Abstract
Background
Divorce is a major life stressor that can have economic, emotional, and physical health consequences. However, the cumulative association between divorce and risks for acute myocardial infarction (AMI) is unknown. This study investigated the association between lifetime exposure to divorce and the incidence of AMI in U.S. adults.
Methods and Results
We used nationally representative data from a prospective cohort of ever-married adults aged 45 to 80 (n=15,827) who were followed biennially from 1992 to 2010. Approximately 14% of men and 19% of women were divorced at baseline and more than one-third of the cohort had at least one divorce in their lifetime. In 200,524 person-years of follow-up, 8% (n=1,211) of the cohort had an AMI and age-specific rates of AMI were consistently higher in those who were divorced relative to those who were continuously married (P<.05). Results from competing-risk hazard models showed that AMI risks were significantly higher in women who had 1 divorce (HR, 1.24; 95% CI, 1.01-1.55), 2 or more divorces (HR, 1.77; 95% CI, 1.30-2.41), and among the remarried (HR, 1.35; 95% CI, 1.07-1.70) compared with continuously married women after adjusting for multiple risk factors. Multivariable-adjusted risks were elevated only in men with a history of 2 or more divorces (HR, 1.30; 95%CI, 1.02-1.66) relative to continuously married men. Men who remarried had no significant risk for AMI. Interaction terms for sex were not statistically significant.
Conclusions
Divorce is a significant risk factor for AMI. The risks associated with multiple divorces are especially high in women and are not reduced with remarriage.
Keywords: acute myocardial infarction, divorce, social factors
Coronary heart disease afflicts nearly half of U.S. men and more than a third of U.S. women after age 40 and is the single largest killer of Americans.1-4 According to recent estimates, nearly 1 million adults will have an acute myocardial infarction (AMI) this year—approximately one every 44 seconds—and cost the United States nearly $12 billion in hospital expenses.5 Although major risk factors for AMI have been widely documented—e.g., smoking, hypertension, diabetes3,6-9—the associations between social stressors and AMI risks are not well understood. By age 50, more than a third of all adults will have divorced and upwards of a quarter will have married two or more times.10 Although studies have shown that divorce is a major life stressor linked to poor health outcomes,11-17 research has focused almost entirely on the cross-sectional risks related to current marital status and have largely ignored lifetime exposure to divorce and its potential consequences for the cardiovascular health of men and women.13,16,18-23
It is well documented that men have significantly greater risk of AMI than women,1,3,24 and on average, experience their first event 7 years earlier than women (age 65 vs. 72, respectively).3 Patterns of divorce and remarriage also differ by gender. For example, men are much more likely to remarry after divorce than women, and among those who remarry, men remarry sooner than women.10,25 There is also evidence to suggest that marital loss has a greater impact on the health of women than men;21,26 particularly cardiovascular health.16 The reasons for these differences are not entirely known; however, studies have shown that divorced women suffer greater economic losses and emotional distress than divorced men;16,26-29 alternatively, divorced men lack the social control and obligations of marriage that encourage a healthy diet, moderate alcohol consumption, and the avoidance of smoking.30-32
This study is the first prospective investigation of the cumulative association between divorce and risks for AMI in U.S. men and women. We used data from a nationally representative sample of middle-aged and older adults followed biennially from 1992 to 2010 to examine how marital status and the number of divorces in one's lifetime were associated with incident AMI. We examined the associations separately in men and women and assessed whether and to what extent multiple socioeconomic, psychosocial, and behavioral risk factors contributed to the associations.
Methods
Study Population
Nationally representative data from the Health and Retirement Study (HRS) were used for analysis. The HRS is an ongoing prospective cohort study of U.S. adults over the age of 50 sponsored by the National Institute on Aging (NIA) and the Institute for Social Research at the University of Michigan.33 The original HRS cohort included 9,824 age-eligible respondents born in 1931 to 1941 who have been interviewed biennially since 1992. The initial response rate was 82% and re-interview response rates were approximately 94% for 1994-2010, with low attrition due to non-response and lost tracking. Since 1998, the HRS has been supplemented with age-selective birth cohorts to replenish the nationally representative sample of older adults. Details of the multistage sampling design, implementation, and response rates have been documented in detail elsewhere.33
Data for the study come from 16,694 participants from the original HRS birth cohort, the War Baby cohort (WB: 1942-1947), and Early Baby-Boom cohort (EBB: 1948-1953) who were first interviewed in 1992, 1998, and 2004, respectively, and re-interviewed every two years through 2010. We excluded 854 adults (∼5%) who never married and an additional thirteen adults who reported an AMI prior to baseline. A person-year file was constructed from the respondents' age-specific cumulative exposure to AMI so that each observation was a record for every additional year beyond their age at entry in the study. Analyses were restricted to 15,827 adults aged 45-65 at baseline who reported having ever married (94.9%) and had complete data for the study variables (<1%). On average, HRS participants contributed approximately 8 person-years over the 18-year study period. A total of 1,211 AMI events (7.7%) were reported during the 200,531 person-years of observation. The data used in this were deemed exempt from the Duke University institutional review board because the data were de-identified and publically accessible.
Measurement
A distinctive feature of the HRS is the detailed collection of data on marital relationships, family structure, and related changes. More than 50 years of prospective and retrospective data from HRS interviews were used to reconstruct marital histories for all study participants. Marital information was ascertained from detailed responses to interview questions about the beginning/ending dates (in years and/or months) of all marriages and marital losses reported by HRS, WB, and EBB cohort members. The subjects' month/year-specific information was converted to age-specific data using date of birth, date of interview, and date of event. Time-varying dichotomous measures were included to capture stability and changes in marital status (continuously married, divorced, widowed, or remarried) and the cumulative number of divorces (0, 1, or ≥2 divorces) experienced by participants. Being continuously married (i.e., never divorced or widowed) was the reference group in the analyses. The small number of study subjects with more than two divorces prohibited additional categorizations of divorce for analysis.
Multivariable models adjusted for background characteristics that included age at study entry, HRS study cohort (WB, EBB, or initial HRS), race/ethnicity (Hispanic, non-Hispanic white, non-Hispanic black, or non-Hispanic other race), and geographic region (South or other). Several categories of previously identified cardiovascular risks also were examined as possible factors contributing to the associations. Socioeconomic factors included the respondents' reports of educational attainment (years), primary lifetime occupational status (professional, managerial, or other occupation), employment status (employed, unemployed, or retired), total income in thousands of dollars (logarithmic scale), and health insurance coverage from any source (yes or no). Psychosocial factors included living arrangement (lives alone or not), number of children (no children or ≥ 1 child), and the number of depressive symptoms measured by the 8-item abbreviated Center for Epidemiologic Studies Depression Scale (CES-D; range=0-8). Behavioral factors included current smoking status (yes or no), alcohol use (0, 1-2, or ≥3 drinks per day), and vigorous physical exercise (<3 or ≥3 times per week). Physiological status was also included as body mass index (calculated as weight in kilograms divided by height in meters squared; <18.5 [underweight], 18.5-24.9 [normal weight], 25.0-29.9 [overweight], or ≥30.0 [obese]), hypertension (yes or no), and diabetes mellitus (yes or no). An indicator for whether respondents had ever been widowed (yes or no) also was included.
The covariate data were obtained from baseline and follow-up interviews (every 24 months) and the coding of study measures was facilitated by using HRS data files provided by RAND's Center for the Study of Aging—funded by NIA and the Social Security Administration.34 Missing data was minimal across study variables for follow-up measurements (∼ 2-3%) and preliminary analyses showed that the results were unchanged using multivariable and mean imputation methods. Preliminary analyses also included variables for age at first marriage and spouses from the same HRS household; however, these variables were dropped from the final models because of multicollinearity with other covariates (namely marital variables). Alternative coding strategies were also assessed for the continuous variables (e.g., logged, polynomial, and grouped-ordinal scales) and categorical variables (e.g., different cutpoints, categories, and reference groups) included in the models and did not alter the central findings.
With the exception of baseline age, sex, race, and ethnicity, all measures were time varying and time lagged (observed in the previous wave [i.e., within the prior 24 months]) in the prospective analyses to establish temporal order when estimating the associations between the covariates and subsequent AMI.35,36 Alternative lag times (e.g., no lag, 12-months, 48-months, etc.) also were assessed and produced largely consistent results.
Outcome
The age-specific incidence of AMI was the main outcome for analysis. At each survey interview, study participants were asked whether they had “a heart attack or myocardial infarction” and in what year (and month after 1994) it occurred. Age of the event was calculated from the respondents' dates of birth and the event. Although subjects' reports of AMI are less precise than clinical data, studies have shown general consistency between diagnostic reports of AMI from survey respondents and those from medical evaluations.37-40 The AMI outcome is analyzed as the time-to-event when either an AMI occurred or when the observation period ended for the cohort (i.e., censored). Four hundred sixty two subjects (2.9%) died during the study and were censored at their age of death. Of the 1211 AMIs, 29 (2.4%) were reported at ages that were difficult to distinguish temporally from the time of divorce. However, by design, the time-varying measures of marital status and divorce were time lagged to ignore divorces that were reported concurrently with AMI for these 29 subjects.35,36
Statistical Analysis
Baseline characteristics of the HRS sample were computed for all participants and for men and women. Comparisons by sex were calculated with t tests for continuous and count variables and χ2 tests for categorical variables. P values were based on 2-tailed tests and considered statistically significant at P <.05. Although only a small number of deaths occurred during the study period, competing-risk hazard models were estimated to account for potential bias due to selective mortality.41 This method was also effective for using the rich time-varying data and for taking into account the temporal order of exposure to divorce and AMI events.36,41 Results from Cox proportional hazard models were nearly identical to those presented here, with only negligible changes in the point estimates and CIs (± .01-.001). Age-adjusted cumulative incidence rates were plotted to describe differences in age-specific rates of AMI for men and women by marital status and cumulative number of divorces. Multivariable competing-risk models were then used to estimate the adjusted hazard ratios (HRs) and 95% confidence intervals of AMI associated with marital status and the cumulative number of divorces. The number of tied events relative to the number at risk was low (<1%), and partial likelihood estimation was nearly identical using Breslow (reported herein) and Efron approximations in preliminary analyses.
The first set of multivariable models examined AMI risks associated with marital status and the cumulative number of divorces by sex and adjusted for age, study cohort, race/ethnicity, and geographic region. The second set of multivariable analyses included additional sets of covariates to examine the potential factors contributing to AMI risks in men and women. Model 1 adjusted for sociodemographic background and physiological status. Subsequent models included Model 1 adjustments with additional covariates for socioeconomic factors (Model 2), psychosocial factors (Model 3), behavioral factors (Model 4), and all covariates (Model 5). Akaike information criteria (AIC) values were used to compare log-likelihood functions to assess model fit across the non-nested models.42 Analyses were conducted separately for men and women to account for sex differences in AMI risks, divorce/remarriage patterns, and the mechanisms thought to account for the cardiovascular risks associated with divorce in women and men.1,3,14 Interaction terms were estimated to assess whether the associations were significantly different for men and women. All models were weighted for the complex sampling design to produce unbiased variance estimates and results that are generalizable to U.S. older adults who ever married.
Three sets of sensitivity analyses were also conducted. First, although the analyses adjusted for a large number and range of confounding factors, it is possible that additional unmeasured confounding (i.e. residual confounding) may have accounted for the findings.36 Results from gamma-distributed frailty models demonstrated that the findings and overall conclusions remained the same when accounting for potential bias from unobserved measures. Second, measures for marital status and number of divorces were estimated separately because preliminary analyses indicated a high degree of bivariate correlation and multicollinearity in the models—condition values were > 60, with the largest variance decomposition proportions and variance inflation factors among the marital variables. Finally, tests of interactions with analysis time and tests of Schoenfeld residuals using robust variance-covariance matrix estimation indicated that the proportional hazards assumption was not violated. All analyses were conducted using Stata 12.0 (StataCorp, College Station, TX).
Results
Baseline characteristics of the study participants are presented in Table 1. Women in the study were younger on average and more likely to be non-Hispanic black than men. Women were also less likely to be employed, have health insurance, had lower levels of education and income, exercised less, lived alone, and had more depressive symptoms than men. Rates of smoking, excess alcohol consumption, unhealthy BMI, diagnoses of hypertension or diabetes mellitus, and the occurrence of AMI were significantly higher in men than women. Men were more likely to have worked in professional or managerial positions and less likely to have children than women. Men were also more likely to be continuously married or remarried at baseline; whereas women were more likely to be divorced or widowed. The cumulative number of divorces was not significantly different for men and women (P=.212) at baseline. Men and women with multiple divorces were significantly more likely to be low educated, uninsured, and in lower-level occupations; and have higher rates of depressive symptoms, smoking, excessive drinking, and diagnosed hypertension than those who were continuously married (results not shown). For the total 200,531 person-years of observation, 106,303 were spent married, 30,273 were divorced, 18,697 were widowed, and 45,258 were remarried.
Table 1. Characteristics of Study Participants from the Health and Retirement Study (HRS) at Baseline.
| Total (n = 15827) |
Men (n = 7264) |
Women (n = 8563) |
P Value |
|
|---|---|---|---|---|
| Sociodemographic Background | ||||
| Age, mean (SD), y | 54.3 (4.08) | 55.1 (3.96) | 53.5 (4.04) | <.001 |
| Study cohort, 1942-1947 | 2242 (14.2) | 1087 (15.0) | 1155 (13.5) | .008 |
| Study cohort, 1948-1953 | 2881 (18.2) | 1348 (18.6) | 1533 (17.9) | .288 |
| Hispanic | 1541 (9.74) | 693 (9.54) | 848 (9.90) | .443 |
| Non-Hispanic Black | 2424 (15.3) | 1005 (13.8) | 1419 (16.6) | <.001 |
| Non-Hispanic other race | 397 (2.51) | 183 (2.52) | 214 (2.50) | .936 |
| Lives in the South | 6406 (40.5) | 2918 (40.2) | 3488 (40.7) | .472 |
| Marital Status | ||||
| Continuously married | 8908 (56.3) | 4278 (58.9) | 4630 (54.1) | <.001 |
| Remarried | 3624 (22.9) | 1903 (26.2) | 1721 (20.1) | |
| Divorced | 2571 (16.2) | 989 (13.6) | 1582 (18.5) | |
| Widowed | 724 (4.57) | 94 (1.29) | 630 (7.36) | |
| Cumulative Number of Divorces | ||||
| 0 Divorces | 10331 (65.3) | 4718 (65.0) | 5613 (65.6) | .212 |
| 1 Divorces | 4181 (26.4) | 1912 (26.3) | 2269 (26.5) | |
| ≥ 2 Divorces | 1315 (8.31) | 634 (8.73) | 681 (7.95) | |
| Socioeconomic Factors | ||||
| Years of education, mean (SD) | 12.5 (3.12) | 12.6 (3.31) | 12.4 (2.95) | <.001 |
| Lifetime occupation, professional or managerial | 4339 (27.4) | 2165 (29.8) | 2174 (25.4) | <.001 |
| Not employed | 4462 (28.2) | 1523 (21.0) | 2939 (34.3) | <.001 |
| Total income in thousands of dollars, mean (SD) | 24.6 (41.8) | 34.6 (55.2) | 16.2 (22.0) | <.001 |
| No health insurance | 2512 (15.9) | 1039 (14.3) | 1473 (17.2) | <.001 |
| Psychosocial Factors | ||||
| Lives alone | 1411 (8.92) | 540 (7.43) | 871 (10.2) | <.001 |
| No children | 821 (5.19) | 448 (6.17) | 373 (4.36) | <.001 |
| CES-D depressive symptoms, mean (SD) | 1.89 (1.99) | 1.60 (1.84) | 2.13 (2.07) | <.001 |
| Behavioral Factors | ||||
| Current smoker | 4066 (25.7) | 2015 (27.7) | 2051 (24.0) | <.001 |
| No alcohol consumption | 5939 (37.5) | 2174 (30.0) | 3765 (44.0) | <.001 |
| Excess alcohol consumption | 1959 (12.4) | 963 (13.3) | 996 (11.6) | .002 |
| No vigorous exercise | 11697 (73.9) | 5249 (72.3) | 6448 (75.3) | <.001 |
| Physiological Status | ||||
| Underweight, BMI < 18.5 | 199 (1.26) | 35 (0.48) | 164 (1.91) | <.001 |
| Normal weight, BMI 18.5-24.9 | 5113 (32.3) | 1918 (26.4) | 3195 (37.3) | |
| Overweight, BMI 25.0-29.9 | 6493 (41.0) | 3591 (49.4) | 2902 (33.9) | |
| Obese, BMI ≥ 30.0 | 2720 (17.2) | 1279 (17.6) | 1441 (16.8) | |
| Hypertension | 5062 (32.0) | 2419 (33.3) | 2643 (30.9) | <.001 |
| Diabetes | 1444 (9.12) | 708 (9.75) | 736 (8.60) | .012 |
| AMI during study period | 1211 (7.65) | 762 (10.5) | 449 (5.24) | <.001 |
Abbreviations: SD, standard deviation; CES-D, Center for Epidemiologic Studies Depression scale; AMI, acute myocardial infarction; BMI, body mass index.
P values calculated by analysis of variance or x2 tests.
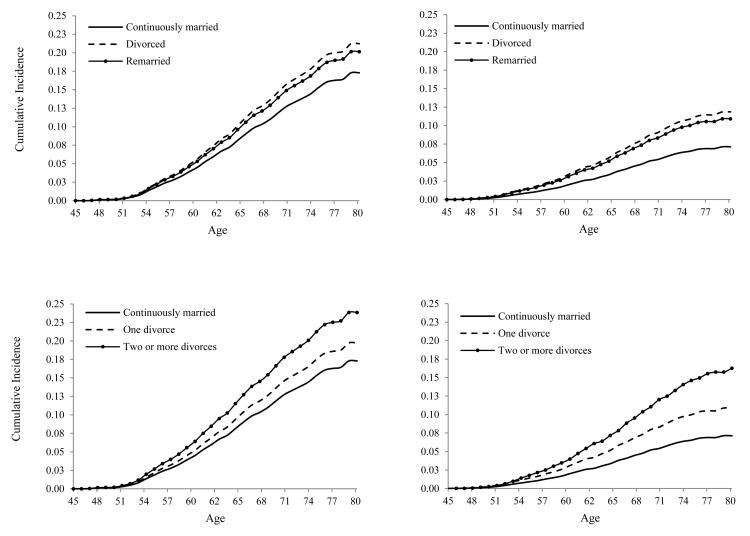
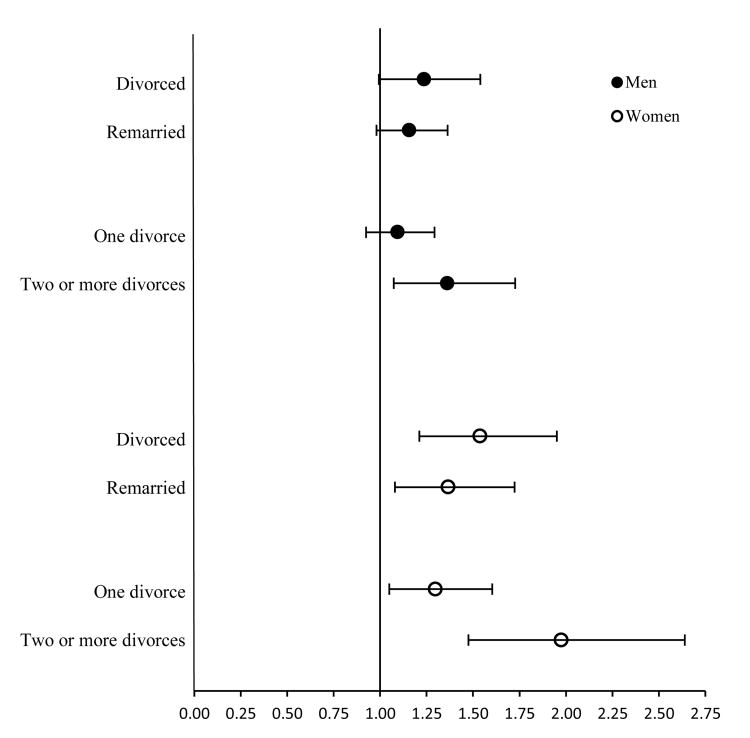
Cumulative incidence plots shown in Figure 1 demonstrate significant differences in age-specific rates of AMI between those with a history of divorce and those continuously married for men and women (with the exception of men with one previous divorce). Figure 2 illustrates the sociodemographically-adjusted HRs for marital status and the cumulative number of divorces related to AMI. Results showed that divorced men and women had significantly higher risks of AMI than their continuously married counterparts. Remarried women also had increased risks for AMI compared with continuously married women. One lifetime divorce was significantly associated with AMI in women but not in men and a history of two or more divorces was significantly associated with incident AMI in both sexes after accounting for differences in age, study cohort, race, ethnicity, and geographic region.
Figure 1.
Age-Adjusted Cumulative Incidence of Acute Myocardial Infarction (AMI) by Marital Status and Cumulative Number of Divorces in U.S. Men and Women
Note: Marital groups are significantly different from continuously married (reference) at P < .05 with the exception of men with one divorce (*).
Figure 2.
Adjusted Hazard Ratios for Acute Myocardial Infarction (AMI) by Marital Status and Cumulative Number of Divorces in U.S. Men and Women
Error bars indicate 95% confidence intervals.
Models were adjusted for age, study cohort, race, ethnicity, geographic region, ever widowed; and were estimated separately for marital status and number of divorces in men and women.
Table 2 reports the covariate-adjusted HRs for the marital variables in men and women controlling for sociodemographic background and physiological status. Results for Model 1 showed that AMI risks were significantly higher in women who were divorced (HR, 1.52; 95% CI, 1.20-1.93), remarried (HR, 1.39; 95% CI, 1.10-1.76), and among women with a history of one and/or multiple divorces (HR, 1.29; 95% CI, 1.05-1.60 and HR, 2.04; 95% CI, 1.53-2.73, respectively) relative to continuously-married women. The relative risks for AMI were significantly higher only in men who were currently divorced (HR, 1.26; 95% CI, 1.01-1.58) or had multiple divorces (HR, 1.38; 95% CI, 1.09-1.76). Models 2, 3, and 4 showed that additional adjustments for socioeconomic, psychosocial, and behavioral factors only partially reduced the associations between divorce and AMI. For men, we found that socioeconomic factors (namely employment status and occupational status) in Model 2 were attributable to the largest reduction in risks related to divorce. Estimated AIC values indicated that each category of covariates had comparable levels of explanatory power. For women, we found that psychosocial factors (namely depressive symptoms) in Model 3 had the largest reduction in risks related to divorce—which were also reflected in the AIC values. The fully adjusted results (Model 5) showed that risks for AMI remained elevated in men (HR, 1.30; 95% CI, 1.02-1.66) and women (HR, 1.77; 95% CI, 1.30-2.41) with two or more lifetime divorces compared with continuously married men and women. Risks for AMI were also significantly higher in women who were currently divorced (HR, 1.36; 95% CI, 1.04-1.78) and remarried (HR, 1.35; 95% CI, 1.07-1.70) compared with women who were stably married. Men who were divorced and remarried had no significant risk for AMI.
Table 2. Adjusted Hazard Ratios (95% CI) for Acute Myocardial Infarction Associated with Marital Status and Number of Divorces in U.S. Older Men and Women.
| Hazard Ratio (95% CI) | |||||
|---|---|---|---|---|---|
|
| |||||
| Model 1 | Model 2 | Model 3 | Model 4 | Model 5 | |
| Men† | |||||
| Marital Status | |||||
| Continuously married | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| Divorced | 1.26 (1.01-1.58) | 1.19 (0.95-1.48) | 1.32 (1.02-1.71) | 1.23 (0.99-1.54) | 1.27 (0.98-1.65) |
| Remarried | 1.17 (0.99-1.38) | 1.16 (0.98-1.36) | 1.15 (0.97-1.35) | 1.17 (0.99-1.38) | 1.13 (0.96-1.34) |
| AIC value | 12643.41 | 12610.44 | 12604.36 | 12604.4 | 12564.01 |
| Number of Divorces | |||||
| Continuously married | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| 1 Divorce | 1.12 (0.95-1.33) | 1.09 (0.92-1.30) | 1.11 (0.94-1.32) | 1.11 (0.94-1.31) | 1.10 (0.92-1.30) |
| ≥ 2 Divorces | 1.38 (1.09-1.76) | 1.32 (1.04-1.68) | 1.35 (1.06-1.73) | 1.33 (1.05-1.68) | 1.30 (1.02-1.66) |
| AIC value | 12642.21 | 12609.29 | 12604.17 | 12604.00 | 12564.06 |
| Women† | |||||
| Marital Status | |||||
| Continuously married | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| Divorced | 1.52 (1.20-1.93) | 1.56 (1.22-1.98) | 1.41 (1.09-1.83) | 1.43 (1.12-1.82) | 1.36 (1.04-1.78) |
| Remarried | 1.39 (1.10-1.76) | 1.37 (1.09-1.73) | 1.35 (1.07-1.70) | 1.39 (1.10-1.76) | 1.35 (1.07-1.70) |
| AIC value | 7524.98 | 7495.08 | 7430.61 | 7473.97 | 7397.71 |
| Number of Divorces | |||||
| Continuously married | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| 1 Divorce | 1.29 (1.05-1.60) | 1.33 (1.07-1.64) | 1.26 (1.01-1.56) | 1.25 (1.01-1.55) | 1.24 (1.00-1.55) |
| ≥ 2 Divorces | 2.04 (1.53-2.73) | 2.03 (1.51-2.72) | 1.84 (1.36-2.49) | 1.91 (1.42-2.56) | 1.77 (1.30-2.41) |
| AIC value | 7517.97 | 7488.31 | 7425.75 | 7468.60 | 7393.51 |
Abbreviations: HR, hazard ratio; CI, confidence interval; AIC, Akaike information criterion.
Model 1 adjusted for age, study cohort, race, ethnicity, geographic region, ever widowed, BMI, hypertension, and diabetes.
Model 2 includes Model 1 + education, employment, income, and health insurance.
Model 3 includes Model 1 + lives alone, no children, and CES-D depressive symptoms.
Model 4 includes Model 1 + smoking status, alcohol use, and physical exercise.
Model 5 includes Model 1 + all covariates.
Models for marital status and number of divorces were estimated separately for men and women.
Overall, the relative risks associated with multiple divorces in women were comparable to other major risk factors in the estimated models, such as smoking (HR, 1.53; 95%CI, 1.21-1.93), hypertension (HR, 1.73; 95% CI, 1.38-2.17), and diabetes mellitus (HR, 1.81; 1.44-2.28). Although the magnitudes of the HRs for divorce history were larger among women than men, the interaction terms for sex were not statistically significant. However, results showed that depressive symptoms had a significantly greater effect among women than among men (P=.008) and that occupational status had a significantly greater effect among men than among women (P=.013).
Discussion
Our study is the first to examine the association between lifetime exposure to divorce and risks for AMI in a contemporary cohort of U.S. older adults. Results demonstrated that cumulative exposure to divorce increased risks of AMI in men and women and that the associations were not accounted for by socioeconomic, psychosocial, behavioral, or physiological factors. Women with multiple divorces were at especially high risk of AMI. We also found that remarried women had risks that were similar in magnitude to divorced women; whereas men who remarried had no significant risk for AMI.
Previous studies have documented cross-sectional associations between marital status and multiple health outcomes.17,19,20 The current study is the first to demonstrate the longitudinal association between divorce and AMI and extends our understanding of lifetime exposure to social stressors and cardiovascular risks. The results of this study contribute to mounting evidence that AMI risks associated with social stressors are of the relative magnitude of established risk factors such as smoking, diabetes, and hypertension.43 In women, for example, we found that the multivariable-adjusted risks associated with hypertension (HR=1.73) and diabetes (HR=1.81) were comparable to the risks observed in women with a history of two or more divorces (HR=1.77). The risks attributable to divorce are also analogous to the association recently documented between lifetime exposure to job loss(es) and AMI.43 Our findings for divorce largely mirror these protracted and cumulative associations in acquired risk related to unemployment.
Two additional findings are notable. First, this study showed that remarried women had risks for AMI that were nearly equivalent in magnitude to divorced women (HRs=1.35 vs. 1.36, respectively) relative to continuously married women. This pattern has been observed in related research. For example, studies have shown that remarried women have greater levels of physical and psychological illness than women who were continuously married; whereas remarried men did not differ in health outcomes relative to continuously married men.26,27 Therefore, our findings corroborate existing evidence to suggest that remarriage after divorce may not confer the same health benefits for women as for men. Second, we examined whether the association between divorce and AMI has strengthened or weakened over time as the prevalence of and attitudes toward divorce have changed in American society. Supplementary analyses of interactions between successive birth cohorts and the marital covariates indicated that there were no significant changes in the associations during this study period.
An important area for future research will be to investigate the mechanisms underlying these findings and to identify possible interventions to reduce these risks. The prevailing argument is that divorce has a negative impact on the economic, behavioral, and emotional well-being of individuals that reduces their ability to prevent, detect, and treat illness.13,15,28-30,44 Contrary to expectations and existing literature, we found that losses of income and health insurance,26,29 and increases in depressive symptoms, alcohol use, and smoking,21,28,30 did not account for the excess risks attributable to a history of divorce in men and women. We suspect that the acute and chronic stress associated with divorce may have played an important role in our findings for both sexes.45,46 Indeed, studies have recently identified possible biological mechanisms (e.g., blood pressure reactivity, elevated cortisol, and hemoglobin A1c) related to the stress of divorce that warrant additional investigation as they relate to increased risk for AMI.17,47,48 Relatedly, we also suspect that a history of divorce may have had negative consequences for medication adherence, healthcare utilization, and disease management that may have precipitated or worsened vascular pathology.15,18,49,50 Accordingly, studies have shown that spouses (particularly wives) encourage concordant health behaviors—such as proper diet, exercise, and medication compliance—that promote cardiovascular health.30-32 Therefore, we encourage future studies to explore these mechanisms to help explain how repeated exposure to divorce incurs increasing risks for AMI.
Major strengths of this study included panel data from a large, representative sample of middle-aged and older U.S. adults, the use of retrospective histories and prospective data spanning almost 20 years, and multivariable competing-risk hazard models that utilized time-varying covariates to estimate incidence of AMI. The HRS provides the only known source of data that includes measures of AMI along with rich time-varying measures of marital life and numerous socioeconomic, psychosocial, behavioral, and physiological covariates. Our study demonstrated significant associations between divorce history and AMI after adjusting for the confounding effects of numerous cardiovascular risk factors. The time-varying covariates also captured changes in many of the socioeconomic, psychosocial, and behavioral factors thought to account for the elevated risks following a divorce.
Despite the strengths of this study, we acknowledge several limitations. Although the data were rich in the number and scope of measured covariates, we lacked certain clinical parameters. First, we acknowledge that the analyses of AMI are based on self-reported data and not medical evaluations. However, studies generally have shown consistency between diagnostic reports of AMI from survey respondents and those from medical evaluations—with self-reported AMI having a high degree of sensitivity (90-98%), specificity (98-99%), and overall agreement (94-98%) with medical data.37-40 Nevertheless, we acknowledge that self-reported AMI is less accurate than medical reports and future studies are warranted to validate these findings with medical assessments. Another limitation is the possibility that additional unmeasured factors may have contributed to the associations. For example, data were not available for the treatment and control of hypertension, diabetes, and hyperlipidemia prior to AMI; or other prophylactic measures to reduce the likelihood of infarction (e.g., prior revascularization). We also could not identify the characteristics or quality of past marriages or the circumstances of divorce. Although detailed measures of past marital relationships were not available, the multivariable analyses showed that depressive symptoms and maladaptive behaviors did not account for the findings. Relatedly, we lacked direct measures of stress, anxiety, and the loss of social support that may have contributed to the association between divorce and subsequent AMI.
The results from this study provide new and actionable knowledge that have the potential to assist in clinical decision-making and improve quality of care. Although marital events are not amenable to medical intervention, knowledge about the risks associated with divorce will be useful for personalizing care and preventing new or recurrent AMI. For example, we found that divorced women—particularly those who experienced multiple divorces—may benefit from additional screening and/or treatment for depression or other symptoms of distress. Likewise, men who have been divorced more than once—particularly men in lower-level occupations—may benefit from consultation for smoking, alcohol use, or other maladaptive behaviors that accompany the stress of marital loss. New insights such as these will help providers identify and treat adults at potentially high risk of AMI, as well as provide patients a new (or heightened) awareness of their social risks that go beyond the cautionary litany of poor diet, inactivity, and smoking.
In sum, results from our large prospective cohort study demonstrated an association between one's lifetime exposure to divorce and risks for a major cardiovascular event. The relative risks attributable to divorce were comparable in magnitude to other traditional risk factors and accumulated with increasing exposure to divorce, particularly in women. Future studies are needed to further examine the mechanisms contributing to these associations and to assess how such information can be used to target and aggressively treat vulnerable segments of the population.
Supplementary Material
Acknowledgments
Sources of Funding: Support for this study was provided by the National Institute on Aging (NIA) grant R03AG042712.
The funding source (NIA) had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication. The views expressed in this article are those of the authors and do not necessarily reflect those of Duke University.
Footnotes
Disclosures: No conflicts of interests are declared.
References
- 1.Lloyd-Jones DM, Larson MG, Beiser A, Levy D. Lifetime risk of developing coronary heart disease. Lancet. 1999;353:89–92. doi: 10.1016/S0140-6736(98)10279-9. [DOI] [PubMed] [Google Scholar]
- 2.Xu J, Kochanek KD, Murphy S, Tejada-Vera B. Deaths: Final Data for 2007. Vol. 58. Hyattsville, Md: National Center for Health Statistics; 2010. National Vital Statistics Reports. [PubMed] [Google Scholar]
- 3.Roger VL, Go AS, Lloyd-Jones DM, Adams RJ, Berry JD, Brown TM, Carnethon MR, Dai S, de Simone G, Ford ES, Fox CS, Fullerton HJ, Gillespie C, Greenlund KJ, Hailpern SM, Heit JA, Ho PM, Howard VJ, Kissela BM, Kittner SJ, Lackland DT, Lichtman JH, Lisabeth LD, Makuc DM, Marcus GM, Marelli A, Matchar DB, McDermott MM, Meigs JB, Moy CS, Mozaffarian D, Mussolino ME, Nichol G, Paynter NP, Rosamond WD, Sorlie PD, Stafford RS, Turan TN, Turner MB, Wong ND, Wylie-Rosett J American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Heart disease and stroke statistics—2011 update: a report from the American Heart Association. Circulation. 2011;123:e18–e209. doi: 10.1161/CIR.0b013e3182009701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Centers for Disease Control and Prevention. National Center for Health Statistics. Health Data Interactive. [Accessed November 1, 2011]; http://www.cdc.gov/nchs/hdi.htm.
- 5.Torio CM, Andrews RM. National Inpatient Hospital Costs: The Most Expensive Conditions by Payer, 2011. Vol. 1. Agency for Healthcare Research and Quality; Rockville, MD: 2013. HCUP Statistical Brief #160. [PubMed] [Google Scholar]
- 6.Yusuf S, Hawken S, Ounpuu S, Dans T, Avezum A, Lanas F, McQueen M, Budaj A, Pais P, Varigos J, Lisheng L, for the INTERHEART Study Investigators Effect of potentially modifiable risk factors associated with myocardial infarction in 52 countries (the INTERHEART study): case-control study. Lancet. 2004;364:937–952. doi: 10.1016/S0140-6736(04)17018-9. [DOI] [PubMed] [Google Scholar]
- 7.Greenland P, Knoll MD, Stamler J, Neaton JD, Dyer AR, Garside DB, Wilson PW. Major risk factors as antecedents of fatal and nonfatal coronary heart disease events. JAMA. 2003;290:891–897. doi: 10.1001/jama.290.7.891. [DOI] [PubMed] [Google Scholar]
- 8.Maruthur NM, Wang NY, Appel LJ. Lifestyle interventions reduce coronary heart disease risk: results from the PREMIER Trial. Circulation. 2009;119:2026–2031. doi: 10.1161/CIRCULATIONAHA.108.809491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Zhao G, Ford ES, Li C, Mokdad AH. Are United States adults with coronary heart disease meeting physical activity recommendations? Am J Cardiol. 2008;101:557–561. doi: 10.1016/j.amjcard.2007.10.015. [DOI] [PubMed] [Google Scholar]
- 10.Kreider RM, Ellis R. Current Population Reports. U.S. Census Bureau; Washington, DC: 2011. Number, timing, and duration of marriages and divorces: 2009; pp. P70–125. [Google Scholar]
- 11.Jenkins CD. Psychologic and social precursors of coronary disease. New Engl J Med. 1971;284:244–55. doi: 10.1056/NEJM197102042840506. [DOI] [PubMed] [Google Scholar]
- 12.Venters M, Jacobs DR, Pirie P, Luepker RV, Folsom AR, Gillum RF. Marital-status and cardiovascular risk:The minnesota-heart-survey and the minnesota-heart-health-program. Prev Med. 1986;15:591–605. doi: 10.1016/0091-7435(86)90064-2. [DOI] [PubMed] [Google Scholar]
- 13.O'Rand A, Hamil-Luker J. Processes of cumulative adversity: childhood disadvantage and increased risk of heart attack across the life course. J Gerontol B-Psychol. 2005;60:117–24. doi: 10.1093/geronb/60.special_issue_2.s117. [DOI] [PubMed] [Google Scholar]
- 14.Gerward SP, Tydén G, Engström B, Hedblad Marital status and occupation in relation to short-term case fatality after a first coronary event - a population based cohort. BMC Public Health. 2010;10:235. doi: 10.1186/1471-2458-10-235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Koskenvuo M, Kaprio J, Romo M, Langinvainio H. Incidence and prognosis of ischemic-heart-disease with respect to marital-status and social-class - a national record linkage study. J Epidemiol Commun H. 1981;35:192–196. doi: 10.1136/jech.35.3.192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Zhang ZM, Hayward MD. Gender, the marital life course, and cardiovascular disease in late midlife. J Marriage Fam. 2006;68:639–657. [Google Scholar]
- 17.Molloy GJ, Stamatakis E, Randall G, Hamer M. Marital status, gender and cardiovascular mortality: Behavioural, psychological distress and metabolic explanations. Soc Sci Med. 2009;69:223–28. doi: 10.1016/j.socscimed.2009.05.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Reviere R, Eberstein IW. Work, marital status, and heart disease. Health Care Women Int. 1992;13:393–399. doi: 10.1080/07399339209516016. [DOI] [PubMed] [Google Scholar]
- 19.Lindegard B, Langman MJS. Marital state, alcohol-consumption, and liability to myocardial-infarction, stroke, diabetes-mellitus, or hypertension in men from gothenburg. BMJ. 1985;291:1529–1533. doi: 10.1136/bmj.291.6508.1529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Blom M, Georgiades A, László KD, Alinaghizadeh H, Janszky I, Ahnve S. Work and marital status in relation to depressive symptoms and social support among women with coronary artery disease. J WomensHealth. 2007;16:1305–1316. doi: 10.1089/jwh.2006.0191. [DOI] [PubMed] [Google Scholar]
- 21.Dupre ME, Beck AN, Meadows SO. Marital trajectories and mortality among U.S. adults. Am J Epidemiol. 2009;170:546–555. doi: 10.1093/aje/kwp194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.George LK. Sociological perspectives on life transitions. Annu Rev Sociol. 1993;19:353–375. [Google Scholar]
- 23.Zhang ZM. Marital history and the burden of cardiovascular disease in midlife. Gerontologist. 2006;46:266–270. doi: 10.1093/geront/46.2.266. [DOI] [PubMed] [Google Scholar]
- 24.Towfighi A, Zheng L, Ovbiagele B. Sex-specific trends in midlife coronary heart disease risk and prevalence. Arch Intern Med. 2009;169:1762–1766. doi: 10.1001/archinternmed.2009.318. [DOI] [PubMed] [Google Scholar]
- 25.Pew Research Center. [Accessed November 14, 2014]; http://www.pewsocialtrends.org/2014/11/14/four-in-ten-couples-are-saying-i-do-again/
- 26.Hughes ME, Waite LJ. Marital biography and health at mid-life. J Health Soc Behav. 2009;50:344–358. doi: 10.1177/002214650905000307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Barrett AE. Marital trajectories and mental health. J Health Soc Behav. 2000;41:451–464. [PubMed] [Google Scholar]
- 28.LaPierre TA. The enduring effects of marital status on subsequent depressive symptoms among women: Investigating the roles of psychological, social, and financial resources. J Epidemiol Comm Health. 2012;66:1056–1062. doi: 10.1136/jech-2011-200383. [DOI] [PubMed] [Google Scholar]
- 29.Smock PJ, Manning WD, Gupta S. The effect of marriage and divorce on women's economic well-being. Am Sociol Rev. 1999;64:794–812. [Google Scholar]
- 30.Umberson D. Gender, marital status and the social control of health behavior. Soc Sci Med. 1992;34:907–917. doi: 10.1016/0277-9536(92)90259-s. [DOI] [PubMed] [Google Scholar]
- 31.DiCastelnuovo A, Quacquaruccio G, Donati MB, Gaetano G, Iacoviello L. Spousal concordance for major coronary risk factors: a systematic review and meta-analysis. Am J Epidemiol. 2009;169:1–8. doi: 10.1093/aje/kwn234. [DOI] [PubMed] [Google Scholar]
- 32.Meyler D, Stimpson JP, Peek K. Health concordance within couples: a systematic review. Soc Sci Med. 2007;64:2297–2310. doi: 10.1016/j.socscimed.2007.02.007. [DOI] [PubMed] [Google Scholar]
- 33.Health and Retirement Study (HRS): A Longitudinal Study of Health, Retirement, and Aging. Sponsored by the National Institute on Aging. [Accessed August 18, 2010]; http://hrsonline.isr.umich.edu.
- 34.Produced by the RAND Center for the Study of Aging, with funding from the National Institute on Aging and the Social Security Administration. Santa Monica, CA: [Accessed December 14, 2010]. RAND HRS Data, Version L. http://hrsonline.isr.umich.edu/index.php?p=shoavail&iyear=X7. [Google Scholar]
- 35.Fisher LD, Lin DY. Time-dependent covariates in the Cox proportional-hazards regression model. Annu Rev Public Health. 1999;20:145–157. doi: 10.1146/annurev.publhealth.20.1.145. [DOI] [PubMed] [Google Scholar]
- 36.Allison PD. Survival Analysis Using the SAS System: A Practical Guide. Cary, NC: SAS Institute; 1995. [Google Scholar]
- 37.Okura Y, Urban LH, Mahoney DW, Jacobsen SJ, Rodeheffer RJ. Agreement between self-report questionnaires and medical record data was substantial for diabetes, hypertension, myocardial infarction and stroke but not heart failure. J Clin Epidemiol. 2004;57:1096–1103. doi: 10.1016/j.jclinepi.2004.04.005. [DOI] [PubMed] [Google Scholar]
- 38.Tretli S, Lund-Larsen PG, Foss OP. Reliability of questionnaire information on cardiovascular disease and diabetes: cardiovascular disease study in Finnmark county. J Epidemiol Community Health. 1982;36:269–73. doi: 10.1136/jech.36.4.269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Machon M, Arriola L, Larranaga N, Amiano P, Moreno-Iribas C, Agudo A, Ardanaz E, Barricarte A, Buckland G, Chirlaque MD, Gavrila D, Huerta JM, Martínez C, Molina E, Navarro C, Quiros JR, Rodríguez L, Sanchez MJ, González CA, Dorronsoro M. Validity of self-reported prevalent cases of stroke and acute myocardial infarction in the Spanish cohort of the EPIC study. J Epidemiol Community Health. 2013;67:71–75. doi: 10.1136/jech-2011-200104. [DOI] [PubMed] [Google Scholar]
- 40.Harlow SD, Linet MS. Agreement between questionnaire data and medical records: The evidence for accuracy of recall. Am J Epidemiol. 1989;129:233–248. doi: 10.1093/oxfordjournals.aje.a115129. [DOI] [PubMed] [Google Scholar]
- 41.Fine JP, Gray RJ. A proportional hazards model for the subdistribution of a competing risk. J Am Stat Assoc. 1999;94:496–509. [Google Scholar]
- 42.Akaike H. A new look at the statistical model identification. IEEE Transactions on Automatic Control. 1974;19:716–723. [Google Scholar]
- 43.Dupre ME, George LK, Liu G, Peterson ED. The cumulative impact of unemployment on risks of acute myocardial infarction. Arch Int Med. 2012;172:1731–1737. doi: 10.1001/2013.jamainternmed.447. [DOI] [PubMed] [Google Scholar]
- 44.Lavelle B, Smock PJ. Divorce and women's risk of health insurance loss. J Health Soc Behav. 2012;53:413–431. doi: 10.1177/0022146512465758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Steptoe A, Kivimäki M. Stress and cardiovascular disease. Nat Rev Cardiol. 2012;9:360–70. doi: 10.1038/nrcardio.2012.45. [DOI] [PubMed] [Google Scholar]
- 46.Orth-Gomer K, Wamala SP, Horsten M, Schenck-Gustafsson K, Schneiderman N, Mittleman MA. Marital stress worsens prognosis in women with coronary heart disease - The Stockholm Female Coronary Risk Study. JAMA. 2000;284:3008–3014. doi: 10.1001/jama.284.23.3008. [DOI] [PubMed] [Google Scholar]
- 47.Sbarra DA, Law RW, Lee LA, Mason AE. Marital dissolution and blood pressure reactivity: Evidence for the specificity of emotional intrusion-hyperarousal and task-rated emotional difficulty. Psychosom Med. 2009;71:532–540. doi: 10.1097/PSY.0b013e3181a23eee. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Tobe SW, Kiss A, Sainsbury S, Lesin M, Geerts R, Baker B. The impact of job strain and marital cohesion on ambulatory blood pressure during 1 year: The double exposure study. Am J Hypertens. 2007;20:148–153. doi: 10.1016/j.amjhyper.2006.07.011. [DOI] [PubMed] [Google Scholar]
- 49.Wu J, Lennie TA, Chung ML, Frazier SK, Dekker RD, Biddle MJ, Moser DK. Medication adherence mediates the relationship between marital status and event-free survival in patients with heart failure. Circulation. 2009;120:S516. doi: 10.1016/j.hrtlng.2011.09.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Molloy GJ, Hamer M, Randall G, Chida Y. Marital status and cardiac rehabilitation attendance: a meta-analysis. Eur J Cardio Prev Rehab. 2008;15:557–561. doi: 10.1097/HJR.0b013e3283063929. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.