Abstract
Objectives
Little data existaboutthe magnitude and characteristics ofelderly patientswho are hospitalized foran ST-segment elevation acute myocardial infarction (STEMI)who do not undergo cardiac catheterization and/ora percutaneous coronary intervention (PCI).Our study objectives were to describe decade long trends (1999-2009)in the rates of not undergoingcardiaccatheterizationand PCI among patients>65 years old presenting with an STEMI and factors associated with not undergoing these procedures.
Design
Observational study.
Setting
Population-based study.
Participants
960residents of theWorcester (MA) metropolitan area 65 years and older who were hospitalized for an STEMI in 6 biennial periods between 1999 and 2009 at all 11central MA medical centers.
Measurements
Analyses were conducted to examine the characteristics of patients who did not undergo cardiac catheterization overall, and further stratified into 2 age strata (65-74 years and >75 years)
Results
Between 1999and 2009, dramatic declines (from 59.4% to 7.5%)were observed in the proportion ofolder patients who did not undergo cardiac catheterization at all greater Worcester hospitalsThese declines were observed in patients65-74 yearsold (58.4%to6.7%) as well as in patients 75 years and older(69.4% to13.5%).The proportion of patients not receiving a PCI after undergoing a cardiac catheterization decreased from 36.6% (in 1999) to 6.5% (in 2009). Women, patients with a prior MI, those with do not resuscitate orders, and patients withvarious comorbidities were less likely to have undergone these procedures thanrespective comparison groups.
Conclusion
Older patients who develop an STEMI are increasingly likely to undergo cardiac catheterizationand a PCI but several high risk groups remain less likely to undergo these procedures.
Keywords: Cardiac catheterization, elderly patients, ST-segment elevation acute myocardial infarction
INTRODUCTION
Coronary heart disease remains a leading cause of morbidity and mortality in the United States, especially among the elderly. In 2009, almost two-thirds of Americans who died from coronary disease were elderly1-4.Patients 65 years and older who develop an ST-segment elevation acute myocardial infarction (STEMI) are significantly less likely to undergo cardiac catheterization and receive a percutaneous coronary intervention (PCI) than younger individuals; these differences are due, in part, to the results ofseveral studies from the pre-stent era whichshowed lower success rates of PCI in the elderly1-3. Limitedevidence from clinical trials, however, has shown thatthese diagnostic and interventional procedures may be effectivetreatment options for elderly patients3,4, butcurrent guidelines remain unclear in defining recommendations for the receipt of these treatment approaches in this high risk population.
Recent studies havedemonstrated declinesin the hospital and long-term mortality associated with an STEMI, in parallel with the greater use of coronary reperfusion therapyand secondary prevention treatment modalities1-6.Due to concerns about potential adverse effects in the elderly, however, olderpatientswith an STEMI, especially those with multiple comorbidities, tend to be treated less aggressively than younger patients2,6. This is particularly unfortunate, however, since the elderly may be more likely to derive greater benefit from coronary revascularization2,6.Although several previous studies have examined trends in the utilization of cardiac catheterization and PCI in patients hospitalized with an STEMI3,4,6, information on the use of, and relatively recent trends therein, cardiac catheterization and PCI in elderly patients hospitalized with an STEMI, and the characteristics of those who do not receive these diagnostic and interventional procedures, is extremelylimited4,6.
The primary objective of this population-based study was to describe decade long trends (1999-2009) in the rates of notundergoing cardiac catheterization and receiving a PCI in patients65 years and older presenting with anSTEMI. A secondary study goal was to describe the characteristics of elderly patients who did notreceive these coronarydiagnostic and reperfusion approaches. Data from the Worcester Heart Attack Study were used for purposes of this investigation7-11.
METHODS
The Worcester Heart Attack Study is an ongoing population-based investigation which is examining long-term trends in the incidence rates, in-hospital, and post-discharge case-fatality rates (CFRs) of greater Worcester (MA) (2000 census = 478,000) residents hospitalized with acute myocardial infarction (AMI) at all central Massachusetts medical centers. In brief, the medical records of greater Worcester residents admitted to all 11 hospitals throughout central Massachusetts with a discharge diagnosis of AMI and related coronary disease rubrics were individually reviewed and validated by trained study staff according to pre-established diagnostic criteria7-11. The 6 cohorts included in the present investigation were hospitalized for AMI on a biennial basis in 1999, 2001, 2003, 2005, 2007, and 2009.We restricted the present study sample to these years because we were interested in examining relatively contemporary trends in the use of cardiac catheterization and PCI in patients 65 years and older hospitalized with an STEMI. The diagnosis of STEMI was made according to standardized criteria that we have previously used in this large observational study11,12.A diagnosis of STEMI was made when new ST-segment elevation was present at the J point in 2 or more contiguous leads. Troponin assays were infrequently used for the diagnosis of AMI in our study population before 2003 and were not considered in the diagnosis of AMI at that time. In contrast, serum troponin levels were routinely measured in our hospitalized patient population from 2003 on and the results of this biomarker assay become incorporated into the diagnostic criteria for AMI from this point forward11.
Data Collection
Trained physicians and nurses abstracted demographic and clinical data from the medical records of greater Worcester residents hospitalized with independently confirmed AMI. Abstracted information included patient’s age, sex, medical history, AMI order (initial vs. prior), physiologic factors, laboratory findings, length of hospital stay, hospital-associated delay to receipt of cardiac catheterization, and hospital survival status7.
Data analysis
Differences in the demographic and clinical characteristics of older patients who did and did not undergo cardiac catheterizationoverall, and further stratified according to age (65 to 74 years and 75 years and older), were examined through the use of chi-square tests for discrete variables and ANOVA for continuous variables. For ease of analysis and interpretation, trends in various patient characteristics were examined during the following aggregated study years: 1999/01, 2003/05, and 2007/09.Crude and multivariable adjusted logistic regression analyses were used to examine factors associated with notundergoing a cardiac catheterizationand PCI during hospitalizationfor all elderly patients with a STEMI and separately for those aged 65-74 years and for those aged 75 years and older.
We performed an additional subgroup analysis excluding patients who had a do not resuscitate (DNR) order in their hospital medical records. This secondary analysis was performed since DNR status was shown to be a strong predictor of not undergoing cardiac catheterization and there may have been differences in the profile of patients not undergoing a cardiac catheterization without a DNR order.We performed two additional subgroup analyses. One explored decade long trends in patients 85 years and older who did not undergo cardiac catheterization to compare trends in our oldest elderly patients to those in patients aged 75 to 84 years.The other subgroup analysis examined potential changes in the 30-day mortality rates during the years under study in the entire study population after controlling for potential confounding variables of prognostic importance. We also performed this subgroup analysis in elderly patients who underwent a cardiac catheterization and/or a PCI.
RESULTS
A total of 960 metropolitan Worcester residents aged 65 years and older were hospitalized with an independently confirmed STEMI during the years under study (Table 1). The average age of this population was approximately 78 years and 45% were women.
Table 1.
Characteristics of Patients with ST Segment Elevation Acute Myocardial Infarction Who Did Not Undergo Cardiac Catheterization
| All Patients | 65-74 years old | ≥75 years old | ||||
|---|---|---|---|---|---|---|
|
| ||||||
| % not | % not | % not | ||||
| n | undergoing | n | undergoing | n | undergoing | |
| Total | 960 | 39.7 | 354 | 23.2 | 606 | 49.3** |
| Female | 504 | 44.6 | 132 | 24.2 | 372 | 51.9** |
| Male | 456 | 34.2 | 222 | 22.5 | 234 | 45.3** |
| Prior AMI | 301 | 44.5 | 104 | 25.0 | 197 | 54.8** |
| Initial AMI | 659 | 37.5 | 250 | 22.4 | 409 | 46.7** |
| Do Not Resuscitate Order | 293 | 64.2 | 36 | 50.0 | 257 | 66.2 |
| Medical History | ||||||
| Atrial Fibrillation | 125 | 57.6 | 27 | 44.4 | 98 | 61.2 |
| Heart Failure | 196 | 60.7 | 53 | 34.0 | 143 | 70.6** |
| Hypertension | 699 | 39.1 | 240 | 20.8 | 459 | 48.6** |
| Peripheral Vascular Disease | 147 | 39.5 | 56 | 28.6 | 91 | 46.2 |
| Stroke | 115 | 55.7 | 36 | 30.6 | 79 | 67.1* |
| Diabetes | 286 | 40.2 | 118 | 23.7 | 168 | 51.8** |
| Chronic Obstructive | 180 | 45.6 | 59 | 30.5 | 121 | 52.9 |
| Pulmonary Disease | ||||||
| Chronic Kidney Disease | 149 | 47.7 | 51 | 25.5 | 98 | 59.2* |
| Bleeding | 60 | 50.0 | 16 | 31.2 | 44 | 56.8* |
| Anemia | 299 | 49.2 | 85 | 31.8 | 214 | 66.8** |
| Use of anticoagulants before hospitalization |
60 | 38.5 | 54 | 23.8 | 26 | 45.5 |
| All Comorbidities+ | ||||||
| 0-1 | 180 | 17.2 | 80 | 7.5 | 100 | 25.1** |
| 2-3 | 214 | 22.4 | 77 | 7.8 | 137 | 30.7 |
| ≥4 | 566 | 53.4 | 197 | 35.5 | 369 | 62.9 |
AMI: acute myocardial infarction
p-value <0.01;
p-value <0.001
All comorbidities: atrial fibrillation, heart failure, hypertension, peripheral vascular disease, stroke, diabetes, chronic obstructive pulmonary disease, chronic kidney disease, and anemia
Decade long trends in the receipt of cardiac catheterization and PCI
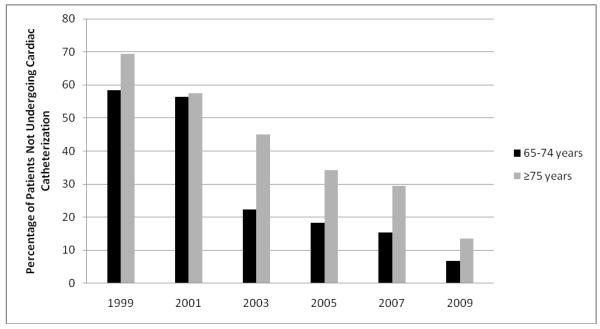
Marked declines were observed in the proportion ofelderly patients who did notundergo cardiac catheterization during the years under study, decreasing from59.4% in 1999 to 7.5% in 2009. The proportion of patients 65-74 years old whodid notundergo cardiac catheterizationdecreased from 58.4% in 1999 to 6.7% in 2009 andfrom 69.4% in 1999 to 13.5% in 2009 in patients 75 years and older (Figure 1). Similarly, significant declines were observed in the proportion of patients who underwent cardiac catheterization and did not receive a PCI during their indexhospitalization from 35.6% in 1999 to 6.5% in 2009.These rates declined from28.9% in 1999 to 6.7% in 2009 among those 65-74 years old and from 42.9% in 1999 to 6.3% in 2009 in the oldeststudy patients.
Figure 1.
Trends in Not Undergoing Cardiac Catheterization According to Age
We examined decade long trends in the lack of receipt of cardiac catheterization in patients 85 years and older and compared these trends to those 75 to 84 years old. Due to the relatively small sample of patients 85 years and older, we aggregated the years under study in a biennial fashion. Significant declines wereobserved in the proportion of patients who did not undergo cardiac catheterization from our earliest to most recent study years. Among patients aged 75-84 years, the proportion of those did not undergo cardiac catheterization decreased from 50.5% to 10.0% between 1999/2001 to 2007/2009, respectively. Among those 85 years and older, the percentage of patients who did not undergo cardiac catheterization decreased from 85.2% to 62.9% during the corresponding periods under study.
Patient characteristics associated with notundergoingcardiac catheterization and PCI
Overall, women, those with a prior AMI, patients with a DNR order, those witheach of the comorbidities examined, with the exception of hypertension and peripheral vascular disease, and patients who did notpresent with either chest pain, left arm and shoulder pain, diaphoresis, or dyspneawere less likely to have undergone cardiac catheterization as compared with respective comparison groups (p<0.001) (Table 1).
In examining possible age-specific differences in the receipt ofcardiac catheterization, similarfactors, with somewhat exaggerated differences, were found among patients older than 75 yearswhereas slightlyattenuated differences, but similar trends, were observed inpatientslessthan 75 years old(Table 1).Similar characteristics and risk factors were found when we examinedthe characteristics of those who did not receive a PCI, overall and in the two age strata examined.
Decade long trends in the characteristics of patients who did not undergo cardiac catheterization
There were no marked differences found when we examined possible differences in the characteristics of patients who did notundergo cardiac catheterization in ourearlier (1999/01), as compared with the most recent (2007/09), hospitalized patient cohorts among patients65-74 years old (Table 2).In patients 75 years and older, however, women, patients with aprior MI, those with aDNR order, and those with any of the selected comorbidities, with the exception of peripheral vascular disease, remained at higher risk for notundergoing cardiac catheterization during the years under study (Table 2).
Table 2.
Trends in the Characteristics of Patients Who Did Not Undergo Cardiac Catheterization According to Age
| 65-74 years | ≥75 years | |||||||
|---|---|---|---|---|---|---|---|---|
|
| ||||||||
| 1999/01 | 2007/09 | 1999/01 | 2007/09 | |||||
| n | % | n | % | n | % | n | % | |
| Total | 167 | 38.3 | 69 | 12.5 | 306 | 76.1 | 105 | 29.8 |
| Female | 70 | 38.6 | 27 | 0 | 180 | 66.1 | 58 | 25.9 |
| Male | 97 | 38.1 | 42 | 7.1 | 126 | 60.3 | 47 | 21.3 |
| Prior AMI | 47 | 42.6 | 28 | 7.1 | 95 | 67.4 | 35 | 34.3 |
| Initial AMI | 120 | 36.7 | 41 | 2.4 | 211 | 62.1 | 70 | 18.6 |
| Do Not Resuscitate Order | 15 | 66.7 | 7 | 42.9 | 127 | 78.0 | 41 | 48.8 |
| Medical History | ||||||||
| Atrial Fibrillation | 14 | 71.4 | 3 | 0 | 49 | 69.4 | 19 | 52.6 |
| Heart Failure | 25 | 60.0 | 11 | 0 | 75 | 81.3 | 18 | 55.6 |
| Hypertension | 103 | 35.0 | 54 | 14.8 | 227 | 61.7 | 85 | 28.2 |
| Peripheral Vascular Disease | 21 | 47.6 | 17 | 11.8 | 40 | 67.5 | 23 | 21.7 |
| Stroke | 22 | 45.5 | 4 | 0 | 42 | 76.2 | 13 | 53.9 |
| Diabetes | 45 | 46.7 | 26 | 0 | 85 | 68.3 | 31 | 25.8 |
| Chronic Obstructive Pulmonary | 27 | 48.2 | 10 | 0 | 58 | 65.5 | 16 | 25.0 |
| Disease | ||||||||
| Chronic Kidney Disease | 18 | 50.0 | 13 | 0 | 28 | 78.6 | 30 | 40.0 |
| Bleeding | 5 | 80.0 | 5 | 0 | 21 | 61.9 | 7 | 28.6 |
| Anemia | 40 | 57.5 | 15 | 0 | 116 | 69.8 | 36 | 27.8 |
| Use of anticoagulants before hospitalization |
12 | 27.3 | 0 | 19 | 52.6 | 9 | 55.6 | |
AMI: acute myocardial infarction
To more systematically examinefactors associated with not undergoing cardiac catheterization, we carried out a series of multivariable adjusted regression analyses controlling for several potentially confounding factors of prognostic importance including the time period under study, patient’s sex, race, marital status, history of several cardiovascular and non-cardiovascular co-morbidities, laboratory and physiologic findings, and patient’s acute symptoms (Table 3).There were no statistically significant factors associated with notundergoingcardiac catheterization in patients 65-74 years old. Patients with a history of heart failureor strokewere at higher risk fornotundergoing cardiaccatheterizationamong patients 75 years and older compared to patients without these previously diagnosed comorbidities.Similar risk factors were found in both age strata in patients who underwent cardiac catheterization but did not receive a PCI after undergoing this diagnostic procedure (data not shown).
Table 3.
Factors Significantly Associated With Not Undergoing Cardiac Catheterization Overall and According to Age
| All Patients | 65-74 years old | ≥75 years old | ||||
|---|---|---|---|---|---|---|
|
| ||||||
| Factor | Crude OR+ (95% CI) |
Adjusted OR (95% CI) |
Crude OR (95% CI) |
Adjusted OR (95% CI) |
Crude OR (95% CI) |
Adjusted OR (95% CI) |
| Study year | ||||||
| 2003/2005 | 0.35 (0.26,0.48) | 0.33(0.24,0.46) | 0.23(0.13,0.48) | 0.23(0.12,0.45) | 0.39(0.27,0.56) | 0.35(0.24,0.53) |
| 2007/2009 | 0.16(0.10,0.25) | 0.17(0.11,0.27) | 0.07(0.02,0.24) | 0.08(0.02,0.26) | 0.18(0.11,0.30) | 0.20(0.12,0.33) |
| Male | 0.64(0.50,0.84) | 0.75(0.55,1.03) | 0.91(0.55,1.51) | 0.86(0.48,1.55) | 0.77(0.55,1.07) | 0.98(0.66,1.46) |
| Married | 0.57(0.44,0.74) | 0.62(0.46,0.85) | 1.38(0.81,2.35) | 1.59(0.86,2.95) | 0.49(0.36,0.69) | 0.50(0.34,0.74) |
| Initial AMI | 0.75(0.57,0.99) | 0.87(0.51,1.48) | 0.72(0.51,1.02) | |||
| Comorbidities | ||||||
| Atrial Fibrillation | 2.31(1.58,3.39) | 2.94(1.31,6.56) | 1.78(1.14,2.77) | |||
| Heart Failure | 2.96(2.14,4.09) | 1.90(1.01,3.58) | 3.22(2.15,4.82) | |||
| Hypertension | 0.91(0.68,1.21) | 0.67(0.40,1.13) | 0.88(0.61,1.28) | |||
| Peripheral Vascular | 0.99(0.69,1.42) | 1.41(0.74,2.67) | 0.86(0.55,1.35) | |||
| Disease | ||||||
| Stroke | 2.09(1.41,3.10) | 1.53(0.72,3.26) | 2.33(1.41,3.84) | |||
| Diabetes | 1.03(0.78,1.37) | 1.15(0.80,1.63) | 1.05(0.62,1.77) | |||
| Chronic Obstructive | 1.35(0.97,1.87) | 1.58(0.85,2.94) | 1.19(0.80,1.78) | |||
| Pulmonary Disease | ||||||
| Chronic Kidney Disease | 1.47(1.04,2.09) | 1.16(0.59,2.30) | 1.61(1.04,2.49) | |||
| Bleeding | 0.64(0.38,1.08) | 0.65(0.22,1.93) | 0.72(0.39,1.34) | |||
| Anemia | 1.76(1.34,2.33) | 1.81(1.05,3.12) | 1.52(1.09,2.12) | |||
| Use of anticoagulants before hospitalization |
0.93(0.55,1.55) | 1.14(0.40,3.24) | 0.85(0.46,1.57) | |||
| Estimated Glomerular | 1.48(0.78,2.83) | 1.30(0.42,3.98) | 1.38(0.60,3.16) | |||
| Filtration Rate | ||||||
| <60mL/min/1.73 m2 | ||||||
| Serum Glucose level | 1.25(0.94,1.67) | 1.89(1.09,3.27) | 0.96(0.68,1.36) | |||
| >200mg/dl at admission | ||||||
| Systolic BP >120mm Hg | 0.97(0.75,1.26) | 1.11(0.68,1.82) | 1.00(0.72,1.37) | |||
| Diastolic BP >90 mm Hg | 0.83(0.62,1.11) | 1.18(0.70,1.99) | 0.77(0.53,1.11) | |||
| Symptoms | ||||||
| Chest pain | 0.25(0.19,0.33) | 0.29(0.17,0.50) | 0.25(0.18,0.36) | |||
| Left arm pain | 0.56(0.40,0.77) | 0.62(0.35,1.11) | 0.63(0.41,0.95) | |||
| Left shoulder pain | 0.42(0.24,0.70) | 0.40(0.15,1.05) | 0.51(0.26,0.99) | |||
| Diaphoresis | 0.52(0.40,0.68) | 0.76(0.46,1.24) | 0.52(0.37,0.72) | |||
| Dyspnea | 0.63(0.33,1.20) | 0 | 0.70(0.35,1.42) | |||
AMI: acute myocardial infarction +OR = odds ratio
respective comparison groups: 1999/2001, women, nonwhite, not married, absence of selected comorbidities, not on anticoagulants, eGFR>60mL/min/1.73 m2, serum glucose <200 mg/dl, systolic blood pressure <120 mmHg, diastolic blood pressure <90 mmHg, absence of selected symptoms.
Despite the non-randomized nature of this investigation, and the potential for confounding by treatment indication, we carried out a series of unadjusted and multivariable adjusted regression analyses in our total study populationfor purposes of examining trends in 30-day mortality rates during the years under study after controlling for important potential confounders of prognostic importance including demographic factors, comorbidities, and the receipt of in-hospital medical treatment and cardiac interventions. We found a non-significant declinein the ORs for dying within 30 days after the patient’s index hospitalization, from 1.40(95% CI 0.87, 2.26) in 1999 to 1.17(95% CI0.54, 2.50) in 2009, respectively(p=0.69). Similar trends of improving short-term survival were observed in elderly patients undergoing cardiac catheterization and/or a PCI.
In examining possible differences in the factors associated with not undergoing cardiac catheterization in elderly patients without a DNR order, relatively similar factors were found to be associated with not undergoing a cardiac catheterization as in our entire study population. In particular, older patients and those with a previous history of heart failure, stroke, chronic kidney disease, or anemia had a lower probability of undergoing cardiac catheterization than respective comparison groups.
DISCUSSION
The results of this descriptive observational study showed that the use of cardiac catheterization and PCI increasedmarkedly inelderly patients who were hospitalized at all central Massachusetts medical centers between 1999and 2009 with an STEMI. Despite these positive trends, several subsets of this population, notably women, those with a DNR order, and those with multiple co-morbidities were less likely to haveundergonecardiac catheterization than respective comparison groups.
Trends in the Receipt of Cardiac Catheterization and PCI
Several studies in and outside of the U.S., as well as our findings showing marked declines in the proportion of elderly patients who did not undergo cardiac catheterization, have demonstrated a greater utilization of cardiac catheterization and PCI in elderly patients with AMI during varying time periods. A Scottish study (2000 to 2007, n = 31,758) anda Danish study (2002 to 2009, n = 3,796) showed that older patients constituted an increasingly greater percentage of the population who received a PCI during hospitalization for AMI13,14. Similarly, using data from the Swedish Coronary Angiography and Angioplasty Registry, among 4, 876 patients 80 years and older with an STEMI, the proportion of elderly patients undergoing PCI increased from 10% in 2001 to 17% in 201015.A national study of 1.4 million elderly patients hospitalized with an STEMI between 2001 and 2010 found a significant increase in the use of PCI from 20.4% in 2001 to 53.9% in 2010 among patients 65 -79 years old, and from 9.2% to 31.2% in patients 80 years and older. Despite encouraging trends in the receipt of a PCI, older patients remained at higher risk for dying in the hospital after a PCI4.
These collective findings suggest thatwhile there have been significant increases in the use of cardiac catheterization and PCIin the elderly over time, this group remainsat considerablyhigher risk for dying during hospitalization for an STEMI.Further studies in these high risk populationsremain needed.
Factors Associated with Not Undergoing Cardiac Catheterization
To date, there have beena limited number of studies that have examined factors that may predispose an elderly patient who is experiencing an STEMI to not undergo cardiac catheterization or receive a PCI. A study of more than 53,000 patients hospitalized with an STEMI in all Florida hospitals between 2001 and 2005 found that women and individuals older than 75 years were less likely to have received a same day PCI than respective comparison groups16. A study of 1,064 patients treated for an STEMI in a Pennsylvania community hospital found that a higher percentage of men than women underwent cardiac catheterization17whereas a recent study that included 68,025 patients with a STEMI found that patients 85 years and older were significantly less likely to have received coronary reperfusion therapy than their younger counterparts18.
In a study examining all Florida hospital discharges between 2006 and 2007, important predictors for patients who developed an STEMI and were 75 years or older to not undergo a cardiac catheterization included being female, African-American, and having dementia19. Due to the low representation of minorities in our study population, we were unable to examine the influence of race/ethnicity as a possible predictor of notundergoing cardiac catheterization or receiving a PCI. The study in Florida showed that several comorbidities were associated with decreased utilization of cardiac catheterization19.This study also found that women, those from lower socioeconomic strata, and patients with select chronic conditions were less likely to have received a subsequent PCI after undergoing cardiac catheterization19. Our study also found that patients with a history of heart failure, chronic kidney disease, or stroke were less likely to have undergone cardiac catheterization than patients without these previously diagnosed comorbidities.
One potential explanation for our observed sex differences in the receipt of cardiac catheterization may stem from the decreased likelihood for women to experience classic symptoms of AMI such as chest pain20. This dovetails with our findings which showed that patients who did not present with chest, left arm, or left shoulder pain were less likely to have undergone cardiac catheterization than patients who presented with these acute symptoms. On the other hand, since women were older than men at the time of being hospitalized for an STEMI in the present study, this may have contributed to their lower receipt of this diagnostic procedure.
Our finding that patients with a DNR order were less likely to have undergone cardiac catheterization during the years under study could have resulted from a multiplicity of factors. DNR patients are more likely to be sicker and present with a greater number of comorbidities at the time of hospitalization than patients who do not have a DNR order21.Inasmuch, the lower receipt of cardiac catheterization in these patients could have resulted from them being perceived as riskier candidates for intervention. However, data showing that DNR patients are at higher risk for dying during hospitalization for AMI, even after adjusting for multiple factors, has raised concerns about the denial of care for these patients22. A survey of 241 physicians at a Baltimore medical center found that physicians were significantly less likely to order central line placement, blood cultures, and blood transfusions for hypothetical DNR patients compared to hypothetical patients without a DNR order23. While our results cannot confirm physician bias in withholding cardiac catheterization for patients with a DNR order, they do suggest the need for further research in this area.
The presence of certain and multiple comorbidities may deter cardiac catheterization use due to concerns for higher procedural-related morbidity and mortality. Several studies have, however, presented contradictory evidence on how conditions such as chronic obstructive pulmonary disease (COPD) and end-stage renal disease are associated with in-hospital mortality after receipt of a PCI24. Physicians are challenged in balancing the risks of inaction following a STEMI with procedural-related complications for these complex, high risk patients. However, as the average age of patients hospitalized with AMI continues to increase25, there will likely be more patients presenting with multiple comorbidities in whom the benefits and risks of undergoing a PCI need to be considered and more systematically evaluated.
Study Strengths and Limitations
The main strengths of our observational study include the large elderly patient samplehospitalized witha confirmed STEMI and the collection of data over a decade long period of study. Our sample included a relatively large representation of women, patients having either a first or prior MI, and patients with various comorbidities.
We acknowledge several limitations associated with our study. Our study was carried out among residents of central Massachusetts, who were primarily Caucasian, and, therefore, we were unable to examine the impact of race/ethnicity on our principal study outcomes as well as whether the present findings are applicable to other geographic settings. Since the American population is becoming more diverse and health disparities continue to exist, it will become important for future studies to examine differences in the receipt of diagnostic and interventional cardiac procedures according to race/ethnicity as well as in different population settings.We also did not have systematically collected information available on several additional factors that might have affected the present results including the effects of dementia and impaired cognition, frailty, depression, functional status, metastatic cancer, morbid obesity, tobacco use, or recent surgical procedures.We also did not have data available on the reasons for not performing cardiac catheterization and/or PCI, including patient and physician preferences. We also did not adjust for the impact of several hospital clinical complications on the receipt of cardiac catheterization or PCI, and excluded from the study those patients who died during their index hospitalization for STEMI, since we were unable to classify the time of occurrence of these events and receipt of the diagnostic and interventional procedures examined.
CONCLUSIONS
Our study of elderly patients hospitalized with an STEMI inall central Massachusetts medical centers between 1999 and 2009 demonstrated an increased utilization of cardiac catheterization and PCI in these older adults. However, we were unable to determine whetherthe management of these older patients was appropriate, excessive, or inadequate. We also showed that several demographic and clinical factors were associated with a higher risk of not undergoing cardiac catheterization in the setting of a STEMI.As these interventions become more common in older hospitalized patients, and more elderly patients with single and multiplecomorbidities are included in clinical trials, further characterization of in-hospital and long-term outcomes in these individuals should be undertaken so that these patients can obtain benefits from these diagnostic and interventional procedures as younger patients have.
ACKNOWLEDGMENTS
We wish to acknowledge all persons involved in the review of data for this project as well as to our collaborators at all hospitals in the Worcester metropolitan area.
Funding Source: National Institutes of Health (RO1 HL35434).
Dr. Tisminetzky is funded by Diversity Supplement R01 HL35434-29.
Partial salary support is additionally provided to Drs. Goldberg and Gore by National Institutesof Health grant 1U01HL105268-01.
Footnotes
Conflicts of Interest: The cooperation of all participating hospitals in the Worcester metropolitan area made this research possible. Dr. Tisminetzky is funded by Diversity Supplement R01 HL35434-29. Partial salary support is additionally provided to Drs. Goldberg and Gore by National Institutes of Health grant 1U01HL105268-01 and R01 HL35434. There are no conflicts of interest to report on behalf of the study authors.
Author Contributions: All authors contributed in the study design, data analysis and interpretation, write-up, and critical review of the information contained in this article.
Sponsors Role: None.
REFERENCES
- 1.Alexander KP, Newby LK, Armstrong PW, et al. Acute Coronary Care in the Elderly, Part II: ST-Segment–Elevation Myocardial Infarction: A Scientific Statement for Healthcare Professionals From the American Heart Association Council on Clinical Cardiology: In Collaboration With the Society of Geriatric Cardiology. Circulation. 2007;115:2570–2589. doi: 10.1161/CIRCULATIONAHA.107.182616. [DOI] [PubMed] [Google Scholar]
- 2.Mehta RH, Rathore SS, Radford MJ, et al. Acute myocardial infarction in the elderly: Differences by age. J Am Coll Cardiol. 2001;38:736–741. doi: 10.1016/s0735-1097(01)01432-2. [DOI] [PubMed] [Google Scholar]
- 3.Task Force on the management of ST-segment elevation acute myocardial infarction of the European Society of Cardiology (ESC) Steg PG, James SK, Atar D, et al. ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation. Eur Heart J. 2012;33:2569–2619. doi: 10.1093/eurheartj/ehs215. [DOI] [PubMed] [Google Scholar]
- 4.Khera S, Kolte D, Palaniswamy C, et al. ST-elevation myocardial infarction in the elderly-temporal trends in incidence, utilization of percutaneous coronary intervention and outcomes in the United States. Int J Cardiol. 2013;168:3683–3690. doi: 10.1016/j.ijcard.2013.06.021. [DOI] [PubMed] [Google Scholar]
- 5.Fox KA, Steg PG, Eagle KA. Decline in rates of death and heart failure in acute coronary syndromes, 1999–2006. JAMA. 2007;297:1892–1900. doi: 10.1001/jama.297.17.1892. [DOI] [PubMed] [Google Scholar]
- 6.Cantor WJ, Goodman SG, Cannon CP, et al. Early cardiac catheterization is associated with lower mortality only among high-risk patients with ST- and non-ST-elevation acute coronary syndromes: observations from the OPUS-TIMI 16 trial. Am Heart J. 2005;149:275–283. doi: 10.1016/j.ahj.2004.05.055. [DOI] [PubMed] [Google Scholar]
- 7.Floyd KC, Yarzebski J, Spencer FA, et al. A 30 year perspective (1975-2005) into the changing landscape of patients hospitalized with initial acute myocardial infarction: Worcester Heart Attack Study. Circ Cardiovasc Qual Outcomes. 2009;2:88–95. doi: 10.1161/CIRCOUTCOMES.108.811828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Goldberg RJ, Gore JM, Alpert JS, et al. Recent changes in attack and survival rates of acute myocardial infarction (1975 through 1981). The Worcester Heart Attack Study. JAMA. 1986;255:2774–2779. [PubMed] [Google Scholar]
- 9.Goldberg RJ, Spencer FA, Yarzebski J, et al. A 25-year perspective into the changing landscape of patients hospitalized with acute myocardial infarction (the Worcester Heart Attack Study) Am J Cardiol. 2004;94:1373–1378. doi: 10.1016/j.amjcard.2004.07.142. [DOI] [PubMed] [Google Scholar]
- 10.Goldberg RJ, Yarzebski J, Lessard D, et al. Decade-long trends and factors associated with time to hospital presentation in patients with acute myocardial infarction: The Worcester Heart Attack study. Arch Intern Med. 2000;160:3217–3223. doi: 10.1001/archinte.160.21.3217. [DOI] [PubMed] [Google Scholar]
- 11.McManus DD, Gore J, Yarzebski J, et al. Recent trends in the incidence, treatment, and outcomes of patients with STEMI and NSTEMI. Am J Med. 2011;124:40–47. doi: 10.1016/j.amjmed.2010.07.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Thygesen K, Alpert JS, Jaffe AS, et al. Writing Group on the Joint ESC/ACCF/AHA/WHF Task Force for the Universal Definition of Myocardial Infarction. Thygesen K, Alpert JS, White HD, et al. ESC Committee for Practice Guidelines (CPG) Third universal definition of myocardial infarction. Eur Heart J. 2012;33:2551–2567. [Google Scholar]
- 13.Johnman C, Oldroyd KG, Mackay D, et al. Percutaneous coronary intervention in the elderly: Changes in case-mix and periprocedural outcomes in 31,758 patients treated between 2000 and 2007. Circ Cardiovasc Interv. 2010;3:341–345. doi: 10.1161/CIRCINTERVENTIONS.109.928705. [DOI] [PubMed] [Google Scholar]
- 14.Antonsen L, Jensen LO, Thayssen P, et al. Comparison of outcomes of patients >/= 80 years of age having percutaneous coronary intervention according to presentation (stable vs unstable angina pectoris/non-ST-segment elevation myocardial infarction vs ST-segment elevation myocardial infarction) Am J Cardiol. 2011;108:1395–1400. doi: 10.1016/j.amjcard.2011.06.062. [DOI] [PubMed] [Google Scholar]
- 15.Velders MA, James SK, Libungan B, et al. Prognosis of elderly patients with ST-elevation myocardial infarction treated with primary percutaneous coronary intervention in 2001 to 2011: A report from the Swedish Coronary Angiography and Angioplasty Registry (SCAAR) registry. Am Heart J. 2014:666–673. doi: 10.1016/j.ahj.2014.01.013. [DOI] [PubMed] [Google Scholar]
- 16.Pathak EB, Strom JA. Disparities in use of same-day percutaneous coronary intervention for patients with ST-elevation myocardial infarction in Florida, 2001-2005. Am J Cardiol. 2008;102:802–808. doi: 10.1016/j.amjcard.2008.05.023. [DOI] [PubMed] [Google Scholar]
- 17.Greenberg MR, Miller AC, Mackenzie RS, et al. Analysis of sex differences in preadmission management of ST-segment elevation (STEMI) myocardial infarction. Gen Med. 2012;9:329–334. doi: 10.1016/j.genm.2012.07.002. [DOI] [PubMed] [Google Scholar]
- 18.Zaman MJ, Stirling S, Shepstone L, et al. The association between older age and receipt of care and outcomes in patients with acute coronary syndromes: A cohort study of the Myocardial Ischaemia National Audit Project (MINAP) Eur Heart J. 2014;35:1551–1558. doi: 10.1093/eurheartj/ehu039. [DOI] [PubMed] [Google Scholar]
- 19.Chanti-Ketterl M, Pathak EB, Andel R, et al. Dementia: A barrier to receiving percutaneous coronary intervention for elderly patients with ST-elevated myocardial infarction. Int J Geriatr Psychiatry. 2014;29:906–914. doi: 10.1002/gps.4078. [DOI] [PubMed] [Google Scholar]
- 20.Canto JG, Goldberg RJ, Hand MM, et al. Symptom presentation of women with acute coronary syndromes: Myth vs reality. Arch Intern Med. 2007;167:2405–2413. doi: 10.1001/archinte.167.22.2405. [DOI] [PubMed] [Google Scholar]
- 21.Wenger NS, Pearson ML, Desmond KA, et al. Epidemiology of do-not-resuscitate orders: Disparity by age, diagnosis, gender, race, and functional impairment. Arch Intern Med. 1995;155:2056–2062. [PubMed] [Google Scholar]
- 22.Shepardson LB, Youngner SJ, Speroff T, et al. Increased risk of death in patients with do-not-resuscitate orders. Med Care. 1999;37:727–737. doi: 10.1097/00005650-199908000-00003. [DOI] [PubMed] [Google Scholar]
- 23.Beach MC, Morrison RS. The effect of do-not-resuscitate orders on physician decision-making. J Am Geriatr Soc. 2002;50:2057–2061. doi: 10.1046/j.1532-5415.2002.50620.x. [DOI] [PubMed] [Google Scholar]
- 24.Pathak EB, Strom JA. Percutaneous coronary intervention, comorbidities, and mortality among emergency department-admitted ST-elevation myocardial infarction patients in Florida. J Interv Cardiol. 2010;23:205–215. doi: 10.1111/j.1540-8183.2010.00541.x. [DOI] [PubMed] [Google Scholar]
- 25.Berger JS, Sanborn TA, Sherman W, et al. Effect of chronic obstructive pulmonary disease on survival of patients with coronary heart disease having percutaneous coronary intervention. Am J Cardiol. 2004;94:649–651. doi: 10.1016/j.amjcard.2004.05.034. [DOI] [PubMed] [Google Scholar]