Abstract
Background:
Direct immunofluorescence (DIF) test for tissue-bound autoantibodies, has been found to be of value in the diagnosis of several dermatological disorders. The location and pattern of deposition of immunoreactants helps in classifying various immune-mediated diseases.
Aims and Objectives:
The aim of this study was to analyze the concordance between the clinical, histopathological and DIF diagnosis in bullous and nonbullous lesions of the skin, and thus determine the impact of immunofluorescence on diagnosis.
Materials and Methods:
A total of 215 skin biopsies performed in suspected immune-mediated vesiculobullous disease, vasculitis or dermatosis, were studied. Histopathological examination was done along with DIF study for deposits of immunoglobulin G(IgG), IgA, IgM, and C3.
Results:
Direct immunofluorescence was positive in 103/215 cases. There was very good concordance between the clinical, histological and DIF results (observed agreement = 93.4%, κ =0.90, with 95% confidence interval = 0.86–0.94). The overall sensitivity of DIF in immune-mediated skin disorders was 98.0%. DIF was positive in 52/53 cases (98.1%) in the pemphigus group and 24/25 (96.0%) bullous pemphigoid cases. None of the clinically suspected cases of dermatitis herpetiformis showed DIF positivity. A positive lupus band test was seen in 9/9 (100%) cases of lupus erythematosus. DIF was positive in 10/10 (100%) clinically suspected cases of Henoch–Schönlein purpura. In 110 cases, negative DIF results helped to rule out immune-mediated vesiculobullous disorders, lupus erythematosus and vasculitis, and the final diagnosis was made on the basis of the clinical features and/or histopathology.
Conclusion:
Direct immunofluorescence is a useful supplement for the accurate diagnosis of immune-mediated dermatological disorders, and helps to classify various autoimmune bullous disorders. When the clinical features/histopathology are inconclusive, the diagnosis often can be made on the basis of the DIF findings alone. A combination of the clinical features, histopathology and DIF usually gives the best results.
Keywords: Direct immunofluorescence, interface dermatitis, skin biopsy, systemic lupus erythematosus, vasculitis, vesiculobullous lesions
INTRODUCTION
Autoimmune cutaneous vesiculobullous diseases are rare, varying in incidence from 0.5 to 3.2 cases/100,000 population/year.[1] On account of their rarity and heterogeneous symptoms, these diseases often pose a major diagnostic challenge. It is essential to rapidly and accurately establish the diagnosis of vesiculobullous disorders in order to plan proper treatment and define a prognosis. Direct immunofluorescence (DIF) test for tissue-bound autoantibodies provides a useful adjunct for the diagnosis of autoimmune bullous disorders, helping to classify histologically similar conditions which differ in their treatment protocols and prognosis. In addition, DIF in conjunction with histopathology, can be a useful supplement to clinical and histological examination in the diagnosis of a variety of other dermatological diseases which include connective tissue disorders, vasculitides, and conditions such as lichen planus and sometimes, psoriasis.[2] DIF also aids in monitoring response to therapy and predicting relapse.[2] By DIF, the presence of immune complexes in the skin biopsy at various locations such as intraepidermal, the dermo-epidermal junction (DEJ), dermal blood vessels, etc., helps to arrive at a diagnosis.[3,4] The aim of this study conducted in the South Indian population was to analyze the concordance between the clinical, histopathological and DIF diagnosis in bullous and nonbullous lesions of the skin, and thus determine the contribution of immunofluorescence in diagnosing these conditions.
MATERIALS AND METHODS
This cross-sectional study was done on a total of 215 consecutive cases received in the Department of Pathology over a three-year period. The clinical data was provided by the consultants from the Department of Dermatology. The skin biopsies in these cases, were submitted to establish or rule out a diagnosis of immune-mediated vesiculobullous disease, vasculitis or dermatosis. For every patient, two samples of biopsy tissue were processed, one for histopathology and the other for DIF. In all cases, biopsy for histopathology was drawn from a representative skin lesion, fixed in 10% formalin and subjected to conventional histopathological study with hematoxylin and eosin staining. In cases of suspected autoimmune bullous disorders, the biopsy for DIF was taken from the perilesional skin, while in other conditions, it was taken from the lesional skin. The tissue for DIF was put in saline and transported to the pathology laboratory immediately. Transport medium (Michel's medium) was not required for any of the cases, as transit time for the samples was minimal.
For the frozen sections, skin biopsy specimens were embedded in optimal cutting temperature (OCT) medium and 4 micron-thick sections were cut on a cryostat. A minimum of 10 sections were cut for each case. Two sections were taken on each slide and the slides were dipped in cold acetone for 5 min. The slides were either stained immediately or stored at –20°C before staining. For staining, sections were brought to room temperature, air dried, washed with phosphate-buffered saline (PBS) at pH 7.4 for 10 min, and layered with fluorescein isothiocyanate (FITC)-conjugated rabbit antihuman immunoglobulin G(IgG), IgA, IgM, and C3 (dilution 1:20). These slides were incubated for 2 h in a moist chamber at room temperature. The sections were then washed with PBS for 10 min, mounted in buffered glycerine, and viewed under a fluorescence microscope.
The DIF results were recorded by taking into consideration the nature of the immune deposits (IgG/IgA/IgM/C3); the location of the immune deposits (intercellular spaces in epidermis/DEJ or basement membrane zone-(BMZ)/subepidermal blood vessels/colloid bodies, etc.); the extent (focal/diffuse); the intensity of fluorescence (+ to ++++); and the pattern of immune complex deposits (granular/linear).[5]
The definite diagnoses were based on a combination of the clinical, histopathological and immunofluorescence findings.
Statistical methods
The data was entered in MS excel and was analyzed using statistical package for the social sciences (SPSS) version 18.0 (SPSS Inc.'s). To test for concordance between the clinical, histopathological and DIF diagnosis, Cohen's Kappa statistics was used. To test for the difference between paired proportions viz. between the clinical and histopathological diagnosis, between the clinical and DIF diagnosis, and between the histopathological and DIF diagnosis, McNemar's test was used. Sensitivity was calculated for DIF and histopathology. P < 0.05 was considered statistically significant.
RESULTS
Of the 215 cases studied, 98 were males and 117 females (male: female = 1:1.2). The age of the patients ranged from 2 to 94 years. Table 1 shows the distribution of the various skin disorders studied. Table 2 enumerates the clinical, histological, DIF, and final diagnosis of 102 immune-mediated skin disorders that were encountered.
Table 1.
Distribution of the various skin disorders studied (n = 215)
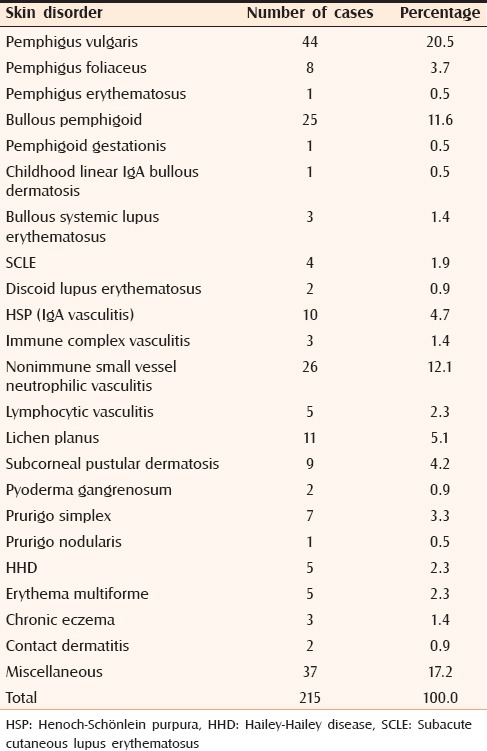
Table 2.
Clinical, histological and DIF diagnosis and the final diagnosis in the 102 immune-mediated skin disorders
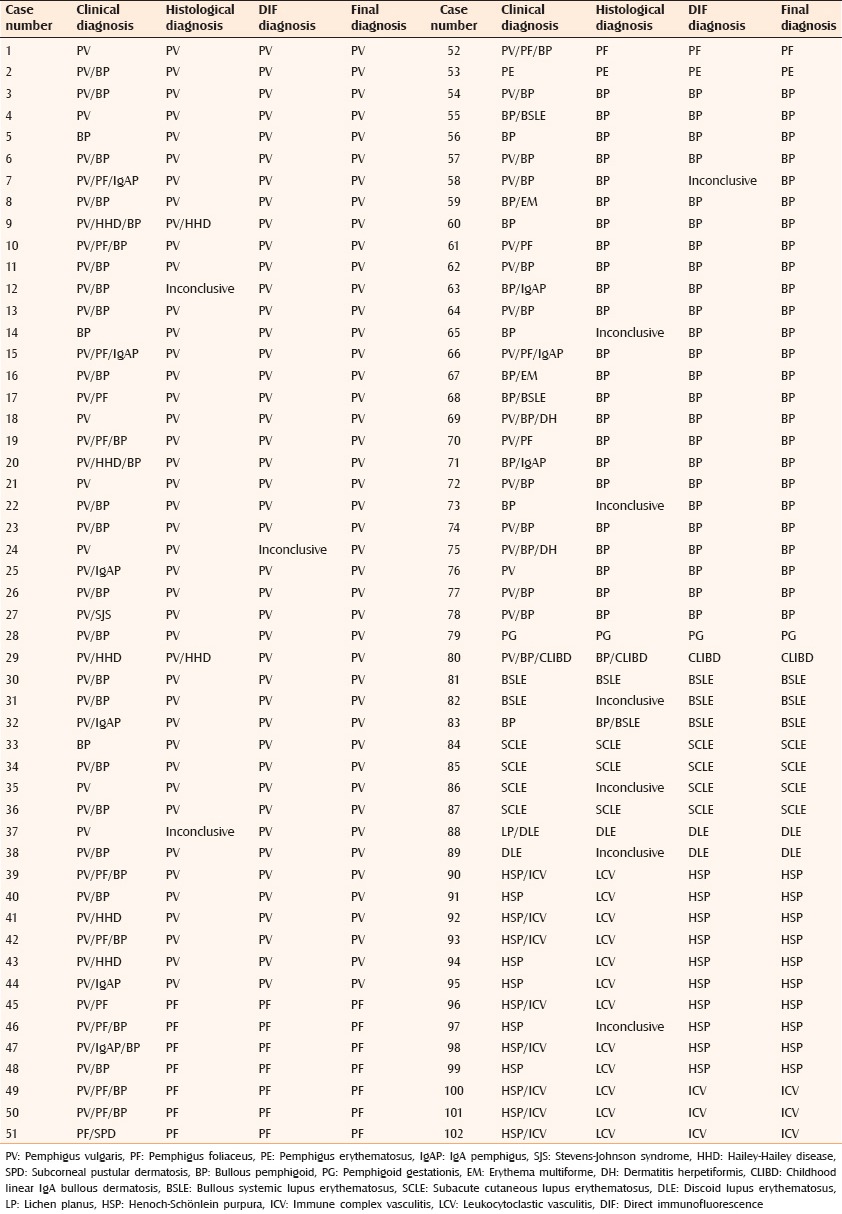
The clinico-histological, clinico-immunological and histological-immunological concordance was tested using McNemar's test of significance. It was found that histopathology and DIF gave comparable results, that is, the difference in results by the two methods was not statistically significant (P = 0.109, combined sensitivity = 92%). The clinical and histopathology results were also comparable. The difference in results by the two methods was not statistically significant (P = 0.1815, combined sensitivity = 89%). Comparison of the clinical and DIF results (clinico-immunological concordance), showed P value of 0.152, and combined sensitivity of 91%, which again indicated good concordance. Kappa statistics was used to compare the clinico-histological-immunological concordance. There was a very good agreement between these three methods (observed agreement = 93.4%, κ =0.90, with 95% confidence interval = 0.86–0.94).
Table 3 shows the histopathological and DIF results in 102 cases of immune-mediated skin disorders. Only 2 of these cases – one each of pemphigus vulgaris and bullous pemphigoid – showed a negative DIF result despite classical clinical and histopathological features. Thus, DIF was positive in 103 cases (100 immune-mediated skin disorders and 3 lichen planus), and negative in 112 cases. DIF was taken as the gold standard since the results were consistent. There were no false-positive DIF results. Thus, the overall sensitivity of DIF in immune-mediated skin disorders was 98.0%. Histopathology was conclusive in 94/102 (92.2%) cases. In 8/102 (7.8%) cases [Table 3], histopathology was not very contributory to the diagnosis, and only DIF could give the accurate diagnosis. Thus, the overall sensitivity of histopathology in immune-mediated skin disorders was 92.2%. Table 4 shows the sensitivity of DIF and histopathology in the common immune-mediated skin disorders. Table 5 summarizes the DIF results in the 103 DIF-positive cases.
Table 3.
Histopathological and direct immunofluorescence results in immune-mediated skin disorders (total=102, DIF positivity=100/102)
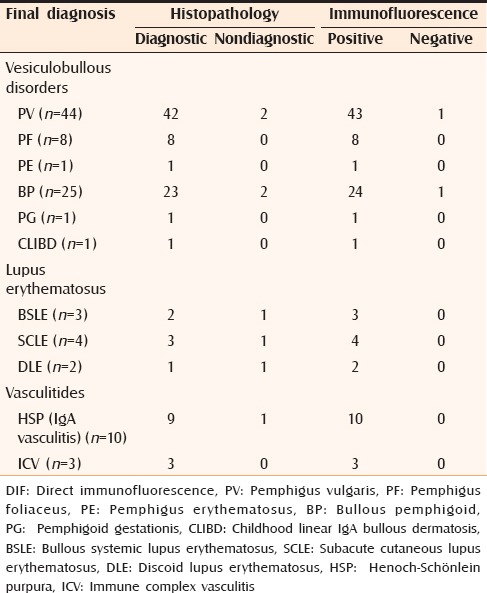
Table 4.
Sensitivity of DIF and histopathology
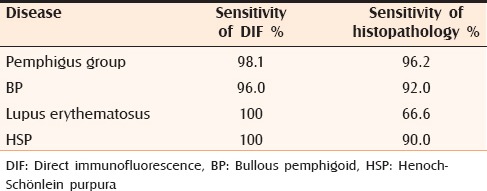
Table 5.
Direct immunofluorescence results in the various direct immunofluorescence-positive skin disorders (total=103)
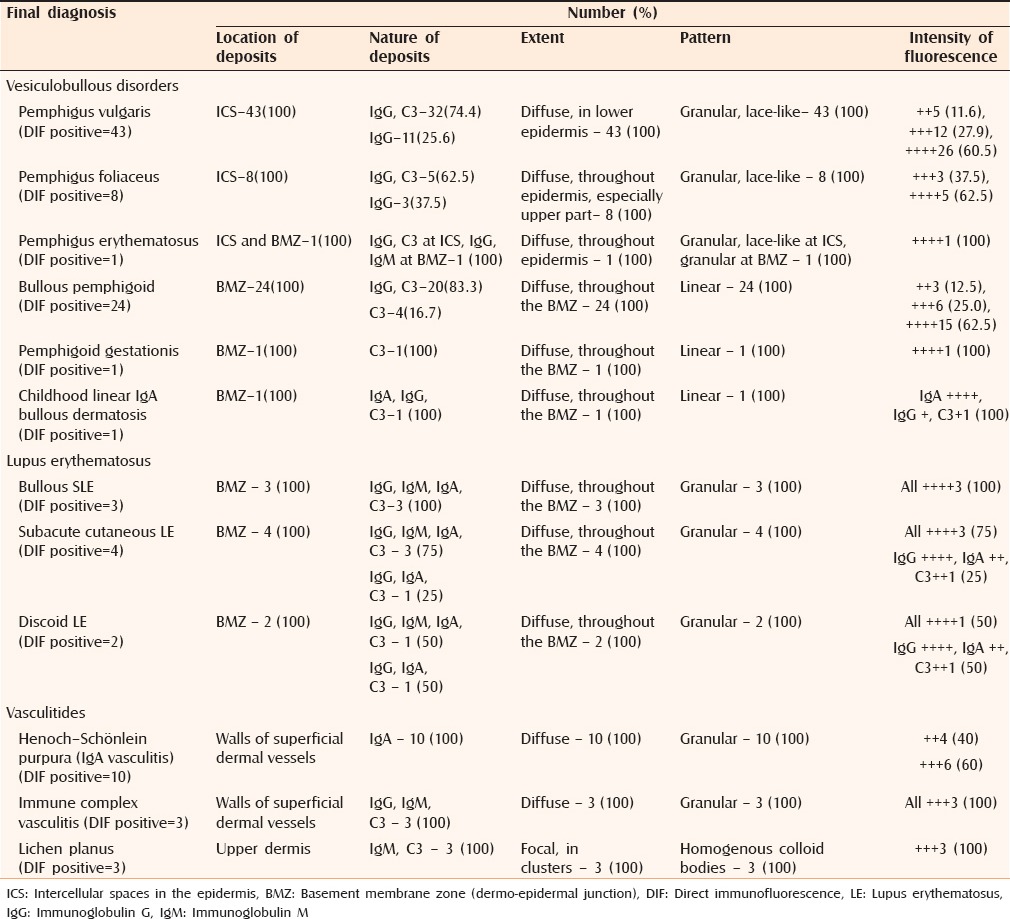
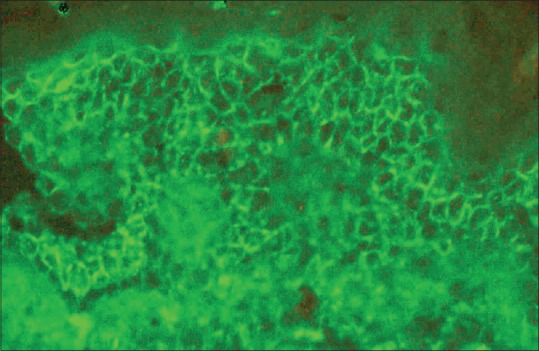
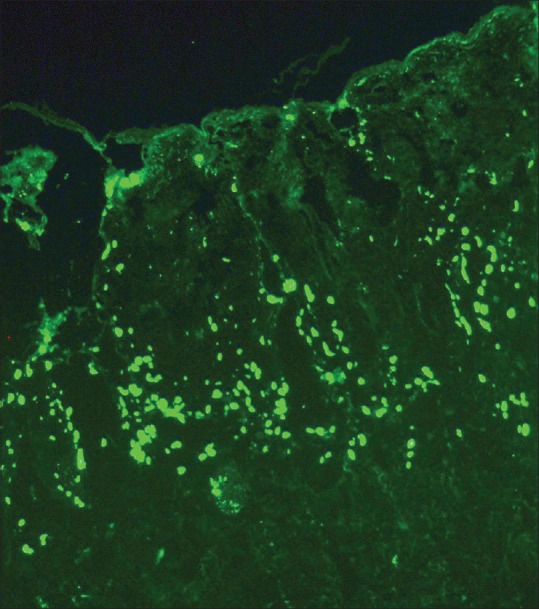
In the pemphigus group, DIF positivity was seen in 52/53 cases (98.1%) [Figure 1]. In two cases of pemphigus vulgaris, histology showed complete desquamation of the roof of the bulla with preservation of only the basal layer of the epidermis focally. In these cases, a definite diagnosis of pemphigus vulgaris was made on the basis of clinical features and DIF findings. In all the 8 cases of pemphigus foliaceus and in the single case of pemphigus erythematosus, the DIF results and histopathology correlated well. In the bullous pemphigoid category, DIF positivity was seen in 24/25 cases (96.0%) [Figure 2]. In two cases of bullous pemphigoid, the skin biopsy taken for histopathology showed loss of the epidermis over the bulla, but a dense eosinophilic and mononuclear infiltrate was present in the floor of the bulla and around the dermal blood vessels. In these two cases, a conclusive diagnosis of bullous pemphigoid was made on the basis of the DIF findings in conjunction with the clinical and histopathological features.
Figure 1.
Pemphigus vulgaris – Direct immunofluorescence showing granular deposits of immunoglobulin G (IgG) (+++) in the intercellular spaces of the lower epidermis (fluorescein isothiocyanate anti-IgG, ×200)
Figure 2.
Bullous pemphigoid – Direct immunofluorescence showing linear deposits of C3 (+++) at the dermo-epidermal junction (basement membrane zone) (fluorescein isothiocyanate anti-C3, ×200)
In the lone case of pemphigoid gestationis, histopathology showed a subepidermal bulla containing numerous eosinophils, along with papillary dermal edema. The diagnosis was confirmed by DIF, which showed linear deposition of C3 along the BMZ in perilesional skin. In one case where there were subepidermal blisters in a child, the diagnosis of childhood linear IgA bullous dermatosis was possible on DIF, which showed predominantly linear IgA deposits along the DEJ along with weak staining for IgG and C3.
In the present study, none of the clinically suspected cases of dermatitis herpetiformis (DH) showed positivity on DIF. Even the histopathologic findings were nonspecific in these cases. Hence, no case of DH was diagnosed by the pathologists. The final diagnosis and treatment were based on the clinical assessment by the dermatologists alone.
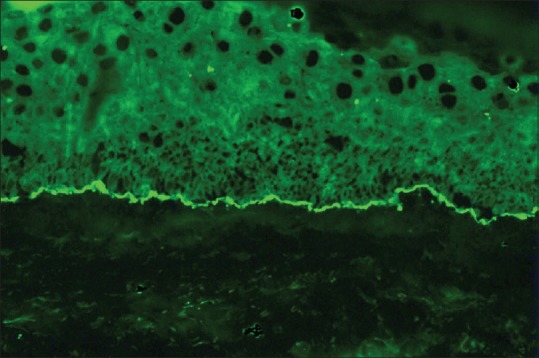
Among the connective tissue disorders, a positive lupus band test (LBT) was seen on DIF only in lupus erythematosus [Figure 3a and b], where it was seen in 9/9 (100%) cases. In 7 of these cases, full-house LBT positivity with IgG, IgA, IgM and C3 was obtained. In the remaining two cases – one discoid lupus erythematosus (DLE) and the other subacute cutaneous lupus erythematosus (SCLE) – IgG was intensely positive, and was accompanied by IgA and C3. In one case of systemic lupus erythematosus (SLE), the perilesional skin also showed vasculitis of dermal vessels, while another case also showed in vivo positivity for antinuclear antibodies (ANA) in the nuclei of the keratinocytes. In one case that was clinically diagnosed as bullous pemphigoid, the characteristic DIF pattern led to a diagnosis of bullous SLE, which was subsequently confirmed by ANA studies. In one case each of bullous SLE, SCLE, and DLE, the LBT was clearly positive, although the histopathological findings were not specific for these conditions.
Figure 3.
Systemic lupus erythematosus (SLE) – (a) Direct immunofluorescence (DIF) showing dense granular continuous deposits of immunoglobulin G (IgG) (++++) along the dermo-epidermal junction (lupus band test) (fluorescein isothiocyanate anti-IgG, ×200) SLE – (b) DIF showing dense granular continuous deposits of IgA (++++) along the dermo-epidermal junction (lupus band test) (fluorescein isothiocyanate anti-IgA, ×200)
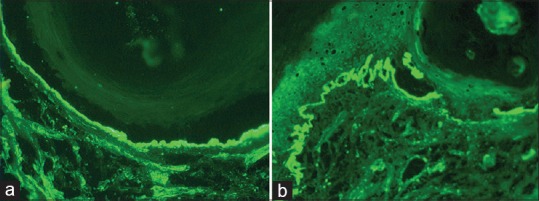
Direct immunofluorescence was positive in 13/44 (29.5%) cases of vasculitis, of which 10 proved to be Henoch–Schönlein purpura (HSP) [Figure 4]. There was correlation between the clinical features and DIF in 10/10 (100%), and between DIF and histopathology in 9/10 (90%) of HSP cases. In 29 cases of small vessel neutrophilic vasculitis (leukocytoclastic vasculitis) of cause other than HSP, only 3 (10.3%) showed deposits of IgG, IgM and C3 in the dermal vessel walls, and were thus proved to be immune complex-mediated. In the remaining 26 cases, DIF being negative, a diagnosis of nonimmune leukocytoclastic vasculitis, probably infection-mediated, was made.
Figure 4.
Henoch–Schönlein purpura – Direct immunofluorescence showing granular deposits of immunoglobulin A (IgA) (+++) in the walls of the superficial dermal vessels (fluorescein isothiocyanate anti-IgA, ×200)
Table 6 outlines the 113 cases where the final diagnoses of the skin disorders were made on the basis of clinical features and histopathology. Three out of 11 cases of lichen planus (27.3%) subjected to DIF showed IgM and C3 staining within the colloid bodies in the papillary dermis. These colloid bodies were clustered in groups of 10 or more [Figure 5]. However, the presence of colloid bodies could not be taken as a diagnostic finding in lichen planus and the final diagnosis was made by histopathology. In 110 cases, a negative DIF result helped to rule out immune-mediated vesiculobullous disorders, lupus erythematosus and vasculitis. In these cases, the final diagnosis was made on the basis of the clinical features and/or histopathological findings. Two of the 5 cases of Hailey–Hailey disease showed histopathological features overlapping with those of pemphigus vulgaris; however DIF negativity helped to make a correct diagnosis.
Table 6.
Skin disorders which were diagnosed on the basis of clinical features and histopathology (total=113, DIF positivity=3/113)
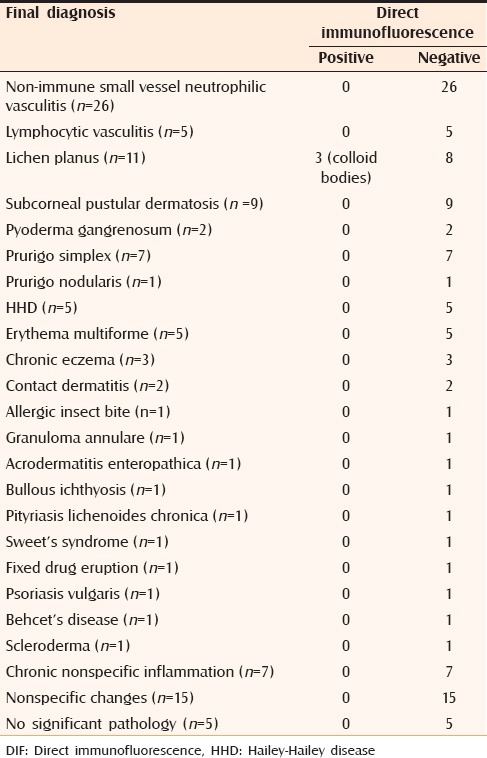
Figure 5.
Lichen planus – Direct immunofluorescence showing a large group of globular colloid bodies having immunoglobulin M (IgM) deposits (+++), in the upper dermis (fluorescein isothiocyanate anti- IgM, ×100)
DISCUSSION
In the present study, there was a very good concordance between the clinical, histological and DIF results. The overall results of DIF in immune-mediated skin disorders were very good with only two cases (one of pemphigus vulgaris and one of bullous pemphigoid) showing discordant results. DIF was helpful in making an accurate diagnosis when the clinical features/histology were not typical, and for confirmation of the diagnosis in all cases where the clinical features and histology were typical. In many situations, a negative DIF result was also important since it helped to exclude an immune basis for the disease, even though it could not provide a precise diagnosis. There were no false-positive DIF results.
Vesiculobullous lesions accounted for 78.4% of the immune-mediated skin disorders and 37.3% of the total skin disorders studied. In the present study, 78/80 (97.5%) vesiculobullous skin lesions gave diagnostic results on DIF. Inchara and Rajalakshmi[6] found that 73% cases of vesiculobullous lesions in their study showed DIF patterns concordant with the clinical/histologic diagnosis. The sensitivity of DIF was 88% in the pemphigus group in their study.[6] We had a very high DIF sensitivity of 98.1% (52/53) in the pemphigus group. In 43/44 (97.7%) pemphigus vulgaris cases, DIF was positive. Minz et al.[5] were able to detect 70% of clinically diagnosed vesiculobullous lesions of the skin by DIF, and 18/22 (81.8%) cases of pemphigus vulgaris in their study were DIF-positive. Treatment-induced changes were a cause of false-negative DIF results;[5] however, we did not encounter any such problem. In pemphigus, DIF becomes positive early in the disease, and complement deposition shows an increase or reappears in patients who have a relapse.[7] Thus, DIF can be useful to predict imminent relapse in pemphigus patients in remission. However, it may not be a good prognostic marker for disease activity as it tends to remain positive long after clinical remission.[7]
In the study by Minz et al.,[5] DIF was positive in only 7/13 (53.8%) suspected cases of bullous pemphigoid, and a combination of DIF with histopathology improved the sensitivity of detection of bullous pemphigoid. Inchara and Rajalakshmi[6] found the sensitivity of DIF in bullous pemphigoid to be 82%. In the present study, 24/25 (96%) bullous pemphigoid cases were DIF-positive, with only one case showing false-negative DIF result. Other methods that are helpful in the precise identification of blistering disorders include indirect immunofluorescence for circulating autoantibodies, and the salt-split skin technique for exact localization of the level of split in the basement membrane, in case of subepidermal bullous disorders.[3,4] These investigations were, however, outside the purview of our study.
Pemphigoid gestationis or herpes gestationis is a rare autoimmune subepidermal blistering disorder that develops in the second or third trimester of pregnancy. We were able to confirm the diagnosis of pemphigoid gestationis in one case by the characteristic DIF pattern.[8,9] Linear IgA bullous dermatosis is another subepidermal blistering condition that is clinically similar to bullous pemphigoid, and DIF is required to differentiate the two. The typical DIF finding of linear IgA deposits along the DEJ[10,11] helped us to make the correct diagnosis in the lone case of linear IgA bullous dermatosis.
In the present study, we could not confirm any case of DH by histopathology from the lesion or DIF from the perilesional skin. In the experience of Inchara and Rajalakshmi,[6] all four biopsy-proven cases of DH were DIF-negative, however two of them responded to specific treatment for DH. Lebe et al.[12] found a clinical and histopathological/DIF concordance of only 5.2% in DH. Minz et al.[5] also noted that in DH the histology and DIF findings are nonspecific. Thus, many authors conclude that in suspected DH, in the absence of the characteristic DIF pattern, one should rely on the clinical features, serology and response to treatment, rather than DIF or histopathology in order to make a correct diagnosis.[5,6,13] False-negative results can be obtained in DH if the biopsy for DIF is taken from the lesional site as inflammation in lesional skin degrades the immunoreactants, resulting in failure to obtain the diagnostic granular pattern.[5]
Among the lupus group of disorders, a positive LBT has been described in the lesional skin in > 90% cases of SLE, 60% of SCLE, and 90% of DLE. In patients with active disease, the nonlesional sun-protected skin shows a positive LBT in 90% cases of SLE, 30% of SCLE and 0–10% of DLE.[14] Minz et al.[5] obtained a demonstrable band test in only 71% patients with SLE and 59% with DLE, probably on account of the lesions being in the late stage or treated. Some authors have found that the LBT is not specific for lupus erythematosus, but may also be seen in other connective tissue disorders and even as a false-positive result in some unrelated disorders.[5,14] However, in the present study, the LBT was seen only in lupus erythematosus, and in 100% of these cases. The lone case of diffuse scleroderma that was subjected to DIF showed a negative LBT.
Only 13 (29.5%) of our 44 cases of vasculitis were DIF-positive. Ten cases of HSP could be diagnosed on DIF, however, immune complex vasculitis could be proved in only three cases. The number of proven cases of immune-complex vasculitis turned out to be very small in comparison to the study by Minz et al.[5] on the North Indian population, where DIF was able to detect 23/26 (89%) HSP cases and confirm immune complex vasculitis in 41/45 (91%) cases. Nandeesh and Tirumalae[15] report an overall DIF positivity of 39% in cutaneous vasculitis, with 43/48 (90%) cases of suspected HSP showing positivity. They found that positivity rates are highest when biopsies are taken within 48 h after onset of lesions.
Immunoreactants at the colloid (cytoid) bodies have been found on DIF in 44.4% cases with interface dermatitis.[16] Kulthanan et al.[17] found colloid bodies in 60% of their lichen planus cases. Only 3/11 (27.3%) of our cases of lichen planus subjected to DIF showed positivity in the colloid bodies; the remaining eight were DIF-negative. However, the presence of colloid bodies could not be taken as a diagnostic finding in lichen planus and the final diagnosis was made only on histopathology. Colloid bodies have been described in a variety of other conditions such as LE, bullous pemphigoid, vasculitis, erythema multiforme, panniculitis and scleroderma/morphea.[16,18] A strong intensity and high quantity of colloid bodies favor the diagnosis of interface dermatitis.[16,18] The most common immunoreactant in the colloid bodies is usually IgM,[16] as was our experience. Colloid bodies are formed either from apoptosis of keratinocytes or from destruction of thickened basement membrane.[16] Shaggy fibrin was noted at the DEJ in 56% of cases of lichen planus in one study.[17]
CONCLUSION
With appropriate sampling and prompt processing, DIF is a useful supplement for the accurate diagnosis of immune-mediated dermatological disorders, and helps to classify various autoimmune bullous disorders. When the clinical features/histopathology are typical as in bullous disorders, lupus erythematosus and vasculitis, DIF confirms the diagnosis. However, there are situations where the clinical features/histopathology are inconclusive and the diagnosis can be made on the basis of the DIF findings alone. A negative DIF helps to rule out immunological cause for the dermatological disorder. Combined analysis of clinical features, histopathology and DIF usually delivers the best result.
ACKNOWLEDGMENTS
The authors are grateful to Dr. N. S. Murthy, Professor and Research Coordinator, M.S. Ramaiah Medical College, Bangalore, and Ms. Radhika K., Statistician and Lecturer, Department of Community Medicine, M.S. Ramaiah Medical College, Bangalore, for their assistance in the statistical analysis.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared
REFERENCES
- 1.Khan WA, Valand AG. Pattern of non infectious vesiculobullous and vesiculopustular skin diseases in a large tertiary care hospital. Bombay Hosp J. 2010;52:172–6. [Google Scholar]
- 2.Chhabra S, Minz RW, Saikia B. Immunofluorescence in dermatology. Indian J Dermatol Venereol Leprol. 2012;78:677–91. doi: 10.4103/0378-6323.102355. [DOI] [PubMed] [Google Scholar]
- 3.Elenitsas R, Nousari CH, Seykora JT. Laboratory methods. In: Elder DE, Elenitsas R, Johnson BL, Murphy GF, editors. Lever's Histopathology of the Skin. 9th ed. Philadelphia: JB Lippincott; 2005. pp. 59–73. [Google Scholar]
- 4.Weedon D, editor. Weedon's Skin Pathology. 3rd ed. China: Churchill Livingstone Elsevier; 2010. The vesiculobullous reaction pattern; pp. 124–68. [Google Scholar]
- 5.Minz RW, Chhabra S, Singh S, Radotra BD, Kumar B. Direct immunofluorescence of skin biopsy: Perspective of an immunopathologist. Indian J Dermatol Venereol Leprol. 2010;76:150–7. doi: 10.4103/0378-6323.60561. [DOI] [PubMed] [Google Scholar]
- 6.Inchara YK, Rajalakshmi T. Direct immunofluorescence in cutaneous vesiculobullous lesions. Indian J Pathol Microbiol. 2007;50:730–2. [PubMed] [Google Scholar]
- 7.Sethi KJ, Kanwar AJ, Kaur S, Sehgal S. Direct immunofluorescence as a diagnostic and prognostic marker in pemphigus. Indian J Dermatol Venereol Leprol. 1992;58:379–83. [Google Scholar]
- 8.Lu PD, Ralston J, Kamino H, Stein JA. Pemphigoid gestationis. Dermatol Online J. 2010;16:10. [PubMed] [Google Scholar]
- 9.Thomas S, Rajan U, George S, George M. Postpartum pemphigoid gestationis. Indian J Dermatol. 2012;57:146–8. doi: 10.4103/0019-5154.94291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Monia K, Aida K, Amel K, Ines Z, Becima F, Ridha KM. Linear IgA bullous dermatosis in Tunisian children: 31 cases. Indian J Dermatol. 2011;56:153–9. doi: 10.4103/0019-5154.80406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Onodera H, Mihm MC, Jr, Yoshida A, Akasaka T. Drug-induced linear IgA bullous dermatosis. J Dermatol. 2005;32:759–64. doi: 10.1111/j.1346-8138.2005.tb00839.x. [DOI] [PubMed] [Google Scholar]
- 12.Lebe B, Gül Nýflýoğlu G, Seyrek S, Ellýdokuz H. Evaluation of clinical and histopathologic/direct immunofluorescence diagnosis in autoimmune vesiculobullous dermatitis: Utility of direct immunofluorescence. Turk Patoloji Derg. 2012;28:11–6. doi: 10.5146/tjpath.2012.01091. [DOI] [PubMed] [Google Scholar]
- 13.Sousa L, Bajanca R, Cabral J, Fiadeiro T. Dermatitis herpetiformis: Should direct immunofluorescence be the only diagnostic criterion? Pediatr Dermatol. 2002;19:336–9. doi: 10.1046/j.1525-1470.2002.00096.x. [DOI] [PubMed] [Google Scholar]
- 14.Crowson AN, Magro C. The cutaneous pathology of lupus erythematosus: A review. J Cutan Pathol. 2001;28:1–23. doi: 10.1034/j.1600-0560.2001.280101.x. [DOI] [PubMed] [Google Scholar]
- 15.Nandeesh B, Tirumalae R. Direct immunofluorescence in cutaneous vasculitis: Experience from a referral hospital in India. Indian J Dermatol. 2013;58:22–5. doi: 10.4103/0019-5154.105280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Chularojanamontri L, Tuchinda P, Triwongwaranat D, Pinkaew S, Kulthanan K. Diagnostic significance of colloid body deposition in direct immunofluorescence. Indian J Dermatol Venereol Leprol. 2010;76:373–7. doi: 10.4103/0378-6323.66583. [DOI] [PubMed] [Google Scholar]
- 17.Kulthanan K, Jiamton S, Varothai S, Pinkaew S, Sutthipinittharm P. Direct immunofluorescence study in patients with lichen planus. Int J Dermatol. 2007;46:1237–41. doi: 10.1111/j.1365-4632.2007.03396.x. [DOI] [PubMed] [Google Scholar]
- 18.Wu YH, Lin YC. Cytoid bodies in cutaneous direct immunofluorescence examination. J Cutan Pathol. 2007;34:481–6. doi: 10.1111/j.1600-0560.2006.00641.x. [DOI] [PubMed] [Google Scholar]


