Abstract
Objective:
To compare the injection pain and speed of local anesthetic effect induced by tissue infiltration of mepivacaine 2% with epinephrine 1:100,000 versus articaine 4% with epinephrine 1:100,000 in securing mandibular first molar pulp anesthesia.
Materials and Methods:
Totally, 25 patients were recruited in a crossover, randomized, double-blind study. Each subject received injections of mepivacaine 2% with epinephrine 1:100,000 as inferior alveolar nerve block (IANB) supplemented with either articaine 4% with epinephrine 1:100,000 (septocaine) or mepivacaine 2% buccal infiltration (BI) injection on two visits. The time of first numbness to associated lip, tongue and tooth was recorded by asking the participant directly and using electrical pulp tester. Anesthetic success was considered when two consecutive maximal stimulation on pulp testing readings without sensation. The patients rated the pain of infiltration using a 100 mm visual analog scale immediately after receiving each injection. The pain scores were compared using the paired t-test.
Results:
There were significant differences in the meantime of first numbness to associated lip and tooth of volunteers between mepivacaine and articaine BI groups P = 0.03 and 0.002. Volunteers in articaine group recorded earlier lip and teeth numbness than those in mepivacaine group. There were significant differences between the mean pain scores for volunteers in the post IANB and postbuccal injection groups (t-test: P <0.001). Mepivacaine IANB injection was significantly more painful than articaine/mepivacaine buccal injection.
Conclusions:
About 4% articaine was faster than 2% mepivacaine (both with 1:100,000 adrenaline) in anesthetizing the pulps of lower molar teeth after BIs. Earlier lip and teeth numbness were recorded in articaine group. Articaine and mepivacaine BIs were more comfortable than mepivacaine IANB injections.
Keywords: Articaine, buccal infiltration, inferior alveolar nerve block, mandibular permanent teeth, mepivacaine
INTRODUCTION
Increasing failure rate of dental local anesthetic injections especially in the mandibular molars is a continual challenge in dentistry. Supplemental injection techniques are essential to be used in cases where the conventional local anesthetic techniques have failed.[1] A study by Meechan,[2] reported that the inferior alveolar nerve block (IANB) is associated with a failure rate of 15% in patients with normal tissue. However, the failure rate of IANB in teeth with irreversible pulpitis is as high as 44-81%.[3] Supplemental buccal infiltration (BI) with articaine was significantly more effective than lidocaine.[4]
Monteiro et al.[5] stated that the emergency treatment of teeth with irreversible pulpitis, using single conventional anesthetic technique were not 100% pain-free. So, additional anesthetic techniques should be employed before commencing the root canal treatment in order to overcome the failure of local anesthetic injections.
Brandt et al.[6] assessed published evidence from controlled clinical trials regarding the efficacy of using articaine versus lidocaine for achieving pulpal anesthesia when the infiltration mode of administration is used. The findings of their study revealed that the supporting evidence is still premature to recommend articaine for mandibular teeth with irreversible pulpitis.
Buccal infiltrations with 4% articaine for mandibular first molars can be a useful alternative for clinicians when compared with IANB with 2% lidocaine. It has a faster onset and a similar success rate.[7]
Kanaa et al.[8] reported that the success rate of pulpal anesthesia in mandible teeth using a combination of IANB injection and articaine BI was more successful than IANB alone. With regards to the injection site discomfort, IANB with lidocaine (IANB) was more painful than articaine BI.
Dudkiewicz et al.[9] reported that the using of articaine 4% infiltration in pediatric patients produce an appropriate deep anesthesia of posterior primary mandibular teeth. Higher lipid solubility of articaine compared to lidocaine could be the reason for its rapid diffusion through bone onto the lingual side of each tooth. Recently, there had been an apparent increase in dysesthesia following regional nerve block injections associated with the use of articaine. So, articaine is considered as an alternative to lidocaine for local anesthesia in dentistry.[10,11]
The primary aim of this study is to evaluate the length of time for achieving first numbness to associated lip and teeth following BI either with 2% mepivacaine or with 4% articaine in securing mandibular first molar pulp anesthesia. Our null hypothesis stated that the BIs of mepivacaine and articaine following mepivacaine IANB injections have equal length of time for achieving first numbness to associated lip and teeth.
MATERIALS AND METHODS
Twenty-five volunteers who were with in the correct age range (16–60 years old) were randomly allocated to one of the study groups. Two volunteers were excluded because they got fainted following first local anesthetic injection. The final sample size, therefore, comprised 23 patients. Official clearances and ethical approval were obtained from the Taibah College of Dentistry in Al Madinah Al Munawwarah, Saudi Arabia. Following reading the information sheet and signing the formal consent form, two regimens were randomly administered with at least 1-week apart. Randomization was achieved by an independent observer. Treatment group one had mepivacaine IANB and mepivacaine BI. IANB was performed by inserting the local anesthetic needle midway between the internal oblique ridge and the pterygomandibular raphe. The needle was advanced until an adequate bony contact was achieved (IANB: Direct or Halstead approach), then, 1.8 mL mepivacine 2% with epinephrine 1:100,000, was delivered slowly over 60 s after aspiration plus a 1.8 mL mepivacaine infiltration in the buccal reflected mucosa adjacent to the mandibular first molar over 60 s. Treatment group two had mepivacaine 2% IANB and articaine 4% with epinephrine 1:100,000 BI. Both volunteers and the researcher carrying out the assessment were blind as to which local anesthetic BI regimen, was administered. All injections were given by the same dental surgeon. The discomfort of the injections was recorded by the volunteers after each treatment on standard 100 mm visual analogue scales (VAS), tagged at the endpoints with “no pain” (0 mm) and “unbearable pain” (100 mm). After all injections, the volunteers were asked to subjectively gauge soft tissue anesthesia of the lower lip, tongue, and teeth as soon as numbness was felt. The researcher who made all the anesthetic effectiveness and pain assessments was completely independent of the whole process. The onset of pulp anesthesia was determined using electrical pulp tester (parkell products USA: Digitest pulp vitality tester: STOCK NO. D626D with maximum stimulation 64). Anesthetic success was defined when two or more consecutive episodes of maximal pulp stimulation (64 reading) without sensation were recorded. Evaluation was made before injection (baseline) and at intervals of 2 min for the first 10 min after injection.
RESULTS
There were 25 volunteers who were with in the correct age range for the study and who were randomly allocated to one of the study groups. Two volunteers were excluded because they got fainted following first local anesthetic injection and decided to cancel their participation in the study. The final sample size, therefore, comprised 23 patients. The statistical analysis was performed using a software package (SPSS; version 20, SPSS Inc., Chicago, IL). All (23 volunteers) achieved anesthetic success for first molar pulp anesthesia following mepivacaine/articaine BI within 10 min and continuously sustained for 45 min postinjection.
Time of first numbness to associated lip, tongue and teeth
Tables 1, 2 and Figure 1 summarize the overall outcome of the time of first numbness to associated lip, tongue and tooth of the 23 volunteers who participated in the study. The mean time of first numbness to associated lip, tongue and tooth was 1.87, 1.81 and 2.82 min (standard deviation [SD] 1.159, 1.362 and 1.477, Table 1).
Table 1.
Description of time of first numbness to associated lip, tongue and teeth of the volunteers in the study
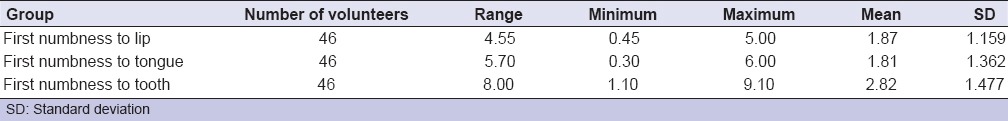
Table 2.
Comparisons between mean time of first numbness to associated lip, tongue and tooth of the volunteers in mepivacaine and articaine infiltration groups
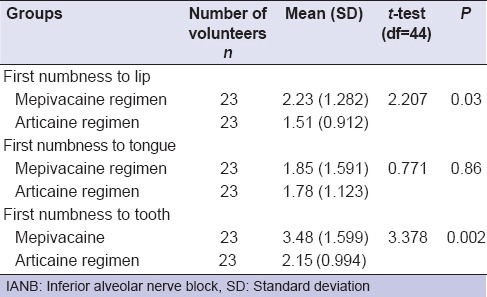
Figure 1.
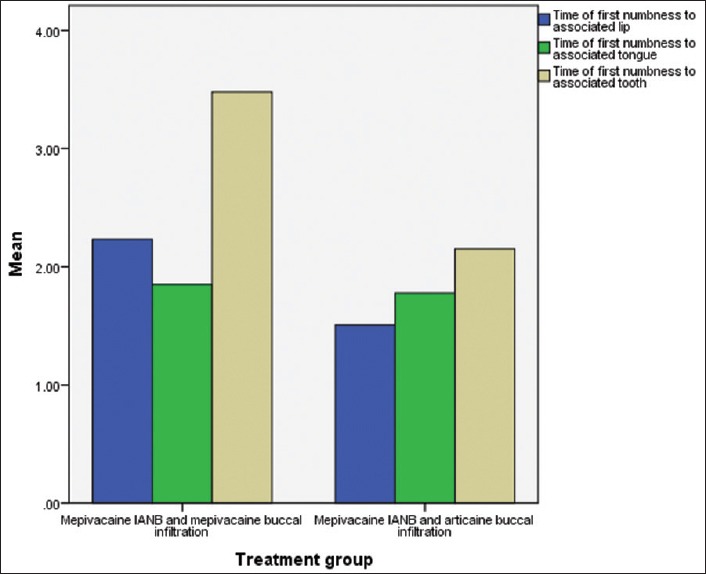
Clustered bar charts showing the mean time of first numbness to associated lip, tongue and tooth of volunteers in the mepivacaine and articaine buccal infiltration groups
The mean time of first numbness to associated lip, tongue and tooth of volunteers in mepivacaine BI group were 2.23, 1.85 and 3.48 min (SD 1.282, 1.591 and 1.599). Whereas, the mean time of first numbness to associated lip, tongue and tooth of volunteers of patient in articaine BI group were 1.51, 1.78 and 2.15 min (SD 0.912, 1.123 and 0.994).
There were significant differences in the meantime of first numbness to associated lip and tooth of volunteers between mepivacaine and articaine BI groups P = 0.03 and 0.002 [Table 2]. In the light of this result, volunteers in articaine group recorded earlier lip and teeth numbness than those in mepivacaine group.
There were no significant differences in the meantime of first numbness to associated tongue of volunteers between the two BI groups (P > 0.05).
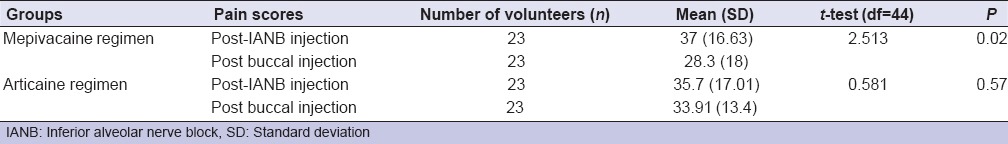
Injection discomfort
The discomfort of the injections was recorded by the volunteers after each treatment on standard 100 mm VAS, tagged at the endpoints with “no pain” (0 mm) and “unbearable pain” (100 mm). The range pain injection score of volunteers in the study was from 10 to 80 years. The mean pain scores for post IANB and buccal injections were 36.30 and 31.09 mm respectively (SD 16.648 and 31.09). These figures are illustrated in Table 3.
Table 3.
Comparisons between mean pain injection scores for volunteers in post-IANB and post buccal injection groups
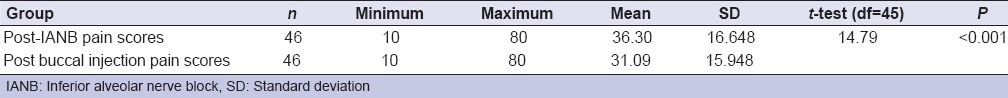
There were significant differences between the mean pain scores for volunteers in the post IANB and postbuccal injection groups [t-test: P < 0.001, Table 3]. Mepivacaine IANB injection was significantly more painful than articaine/mepivacaine buccal injection.
For both mepvacaine and articaine groups, changes in pain injection scores from post IANB score to postbuccal injection score were made using the paired sample t-test. There was a significant difference for mepivacaine group when comparing the post IANB scores with the postbuccal injection scores [P = 0.02, Table 4]. Mepivacaine buccal injection was significantly more comfortable than articaine buccal injection.
Table 4.
Comparisons between mean post-IANB pain scores and post buccal injection for volunteers in the mepivacaine and articaine groups
Volunteer's age
The range age of volunteers in the study was from 17 to 55 years. The mean age was 29.9 years (SD 10.77).
The mean age 30 was used as a cut-off point to split the participants into two groups; the first group comprised volunteers who were aged between 17 and 29 years, the second group comprised volunteers who were aged between 30 and 55 years.
The application of the t-test revealed that there were significant differences in the mean pain injection scores between the two age groups (P < 0.05). This was at 2 times intervals post IANB and postbuccal injections
It was found that volunteers aged between 17 and 29 years recorded significantly higher pain scores than volunteers aged between 30 and 55 years following either IANB or buccal injection [mean = 42.69, 28, 35.38 and 25.50 respectively; P < 0.01, Table 5]. So, older volunteers were significant.
Table 5.
Comparisons between mean pain injection scores for the volunteers aged 17-29 years and 30-55 years, post-IANB and buccal injections
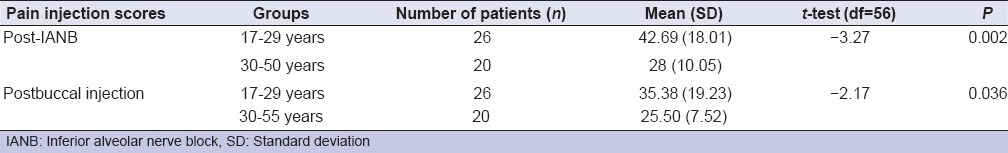
More comfortable during dental injection of local anesthetics than younger ones.
DISCUSSION
Pain control in dentistry is an important factor, to reduce the fear and anxiety associated with dental procedures. Better local anesthesia and treatment techniques may decrease cardiovascular risk caused by anxiety and improve the dental treatment.[12,13]
Although the sample size of this study was to some extent small because the difficulties in recruiting large number of volunteers, the results of this study showed that the volunteers in articaine group recorded earlier lip and teeth numbness and shorter onset time than those in mepivacaine group. These differences were statistically significant (P < 0.05). This outcome could be considered as good evidence to conclude that the use of articaine BI was faster in action than mepivacaine for securing pulp anesthesia in mandibular molars. This result is consistence with the findings from the study by Hawkins and Moore[11] who reported that the clinical advantages for using articaine infiltration includes rapid onset, longer duration of action and greater diffusing property over lignocaine and the elimination of the need for a painful palatal injection were demonstrated.
High lipid solubility of articaine, it might give the explanation for its advantage over mepivacaine in terms of earlier lip and teeth numbness and rapid onset time.[14] The presence of a tiophene ring increases articaine's potency and according to some authors[15,16] its ability to diffuse can produce pulpal anesthesia in mandibular teeth after infiltration anesthesia. Palatal anesthesia can also be achieved after maxillary BI.[17] High concentration of articain 4% used in this study could be the reason for its superiority over mepivacaine. A study by Gupta and Hopkins[18] demonstrated that the use of different doses of bupivacaine for supraclavicular block was not dependent on the concentration. Lowering the concentration or the strength of the local anesthetic leads to an increase in the volume required for a successful block. Kanaa et al.[19] reported that there was no significant difference in efficacy between 4% articaine with 1:100,000 epinephrine and 2% lidocaine with 1:80,000 epinephrine in achieving anesthesia in maxillary teeth with irreversible pulpitis after BI.
A result of the systematic review carried out by Meechan[20] provided support for the argument that articaine is more effective than lignocaine in providing anesthetic success in the first molar region for routine dental procedures. 4% articaine offers better clinical performance than 2% lidocaine, particularly in terms of latency and duration of the anesthetic effect. However, no statistically significant differences in anesthetic efficacy were recorded between the two solutions.[21,22] In addition, Ashraf et al.[23] conducted a double-blind randomized trial on 125 patients to compare the anesthetic success rate of BI injections of articaine and lidocaine when supplemented with an IANB using either 2% lidocaine or 4% articaine. The outcome of this study revealed that the combination of IANB with 4% articaine and BI with 4% articaine is more effective than lidocaine in performing the endodontic treatments of mandibular molars with irreversible pulpitis. 4% articaine without epinephrine is considered as a suitable anesthetic agent for the mandibular teeth extractions after IANB. It can be administered to the dental patient with conditions is a contraindication to epinephrine.[24] On the contrary, a study was conducted to evaluate the effect of supplemental lingual infiltration with 4% articaine of mandibular molars following an IANB with 2% lidocaine plus BI of 4% articaine in patients with irreversible pulpitis. Their findings revealed that the using of supplemental lingual infiltrations did not improve the anesthetic success after IANB plus BI.[25]
The findings of this study revealed that mepivacaine IANB injection was significantly more painful than articaine/mepivacaine buccal injection. Mepivacaine buccal injection was significantly more comfortable than articaine buccal injection. Increased discomfort of the injection following 2% mepivacaine IANB might be as a result of direct contact for the needle with IAN, speed of injection or patient with needle phobia.[19,26,27] Meechan[20] reported that the clinical impact of articaine's higher postinjection pain scores than lignocaine is negligible. It was found that volunteers aged between 17 and 29 years recorded significantly higher pain scores than volunteers aged between 30 and 55 years following either IANB or buccal injection (P < 0.01). So, older volunteers were significantly more comfortable during dental injection of local anesthetics than younger ones. This result is consistence with the findings from the study by Gazal et al.[28] who found that younger children were more distressed following the extraction of teeth under GA than those who were older.
CONCLUSION
Articaine has better potency, rapid onset of action, earlier lip and teeth numbness compared to the mepivacaine group. Articaine/mepivacaine buccal injection was significantly more comfortable than mepivacaine IANB. Further studies with large simple size are required to confirm these results.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
REFERENCES
- 1.Idris M, Sakkir N, Naik KG, Jayaram NK. Intraosseous injection as an adjunct to conventional local anesthetic techniques: A clinical study. J Conserv Dent. 2014;17:432–5. doi: 10.4103/0972-0707.139828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Meechan JG. Supplementary routes to local anaesthesia. Int Endod J. 2002;35:885–96. doi: 10.1046/j.1365-2591.2002.00592.x. [DOI] [PubMed] [Google Scholar]
- 3.Matthews R, Drum M, Reader A, Nusstein J, Beck M. Articaine for supplemental buccal mandibular infiltration anesthesia in patients with irreversible pulpitis when the inferior alveolar nerve block fails. J Endod. 2009;35:343–6. doi: 10.1016/j.joen.2008.11.025. [DOI] [PubMed] [Google Scholar]
- 4.Rogers BS, Botero TM, McDonald NJ, Gardner RJ, Peters MC. Efficacy of articaine versus lidocaine as a supplemental buccal infiltration in mandibular molars with irreversible pulpitis: A prospective, randomized, double-blind study. J Endod. 2014;40:753–8. doi: 10.1016/j.joen.2013.12.022. [DOI] [PubMed] [Google Scholar]
- 5.Monteiro MR, Groppo FC, Haiter-Neto F, Volpato MC, Almeida JF. 4% articaine buccal infiltration versus 2% lidocaine inferior alveolar nerve block for emergency root canal treatment in mandibular molars with irreversible pulpits: A randomized clinical study. Int Endod J. 2015;48:145–52. doi: 10.1111/iej.12293. [DOI] [PubMed] [Google Scholar]
- 6.Brandt RG, Anderson PF, McDonald NJ, Sohn W, Peters MC. The pulpal anesthetic efficacy of articaine versus lidocaine in dentistry: A meta-analysis. J Am Dent Assoc. 2011;142:493–504. doi: 10.14219/jada.archive.2011.0219. [DOI] [PubMed] [Google Scholar]
- 7.Jung IY, Kim JH, Kim ES, Lee CY, Lee SJ. An evaluation of buccal infiltrations and inferior alveolar nerve blocks in pulpal anesthesia for mandibular first molars. J Endod. 2008;34:11–3. doi: 10.1016/j.joen.2007.09.006. [DOI] [PubMed] [Google Scholar]
- 8.Kanaa MD, Whitworth JM, Corbett IP, Meechan JG. Articaine buccal infiltration enhances the effectiveness of lidocaine inferior alveolar nerve block. Int Endod J. 2009;42:238–46. doi: 10.1111/j.1365-2591.2008.01507.x. [DOI] [PubMed] [Google Scholar]
- 9.Dudkiewicz A, Schwartz S, Laliberté R. Effectiveness of mandibular infiltration in children using the local anesthetic Ultracaine (articaine hydrochloride) J Can Dent Assoc. 1987;53:29–31. [PubMed] [Google Scholar]
- 10.Pedlar J. Re: Prolonged paraesthesia following inferior alveolar nerve block using articaine. Br J Oral Maxillofac Surg. 2003;41:202. doi: 10.1016/s0266-4356(03)00030-5. [DOI] [PubMed] [Google Scholar]
- 11.Hawkins JM, Moore PA. Local anesthesia: Advances in agents and techniques. Dent Clin North Am. 2002;46:719–32. doi: 10.1016/s0011-8532(02)00020-4. ix. [DOI] [PubMed] [Google Scholar]
- 12.Gazal G, Fareed M, Zafar MS. Effectiveness of gaseous and intravenous inductions on children's anxiety and distress during extraction of teeth under general anesthesia. Saudi J Anaesth. 2015;9:33–36. doi: 10.4103/1658-354X.146282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Oliveira PC, Volpato MC, Ramacciato JC, Ranali J. Articaine and lignocaine efficiency in infiltration anaesthesia: A pilot study. Br Dent J. 2004;197:45–6. doi: 10.1038/sj.bdj.4811422. [DOI] [PubMed] [Google Scholar]
- 14.Wynn RL, Bergman SA, Meiller TF. Paresthesia associated with local anesthetics: A perspective on articaine. Gen Dent. 2003;51:498–501. [PubMed] [Google Scholar]
- 15.Lipp M, Daublander M. In: Proceedings of the International Symposium on Local Analgesia in Dentistry. London: Faculty of General Dental Practitioners; 1999. The German experience of articaine; pp. 21–2. [Google Scholar]
- 16.Sloss DR. In: Proceedings of the International Symposium on Local Analgesia in Dentistry. London: Faculty of General Dental Practitioners; 1999. Articaine in dental practice; pp. 23–4. [Google Scholar]
- 17.Stanley M. US Elsevier: Mosby. 5th ed 2004. Handbook of Local Anesthesia. [Google Scholar]
- 18.Gupta PK, Hopkins PM. Effect of concentration of local anaesthetic solution on the ED50 of bupivacaine for supraclavicular brachial plexus block. Br J Anaesth. 2013;111:293–6. doi: 10.1093/bja/aet033. [DOI] [PubMed] [Google Scholar]
- 19.Kanaa MD, Whitworth JM, Meechan JG. A prospective randomized trial of different supplementary local anesthetic techniques after failure of inferior alveolar nerve block in patients with irreversible pulpitis in mandibular teeth. J Endod. 2012;38:421–5. doi: 10.1016/j.joen.2011.12.006. [DOI] [PubMed] [Google Scholar]
- 20.Meechan JG. The use of the mandibular infiltration anesthetic technique in adults. J Am Dent Assoc. 2011;142:19S–24. doi: 10.14219/jada.archive.2011.0343. [DOI] [PubMed] [Google Scholar]
- 21.Kambalimath DH, Dolas RS, Kambalimath HV, Agrawal SM. Efficacy of 4% Articaine and 2% Lidocaine: A clinical study. J Maxillofac Oral Surg. 2013;12:3–10. doi: 10.1007/s12663-012-0368-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Thakare A, Bhate K, Kathariya R. Comparison of 4% articaine and 0.5% bupivacaine anesthetic efficacy in orthodontic extractions: Prospective, randomized crossover study. Acta Anaesthesiol Taiwan. 2014;52:59–63. doi: 10.1016/j.aat.2014.04.006. [DOI] [PubMed] [Google Scholar]
- 23.Ashraf H, Kazem M, Dianat O, Noghrehkar F. Efficacy of articaine versus lidocaine in block and infiltration anesthesia administered in teeth with irreversible pulpitis: A prospective, randomized, double-blind study. J Endod. 2013;39:6–10. doi: 10.1016/j.joen.2012.10.012. [DOI] [PubMed] [Google Scholar]
- 24.Dou L, Luo J, Yang D. Anaesthetic efficacy of supplemental lingual infiltration of mandibular molars after inferior alveolar nerve block plus buccal infiltration in patients with irreversible pulpitis. Int Endod J. 2013;46:660–5. doi: 10.1111/iej.12042. [DOI] [PubMed] [Google Scholar]
- 25.Kämmerer PW, Palarie V, Daubländer M, Bicer C, Shabazfar N, Brüllmann D, et al. Comparison of 4% articaine with epinephrine (1:100,000) and without epinephrine in inferior alveolar block for tooth extraction: Double-blind randomized clinical trial of anesthetic efficacy. Oral Surg Oral Med Oral Pathol Oral Radiol. 2012;113:495–9. doi: 10.1016/j.tripleo.2011.04.037. [DOI] [PubMed] [Google Scholar]
- 26.Beena JP. Dental subscale of children's fear survey schedule and dental caries prevalence. Eur J Dent. 2013;7:181–5. doi: 10.4103/1305-7456.110166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Alsarheed M. Children's Perception of Their Dentists. Eur J Dent. 2011;5:186–90. [PMC free article] [PubMed] [Google Scholar]
- 28.Gazal G, Bowman R, Worthington HV, Mackie IC. A double-blind randomized controlled trial investigating the effectiveness of topical bupivacaine in reducing distress in children following extractions under general anaesthesia. Int J Paediatr Dent. 2004;14:425–31. doi: 10.1111/j.1365-263X.2004.00587.x. [DOI] [PubMed] [Google Scholar]


