkinson HH, Bastien A, Chen J, et al. Health-related quality of life and cost-effectiveness components of the Action to Control Cardiovascular Risk in Diabetes (ACCORD) trial: rationale and design. American Journal of Cardiology. 2007;99(12A):90i–102i. doi: 10.1016/j.amjcard.2007.03.027. [DOI] [PubMed] [Google Scholar]
- ADVANCE/AdRem {published data only}.ADVANCE Collaborative Group. ADVANCE - Action in Diabetes and Vascular Disease: patient recruitment and characteristics of the study population at baseline. Diabetic Medicine. 2005;22(7):882–8. doi: 10.1111/j.1464-5491.2005.01596.x. [DOI] [PubMed] [Google Scholar]; ADVANCE Collaborative Group. Effects of a fixed combination of perindopril and indapamide on macrovascular and microvascular outcomes in patients with type 2 diabetes mellitus (the ADVANCE trial): a randomised controlled trial. Lancet. 2007;370(9590):829–40. doi: 10.1016/S0140-6736(07)61303-8. [DOI] [PubMed] [Google Scholar]; ADVANCE Collaborative Group. Intensive blood glucose control and vascular outcomes in patients with type 2 diabetes. The New England Journal of Medicine. 2008;358(24):2560–72. doi: 10.1056/NEJMoa0802987. [DOI] [PubMed] [Google Scholar]; ADVANCE Management Committee. Study rationale and design of ADVANCE: Action in Diabetes and Vascular Disease - preterax and diamicron MR controlled evaluation. Diabetologia. 2001;44(9):1118–20. doi: 10.1007/s001250100612. [DOI] [PubMed] [Google Scholar]; Beulens JWJ, Patel A, Vingerling JR, Cruickshank JK, Hughes AD, Stanton A, et al. Effects of blood pressure lowering and intensive glucose control on the incidence and progression of retinopathy in patients with type 2 diabetes mellitus: a randomized controlled trial. Diabetologia. 2009;52(10):2027–46. doi: 10.1007/s00125-009-1457-x. [DOI] [PubMed] [Google Scholar]; * Patel A, Chalmers J, Neal B, Chapman N, Girgis S, MacMahon S. Blood pressure lowering in diabetes: a brief review of current evidence and description of a new trial. Clinical and Experimental Pharmacology and Physiology. 2001;28(12):1108–11. doi: 10.1046/j.1440-1681.2001.03581.x. [DOI] [PubMed] [Google Scholar]; Poulter NR. Blood pressure and glucose control in subject with diabetes: new analysis from ADVANCE. Journal of Hypertension. 2009;27(1):S3–8. doi: 10.1097/01.hjh.0000354417.70192.be. [DOI] [PubMed] [Google Scholar]; Stolk RP, Vingerling JR, Cruickshank JK, Hughes AD, Stanton A, Juming L, et al. Rationale and design of the AdRem study: evaluating the effects of blood pressure lowering and intensive glucose control on vascular retinal disorders in patients with type 2 diabetes mellitus. Contemporary Clinical Trials. 2007;28(1):6–17. doi: 10.1016/j.cct.2006.08.011. [DOI] [PubMed] [Google Scholar]; Stolk RP, van Schooneveld MJ, Cruickshank JK, Hughes AD, Stanton A, Lu J, et al. Retinal vascular lesions in patients of Caucasian and Asian origin with type 2 diabetes: baseline results from the ADVANCE Retinal Measurements (AdRem) study. Diabetes Care. 2008;31(4):708–13. doi: 10.2337/dc07-1657. [DOI] [PubMed] [Google Scholar]
- BENEDICT {published data only}.BENEDICT Group. The BErgamo NEphrologic DIabetes Complications Trial (BENEDICT) Controlled Clinical Trials. 2003;24(4):442–61. doi: 10.1016/s0197-2456(03)00028-x. [DOI] [PubMed] [Google Scholar]; Ruggenenti P, Fassi A, Parvanova I, Bruno S, Iliev IP, Brusegan V, et al. Preventing microalbuminuria in type 2 diabetes. The New England Journal of Medicine. 2004;351(19):1941–51. doi: 10.1056/NEJMoa042167. [DOI] [PubMed] [Google Scholar]; Ruggenenti P, Iliev I, Filipponi M, Tadini S, Perna A, Ganeva M. Effect of trandolapril on regression of retinopathy in hypertensive patients with type 2 diabetes: a prespecified analysis of the benedict trial. Journal of Ophthalmology. 2010;2010 doi: 10.1155/2010/106384. Article ID 106384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chase {published data only}.Chase HP, Garg SK, Harris S, Hoops S, Jackson WE, Holmes DL. Angiotensin-converting enzyme inhibitor treatment for young normotensive diabetic subjects: a two-year trial. Annals of Ophthalmology. 1993;25(8):284–9. [PubMed] [Google Scholar]
- DEMAND {published data only}.Ruggenenti P, Lauria G, Iliev IP, Fassi A, Ilieva AP, Rota S. Effects of manidipine and delapril in hypertensive patients with type 2 diabetes mellitus: the Delapril and Manidipine for Nephroprotection in Diabetes (DEMAND) randomized clinical trial. Hypertension. 2011;58(5):776–83. doi: 10.1161/HYPERTENSIONAHA.111.174474. [DOI] [PubMed] [Google Scholar]
- DIRECT Prevent 1 {published data only}.Chaturvedi N, Porta M, Klein R, Orchard T, Fuller J, Parving HH, et al. Effect of candesartan on prevention (DIRECT-Prevent 1) and progression (DIRECT-Protect 1) of retinopathy in type 1 diabetes: randomised, placebo-controlled trials. Lancet. 2008;372(9647):1394–402. doi: 10.1016/S0140-6736(08)61412-9. [DOI] [PubMed] [Google Scholar]; * Chaturvedi N DIRECT Programme Study Group. The DIabetic REtinopathy Candesartan Trials (DIRECT) Programme, rationale and study design. Journal of the Renin-Angiotensin-Aldosterone System. 2002;3(4):255–61. doi: 10.3317/jraas.2002.047. [DOI] [PubMed] [Google Scholar]; DIRECT Programme Study Group. The DIabetic REtinopathy Candesartan Trials (DIRECT) Programme: baseline characteristics. Journal of the Renin-Angiotensin-Aldosterone System. 2005;6(1):25–32. doi: 10.3317/jraas.2005.003. [DOI] [PubMed] [Google Scholar]; Sjolie AK, Klien R, Portat M, Orchard T, Fuller J, Parving HH, et al. Retinal microaneurysm count predicts progression and regression of diabetic retinopathy. Post-hoc results from the DIRECT Programme. Diabetic Medicine. 2011;28(3):345–51. doi: 10.1111/j.1464-5491.2010.03210.x. [DOI] [PubMed] [Google Scholar]
- DIRECT Protect 1 {published data only}.Chaturvedi N, Porta M, Klein R, Orchard T, Fuller J, Parving HH, et al. Effect of candesartan on prevention (DIRECT-Prevent 1) and progression (DIRECT-Protect 1) of retinopathy in type 1 diabetes: randomised, placebo-controlled trials. Lancet. 2008;372(9647):1394–402. doi: 10.1016/S0140-6736(08)61412-9. [DOI] [PubMed] [Google Scholar]; * Chaturvedi N DIRECT Programme Study Group. DIabetic REtinopathy Candesartan Trials (DIRECT) Programme, rationale and study design. Journal of the Renin-Angiotensin-Aldosterone System. 2002;3(4):255–61. doi: 10.3317/jraas.2002.047. [DOI] [PubMed] [Google Scholar]; DIRECT Programme Study Group. DIabetic REtinopathy Candesartan Trials (DIRECT) Programme: baseline characteristics. Journal of the Renin-Angiotensin-Aldosterone System. 2005;6(1):25–32. doi: 10.3317/jraas.2005.003. [DOI] [PubMed] [Google Scholar]
- DIRECT Protect 2 {published data only}.Chaturvedi N DIRECT Programme Study Group. DIabetic REtinopathy Candesartan Trials (DIRECT) Programme, rationale and study design. Journal of the Renin-Angiotensin-Aldosterone System. 2002;3(4):255–61. doi: 10.3317/jraas.2002.047. [DOI] [PubMed] [Google Scholar]; DIRECT Programme Study Group. DIabetic REtinopathy Candesartan Trials (DIRECT) Programme: baseline characteristics. Journal of Renin-Angiotensin-Aldosterone System. 2005;6(1):25–32. doi: 10.3317/jraas.2005.003. [DOI] [PubMed] [Google Scholar]; * Sjolie AK, Klein R, Porta M, Orchard T, Fuller J, Parving HH, et al. Effect of candesartan on progression and regression of retinopathy in type 2 diabetes (DIRECT-Protect 2): a randomised placebo-controlled trial. Lancet. 2008;372(9647):1385–93. doi: 10.1016/S0140-6736(08)61411-7. [DOI] [PubMed] [Google Scholar]
- EUCLID {published data only}.Chaturvedi N, Fuller JH, Pokras F, Rottiers R, Papazoglou N, Aiello LP, et al. Circulating plasma vascular endothelial growth factor and microvascular complications of type 1 diabetes mellitus: the influence of ACE inhibition. Diabetes Medicine. 2001;18(4):288–94. doi: 10.1046/j.1464-5491.2001.00441.x. [DOI] [PubMed] [Google Scholar]; Chaturvedi N, Sjolie AK, Stephenson JM, Abrahamian H, Keipes M, Castellarin A, et al. Effect of lisinopril on progression of retinopathy in normotensive people with type 1 diabetes. Lancet. 1998;351(9095):28–31. doi: 10.1016/s0140-6736(97)06209-0. [DOI] [PubMed] [Google Scholar]; * EUCLID Study Group. Randomised placebo-controlled trial of lisinopril in normotensive patients with insulin-dependent diabetes and normoalbuminuria or microalbuminuria. Lancet. 1997;349(9068):1787–92. [PubMed] [Google Scholar]; Sjolie AK, Chaturvedi N, Fuller J EUCLID Study Group. Effect of lisinopril on progression of retinopathy and microalbuminuria in normotensive subjects with insulin-dependent diabetes mellitus [Effekt af lisinopril på progression af retinopati og mikroalbuminuri hos normotensive personer med insulinafhængig diabetes mellitus] Ugeskrift for Laeger. 1999;161(7):949–52. [PubMed] [Google Scholar]; Sjolie AK, Stephenson J, Aldington S, Kohner E, Janka H, Stevens L, et al. Retinopathy and vision loss in insulin-dependent diabetes in Europe. The EURODIAB IDDM Complications Study. Ophthalmology. 1997;104(2):252–60. doi: 10.1016/s0161-6420(97)30327-3. [DOI] [PubMed] [Google Scholar]
- Pradhan {published data only}.Pradhan R, Fong D, March C, Jack R, Rezapour G, Norris K, et al. Angiotensin-converting enzyme inhibition for the treatment of moderate to severe diabetic retinopathy in normotensive type 2 diabetic patients. A pilot study. Journal of Diabetes and Its Complications. 2002;16(6):377–81. doi: 10.1016/s1056-8727(02)00188-5. [DOI] [PubMed] [Google Scholar]
- RASS {published data only}.Klein R, Moss SE, Sinaiko AR, Zinman B, Gardiner R, Suissa S, et al. The relation of ambulatory blood pressure and pulse rate to retinopathy in type 1 diabetes mellitus. The Renin-Angiotensin System Study. Ophthalmology. 2006;113(12):2231–6. doi: 10.1016/j.ophtha.2006.06.003. [DOI] [PubMed] [Google Scholar]; Klein R, Zinman B, Gardiner R, Suissa S, Donnelly SM, Sinaiko AR, et al. The relationship of diabetic retinopathy to preclinical diabetic glomerulopathy lesions in type 1 diabetic patients. The Renin-Angiotensin System Study. Diabetes. 2005;54(2):527–33. doi: 10.2337/diabetes.54.2.527. [DOI] [PubMed] [Google Scholar]; Mauer M, Zinman B, Gardiner R, Drummond KN, Suissa S, Donnelly SM, et al. ACE-I and ARBs in early diabetic retinopathy. Journal of the Renin-Angiotensin-Aldosterone System. 2002;3(4):262–9. doi: 10.3317/jraas.2002.048. [DOI] [PubMed] [Google Scholar]; Mauer M, Zinman B, Gardiner R, Suissa S, Sinaiko A, Strand T, et al. Renal and retinal effects of enalapril and losartan in type 1 diabetes. The New England Journal of Medicine. 2009;361(1):40–51. doi: 10.1056/NEJMoa0808400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steno-2 {published data only}.Gaede P, Vedel P, Larsen N, Jensen GVH, Parving HH, Pedersen O. Multifactorial intervention and cardiovascular disease in patients with type 2 diabetes. The New England Journal of Medicine. 2003;348(5):383–93. doi: 10.1056/NEJMoa021778. [DOI] [PubMed] [Google Scholar]; Gaede P, Vedel P, Parving HH, Pedersen O. Intensified multifactorial intervention in patients with type 2 diabetes mellitus and microalbuminuria: the Steno type 2 randomised study. Lancet. 1999;353(9153):617–22. doi: 10.1016/S0140-6736(98)07368-1. [DOI] [PubMed] [Google Scholar]; * Vaag AA. Glycemic control and prevention of microvascular and macrovascular disease in the Steno 2 study. Endocrine Practice. 2006;12(Suppl 1):89–92. doi: 10.4158/EP.12.S1.89. [DOI] [PubMed] [Google Scholar]
- UKPDS/HDS {published data only}.Clarke PM, Gray AM, Briggs A, Stevens RJ, Matthews DR, Holman RR, et al. Cost-utility analyses of intensive blood glucose and tight blood pressure control in type 2 diabetes (UKPDS 72) Diabetologia. 2005;48(5):868–77. doi: 10.1007/s00125-005-1717-3. [DOI] [PubMed] [Google Scholar]; Gray A, Clarke P, Farmer A, Holman R. Implementing intensive control of blood glucose concentration and blood pressure in type 2 diabetes in England: cost analysis (UKPDS 63) BMJ. 2002;325(7369):860. doi: 10.1136/bmj.325.7369.860. [DOI] [PMC free article] [PubMed] [Google Scholar]; Gray A, Clarke P, Raikou M, Adler A, Stevens R, Neil A, et al. An economic evaluation of atenolol vs. captopril in patients with type 2 diabetes (UKPDS 54) Diabetes Medicine. 2001;18(6):438–44. doi: 10.1046/j.1464-5491.2001.00485.x. [DOI] [PubMed] [Google Scholar]; Holman RR, Paul SK, Bethel MA, Andrew H, Neil W, Matthews DR. Long-term follow-up after tight control of blood pressure in type 2 diabetes. The New England Journal of Medicine. 2008;359(15):1565–76. doi: 10.1056/NEJMoa0806359. [DOI] [PubMed] [Google Scholar]; Hypertension in Diabetes Study Group. Hypertension in Diabetes Study III. Prospective study of therapy of hypertension in type 2 diabetic patients: efficacy of ACE inhibition and β-blockade. Diabetic Medicine. 1994;11(8):773–82. [PubMed] [Google Scholar]; Hypertension in Diabetes Study Group. Hypertension in Diabetes Study IV. Therapeutic requirements to maintain tight blood pressure control. Diabetologia. 1996;39(12):1554–61. doi: 10.1007/s001250050614. [DOI] [PubMed] [Google Scholar]; Kohner EM, Stratton IM, Aldington SJ, Turner RC, Matthews DR UK Prospective Diabetes Study Group. Microaneurysms in the development of diabetic retinopathy (UKPDS 42) Diabetologia. 1999;42(9):1107–12. doi: 10.1007/s001250051278. [DOI] [PubMed] [Google Scholar]; Stratton IM, Kohner EM, Aldington SJ, Turner RC, Holman RR, Manley SE, et al. UKPDS 50: Risk factors for incidence and progression of retinopathy in type II diabetes over 6 years from diagnosis. Diabetologia. 2001;44(2):156–63. doi: 10.1007/s001250051594. [DOI] [PubMed] [Google Scholar]; UK Prospective Diabetes Study (UKPDS) Group. Intensive blood-glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes (UKPDS 33) Lancet. 1998;352(9131):837–53. [PubMed] [Google Scholar]; UK Prospective Diabetes Study Group. Cost effectiveness analysis of improved blood pressure control in hypertensive patients with type 2 diabetes: UKPDS 40. BMJ. 1998;317(7160):720–6. [PMC free article] [PubMed] [Google Scholar]; UK Prospective Diabetes Study Group. Efficacy of atenolol and captopril in reducing risk of macrovascular and microvascular complications in type 2 diabetes: UKPDS 39. BMJ. 1998;317(7160):713–20. [PMC free article] [PubMed] [Google Scholar]; UK Prospective Diabetes Study Group. Quality of life in type 2 diabetic patients is affected by complications but not by intensive policies to improve blood glucose or blood pressure control (UKPDS 37) Diabetes Care. 1999;22(7):1125–36. doi: 10.2337/diacare.22.7.1125. [DOI] [PubMed] [Google Scholar]; UK Prospective Diabetes Study Group. Risks of progression of retinopathy and vision loss related to tight blood pressure control in type 2 diabetes mellitus. UKPDS 69. Archives of Ophthalmology. 2004;122(11):1631–40. doi: 10.1001/archopht.122.11.1631. [DOI] [PubMed] [Google Scholar]; UK Prospective Diabetes Study Group. Tight blood pressure control and risk of macrovascular and microvascular complications in type 2 diabetes: UKPDS 38. BMJ. 1998;317(7160):703–13. [PMC free article] [PubMed] [Google Scholar]; UK Prospective Diabetes Study Group. UK Prospective Diabetes Study (UKPDS). VIII. Study design, progress and performance. Diabetologia. 1991;34(12):877–90. [PubMed] [Google Scholar]
References to studies excluded from this review
- Araki 2012 {published data only}.Araki A, Iimuro S, Sakurai T, Umegaki H, Iijima K, Nakano H, et al. Long-term multiple risk factor interventions in Japanese elderly diabetic patients: the Japanese Elderly Diabetes Intervention Trial-study design, baseline characteristics and effects of intervention. Geriatrics and Gerontology International. 2012;12(Suppl 1):7–17. doi: 10.1111/j.1447-0594.2011.00808.x. [DOI] [PubMed] [Google Scholar]
- Auyanet 2010 {published data only}.Auyanet I, Rodriguez LJ, Esparza N, Cabrera F, Rossique P, Suria S, et al. Does carvedilol minimize the requirements for laser photocoagulation in diabetic retinopathy? [Minimiza el carvedilol los requerimientos de fotocoagulacion laser en la retinopatia diabetica?] Nefrologia. 2010;30(issue 4):473–4. doi: 10.3265/Nefrologia.pre2010.May.10386. [DOI] [PubMed] [Google Scholar]
- CALM-II {published data only}.Andersen NH, Knudsen ST, Poulsen PL, Poulsen SH, Helleberg K, Eiskjaer H, et al. Dual blockade with candesartan cilexetil and lisinopril in hypertensive patients with diabetes mellitus: rationale and design. Journal of the Renin-Angiotensin-Aldosterone System. 2003;4(2):96–9. doi: 10.3317/jraas.2003.019. [DOI] [PubMed] [Google Scholar]; Andersen NH, Poulsen PL, Knudsen ST, Poulsen SH, Eiskjaer H, Hansen KW, et al. Long-term dual blockade with candesartan and lisinopril in hypertensive patients with diabetes: the CALM II study. Diabetes Care. 2005;28(2):273–7. doi: 10.2337/diacare.28.2.273. [DOI] [PubMed] [Google Scholar]
- Chang 2011 {published data only}.Chang CH, Chuang LM. Effects of medical therapies on retinopathy progression in type 2 diabetes: Is blood pressure control the lower the better? Journal of Diabetes Investigation. 2011;2(2):101–3. doi: 10.1111/j.2040-1124.2010.00085.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DCCT {published data only}.Genuth S, Lipps J, Lorenzi G, Nathan DM, Davis MD, Lachin JM, et al. Effect of intensive therapy on the microvascular complications of type 1 diabetes mellitus. JAMA. 2002;287(19):2563–9. doi: 10.1001/jama.287.19.2563. [DOI] [PMC free article] [PubMed] [Google Scholar]; The Diabetes Control and Complications Trial Research Group. Effect of intensive diabetes management on macrovascular events and risk factors in the Diabetes Control and Complications Trial. American Journal of Cardiology. 1995;75(14):894–903. doi: 10.1016/s0002-9149(99)80683-3. [DOI] [PubMed] [Google Scholar]; The Diabetes Control and Complications Trial/Epidemiology of Diabetes Interventions and Complications Research Group. Epidemiology of Diabetes Interventions and Complications (EDIC). Design, implementation, and preliminary results of a long-term follow-up of the Diabetes Control and Complications Trial cohort. Diabetes Care. 1999;22(1):99–111. doi: 10.2337/diacare.22.1.99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Durruty 2000 {published data only}.Durruty P, Carpentier C, Krause P, Garcia de los Rios M. Evaluation of retinal involvement in type 2 diabetics with microalbuminuria. [Evaluacion del compromiseo retinal en diabeticos tipo 2 microalbuminuricos]. Revista Medica de Chile. 2000;128(10):1085–92. [PubMed] [Google Scholar]
- Faguer de Moustier 1989 {published data only}.Faguer de Moustier B, Paoli V, Tchobroutsky G. Metabolic controlled trial of nicardipine in type 2 diabetic patients with slight hypertension. Current Therapeutic Research, Clinical and Experimental. 1989;45(4):690–704. [Google Scholar]
- Harrold 1969 {published data only}.Harrold BP, Marmion VJ, Gough KR. A double-blind controlled trial of clofibrate in the treatment of diabetic retinopathy. Diabetes. 1969;18(5):285–91. doi: 10.2337/diab.18.5.285. [DOI] [PubMed] [Google Scholar]
- Jackson 1992 {published data only}.Jackson WE, Holmes DL, Garg SK, Harris S, Chase HP. Angiotensin-converting enzyme inhibitor therapy and diabetic retinopathy. Annals of Ophthalmology. 1992;24(3):99–103. [PubMed] [Google Scholar]
- JDCS 2011 {published data only}.Kawasaki R, Tanaka S, Tanaka S, Yamamoto T, Sone H, Ohashi Y, et al. Incidence and progression of diabetic retinopathy in Japanese adults with type 2 diabetes: 8 year follow-up study of the Japan Diabetes Complications Study (JDCS) Diabetologia. 2011;54(9):2288–94. doi: 10.1007/s00125-011-2199-0. [DOI] [PubMed] [Google Scholar]; Sone H, Tanaka S, Iimuro S, Tanaka S, Oida K, Yamasaki Y, et al. Long-term lifestyle intervention lowers the incidence of stroke in Japanese patients with type 2 diabetes: a nationwide multicentre randomised controlled trial (the Japan Diabetes Complications Study) Diabetologia. 2010;53(3):419–28. doi: 10.1007/s00125-009-1622-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Larsen 1990 {published data only}.Larsen M, Hommel E, Parving HH, Lund-Andersen H. Protective effect of captopril on the blood-retina barrier in normotensive insulin-dependent diabetic patients with nephropathy and background retinopathy. Graefe’s Archive of Clinical and Experimental Ophthalmology. 1990;228(6):505–9. doi: 10.1007/BF00918480. [DOI] [PubMed] [Google Scholar]
- Lehsten 1996 {published data only}.Lehsten K, Becker B, Michaelis D, Eggert HJ, Rjasanowski I, Salzsieder E. On the prospective significance of age at onset of diabetes, metabolic control, and hypertension for the development of diabetic retinopathy in patients with IDDM. Diabetes und Stoffwechsel. 1996;5(1):18–25. [Google Scholar]
- Malik 1998 {published data only}.Malik RA, Williamson S, Abbott C, Carrington AL, Iqbal J, Schady W, et al. Effect of angiotensin-converting-enzyme (ACE) inhibitor trandolapril on human diabetic neuropathy: randomised double-blind controlled trial. Lancet. 1998;352(9145):1978–81. doi: 10.1016/S0140-6736(98)02478-7. [DOI] [PubMed] [Google Scholar]
- MCSG 1995 {published data only}.Microalbuminuria Collaborative Study Group. Intensive therapy and progression to clinical albuminuria in patients with insulin dependent diabetes mellitus and microalbuminuria. BMJ. 1995;311(7011):973–7. [PMC free article] [PubMed] [Google Scholar]
- Mehlsen 2011 {published data only}.Mehlsen J, Jeppesen P, Erlandsen M, Poulsen PL, Bek T. Lack of effect of short-term treatment with amlodipine and lisinopril on retinal autoregulation in normotensive patients with type 1 diabetes and mild diabetic retinopathy. Acta Ophthalmologica. 2011;89(8):764–8. doi: 10.1111/j.1755-3768.2009.01847.x. [DOI] [PubMed] [Google Scholar]
- Newsom 1991 {published data only}.Newsom RS, Rassam SM, Kohner EM. The effect of beta blockers on retinal blood flow in diabetic patients. European Journal of Ophthalmology. 1991;1(3):131–6. doi: 10.1177/112067219100100305. [DOI] [PubMed] [Google Scholar]
- Patel 1998 {published data only}.Patel V, Rassam SM, Chen HC, Jones M, Kohner EM. Effect of angiotensin-converting enzyme inhibition with perindopril and beta-blockade with atenolol on retinal blood flow in hypertensive diabetic subjects. Metabolism: Clinical and Experimental. 1998;47(12 Suppl 1):28–33. doi: 10.1016/s0026-0495(98)90368-7. [DOI] [PubMed] [Google Scholar]
- Porush 2000 {published data only}.Porush JG. The benefits of angiotensin II receptor antagonists in high-risk hypertensive patients with diabetes. European Heart Journal Supplements. 2000;2(B):B22–7. [Google Scholar]
- Rachmani 2000 {published data only}.Rachmani R, Lidar M, Levy Z, Ravid M. Effect of enalapril on the incidence of retinopathy in normotensive patients with type 2 diabetes. European Journal of Internal Medicine. 2000;11(1):48–50. [Google Scholar]
- Rachmani 2002 {published data only}.Rachmani R, Levi Z, Slavachevski I, Avin M, Ravid M. Teaching patients to monitor their risk factors retards the progression of vascular complications in high-risk patients with type 2 diabetes mellitus-a randomized prospective study. Diabetic Medicine. 2002;19(5):385–92. doi: 10.1046/j.1464-5491.2002.00701.x. [DOI] [PubMed] [Google Scholar]
- Rassam 1997 {published data only}.Rassam SMB, Patel VJ, Kohner E. Effect of ACE-inhibitors on retinopathy score and retinal hemodynamics in normotensive diabetic subjects. American Academy of Ophthalmology. 1997:207. [Google Scholar]
- Schwartz 1998 {published data only}.Schwartz MM, Lewis EJ, Leonard-Martin T, Lewis JB, Batlle D The Collaborative Study Group. Renal pathology patterns in type II diabetes mellitus: relationship with retinopathy. Nephrology Dialysis Transplantation. 1998;13(10):2547–52. doi: 10.1093/ndt/13.10.2547. [DOI] [PubMed] [Google Scholar]
- Wang 2012 {published data only}.Wang N, Zheng Z, Jin HY, Xu X. Treatment effects of captopril on non-proliferative diabetic retinopathy. Chinese Medical Journal. 2012;125(2):287–92. [PubMed] [Google Scholar]
References to studies awaiting assessment
- ABCD-2V {published data only}.Bedigian M. Improving the prognosis of diabetic patients: evaluating the role of intensive versus moderate blood pressure control with selective angiotensin II receptor block (ARB) therapy. Journal of the Renin-Angiotensin-Aldosterone System. 2000;1(Suppl 2):25–8. doi: 10.3317/jraas.2000.050. [DOI] [PubMed] [Google Scholar]; Bedigian MP, Estacio RO, Jefferes BW, Biggerstaff S, Schrier RW. Baseline characteristics of the hypertensive cohort of the appropriate blood pressure control in diabetes trial -part 2 with valsartan (ABCD-2V) American Journal of Hypertension. 2000;13(4 Pt 2):56A–7A. [Google Scholar]; * Estacio RO, Coll JR, Tran ZV, Schrier RW. Effect of intensive blood pressure control with valsartan on urinary albumin excretion in normotensive patients with type 2 diabetes. American Journal of Hypertension. 2006;19(12):1241–8. doi: 10.1016/j.amjhyper.2006.05.011. [DOI] [PubMed] [Google Scholar]; Shrier RW, Estacio RO, Jeffers BW, Biggerstaff S, Krinsk E, Pincus JR, et al. ABCD-2V: Appropriate blood pressure control in diabetes - part 2 with valsartan. American Journal of Hypertention. 1999;12(4 Pt 2):141A. [Google Scholar]
- ADDITION 2014 {published data only}.Sandbæk A, Griffin SJ, Sharp SJ, Simmons RK, Borch-Johnsen K, Rutten GE, et al. Effect of early multifactorial therapy compared with routine care on microvascular outcomes at 5 years in people with screen-detected diabetes: a randomized controlled trial: The ADDITION-Europe Study. Diabetes Care. 2014;37(7):2015–23. doi: 10.2337/dc13-1544. [DOI] [PubMed] [Google Scholar]
- ROADMAP {published data only}.Haller H, Viberti GC, Mimran A, Remuzzi G, Rabelink AJ, Ritz E, et al. Preventing microalbuminuria in patients with diabetes: rationale and design of the Randomised Olmesartan and Diabetes Microalbuminuria Prevention (ROADMAP) study. Journal of Hypertension. 2006;24(2):403–8. doi: 10.1097/01.hjh.0000202820.56201.e6. [DOI] [PubMed] [Google Scholar]
References to ongoing studies
- AdDIT {published data only}.AdDIT Research Group. Adolescent type 1 diabetes cardio-renal intervention trial (AdDIT) BMC Pediatrics. 2009;9:79. doi: 10.1186/1471-2431-9-79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- NCT00134160 {published data only}. NCT00134160. [accessed 30 July 2013];The study comparing the incidence of cardiovascular events between high-dose ARB monotherapy and combination therapy with ARB and calcium channel blocker in Japanese elderly hypertensive patients at high cardiovascular risk. clinicaltrials.gov/ct2/show/NCT00134160.
- NCT00300976 {published data only}. NCT00300976. [accessed 30 July 2013];A randomized controlled study of the intensive therapy and the conventional therapy for the suppression of the vascular complications in the type 2 diabetic patients. clinicaltrials.gov/ct2/show/NCT00300976.
Additional references
- ADA 1998.American Diabetes Association. Diabetic retinopathy. Diabetes Care. 1998;21(1):157–9. [PubMed] [Google Scholar]
- Buch 2004.Buch H. Prevalence and causes of visual impairment and blindness among Scandinavian adults: the Copenhagen City Eye Study. Ophthalmology. 2004;111(1):53–61. doi: 10.1016/j.ophtha.2003.05.010. [DOI] [PubMed] [Google Scholar]
- CDC 2011.Centers for Disease Control and Prevention. National diabetes fact sheet: national estimates and general information on diabetes and prediabetes in the United States, 2011. Atlanta (GA): U.S. Department of Health and Human Services, Centers for Disease Control and Prevention; 2011. [Google Scholar]
- Chew 1996.Chew E. Association of elevated serum lipid levels with retinal hard exudates in diabetic retinopathy. Early Treatment Diabetic Retinopathy Study (ETDRS) Report 22. Archives of Ophthalmology. 1996;114(9):1079–84. doi: 10.1001/archopht.1996.01100140281004. [DOI] [PubMed] [Google Scholar]
- Cushman 2007.Cushman WC, Grimm RH, Jr, Cutler JA, Evans GW, Capes S, Corson MA, et al. Rationale and design for the blood pressure intervention of the Action to Control Cardiovascular Risk in Diabetes (ACCORD) trial. American Journal of Cardiology. 2007;99(12A):44i–55i. doi: 10.1016/j.amjcard.2007.03.005. [DOI] [PubMed] [Google Scholar]
- DCCT 1993.The Diabetes Control and Complications Trial Research Group. The effect of intensive treatment of diabetes on the development and progression of long-term complications in insulin-dependent diabetes mellitus. The New England Journal of Medicine. 1993;329(14):977–86. doi: 10.1056/NEJM199309303291401. [DOI] [PubMed] [Google Scholar]
- Desai 2001.Desai M, Pratt LA, Lentzner H, Robinson KN. Trends in vision and hearing among older Americans. Aging Trends. 2001;(2):1–8. doi: 10.1037/e620682007-001. [DOI] [PubMed] [Google Scholar]
- DRCR.net 2010.Elman MJ, Aiello LP, Beck RW, Bressler NM, Bressler SB, Edwards AR, et al. Diabetic Retinopathy Clinical Research Network. Randomized trial evaluating ranibizumab plus prompt or deferred laser or triamcinolone plus prompt laser for diabetic macular edema. Ophthalmology. 2010;117(6):1064–77. doi: 10.1016/j.ophtha.2010.02.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DRS10 1985.Rand LI, Prud’homme GJ, Ederer F, Canner PL. Factors influencing the development of visual loss in advanced diabetic retinopathy. Diabetic Retinopathy Study (DRS) report number 10. Investigative Ophthalmology and Visual Science. 1985;26(7):983–91. [PubMed] [Google Scholar]
- DRS2 1978.The Diabetes Retinopathy Study Research Group. Photocoagulation treatment of proliferative diabetic retinopathy: the second report of Diabetic Retinopathy Study findings. Ophthalmology. 1978;85(1):82–106. doi: 10.1016/s0161-6420(78)35693-1. [DOI] [PubMed] [Google Scholar]
- DRS5 1981.The Diabetic Retinopathy Study Research Group. Photocoagulation treatment of proliferative diabetic retinopathy: relationship of adverse treatment effects to retinopathy severity. Diabetic Retinopathy Study report number 5. Developments in Ophthalmology. 1981;2:248–56. [PubMed] [Google Scholar]
- DRS8 1981.The Diabetic Retinopathy Study Research Group. Photocoagulation treatment of proliferative diabetic retinopathy. Clinical application of Diabetic Retinopathy Study (DRS) findings. DRS report number 8. Ophthalmology. 1981;88(7):583–600. [PubMed] [Google Scholar]
- EDPRG 2004a.The Eye Diseases Prevalence Research Group. Causes and prevalence of visual impairment among adults in the United States. Archives of Ophthalmology. 2004;122(4):477–85. doi: 10.1001/archopht.122.4.477. [DOI] [PubMed] [Google Scholar]
- EDPRG 2004b.The Eye Diseases Prevalence Research Group. The prevalence of diabetic retinopathy among adults in the United States. Archives of Ophthalmology. 2004;122(4):552–63. doi: 10.1001/archopht.122.4.552. [DOI] [PubMed] [Google Scholar]
- EDPRG 2004c.The Eye Diseases Prevalence Research Group. The prevalence of diabetic retinopathy among adult type 1 diabetic persons in the United States. Archives of Ophthalmology. 2004;122(4):546–51. doi: 10.1001/archopht.122.4.546. [DOI] [PubMed] [Google Scholar]
- ETDRS1 1985.Early Treatment Diabetic Retinopathy Study Research Group. Photocoagulation for diabetic macular edema. Early Treatment Diabetic Retinopathy Study report number 1. Archives of Ophthalmology. 1985;103(12):1796–806. [PubMed] [Google Scholar]
- ETDRS10 1991.Early Treatment Diabetic Retinopathy Study Research Group. Grading diabetic retinopathy from stereoscopic color fundus photographs--an extension of the modified Airlie House classification. ETDRS report number 10. Ophthalmology. 1991;98(5 Suppl):786–806. [PubMed] [Google Scholar]
- ETDRS12 1991.Early Treatment Diabetic Retinopathy Study Research Group. Fundus photographic risk factors for progression of diabetic retinopathy. ETDRS report number 12. Ophthalmology. 1991;98(5 Suppl):823–33. [PubMed] [Google Scholar]
- ETDRS18 1998.Davis MD, Fisher MR, Gangnon RE, Barton F, Aiello LM, Chew EY, et al. Risk factors for high-risk proliferative diabetic retinopathy and severe visual loss: Early Treatment Diabetic Retinopathy Study report number 18. Investigative Ophthalmology and Visual Science. 1998;39(2):233–52. [PubMed] [Google Scholar]
- ETDRS9 1991.Early Treatment Diabetic Retinopathy Study Research Group. Early photocoagulation for diabetic retinopathy. ETDRS report number 9. Ophthalmology. 1991;98(5 Suppl):766–85. [PubMed] [Google Scholar]
- Ferris 1993.Ferris FL., 3rd How effective are treatments for diabetic retinopathy? JAMA. 1993;269(10):1290–1. [PubMed] [Google Scholar]
- Fong 2004.Fong DS, Aiello L, Gardner TW, King GL, Blankenship G, Cavallerano JD, et al. Retinopathy in diabetes. Diabetes Care. 2004;27(Suppl 1):S84–7. doi: 10.2337/diacare.27.2007.s84. [DOI] [PubMed] [Google Scholar]
- Frank 2004.Frank RN. Medical progress: diabetic retinopathy. The New England Journal of Medicine. 2004;350(1):48–58. doi: 10.1056/NEJMra021678. [DOI] [PubMed] [Google Scholar]
- Gillow 1999.Gillow JT, Gibson JM, Dodson PM. Hypertension and diabetic retinopathy--what’s the story? British Journal of Ophthalmology. 1999;83(9):1083–7. doi: 10.1136/bjo.83.9.1083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Giuffre 2004.Giuffre G, Lodato G, Dardanoni G. Prevalence and risk factors of diabetic retinopathy in adult and elderly subjects: The Castedaccia Eye Study. Graefe’s Archives of Clinical and Experimental Ophthalmology. 2004;242(7):535–40. doi: 10.1007/s00417-004-0880-4. [DOI] [PubMed] [Google Scholar]
- Glanville 2006.Glanville JM, Lefebvre C, Miles JN, Camosso-Stefinovic J. How to identify randomized controlled trials in MEDLINE: ten years on. Journal of the Medical Library Association. 2006;94(2):130–6. [PMC free article] [PubMed] [Google Scholar]
- Grey 1989.Grey RHB. Blind and partial sight registration in Avon. British Journal of Ophthalmology. 1989;73(2):88–94. doi: 10.1136/bjo.73.2.88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hansson 1998.Hansson L, Zanchetti A, Carruthers SG, Dahlof B, Elmfeldt D, Julius S, et al. Effects of intensive blood-pressure lowering and low-dose aspirin in patients with hypertension: principal results of the Hypertension Optimal Treatment (HOT) randomised trial. HOT Study Group. Lancet. 1998;351(9118):1755–62. doi: 10.1016/s0140-6736(98)04311-6. [DOI] [PubMed] [Google Scholar]
- Harris 1998.Harris MI, Klein R, Cowie CC, Rowland M, Byrd-Holt DD. Is the risk of diabetic retinopathy greater in non-Hispanic blacks and Mexican Americans than in non-Hispanic whites with type-2 diabetes? A US population study. Diabetes Care. 1998;21(8):1230–5. doi: 10.2337/diacare.21.8.1230. [DOI] [PubMed] [Google Scholar]
- Hayward 2002.Hayward LM. What is the prevalence of visual impairment in the general and diabetic populations: are there ethnic and gender differences? Diabetic Medicine. 2002;19(1):27–34. doi: 10.1046/j.0742-3071.2001.00603.x. [DOI] [PubMed] [Google Scholar]
- Higgins 2011.Higgins JPT, Altman DG, Green S, editors. Cochrane Handbook for Systematic Reviews of Interventions. The Cochrane Collaboration; 2011. Chapter 8: Assessing risk of bias in included studies. Version 5.1.0 (updated March 2011) Available from www.cochrane-handbook.org. [Google Scholar]
- HOPESI 2000.Heart Outcomes Prevention Evaluation Study Investigators. Effects of ramipril on cardiovascular and microvascular outcomes in people with diabetes mellitus: results of the HOPE study and MICRO-HOPE sub-study. Lancet. 2000;355(9200):253–9. [PubMed] [Google Scholar]
- Keen 2001.Keen H. The appearance of retinopathy and progression to proliferative retinopathy: the WHO multinational study of vascular disease in diabetes. Diabetologia. 2001;44(Suppl 2):S22–30. doi: 10.1007/pl00002935. [DOI] [PubMed] [Google Scholar]
- Klein 1984a.Klein R, Klein BE, Moss SE, Davis MD, DeMets DL. The Wisconsin Epidemiologic Study of Diabetic Retinopathy II. Prevalence and risk of diabetic retinopathy when age at diagnosis is less than 30 years. Archives of Ophthalmology. 1984;102(4):520–6. doi: 10.1001/archopht.1984.01040030398010. [DOI] [PubMed] [Google Scholar]
- Klein 1984b.Klein R, Klein BE, Moss SE, Davis MD, DeMets DL. The Wisconsin Epidemiologic Study of Diabetic Retinopathy III. Prevalence and risk of diabetic retinopathy when age at diagnosis is 30 or more years. Archives of Ophthalmology. 1984;102(4):527–32. doi: 10.1001/archopht.1984.01040030405011. [DOI] [PubMed] [Google Scholar]
- Klein 1988.Klein R, Klein BE, Moss SE, Davis MD, DeMets DL. Glycosylated hemoglobin predicts the incidence and progression of diabetic retinopathy. JAMA. 1988;260(19):2864–71. [PubMed] [Google Scholar]
- Klein 1989a.Klein R, Moss SE, Klein BE, Davis MD, DeMets DL. The Wisconsin Epidemiologic Study of Diabetic Retinopathy XI. The incidence of macular edema. Ophthalmology. 1989;96(10):1501–10. doi: 10.1016/s0161-6420(89)32699-6. [DOI] [PubMed] [Google Scholar]
- Klein 1989b.Klein R, Klein BE, Moss SE, Davis MD, DeMets DL. Is blood pressure a predictor of the incidence or progression of diabetic retinopathy? Archives of Internal Medicine. 1989;149(11):2427–32. [PubMed] [Google Scholar]
- Klein 2002a.Klein R, Klein BE. Blood pressure control and diabetic retinopathy. British Journal of Ophthalmology. 2002;86(4):365–7. doi: 10.1136/bjo.86.4.365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klein 2002b.Klein R. The association of atherosclerosis, vascular risk factors, and retinopathy in adults with diabetes: the atherosclerosis risk in communities study. Ophthalmology. 2002;109(7):1225–34. doi: 10.1016/s0161-6420(02)01074-6. [DOI] [PubMed] [Google Scholar]
- Krakoff 2003.Krakoff J, Lindsay RS, Looker HC, Nelson RG, Hanson RL, Knowler WC. Incidence of retinopathy and nephropathy in youth-onset compared with adult-onset type 2 diabetes. Diabetes Care. 2003;26(1):76–81. doi: 10.2337/diacare.26.1.76. [DOI] [PubMed] [Google Scholar]
- Krumpaszky 1999.Krumpaszky HG. Blindness incidence in Germany. A population-based study from Wurttemberg-Hohenzollern. Ophthalmologica. 1999;213(3):176–82. doi: 10.1159/000027415. [DOI] [PubMed] [Google Scholar]
- Kullberg 2002.Kullberg CE, Abrahamsson M, Arnqvist HJ, Finnstrom K, Ludvigsson J VISS Study Group. Prevalence of retinopathy differs with age at onset of diabetes in a population of patients with type 1 diabetes. Diabetes Medicine. 2002;19(11):924–31. doi: 10.1046/j.1464-5491.2002.00839.x. [DOI] [PubMed] [Google Scholar]
- Leske 2003.Leske C. Incidence of diabetic retinopathy in the Barbados Eye Studies. Ophthalmology. 2003;110(5):941–7. doi: 10.1016/S0161-6420(03)00086-1. [DOI] [PubMed] [Google Scholar]
- Mangione 2001.Mangione CM, Lee PP, Gutierrez PR, Spritzer K, Berry S, Hays RD, et al. Development of the 25-item National Eye Institute Visual Function Questionnaire. Archives of Ophthalmology. 2001;119(7):1050–8. doi: 10.1001/archopht.119.7.1050. [DOI] [PubMed] [Google Scholar]
- Mohamed 2007.Mohamed Q, Gillies MC, Wong TY. Management of diabetic retinopathy. A systematic review. JAMA. 2007;298(8):902–16. doi: 10.1001/jama.298.8.902. [DOI] [PubMed] [Google Scholar]
- Moss 1996.Moss S, Klein R, Klein BE. Cigarette smoking and ten-year progression in diabetic retinopathy. Ophthalmology. 1996;103(9):1438–42. doi: 10.1016/s0161-6420(96)30486-7. [DOI] [PubMed] [Google Scholar]
- Porta 2001.Porta M, Sjoelie AK, Chaturvedi N, Stevens L, Rottiers R, Veglio M, et al. Risk factors for progression to proliferative diabetic retinopathy in the EURODIAB Prospective Complications Study. Diabetologia. 2001;44(12):2203–9. doi: 10.1007/s001250100030. [DOI] [PubMed] [Google Scholar]
- PPP 2012.American Academy of Ophthalmology Retina Panel. Diabetic Retinopathy. San Francisco, CA: American Academy of Ophthalmology; 2008. Preferred Practice Patterns® Guidelines. (4th printing 2012) Available at: www.aao.org/ppp. [Google Scholar]
- RevMan 2014.The Nordic Cochrane Center, The Cochrane Collaboration. Review Manager (RevMan). 5.3. Copenhagen: The Nordic Cochrane Center, The Cochrane Collaboration; 2014. [Google Scholar]
- Rosenberg 1996.Rosenberg T, Klie F. Current trends in newly registered blindness in Denmark. Acta Ophthalmologica Scandinavica. 1996;74(4):395–8. doi: 10.1111/j.1600-0420.1996.tb00716.x. [DOI] [PubMed] [Google Scholar]
- Sivaprasad 2012.Sivaprasad S, Gupta B, Crosby-Nwaobi R, Evans J. Prevalence of diabetic retinopathy in various ethnic groups: a worldwide perspective. Survey of Opthalmology. 2012;57(4):347–70. doi: 10.1016/j.survophthal.2012.01.004. [DOI] [PubMed] [Google Scholar]
- Sjølie 2011.Sjølie AK, Dodson P, Hobbs FR. Does renin-angiotensin system blockade have a role in preventing diabetic retinopathy? A clinical review. International Journal of Clinical Practice. 2011;65(2):148–53. doi: 10.1111/j.1742-1241.2010.02552.x. [DOI] [PubMed] [Google Scholar]
- Smith 2011.Smith JM, Steel DHW. Anti-vascular endothelial growth factor for prevention of postoperative vitreous cavity haemorrhage after vitrectomy for proliferative diabetic retinopathy. Cochrane Database of Systematic Reviews. 2011;(5) doi: 10.1002/14651858.CD008214.pub2. [DOI] [PubMed] [Google Scholar]
- Tapp 2003.Tapp RJ, Shaw JE, Harper CA, de Courten MP, Balkau B, McCarty DJ, et al. The prevalence of and factors associated with diabetic retinopathy in the Australian population. Diabetes Care. 2003;26(6):1731–7. doi: 10.2337/diacare.26.6.1731. [DOI] [PubMed] [Google Scholar]
- Thomas 2014.Thomas RL, Dunstan FD, Luzio SD, Chowdhury SR, North RV, Hale SL, et al. Prevalence of diabetic retinopathy within a national diabetic retinopathy screening service. British Journal of Ophthalmology. 2015;99(1):64–8. doi: 10.1136/bjophthalmol-2013-304017. [DOI] [PubMed] [Google Scholar]
- UKPDS33 1998.UK Prospective Diabetes Study Group. Intensive blood-glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes (UKPDS 33) Lancet. 1998;352(9131):837–53. [PubMed] [Google Scholar]
- UKPDS38 1998.UK Prospective Diabetes Study Group. Tight blood pressure control and risk of macrovascular and microvascular complications in type 2 diabetes (UKPDS 38) BMJ. 1998;317(7160):703–13. [PMC free article] [PubMed] [Google Scholar]
- van Leiden 2002.van Leiden HA. Blood pressure, lipids, and obesity are associated with retinopathy: The Hoorn Study. Diabetes Care. 2002;25(8):1320–5. doi: 10.2337/diacare.25.8.1320. [DOI] [PubMed] [Google Scholar]
- van Leiden 2003.van Leiden HA. Risk factors for incident retinopathy in a diabetic and non-diabetic population: The Hoorn Study. Archives of Ophthalmology. 2003;121(2):245–51. doi: 10.1001/archopht.121.2.245. [DOI] [PubMed] [Google Scholar]
- Virgili 2014.Virgili G, Parravano M, Menchini F, Evans JR. Anti-vascular endothelial growth factor for diabetic macular oedema. Cochrane Database of Systematic Reviews. 2014;(10) doi: 10.1002/14651858.CD007419.pub4. [DOI] [PubMed] [Google Scholar]
- Wild 2004.Wild S, Roglic G, Green A, Sicree R, King H. Global prevalence of diabetes: estimates for the year 2000 and projections for 2030. Diabetes Care. 2004;27(5):1047–53. doi: 10.2337/diacare.27.5.1047. [DOI] [PubMed] [Google Scholar]
- Zhang 2001.Zhang L, Krzentowski G, Albert A, Lefebvre PJ. Risk of developing retinopathy in Diabetes Control and Complication Trial type 1 diabetic patients with good or poor metabolic control. Diabetes Care. 2001;24(7):1275–9. doi: 10.2337/diacare.24.7.1275. [DOI] [PubMed] [Google Scholar]
- Zhang 2010.Zhang X, Saaddine JB, Chou CF, Cotch MF, Cheng YJ, Geiss LS, et al. Prevalence of diabetic retinopathy in the United States, 2005–2008. JAMA. 2010;304(6):649–56. doi: 10.1001/jama.2010.1111. [DOI] [PMC free article] [PubMed] [Google Scholar]
References to other published versions of this review
- Sleilati 2009.Sleilati G, Frank RN, Mathew MC. Blood pressure control for diabetic retinopathy. Cochrane Database of Systematic Reviews. 2006;(3) doi: 10.1002/14651858.CD006127. [DOI] [PMC free article] [PubMed] [Google Scholar]