Abstract
The smartphone is one of the biggest revolutions in the era of information technology. Its built in camera offers several advantages. Dermatologists, who handle a specialty that is inherently visual, are most benefited by this handy technology. Here in this article, we attempt to provide an overview of smartphone photography in clinical dermatology in order to help the dermatologist to get the best out of the available camera for clinical imaging and storage
Keywords: Applications, apps, clinical photography, imaging, smartphone
INTRODUCTION AND BACKGROUND
Dermatology is a visual specialty, and clinical imaging is now considered to be an essential part of follow up and documentation. Virtually all dermatologists own a smartphone and many of them routinely use them for clinical photography. There is a high level of smartphone ownership and usage among medical students and junior doctors too.[1] A number of smartphone applications that offer valuable clinical utility are now available.[2,3] The ease of capturing and sharing images with a smartphone makes it useful in clinical photography.
A study has shown that dermatology registrars take clinical photographs mainly for five reasons: (1) To gain advice from peers/consultants; (2) for treatment and disease monitoring purposes; (3) for teaching/academic purposes; (4) to share with colleagues; and (5) for research and publication.[4] However, clinical photography using smartphones does not measure up to standard digital cameras in terms of image quality. This article discusses some of the important issues involved in using smartphones for clinical photography and also attempts to provide tips to optimize the use of smartphone cameras in clinical imaging.
WHAT IS A SMARTPHONE?
A smartphone is fundamentally a mobile phone, which can perform most of the functions of a computer, has a relatively larger screen, and has an operating system that can run a variety of applications [apps]. An “App” is a self-contained program or software designed to fulfill a particular purpose that can be downloaded and installed onto a mobile device to perform the action effectively.
The smartphone camera
Like the conventional digital camera, images are received in a digital format on the sensors and are saved on the built-in memory of the phone. The image quality may come close to that of the digital camera in terms of megapixel count, but the sensor size being physically small, the megapixel count cannot be equated to that of a digital camera. For example, a 10 megapixel sensor on an average smartphone camera produces an image, which has a much lower resolution compared with a 10 megapixel sensor on a digital single lens reflex (SLR) camera. Moreover, there is the issue of limitation of space in smartphones to accommodate other components such as lenses, apertures, and flash. Another major drawback is the absent or inadequate optical zoom. For dedicated digital cameras, for close-up images, lesions can be zoomed on using the optical zoom, thus avoiding lens distortion during closeup photography. Taking the camera too close to the lesions tends to produce a spherical distortion, which might look odd, especially in facial photographs [Figure 1]. Some newer smartphones are equipped with optical zooms ranging from 3 × to 10 × magnification (eg, Samsung Galaxy™ K zoom smartphone has a 10 × optical zoom). Newer smartphones also have an optical image stabilizer, which can be very handy to reduce shake and blurring of images. This also facilitates low light photography.
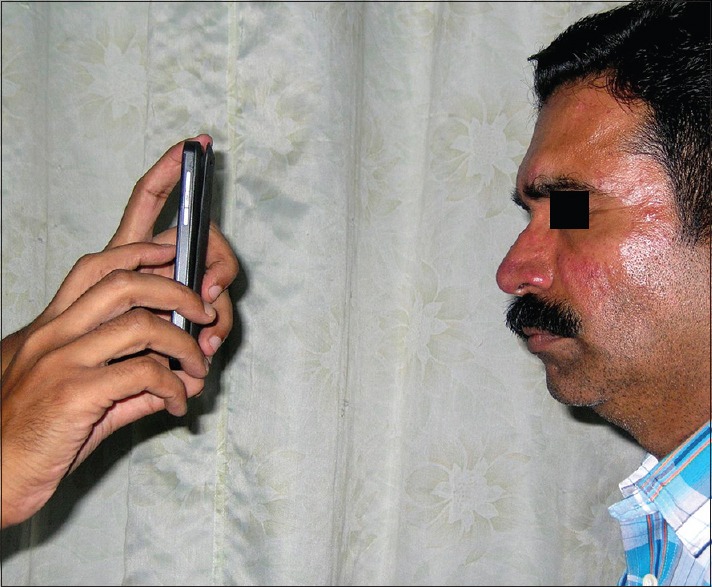
Figure 1.

A comparison of clinical images of the face of a patient with rosacea taken with a (a) BlackBerry Z10™ Smartphone camera 8MP and (b) a dedicated camera Nikon Cool Pix4MP. The image with the mobile phone is distinctly less sharp though it too conveys enough information about the nature of the lesions. The slight distortion of the facial shape is also noticeable with the mobile phone image
Clinical photography using smartphones: Is it different from normal clinical photography?
In clinical photography, essentially all the important rules of conventional and digital photography apply to smartphone photography as well. Here are some important points:
Ensure that a written consent is obtained from the patient prior to photography. This becomes more important for images of the face, tattoos, etc., where the identity is compromised
Maintain a distraction-free and consistent background. A plain light blue or green background is considered ideal. Because taking pictures with a smartphone is so easy, this point is often neglected
Take multiple images whenever possible; poor images can always be deleted later. Image previews on the large screen of the mobile phone may be deceptive. The true quality of the image can only be appreciated after the image is transferred to a computer and viewed on the computer monitor [Figure 2]. Also capture images from different angles. A minimum of two views are recommended: (1) from a distance showing the lesions in relation to the whole body/important anatomical structures, and (2) a close-up view showing the morphology of individual lesions
Lighting and positioning of the patient are the most important concerns in terms of ensuring consistency of images for follow up and documentation processes. A dedicated area of the clinic with fixed lighting conditions is ideal for clinical photography. In general it is better to use a flash (if available) at all times as it tends reduce image blur[6]
Ensure that proper focus is achieved and the lesion in question is properly focused on. Smartphones allow “touch focus” and one can tap on the lesion on screen to lock focus. It is important to remember that a blurred photograph is of no value in clinical photography.
Figure 2.

Images taken with (a) Compact camera and (b) Smartphone showing the blurriness of the image, which was not so evident on preview and hence deceptive on the large screen of the smartphone
How to operate a smart phone camera?
Always ensure that the phone is held firm with both hands and exposing is done with the index finger of the right hand (unless the operator is left handed). Ensure that you have used the highest resolution available to ensure that the photos look good even while viewing on a larger screen or in prints. It would be ideal to hold the smartphone parallel to the area of interest of the subject to avoid errors like improper angulation. The area of interest should be centred to the middle of the frame [Figure 3].
Figure 3.
Ideal positioning of the mobile phone for taking images of lesions over the face
Tripods are available in the market even for smartphones these days, which can be used for close-up photography [Figure 4a and b]. A simple method is to stabilize the lower edge of the phone on a flat surface such as a table (you can use books to increase the height of the base as needed).
Figure 4.

(a) Gorillapod, a very versatile and handy tool to avoid shake for close-up photography. Image accessed from http://commons.wikimedia.org/wiki/File:Gorillapod-with-camera.jpg (b) Monopod for smartphone. (Image Courtesy of Dr. Feroz K., Consultant Dermatologist, Skin Care Clinic, Kannur, Kerala, India)
While taking general views, it is better to turn the flash on, but it may be better turn it off when taking close-up shots as to avoid interference with the image quality in case of pigmented lesions. Unless otherwise indicated, it is important to include the point of interest in the middle of the frame. As mentioned before, it is always better to shoot multiple images with a consistent background so that the clinician does not regret capturing a bad image later.
Advantages of smartphone photography
The major advantage of clinical photography using smartphones is the ease of capturing and also transfer of images. The smartphone cameras in general are now well equipped to shoot in any kind of lighting. Because the smartphone is an indispensable gadget in our daily lives, it is like living with a camera 24 × 7. Bigger view finder and grids (that are also available on the smart phone screen) make it easy to frame and freeze the desired area of interest
Teledermatology and e-consultation: With the advantage of connectivity incorporated into the smartphones, sharing clinical images and obtaining any number of opinions from any corner of the globe in a jiffy is now a reality. Social networking apps such as WhatsApp®, Tango®, and Facebook® are such virtual worlds on the clinician's fingertips. Dermatologists working in remote and geographically inaccessible areas are now at ease as they have any number of opinions a few “share” away (sharing is the process of transmitting data on electronic media). Recent studies have shown the effectiveness of mobile phones in teledermatology consultations using such apps.[6] Mobile phones are particularly useful for patient-initiated teledermatology for follow up of chronic skin conditions, although it will probably never be a good enough replacement for a physical review. There are many clinical case discussion fora on Facebook in which a good percentage of images put up for discussion are taken using smartphones
Video photomicroscopy: This is one feature where the smartphone actually scores over the compact camera in clinical photography. It is easy to take real-time videos and transmit them using Internet connectivity.[7] The video feature in the smartphone can also be used for recording small dermatosurgical procedures and preserving them for posterity or using them for educational purposes
Saving space and time: The digital photography equipment can be heavy and cumbersome for a person on the move, which to a certain extent can be overcome by the camera embedded in the smartphone. With the live connectivity one can set the images to be uploaded to a cloud or backed up on the laptop on a day-to-day basis, thus precluding any loss of images due to accidental erasure or technical mishaps on the smartphone memory.
Patient-initiated photography: Some conditions on the body may not be visible to the patient; or he/she may not wish to be bared in the consulting room; or they may be evanescent or shortlived, occurring at odd times. In such situations, the patients can be taught to keep a record of the clinical situation. Even follow up of some conditions such as repigmentation of a vitiligo patch postoperatively can be very rewarding and encouraging for the patients themselves. Patients will be willing to share them with the clinician, saving time and resources on travel and other logistics.
Disadvantages and limitations of smartphone photography
The wide variation in the available camera resolution and the lens quality is an issue, which needs to be kept in mind when using smartphones for clinical photography. As mentioned before, high resolution of a smartphone camera in terms of megapixels does not equate to that of a dedicated camera with the same megapixel range. This is because of the smaller sensor size of the smartphone camera
Lack of consistent lighting is another drawback of smartphone photography. This becomes a major issue while shooting images of depigmented lesions such as vitiligo, nevus depigmentosus, or a hypopigmented patch in Hansen's disease [Figure 5]
Additional flexibility in terms of optical zoom, white balance, and exposure settings are not available in all smartphones.
Figure 5.
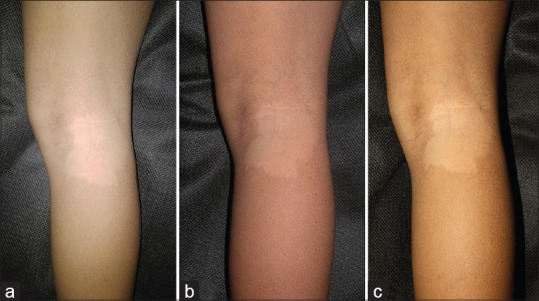
Images of a nevus depigmentosus patch in a child taken in auto flash mode. (a) Smartphone camera (BlackBerry Z10™) (b) CANON EOS™450D (c) NikonCoolPix™ 4800. The excessive “whiteness” of the lesion is evident in the image shot with the smartphone
Macro mode is not a standard feature in all the smartphone cameras, which is a limitation when taking close-up images. Even in smartphone cameras having a dedicated macro mode, the quality does not match up to that of the macro mode of dedicated cameras. Focusing an external light on the lesion can improve the quality of macro images taken with a smart phone with the flash off.
ADD-ONS/ACCESSORIES
Various add-ons are available in the software and hardware market to enhance the versatility of smartphone for clinical photography. One such very useful utility is a Handyscope® (FotoFinder systems GmbH), which can be attached to smartphones and serves the purpose of effective dermoscopy. These devices are especially useful in the context of e-dermoscopy or teledermoscopy, in which dermoscopic images can also be transmitted along with the clinical images for tele consultations.[8] The main drawback of this device in the context of its use in developing nations is the relatively high cost (starting from approximately 35,000INR/700USD). Moreover, most of these devices are compatible with only one particular make of smartphones, limiting their utility. The authors had developed a simple effective tool to use any smartphone camera as a cheap and effective alternative for mobile dermoscopy.[9]
Attachable external macro lenses are also available for smartphones and these can be theoretically useful in taking close-up views of skin lesions. However, the quality of the image is nothing near that of dedicated macro lenses for digital SLR cameras and we would not recommend the same for routine clinical photography using smartphones. At present, even add-on LED lights are available, which can increase the capability of the phone camera in low light situations.
A useful product combining different accessories is the mCAMLITE® made by Action Life Media, which combines a tripod, accessory mounts, and accessory lenses in an aluminum frame body, which can be customized for most modern smartphones. Details are available at: http://www.actionlifemedia.com/mcam.
CAUTION AND CARE OF IMAGES IN SMARTPHONES
If you are using your smartphone regularly for clinical imaging, use the external memory card not less than 2 GB at least. Also it is ideal to transfer the images to other sources such as the computer, external hard disks, or cloud storage periodically at least at weekly intervals to be on the safer side of a system crash, which is common in some of the smartphones despite of the best operating system being in place. In most of the smartphones, the images are either set by the user or the machine to be stored in the memory card. One has to be very careful while giving the smartphones for repair or service as we often forget to remove the memory card unlike in the digital camera. Even erasure is not necessarily final as there are advanced softwares that can retrieve images from memory cards even if they are deleted. Recuva® a freeware available from www.recuva.com is one such utility to retrieve erased images. So it is always advisable to remove the memory cards from smartphone whenever they are given for repair or resold. There is always a possibility (although remote) for misuse of images, which is a violation of trust and privacy of the patient.
ETHICAL AND LEGAL ISSUES
The misuse of clinical photography has become an area of growing concern among medical indemnity agencies.[10] It is always desirable to take a consistent and cautious approach to clinical imaging. Obtaining valid informed consent from patients or informants and also maintaining adequate medical records and providing secure systems for data storage will help the clinicians to ensure patient confidentiality and maintain a sound patient-clinician relationship. It also protects practitioners from possible disciplinary and medicolegal litigations.[4] Patients who allow clinicians to share their images among clinicians to aid in the diagnosis should be given the assurance that their confidentiality will be preserved. The clinicians receiving images for a second opinion are bound by the same ethical and legal regulations as those taking the images.[4,11] The smartphones being a pocket computer may have various other apps installed, which at the time of installation take the owner's permission to even access images in the phone, raising phone security and privacy concerns. This possibility also should not be neglected or taken lightly.
SOME USEFUL APPS FOR SMARTPHONE PHOTOGRAPHY IN DERMATOLOGY PRACTICE
ClinPix is an app, which we found to be very useful for storing and organizing clinical photographs. It is primarily intended for physicians, especially in specialties such as dermatology, who need to keep track of skin lesions. However, it might be useful to anyone wanting to securely store photographs on his or her smartphone and keep them organized for clinical use. Details are available at: http://play.google.com/store/apps/details?id = com.dermvision.clinpix
AppwoRx is another useful application for clinical photography with special features such as anatomy cataloging, integration with electronic medical records, and “photoghosting” (using previous patient photos as an outline to ensure consistent followup images). Details are available at: http://myappworx.com/rxphoto
PicSafeMedi is an app for secure sharing of medical images among doctors. Details are available at: http://picsafe.com/medi
Camera + and Camera awesome [Figure 6]: These apps enhance the feature set of a smartphone camera by providing advanced settings such as splitting the focus and exposure. Details are available at: http://itunes.apple.com/in/app/camera+/id329670577?mt = 8
Snapseed and Photoshop Express are editing apps that can be useful for advanced editing such as changing the exposure, white balance, sharpness, cropping, and so forth. Details are available at: http://play.google.com/store/apps/details?id = com.niksoftware.snapseedandhl = en and http://itunes.apple.com/in/app/snapseed/id439438619?mt = 8
Magnifier app [Figure 7]. This app allows images to be magnified upto three times (3×) allowing the clinician to visualize the subject in greater detail. Details are available at: http://itunes.apple.com/in/app/magnifying-glass-light-digital/id406048120?mt = 8
Figure 6.

Camera+ app screenshot: Allows advanced controls such as independent focus and exposure
Figure 7.
Screenshot of the Magnifier app: Allow up to 3×-4× magnification and image capture
We would like to quote a paragraph verbatim from JAMA Dermatology (erstwhile Archives of Dermatology), which we feel holds true for smartphone photography in clinical practice. “Though the technology of medical photography has evolved tremendously from the early pinhole cameras of the 1800s to the digital cameras of today, proper image composition to demonstrate the disease or clinical process of the patient without distraction remains a timeless art. No technological innovation can substitute for proper image composition. Innovations in photographic technology are simply tools to help the clinician photographer more rapidly and efficiently capture and process the image, whether properly composed or not. Ultimately, though, composition is still in the hands of the clinical photographer.”[12]
DISCLAIMER
A lot of research and literature review has gone into the preparation of this article and utmost care has been taken to ensure the correctness of the information provided in the article. We do not have affiliation to any manufacturer or developer [software or hardware] and we shall not be responsible for any consequences thereof. The readers are requested to thoroughly screen the information and look for reviews prior to purchasing or installing any software on their smartphones or handheld devices.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared
REFERENCES
- 1.Payne KB, Wharrad H, Watts K. Smartphone and medical related App use among medical students and junior doctors in the United Kingdom (UK): A regional survey. BMC Med Inform Decis Mak. 2012;12:121. doi: 10.1186/1472-6947-12-121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Franki OI. Smartphone apps for orthopaedic surgeons. Clin Orthop Relat Res. 2011;469:2042–8. doi: 10.1007/s11999-011-1904-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Vinekar A, Gilbert C, Dogra M, Kurian M, Shainesh G, Shetty B, et al. The KIDROP model of combining strategies for providing retinopathy of prematurity screening in underserved areas in India using wide-field imaging, tele-medicine, non-physician graders and smart phone reporting. Indian J Ophthalmol. 2014;62:41–9. doi: 10.4103/0301-4738.126178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kunde L, McMeniman E, Parker M. Clinical photography in dermatology: Ethical and medico-legal considerations in the age of digital and smartphone technology. Australas J Dermatol. 2013;54:192–7. doi: 10.1111/ajd.12063. [DOI] [PubMed] [Google Scholar]
- 5.Kaliyadan F, Manoj J, Venkitakrishnan S, Dharmaratnam AD. Basic digital photography in dermatology. Indian J Dermatol Venereol Leprol. 2008;74:532–6. doi: 10.4103/0378-6323.44334. [DOI] [PubMed] [Google Scholar]
- 6.Kaliyadan F, Amin TT, Kuruvilla J, Ali WH. Mobile teledermatology--patient satisfaction, diagnostic and management concordance, and factors affecting patient refusal to participate in Saudi Arabia. J Telemed Telecare. 2013;19:315–9. doi: 10.1177/1357633X13501778. [DOI] [PubMed] [Google Scholar]
- 7.Górgolas M, Cuadros J. Images in clinical medicine. Video Photomicroscopy. N Engl J Med. 2014;371:e4. doi: 10.1056/NEJMicm1105786. [DOI] [PubMed] [Google Scholar]
- 8.Kroemer S, Frühauf J, Campbell TM, Massone C, Schwantzer G, Soyer HP, et al. Mobile teledermatology for skin tumour screening: Diagnostic accuracy of clinical and dermoscopic image tele-evaluation using cellular phones. Br J Dermatol. 2011;164:973–9. doi: 10.1111/j.1365-2133.2011.10208.x. [DOI] [PubMed] [Google Scholar]
- 9.Kaliyadan F, Ashique KT. A simple and cost-effective device for mobile dermoscopy. Indian J Dermatol Venereol Leprol. 2013;79:817–9. doi: 10.4103/0378-6323.120740. [DOI] [PubMed] [Google Scholar]
- 10.Mahar D, Foley P, Sheed-Finck A, Baker CS. Legal considerations of consent and privacy in the context of clinical photography in Australian medical practice. Med J Aust. 2013;198:48–9. doi: 10.5694/mja12.11086. [DOI] [PubMed] [Google Scholar]
- 11.Scheinfeld N. Photographic images, digital imaging, and the law. Arch Dermatol. 2004;140:473–6. doi: 10.1001/archderm.140.4.473. [DOI] [PubMed] [Google Scholar]
- 12.Bhatia AC. The clinical image: Archiving clinical processes and an entire specialty. Arch Dermatol. 2006;142:96–8. doi: 10.1001/archderm.142.1.96. [DOI] [PubMed] [Google Scholar]


