Abstract
This paper presents an overview of mandibular advancement device (MAD). The primary purpose of MAD is to move the mandible forwards relative to maxilla in ordered to widen the airway to prevent to closure.
KEY WORDS: Mandibular advancement device, sleep apnea, snoring
Obstructive sleep apnea (OSA) is a condition wherein there is repetitive and intermittent occlusion of the upper airway (UA) during sleep.[1] This closure occurs due to inspiratory collapse of the pharyngeal walls. If complete closure occurs, it results in apnea; if partial closure occurs, hypopnea results. Although snoring occurs in majority of population, it has significant ramifications. If repetitive apnea occurs in a patient, many times a night, for years together, there will be considerable changes in the (1) nervous system (2) myocardial and cerebral circulation (3) pulmonary and systemic circulation.
Snoring is an expression of the pharyngeal narrowing. It is due to the vibration of the soft parts of the UA, that is, the pharyngeal walls, veils of the palate and the uvula. It is the commonest symptom reported by the patient or the spouse. The nocturnal signs are xerostomia, salivation, altered sleep – patterns, suffocative feeling. The daytime signs include irritability, headache, depression gastroesophageal reflux etc.
Principal and Professor, Sree Balaji Dental College, Bharath University
Postgraduate Student, Sree Balaji Dental College, Bharath University.
First description of this disorder was reported in 1965[2] and since then many treatments have been suggested. Treatment for OSA can be (1) continuous positive airway pressure (CPAP) (2) surgery (3) oral appliances.[3] While CPAP has been the treatment of choice, it needs sealed tubing and a power source connected device and use of mask interface. Hence, more often patients develop intolerance. Surgery may have serious side-effects like scarring in soft palate.
Mandibular advancement device (MAD) has been a novel method in the management of snoring and OSA. For mild to moderate sleep apnea, MADs have been a boon. A guideline published by American Academy of sleep Medicine in 1995 stated that MAD was indicated as first-line therapy for mild OSA and a second-line therapy for moderate to severe OSA.
In 1902, Pierre Robin proposed the use of a device (Monobloc), with the purpose of procuring a functional advancement of the jaw, dragging it forward to a more advanced position. Initial publications about oral appliances in the treatment of snoring appeared way back in 1980's. Currently, there are more than 50 types of devices used for treating snoring. There are two versions of MAD's.
Fixed advancement MAD
Adjustable advancement MAD.
The American Sleep Disorders Association defines MAD as a device which is introduced into the mouth and modifies the position of the jaw, the tongue and other supporting structures of the UA for the treatment of chronic snoring and OSA. They are considered a valid alternative, which can be the first choice in simple snorers, mild OSA patients, mild-moderate OSA with low body mass index, and patients suffering from the syndrome of increased resistance of the upper airway; and a second choice in patients who do not improve or cannot tolerate positive pressure devices, patients at high surgical risk and who react badly to surgical treatment.[4]
Aim
The aim of the MAD is to improve the patient's sleep quality as well as that of the relatives or roommates, by reducing or eliminating snoring and respiratory pauses during sleep.
Mechanism of mandibular advancement devices
Mandibular advancement devices carry out an anterior and inferior movement of the jaw, generating anatomical variations in the UA that enable an increase in the pharyngeal area.[1] This movement stabilizes and fixes the jaw and the hyoid bone, preventing the posterorotation of these structures during the decubitus, preventing blockage of the airway. Although its main effect appears in the velopharyngeal area, it has repercussions for all the pharyngeal segments. There is initially an increase in rigidity and a swelling of the space between the anterior and posterior pharyngeal pillars. The soft palate is displaced ventrally, and this increases the caliber of the lateral walls of the velopharyngeal area which are factors that drastically reduce snoring [Figure 1].
Figure 1.
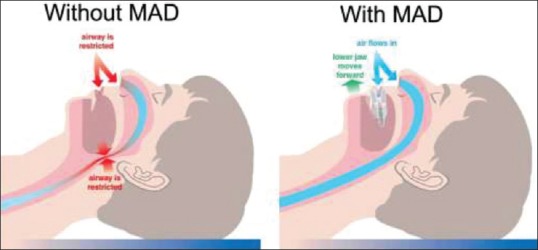
Mandibular advancement device with and without
Functional mandibular advancement induces changes in the position of the hyoid bone towards a more forward position. It creates a new position of balance of the suprahyoid musculature, which in turn, favors an increase in volume and permeability of the UA. The UA is widened particularly in its lateral dimension.[5] The pharyngeal fat pads relocate laterally from the airway and the tongue base muscles move anteriorly. This leads to a reduction in pharyngeal collapsibility.
Mandibular titration
The degree of mandibular advancement is an important modulator of the treatment outcome, since there is a dose-dependent effect on nocturnal oxygenation and pharyngeal collapsibility. A small advancement produces a less satisfactory effect, while too large an advancement produces more treatment effect. Excessive advancement produces more side-effects. Suggest that >75% of maximum protrusion is needed for a satisfactory effect. However, inappropriately large mandibular advancements should be avoided, since the long-term negative side-effects on occlusion and the temporomandibular joints are unknown. There is currently no agreement regarding the method for measuring and defining the degree of mandibular repositioning in the individual patient. A titration procedure millimeter by millimeter has, therefore, been recommended in order to achieve optimal results.[6]
A MAD is usually adjusted using a screw located in the mid-line, anteriorly or in the palate, or laterally with arms of different lengths or screws on both sides of the appliance. Some designs permit the opening of the mandible and some lateral movement, while others fixate the jaws more rigidly [Figure 2].
Figure 2.

Mandibular titration
Side-Effects of Mandibular Advancement Devices
Jaw pain, tenderness of teeth and hypersalivation have been reported. Some patients require an adaptation period which can extend for many months.[7]
Assessment of Mandibular Advancement
Polysomnographic analysis of the patients is currently used to evaluate the treatment outcome. It is also the equipment used to diagnose OSA.
Conclusion
Mandibular advancement device has proved to be a useful device in the treatment of snoring and OSA. In a normal person with simple snoring without any systemic illness, MAD can be suggested to the patient by the dentist or the chest physician. Nevertheless, in the case of severe OSA, cardio-respiratory evaluation must be done prior to treatment. Since, all patients cannot be treated by the modalities in vogue; there is a need to search for new treatment options. Also, long-term evaluation of MAD's must be undertaken to assess the efficacy.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.Rodríguez-Lozano FJ, Sáez-Yuguero Mdel R, Linares Tovar E, Bermejo Fenoll A. Sleep apnea and mandibular advancement device. Revision of the literature. Med Oral Patol Oral Cir Bucal. 2008;13:E549–54. [PubMed] [Google Scholar]
- 2.Gastaut H, Tassinari CA, Duron B. Polygraphic study of diurnal and nocturnal (hypnic and respiratory) episodal manifestations of Pickwick syndrome. Rev Neurol (Paris) 1965;112:568–79. [PubMed] [Google Scholar]
- 3.Lee CH, Mo JH, Choi IJ, Lee HJ, Seo BS, Kim DY, et al. The mandibular advancement device and patient selection in the treatment of obstructive sleep apnea. Arch Otolaryngol Head Neck Surg. 2009;135:439–44. doi: 10.1001/archoto.2009.31. [DOI] [PubMed] [Google Scholar]
- 4.Cobo JM, de Carlos F, Suarez AA. “Mandibular advancement device (MAD®) to treat sleep apnoea – Hypopnoea syndrome and chonic snoring”: 25th Southern Biomedical Engineering Conference 2009. IFMBE Proc. 2009;24:349–54. [Google Scholar]
- 5.Chan AS, Sutherland K, Schwab RJ, Zeng B, Petocz P, Lee RW, et al. The effect of mandibular advancement on upper airway structure in obstructive sleep apnoea. Thorax. 2010;65:726–32. doi: 10.1136/thx.2009.131094. [DOI] [PubMed] [Google Scholar]
- 6.Fleury B, Rakotonanahary D, Petelle B, Vincent G, Pelletier Fleury N, Meyer B, et al. Mandibular advancement titration for obstructive sleep apnea: Optimization of the procedure by combining clinical and oximetric parameters. Chest. 2004;125:1761–7. doi: 10.1378/chest.125.5.1761. [DOI] [PubMed] [Google Scholar]
- 7.Marklund M, Verbraecken J, Randerath W. Non-CPAP therapies in obstructive sleep apnoea: Mandibular advancement device therapy. Eur Respir J. 2012;39:1241–7. doi: 10.1183/09031936.00144711. [DOI] [PubMed] [Google Scholar]


