Abstract
Background
Breast projection is a critical element of breast reconstruction aesthetics, but little has been published regarding breast projection as the firm expander is changed to a softer implant. Quantitative data representing this loss in projection may enhance patient education and improve our management of patient expectations.
Methods
Female patients who were undergoing immediate tissue-expander breast reconstruction with the senior author were enrolled in this prospective study. Three-dimensional camera software was used for all patient photographs and data analysis. Projection was calculated as the distance between the chest wall and the point of maximal projection of the breast form. Values were calculated for final tissue expander expansion and at varying intervals 3, 6, and 12 months after implant placement.
Results
Fourteen breasts from 12 patients were included in the final analysis. Twelve of the 14 breasts had a loss of projection at three months following the implant placement or beyond. The percentage of projection lost in these 12 breasts ranged from 6.30% to 43.4%, with an average loss of projection of 21.05%.
Conclusions
This study is the first prospective quantitative analysis of temporal changes in breast projection after expander-implant reconstruction. By prospectively capturing projection data with three-dimensional photographic software, we reveal a loss of projection in this population by three months post-implant exchange. These findings will not only aid in managing patient expectations, but our methodology provides a foundation for future objective studies of the breast form.
Keywords: Breast, Breast implants, Esthetics
INTRODUCTION
Tissue expansion is an accepted and widely used method for breast reconstruction, with shorter operative times and diminished donor-site morbidity compared to autologous tissue options [1,2]. While surgical techniques for this method have improved in recent years and expanders have evolved in terms of shape and constitution, maintaining breast projection remains a challenge [3,4]. Tissue expanders work to stretch the overlying skin after mastectomy, creating an enlarged, projected pocket for placement of a permanent implant. Many patients may enjoy the projection they achieve with tissue expansion and expect to maintain similar projection following permanent implants are placed. However, preserving this projection after the expander is exchanged for a softer implant is often difficult due to skin retraction and settling of the implant. It is therefore important to educate patients on this predicted loss of projection in an effort to appropriately manage expectations.
To date, no studies have quantitatively reported on breast projection in expander-implant reconstruction. Previous studies analyzing aesthetic outcomes after tissue expander breast reconstruction have often relied upon varying numeric scales of global appearance [5,6,7]. A majority of these investigations focused on overall aesthetics and perceived symmetry, contour, scarring, and inframammary fold (IMF) definition; very few have attempted to systematically and quantitatively evaluate breast projection. The recent and fairly widespread adoption of three-dimensional (3D) imaging software now offers clinicians the ability to quantitatively evaluate aesthetic features, such as implant projection [8,9,10]. We therefore endeavored to prospectively track breast projection following expander exchange, measuring projection dimensions with 3D computer software. By analyzing a critical feature of breast aesthetics and reconstruction in a quantitative and prospective fashion, we hope to provide insight on the temporal changes related to breast projection in implant-based breast reconstruction to better manage patient expectations.
METHODS
Patient population
Female patients who were undergoing mastectomy with immediate tissue expander breast reconstruction with the senior author (J.K.) were offered participation in this prospective study. Participating patients were between the ages of 25 and 85. Patients with a history of prior radiation were excluded. Fifteen patients were enrolled and received the Contour Profile tissue expander during their reconstruction.
Data collection
Patient medical information, including preoperative demographics and operative details, was obtained through a review of electronic medical records. Collected variables included age, body mass index (BMI), comorbidities, and adjuvant radiation. 3D images were taken at the initial consultation and at each scheduled follow-up visit. Scheduled follow-up visits included: one to two weeks post-expander placement, tissue expansion nurse visits, immediately before implant exchange, one to two weeks after implant exchange, three months post-implant exchange, six months post-implant exchange, and one year post-implant exchange. All captured data was de-identified to comply with the Health Insurance Portability and Accountability Act of 1996.
Image analysis
The Canfield Vectra Three-Dimensional Camera Software (Canfield Scientific Inc., Fairfield, NJ, USA) was used for all patient photographs and projection analysis. The validity and reliability of 3D breast imaging for human subjects has been confirmed by several authors [10,11,12]. The software was used to highlight the entire breast form to allow for subsequent isolation of the chest wall from the overlying breast tissue (Fig. 1A). Landmarks were manually placed at the point of maximal projection, the IMF, the convergence of the left and right IMF, and the sternal notch. Projection was defined as the distance from the chest wall to the point of maximal projection of the breast form in millimeters (Fig. 1B, C). Percent change was normalized to measurements recorded at final tissue expander expansion. Additional 3D linear measurements included nipple to IMF distance (mm) and sternal notch to nipple distance (mm). Image analysis was performed independently by two members of the Division of Plastic and Reconstructive Surgery with the average of their calculations used as final results.
Fig. 1. Calculation of projection in three-dimensional photographs.
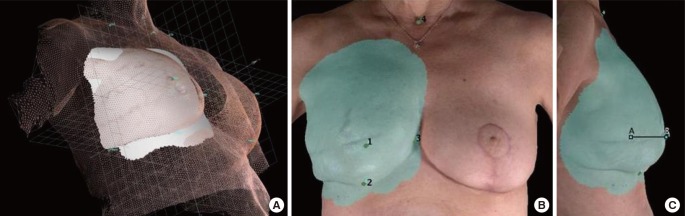
(A) Use of three-dimensional software to highlight the breast form and calculate projection. (B) 1, calculated right nipple (point of maximal projection); 2, right inframammary fold; 3, convergence of left and right inframammary folds; 4, sternal notch. (C) Projection is the distance between A and B. In this representative postoperative photograph, projection is 40.8-mm. A, chest wall; B, point of maximal projection.
RESULTS
Fourteen breasts from 12 patients were included in the final analysis. The average age of the participants was 56.5 years. The average BMI was 28.0. Hypertension was the most common comorbidity in the cohort (41.67%), followed by diabetes (27.27%). None of the patients received preoperative radiation, and a quarter of the participants underwent postoperative radiation. Median time from tissue expander placement to permanent implant exchange was 183.16 days (range, 101-377 days). Median time from last expansion to implant exchange was 53 days (range, 23-225 days).
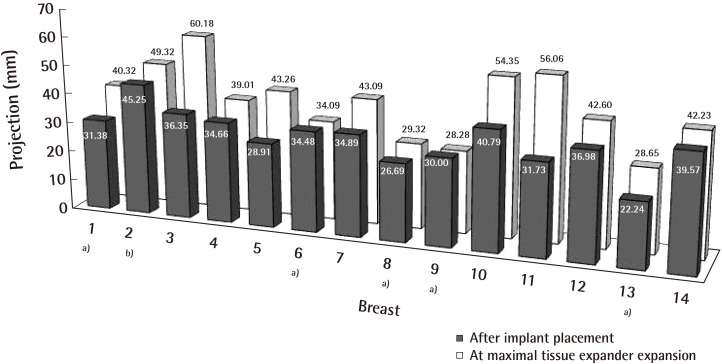
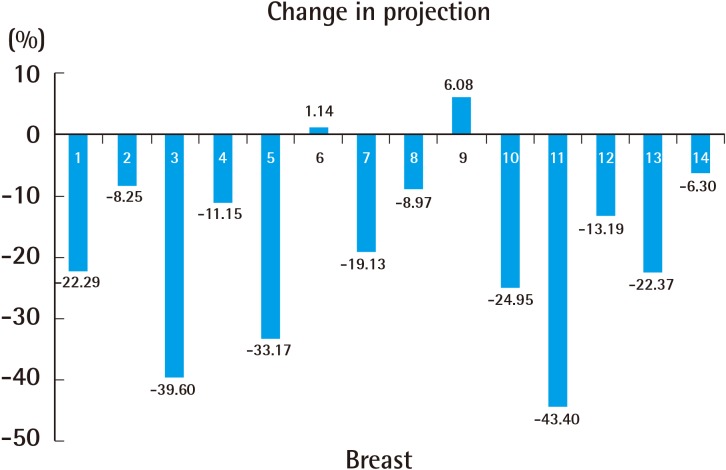
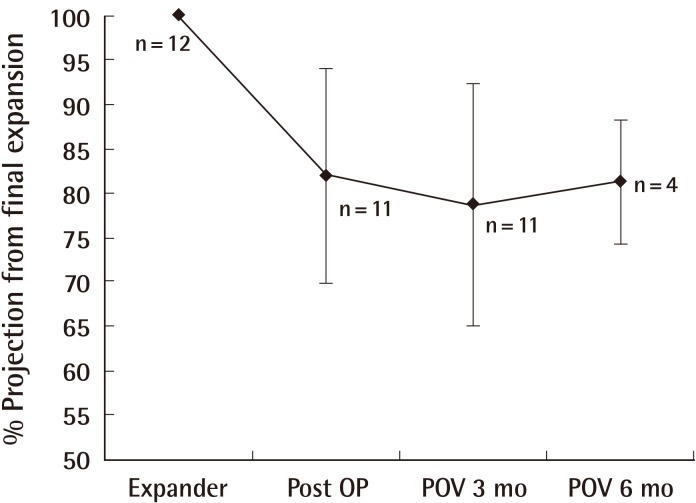
Analysis of 3D photographs revealed that loss of projection occurred in 12 of the 14 breasts at three months following implant placement or beyond (Fig. 2). The percentage of projection lost in these 12 breasts ranged from 6.30% to 43.40% (mean loss±standard deviation, 21.04%±12.43%) (Fig. 3). Fig. 4 illustrates the mean loss in projection over time. Representative photographic results are shown in Fig. 5. The two breasts with a gain in maximal projection had a 1.14% and 6.08% increase, respectively. This correlated to an average gain of 3.61%.
Fig. 2. Breast projection with expanders versus implants.
Projection values (in millimeters) from final expansion to last postoperative visit. Data is shown per breast. a)Last postoperative visit (POV) was at 6 months; b)Last POV was at 1 year. All others had their last POV at 3 months.
Fig. 3. Percent change in breast projection.
Percent change in breast projection from final tissue expander expansion to last postoperative visit following implant placement.
Fig. 4. Temporal loss of projection.
Excludes 2 breasts that gained projection. Post OP, postoperative; POV, postoperative visit.
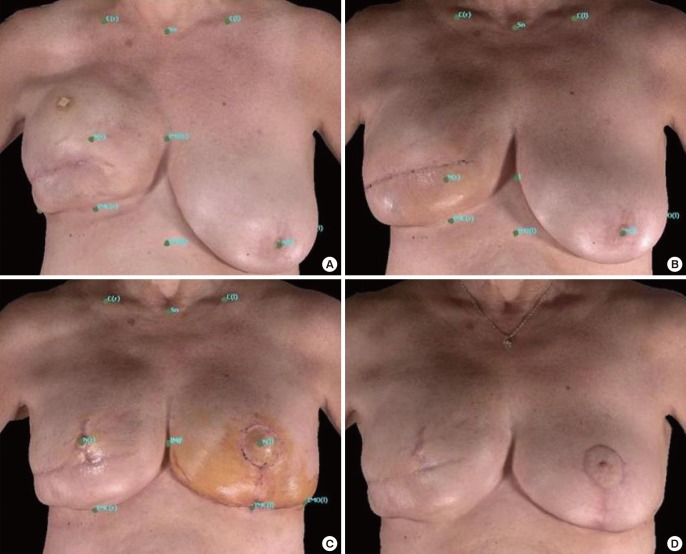
Fig. 5. Photographic evolution of the reconstructed breast.
Representative photographs demonstrating changes in breast shape over time. (A) At final expansion, projection was 54.4-mm (100%), (B) post-implant exchange, projection 43.5-mm (83.8%), (C) 3-months postoperative projection 45.0-mm (82.8%), (D) 6-months postoperative projection 40.8-mm (75.1%).
In the vertical dimension, there was a mean decrease in nipple to IMF distance of 2.98±12.83 mm. Sternal notch to nipple distance increased by an average of 9.26±18.53 mm.
DISCUSSION
Aesthetic results following breast reconstruction contribute greatly to patients' overall satisfaction and quality of life [4,13]. Currently, the most commonly performed breast reconstruction is two-stage expander-implant reconstruction [14]. One of the central features of breast reconstruction aesthetics is breast projection. Loss of this projection at the completion of reconstruction is often subjectively noted by the surgeon and may be disheartening and anxiety provoking for the patient after several months of expansion. While surgeons may discuss an anticipated loss in projection with patients, quantitative data defining the predicted loss is needed to enrich physician-patient dialogue and temper patient expectations.
Three-dimensional photography has gained popularity for prospective patient consultation by providing a personalized visual for patient expectations, particularly in aesthetic surgery. Over a decade has passed since reports of 3D imaging of the breast were published, yet relatively few studies have utilized this powerful tool for critical analysis of outcomes [8,11]. Kovacs et al. [9] used 3D imaging to evaluate postoperative volume and shape changes after breast augmentation. Quan et al. [15] utilized 3D imaging to study longitudinal changes in breast volume and contour after medial pedicle breast reduction. Tepper et al. [16] performed volumetric analysis to evaluate symmetry after unilateral implant-based reconstruction with balancing procedures. Ours is the first study to analyze breast projection in two-stage implant-based reconstruction in a prospective manner using 3D imaging tools.
Notably, our analysis revealed that a majority of patients (12 out of 14 breasts) suffered from an average loss of projection of nearly one-quarter of the projection achieved at final tissue expander expansion. This single objective finding raises several practical questions: Should tissues be over-expanded in anticipation of projection loss? Is there an optimal expansion schedule to minimize projection changes? What is the efficacy of new technological refinements such as higher profile implants or expanders [17,18] or acellular dermal matrix to preserve projection? Currently, there is a paucity of quantitative data regarding projection after tissue expander reconstruction to clearly guide our clinical decision-making. We propose that these questions may uniquely be addressed through prospective, longitudinal studies utilizing objective photographic methods presented herein. Despite the intellectual curiosities raised, our findings provide valuable data for patient counseling and expectation management.
Loss of projection may be attributed to tissue retraction, given the viscoelastic properties of skin and the biomechanical principles of tissue expansion. 3D studies of projection gain after breast augmentation have demonstrated on average 20% less gain than expected based on implant dimensions [9,19], perhaps highlighting the impact of inherent tissue forces on the overall projection achieved. Given the difference in rigidity between the tissue expander and a permanent implant, outward resistance to tissue retraction decreased and contributed to loss of projection. Postoperative fibrotic changes, due to adjuvant radiation or capsular contracture, likely also contribute to loss of projection. Anecdotally, the two breasts with the greatest loss of projection received adjuvant radiation therapy; however, our analysis does not provide authoritative data to confirm or dispute the effect of radiation.
Moreover, creep, the stretching of a material under a constant tension over time, and related stress relaxation, the decrease in internal stresses due to a constant stretch occurs to a greater extent when tissue expansion is maintained for longer periods [20]. It is during this relaxation period that histologic and biochemical changes occur, including epithelial proliferation, collagen synthesis, and recovery from expansion-induced tissue ischemia [21]. Experimentally, it has been shown that there is no difference between rapid tissue expansion and slower expansion, but rather it is the maintenance period-the period for which the tissue is held at a certain strain-that affects final tissue surface area [22,23]. In our study, the median maintenance period between the last expansion and surgery was 53 days. Clinically, the expansion schedule is often patient-driven, influenced by patient comfort and acceptance of overall reconstruction time; however, it is important to be cognizant of the underlying mechanisms of expansion, as they may affect final outcomes.
Downward displacement of the implant similar to "bottoming out" may also contribute to loss of projection. This could be more likely in cases where capsultomies were performed, as noted in six of the 14 breasts (Table 1). "Bottoming out" is not an infrequent occurrence with mastopexy and reduction mammoplasty and has been observed with implant displacement in augmentation mammoplasty [24,25]. Vegas and Martin Del Yerro [23] discussed the mechanics of materials as applied to breast augmentation, and suggested that in the high-compliance, low-stiffness breast, or perhaps in an older mastectomy patient, creep deformation and a bottoming out deformity were likely outcomes if a large implant was used. Using 3D photographic tracking, Quan et al. [15] reported that a 6% migration of breast parenchyma from the upper to lower pole was associated with a 10.6-mm loss of projection after reduction mammaplasty. In our series, there was a trend towards vertical descent of the maximal point of projection.
Table 1. Patient information (per breast).
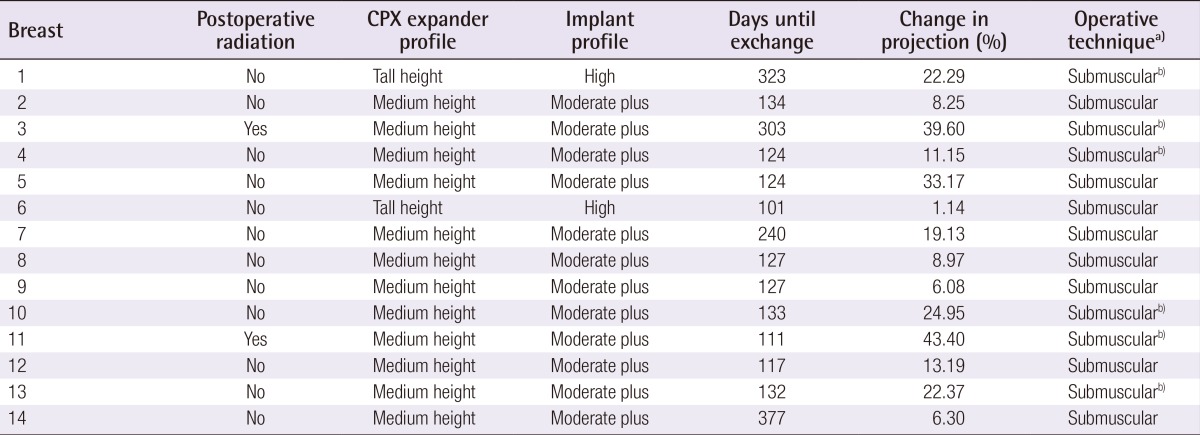
CPX, Contour Profile tissue expander.
a)None of the cases required acellular dermis placement; b)Capsulotomy performed at time of implant placement.
Our data has substantiated the putative loss of projection previously associated with expander-implant breast reconstruction. The two breasts with a reported increase in projection were exceptions to this trend. One explanation for the noted increase may have been that the tissue expanders were compressed in some manner during the final expansion picture, leading to slightly lower projection values. Additionally, a larger implant than initially anticipated may have been inserted due to patient preference and an accommodating tissue pocket.
While this study provides much needed quantitative data on breast projection after expander-implant reconstruction, there are limitations to this investigation. First, we utilized a small patient population. The data presented in this study therefore serves as a foundation for future larger studies. Second, projection measurements may have been subject to human error although previous studies have reported good inter-rater reliability [10]. Lastly, we instituted a minimum follow-up period of three months for inclusion in the projection analysis. Long term outcomes from prosthetic reconstruction, including capsular contracture and malposition, will be captured in a future extrapolated analysis and reported in follow up studies.
This study serves as the first prospective, systematic analysis of temporal changes in breast projection during expander-implant reconstruction. Our results reveal that a majority of breasts suffered a loss of projection by three months after implant placement. This analysis will help reconstructive surgeons with patient education and more effectively manage patient expectations. Furthermore, our methodology provides a foundation for future objective studies of the breast form.
Footnotes
No potential conflict of interest relevant to this article was reported.
References
- 1.Hirsch EM, Seth AK, Dumanian GA, et al. Outcomes of tissue expander/implant breast reconstruction in the setting of prereconstruction radiation. Plast Reconstr Surg. 2012;129:354–361. doi: 10.1097/PRS.0b013e31823ae8b1. [DOI] [PubMed] [Google Scholar]
- 2.Mioton LM, Smetona JT, Hanwright PJ, et al. Comparing thirty-day outcomes in prosthetic and autologous breast reconstruction: a multivariate analysis of 13,082 patients? J Plast Reconstr Aesthet Surg. 2013;66:917–925. doi: 10.1016/j.bjps.2013.03.009. [DOI] [PubMed] [Google Scholar]
- 3.Gui GP, Tan SM, Faliakou EC, et al. Immediate breast reconstruction using biodimensional anatomical permanent expander implants: a prospective analysis of outcome and patient satisfaction. Plast Reconstr Surg. 2003;111:125–138. doi: 10.1097/01.PRS.0000037752.95854.41. [DOI] [PubMed] [Google Scholar]
- 4.Spear SL, Pelletiere CV. Immediate breast reconstruction in two stages using textured, integrated-valve tissue expanders and breast implants. Plast Reconstr Surg. 2004;113:2098–2103. doi: 10.1097/01.prs.0000122406.99750.c3. [DOI] [PubMed] [Google Scholar]
- 5.Eriksen C, Lindgren EN, Frisell J, et al. A prospective randomized study comparing two different expander approaches in implant-based breast reconstruction: one stage versus two stages. Plast Reconstr Surg. 2012;130:254e–264e. doi: 10.1097/PRS.0b013e3182589ba6. [DOI] [PubMed] [Google Scholar]
- 6.Eriksen C, Lindgren EN, Olivecrona H, et al. Evaluation of volume and shape of breasts: comparison between traditional and three-dimensional techniques. J Plast Surg Hand Surg. 2011;45:14–22. doi: 10.3109/2000656X.2010.542652. [DOI] [PubMed] [Google Scholar]
- 7.McGeorge DD, Mahdi S, Tsekouras A. Breast reconstruction with anatomical expanders and implants: our early experience. Br J Plast Surg. 1996;49:352–357. doi: 10.1016/s0007-1226(96)90002-8. [DOI] [PubMed] [Google Scholar]
- 8.Galdino GM, Nahabedian M, Chiaramonte M, et al. Clinical applications of three-dimensional photography in breast surgery. Plast Reconstr Surg. 2002;110:58–70. doi: 10.1097/00006534-200207000-00012. [DOI] [PubMed] [Google Scholar]
- 9.Kovacs L, Eder M, Hollweck R, et al. New aspects of breast volume measurement using 3-dimensional surface imaging. Ann Plast Surg. 2006;57:602–610. doi: 10.1097/01.sap.0000235455.21775.6a. [DOI] [PubMed] [Google Scholar]
- 10.Losken A, Seify H, Denson DD, et al. Validating three-dimensional imaging of the breast. Ann Plast Surg. 2005;54:471–476. doi: 10.1097/01.sap.0000155278.87790.a1. [DOI] [PubMed] [Google Scholar]
- 11.Nahabedian MY, Galdino G. Symmetrical breast reconstruction: is there a role for three-dimensional digital photography? Plast Reconstr Surg. 2003;112:1582–1590. doi: 10.1097/01.PRS.0000085818.54980.C4. [DOI] [PubMed] [Google Scholar]
- 12.Tepper OM, Small K, Rudolph L, et al. Virtual 3-dimensional modeling as a valuable adjunct to aesthetic and reconstructive breast surgery. Am J Surg. 2006;192:548–551. doi: 10.1016/j.amjsurg.2006.06.026. [DOI] [PubMed] [Google Scholar]
- 13.Tepper OM, Unger JG, Small KH, et al. Mammometrics: the standardization of aesthetic and reconstructive breast surgery. Plast Reconstr Surg. 2010;125:393–400. doi: 10.1097/PRS.0b013e3181c4966e. [DOI] [PubMed] [Google Scholar]
- 14.American Society of Plastic Surgeons. 2012 Plastic surgery statistics report [Internet] Arlington Heights, IL: American Society of Plastic Surgeons; 2015. [July 19, 2013]. Available from: http://www.plasticsurgery.org/news-and-resources/2012-plastic-surgery-statistics.html. [Google Scholar]
- 15.Quan M, Fadl A, Small K, et al. Defining pseudoptosis (bottoming out) 3 years after short-scar medial pedicle breast reduction. Aesthetic Plast Surg. 2011;35:357–364. doi: 10.1007/s00266-010-9615-6. [DOI] [PubMed] [Google Scholar]
- 16.Tepper OM, Small KH, Unger JG, et al. 3D analysis of breast augmentation defines operative changes and their relationship to implant dimensions. Ann Plast Surg. 2009;62:570–575. doi: 10.1097/SAP.0b013e31819faff9. [DOI] [PubMed] [Google Scholar]
- 17.Mentor. Mentor memory gel silicone gel-filled breast implants product insert data sheet [Internet] Santa Barbara, CA: Mentor; 2014. [July 19, 2013]. Available from: http://www.fda.gov/downloads/MedicalDevices/ProductsandMedicalProcedures/ImplantsandProsthetics/BreastImplants/UCM245623.pdf. [Google Scholar]
- 18.Eriksen C, Stark B. Early experience with the crescent expander in immediate and delayed breast reconstruction. Scand J Plast Reconstr Surg Hand Surg. 2006;40:82–88. doi: 10.1080/02844310500410344. [DOI] [PubMed] [Google Scholar]
- 19.Tepper OM, Karp NS, Small K, et al. Three-dimensional imaging provides valuable clinical data to aid in unilateral tissue expander-implant breast reconstruction. Breast J. 2008;14:543–550. doi: 10.1111/j.1524-4741.2008.00645.x. [DOI] [PubMed] [Google Scholar]
- 20.Wilhelmi BJ, Blackwell SJ, Mancoll JS, et al. Creep vs. stretch: a review of the viscoelastic properties of skin. Ann Plast Surg. 1998;41:215–219. doi: 10.1097/00000637-199808000-00019. [DOI] [PubMed] [Google Scholar]
- 21.Mustoe TA, Bartell TH, Garner WL. Physical, biomechanical, histologic, and biochemical effects of rapid versus conventional tissue expansion. Plast Reconstr Surg. 1989;83:687–691. doi: 10.1097/00006534-198904000-00015. [DOI] [PubMed] [Google Scholar]
- 22.Zeng YJ, Xu CQ, Yang J, et al. Biomechanical comparison between conventional and rapid expansion of skin. Br J Plast Surg. 2003;56:660–666. doi: 10.1016/s0007-1226(03)00217-0. [DOI] [PubMed] [Google Scholar]
- 23.Vegas MR, Martin Del Yerro JL. Stiffness, compliance, resilience, and creep deformation: understanding implant-soft tissue dynamics in the augmented breast: fundamentals based on materials science. Aesthetic Plast Surg. 2013;37:922–930. doi: 10.1007/s00266-013-0197-y. [DOI] [PubMed] [Google Scholar]
- 24.Zehm S, Puelzl P, Wechselberger G, et al. Inferior pole length and long-term aesthetic outcome after superior and inferior pedicled reduction mammaplasty. Aesthetic Plast Surg. 2012;36:1128–1133. doi: 10.1007/s00266-012-9938-6. [DOI] [PubMed] [Google Scholar]
- 25.Kaufman D. Pocket reinforcement using acellular dermal matrices in revisionary breast augmentation. Clin Plast Surg. 2012;39:137–148. doi: 10.1016/j.cps.2012.02.001. [DOI] [PubMed] [Google Scholar]