Abstract
Burning mouth syndrome (BMS) is a complex disorder that is characterized by warm or burning sensation in the oral mucosa without changes on physical examination. It occurs more commonly in middle-aged and elderly women and often affects the tip of the tongue, lateral borders, lips, hard and soft palate. This condition is probably of multi-factorial origin, often idiopathic, and its etiopathogensis is unknown. BMS can be classified into two clinical forms namely primary and secondary BMS. As a result, a multidisciplinary approach is required for better control of the symptoms. In addition, psychotherapy and behavioral feedback may also help eliminate the BMS symptoms.
KEY WORDS: Burning mouth syndrome, harmones, patch test
Burning mouth syndrome (BMS) refers to chronic orofacial pain without any visible mucosal changes or lesions such as stomatodynia, glossodynia, neuropathic pain, glossopyrosis and scalded mouth syndrome.[1] It is characterized mainly by an intense burning or stinging including nutritional deficiencies, hormonal changes associated with xerostomia, menopause, local oral infections, denture-related lesions, hypersensitivity reactions, and a number of systemic conditions including diabetes mellitus.[1] The International Association for the Study of Pain and International Headache Society defines it as a “distinctive nosological entity, including ‘all forms of burning sensation in the mouth with stinging sensation or pain, in an oral mucosa that appears clinically normal in the absence of local or systemic diseases or alterations.”[2] BMS is seen more commonly in postmenopausal women [Table 1].[3]
Table 1.
Clinical characteristics and etiologies of burning mouth syndrome
Epidemiology
The prevalence rate of BMS ranges from 0.7% to 4.6% of general population. The prevalence of BMS increases with age among both sexes, but not in children or in teenagers. It mainly affects females in the fifth to sixth decades of life.[4] The true cause BMS remains unknown. BMS clinical conditions include geographic tongue, candidiasis, hypo salivation, parafunctional habits, diabetes and adverse effects of drugs.[5]
Pathogenesis
Burning mouth syndrome is poorly understood. Origin includes variety of factors such as local, systemic and psychological factors like stress, anxiety and depression.[6] Salivary gland dysfunction plays an important role in BMS.[7]
Classification and subtypes
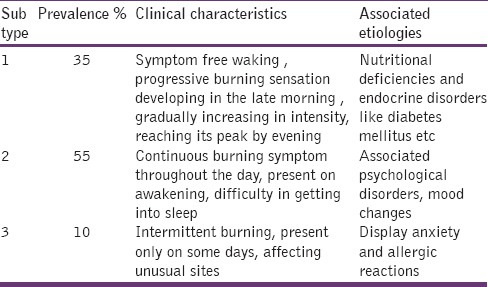
Lamey and Lewis have suggested classifying BMS into three subtypes according to variations in daily fluctuations of symptoms.
Lamey and Lewis classification of BMS.[8]
Scala et al. classified BMS into two categories namely ‘Primary or idiopathic’ BMS, in which local or systemic causes cannot be identified, but involving peripheral or central neuropath logical pathways. “Secondary” BMS, resulting from local, systemic or psychological factors.[7] The neurogenic factors differ in these subgroups, and will require different treatment modalities.[9]
Clinical Features
More common in females than males. In females peri and postmenopausal, parafunctional activities are increased, pain may vary, difficulty in speaking, nausea, gagging, head ache, shoulder pain. In oral cavity, unexplained pain and burning sensation of the soft tissues, xerostomia, painful teeth, TMJ disorder, muscular dystrophies in jaws, geographic tongue, mucosa appears normal, altered taste sensation.[1]
Diagnosis
Diagnosis of BMS is based on following steps:
To rule-out history of pain
To check through clinical examination
Information on previous or current psychosocial and psychological well-being
To measure salivary flow rates and taste function
Neurological imaging and examine the pathology and degenerative disorders
Oral cultures to confirm suspected infections
Patch test for allergic individuals
Gastric reflux studies
Hematological test to rule out nutritional, hormonal, autoimmune conditions.[8]
Treatment
Burning mouth syndrome patients shown great response in long-term therapy and attitude.[10] If any local, systemic or psychological factors are evident, to treat or eliminate. Clinical examination is crucial for the diagnosis of BMS patients. Management of BMS can be broadly discussed under three topics namely topical medications, systemic medications and behavioral interactions. Medications used for BMS include antidepressants, analgesics, antiepileptic, antifungal, antibacterial, sialagogues, antihistamines, anxiolytics, antipsychotics and vitamin, mineral, and hormonal replacements.[8]
Topical medications
The topical application of clonazepam (by sucking a tablet of 1 mg), 3 times a day for 14 days can reduce the burning symptoms without causing side effect of its systemic.[11] Aloe Vera gel helps to reduce the burning sensation and pain in the sore areas of the tongue with a protector.[12]
Systemic medication
Anti-depressants like amitriptyline, imipramine, clomipramine and nortriptyline are useful in treating BMS, and some authors contraindicate these drugs as worsen the condition in patients with dry mouth.[8]
Alpha-lipoic acid acts as an anti-oxidant and powerful neuroprotective agent that prevent nerve damage and regenerating other antioxidants such as vitamin C and E, thereby reducing the symptoms.[13] The patient must be advised to take medications for gastric protection.[14] Hormonal replacement therapy can reduce the burning symptoms and pain in peri and postmenopausal women.[15]
Behavioral Interventions
Multidisciplinary approach has been the beneficiary in some individuals. In addition combined therapy of psychotherapy and psycho-pharmacotherapy may also help to eliminate the BMS symptoms.[16]
Conclusion
Burning mouth syndrome is a difficult and challenging problem for the dental practitioners. The key to successful management is a good diagnostic work-up and co-ordination between the dental practitioners, psychologist and physician.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.Sunil A, Mukunda A, Gonsalves MN, Basheer AB, Deepthi An overview of burning mouth syndrome. Indian J Clin Pract. 2012;23:145–52. [Google Scholar]
- 2.Dodick DW, Matharu MS, May A, Olesen J. Vol. 24. UK: The International Classification of Headache Disorders; 2004. Cephalalgia; pp. 9–160. [DOI] [PubMed] [Google Scholar]
- 3.Klasser GD, Fischer DJ, Epstein JB. Burning mouth syndrome: Recognition, understanding, and management. Oral Maxillofac Surg Clin North Am. 2008;20:255–71. doi: 10.1016/j.coms.2007.12.012. vii. [DOI] [PubMed] [Google Scholar]
- 4.Aggarwal A, Panat SR. Burning mouth syndrome: A diagnostic and therapeutic dilemma. J Clin Exp Dent. 2012;4:e180–5. doi: 10.4317/jced.50764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Spanemberg JC, Rodríguez de Rivera Campillo E, Salas EJ, López López J. Burning Mouth Syndrome: Update. Oral Health Dent Manag. 2014;13:418–24. [PubMed] [Google Scholar]
- 6.Barker KE, Savage NW. Burning mouth syndrome: An update on recent findings. Aust Dent J. 2005;50:220–3. doi: 10.1111/j.1834-7819.2005.tb00363.x. [DOI] [PubMed] [Google Scholar]
- 7.Scala A, Checchi L, Montevecchi M, Marini I, Giamberardino MA. Update on burning mouth syndrome: Overview and patient management. Crit Rev Oral Biol Med. 2003;14:275–91. doi: 10.1177/154411130301400405. [DOI] [PubMed] [Google Scholar]
- 8.Aravindhan R, Vidyalakshmi S, Kumar MS, Satheesh C, Balasubramanium AM, Prasad VS. Burning mouth syndrome: A review on its diagnostic and therapeutic approach. J Pharm Bioallied Sci. 2014;6:S21–5. doi: 10.4103/0975-7406.137255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Jääskeläinen SK. Path physiology of primary burning mouth syndrome. Clin Neurophysiol. 2012;123:71–7. doi: 10.1016/j.clinph.2011.07.054. [DOI] [PubMed] [Google Scholar]
- 10.Bergdahl J, Anneroth G, Perris H. Cognitive therapy in the treatment of patients with resistant burning mouth syndrome: A controlled study. J Oral Pathol Med. 1995;24:213–5. doi: 10.1111/j.1600-0714.1995.tb01169.x. [DOI] [PubMed] [Google Scholar]
- 11.Gremeau-Richard C, Woda A, Navez ML, Attal N, Bouhassira D, Gagnieu MC, et al. Topical clonazepam in stomatodynia: A randomised placebo-controlled study. Pain. 2004;108:51–7. doi: 10.1016/j.pain.2003.12.002. [DOI] [PubMed] [Google Scholar]
- 12.López-Jornet P, Camacho-Alonso F, Molino-Pagan D. Prospective, randomized, double-blind, clinical evaluation of Aloe vera Barbadensis, applied in combination with a tongue protector to treat burning mouth syndrome. J Oral Pathol Med. 2013;42:295–301. doi: 10.1111/jop.12002. [DOI] [PubMed] [Google Scholar]
- 13.Granot M, Nagler RM. Association between regional idiopathic neuropathy and salivary involvement as the possible mechanism for oral sensory complaints. J Pain. 2005;6:581–7. doi: 10.1016/j.jpain.2005.03.010. [DOI] [PubMed] [Google Scholar]
- 14.Buchanan J, Zakrzewska J. Burning mouth syndrome. Clin Evid. 2005;14:1685–90. [PubMed] [Google Scholar]
- 15.Forabosco A, Criscuolo M, Coukos G, Uccelli E, Weinstein R, Spinato S, et al. Efficacy of hormone replacement therapy in postmenopausal women with oral discomfort. Oral Surg Oral Med Oral Pathol. 1992;73:570–4. doi: 10.1016/0030-4220(92)90100-5. [DOI] [PubMed] [Google Scholar]
- 16.Sun A, Wu KM, Wang YP, Lin HP, Chen HM, Chiang CP. Burning mouth syndrome: A review and update. J Oral Pathol Med. 2013;42:649–55. doi: 10.1111/jop.12101. [DOI] [PubMed] [Google Scholar]


