Abstract
Background and Objectives
There is large cross-sectional variation in fall rates among hospital units with similar patient populations. It is not known whether the differences underlying this variability are consistent across time. The twofold purpose of this study was to determine the proportion of variation in long-term fall rates attributable to between-unit, rather than within-unit, variability; and to identify unit- and hospital-level characteristics associated with persistently low- and high-fall units.
Design, Setting, and Participants
We extracted 24 consecutive months of data on inpatient falls and unit characteristics for non-subspecialty medical units (n=800) in U.S. general hospitals from the National Database of Nursing Quality Indicators®. We identified 80 low-fall and 74 high-fall units based on monthly rankings of fall rates and compared these 2 groups on unit- and hospital-level characteristics.
Measurements
Monthly self-reported unit fall rates (falls per 1,000 patient days).
Results
An estimated 87% of variation in 24-month fall rates was due to between-unit differences. With the exception of patient days, a proxy for unit bed size, low- and high-fall units did not differ on nurse staffing or any other unit or hospital characteristic variable.
Conclusion
There are medical units with persistently low and persistently high fall rates. High-fall units had higher patient volume, suggesting patient turnover as a variable for further study. Understanding additional factors underlying variability in long-term fall rates could lead to sustainable interventions for reducing inpatient falls.
Keywords: Patient safety, accidental falls, nursing
INTRODUCTION
Accidental falls are among the most common adverse events reported in hospitals. By some estimates one million or more patient falls occur annually during hospitalization in the U.S.,1 with a quarter or more complicated by injury.2–4 Fall-related injuries can result in increased length of hospital stay,5,6 greater health care expenditures,6,7 and litigation.8 Moreover, up to 11,000 U.S. patients die annually due to injuries sustained from a fall during hospitalization.1 In 2008 the Centers for Medicare & Medicaid Services (CMS) listed injurious falls as one of eight “never events”—reasonably preventable safety breaches which should never occur during hospital care—and no longer reimburses for care associated with diagnosis and treatment of injuries related to falls during hospitalization. Despite this regulatory change in reimbursement and the availability of numerous fall prevention guidelines, hospital fall rates have been decreasing at an unacceptably slow rate over the past several years.2,9
Fall rates in acute care hospital units range from 1.3 to 8.9 per 1,000 bed-days.2,10 Although higher rates are reported in certain types of units (e.g., neurology), researchers have reported large unexplained variation in fall rates among hospital units with similar patient populations.2,9,11 What is not known is the extent to which differences in fall rates among units with similar populations remain consistent across time. If rates are persistently different between units with similar populations then factors other than patient characteristics may account for the lack of progress in decreasing hospital falls. The twofold purpose of this study was to determine the proportion of variation in long term fall rates attributable to between-unit, rather than within-unit, variability and to identify available unit- and hospital-level characteristics associated with persistently high- and low- fall units.
METHODS
Sample and Data
We obtained data for this exploratory study from the National Database of Nursing Quality Indicators® (NDNQI®), a project launched by the American Nurses Association (ANA) and recently acquired by Press Ganey Associates, Inc. that involves over 2,000 U.S. hospitals. The NDNQI was established in 1998 to create a database for providing acute care hospitals with comparative information on nursing-related structure, process, and outcome indicators, including indicators related to falls and nurse staffing. The database is operated by the School of Nursing at the University of Kansas Medical Center with oversight from the institution’s human subjects committee.
The NDNQI trains personnel in participating hospitals to collect and report monthly data on falls and nurse staffing according to a detailed set of data collection definitions and guidelines. The rigorous data submission process is coupled with extensive data cleaning to ensure the ongoing reliability of NDNQI data. Although the set of NDNQI hospitals is not a proportionate sample, it includes one-third of all U.S. hospitals, and general hospitals of all types and sizes from various regions are represented in the database.
We extracted all available 2009–2010 NDNQI falls and nurse staffing data for medical (as distinct from surgical or medical-surgical combined) units in U.S. general hospitals. After excluding 865 units reporting a designated specialty (e.g., neurology) and 673 units for which complete fall rate data (i.e., both the total fall count and the number of inpatient days) were not available for all 24 study months, we were left with a sample of 800 units.
For each of the 800 sample units we computed the 24-month rate of total falls per 1,000 patient days by summing the 24 monthly counts of total falls, dividing the result by the sum of the 24 monthly patient day counts, and multiplying by 1,000. For descriptive purposes we also computed 24-month rates of injurious falls. The NDNQI considers falls resulting in any sign or symptom of injury (including pain, bruising, muscle/joint strain, fracture, or any wound requiring cleaning or dressing) or in death to be injurious falls.
Within- and between-unit variation in fall rates
We used the 24-month total fall rates to estimate the proportion of variation in long-term fall rates accounted for by variation among units. We obtained this estimate as follows. Assuming Poisson-distributed fall counts, we subtracted the Poisson variance (estimated from the observed fall rates) from the total sample variance to obtain the estimated between-unit variance.12 Dividing the between-unit variance by the total sample variance yielded an estimate of the proportion of variability due to between-unit differences. We also computed the coefficient of variation by dividing the between-unit standard deviation by the study-wide fall rate.
Identifying low- and high-fall units
To identify units with consistently low or high fall rates, we computed monthly fall rates for each unit (based on the count of total falls and patient days for the month), rank-ordered these rates within each month, and classified each unit into one of four quartiles (0 to 3) for each month based on its ranked fall rate. We then summed each unit’s quartile scores across the 24 study months, obtaining a score for each unit that could range from 0 (for units in the lowest fall quartile in all 24 months) to 72 (for units in the highest fall quartile across all 24 months). We selected units scoring in the bottom decile (N = 80) or top decile (N = 74) on this measure for comparison. (The number in the top decile was less than 10% of the total number of units due to ties.)
Comparing low- and high-fall units
Fall rates
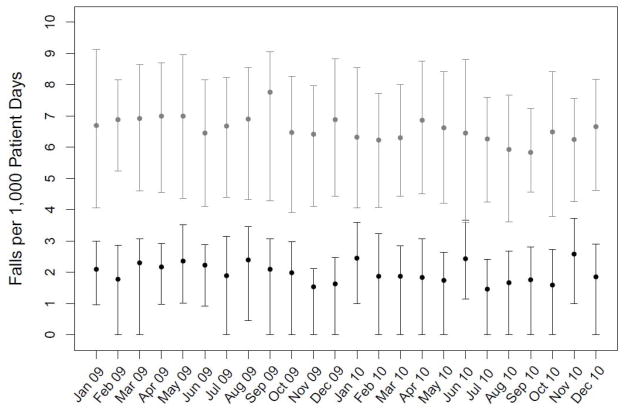
We compared the low- and high-fall units on both their 24-month total fall rates and 24-month injurious fall rates. In addition, to illustrate the distinction between the low- and high-fall units, we plotted the monthly mean total fall rate and inter-quartile range for each group across the months of the study.
Unit characteristics
We compared low- and high-fall units on four unit-level variables. Using data on nurse staffing (available for 94% of the study’s 19,200 unit-months), we computed total nursing care hours per patient day for each unit by summing the hours of care provided by registered nurses (RNs), licensed practical nurses (LPNs), and assistive personnel in direct care roles across the 24 study months and dividing by total inpatient days during the study. RN mix was computed as the percentage of total nursing care hours provided by RNs. The other two comparison variables were total inpatient days and the percent of fallers classified as at risk based on a documented fall risk assessment prior to falling. Data on faller risk status at time of fall were available for 83% of falls.
Hospital characteristics
We also examined several hospital characteristics that might be associated with variation in unit fall rates. The 154 low- and high-fall units came from 128 unique hospitals. There were 17 hospitals with multiple units represented, and 15 of these were homogeneous, comprising only low-fall or only high-fall units. For simplicity, and to avoid violations of independence associated with multiple units clustered within a single hospital, we considered only one unit from each of these homogeneous hospitals in this analysis (equivalent to conducting the analysis at the hospital level). The other two multiple-unit hospitals each comprised one low-fall and one high-fall unit, and these were excluded.
We compared the low- and high-fall units on five hospital characteristic variables: bed size (<300 beds or ≥300 beds), teaching status (academic medical center, regular teaching hospital, or non-teaching hospital), locale (metropolitan or non-metropolitan), U.S. census division (Northeast, South, Midwest, or West), and Medicare case mix index.
Statistical Inference
All analyses were carried out in SAS 9.4 (SAS Institute, Inc., Cary, NC). We used Chi-square tests for associations between low- and high-fall classification and categorical variables. We tested for differences between low- and high-fall units on quantitative variables using Wilcoxon two-sample tests.
RESULTS
Characteristics of sample units
The 800 sample units came from 470 hospitals; 261 (56%) of these were teaching hospitals, 244 (52%) had fewer than 300 staffed beds, and 435 (92%) were located in a metropolitan area. All 50 states and the District of Columbia were represented in the sample.
Within- and between-unit variation in fall rates
Estimates of total, between-unit, and within-unit variability in 24-month fall rates (based on the full sample of 800 units) are provided in Table 1. The coefficient of variation (between-unit standard deviation divided by study-wide fall rate) is also given. Based on the assumption of Poisson-distributed unit fall rates, 87% variation in long-term fall rates is due to differences between units, suggesting that we can reliably distinguish between units with persistently low and persistently high fall rates.
Table 1.
Estimated variation in 24-month inpatient fall rates1 on medical units (n = 800)
| Total variance | Between-unitvariance | Within-unit variance | Coefficient of variation |
|---|---|---|---|
| 1.9 | 1.6 (87%) | 0.3 (13%) | 0.3 |
Fall rate = falls per 1,000 patient-days
Comparing low- and high-fall units
Fall rates
The average 24-month total fall rate for the 800 sample units was 4.1 (SD 1.4) falls per 1,000 patient days. The average injurious fall rate was 0.9 (SD 0.5). For the low- and high-fall units, respectively, the average total fall rates were 2.0 (SD 0.5) and 6.6 (SD 1.2); the average injurious fall rates were 0.5 (SD 0.3) and 1.4 (SD 0.6). Both rates were significantly higher on high-fall units (Wilcoxon two-sample p-values < .001). The mean and interquartile range for the total fall rate are shown by month for the low- and high-fall units in Figure 1.
Figure 1.
Mean total fall rate and inter-quartile range for low- and high-fall units by month. Grey dots and lines indicate means and inter-quartile range values for high-fall units; black dots and lines indicate means and inter-quartile range values for low-fall units.
Unit and hospital characteristics
Unit and hospital characteristics of low- and high-fall units are shown in Table 2. The only unit or hospital characteristic variable with a statistically significant association with classification as a low- or high-fall unit was patient days; high-fall units tended to have more patient days.
Table 2.
Unit and hospital characteristics of low- and high-fall medical units
| Unit characteristics (n=154) | Low-Fall (n=80) | High-Fall (n=74) | p-value |
|---|---|---|---|
| Patient days (thousands) [mean (SD)] | 17.0 (5.9) | 19.5 (5.5) | .01a |
| Fallers at risk (% of falls by at-risk patients) [mean (SD)] | 73.5 (22.1) | 70.1 (23.9) | .34a |
| Total nursing hours per patient day [mean (SD)] | 8.1 (1.8) | 8.4 (1.3) | .20a |
| RN mix (% hours provided by RNs) [mean(SD)] | 62.5 (12.6) | 63.6 (6.8) | .59a |
| Hospital characteristics (n=126) | Low-Fall (n=62) | High-Fall (n=64) | p-value |
|---|---|---|---|
| Bed size (% with 300+ beds) | 62.9 | 57.8 | .56b |
| Teaching status | .60b | ||
| Academic medical center (%) | 19.4 | 14.1 | |
| Regular teaching (%) | 43.6 | 51.6 | |
| Non-teaching (%) | 37.1 | 34.4 | |
| Locale (%metropolitan) | 93.6 | 93.8 | .96b |
| Census division | .09b | ||
| Northeast (%) | 37.1 | 18.8 | |
| South (%) | 38.7 | 50.0 | |
| Midwest (%) | 11.3 | 20.3 | |
| West (%) | 12.9 | 10.9 | |
| Medicare case mix index [mean (SD)] | 1.6 (0.2) | 1.6 (0.2) | .24a |
Notes: SD = standard deviation. RN = registered nurse. Percentages may not sum to 100.0 due to rounding.
P-value from Wilcoxon two-sample test.
P-value from Chi-square test of association.
DISCUSSION
In this large, long-term study of medical nursing units we observed fall rates ranging from 0.2 to 13.3 falls per 1,000 patient days. This confirms previous findings that fall rates vary among nursing units with similar types of patients.2,9,11 Importantly, we were able to identify distinct low- and high-fall units based on long-term fall rates. These results are important for falls research and prevention because they indicate that there is meaningful variability among units, not just noise, driving differences in observed fall rates.
Underlying reasons for this variability can potentially be explained by further studying differences in environment, equipment, procedures, and culture between units with fall rates that are consistently low and units with fall rates that are consistently high. The low- and high-fall units in our study did not differ on most of the unit or hospital characteristic variables we examined, suggesting the need to look beyond the variables that are typically studied as potential correlates of fall rates.
The one significant difference we found between low- and high-fall units was that high-fall units tended to have a greater number of patient days during the study period. To our knowledge this is a new finding and should be verified in other studies. Given that low- and high-fall units were not significantly different on aggregate unit labor quality and quantity measures, one potential explanation for higher-volume units having higher fall rates is that they have higher patient turnover (admissions, discharges, and transfers) than lower-volume units. Consistent with this explanation, Needleman and colleagues13 reported an association between high patient turnover and increased mortality and have suggested the need for staffing projection models that account for the workload of admissions, discharges and transfers. Another potential explanation is that higher-fall, higher-volume units tend to be physically larger than lower-fall, lower-volume units, with greater distances between rooms and nurses’ stations. Unit size and other physical characteristics of units (e.g., lines of sight, distance from bed to bathroom, multiple-floor layouts) should be studied for potential insights into fall risk.
We found little difference in staffing between units with persistently high or low fall rates. This null finding is important for two reasons. First, it casts further doubt on the supposed inverse association between nurse staffing levels and total fall rates,14 and second, it is evidence against the idea that nurses with more time on their hands (i.e., nurses on units with higher staffing levels) are more likely to report falls. If this were the case we would expect a positive association between staffing levels and fall rates.
Our study has several limitations. First, although all 50 states and the District of Columbia were represented in the study, the voluntary nature of hospital participation in the NDNQI may limit the representativeness of the sample. In addition, it is possible that some NDNQI hospitals did not report falls data for all their medical units during the study period. A second limitation is that the falls data were self-reported. It is possible that systematic under-reporting of non-injurious falls could explain some of the difference between low- and high-fall units; however, the average injurious fall rate for high-fall units was nearly three times the average injurious rate for low-fall units, which points to real (not just reported) differences in fall rates. And third, although we limited the sample to medical units, there are a number of unmeasured patient and unit characteristics which could not be controlled for using NDNQI data, including fall risk, medications, capital and equipment resources, policies and procedures, shift-level nurse staffing, and knowledge and attitude of front line and administrative personnel.
Although we explored several variables related to facility and staffing, NDNQI has limited patient-level information. Several factors underlying falls among hospital patients have been identified, including advanced age, use of certain “culprit” drugs, and altered mental status or dementia.15 In addition, fall risk assessment tools based on such factors have been developed.16,17 In previous work patient-level risk factors have been aggregated to estimate unit-level risk,11 but this approach requires further refinement.
Understanding variation is a useful tool for improving health care quality,18,19 and the method of studying variation used here has not been applied previously to inpatient fall rates. Further study in depth of low- and high-fall units, including their physical characteristics, levels of patient turnover, and processes of care, could reveal ways in which low- and high-fall units differ, and may lead to useful approaches to improving fall prevention.
In sum, we have shown that there are persistent differences among nursing unit fall rates. Given the limited change in fall rates over time, the large variation between low- and high-fall units, and the lack of high-quality evidence suggesting sustainable, effective approaches to reducing inpatient falls,10 improving our understanding of the sources of variation among nursing units would move the field of hospital fall prevention forward.
Acknowledgments
Funding: Research funding was provided under contracts with the American Nurses Association and Press Ganey Associates, Inc., and by the National Institutes of Health (NIH/NIA R01-AG033005). Lorraine C. Mion and Ronald I. Shorr have provided expert testimony related to hospital falls.
Sponsors’ Role. The American Nurses Association owned the NDNQI at the time the data were collected; Press Ganey Associates, Inc. purchased the NDNQI while the manuscript was being written. Neither organization had any role in the conception or design of the study, or in data analysis or interpretation.
Footnotes
Conflict of Interest: The editor in chief has reviewed the conflict of interest checklist provided by the authors and has determined that the authors have no financial or any other kind of personal conflicts with this paper.
Author Contributions. All authors participated in designing the study, interpreting results, and drafting the manuscript. Statistical analyses were carried out by VS; the study was conceived by RS.
References
- 1.Currie L. Fall and injury prevention. In: Hughes RG, editor. Patient Safety and Quality: An Evidence-based Handbook for Nurses. Rockville, MD: Agency for Healthcare Research and Quality; 2008. pp. 195–250. AHRQ Publication NO08-0043. [PubMed] [Google Scholar]
- 2.Bouldin EL, Andresen EM, Dunton NE, et al. Falls among adult patients hospitalized in the United States: Prevalence and trends. J Patient Saf. 2013;9:13–17. doi: 10.1097/PTS.0b013e3182699b64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Healey F, Scobie S, Oliver D, et al. Falls in English and Welsh hospitals: A national observational study based on retrospective analysis of 12 months of patient safety incident reports. Qual Saf Health Care. 2008;17:424–430. doi: 10.1136/qshc.2007.024695. [DOI] [PubMed] [Google Scholar]
- 4.Schwendimann R, Buhler H, De Geest S, et al. Characteristics of hospital inpatient falls across clinical departments. Gerontology. 2008;54:342–348. doi: 10.1159/000129954. [DOI] [PubMed] [Google Scholar]
- 5.Brand CA, Sundararajan V. A 10-year cohort study of the burden and risk of in-hospital falls and fractures using routinely collected hospital data. Qual Saf Health Care. 2010;19:e51. doi: 10.1136/qshc.2009.038273. [DOI] [PubMed] [Google Scholar]
- 6.Wong CA, Recktenwald AJ, Jones ML, et al. The cost of serious fall-related injuries at three Midwestern hospitals. Jt Comm J Qual Patient Saf. 2011;37:81–87. doi: 10.1016/s1553-7250(11)37010-9. [DOI] [PubMed] [Google Scholar]
- 7.Rosenthal MB. Nonpayment for performance? Medicare’s new reimbursement rule. N Engl J Med. 2007;357:1573–1575. doi: 10.1056/NEJMp078184. [DOI] [PubMed] [Google Scholar]
- 8.Oliver D, Killick S, Even T, et al. Do falls and falls-injuries in hospital indicate negligent care -- and how big is the risk? A retrospective analysis of the NHS Litigation Authority Database of clinical negligence claims, resulting from falls in hospitals in England 1995 to 2006. Qual Saf Health Care. 2008;17:431–436. doi: 10.1136/qshc.2007.024703. [DOI] [PubMed] [Google Scholar]
- 9.He J, Dunton N, Staggs V. Unit-level time trends in inpatient fall rates of US hospitals. Med Care. 2012;50:801–807. doi: 10.1097/MLR.0b013e31825a8b88. [DOI] [PubMed] [Google Scholar]
- 10.Hempel S, Newberry S, Wang Z, et al. Hospital fall prevention: A systematic review of implementation, components, adherence, and effectiveness. J Am Geriatr Soc. 2013;61:483–494. doi: 10.1111/jgs.12169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Shorr RI, Chandler AM, Mion LC, et al. Effects of an intervention to increase bed alarm use to prevent falls in hospitalized patients: A cluster randomized trial. Ann Intern Med. 2012;157:692–699. doi: 10.7326/0003-4819-157-10-201211200-00005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hayes RJ, Bennett S. Simple sample size calculation for cluster-randomized trials. Int J Epidemiol. 1999;28:319–326. doi: 10.1093/ije/28.2.319. [DOI] [PubMed] [Google Scholar]
- 13.Needleman J, Buerhaus P, Pankratz VS, et al. Nurse staffing and inpatient hospital mortality. N Engl J Med. 2011;364:1037–1045. doi: 10.1056/NEJMsa1001025. [DOI] [PubMed] [Google Scholar]
- 14.Lake ET, Cheung RB. Are patient falls and pressure ulcers sensitive to nurse staffing? West J Nurs Res. 2006;28:654–677. doi: 10.1177/0193945906290323. [DOI] [PubMed] [Google Scholar]
- 15.Oliver D, Healey F, Haines TP. Preventing falls and fall-related injuries in hospitals. Clin Geriatr Med. 2010;26:645–692. doi: 10.1016/j.cger.2010.06.005. [DOI] [PubMed] [Google Scholar]
- 16.Perell KL, Nelson A, Goldman RL, et al. Fall risk assessment measures: An analytic review. J Gerontol A Biol Sci Med Sci. 2001;56:M761–M766. doi: 10.1093/gerona/56.12.m761. [DOI] [PubMed] [Google Scholar]
- 17.Oliver D. Falls risk-prediction tools for hospital inpatients. Time to put them to bed? Age Ageing. 2008;37:248–250. doi: 10.1093/ageing/afn088. [DOI] [PubMed] [Google Scholar]
- 18.Curry LA, Spatz E, Cherlin E, et al. What distinguishes top-performing hospitals in acute myocardial infarction mortality rates? A qualitative study. Ann Intern Med. 2011;154:384–390. doi: 10.7326/0003-4819-154-6-201103150-00003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Rose AJ, Petrakis BA, Callahan P, et al. Organizational characteristics of high- and low-performing anticoagulation clinics in the Veterans Health Administration. Health Serv Res. 2012;47:1541–1560. doi: 10.1111/j.1475-6773.2011.01377.x. [DOI] [PMC free article] [PubMed] [Google Scholar]