Abstract
The word rapid prototyping (RP) was first used in mechanical engineering field in the early 1980s to describe the act of producing a prototype, a unique product, the first product, or a reference model. In the past, prototypes were handmade by sculpting or casting, and their fabrication demanded a long time. Any and every prototype should undergo evaluation, correction of defects, and approval before the beginning of its mass or large scale production. Prototypes may also be used for specific or restricted purposes, in which case they are usually called a preseries model. With the development of information technology, three-dimensional models can be devised and built based on virtual prototypes. Computers can now be used to create accurately detailed projects that can be assessed from different perspectives in a process known as computer aided design (CAD). To materialize virtual objects using CAD, a computer aided manufacture (CAM) process has been developed. To transform a virtual file into a real object, CAM operates using a machine connected to a computer, similar to a printer or peripheral device. In 1987, Brix and Lambrecht used, for the first time, a prototype in health care. It was a three-dimensional model manufactured using a computer numerical control device, a type of machine that was the predecessor of RP. In 1991, human anatomy models produced with a technology called stereolithography were first used in a maxillofacial surgery clinic in Viena.
KEY WORDS: Computed tomography, computer-aided designing, medical resonance imaging, prototypes, rapid prototyping, stereolithography
The term rapid prototyping (RP) designates a set of technologies that allow the realization of automatic physical models based on design data, all through the aid of a computer. These “three-dimensional printers” allow designers to quickly generate defined prototypes of their designs, rather than the simple two-dimensional images. These Prototypes of such achievements provide valuable visual aids. The shift from the visual to the visual-tactile representation of physical objects introduced a new kind of interaction called “touch to comprehend”. In the early days of RP, automotive and aerospace industries dominated the RP application. But this is no longer the case as RP has spread into many other industries.
It has revolutionized the engineering and science, by integrating itself into many aspects of the modern life from entertainment through medicine. It all started in the 70s, when it spreads a new method of medical information based X-ray, that is, the tomographic examination or computerized tomography (CT). RP technologies are a new approach for surgical planning and simulation. They reproduced anatomical objects as three-dimensional physical models, which give the surgeon a realistic impression of complex structures before a surgical intervention.
The need of facing the geometrical complexity has introduced RP into the dental field. It has the potential to become the next generation in fabrication methods in dentistry. Beyond its known contribution related with the diagnosis, education, and surgical planning. This technology is being used in wide areas of dentistry including prosthodontics.
The emergence of the RP technology into prosthodontics has innovated the clinical and laboratory procedures by eliminating or abolishing some intermediate stages and independing the quality of the outcomes from the practitioners skills. This indicates the potential of the new method, which is capable of replacing the traditional “impression-taking and waxing” procedure. RP methods are used to substantially shorten the time for developing patterns, molds, and prototypes. There are many different RP technologies available.
However, the field of RP is still new with much effort to be expanded on improving the speed, accuracy and reliability of the system and widen the range of materials for prototype construction. So the clinician should be aware of potential areas for inaccuracies within models and review the source image in cases where models integrity is in doubt. Another area of improvement will be the cost efficiency as most RP systems are currently too expensive to be affordable.
Basic Principle
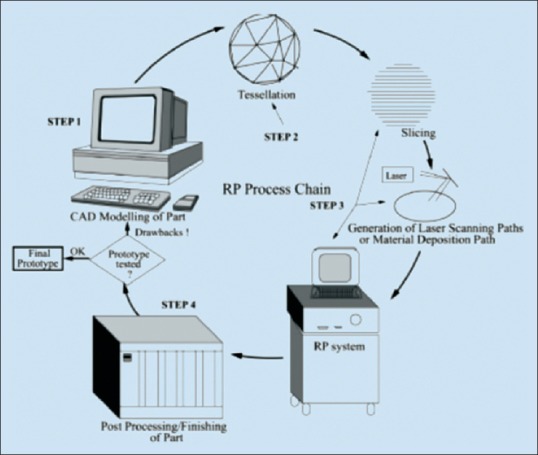
The key idea of this new RP technology is based on the decomposition of three-dimensional computer models in the layers section transverse thin, followed physically forming layers and piling layer by layer. The generation of three-dimensional objects in this manner is an idea almost as old as human civilization. The developments since the Egyptian pyramids were probably block developed layer by layer [Figure 1].[1]
Figure 1.
After basic principle
Classification of Rapid Prototyping Method
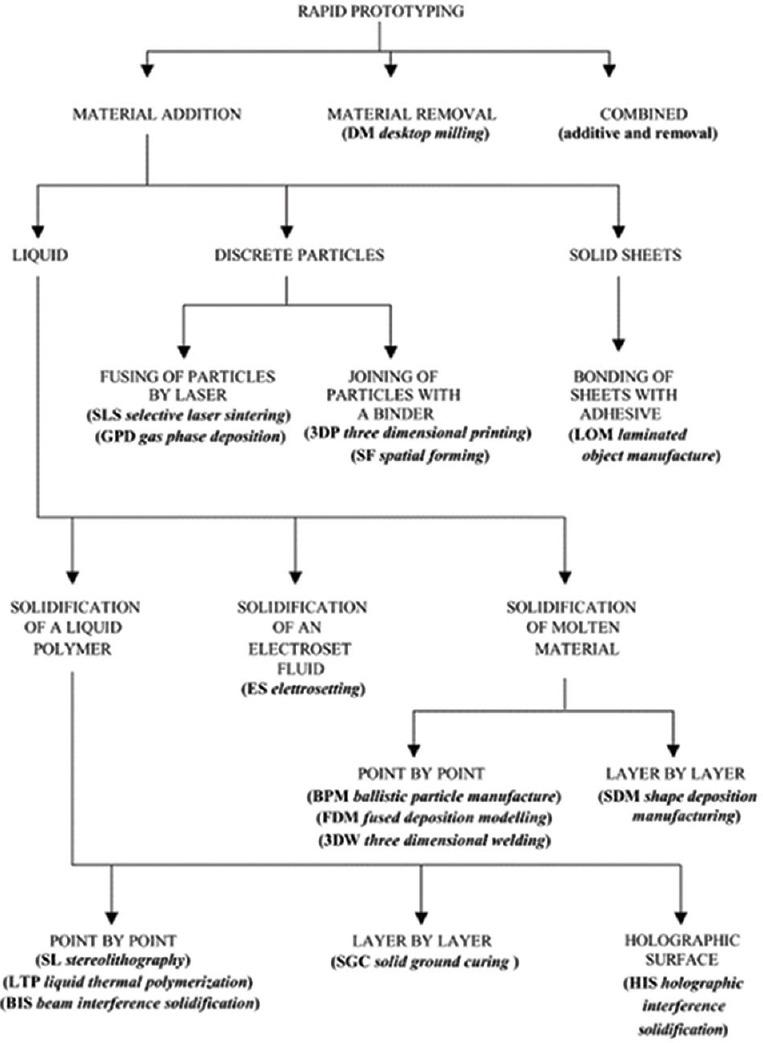
Rapid prototyping technologies may be divided broadly into those involving the addition of material and those involving its removal. According to Kurth, the materials accretion technologies may be divided by the state-of the prototype material before part formation. The liquid based technologies may entail the solidification of the resin on contact with a laser, the solidification of an electrosetting fluid, or the melting and subsequent solidification of prototyping material. The processes using powders compound them either with a laser or by the selective application of binding agent. Those processes that use solid sheets may be classified according to whether the sheets are bonded with a laser or with an adhesive [Figure 2].[1]
Figure 2.
After classification of rapid prototyping method
The most popular among currently available RP technologies is perhaps stereolithography and is the first commercially available rapid prototype. Stereolithography apparatus was invented by Charle Hull of 3D Systems Inc. This relies on a photosensitive monomer resin which from a polymer and solidifies when exposed to ultraviolet (UV) light. Due to the absorption and scattering of the beam this reaction only takes place near the surface. This produces parabolically cylindrical voxels which are characterized by horizontal line width and vertical cure depth. An stereolithography machine consists of a build platform (substrate) which is mounted in a vat of resin and a UV helium-cadmium or argon ion laser.[2] The first layer of the part is imaged on the resin surface by the using information obtained from the three-dimensional solid CAD model. Once the contour of the layer has been scanned, and the interior either hatched or solidly filled, the platform is next lowered to the base of the vat in order to coat the part thoroughly. It is then raised such that the top of the solidified part is level with the surface and a blade wipes the resin leaving exactly one layer of resin above the part. The part is then lowered to one layer below the surface and left until the liquid has settled. This is done to ensure a flat, even surface and to inhibit bubbles formation. The next layer may then be scanned.[3]
Medical Applications of Rapid Prototyping
Medical rapid prototyping is defined as the manufacture of dimensionally accurate physical models of human anatomy derived from medical image data using a variety of RP technologies.[4] Some RP machines had already been in experimental use in the 1970s, and CT was invented in the 1960s by Godfrey N Hounsfield, an electronics engineer, in collaboration with Allan McLeod Cormack, a physicist. However, it was only in the 1990s that an actual three-dimensional model was built to reproduce the anatomy of a patient based on CT images obtained during that patient's examination, thanks to advances in CT scanner quality and the development of specific software for this purpose. RP has been applied to a range of medical specialties, including oral and maxillofacial surgery, dental implantology, neurosurgery, and orthopedics.
Complex diseases in medicine often demand time-consuming surgery. Surgical planning tries to minimize the duration of surgery to reduce the risk of complications. In addition to the normally used imaging modalities, three-dimensional visualization techniques can be applied for supporting the planning process. Such visual representation of medical objects allows simulation of surgical procedures before surgery. The greatest advantage of RP technologies is the precise reproduction of objects from a three-dimensional medical image data set as a physical model which can be looked at and touched by the surgeon.[5]
Medical rapid prototyping is also being developed for use in dental implants. Greater accuracy was achieved with the use of rapid prototyped surgical guides for creating osteotomies in the jaw, and a computer-assisted design/computer-assisted manufacture (CAD/CAM) approach to the fabrication of partial dental frameworks has been developed.[4]
Dental Application of Rapid Prototyping
Orthodontics
Using state-of-the-art CAD/CAM technology, the two normally separate processes of bracket production and bracket positioning are fused into one unit. In this process, the demand for maximum individuality with simultaneously minimized space requirements is put consistently into practice.[6] Another innovative use of the CAD/CAM technology was to create an overcrown able to open the bite through clinical crown lengthening of the mandibular second premolars. Some technology provides clear plastic orthodontic treatment devices. Every one to 2 weeks, the patient receives a new set of splint-like aligners that are intended to continue moving their teeth.[7] This technology utilizes several stereolithography machines to fabricate models upon which plastic sheets are molded. Data sets are obtained by digitizing an impression taken of the patient's teeth. The resulting point sets are separated into individual tooth geometries, which are then positioned according to the orthodontist's treatment plan.
Oral Surgery
Anatomic medical models built with RP technologies represent a new approach for surgical planning and simulation. These techniques allow one to reproduce anatomical objects such as three-dimensional physical models of the skull or other structures, which give the surgeon a realistic impression of complex structures before surgical intervention. The shift from the visual to the visual-tactile representation of anatomical objects introduces a new kind of interaction called “touch to comprehend”.[2] Clinical data indicate that computer-aided RP may be of value in minimizing the extra-oral time and possible injury to transplanted teeth during the process of autotransplantation.[12]
Implantology
Since the advent of osseointegration, the use of dental implants has evolved rapidly over the last decade. Research in the field of oral implantology has led to refinements resulting in highly successful and predictable restorative options for partially as well as completely edentulous patients; however, improper implant placement can have a profound and often detrimental effect on the long-term predictability and success of the implant-supported prosthesis.[8]
The use of computer-aided design/computer-aided manufacturing (CAD/CAM) technology has gained popularity in implant dentistry. The applications pertain to three-dimensional imaging, 3D software (Delcan India, Maharashtra) for treatment planning, fabrication of computer-generated surgical guides using additive RP, as well as fabrication of all-ceramic restorations using subtractive RP.[13] RP technology allows for industrial fabrication of customized three-dimensional objects from computer-aided design (CAD) data.[9]
Maxillofacial Prosthesis
Absence of all or part of the external ear may be either acquired or congenital. When attempting to restore this part with prosthesis, the prosthesis should ideally be customized to restore the anatomy as closely as possible. In so doing, it may be helpful to have a priori knowledge of average values for each index and use these values to help construct prosthesis of the appropriate size and shape. However, individual proportion indices vary from the average, so where the defect is unilateral it is more practical to compare and duplicate proportions from the nondefect side.[10] This process can be difficult and time consuming and demands a high level of artistic skill to form a mirror image and achieve a good esthetic match. Similarly, patients with existing prostheses may need frequent replacements because of color changes, loss of fit, tearing, aging, contamination of the material and general wear. Conventional duplication procedures are often unreliable and inaccurate, as errors may occur at any one of many stages during production.[11]
The advent of CT and magnetic resonance imaging with three-dimensional representation of human anatomy has opened up new perspectives for design and production in the medical field computer manipulation of the data allows for mirroring or modifications to establish the exact dimensions needed, and a computer numeric controlled (CNC) milling machine can be used to manufacture a template for the final prosthesis. CNC milling, however, is limited by difficulties encountered when trying to replicate the complex anatomy of internal features.
The development of RP systems has led to the creation of customized three-dimensional anatomic models that exhibit a level of complexity unknown with CNC-based equipment, primarily because RP methodologies use an additive process of building an object in layers defined by a computer model that has been virtually sliced.[3] This allows for the production of complex shapes with internal detail and undercut areas. One such method is stereolithography, which produces three-dimensional objects by curing a liquid resin under a computer-guided laser. A newer system is the Thermojet Printer (3D Systems): Shenzhen Towell Model Technology Co., Ltd., Shenzhen, China, which operates as a network printer and uses wax as the building material. The advantage of such a system is the ability to cast directly from a wax model.
Applications in maxillofacial prosthodontics
Production of auricular and nasal prosthesis
Obturators
Duplication of existing maxillary/mandibular prosthesis especially crucial when an accurate fit to natural teeth or an osseointegrated implant is needed
Manufacturing of surgical stents for patients with large tumors scheduled for excision
Manufacturing of lead shields to protect healthy tissue during radiotherapy treatment
Fabrications of burn stents, where burned area can be scanned rather than subjecting delicate, sensitive burn tissue to impression-taking procedures.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.Pham DT, Gault RS. A comparision of rapid prototyping technologies. Int J Mach Tools Manuf. 1988;38:1257–87. [Google Scholar]
- 2.Xu F, Wong YS, Loh TH. Toward generic models for comparative evaluation and process selection in rapid prototyping and manufacturing. J Manuf Syst. 2000;19:283–96. [Google Scholar]
- 3.Yan X, Gu P. A review of rapid prototyping technology and systems. comput Aided Des. 1996;24:307–18. [Google Scholar]
- 4.Berry E, Brown JM, Connell M, Craven CM, Efford ND, Radjenovic A, et al. Preliminary experience with medical applications of rapid prototyping by selective laser sintering. Med Eng Phys. 1997;19:90–6. doi: 10.1016/s1350-4533(96)00039-2. [DOI] [PubMed] [Google Scholar]
- 5.Petzold R, Zeilhofer HF, Kalender WA. Rapid protyping technology in medicine – basics and applications. Comput Med Imaging Graph. 1999;23:277–84. doi: 10.1016/s0895-6111(99)00025-7. [DOI] [PubMed] [Google Scholar]
- 6.Wu G, Zhou B, Bi Y, Zhao Y. Selective laser sintering technology for customized fabrication of facial prostheses. J Prosthet Dent. 2008;100:56–60. doi: 10.1016/S0022-3913(08)60138-9. [DOI] [PubMed] [Google Scholar]
- 7.Chan DC, Frazier KB, Tse LA, Rosen DW. Application of rapid prototyping to operative dentistry curriculum. J Dent Educ. 2004;68:64–70. [PubMed] [Google Scholar]
- 8.Lal K, White GS, Morea DN, Wright RF. Use of stereolithographic templates for surgical and prosthodontic implant planning and placement. Part I. The concept. J Prosthodont. 2006;15:51–8. doi: 10.1111/j.1532-849X.2006.00069.x. [DOI] [PubMed] [Google Scholar]
- 9.Papaspyridakos P, Lal K. Complete arch implant rehabilitation using subtractive rapid prototyping and porcelain fused to zirconia prosthesis: A clinical report. J Prosthet Dent. 2008;100:165–72. doi: 10.1016/S0022-3913(08)00110-8. [DOI] [PubMed] [Google Scholar]
- 10.Sykes LM, Parrott AM, Owen CP, Snaddon DR. Applications of rapid prototyping technology in maxillofacial prosthetics. Int J Prosthodont. 2004;17:454–9. [PubMed] [Google Scholar]
- 11.Coward TJ, Watson RM, Wilkinson IC. Fabrication of a wax ear by rapid-process modeling using stereolithography. Int J Prosthodont. 1999;12:20–7. [PubMed] [Google Scholar]
- 12.Winder J, Bibb R. Medical rapid prototyping technologies: State of the art and current limitations for application in oral and maxillofacial surgery. J Oral Maxillofac Surg. 2005;63:1006–15. doi: 10.1016/j.joms.2005.03.016. [DOI] [PubMed] [Google Scholar]
- 13.Ruppin J, Popovic A, Strauss M, Spüntrup E, Steiner A, Stoll C. Evaluation of the accuracy of three different computer-aided surgery systems in dental implantology: Optical tracking vs. stereolithographic splint systems. Clin Oral Implants Res. 2008;19:709–16. doi: 10.1111/j.1600-0501.2007.01430.x. [DOI] [PubMed] [Google Scholar]


