Abstract
The aim of the periodontal treatment is to provide healthy and functional dentition all through a lifetime. In this report, periodontal treatment of a 42-year-old male patient with generalized severe chronic periodontitis is presented. He received initial periodontal treatment together with adjunctive antimicrobials. The devital teeth were endodontically treated, and free gingival grafts were placed at the inadequate keratinized tissue zones before regenerative surgery. Following the surgical treatment using enamel matrix derivatives and xenogenic bone graft combination, the patient was put on a strict recall program. After 12 months, favorable clinical and radiographical improvements were obtained. The 7-year maintenance of the present case with several initially hopeless teeth has been shown and discussed in this report. It can be concluded that optimum oral hygiene level as well as the positive cooperation of the patient enhanced the success of periodontal treatment results even in extremely severe periodontal destruction.
Keywords: Enamel matrix protein derivative, hopeless tooth, long-term, periodontal surgery, severe chronic periodontitis
INTRODUCTION
Chronic periodontitis is a multifactorial infectious disease occurs as a result of challenge between the host response and specific periodontal pathogens characterized by the manifestation of a slow irreversible damage of periodontal supporting tissue loss in a period of time.[1] It has been shown that deep periodontal pockets as a result of alveolar bone destruction have been associated with the increase in the number of tooth loss.[2] It is difficult to define precise prognosis for each individual tooth as well as the overall dentition, however, the key for the success in predicting the prognosis is generally based on knowledge of the literature, accurate compilation of clinical and radiographic parameters, past clinical and surgical experiences and consideration of patient's values and compliance.[3] The aim of this report is to present the 7-year clinical and radiographic follow-up results of periodontal treatment of a patient with generalized severe chronic periodontitis.
CASE REPORT
A 42-year-old male, systemically healthy, nonsmoker patient with generalized severe chronic periodontitis was treated. The periodontal family history of the patient did not reveal any severe periodontal destruction or early tooth loss. The patient did not receive any periodontal treatment previously. The oral examination revealed severe gingival inflammation, suppuration, multiple periodontal abscesses [Figure 1], halitosis, severe teeth mobility, and radiographically established widespread horizontal/vertical severe bone loss [Figure 1]. Furthermore, radiographic examination revealed perio-endo lesions on teeth 25, 36 and 45. Initial periodontal therapy (IPT), endodontic treatment of devital teeth and regenerative periodontal surgery as well as resective procedures was planned for the treatment.
Figure 1.

Clinical and radiographic view of the patient before initial periodontal therapy
Treatment procedures
The patient received IPT including oral hygiene instructions, scaling and root planing using both hand and ultrasonic instruments. Endodontic treatment was implemented to the devital teeth 25, 36, and 45 at least 3 months before surgeries. Following IPT, free gingival grafts (FGG) were placed at the insufficient keratinized tissue zones (tooth numbers 36–35 and 45–46) before the regenerative surgeries [Figure 2a–c].
Figure 2.

(a) One of the free gingival grafts placed on inadequate keratinized tissue zones (b) one month after (c) 12 months after clinical view
The flap surgeries were performed in two separate sessions as for maxilla and mandible. Enamel matrix derivatives (EMD) in gel form (Emdogain®, Straumann) and bovine-derived xenograft (BDX) (BioOss®, Geistlich) combination was used for the treatment of intrabony defects [Figure 3]. For postoperative care the patient received amoxicillin + potassium clavulanate twice a day for 7 days, naproxen sodium, twice a day for 7 days and 0.12% chlorhexidine + benzydamine hydrochloride mouth rinse, twice a day for 4 weeks. Mechanical tooth cleaning was not allowed in the surgical area for the first 4 postoperative weeks. Sutures were removed at 14 days following the surgery. Patient was put on strict recall visits (every 2nd week during the first 2 months postoperatively and once a month for the 1-year observation period). Supportive periodontal treatment was carried out with 4–6 months intervals after 1-year. However, at the 5th year the patient was irregular with his recall sessions and claimed inadvertent reason of spinal surgery. At the end of 7-year follow-up period, extraction of 14 was decided due to increased mobility and extracted tooth crown was splinted to the related region by the use of a fiber adhesive system.
Figure 3.

Clinical view of the intrabony defects during maxillary flap operation
Besides the regenerative procedures, two different periodontal techniques were also implemented in the mandible during the operation. One of them was root resection on tooth number 47 at which a fracture was detected on the mesiobuccal root [Figure 4a–d]. The other application was the tunnel preparation instead of the indicated root resection on tooth 36 [Figure 4e-h]. Since the patient was very eager and insisted on keeping the whole dentition and very good at performing oral hygiene procedures, this tooth was attempted to be kept without removing the distal root.
Figure 4.
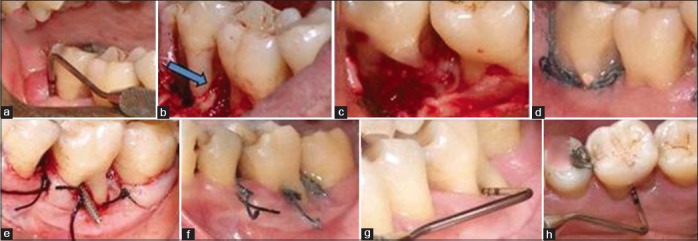
(a) Fistula around tooth number 47 (b) root fracture detected during surgery (c) root resection (d) obstruction of the root canal and 1-week after surgery (e) just after the tunnel operation of tooth number 36 (f) 1-week after the operation (g) 1-month after from buccal aspect (h) 1-month after from lingual aspect
Treatment outcomes
Postoperative healing was uneventful after both surgical sessions. At 12 months, there were considerable clinical and radiographic improvements in all parameters [Table 1]. The obtained clinical and radiographical results were maintained over a period of 7 years. One tooth (number 14) with increasing mobility was lost at the end of 7th year. Tooth number 36 revealed a persisting periapical radiolucency [Figure 5 and Table 1].
Table 1.
Change of the periodontal parameters
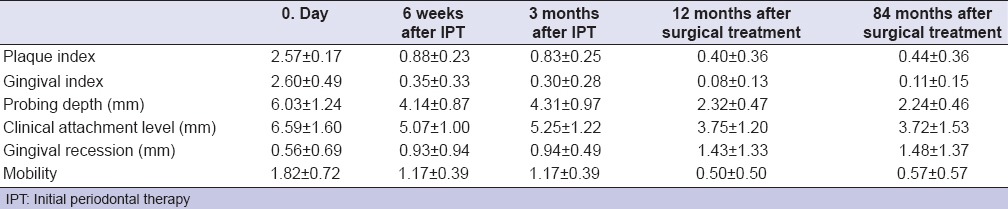
Figure 5.

Clinical and radiographic view 84 months after the operations
DISCUSSION
This case presents the outcomes of regenerative and resective periodontal treatments applied on teeth clinically defined as having hopeless prognosis as a consequence of the presence of a chronic perio-endo lesion and/or attachment loss together with severe periodontal destruction.
The clinical difference between chronic and aggressive periodontitis especially in generalized forms is not clear.[4] The extent and amount of clinical inflammation in generalized aggressive periodontitis appear to be similar to that observed in chronic periodontitis.[4] At that point, clear diagnostic distinction can be made according to age of onset and patients’ family history.[4] In this case, 42-year-old patient affirmed that there were not any individuals with a history of severe destruction or early tooth loss in his family. According to the revealed anamnesis together with the positive correlation between the presence of the local etiological factors and the extent of inflammation, patient was diagnosed as generalized chronic periodontitis.
Recently, continuous multilevel risk assessment-based prognostication systems were proposed.[5,6] In the light of these evidences, it seems possible to retain a tooth with negative prognosis in a well-maintained cooperative patient.[7] In this case, all teeth were treated periodontally and retained with multidisciplinary perio-endo treatment, and favorable clinical improvements were obtained to change their prognosis at 1-year from “hopeless” to “maintainable” condition. Only one premolar tooth was extracted at the end of the 7th year due to the increasing mobility and tooth number 36 revealed periapical radiolucency on the radiograph without any clinical symptoms.
Based on existing evidence, the American Academy of Periodontology suggested several indications for gingival augmentation procedures.[8] We placed FGG onto the insufficient keratinized tissue zones after IPT before flap surgeries.
Today, by the help of various new technologies, biological approaches and biomaterials, the challenge is now to introduce the experience and knowledge contributing to patient outcomes in terms of function, ease of care, esthetics, and long-term maintenance.[9] There are various biomaterial combinations used in the regeneration of periodontal bone defects.[10,11,12] It has been shown that the use of EMD combined with bone graft materials is promising and useful for periodontal regeneration.[13] In this patient, EMD + BDX was used as the regenerative combination. The results of a recent study showed that hopeless teeth can be treated successfully with various regenerative combinations and maintained over a period of 5 years in health and function.[14] The present case report parallel with the aforementioned study revealed encouraging results for regenerative interventions to be considered as suitable alternatives to the extraction of severely compromised teeth with intrabony defects to or beyond the root apex.[14] However, the importance of patient selection, clinicians’ experience and skill, the scientific evidence, treatment plan, a cost/benefit analysis and a strict periodontal supportive care program must be underlined as the keys for the success of periodontal treatment approaches.[14] Although periodontists are recognized as more skilled in predicting tooth prognosis, we must remember that treatment protocol does not work in any case if the patient compliance does not exist.[3]
Within the limits, the following conclusions can be made:
Periodontal regeneration and perio-endo treatment improved the prognosis of hopeless teeth. Teeth had clinically-stable periodontal parameters, comfort and function over 7 years
Periodontal regeneration may be a proper alternative to tooth extraction in teeth compromised by extremely severe intrabony defects
Patient cooperation and his/her health belief and oral hygiene level are of critical importance to provide a healthy/functional dentition and to enhance the success of periodontal treatment in the long-term.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared
REFERENCES
- 1.Kornman KS. Mapping the pathogenesis of periodontitis: A new look. J Periodontol. 2008;79(8 Suppl):1560–8. doi: 10.1902/jop.2008.080213. [DOI] [PubMed] [Google Scholar]
- 2.Matuliene G, Pjetursson BE, Salvi GE, Schmidlin K, Brägger U, Zwahlen M, et al. Influence of residual pockets on progression of periodontitis and tooth loss: Results after 11 years of maintenance. J Clin Periodontol. 2008;35:685–95. doi: 10.1111/j.1600-051X.2008.01245.x. [DOI] [PubMed] [Google Scholar]
- 3.Kao RT. Strategic extraction: A paradigm shift that is changing our profession. J Periodontol. 2008;79:971–7. doi: 10.1902/jop.2008.070551. [DOI] [PubMed] [Google Scholar]
- 4.Kwok V, Caton JG. Commentary: Prognosis revisited: A system for assigning periodontal prognosis. J Periodontol. 2007;78:2063–71. doi: 10.1902/jop.2007.070210. [DOI] [PubMed] [Google Scholar]
- 5.Armitage GC, Cullinan MP. Comparison of the clinical features of chronic and aggressive periodontitis. Periodontol 2000. 2010;53:12–27. doi: 10.1111/j.1600-0757.2010.00353.x. [DOI] [PubMed] [Google Scholar]
- 6.Lang NP, Tonetti MS. Periodontal diagnosis in treated periodontitis. Why, when and how to use clinical parameters. J Clin Periodontol. 1996;23:240–50. doi: 10.1111/j.1600-051x.1996.tb02083.x. [DOI] [PubMed] [Google Scholar]
- 7.DeVore CH, Beck FM, Horton JE. Retained “hopeless” teeth. Effects on the proximal periodontium of adjacent teeth. J Periodontol. 1988;59:647–51. doi: 10.1902/jop.1988.59.10.647. [DOI] [PubMed] [Google Scholar]
- 8.Consensus report. Mucogingival therapy. Ann Periodontol. 1996;1:702–6. doi: 10.1902/annals.1996.1.1.702. [DOI] [PubMed] [Google Scholar]
- 9.Yilmaz S, Kuru B, Altuna-Kiraç E. Enamel matrix proteins in the treatment of periodontal sites with horizontal type of bone loss. J Clin Periodontol. 2003;30:197–206. doi: 10.1034/j.1600-051x.2003.10190.x. [DOI] [PubMed] [Google Scholar]
- 10.Meseli SE, Agrali OB, Peker O, Kuru L. Treatment of lateral periodontal cyst with guided tissue regeneration. Eur J Dent. 2014;8:419–23. doi: 10.4103/1305-7456.137661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sumer M, Keles GC, Cetinkaya BO, Balli U, Pamuk F, Uckan S. Autogenous cortical bone and bioactive glass grafting for treatment of intraosseous periodontal defects. Eur J Dent. 2013;7:6–14. [PMC free article] [PubMed] [Google Scholar]
- 12.Keles GC, Sumer M, Cetinkaya BO, Tutkun F, Simsek SB. Effect of autogenous cortical bone grafting in conjunction with guided tissue regeneration in the treatment of intraosseous periodontal defects. Eur J Dent. 2010;4:403–11. [PMC free article] [PubMed] [Google Scholar]
- 13.Li W, Xiao L, Hu J. The use of enamel matrix derivative alone versus in combination with bone grafts to treat patients with periodontal intrabony defects: A meta-analysis. J Am Dent Assoc. 2012;143:e46–56. doi: 10.14219/jada.archive.2012.0327. [DOI] [PubMed] [Google Scholar]
- 14.Cortellini P, Stalpers G, Mollo A, Tonetti MS. Periodontal regeneration versus extraction and prosthetic replacement of teeth severely compromised by attachment loss to the apex: 5-year results of an ongoing randomized clinical trial. J Clin Periodontol. 2011;38:915–24. doi: 10.1111/j.1600-051X.2011.01768.x. [DOI] [PubMed] [Google Scholar]


