Abstract
Objective:
In general, chemical plaque agents have been used in mouthwashes, gels, and dentifrices. In some situations, application of mouthwashes and dentifrices can be difficult. Therefore, different approaches for oral health-care have been needed. The aim of this study was to evaluate the effect of propolis chewing-gum compared to propolis-containing mouthwash on gingival inflammation and plaque accumulation on patients that refrained from daily oral hygiene procedures for 5 days.
Materials and Methods:
10 college students with systemically healthy and very good oral hygiene and gingival health were included in this randomized, single-blind, crossover 5-day plaque regrowth with a 3-day washout period clinical study. After plaque scores were reduced to zero, participants were asked to refrain from oral hygiene procedures and allocated to either propolis mouthwash or chewing-gum group. Chewing-gum was performed after meals 3 times a day for 20 min mouthwash group was instructed to rinse mouthwash 2 times a day for 1 min. On day 5, the clinical periodontal measurements containing plaque and gingival indexes were taken from the participants.
Results:
The both plaque and gingival indexes of propolis mouthwash group were significantly lower than that of the propolis chewing-gum group (P = 0.005).
Conclusion:
It was demonstrated that the propolis mouthwash was more effective than the propolis chewing gum on the plaque inhibition and the gingival inflammation.
Keywords: Chewing gum, dental plaque, gingival inflammation, mouthwashes, propolis
INTRODUCTION
Chemical antibacterial plaque inhibitors are successfully used as mechanical oral hygiene procedures for providing supragingival cleaning. However, in long term use of the antibacterial chemicals like chlorhexidine have side effects such as bad taste and tooth discoloration.[1,2] Therefore, there is still a need for an antiplaque agent that can be convenient for per day usage and with minimal side-effects.
Antibacterial agents and certain natural products containing medical compounds are used in alternative medicine as therapeutic agents. Certain substances isolated from these products have many potential effects beyond their antimicrobial activity in the treatment, and prevention of periodontal disease has been shown. Among these Arab acaci,[3] eucalyptus extract,[4] mastic,[5] miswak[6] have been tested as antigingivitis and antiplaque agents.
Propolis is the most promising natural product used in the prevention of oral diseases. Natural bee product propolis is rigid resin and mainly contains wax and plant extracts. Propolis has many benefits for human health such as prevention of oral diseases.[7] It can be also used as an antibacterial, antiviral, antifungal,[8] antioxidant[9] and anti-inflammatory agent[10] in homeopathic and herbal health applications, and does not have any side effects.[11] Propolis applications have been shown to be useful in treating oral ulcers and gingivitis in many cases and clinical pilot study.[7,8,9,10,11,12] Propolis extract has antimicrobial activity against facultative anaerobes, Streptococcus mutans, and Gram-positive cocci that can be found in the human oral cavity.[13] Besides, a study evaluating the activity of propolis against periodontal pathogens have shown that propolis may be of clinical value.[14] To prevent tooth decay and treat gingivitis and stomatitis, it can be used as an active agent in mouthwash and toothpaste.[15] In certain studies, dentifrices with propolis have been shown to have excellent plaque removal, plaque prevention, and anti-inflammatory effects[16,17] propolis mouthwash can be an alternative to chemical rinse[7] and when used in subgingival irrigation better improvement of microbiological and clinical parameters are obtained when compared with conventional treatment have been shown.[18,19]
In general, chemical agents are used in toothpastes, mouthwashes, and gels.[20] However, in some cases, the use of mouthwashes and toothpastes are difficult.[21,22] Therefore, different tools are required for oral care. Chewing gums containing antiplaque agents have been tested as an additional tools for daily oral care.[6,7,8,9,10,11,12,13,14,15,16,17,18,19,20,21,22,23] Steinberg et al.[24] had been studied the release of the chlorhexidine from chewing-gum and showed that chewing gums may be an appropriate vehicle for the release of antiplaque agents.
In many countries, chewing gum regularly practiced by many people as a habit and this application has many benefits to oral health.[25] Indirect effects of chewing gum on oral health are saliva flow stimulation[26] and mechanical tooth cleaning.[27]
In the light of this information, it can be considered that the propolis gum might be a good tool to prevent gingival inflammation and plaque accumulation. So far, no study has used propolis gum and compared the efficacy of mouthwash with chewing-gum that both including propolis. The purpose of this study was to evaluate the effect of propolis gum compared to propolis-containing mouthwash on gingival inflammation and plaque accumulation on patients that refrain from daily oral hygiene procedures for 5 days.
MATERIALS AND METHODS
This study was planned as a randomized, single-blind, crossover, 5-day with 3-day washout period clinical study.
Participants
Approval for this study was obtained from the Ethical Committee for Clinical Research, Kirikkale University, School of Dentistry. 10 systemically healthy, nonsmoker college students with very good oral hygiene and gum health without any medical history were included in the study. Informed consent was obtained from participants before enrollment.
Study products
Commercially available propolis-containing gum (Bio BEE Propolis, BioHAYAT, Turkey) provides 0.5% propolis extract, %10 chestnut honey, %1 cinnamon.
Propolis mouthwash was prepared with propolis extract.
Preoperation inspection and prophylaxis
Before starting work, the clinical status of all participants was recorded, and plaque index[28] and gingival index[29] have been taken immediately and after each trial period. At the same time, all participants also had received professional teeth cleaning containing scaling, polishing, and floss applications.
Study design and protocol
Participants randomly divided into two groups including propolis chewing-gum and propolis mouthwash group. Investigator was blind. Participants were advised to refrain from any of the oral hygiene procedures (such as brushing teeth, dental floss) for 5-day. And then participants in chewing-gum group were instructed to use chewing gums 3 times after every meal for 20 min (a total of 1 h/day), and in mouthwash group participants were told to use propolis mouthwash 2 times a day for 1 min. At the end of the day 5th, participants came to the clinic and plaque index and gingival index were taken. Plaque accumulation was assessed on the facial and lingual aspects of all teeth following disclosure with erythrosine dye by a single investigator (NE). After that, 3-day washout period was conducted, in this period participants were applied normal hygiene procedures, following the wash-out period, professional teeth cleaning applications were performed to the participants to obtain zero plaque index scores and the procedure performed in the first period was changed with the other alternative procedure. At day 13th, final examination, similar to that performed at day 5th, took place. Before and after each experiment period professional teeth cleaning was performed to participants, and clinical periodontal measurements were recorded. All scoring assessments were performed by the same clinician.
Statistical analysis
The normality of the data distribution was examined using the Shapiro–Wilk test. Nonnormally distributed data were expressed. Wilcoxon Signed Rank test was also used in variables found significant differences for determining the groups leading to differences. SPSS for Windows Ver. 15.0 (SPSS Inc., Chicago, ILL, USA) and Microsoft Office Excel 2007 programs were used for statistical analysis. Statistical significance level P < 0.05 was significant considered.
RESULTS
Of the 10 selected subjects, 5 were males and 5 females, (age range 18–22 years) all completed the study satisfactorily. All subjects were successfully allocated to the treatments, and there was no drop-out during the study.
Mean full mouth plaque indexes and gingival indexes were used as the main outcome variables. During the study, no side effects from using the chewing gum or mouthwash were reported by the participants.
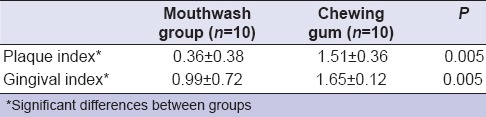
There was a significant difference in the both plaque and gingival indexes between the groups. The plaque index of the mouthwash group was significantly lower than that of the chewing-gum group (P = 0.005) and also the same results were also detectable for the gingival index in mouthwash group compared with chewing-gum group.
Summary statistics (median, interquartile range) of plaque and gingival indices for the propolis mouthwash and chewing-gum groups at day 5 are presented in Table 1.
Table 1.
Plaque and gingival indexes after the experimental period
DISCUSSION
The primary objective of this study was to evaluate the effects of propolis gum and mouthwash on de novo plaque formation on tooth surfaces and gingival inflammation over a 5-day period without mechanical oral hygiene following random use of either chewing-gum or mouthwash.
The degree of plaque accumulation and gingival inflammation was compared between groups (mouthwash and chewing-gum) (n = 10) and significantly lower plaque and gingival indices were measured after propolis mouthwash use compared to the values obtained with the propolis gum. A randomized, cross-over, single-blind design was chosen in order to avoid differences in response to the treatment by different individuals and the sample size used in this study was similar to other studies which have similar purposes like our study.[30,31]
Evidence shows that the mechanical removal of supragingival plaque is the most effective method for the prevention of the periodontal diseases.[32,33] It was demonstrated that the majority of patients have not got a sufficient motivation and skills for the usage of the oral hygiene products.[34] Because of the difficulty to ensure adequate removal of plaque by mechanical means, a need exists for adjunctive methods of mechanical plaque removal that are simple, inexpensive, and convenient for usage by the patients. Many different kinds of chemical substances have been investigated.[35] The major problem of these substances is the relative short contact time between the active agent and the teeth[36] and the existence of negative side effects.[2]
Among the various natural products, propolis has received greater attention due to its broad-spectrum antimicrobial activity against a wide range of pathogenic microorganisms. The mechanism of this inhibition is unknown but is thought to be related to the flavonoid content and cinamic acid of the product.[37] Propolis not only has a strong antibacterial,[38] antifungal,[39] antiviral,[40] antioxidant action,[9] but also has immunity enhancing,[41] pain and inflammation relieving, and wound repair accelerating effects.[42] Propolis plays a role as an anti-inflammatory agent by inhibiting prostaglandin synthesis, activating the thymus gland, supporting the immune system by increasing phagocytic activity, inducing cellular immunity and enhancing healing effects on epithelial tissue.[43] For this reason, it can be considered as a promising agent for the treatment or prevention of periodontal diseases.
Although there is a great interest in the use of antimicrobial agents to replace or to be adjuncts to the mechanical approaches[44] with which carriers, they will be delivered to the oral environment is not clear. The inability of the active product to be retained locally for a sufficient period is still a challenge.[45] It was stated that the effect of the most commonly used agent in formulations chlorhexidine is related to its release from the formulation. The formulations that release bactericides such as antibacterial varnishes and resins have an intrinsic disadvantage in that the effect is transient and greatly diminishes over time.[46]
Gum is a convenient tool for the delivery of many chemical compounds.[4,5,6,7,8,9,10,11,12,13,14,15,16,17,18,19,20,21,22,23] There have been many studies about the gum use as a tool for the transport of the medical substances.[25] The advantage of the use of chewing gum as a tool for drug delivery is it can be used ever, in any place without water and good stabilization of the product by the protection the content of the therapeutic agent from the oxygen, light and water. Gum causes both local (local delivery) and systemic effect by swallowing or absorption of the active agent through the oral mucosa.[47] And also the advantage of the gum instead of the mouth rinse is staying in mouth more longer times and thus lower doses of agents in the gum could be a release for extended periods.[21]
Hitherto, there has not been any work that compares the effect of mouthwash and chewing-gum containing propolis on periodontal parameters. This is the first study that has been compared the two different vehicles containing propolis in preventing plaque formation and gingival inflammation. Propolis extract was used in various forms[7,8,9,10,11,12,13,14,15,16,17,18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48] but in which form its mechanism of action will more effective in periodontal treatment is unknown. In the present study, it seems that the mouthwash form is more effective than chewing-gum on the plaque and gingival indexes. However, the other studies that compared the mouthwash and the chewing-gum obtained opposite results with our study. Ainamo et al.[49] showed that the use of chlorhexidine in the chewing-gum was as effective in plaque inhibition as in the use of chlorhexidine (0.2%) mouthwash 2 times a day, in another study that obtained the similar result was demonstrated that chlorhexidine chewing gum used with normal tooth cleaning provides similar adjunctive benefits to oral hygiene and gingival health as a 0.2% chlorhexidine rinse.[23] But, it should be emphasized that different agent was used in these studies unlike with our study and also our finding can be explained with the onset release of the propolis from the chewing-gum that may take longer than 20 min (the time participants chewed the gum) so that propolis in the gum failed to show its effect.
According to the results of this study, it may be speculated that the propolis mouthwash possesses better antiplaque and antigingivitis effect than propolis gum. This result is compatible with previous studies investigated the effect of the propolis mouthwash suggested that it might be used as a therapeutic, and alternative to chemical mouthwashes.[7,8,9,10,11,12,13,14,15,16,17,18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49]
CONCLUSIONS
Our data show that the propolis mouthwash is more effective than propolis gum on plaque accumulation and gingival inflammation. But further studies are needed to evaluate the efficacy of this gum formulation that will be chewed for more prolonged time as an adjunct to mechanical plaque control, both on plaque and gingivitis and propolis may be compared with other agents and also in different vehicles.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
REFERENCES
- 1.Greenstein G, Berman C, Jaffin R. Chlorhexidine. An adjunct to periodontal therapy. J Periodontol. 1986;57:370–7. doi: 10.1902/jop.1986.57.6.370. [DOI] [PubMed] [Google Scholar]
- 2.Flötra L, Gjermo P, Rölla G, Waerhaug J. Side effects of chlorhexidine mouth washes. Scand J Dent Res. 1971;79:119–25. doi: 10.1111/j.1600-0722.1971.tb02001.x. [DOI] [PubMed] [Google Scholar]
- 3.Gazi MI. The finding of antiplaque features in Acacia Arabica type of chewing gum. J Clin Periodontol. 1991;18:75–7. doi: 10.1111/j.1600-051x.1991.tb01123.x. [DOI] [PubMed] [Google Scholar]
- 4.Nagata H, Inagaki Y, Tanaka M, Ojima M, Kataoka K, Kuboniwa M, et al. Effect of eucalyptus extract chewing gum on periodontal health: A double-masked, randomized trial. J Periodontol. 2008;79:1378–85. doi: 10.1902/jop.2008.070622. [DOI] [PubMed] [Google Scholar]
- 5.Takahashi K, Fukazawa M, Motohira H, Ochiai K, Nishikawa H, Miyata T. A pilot study on antiplaque effects of mastic chewing gum in the oral cavity. J Periodontol. 2003;74:501–5. doi: 10.1902/jop.2003.74.4.501. [DOI] [PubMed] [Google Scholar]
- 6.Amoian B, Moghadamnia AA, Barzi S, Sheykholeslami S, Rangiani A. Salvadora Persica extract chewing gum and gingival health: Improvement of gingival and probe-bleeding index. Complement Ther Clin Pract. 2010;16:121–3. doi: 10.1016/j.ctcp.2009.11.002. [DOI] [PubMed] [Google Scholar]
- 7.Dodwad V, Kukreja BJ. Propolis mouthwash: A new beginning. J Indian Soc Periodontol. 2011;15:121–5. doi: 10.4103/0972-124X.84379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kujumgiev A, Tsvetkova I, Serkedjieva Y, Bankova V, Christov R, Popov S. Antibacterial, antifungal and antiviral activity of propolis of different geographic origin. J Ethnopharmacol. 1999;64:235–40. doi: 10.1016/s0378-8741(98)00131-7. [DOI] [PubMed] [Google Scholar]
- 9.Russo A, Longo R, Vanella A. Antioxidant activity of propolis: Role of caffeic acid phenethyl ester and galangin. Fitoterapia. 2002;73(Suppl 1):S21–9. doi: 10.1016/s0367-326x(02)00187-9. [DOI] [PubMed] [Google Scholar]
- 10.Mossalayi MD, Rambert J, Renouf E, Micouleau M, Mérillon JM. Grape polyphenols and propolis mixture inhibits inflammatory mediator release from human leukocytes and reduces clinical scores in experimental arthritis. Phytomedicine. 2014;21:290–7. doi: 10.1016/j.phymed.2013.08.015. [DOI] [PubMed] [Google Scholar]
- 11.Miguel MG, Antunes MD. Is propolis safe as an alternative medicine? J Pharm Bioallied Sci. 2011;3:479–95. doi: 10.4103/0975-7406.90101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Martínez Silveira G, Gou Godoy A, Oña Torriente R, Palmer Ortiz MC, Falcón Cuéllar MA. Preliminary study of the effects of propolis in the treatment of chronic gingivitis and oral ulceration. Rev Cubana Estomatol. 1988;25:36–44. [PubMed] [Google Scholar]
- 13.Koo H, Gomes BP, Rosalen PL, Ambrosano GM, Park YK, Cury JA. In vitro antimicrobial activity of propolis and Arnica montana against oral pathogens. Arch Oral Biol. 2000;45:141–8. doi: 10.1016/s0003-9969(99)00117-x. [DOI] [PubMed] [Google Scholar]
- 14.Gebara EC, Lima LA, Mayer MP. Propolis antimicrobial activity against periodontopathic bacteria. Braz J Microbiol. 2002;33:365–9. [Google Scholar]
- 15.Gómez-Caravaca AM, Gómez-Romero M, Arráez-Román D, Segura-Carretero A, Fernández-Gutiérrez A. Advances in the analysis of phenolic compounds in products derived from bees. J Pharm Biomed Anal. 2006;41:1220–34. doi: 10.1016/j.jpba.2006.03.002. [DOI] [PubMed] [Google Scholar]
- 16.Botushanov PI, Grigorov GI, Aleksandrov GA. A clinical study of a silicate toothpaste with extract from propolis. Folia Med (Plovdiv) 2001;43:28–30. [PubMed] [Google Scholar]
- 17.Morawiec T, Dziedzic A, Niedzielska I, Mertas A, Tanasiewicz M, Skaba D, et al. The biological activity of propolis-containing toothpaste on oral health environment in patients who underwent implant-supported prosthodontic rehabilitation. Evid Based Complement Alternat Med 2013. 2013 doi: 10.1155/2013/704947. 704947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Gebaraa EC, Pustiglioni AN, de Lima LA, Mayer MP. Propolis extract as an adjuvant to periodontal treatment. Oral Health Prev Dent. 2003;1:29–35. [PubMed] [Google Scholar]
- 19.Coutinho A. Honeybee propolis extract in periodontal treatment: A clinical and microbiological study of propolis in periodontal treatment. Indian J Dent Res. 2012;23:294. doi: 10.4103/0970-9290.100449. [DOI] [PubMed] [Google Scholar]
- 20.van der Ouderaa FJ. Anti-plaque agents. Rationale and prospects for prevention of gingivitis and periodontal disease. J Clin Periodontol. 1991;18:447–54. doi: 10.1111/j.1600-051x.1991.tb02315.x. [DOI] [PubMed] [Google Scholar]
- 21.Simons D, Brailsford S, Kidd EA, Beighton D. The effect of chlorhexidine acetate/xylitol chewing gum on the plaque and gingival indices of elderly occupants in residential homes. J Clin Periodontol. 2001;28:1010–5. doi: 10.1034/j.1600-051x.2001.281104.x. [DOI] [PubMed] [Google Scholar]
- 22.Nuuja T, Meurman JH, Murtomaa H, Kortelainen S, Metteri J. The effect of a combination of chlorhexidine diacetate, sodium fluoride and xylitol on plaque wet weight and periodontal index scores in military academy cadets refraining from mechanical tooth cleaning for 7-day experimental periods. J Clin Periodontol. 1992;19:73–6. doi: 10.1111/j.1600-051x.1992.tb00443.x. [DOI] [PubMed] [Google Scholar]
- 23.Smith AJ, Moran J, Dangler LV, Leight RS, Addy M. The efficacy of an anti-gingivitis chewing gum. J Clin Periodontol. 1996;23:19–23. doi: 10.1111/j.1600-051x.1996.tb00499.x. [DOI] [PubMed] [Google Scholar]
- 24.Steinberg LM, Odusola F, Mandel ID. Remineralizing potential, antiplaque and antigingivitis effects of xylitol and sorbitol sweetened chewing gum. Clin Prev Dent. 1992;14:31–4. [PubMed] [Google Scholar]
- 25.Imfeld T. Chewing gum – facts and fiction: A review of gum-chewing and oral health. Crit Rev Oral Biol Med. 1999;10:405–19. doi: 10.1177/10454411990100030901. [DOI] [PubMed] [Google Scholar]
- 26.Dawes C, Macpherson LM. Effects of nine different chewing-gums and lozenges on salivary flow rate and pH. Caries Res. 1992;26:176–82. doi: 10.1159/000261439. [DOI] [PubMed] [Google Scholar]
- 27.Addy M, Perriam E, Sterry A. Effects of sugared and sugar-free chewing gum on the accumulation of plaque and debris on the teeth. J Clin Periodontol. 1982;9:346–54. doi: 10.1111/j.1600-051x.1982.tb02101.x. [DOI] [PubMed] [Google Scholar]
- 28.Turesky S, Gilmore ND, Glickman I. Reduced plaque formation by the chloromethyl analogue of victamine C. J Periodontol. 1970;41:41–3. doi: 10.1902/jop.1970.41.41.41. [DOI] [PubMed] [Google Scholar]
- 29.Loe H. The gingival index, the plaque index and the retention index systems. J Periodontol. 1967;38:610–6. doi: 10.1902/jop.1967.38.6.610. [DOI] [PubMed] [Google Scholar]
- 30.Quirynen M, Avontroodt P, Peeters W, Pauwels M, Coucke W, van Steenberghe D. Effect of different chlorhexidine formulations in mouthrinses on de novo plaque formation. J Clin Periodontol. 2001;28:1127–36. doi: 10.1034/j.1600-051x.2001.281207.x. [DOI] [PubMed] [Google Scholar]
- 31.Sekino S, Ramberg P, Uzel NG, Socransky S, Lindhe J. Effect of various chlorhexidine regimens on salivary bacteria and de novo plaque formation. J Clin Periodontol. 2003;30:919–25. doi: 10.1034/j.1600-051x.2003.00420.x. [DOI] [PubMed] [Google Scholar]
- 32.Loe H, Theilade E, Jensen SB. Experimental gingivitis in man. J Periodontol. 1965;36:177–87. doi: 10.1902/jop.1965.36.3.177. [DOI] [PubMed] [Google Scholar]
- 33.van der Weijden F, Slot DE. Oral hygiene in the prevention of periodontal diseases: The evidence. Periodontol 2000. 2011;55:104–23. doi: 10.1111/j.1600-0757.2009.00337.x. [DOI] [PubMed] [Google Scholar]
- 34.Lindhe J, Koch G. The effect of supervised oral hygiene on the gingiva of children. Progression and inhibition of gingivitis. J Periodontal Res. 1966;1:260–7. doi: 10.1111/j.1600-0765.1966.tb01870.x. [DOI] [PubMed] [Google Scholar]
- 35.Hancock EB. Periodontal diseases: Prevention. Ann Periodontol. 1996;1:223–49. doi: 10.1902/annals.1996.1.1.223. [DOI] [PubMed] [Google Scholar]
- 36.Oosterwaal PJ, Mikx FH, van den Brink ME, Renggli HH. Bactericidal concentrations of chlorhexidine-digluconate, amine fluoride gel and stannous fluoride gel for subgingival bacteria tested in serum at short contact times. J Periodontal Res. 1989;24:155–60. doi: 10.1111/j.1600-0765.1989.tb00871.x. [DOI] [PubMed] [Google Scholar]
- 37.Bankova V, Christov R, Kujumgiev A, Marcucci MC, Popov S. Chemical composition and antibacterial activity of Brazilian propolis. Z Naturforsch C. 1995;50:167–72. doi: 10.1515/znc-1995-3-402. [DOI] [PubMed] [Google Scholar]
- 38.Kujumgiev A, Bankova V, Ignatova A, Popov S. Antibacterial activity of propolis, some of its components and their analogs. Pharmazie. 1993;48:785–6. [PubMed] [Google Scholar]
- 39.Ota C, Unterkircher C, Fantinato V, Shimizu MT. Antifungal activity of propolis on different species of Candida. Mycoses. 2001;44:375–8. doi: 10.1046/j.1439-0507.2001.00671.x. [DOI] [PubMed] [Google Scholar]
- 40.Amoros M, Sauvager F, Girre L, Cormier M. In vitro anti-viral activity of propolis. Apidologie. 1992;23:231–40. [Google Scholar]
- 41.Orsolic N, Basic I. Immunomodulation by water-soluble derivative of propolis: A factor of antitumor reactivity. J Ethnopharmacol. 2003;84:265–73. doi: 10.1016/s0378-8741(02)00329-x. [DOI] [PubMed] [Google Scholar]
- 42.Burdock GA. Review of the biological properties and toxicity of bee propolis (propolis) Food Chem Toxicol. 1998;36:347–63. doi: 10.1016/s0278-6915(97)00145-2. [DOI] [PubMed] [Google Scholar]
- 43.Ozan F, Sümer Z, Polat ZA, Er K, Ozan U, Deger O. Effect of mouthrinse containing propolis on oral microorganisms and human gingival fibroblasts. Eur J Dent. 2007;1:195–201. [PMC free article] [PubMed] [Google Scholar]
- 44.Wilson M. Susceptibility of oral bacterial biofilms to antimicrobial agents. J Med Microbiol. 1996;44:79–87. doi: 10.1099/00222615-44-2-79. [DOI] [PubMed] [Google Scholar]
- 45.Schwach-Abdellaoui K, Vivien-Castioni N, Gurny R. Local delivery of antimicrobial agents for the treatment of periodontal diseases. Eur J Pharm Biopharm. 2000;50:83–99. doi: 10.1016/s0939-6411(00)00086-2. [DOI] [PubMed] [Google Scholar]
- 46.Faraj JA, Dorati R, Schoubben A, Worthen D, Selmin F, Capan Y, et al. Development of a peptide-containing chewing gum as a sustained release antiplaque antimicrobial delivery system. AAPS Pharm Sci Tech. 2007;8:26. doi: 10.1208/pt0801026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Ly KA, Milgrom P, Rothen M. The potential of dental-protective chewing gum in oral health interventions. J Am Dent Assoc. 2008;139:553–63. doi: 10.14219/jada.archive.2008.0215. [DOI] [PubMed] [Google Scholar]
- 48.Pereira EM, da Silva JL, Silva FF, De Luca MP, Ferreira EF, Lorentz TC, et al. Clinical evidence of the efficacy of a mouthwash containing propolis for the control of plaque and gingivitis: A phase II study. Evid Based Complement Alternat Med 2011. 2011 doi: 10.1155/2011/750249. 750249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Ainamo J, Nieminen A, Westerlund U. Optimal dosage of chlorhexidine acetate in chewing gum. J Clin Periodontol. 1990;17:729–33. doi: 10.1111/j.1600-051x.1990.tb01061.x. [DOI] [PubMed] [Google Scholar]


