INTRODUCTION
Peripheral arterial disease (PAD) affects approximately 20% of patients aged ≥60 years.1 A GP with an average list size of 1800 patients can expect to have 50–60 patients with PAD. Ankle-brachial pressure index (ABPI), which is the ratio of the ankle to brachial systolic pressure measured by sphygmomanometer and hand-held Doppler ultrasound probe, is used to assess PAD in general practice. ABPI has been shown to have a sensitivity of 95% and specificity of 99% compared to angiographic imaging,2 however it is relatively time-consuming and requires adequately trained staff. There are limitations with ABPI in patients with diabetes, renal disease, and older people where an underestimation of disease can occur with a falsely high ratio due to the presence of incompressible calcified blood vessels.
Clinical Question
Can peripheral arterial disease be accurately diagnosed in general practice?
DIAGNOSTIC CHALLENGES
The characteristic clinical diagnostic feature of PAD is intermittent claudication (IC), muscle pain brought on by exercise, relieved by rest and experienced in the calf with femoropopliteal disease and in the buttock, hip or thigh with aortoiliac disease. However it is sometimes difficult to distinguish clinically between claudication and leg pain from other causes such as spinal stenosis.
ABPI methodology
The first problem we face is that a significant proportion of patients in general practice who are arteriopaths are asymptomatic and ABPI has been routinely adopted to confirm and quantify the diagnosis of peripheral vascular disease in those with IC. Unfortunately the exact methodology is not standardised, beginning with a choice of three arteries in the ankle each with potentially differing pressures and some of which are commonly congenitally absent. Similarly the clinician has a choice of two arms for the brachial pressure and there is no consensus on how the central reference pressure should be assessed. Indeed, arteriosclerosis is a systemic disease. Failure to lie supine can introduce a hydrostatic pressure difference between arm and leg. A number of environmental factors such as ambient temperature can also affect peripheral vasomotor tone. The occlusive cuff method itself has been called into question with a likely underestimate of true pressure drop varying with site of lesion and which may be exacerbated with baseline hypotension or hypertension confounding ABPI readings. Finally, there is no consensus on normal ranges for ABPI ratios, and hence referral thresholds, evidenced by its absence in the most recent National Institute for Health and Care Excellence guidance.3
Limitations of ABPI
As well as methodological limitations and despite the claimed 95% sensitivity and 99% specificity, there are a number of problematic assumptions. Many of the studies of ABPI have used control subjects that are clinically asymptomatic volunteers rather than angiographically proven normals. A rich collateral vessel network may be responsible for a proportion of asymptomatic PAD patients and ABPI would fail to unmask this cohort. Heavy arterial calcification resulting in incompressible arteries in diabetic, renal, and older patients renders the ABPI non-diagnostic. This is also problematic in rarer conditions such as systemic sclerosis and rheumatic diseases. There is a need for a non-invasive alternative to ABPI for assessing peripheral vascular disease in general practice.
PHOTOPLETHYSMOGRAPHY
Photoplethysmography (PPG) is offering a new look at diagnosis and management of PAD in general practice. PPG is a low cost, non-invasive, simple-to-use, and fast- to-perform optical technique based on peripheral pulse waveform analysis and has been shown to have good sensitivity and specificity for PAD when compared to ABPI.4 However the place of this technology in general practice is yet to be established.
Methodology and challenges
PPG typically uses near-infrared (or red) light to measure the changes in tissue blood volume associated with each heartbeat.5 In its simplest form a light source is directed towards the tissue microvascular bed, for example to the ear lobe, finger, or toe pad, and an adjacent photodetector measures the small changes in light absorption to form a PPG pulse waveform (Figure 1). Although the exact nature of PPG is not fully understood its signatures in health and vascular disease have been described and reviewed by Allen.5
Figure 1.
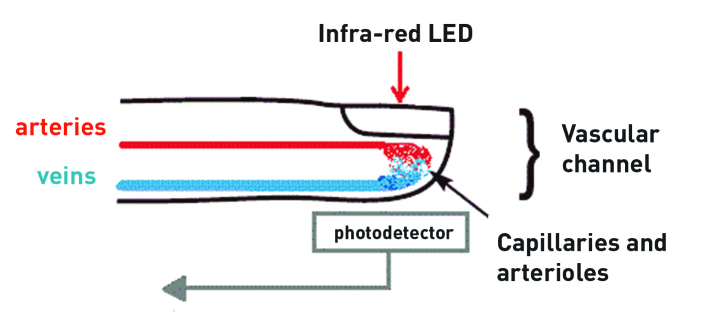
Photoplethysmography.
The waveforms from PPG technology are typically pulsatile and can be compared between sites such as the toes and fingers. In PAD a damping effect is produced with a reduction in amplitude and changes in waveform shape and timing compared to a healthy vascular bed.
A simpler variant of PPG, pulse oximetry, has already been successfully deployed in general practice. The next stage in the development of this technology is in its routine use for PAD patients in general practice.
WHAT IT MEANS FOR GENERAL PRACTICE
The key determinant to the successful embedding of advanced PPG technology in general practice is the ability to produce clear results indicating significant or non-significant disease and for it to be reliably delivered by a range of primary care professionals. The purpose of such technology will be:
to identify a cohort of patients in whom there is no significant PAD and who can be reassured;
to identify a cohort of patients in whom there is significant PAD and make onward referral for further evaluation and/or intervention; and
to identify a cohort of patients with mild PAD where primary care management is indicated (Box 1).
Box 1. Summary of PAD management and annual monitoring in general practice.
Assessment of symptoms
Ankle-brachial pressure index (ABPI) estimation
Smoking cessation advice
Cholesterol lowering
Blood pressure management
Weight management and exercise
HBA1c estimation
Anti-platelet treatment
PAD is a window on widespread atherosclerotic cardiovascular disease6 and advanced PPG technology may give opportunities for cardiovascular screening in the future.
FURTHER WORK
With support from the National Institute for Health Research Invention for Innovation scheme, the Novel Test Evaluating Peripheral Arterial Disease (NOTEPAD) project will develop a PPG device for use in primary care. It remains to be seen whether PPG technology can produce an output that guides the management of PAD in general practice. Technological advances in PAD management have lagged behind in comparison with coronary heart disease and stroke management. It is the intention of the NOTEPAD investigators to develop and demonstrate the worth of this technology to the primary care clinician.
Funding
This report is independent research funded by the National Institute for Health Research (Invention for Innovation, ‘Innovative photoplethysmography technology for rapid noninvasive assessment of peripheral arterial disease in primary care,’ II-C1-0412-20003). Views expressed in this publication are those of the authors and not necessarily those of the NHS, the NIHR or the Department of Health.
Provenance
Freely submitted; not externally peer reviewed.
Competing interests
John Allen and Andrew Simms are employed by The Newcastle upon Tyne Hospitals NHS Foundation Trust which holds the majority rights to the intellectual property of the NOTEPAD technology.
Discuss this article
Contribute and read comments about this article: bjgp.org/letters
REFERENCES
- 1.Fowkes FG, Housley E, Cawood EH, et al. Edinburgh Artery Study: prevalence of asymptomatic and symptomatic peripheral arterial disease in the general population. Int J Epidemiol. 1991;20(2):384–392. doi: 10.1093/ije/20.2.384. [DOI] [PubMed] [Google Scholar]
- 2.Bernstein EF, Fronek A. Current status of noninvasive tests in the diagnosis of peripheral arterial disease. Surg Clin North Am. 1982;62(3):473–487. doi: 10.1016/s0039-6109(16)42739-8. [DOI] [PubMed] [Google Scholar]
- 3.National Institute for Health and Care Excellence Lower limb peripheral arterial disease: diagnosis and management. p. CG147. http://www.nice.org.uk/guidance/cg147 (accessed 28 Apr 2015) [PubMed]
- 4.Allen J, Overbeck K, Nath AF, et al. A prospective comparison of bilateral photoplethysmography versus the ankle-brachial pressure index for detecting and quantifying lower limb peripheral arterial disease. J Vasc Surg. 2008;47(4):794–802. doi: 10.1016/j.jvs.2007.11.057. [DOI] [PubMed] [Google Scholar]
- 5.Allen J. Photoplethysmography and its application in clinical physiological measurement. Physiol Meas. 2007;28(3):R1–39. doi: 10.1088/0967-3334/28/3/R01. [DOI] [PubMed] [Google Scholar]
- 6.Doobay AV, Anand SS. Sensitivity and specificity of the ankle-brachial index to predict future cardiovascular outcomes: a systematic review. Arterioscler Thromb Vasc Biol. 2005;25(7):1463–1469. doi: 10.1161/01.ATV.0000168911.78624.b7. [DOI] [PubMed] [Google Scholar]


