INTRODUCTION
Per year, there are approximately 50,000 HIV infection in the United States[1], and the HIV epidemic continues to disproportionately affect the lives of men who have sex with men (MSM). Public health researchers and practitioners have increasingly highlighted the importance of structural determinants on the HIV epidemic, building on a long tradition of research and practice in social and behavioral sciences. Although scientific advances have demonstrated the efficacy of biomedical HIV prevention interventions, including pre- and post-exposure prophylaxis (PrEP and PEP, respectively), to protect against HIV transmission,[2–4] social contexts affect environments in which people live and can present barriers to implementation and adherence to this individual-level intervention.[5–9] The effectiveness of both PEP and PrEP is highly correlated with adherence to the regimen.[2,3,10,11] Psychosocial processes such as depression adversely affect adherence to antiretroviral therapy,[12] and macro-level environments strongly influence these psychosocial factors.[9,13] Given the recent shifts in state-level policies to protect sexual minorities in the United States[14], further research into the impact of the social environment on the awareness and acceptability of prevention tools, such as PrEP, is a critical area for public health today.
Recently, research among sexual minority populations has increasingly considered the role of stigma related to sexual orientation at the individual, interpersonal and structural level in affecting risk for adverse health outcomes.[15,16] Stigma is broadly defined as negative attitudes, relative powerlessness, and loss of status related to a particular characteristic.[17,18] Experiences of stigma can occur at the individual (i.e., self-stigma), interpersonal (i.e., enacted or experienced stigma), and structural [16] levels. Structural stigma related to sexual orientation (henceforth, “structural stigma”) has been defined as “societal-level conditions, cultural norms, and institutional policies and practices that constrain the opportunities, resources, and wellbeing of the stigmatized”.[19]
Among MSM, individual and interpersonal forms of stigma have been associated with decreased access to healthcare in diverse settings[20,21], with increased HIV risk, and adverse mental health conditions.[22–24] However, few empirical investigations have investigated the relationship between structural stigma and HIV prevention among MSM. To address this gap, we conducted an online survey of MSM in the United States that was designed to assess sexual behaviors, awareness and use of PEP and PrEP, and comfort with primary care providers. We hypothesized that individuals living in areas with higher structural stigma (increased anti-gay prejudicial social environments at the state level) would have decreased awareness and utilization of PEP and PrEP, decreased condom use, and reduced ability to discuss sexual risk and HIV prevention strategies with primary care providers.
METHODS
Participants and Procedures
In August 2013, an anonymous survey was conducted among members of one of the largest Internet sites for men seeking social or sexual interactions with other men in the United States. An electronic email recruitment message was sent to all users of the site who resided in the United States at the time of the study, including a description of the study purpose and included a link to the study website. Upon visiting the study website, individuals were directed to a more detailed description of study procedures and, if interested, proceeded to the study consent form and to then to the study questionnaire. Analyses were restricted to individuals who were HIV uninfected at the time of the survey (by self report), provided the zip code of their current residence, and completed the desktop administration of the survey, since not all questions related to access to providers were asked in the mobile version of the survey. Of 65,935 emails that were opened on a desktop/laptop, 11,656 individuals clicked through to the survey (17.7%) and 7,531 (64.6%) started the survey, of whom 5,445 (72.3%) completed the survey. Of these, 4,098 (75.2%) provided valid zip code information and state of residence could be determined. Incentives were not provided for participation in the survey. The study was approved by the Institutional Review Board at The Fenway Institute, Boston, MA.
Measures
Demographics
State of residence was ascertained by asking in what zip code participants currently lived and was captured via a validated content field. Respondents were asked about their age, education (categorized as college graduate or above versus less than college graduate), annual income before taxes (categorized as less than $6,000, $6,000–$11,999, $12,000–$17,999, $18,000–$23,999, $24,000–$29,999, $30,000–$59,999, and $60,000 or more), sexual identity (coded as gay/homosexually-identified, bisexual, or heterosexual/straight-identified), and racial/ethnic identity (including white/Caucasian, African American/Black, Latino, or Asian/Pacific Islander).
PrEP and PEP Awareness and Use
Participants were asked about their awareness of PEP and PrEP by asking 1) “Before today, had you heard about PEP (i.e., post-exposure prophylaxis, medication taken by mouth AFTER a sexual encounter where you believe you may have been exposed to HIV?)” and 2) “Before today, had you heard about PrEP (i.e., pre-exposure prophylaxis, medication taken by mouth BEFORE sex as protection against HIV infection?)”. Participants were also asked if they had ever taken PEP or PrEP. Answers were coded dichotomously (yes/no).
Sexual behaviors
Participants were asked the number of men with whom they had condomless anal insertive or receptive intercourse (i.e., sex without a condom) in the previous 3 months; those who reported ≥1 episode of insertive and/or receptive condomless anal intercourse (CAI) were coded as having engaged in CAI in the last 3 months.
Access to healthcare
Participants were asked if they had visited a doctor, nurse, or other healthcare provider in the past 12 months, and if they had a primary care provider (PCP). If participants responded affirmatively, they were then asked if they were comfortable discussing with their primary healthcare provider that they had had sex with a man (coded yes/no). They were also asked if they had ever discussed with their primary provider (1) having CAI with a man or (2) ways to protect themselves against HIV infection during sex. Insurance status was assessed by asking what kind of health insurance coverage participants had (coded as any vs. no health insurance). Individual health insurance was included as a covariate since health insurance coverage has been shown to be associated with HIV-related outcomes such as medication adherence. As a general proxy for access to healthcare at the state level, the percent of the population in each state that was uninsured was included as an additional covariate because it was hypothesized that states with lower insurance coverage may be less supportive and also have fewer PEP/PrEP providers. This variable was assessed with data from the United States Census Bureau (http://www.census.gov/hhes/www/hlthins/data/index.html) and was defined as the average percent of the state’s population that was uninsured between 2010 and 2012.
State-level HIV prevalence
The number of people living with HIV per 100,000 population by state was included as an additional covariate to account for the state of the HIV epidemic in each state. This variable was measured by the Centers for Disease Control and Prevention’s HIV surveillance report for 2011.[25]
State-level structural stigma
State-level structural stigma is a composite variable addressing dimensions of prejudicial social environments at the state level, constructed according to identical methodology used in previous studies[26,27] and updated to reflect current state-level laws, policies, and demographics. This variable consisted of 4 components. First, we used a measure of the density of same-sex couples as defined by same-sex couples per 1,000 households in the state, drawn from 2010 U.S. census data. This measure was selected as an indicator of structural stigma given that a higher density of same-sex couples in a state indicates that same-sex relationships are more normative in that state. The index was calculated using the total number of households, as well as the number of households headed by a male and female same-sex unmarried partner couple for each census tract or county.[28]
The second variable was the proportion of public high schools with Gay-Straight Alliances (GSAs) per state. GSAs, which work towards creating a safe and supportive community in the school, are student-led organizations that provide a safe and supportive environment for the lesbian, gay, bisexual, and transgender (LGBT) community and their straight allies. This measure was selected as an indicator of structural stigma because a higher proportion of GSAs indicates schools that are committed to providing safe spaces for LGBT youth. Data on GSAs were obtained from Gay, Lesbian, and Straight Education Network for the year 2006; the number of public high schools in the state was obtained from the National Center for Education Statistics. We divided the number of GSAs by the number of public high schools in that state to create this item.
The third measure included state policies and laws related to sexual orientation discrimination (including legalized marriage for same-sex couples, employment non-discrimination laws, protections against hate crimes, and legality of joint adoption for same-sex couples) as of May 2013.[29] Laws and policies were included as one dimension of structural stigma because they indicate macro-level support and protection for sexual minority populations. For laws and policies, a summary variable was created summing the 4 laws together, such that any given state could range from 0 (no protective laws/policies) to 4 (the state has all 4 protective laws/policies).
The fourth measure was public opinion toward homosexuality and citizenship rights for same-sex couples as assessed through 41 national opinion polls.[15] Lax and Phillips[30] aggregated responses from 41 national polls from the Roper Center’s iPol archive, dating from 1999–2008. These polls, which were random national samples conducted by various organizations (e.g., Gallup, Pew), yielded approximately 80,000 responses. Policy-specific opinions were collected for the following areas: gay adoption, hate crimes, health benefits, discrimination in jobs and housing, marriage, sodomy, and civil unions (e.g., “Do you think there should be adoption rights for gay and lesbian couples?”). We used the mean value for these 7 opinions by state. This measure was included as a measure of social acceptance of sexual minority populations.
To create a composite variable for each of these 4 variables, a z-score was calculated for each dimension, which was then summed. The Cronbach’s alpha for the summary score for the 4 components of the composite variable was 0.87, suggesting high internal consistency. A principal components analysis resulted in the variables loading on to a single component with an eigenvalue of 3.16, suggesting that the items are loading onto a single construct of structural stigma, providing support for construct validity. Correlation coefficients between the four variables ranged from 0.62 (between the density of same-sex couples and proportion of public high schools with GSAs) and 0.78 (between laws/policies and public opinion towards homosexuality). Construct validity was established through previous work demonstrating that the measure was associated with suicide, tobacco use, and illicit drug use among LGB, but not heterosexual, populations.[26,31–33] The structural stigma variable was linked to survey responses through participants’ state of residence. For the composite structural stigma variable, a higher score indicates a more protective social environment (i.e., lower levels of structural stigma). The composite structural stigma score ranged from a low of −4.46 (Mississippi), with highest level of structural stigma (i.e., least supportive environment), to 7.90 (Massachusetts), with the lowest level of structural stigma (i.e., most supportive environment, Figure 1).
Figure 1.
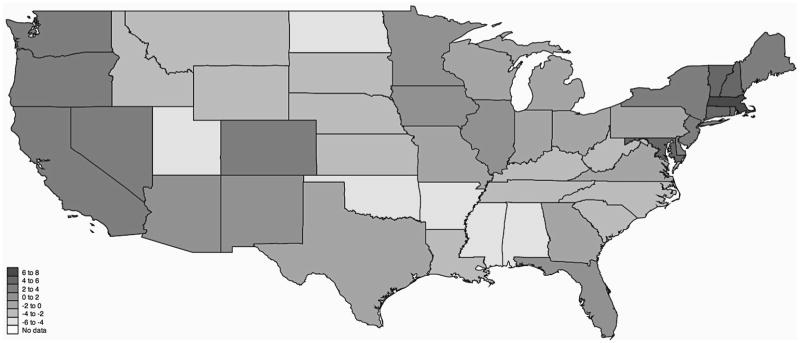
State-level structural stigma related to sexual orientation. Lighter shades of blue indicate less supportive social environments (higher structural stigma); darker shades of blue indicate more supportive social environments (lower structural stigma).
Statistical Analysis
Descriptive statistics were calculated for demographic, sexual behavior, awareness/use of PEP and PrEP, and provider communication variables. Logistic generalized estimating equation (GEE) models were used to assess the association between structural stigma and independent variables, using an exchangeable correlation matrix. A GEE approach was used to account for within-state clustering (i.e., individuals nested within states). Primary analyses modeled the structural stigma score continuously as the independent variable of interest. Ten models were run, one for each dependent variable of interest, including CAI, having heard of PEP, having taken PEP, having heard of PrEP, having taken PrEP, having been to a doctor in the previous 12 months, having a primary provider, comfort discussing having sex with men with provider, discussing CAI with provider, and discussing HIV prevention with provider. Multivariable GEE models adjusting for potentially confounding factors, including age, race/ethnicity, individual insurance coverage, state-level insurance coverage for analyses related to PEP and PrEP and providers, number of people living with HIV per 100,000 population per state, sexual identity, education, and income were run to assess the adjusted association between structural stigma and each independent variable of interest. Models assessing comfort with PCPs and having discussed CAI and HIV prevention were restricted to individuals who reported having a PCP. As a sensitivity analysis, all analyses were re-run using the structural stigma score as a categorical variable by quartile. For analyses considering use of PrEP and PEP, a sensitivity analysis was run limiting the sample only to those who had previously heard of PrEP or PEP, respectively. A complete case analysis was conducted for all analyses. All analyses were run in Stata 13.0 (StataCorp, College Station, TX).
RESULTS
Table 1 lists descriptive characteristics for the study sample. The median age was 44 years (interquartile range [IQR] 33 to 52 years). Most participants (85.2%) identified as White/Caucasian and as gay/homosexual (78.0%). While most participants had visited a healthcare provider in the past year (88.0%) and had a primary care provider (84.0%), fewer were comfortable disclosing to their primary care provider that they had had sex with a man (55.0%) or had discussed CAI (36.7%) or HIV prevention strategies (40.3%) with their primary care provider.
Table 1.
Descriptive characteristics of the study sample (N=4,098)
| Median, IQR or N, % | |
|---|---|
|
| |
| Age (median, IQR) | 45.5 (34 to 53) |
|
| |
| Race/Ethnicity | |
| White/Caucasian | 3,521 (86.1%) |
| Black/African American | 168 (4.1%) |
| Latino/Hispanic | 274 (6.7%) |
| Asian | 114 (2.8%) |
| Native American | 104 (2.5%) |
| Multiracial | 105 (2.6%) |
|
| |
| Any health insurance coverage | 3,520 (86.1%) |
|
| |
| Sexual identity | |
| Gay/homosexual | 3,285 (70.1%) |
| Bisexual | 890 (21.7%) |
| Heterosexual/straight | 105 (2.6%) |
|
| |
| College graduate or higher education | 2,894 (70.7%) |
|
| |
| Income | |
| <$6,000 | 201 (5.0%) |
| $6,000 to 11,999 | 191 (4.7%) |
| $12,000 to 17,999 | 191 (4.7%) |
| $18,000 to 23,999 | 246 (6.1%) |
| $24,000 to 29,999 | 275 (6.8%) |
| $30,000 to 59,999 | 1,137 (28.2%) |
| $60,000+ | 1,791 (44.4%) |
|
| |
| Any condomless anal intercourse in past 3 months | 1,872 (59.7%) |
|
| |
| Heard of PEP | 1,743 (42.5%) |
|
| |
| Ever taken PEP | 129 (3.2%) |
|
| |
| Heard of PrEP | 1,224 (29.9%) |
|
| |
| Ever taken PrEP | 50 (1.2%) |
|
| |
| Been to doctor in past 12 months | 3,629 (88.5%) |
|
| |
| Have primary care provider | 3,434 (84.0%) |
|
| |
| Comfort discussing male-male sex with primary provider | 1,892 (55.0%) |
|
| |
| Ever discussed condomless anal intercourse with primary provider | 1,255 (36.5%) |
|
| |
| Ever discussed HIV prevention with primary provider | 1,334 (38.9%) |
Abbreviations: IQR, interquartile range; PEP, post-exposure prophylaxis; PrEP, pre-exposure prophylaxis
Table 2 presents associations between state-level structural stigma and CAI as well as awareness of and having taking PEP and PrEP, modeled per one-unit increase in the structural stigma score and categorically by quartile. In multivariable models, lower structural stigma was associated with decreased odds of CAI in the previous 3 months (Adjusted Odds Ratio (aOR) 0.97, 95% Confidence Interval [CI]: 0.94–0.99). Lower levels of structural stigma were also associated with increased odds of having heard of PEP (aOR 1.06, 95% CI: 1.02–1.09) and PrEP (aOR 1.21, 95% CI: 1.01–1.44) as well as with having taken PEP (aOR 1.10, 95% CI: 1.00–1.21) and PrEP (aOR 1.23, 95% CI: 1.10–1.38). In sensitivity analyses restricted only to those who had heard of PEP, structural stigma was no longer statistically significantly associated with having taken PEP (aOR 1.07, 95% CI: 0.97–1.18). Restricting only to those who had heard of PrEP, results for the association between structural stigma and having taken PrEP did not change (aOR 1.21, 95% CI: 1.08–1.35). Sensitivity analyses modeling the structural stigma score categorically (by quartile) were generally consistent with continuous results, with stronger effects seen in higher quartiles.
Table 2.
Association between state-level structural stigma related to sexual orientation1 and HIV risk behavior and experience with HIV pre- and post-exposure prophylaxis, United States, 2013
| Modeled Continuously (Per One-Unit Increase in Structural Stigma) | Modeled Categorically | ||||||||
|---|---|---|---|---|---|---|---|---|---|
|
| |||||||||
| Bivariate2 | Multivariable3 | Bivariate2 | Multivariable3 | ||||||
|
| |||||||||
| OR (95% CI) | P-value | aOR (95% CI) | P-value | OR (95% CI) | P-value | aOR (95% CI) | P-value | ||
|
| |||||||||
| Any CAI | 0.97 (0.94 to 1.00) | 0.02 | 0.97 (0.94 to 0.99) | 0.02 | 1st Quartile4 | 1.00 | 1.00 | ||
| 2nd Quartile | 0.90 (0.66 to 1.23) | 0.53 | 0.84 (0.62 to 1.16) | 0.29 | |||||
| 3rd Quartile | 0.80 (0.59 to 1.08) | 0.15 | 0.74 (0.55 to 1.00) | 0.051 | |||||
| 4th Quartile | 0.83 (0.62 to 1.11) | 0.21 | 0.71 (0.52 to 0.97) | 0.03 | |||||
|
| |||||||||
| Heard of PEP | 1.06 (1.02 to 1.10) | 0.001 | 1.06 (1.02 to 1.09) | 0.001 | 1st Quartile4 | 1.00 | 1.00 | ||
| 2nd Quartile | 1.09 (0.81 to 1.48) | 0.57 | 1.02 (0.79 to 1.32) | 0.87 | |||||
| 3rd Quartile | 1.21 (0.90 to 1.62) | 0.21 | 1.09 (0.85 to 1.40) | 0.49 | |||||
| 4th Quartile | 1.87 (1.40 to 2.50) | <0.001 | 1.70 (1.31 to 2.21) | <0.001 | |||||
|
| |||||||||
| Ever taken PEP | 1.10 (1.01 to 1.20) | 0.025 | 1.10 (1.00 to 1.21) | 0.050 | 1st Quartile4 | 1.00 | 1.00 | ||
| 2nd Quartile | 0.93 (0.37 to 2.33) | 0.88 | 0.88 (0.34 to 2.25) | 0.79 | |||||
| 3rd Quartile | 0.97 (0.40 to 2.33) | 0.94 | 0.97 (0.39 to 2.38) | 0.94 | |||||
| 4th Quartile | 2.24 (1.01 to 4.97) | 0.047 | 1.96 (0.82 to 4.69) | 0.13 | |||||
|
| |||||||||
| Heard of PrEP | 1.05 (1.01 to 1.09) | 0.02 | 1.21 (1.01 to 1.44) | 0.035 | 1st Quartile4 | 1.00 | 1.00 | ||
| 2nd Quartile | 1.28 (0.89 to 1.85) | 0.19 | 1.21 (0.86 to 1.71) | 0.27 | |||||
| 3rd Quartile | 1.39 (0.98 to 1.98) | 0.07 | 1.31 (0.94 to 1.82) | 0.11 | |||||
| 4th Quartile | 1.77 (1.25 to 2.51) | 0.001 | 1.66 (1.17 to 2.36) | 0.005 | |||||
|
| |||||||||
| Ever taken PrEP | 1.13 (1.03 to 1.25) | 0.01 | 1.23 (1.10 to 1.38) | <0.001 | 1st Quartile4 | 1.00 | 1.00 | ||
| 2nd Quartile | 0.83 (0.25 to 2.70) | 0.75 | 0.59 (0.19 to 1.79) | 0.35 | |||||
| 3rd Quartile | 0.73 (0.23 to 2.34) | 0.60 | 0.58 (0.20 to 1.70) | 0.32 | |||||
| 4th Quartile | 2.51 (0.91 to 6.91) | 0.08 | 2.28 (0.87 to 5.96) | 0.09 | |||||
Abbreviations: CAI, condomless anal intercourse; OR, odds ratio; CI, confidence interval; PEP, post-exposure prophylaxis; PrEP, pre-exposure prophylaxis
Higher scores represent more supportive environments (less state-level structural stigma);
Logistic generalized estimating equation;
Multivariable logistic generalized estimating equation adjusting for age, race/ethnicity, insurance status (individual and state-level coverage for PEP/PrEP models), state-wide HIV prevalence, sexual identity, education, and income.
First quartile represents states with highest levels of structural stigma and 4th quartile represents those with lowest levels of structural stigma
Table 3 presents associations between state-level structural stigma and provider-related variables, modeled both continuously (per one-unit increase in the structural stigma score) and categorically (by quartile). Lower levels of structural stigma were associated with increased odds of being comfortable discussing the following with a primary care provider: having had sex with a man (aOR 1.08, 95% CI: 1.05–1.11); having discussed CAI (aOR 1.06, 95% CI: 1.02–1.10); and having discussed HIV prevention strategies (aOR 1.06, 95% CI: 1.02–1.10). Analyses modeling the structural stigma score categorically were consistent with modeling the score continuously.
Table 3.
Association between state-level structural stigma related to sexual orientation1 and provider communication factors, United States, 2013
| Modeled Continuously (Per One-Unit Increase in Structural Stigma) | Modeled Categorically | ||||||||
|---|---|---|---|---|---|---|---|---|---|
|
| |||||||||
| Bivariate2 | Multivariable3 | Bivariate2 | Multivariable3 | ||||||
|
| |||||||||
| OR (95% CI) | P-value | aOR (95% CI) | P-value | OR (95% CI) | P-value | aOR (95% CI) | P-value | ||
|
| |||||||||
| Been to doctor in past 12 months | 1.03 (1.00 to 1.07) | 0.08 | 1.02 (0.97 to 1.06) | 0.50 | 1st Quartile4 | Ref | Ref | Ref | |
| 2nd Quartile | 0.94 (0.64 to 1.37) | 0.75 | 0.84 (0.57 to 1.22) | 0.35 | |||||
| 3rd Quartile | 1.02 (0.71 to 1.48) | 0.92 | 0.82 (0.56 to 1.20) | 0.31 | |||||
| 4th Quartile | 1.25 (0.86 to 1.82) | 0.25 | 0.93 (0.62 to 1.40) | 0.73 | |||||
|
| |||||||||
| Have a primary provider | 1.04 (1.01 to 1.07) | 0.02 | 0.97 (0.93 to 1.01) | 0.14 | 1st Quartile4 | Ref | Ref | Ref | Ref |
| 2nd Quartile | 0.93 (0.59 to 1.17) | 0.28 | 0.83 (0.58 to 1.19) | 0.31 | |||||
| 3rd Quartile | 1.00 (0.71 to 1.40) | 0.98 | 0.72 (0.51 to 1.03) | 0.07 | |||||
| 4th Quartile | 1.23 (0.87 to 1.74) | 0.24 | 0.74 (0.51 to 1.08) | 0.12 | |||||
|
| |||||||||
| Comfort discussing having sex with men with provider | 1.08 (1.05 to 1.12) | <0.001 | 1.08 (1.05 to 1.11) | <0.001 | 1st Quartile4 | Ref | Ref | Ref | Ref |
| 2nd Quartile | 1.81 (1.37 to 2.39) | <0.001 | 1.74 (1.31 to 2.29) | <0.001 | |||||
| 3rd Quartile | 2.00 (1.53 to 2.61) | <0.001 | 1.94 (1.48 to 2.54) | <0.001 | |||||
| 4th Quartile | 2.59 (1.99 to 3.38) | <0.001 | 2.49 (1.87 to 3.32) | <0.001 | |||||
|
| |||||||||
| Ever discussed CAI with primary provider | 1.07 (1.03 to 1.10) | <0.001 | 1.06 (1.02 to 1.10) | 0.001 | 1st Quartile4 | Ref | Ref | Ref | Ref |
| 2nd Quartile | 1.16 (0.92 to 1.46) | 0.21 | 1.15 (0.83 to 1.59) | 0.39 | |||||
| 3rd Quartile | 1.18 (0.94 to 1.47) | 0.15 | 1.17 (0.86 to 1.60) | 0.32 | |||||
| 4th Quartile | 1.57 (1.27 to 1.94) | <0.001 | 1.73 (1.25 to 2.40) | 0.001 | |||||
|
| |||||||||
| Ever discussed HIV prevention with primary provider | 1.06 (1.02 to 1.09) | 0.001 | 1.06 (1.02 to 1.10) | 0.002 | 1st Quartile4 | Ref | Ref | Ref | Ref |
| 2nd Quartile | 1.65 (1.18 to 2.30) | 0.003 | 1.50 (1.04 to 2.17) | 0.03 | |||||
| 3rd Quartile | 1.55 (1.12 to 2.13) | 0.008 | 1.47 (1.03 to 2.10) | 0.04 | |||||
| 4th Quartile | 1.97 (1.44 to 2.71) | <0.001 | 1.80 (1.22 to 2.64) | 0.003 | |||||
Abbreviations: OR, odds ratio; CI, confidence interval; aOR, adjusted odds ratio; CAI, condomless anal intercourse
Higher scores represent more supportive environments (less state-level structural stigma);
Logistic generalized estimating equation;
Multivariable logistic generalized estimating equation adjusting for age, race/ethnicity, insurance status (individual and state-level coverage), state-wide HIV prevalence, sexual identity, education, and income.
First quartile represents states with highest levels of structural stigma and 4th quartile represents those with lowest levels of structural stigma.
DISCUSSION
The results of this study indicate that high state-level structural stigma (less state-level supportive environments for LGBT people) is significantly associated with increased sexual risk behavior, decreased awareness and use of antiretroviral chemoprophylaxis, and decreased comfort discussing sexual behavior with primary care providers among HIV uninfected MSM in the United States. The combination of these factors suggests that structural stigma may be a particularly important contributor to the current dynamics of the HIV epidemic among MSM in the United States.
Lower levels of state-level structural stigma were associated with reductions in CAI. One potential mechanism explaining this relationship is internalized stigma, which is associated with HIV risk behaviors among MSM.[24,34–36] For men living in more stigmatizing communities, negative social attitudes and environments may be internalized, which may lead to increased engagement in HIV-associated risk behavior. A multinational study in Europe demonstrated that stigmatizing structural-level policies are associated with internalized homonegativity,[37] and this relationship likely exists in the United States as well, though this hypothesis awaits empirical testing.
In addition to increased HIV risk behavior, structural stigma was associated with decreased awareness of both PEP and PrEP as HIV prevention strategies. In states with higher levels of structural stigma, it is possible that there are fewer providers who prescribe PEP or PrEP and less community awareness of these HIV prevention strategies. Individuals living in high structural stigma states were also less likely to have taken PEP or PrEP, which may be a function of reduced awareness about these modalities, as well as lack of access to providers who prescribe PEP and/or PrEP. Importantly, we adjusted for general access to healthcare via the percent uninsured in the state, indicating that the relationship between structural stigma and PEP/PrEP use is independent of general insurance coverage. Nevertheless, future studies would benefit from incorporating specific measures of PEP and PrEP use at the state level as additional covariates.
Third, men living in states with higher levels of structural stigma were less likely to report discussing having sex with men, CAI, and HIV prevention strategies with their providers. Some research arising from less socially supportive environments has suggested that enacted stigma is associated with decreased healthcare seeking among MSM.[21] In more stigmatizing social environments, the perception of potential discrimination from healthcare providers may prevent individuals from discussing HIV prevention strategies, even if they are engaged in care. In these settings, there may be a greater anticipation of discrimination accompanying disclosure of a minority sexual orientation that prevents individuals from being willing to discuss sexual behaviors and HIV prevention with their providers.[38] Additionally, in states with increased anti-gay prejudice, fewer LGBT-friendly healthcare providers and facilities may exist. These results highlight that interventions with healthcare providers to reduce healthcare-related stigma, especially in states with high-structural stigma, may help individuals who are engaged in care to be more comfortable discussing important HIV-related topics with their providers.
The results of this study must be considered in the context of several limitations. The study population was recruited from an online social and sexual networking website, and study participants are not representative of all MSM. However, all 50 states in the United States were represented in this sample, providing adequate variation in level of structural stigma surrounding sexual minorities. Nonetheless, participation differed by state, with considerable differences in the number of participants in some states compared to others, ranging from 9 in Wyoming to 308 in New York. This may limit power in states with less representation, although this is mitigated by using a categorical as well as continuous measure of structural stigma. We did not assess geographic mobility. It is possible that healthier or better-off respondents who originated in higher stigma environments moved to lower stigma environments. However, previous work has shown that health outcomes are not related to mobility among sexual minorities[15], so selection bias is unlikely to fully explain these results.
There may be differences within states that are obscured by a state-level measure (e.g., local ordinances that have protective policies within states that do not confer these protections). The use of a state-level measure may therefore result in some misclassification of our exposure of interest. However, given that state-level structural stigma is a distal determinant of health, we expect that this misclassification would underestimate the relationship between structural stigma and HIV outcomes. Although effect sizes were relatively small, at a population level there could be substantial health benefits associated with reducing structural stigma. For example, a 5-unit increase in the structural stigma measure (i.e., a 5-unit increase in the supportiveness of the social climate), which is plausible given the 12-point range of this measure, would lead to a 48% increase in odds of feeling comfortable discussing same-sex behavior with a primary care provider. At the population level, improvements to the social climate could therefore result in much greater increases in access to PEP, PrEP, and providers. The measure of public opinion was an aggregate measure from 1999–2008, rather than from 2013, the year the study occurred. Although it is likely that public opinions evolved during this period, the measure as an aggregate reflects trends over time. Given that it likely takes some time for changes in stigma to translate into changes in population health, this measure may provide a more accurate representation of public opinion toward homosexuality than would an assessment at a single time point.
Overall, these results provide evidence that state-level structural stigma affects HIV prevention efforts in the United States, underscoring the importance of addressing sources of stigma at multiple levels to improve the health of sexual minority populations. Although legal policies such as the right to marriage are rapidly changing in the United States, the social landscape in the United States varies greatly, and understanding the impact of negative attitudes and policies is crucial to best inform structural interventions and legal reforms that impact the domestic HIV epidemic. The results of this study underscore the urgent need for expanding policy reform and structural interventions to reduce stigma in the United States to improve the health of sexual minorities.
Acknowledgments
Funding: This work was funded by an unrestricted research grant from Gilead Sciences. CEO was supported by a National Institute of Allergy and Infectious Disease T32 NRSA grant (T32AI007535; PI: Seage). CEO is currently supported by a National Institute of Drug Abuse T32 NRSA (T32DA013911; PI: Flanigan). APB is supported by Eunice Kennedy Shriver National Institute of Child Health & Human Development T32 HD049339 (PI: Nathanson) and the National Institutes of Mental Health R25 MH083620 (PI: Flanigan). MLH is supported by a National Institute of Drug Abuse Mentored Research Scientist Development Award (K01 DA032558). DSK is supported by a National Institutes of Mental Health Career Development Award (MH098795).
Footnotes
Meeting Presentation: Results presented in part at the HIV Research for Prevention conference, October 28-31 2014, Cape Town, South Africa
Conflicts of Interest: None to report.
Author Contributions
Design of the study: CEO, APB, MLH, DK, DSN, MJM, KHM. Collected data: DK, DSN, MJM, KHM. Conducted analyses: CEO, APB, MLH. Interpreted results: CEO, APB, MLH, KHM. Critically reviewed and approved the final version of the manuscript: CEO, APB, MLH, DK, DSN, MJM, KHM.
References
- 1.Prejean J, Song R, Hernandez A, Ziebell R, Green T, Walker F, et al. Estimated HIV Incidence in the United States, 2006–2009. PLoS ONE. 2011;6:e17502. doi: 10.1371/journal.pone.0017502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Grant RM, Lama JR, Anderson PL, McMahan V, Liu AY, Vargas L, et al. Preexposure Chemoprophylaxis for HIV Prevention in Men Who Have Sex with Men. N Engl J Med. 2010;363:2587–2599. doi: 10.1056/NEJMoa1011205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Grant RM, Anderson PL, McMahan V, Liu AY, Amico KR, Mehrotra M, et al. Uptake of pre-exposure prophylaxis, sexual practices, and HIV incidence in men and transgender women who have sex with men: a cohort study. The Lancet Infectious Diseases. 2014:1–10. doi: 10.1016/S1473-3099(14)70847-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Cardo DM, Culver DH, Ciesielski CA, Srivastava PU, Marcus R, Abiteboul D, et al. A Case–Control Study of HIV Seroconversion in Health Care Workers after Percutaneous Exposure. N Engl J Med. 1997;337:1485–1490. doi: 10.1056/NEJM199711203372101. [DOI] [PubMed] [Google Scholar]
- 5.Adimora AA, Ramirez C, Schoenbach VJ, Cohen MS. Policies and politics that promote HIV infection in the Southern United States. AIDS. 2014:1. doi: 10.1097/QAD.0000000000000225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Adimora AA, Auerbach JD. Structural Interventions for HIV Prevention in the United States. JAIDS Journal of Acquired Immune Deficiency Syndromes. 2010;55:S132–S135. doi: 10.1097/QAI.0b013e3181fbcb38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hatzenbuehler ML, O’Cleirigh C, Grasso C, Mayer K, Safren S, Bradford J. Effect of Same-Sex Marriage Laws on Health Care Use and Expenditures in Sexual Minority Men: A Quasi-Natural Experiment. Am J Public Health. 2012;102:285–291. doi: 10.2105/AJPH.2011.300382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Pellowski JA, Kalichman SC, Matthews KA, Adler N. A pandemic of the poor: Social disadvantage and the U.S. HIV epidemic. American Psychologist. 2013;68:197–209. doi: 10.1037/a0032694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Oldenburg CE, Perez-Brumer AG, Reisner SL. Poverty matters: contextualizing the syndemic condition of psychological factors and newly diagnosed HIV infection in the United States. AIDS. 2014:1. doi: 10.1097/QAD.0000000000000491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Oldenburg CE, Barnighausen T, Harling G, Mimiaga MJ, Mayer KH. Adherence to Post-Exposure Prophylaxis for Non-forcible Sexual Exposure to HIV: A Systematic Review and Meta-Analysis. AIDS Behav. doi: 10.1007/s10461-013-0567-0. Published Online First: 23 July 2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Chacko L, Ford N, Sbaiti M, Siddiqui R. Adherence to HIV post-exposure prophylaxis in victims of sexual assault: a systematic review and meta-analysis. Sexually Transmitted Infections. 2012;88:335–341. doi: 10.1136/sextrans-2011-050371. [DOI] [PubMed] [Google Scholar]
- 12.Gonzalez JS, WBA, Psaros C, Safren SA. Depression and HIV/AIDS Treatment Nonadherence: A Review and Meta-analysis. J Acquir Immune Defic Syndr. 2011;58:181–187. doi: 10.1097/QAI.0b013e31822d490a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Baral S, Logie CH, Grosso A, Wirtz AL, Beyrer C. Modified social ecological model: a tool to guide the assessment of the risks and risk contexts of HIV epidemics. BMC Public Health. 2013;13:1–1. doi: 10.1186/1471-2458-13-482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Human Rights Campaign. 2013 Annual Report. Human Rights Campaign; 2013. [Google Scholar]
- 15.Hatzenbuehler ML, Bellatorre A, Lee Y, Finch BK, Muennig P, Fiscella K. Structural stigma and all-cause mortality in sexual minority populations. Social Science & Medicine. 2014;103:33–41. doi: 10.1016/j.socscimed.2013.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hatzenbuehler ML, Phelan JC, Link BG. Stigma as a Fundamental Cause of Population Health Inequalities. AJPH. 2013;103:813–821. doi: 10.2105/AJPH.2012.301069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.King EJ, Maman S, Bowling JM, Moracco KE, Dudina V. The Influence of Stigma and Discrimination on Female Sex Workers’ Access to HIV Services in St. Petersburg, Russia. AIDS Behav. 2013;17:2597–2603. doi: 10.1007/s10461-013-0447-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Link BG, Phelan JC. Conceptualizing Stigma. Annual Review of Sociology. 2001:363–385. [Google Scholar]
- 19.Hatzenbuehler ML, Link BG. Introduction to the special issue on structural stigma and health. Social Science & Medicine. 2014;103:1–6. doi: 10.1016/j.socscimed.2013.12.017. [DOI] [PubMed] [Google Scholar]
- 20.Fay H, Baral SD, Trapence G, Motimedi F, Umar E, Iipinge S, et al. Stigma, Health Care Access, and HIV Knowledge Among Men Who Have Sex With Men in Malawi, Namibia, and Botswana. AIDS Behav. 2010;15:1088–1097. doi: 10.1007/s10461-010-9861-2. [DOI] [PubMed] [Google Scholar]
- 21.Risher K, Adams D, Sithole B, Ketende S, Kennedy C, Mnisi Z, et al. Sexual stigma and discrimination as barriers to seeking appropriate healthcare among men who have sex with men in Swaziland. J Int AIDS Soc. 2013;16 doi: 10.7448/IAS.16.3.18715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Diaz RM, Ayala G, Bein E, Henne J, Marin BV. The Impact of Homophobia, Poverty, and Racism on the Mental Health of Gay and Bisexual Latino Men: Findings From 3 US Cities. Am J Public Health. 2001;91:927–932. doi: 10.2105/ajph.91.6.927. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Thomas B, Mimiaga MJ, Mayer KH, Perry NS, Swaminathan S, Safren SA. The influence of stigma on HIV risk behavior among men who have sex with men in Chennai, India. AIDS Care. 2012;24:1401–1406. doi: 10.1080/09540121.2012.672717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Oldenburg C, Biello KB, Colby D, Closson E, Mai T, Nguyen T, et al. Stigma related to sex work among men who engage in transactional sex with men in Ho Chi Minh City, Vietnam. Int J Public Health. 2014:1–8. doi: 10.1007/s00038-014-0562-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Centers for Disease Control and Prevention (CDC) Monitoring Selected National HIV Prevention and Care Objectives by Using HIV Surveillance Data— United States and6 Dependent Areas—2011. 2011. pp. 1–47. [Google Scholar]
- 26.Hatzenbuehler ML. The Social Environment and Suicide Attempts in Lesbian, Gay, and Bisexual Youth. Pediatrics. 2011;127:896–903. doi: 10.1542/peds.2010-3020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hatzenbuehler ML, McLaughlin KA. Structural Stigma and Hypothalamic–Pituitary–Adrenocortical Axis Reactivity in Lesbian, Gay, and Bisexual Young Adults. ann behav med. 2013;47:39–47. doi: 10.1007/s12160-013-9556-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Gates GJ, Ost J. The Gay and Lesbian Atlas. Washington, DC: The Urban Institute Press; 2004. [Google Scholar]
- 29.Itaborahy LP, Zhu J. State-Sponsored Homophobia: A world survey of laws: criminalization, protection, and recognition of same-sex love. International Lesbian Gay Bisexual Trans and Intersex Association; 2013. [Google Scholar]
- 30.Lax JR, Phillips JH. Gay Rights in the States: Public Opinion and Policy Responsiveness. Am Polit Sci Rev. 2009;103:367. [Google Scholar]
- 31.Pachankis JE, Hatzenbuehler ML, Starks TJ. The influence of structural stigma and rejection sensitivity on young sexual minority men’s daily tobacco and alcohol use. Social Science & Medicine. 2014;103:67–75. doi: 10.1016/j.socscimed.2013.10.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Duncan DT, Hatzenbuehler ML, Johnson RM. Neighborhood-level LGBT hate crimes and current illicit drug use among sexual minority youth. Drug and Alcohol Dependence. 2014;135:65–70. doi: 10.1016/j.drugalcdep.2013.11.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Hatzenbuehler ML, Jun H-J, Corliss HL, Austin SB. Structural Stigma and Cigarette Smoking in a Prospective Cohort Study of Sexual Minority and Heterosexual Youth. ann behav med. 2013;47:48–56. doi: 10.1007/s12160-013-9548-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Hatzenbuehler ML, Nolen-Hoeksema S, Erickson SJ. Minority stress predictors of HIV risk behavior, substance use, and depressive symptoms: Results from a prospective study of bereaved gay men. Health Psychology. 2008;27:455–462. doi: 10.1037/0278-6133.27.4.455. [DOI] [PubMed] [Google Scholar]
- 35.Ross MW, Berg RC, Schmidt AJ, Hospers HJ, Breveglieri M, Furegato M, et al. Internalised homonegativity predicts HIV-associated risk behavior in European men who have sex with men in a 38-country cross-sectional study: some public health implications of homophobia. BMJ Open. 2013;3:e001928–e001928. doi: 10.1136/bmjopen-2012-001928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Ross MW, Kajubi P, Mandel JS, McFarland W, Raymond HF. Internalized homonegativity/homophobia is associated with HIV-risk behaviours among Ugandan gay and bisexual men. International Journal of STD & AIDS. 2013;24:409–413. doi: 10.1177/0956462412472793. [DOI] [PubMed] [Google Scholar]
- 37.Berg RC, Ross MW, Weatherburn P, Schmidt AJ. Structural and enviromental factors are associated with internalised homonegativity in men who have sex with men: Findings from the European MSM Internet Survey (EMIS) in 38 countries. Social Science & Medicine. 2013;78:61–69. doi: 10.1016/j.socscimed.2012.11.033. [DOI] [PubMed] [Google Scholar]
- 38.Golub SA, Gamarel KE. The Impact of Anticipated HIV Stigma on Delays in HIV Testing Behaviors: Findings from a Community-Based Sample of Men Who Have Sex with Men and Transgender Women in New York City. AIDS Patient Care and STDs. 2013;27:621–627. doi: 10.1089/apc.2013.0245. [DOI] [PMC free article] [PubMed] [Google Scholar]


