Abstract
Aims:
The aim was to compare the recession coverage outcomes when done macrosurgically and microsurgically.
Background:
Increasing interest in esthetics and the related problems such as hypersensitivity and root caries have favored the development of many root coverage procedures. Recession coverage up to a certain extent has solved these problems, but these procedures need good maintenance after the surgery for long-term benefits. With increasing advances in the field of recession coverage, microscope has added another dimension in undertaking the surgical procedure.
Materials and Methods:
Thirty Miller's Class I and II recession were treated using the sub-epithelial connective tissue graft from the palate. In 15 sites, the graft was placed at the recipient site with unaided eye (Group A) and in other 15 sites the graft was placed using surgical microscope (Group B). Clinical evaluation was done at baseline, 12 weeks and 24 weeks postoperatively using plaque index, gingival index, vertical recession (VR), probing depth, clinical attachment level (CAL), width of attached gingiva, papilla height (PH) and width, malalignment index (MI) and esthetic appearance.
Statistical Analysis Used:
Paired and unpaired Student's t-test along with Wilcoxon Z-test were used to analyze the results and probability of P < 0.05 were accepted to reject the null hypothesis. Pearson correlation was used to correlate two parameters such as VR and CAL and MI and VR.
Results:
Both the techniques demonstrated predictable mean root coverage (Group A 61.78% and Group B 67.58%) at 6 months postsurgery. CAL gain was slightly better in Group B patients when compared to Group A patients. A moderate positive correlation for Group A while a mild correlation in Group B was seen between the MI and VR.
Conclusion:
The use of the microscope enhances the results, but obtaining an expertise in using needs a lot of practice. The periodontal healing by both techniques should be evaluated histologically.
Keywords: Microsurgery, mucogingival surgery, recession, sub-epithelial connective tissue graft
INTRODUCTION
Cosmetic dental surgery goes beyond the face and body to improve the appearance of one's smile and boost confidence. Along with esthetic restorative procedures periodontal plastic surgery makes a major contribution to create a perfect smile. The color match, esthetic appearance and healing of the donor area with primary intention and consequent reduction in postoperative morbidity makes sub-epithelial connective tissue graft one of the most preferred procedures in recession coverage.[1]
Most of the dental treatment historically has been performed with the unaided eye without the use of visual magnification. In recent times, the introduction of the surgical microscope has greatly improved the outcome of dental procedures and the use of microsurgery for periodontal plastic procedures seem to be a natural progression. Along with improved visual acuity periodontal microsurgery also lays emphasis on passive wound closure with the use of microsurgical instruments and sutures. Precise incision and reduced trauma to the tissues results inaccurate approximation and less inflammation and pain[2] and consequently improved wound healing environment.
Over the years, various modifications to the original technique have been developed and this is evident in the smooth hand movements accomplished with increased precision and reduced physiologic tremor. The present study was performed to clinically compare and examine the two different techniques of sub-epithelial connective tissue graft for root recession coverage, that is, graft placement done microsurgically and macrosurgically. Although both the techniques used in this study were effective in predictable root coverage, microsurgical methodology provided a more predictive outcome owing to better vascularization.[3]
MATERIALS AND METHODS
This split-mouth randomized controlled clinical trial was conducted according to guidelines of Helsinki declaration of 1975 revised in 2000.
A total of 7 subjects (6 males and 1 female) with 30 bilateral sites of Miller Class I and Class II gingival recession participated in the study. The study was carried from December 2011, the recruitment of the first patient, to August 2013, the final evaluation of the last patient. The patients were healthy adults selected from the outpatient Department of Periodontology and Oral Implantology at D. A. V. Centenary Dental College and Hospital, Yamunanagar, Haryana. This included three sites per group in 2 patients, 2 sites per group in 4 patients and 1 site per group in 1 patient, that is, a total of 15 sites per group. A complete clinical and radiographic evaluation was performed. Complete medical and dental histories were obtained. Patients selected were 18-67 years old having bilateral isolated or multiple Miller's Class I or Class II gingival recession ≥2 mm when measured from cementoenamel junction (CEJ) on anterior teeth or premolars and malalignment score of up to 4.[4] Teeth selected were vital with no bleeding on probing, clinical indication and/or patient request for recession coverage and sites with an identifiable CEJ. Patients with systemic disease/condition, drugs that could have affected the periodontium and/or affected the outcome of the periodontal surgical procedure, surgically treated areas within the last 2 years, allergies to drugs used during the procedure utilized for the study and roots with restoration were excluded from the study. Patients unable to achieve the optimum level of oral hygiene and current smokers and to use any form of tobacco were also excluded from the study.
At the start of the surgical appointment, bilateral defects were randomly assigned by coin toss to the test group (microsurgical group) and control group (macrosurgical method).[5]
The sites in the study consisted of:
Group A: Recession coverage done with macrosurgical procedure
Group B: Recession coverage done with microsurgical procedure.
This study was evaluated by the board of studies and approved by the ethical committee of Pt. B. D. Sharma University of Health Sciences, Rohtak, Haryana, India.
At the first appointment, all the patients were instructed about the etiology of gingival recession, the natural history of periodontal disease and oral hygiene instructions. The patient allotment was done as explained by the flowchart [Figure 1].
Figure 1.
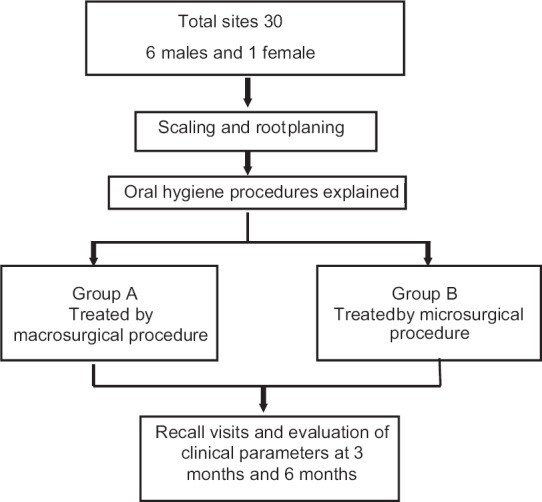
Diagrammatic representation of the study design
Clinical parameters evaluated were plaque index (PI)[6] with the amount of plaque present, Gingival index (GI)[7] as explained by Loe and Silness, vertical recession (VR): Defined as the distance from CEJ to the free gingival margin at the mid buccal level, probing depth the distance from the free gingival margin to the base of the pocket, clinical attachment level (CAL) was the distance from CEJ to the base of the pocket, width of attached gingiva (WAG) was the difference between the CEJ-mucogingival junction and the CEJ-pocket depth, papilla height (PH)[8] was measured from the apex of the papilla parallel to the long axis of the involved tooth to the most apical point of the CEJ (APCEJ), papilla width (PW)[8] was measured along the line connecting the most APCEJ of the involved tooth to the APCEJ of the adjacent mesial and distal teeth. The average value of mesial and distal measurements was calculated and recorded. Both pailla height and width were measured using a divider and a scale. Malalignment index (MI),[4] a comprehensive and objective index, wherein the correlation of proclination and rotation (mesial/distal) of the mandibular/maxillary anterior teeth with the success of root coverage procedures and esthetic appearance.[9] They assessed the esthetic results of the treatment upon three parameters that is, scar appearance marginal profile, papillae appearance whereas no consideration was given to the amount of recession coverage achieved. We assigned the scores for the above parameters on the following scale:
Unsatisfactory outcome
Good outcome
Excellent outcome.
The aforesaid parameters were evaluated at baseline (just prior to surgery), at 12 weeks and at 24 weeks postoperatively.
Surgical procedure
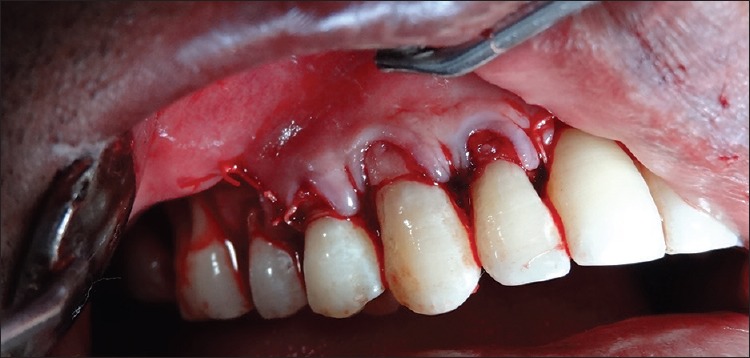
The surgical procedure was performed under aseptic conditions. Area selected for surgery was anaesthetized by utilizing local anesthesia, 2% xylocaine [Figures 2, 3]. A partial thickness flap, with two vertical incisions placed at least one-half to one tooth wider mesio-distally than the area of gingival recession and placement of connective tissue graft, retrieved from palate to recipient was done according to the Langer and Langer technique.[10] The recipient site flap was then directly sutured over the graft with 4-0 silk sutures for Group A. The overlying flap covered the donor tissue as much as possible to provide the dual blood supply to the graft [Figures 4, 5]. A mild compression with gauge soaked with sterile saline solution was done for 5 min to minimize the clot thickness. The palatal wound closure was done with 4-0 silk in both the groups.
Figure 2.

Preoperative Photograph of site treated with macrosurgical procedure
Figure 3.

Preoperative photograph for patient treated with macrosurgical method of recession coverage
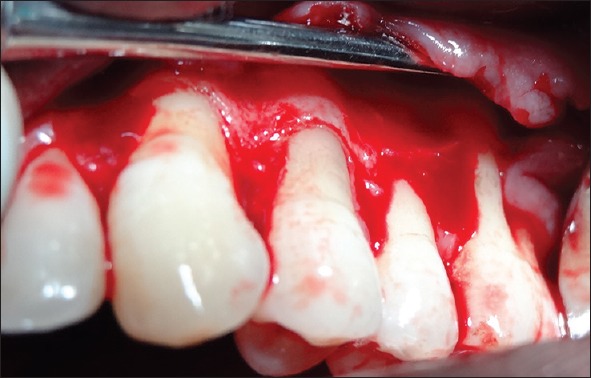
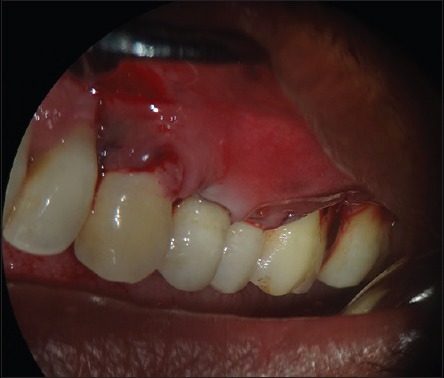
Figure 4.

Intraoperative picture showing the graft secured to the recipient site
Figure 5.
Final suturing of the flap
In Group B patients [Figures 6, 7], apart from using a surgical microscope (Enforte) at a magnification of 10X and 6-0 vicryl sutures (Johnson and Johnson, Maharashtra, India) for graft stabilization and final wound closure, the surgical procedure was kept similar [Figures 8, 9].
Figure 6.

Preoperative photograph of site treated with microsurgical procedure
Figure 7.

Preoperative photograph for patient treated with microsurgical method of recession coverage
Figure 8.
Intraoperative picture showing the prepared recipient site
Figure 9.
Final suturing of the flap as viewed under microscope of ×10 magnification
Postsurgical instructions
Patients were advised to rinse with 0.2% chlorhexidine gluconate twice daily, avoid chewing in surgical area during healing period and refrain from all mechanical plaque control methods in and around the surgical areas for 4-6 weeks. They were prescribed amoxycillin LB 500 mg 3 times daily for 7 days and nonsteroidal antiinflammatory drug's like ibuprofen 400 mg. At the 10th day sutures were removed, and professional tooth cleaning was performed to remove plaque and material alba.
Statistical analysis
The results of this study were analyzed by the paired and unpaired Student's t-test and Wilcoxon Z-test and the probability of P < 0.05 were accepted to reject the null hypothesis. Pearson correlation was used to establish a correlation between parameters. The value was evaluated calculated as “r” where
0 < |r| <0.3: Weak correlation
0.3 < |r| <0.7: Moderate correlation
|r| > 0.7: Strong correlation.
RESULTS
Thirty sites of gingival recession were treated: 15 with macrosurgical procedure (Group A) and 15 with microsurgical procedure (Group B). The groups were matched for age, gender and other parameters at the baseline. In Group A, the mean preoperative recession was between 2 and 6 mm (3.87 ± 1.41), whereas in Group B, preoperative recession ranged from 3 to 6 mm (4.07 ± 0.96) [Graph 1]. Both the techniques demonstrated predictable mean root coverage (Group A 61.78% and Group B 67.58%) at 6 months postsurgery.
Graph 1.
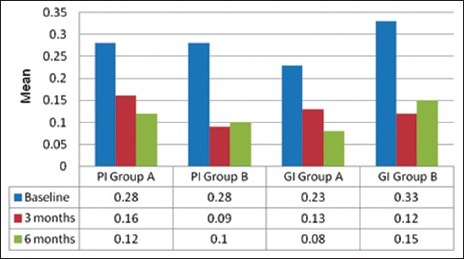
The comparison of plaque and gingival index scores at different time intervals
Complete root coverage was obtained for 3 sites in Group A (20%) and 4 sites in the Group B (26.67%). While as there was no significant difference in the CAL gain between Group A and Group B patients, the values were slightly better in Group B patients when compared to Group A patients (4.9-2.47 [Group A] and 5.60-2.47 [Group B]).
DISCUSSION
The PI and GI scores were kept <30% at baseline and all subsequent intervals. With the improvement in the gingival contour subsequent to recession coverage, the PI and GI scores improved further at 3-6 months intervals. Compared to Group A [Figure 10], the Group B presented with better root coverage at 6 months follow-up [Figure 11]. While as >5 patients showed, a recession coverage of 65-75% root coverage in Group B patients and it was 50-60% for Group A in a similar number of patients. More sites in Group B showed complete and >65% root coverage because of the use of finer suture that led to better approximation of the flap. The results of the study indicated that improved blood supply during early wound healing may be essential and improve the percentage of root coverage as explained by Burkhardt and Lang.[3]
Figure 10.

Six months postoperative photograph for the macrosurgical group
Figure 11.

Six months postoperative photograph for the microsurgical group
The improvement in CAL was statistically significant from baseline to 3 months and baseline to 6 months in both groups, although not much change was observed between 3 month and 6-month period. This implies that the attachment gets established at 3 months, and there is no further improvement thereafter. It has been histologically established that the attachment of the graft to the root surface is mediated by a combination of the epithelial down growth and connective tissue attachment.[11] Harris[12] reported the formation of a long junctional epithelium or a short junctional epithelium with a long connective tissue attachment that did not appear to insert into the cementum, as no regeneration of bone or cementum was observed [Graph 2].
Graph 2.
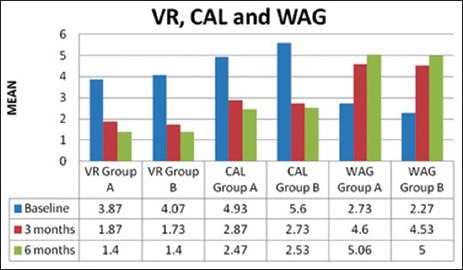
The comparison of various parameters at different time intervals
The correlation between VR and CAL substantiated the CAL gain with a reduction in VR for both the groups. In both groups, a strong positive correlation was found at end of 3 month and 6-month recall period. All these correlations were statistically significant[13] [Graph 3].
Graph 3.
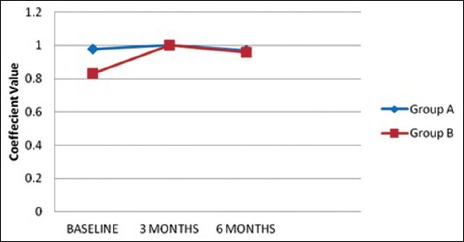
Pearson correlation graph between vertical recession and clinical attachment level
There was a statistically highly significant increase in the measurements of WAG for both the groups from baseline to 3 months and baseline to 6 months [Graph 2]. However, this difference was statistically nonsignificant when intergroup comparisons were done.
Although there was a significant reduction of PH in Group B from baseline to 3 months, it was observed that the patients having a PH of >5 mm resulted in complete root coverage when compared with those with inadequate height.[7]
In Group B, a statistically significant improvement in PW from baseline to 3 months when compared with Group A where a reduction in this parameter was observed. This could result due to maintenance of a better vascularization in Group B patients owing to improved approximation under the surgical microscope.[14]
In our study, also a moderate positive correlation was seen between the MI and VR for Group A while a mild correlation existed between these variables in Group B [Graph 4]. A greater MI score implies a thinner gingiva and consequently compromised vascularization that could have resulted in less than desired effects for Group A patients.[10,14,15]
Graph 4.
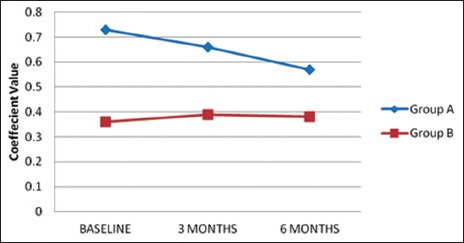
Pearson correlation graph between vertical recession and malalignment index
Evaluation of the esthetic appearance was done by three blinded examiners who subjectively evaluated the presurgical and postsurgical pictures at 12 weeks and 24 weeks postoperatively. They assessed the esthetic results of the treatment with regard to scar appearance, marginal profile and papillae appearance, giving no consideration to recession coverage achieved.[9] Better esthetic outcomes were observed in Group B, when compared to Group A. However, the difference was not statistically significant.
High magnification and proper instrumentation, although allowing greater precision during surgical procedures, cannot by themselves eliminate all possible causes of failure related to mucogingival treatment. The failures may simply be related to the patient's lack of compliance postsurgically or other unpredictable events, irrespective of the use of the microscope. Although both the techniques used in this study were effective in predictable root coverage, in certain situations, one technique may offer the advantage over another technique. The microsurgical procedure requires expertise as far as ergonomics is concerned and the pros and cons should be carefully evaluated to select the best technique. The histological evaluation of the periodontal healing by microsurgical and macrosurgical technique should be undertaken to understand the flap to root attachment.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Sedon CL, Breault LG, Covington LL, Bishop BG. The subepithelial connective tissue graft: Part I. Patient selection and surgical techniques. J Contemp Dent Pract. 2005;6:146–62. [PubMed] [Google Scholar]
- 2.Tibbets LS, Shanelec D. Principles and practice of periodontal microsurgery. Int J Microdent. 2009;1:13–24. [Google Scholar]
- 3.Burkhardt R, Lang NP. Coverage of localized gingival recessions: Comparison of micro – And macrosurgical techniques. J Clin Periodontol. 2005;32:287–93. doi: 10.1111/j.1600-051X.2005.00660.x. [DOI] [PubMed] [Google Scholar]
- 4.Pandit N, Gaba AK, Malik R, Pandit IK. A new index proposed for determination of outcome of recession coverage procedures. Clin Adv Periodontics. 2012;2:49–55. [Google Scholar]
- 5.Nart J, Valles C, Mareque S, Santos A, Sanz-Moliner J, Pascual A. Subepithelial connective tissue graft in combination with a coronally advanced flap for the treatment of Miller Class II and III gingival recessions in mandibular incisors: A case series. Int J Periodontics Restorative Dent. 2012;32:647–54. [PubMed] [Google Scholar]
- 6.Silness J, Loe H. Periodontal disease in pregnancy. II. Correlation between oral hygiene and periodontal condtion. Acta Odontol Scand. 1964;22:121–35. doi: 10.3109/00016356408993968. [DOI] [PubMed] [Google Scholar]
- 7.Loe H, Silness J. Periodontal disease in pregnancy. I. Prevalence and severity. Acta Odontol Scand. 1963;21:533–51. doi: 10.3109/00016356309011240. [DOI] [PubMed] [Google Scholar]
- 8.Haghighati F, Mousavi M, Moslemi N, Kebria MM, Golestan B. A comparative study of two root-coverage techniques with regard to interdental papilla dimension as a prognostic factor. Int J Periodontics Restorative Dent. 2009;29:179–89. [PubMed] [Google Scholar]
- 9.Francetti L, Del Fabbro M, Calace S, Testori T, Weinstein RL. Microsurgical treatment of gingival recession: A controlled clinical study. Int J Periodontics Restorative Dent. 2005;25:181–8. [PubMed] [Google Scholar]
- 10.Langer B, Langer L. Subepithelial connective tissue graft technique for root coverage. J Periodontol. 1985;56:715–20. doi: 10.1902/jop.1985.56.12.715. [DOI] [PubMed] [Google Scholar]
- 11.Guiha R, el Khodeiry S, Mota L, Caffesse R. Histological evaluation of healing and revascularization of the subepithelial connective tissue graft. J Periodontol. 2001;72:470–8. doi: 10.1902/jop.2001.72.4.470. [DOI] [PubMed] [Google Scholar]
- 12.Harris RJ. Successful root coverage: A human histologic evaluation of a case. Int J Periodontics Restorative Dent. 1999;19:439–47. [PubMed] [Google Scholar]
- 13.Andrade PF, Grisi MF, Marcaccini AM, Fernandes PG, Reino DM, Souza SL, et al. Comparison between micro – And macrosurgical techniques for the treatment of localized gingival recessions using coronally positioned flaps and enamel matrix derivative. J Periodontol. 2010;81:1572–9. doi: 10.1902/jop.2010.100155. [DOI] [PubMed] [Google Scholar]
- 14.Cairo F, Mervelt J, Cincinelli S, Franceschi D, Rotundo R, Pini Prato GP. The use of operative microscope in periodontal plastic surgery. A case series. J Parodontol Implantol Orale. 29:281–89. [Google Scholar]
- 15.Burkhardt R, Hürzeler MB. Utilization of the surgical microscope for advanced plastic periodontal surgery. Pract Periodontics Aesthet Dent. 2000;12:171–80. [PubMed] [Google Scholar]


