Abstract
With decreased equipment cost, provision of ultrasound is now feasible in some low resource settings. Screening obstetric ultrasound may identify potential pregnancy complications and with this knowledge, allow women to plan to deliver at the appropriate level of care. In this paper we describe a ten-day course with quality assurance activities to train ultrasound-naïve non-physician healthcare professionals at mid-level health facilities to perform screening obstetric ultrasound. Those trained will participate in a cluster-randomized controlled trial to assess the impact of screening obstetric ultrasound on maternal and newborn outcomes.
Keywords: Screening obstetric ultrasound, complicated pregnancy, low and middle income countries
Introduction
Obstetric ultrasound is widely utilized in upper income countries for screening and for evaluation of pregnancy complications, but its use in lower income countries has been limited. Advances in technology in the last several years have resulted in significant reductions in cost, complexity and size of ultrasound equipment. This has increased the potential for more widespread use of obstetric ultrasound in low and middle income countries (LMIC). Studies have shown that obstetric ultrasound in rural settings in LMIC can improve diagnosis of antenatal complications [1–3]. With the shortage of sonographers and physicians trained in ultrasound in these settings [4], it may be valuable to train other cadres of healthcare personnel in basic obstetric ultrasound screening to serve as medical extenders of hospital-based sonographers. By doing so, obstetric ultrasound may reach more remote populations and help inform women to deliver at the appropriate health facilities.
Ultrasound training in LMIC has been described in several prior studies [1, 5–11]. These training programs have varied in length (5 days to 9 months), subject matter (general ultrasound, obstetrics, emergency medicine) and trainee background (physicians, clinical officers, nurses, midwives). In this paper we describe an intensive 10 day training program in screening obstetric ultrasound followed by a three-month observation and review period, targeted to ultrasound-naïve, non-physician healthcare professionals. Those trained will participate in a study to assess the impact of screening obstetric ultrasound provided at antenatal care in health centers on maternal and newborn outcomes in mostly rural settings.
The details of the study are described elsewhere [12]. Briefly, this cluster-randomized controlled trial (RCT) funded by the Bill and Melinda Gates Foundation and GE Healthcare, is taking place under the auspices of the Global Network for Women’s and Children’s Health Research (the Global Network) and Research Triangle Institute (RTI). The Global Network is a multi-country research network supported by the Eunice Kennedy Shriver National Institute of Child Health and Human Development in which virtually all pregnancy outcomes in the current study clusters are captured through a Maternal-Newborn Health Registry, which was established in 2008 [13]. The study clusters are located in Global Network sites in Chimaltenango District, Guatemala; Kafue and Chongwe Districts, Zambia; Equateur Provence, Democratic Republic of Congo; Busia and Bungoma Counties, Western Provence, Kenya; and Thatta District, Pakistan. For the trial, there are 29 intervention and 29 control clusters, each with approximately 500 births per year.
At the intervention sites, healthcare workers trained in ultrasound will offer screening obstetric ultrasound examinations to patients presenting for routine antenatal visits at 18 to 22 weeks and again at 32 to 36 weeks. Patients identified with complicated or potentially complicated pregnancies (multiple gestation, malpresentation, placenta previa, amniotic fluid abnormalities, intrauterine growth restriction) will be informed of their condition and advised to seek care at an appropriate study healthcare facility according to established referral algorithms. Those patients without complicated pregnancies will be encouraged to deliver at the health center or other facility rather than at home, per local guidelines.
Several outcomes will be evaluated for the trial. The primary outcome is a composite of maternal mortality, maternal near miss, stillbirth, and neonatal mortality. The secondary outcome is the rate of antenatal care utilization and the utilization of health facilities for delivery for women with complicated pregnancies. The effectiveness of the training component will also be evaluated as described below.
In this paper we describe the training component which was developed for this multi-country RCT. Trial results will published on completion of the RCT.
Training Component
The training component of the study (ultrasound course, quality assurance, continuing education) is funded by GE Healthcare and is overseen by the University of Washington, Department of Radiology (UW). In prior discussions with funders it was suggested that UW develop a training component and test its effectiveness in pilot projects. Promising results could then lead to additional funding. With support from GE Foundation, UW partnered with the Ernest Cook Ultrasound Research and Education Institute (ECUREI) in Kampala, Uganda, to develop six-week and four-week screening obstetric courses utilized in two pilot projects in Uganda [14]. Training for the six-week course took place entirely at the ECUREI facility in Kampala. Training for the four-week course took place at ECUREI as well as in the field. Forty-four midwives completed training in the two courses.
UW, at the request of the Millennium Promise, its partner in Isingiro District in Uganda, refined the curriculum to a 10-day course to be conducted at local health facilities and followed by a three month period of observation and review. The aim of this approach was to reduce travel and lodging expenses and limit the time in which trainees were away from their health centers. Two rounds of training using this targeted approach were conducted in the Isingiro District, first by a UW trainer with a local sonographer and then by the local sonographer alone. Based on on-site practical testing by one of the authors (RN), trainees from these later rounds of training tested favorably compared with those from earlier, longer trainings in Kampala. For the five-country Global Network Study, UW elected to conduct trainings at referral hospitals rather than at a central institute and to use the targeted 10-day curriculum, followed by a three month observation and review period at intervention cluster health centers.
The objectives of the course are to teach trainees to perform screening obstetric ultrasound in conjunction with routine antenatal care and to use the results to refer patients to routine follow-up or to a higher level of care. Elements of training include didactic and hands-on instruction, distribution of printed materials, an algorithm approach to follow-up adapted to the local environment, extensive quality assurance activities, and educational outreach visits. Applying lessons learned in prior trainings, the course focuses only on topics necessary to conduct screening ultrasound, emphasizes practical scanning skills and communication with the patient, and incorporates local sonographers in the training.
At the outset, we established that one-third of course time would be devoted to didactic sessions and two-thirds to practical scanning. We also decided to tightly “script” each day, which would include a detailed daily schedule, speaker notes for each PowerPoint slide, and explicit instructions for each practical scanning session. We felt that it was important to plan for trainee attrition during the study. By including a trainer/sonographer from each site in the initial trainings and providing that sonographer with a detailed training blueprint, we felt we would adequately equip that sonographer to become the primary trainer for future courses.
Curriculum Development
The curriculum was developed by a team consisting of an academic radiologist, a private practice radiologist, a sonographer/instructor, and a curriculum consultant from the International Training and Education Center for Health (I-TECH). Each member of the team was experienced in teaching or writing training programs for low-income settings. The team first generated a list of topics that would be necessary to achieve the objectives of the course. Foundational topics included patient communication, safety, and comfort; infection prevention and control; care and security of the equipment; ultrasound physics and instrumentation; and anatomic planes and introduction to tomography. The topics for screening obstetric ultrasound included cardiac activity, fetal number, fetal position, amniotic fluid volume, gestational age, placenta and cervix, fetal growth and well-being, and gross anomalies. Although not part of the screening program, we recognized that patients with complications in the 1st trimester who presented to the study intervention centers would benefit from ultrasound. We therefore included in the course identification of early fetal demise, blighted ovum, ectopic pregnancy, incomplete abortion, and molar pregnancy.
The topics were organized into individual lectures and the team then determined specific points to be covered and images and graphics necessary to help convey those points. One member of the team produced a PowerPoint slide set for each topic, which was reviewed by the other members of the team. The team collaborated on speaker notes for each slide in the set. The slide set was then sent to the I-TECH consultant who edited the text and added graphics to reinforce the material. The slide set was again reviewed and edited until a final version was agreed upon. Each resulting lecture consists of learning objectives, key terms, and the lecture material with speaker notes, a summary, and questions for review. Case studies added at the end of the course were designed to stimulate group discussions on appropriate patient management by synthesizing clinical and ultrasound findings. The topics covered in the case studies were management of placenta previa, breech presentation, fetal demise, blighted ovum, and ectopic pregnancy.
As noted above, we considered the hands-on sessions to be the most important element of the training. These sessions were designed to add skills in a step-wise fashion with both supervised and independent scanning. Using an iterative process similar to that used for developing the lectures, 25 hands-on sessions were written. Each session consisted of objectives, trainer demonstration, trainee practice activities, and detailed instructions for the trainer. Whenever possible, these sessions corresponded with specific lectures.
In addition to scanning skills, hands-on sessions were designed to facilitate effective communication between sonographer and patient. This included explanation of the ultrasound procedure, communication of the results, recommendations for follow-up, and rationale for referral to a higher level care if necessary. There was also emphasis on effective collaboration between sonographer and midwife so communication to the patient is clear and consistent.
Referral algorithms and corresponding flowcharts were developed by the team to be used at the 18 to 22 week screening, the 32 to 36 week screening, and for first trimester bleeding. The screening algorithms included follow-up of malpresentation, placenta previa or low-lying placenta, multiple gestation, fetal anomalies, polyhydramnios, second and third trimester bleeding, oligohydramnios and IUGR, and fetal demise. The first trimester algorithm included follow-up of ultrasound findings such as empty uterus with adnexal mass, empty uterus with echogenic or large amount of free fluid, gestational sac less than 20 mm without a yolk sac, gestational sac greater than 20 mm without a yolk sac, gestational sac greater than 25 mm without a fetal pole, and fetus with no cardiac activity. Basic algorithm flowcharts were incorporated into the lectures and case studies. For the Global Network study, these algorithms were then tailored by each of the five sites to be consistent with local practice and to accommodate the challenges of referral.
Finally, a trainer’s guide and a participant handbook were written. The trainer’s guide contained all lectures and hands-on sessions, detailed training instructions, assessment tools, supplemental charts, algorithms, and suggestions on teaching approaches and tips for the adult learner. The participant handbook contained daily instructions, slides from the lectures with space for notes, supplemental charts, and the referral algorithms.
These materials were used in two rounds of training in Uganda with midwives who had no previous ultrasound experience. The first training was conducted by one of the curriculum’s authors along with a local sonographer. Detailed notes on areas of potential revision were taken during the training. The curriculum team then discussed areas of concern and made revisions as necessary. They included clarifying slide wording, adding additional images, simplifying physics concepts, changing the order of presentation of some topics, modifying the trainer’s manual, adding review questions for each lecture, modifying some of the instructions for hands-on sessions, and supplementing instructions on patient comfort and safety. The local sonographer in Uganda conducted a second round of training and submitted notes on additional potential revisions which the curriculum team incorporated for the version to be used in the Global Network study.
Site Assessment
Prior to training at the Global Network study sites, the UW-Global Network team undertook on-site assessments of each of the training facilities, the study referral hospitals, the study health centers, and the health system within which the study was to be implemented at the five study sites. The training facilities were evaluated for the adequacy of the training environment, the availability of outpatients and inpatients for hands-on training, and the accommodations for the trainers and trainees. At the referral hospitals, the UW team evaluated the availability and willingness of a trained and experienced sonographer to participate in the study, the availability and willingness of an obstetrician to participate in the study, the level of obstetric care provided, and the current system of patient referral from a health center to the referral hospital. Referral hospitals were encouraged to include sonographers from their facilities to participate in the trainings as well. The intention was for the referral sonographers to gain a firm understanding of the ultrasound course and study approach and to build relationships with the trainees serving as their medical extenders. The health centers were evaluated for level of care, current staffing levels, existing infrastructure, extent of antenatal care provided, number and timing of antenatal visits, number of health center deliveries, and referral system. Elements of the health system that were explored included willingness to facilitate training and implementation at the referral hospital and health center levels, awareness of potential changes in referral patterns as a result of the intervention, and participation in community sensitization of the intervention.
Continued Training and Quality Assurance
Although the ten-day course is designed to provide a strong background in basic screening obstetric ultrasound, we recognize that proficiency is achieved through performing more ultrasound scans than can be accomplished during the initial training period. We have therefore incorporated a three-month pilot period immediately following the course and before the beginning of the study to give the trainees the opportunity to scan more patients and to receive feedback and additional training. After completion of the course, the trainees return to their health centers to begin scanning patients. During this pilot period screening ultrasound exams are periodically supervised directly by the local study sonographer, while all exams are reviewed remotely after the scans are completed.
Trainees scan patients at their health centers during routine antenatal visits at 18–22 weeks and again at 32–36 weeks. If they have questions on a scan they can consult the study sonographer on her mobile phone, send the entire study to the study sonographer on flash drive, send the patient to the referral hospital if deemed appropriate, or show the study saved on the ultrasound machine hard drive when the study sonographer meets with the trainee (see below).
After the trainees complete the initial training course the study sonographer travels to the study health centers regularly to observe each trainee performing screening ultrasound studies. The study sonographer observes all aspects of the screening ultrasound examination, including how the trainee communicates with the patient, how the ultrasound scan is integrated into antenatal care provision at the health center, and what the patient’s understanding and impressions of visit are. These observations are repeated throughout the pilot period and scanning skills test are given to each trainee by the study sonographer at the end of week 2, week 4, week 8, and week 12. On the basis of these tests and observations, the study sonographer will meet with trainees as necessary for remedial training.
For each 2nd and 3rd trimester patient scanned the trainees save to the ultrasound machine hard drive images of biparietal diameter, head circumference, abdominal circumference, femur length, amniotic fluid volume, placental position, sagittal fetal presenting part with the cervix, and the OB report page which includes all biometry measurements. They will save images of the cervical length to 32 weeks gestational age if obtainable and placenta-cervix distance if 2 cm or less. The images saved for symptomatic first trimester patients include uterine and adnexal content and biometry as appropriate.
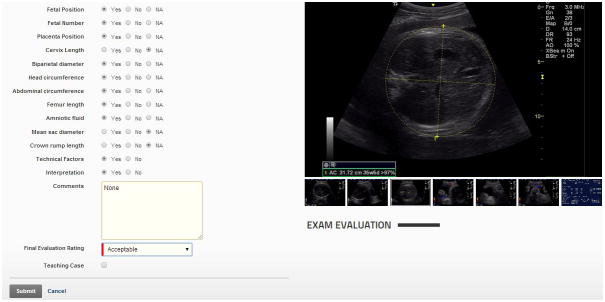
The images are downloaded to a flash drive at each intervention health center. At least once a week the flash drives are collected, returned to the referral hospital with reliable internet access, and uploaded to a quality assurance website developed for the study by RTI. Both local study sonographers and UW reviewers have access to the website and share the quality assurance duties. Reviewers rate the components of each study (fig 1.) for acceptability, write comments as indicated, and assign an overall rating (satisfactory, unsatisfactory, or suboptimal but satisfactory) by established criteria. The studies with accompanying comments are available for review by the study sonographers and trainees. For the pilot period, each study is reviewed and rated. Observations and data on each trainee are used to evaluate performance. At least once a month the training team (study sonographer, local study coordinator, and UW reviewers) discuss trainee performance and devise additional training as needed.
Figure 1.
If trainees pass the scanning skills test within 20 minutes at the end of the pilot period and their performance is otherwise satisfactory, they will become field sonographers and begin the study. As in the pilot period, website review will continue for each field sonographer, but the frequency of image review by random sampling will be individualized by consensus of the training team. The study sonographer will complete a performance review for each field sonographer once a month during the study.
At approximately six months following a site training a UW trainer will visit the study site. The trainer will give a refresher on those components of the screening exam which have proved to be the most challenging. In addition he will expand on some concepts that were covered briefly in the 10 day course (intrauterine growth restriction, incompetent cervix, anomalies). He will tour the health centers to observe not only the ultrasound screenings, but how they are integrated into routine antenatal care, and what patients’ impressions and understanding of the antenatal visit are.
Conclusion
Our approach to training healthcare workers in screening obstetric ultrasound is comprised of several components, including didactic and hands-on instruction, distribution of printed materials, an algorithm approach to follow-up adapted to the local environment, extensive quality assurance activities, a three month pilot period, and continuing education visits. We have aimed to reduce cost by training locally and by limiting to 10 days the time that trainees are required to be away from their posts. In the long term, pre-service training could substantially reduce the costs by training students who are not yet incorporated into the health care system. The pre-service model is also likely to be a more sustainable option than in-service training [15]. If a country were to decide to adopt this approach, establishing pre-service obstetric ultrasound courses for midwife or nurse/midwife schools should be a priority [16].
Whether conducted as in-service or pre-service, certification should be an integral part of the training process. Certification sets minimum standards of individual competencies and requirements for training, testing, and continuing education [17, 18]. As of now, there is no general agreement on certification of healthcare personnel in screening obstetric ultrasound in LMIC.
Finally, strategies similar to ours have been used effectively in other maternal and child health and infectious disease training programs in LMIC [19–21]. But overall, there is little evidence on the effectiveness of various educational strategies for healthcare workers in LMIC [22]. Before scaling up a training program it is important for stakeholders to be aware of the costs and benefits of different approaches. Training programs should include rigorous evaluations to aid decision-makers in allocating funds to those programs that have the greatest likelihood of success. The partners of this study are planning to include an economic analysis of our approach to aid in the decision to take our approach to scale in LMICs. In addition, the Global Network study and an economic analysis of its approach may also help ultrasound manufacturers determine the price point for inexpensive ultrasound units that are simplified, durable and targeted for limited obstetric ultrasound in rural LMIC settings.
Acknowledgments
This study was funded by the Bill & Melinda Gates Foundation, GE Healthcare and grants from the Eunice Kennedy Shriver National Institute of Child Health and Human Development ((U01 HD040636; U01 HD040607; U01 HD058326; U01 HD043464; U01 HD040657). The study ultrasound equipment was donated by GE Healthcare.
With appreciation for guidance from Caroline Signore, MD, Nana Twum-Danso, MD and Rex Widmer, MS.
Footnotes
Conflicts of Interest and Sources of Funding:
No conflicts of interest were declared from the authors.
Contributor Information
Robert Nathan, Department of Radiology, University of Washington, Seattle, WA.
Jonathan Swanson, Department of Radiology, University of Washington, Seattle, WA.
William Marks, Radia, Seattle, WA.
Nicole Goldsmith, University of Washington, Seattle, WA.
Cheryl Vance, C&D Advance Consultants, LLC, San Antonio, TX.
Brian Sserwanga, Radiographer, Millennium Village Project, Ruhirra, Uganda.
David Swanson, University of Washington, Seattle, WA.
Elizabeth M. McClure, Department of Statistics and Epidemiology, RTI International, Research Triangle Park, NC.
Holly Franklin, Department of Statistics and Epidemiology, RTI International, Research Triangle Park, NC.
Waseem Mirza, Department of Radiology, Aga Khan University, Karachi, Pakistan.
Musaku Mwenechanya, Department of Pediatrics, University Teaching Hospital, Lusaka, Zambia.
David Muyodi, Moi University School of Medicine, Eldoret, Kenya.
Lester Figuero, Guatemala City, Guatemala.
Victor Lokomba Bolamba, Département de Gynécologie-Obstétrique, Faculté de Médecine, Université de Kinshasa, Kinshasa, République Démocratique du Congo.
Robert L. Goldenberg, Department of Obstetrics and Gynecology, Columbia University, New York, NY.
References
- 1.Kimberly HH, Murray A, Mennicke M, et al. Focused maternal ultrasound by midwives in rural Zambia. Ultrasound Med Biol. 2010;36(8):1267–72. doi: 10.1016/j.ultrasmedbio.2010.05.017. [DOI] [PubMed] [Google Scholar]
- 2.Kotlyar S, Moore CL. Assessing the utility of ultrasound in Liberia. J Emerg Trauma Shock. 2008;1(1):10–4. doi: 10.4103/0974-2700.41785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Shah SP, Epino J, Bukhman G, et al. Impact of the introduction of ultrasound services in a limited resource setting: rural Rwanda 2008. BMC Int Health Hum Rights. 2009;9:4. doi: 10.1186/1472-698X-9-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kawooya MG. Training for rural radiology and imaging in sub-saharan Africa: addressing the mismatch between services and population. J Clin Imaging Sci. 2012;2:37. doi: 10.4103/2156-7514.97747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Adler D, Mgalula K, Price D, et al. Introduction of a portable ultrasound unit into the health services of the Lugufu refugee camp, Kigoma District, Tanzania. Int J Emerg Med. 2008;1(4):261–6. doi: 10.1007/s12245-008-0074-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Greenwold N, Wallace S, Prost A, et al. Implementing an obstetric ultrasound training program in rural Africa. Int J Gynaecol Obstet. 2013 doi: 10.1016/j.ijgo.2013.09.018. [DOI] [PubMed] [Google Scholar]
- 7.Harris RD, Marks WM. Compact ultrasound for improving maternal and perinatal care in low-resource settings: review of the potential benefits, implementation challenges, and public health issues. J Ultrasound Med. 2009;28(8):1067–76. doi: 10.7863/jum.2009.28.8.1067. [DOI] [PubMed] [Google Scholar]
- 8.Shah S, Noble VE, Umulisa I, et al. Development of an ultrasound training curriculum in a limited resource international setting: successes and challenges of ultrasound training in rural Rwanda. Int J Emerg Med. 2008;1(3):193–6. doi: 10.1007/s12245-008-0053-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Rijken MJ, Lee SJ, Boel ME, et al. Obstetric ultrasound scanning by local health workers in a refugee camp on the Thai-Burmese border. Ultrasound Obstet Gynecol. 2009;34(4):395–403. doi: 10.1002/uog.7350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Langlois Sle P. Focused ultrasound training for clinicians. Crit Care Med. 2007;35(5 Suppl):S138–43. doi: 10.1097/01.CCM.0000260625.63077.05. [DOI] [PubMed] [Google Scholar]
- 11.Steinmetz JP, Berger JP. Ultrasonography as an aid to diagnosis and treatment in a rural African hospital: a prospective study of 1,119 cases. Am J Trop Med Hyg. 1999;60(1):119–23. doi: 10.4269/ajtmh.1999.60.119. [DOI] [PubMed] [Google Scholar]
- 12.McClure EM, Nathan RO, Saleem S, et al. First Look: A cluster-randomized trial of ultrasound to improve pregnancy outcomes in low income country settings. BMC Pregnancy and Childbirth. 2014;14(73) doi: 10.1186/1471-2393-14-73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Goudar SS, Carlo WA, McClure EM, et al. The Maternal and Newborn Health Registry Study of the Global Network for Women’s and Children’s Health Research. Int J Gynaecol Obstet. 2012;118(3):190–3. doi: 10.1016/j.ijgo.2012.04.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Swanson JO, Kawooya MG, Swanson DL, et al. Diagnostic imapct of limited, screening obstetric ultrasound when performed by midwives in rural Uganda. J Perinatol. doi: 10.1038/jp.2014.54. in press. [DOI] [PubMed] [Google Scholar]
- 15.WHO. Child health and development pre-service education. [cited 2014 1/3]; Available from: http://www.emro.who.int/child-health/IMCI-preservice-training/what-is-it.
- 16.I-TECH. Strengthening pre-service education: a vital effort. [cited 2014 1/3]; Available from: http://news.go2itech.org/2012/04/strengthening-pre-service/
- 17.Necochea E. Building stronger human ressources for health through licensure, certification, and accreditation. Global Health Workforce Alliance. [cited 2014 1/4]; Available from: http://www.who.int/workforcealliance/knowledge/toolkit/37/en/index.html.
- 18.WHO. Task shifting to tackle health worker shortages. 2007. [Google Scholar]
- 19.Carlo WA, Goudar SS, Jehan I, et al. Newborn-care training and perinatal mortality in developing countries. N Engl J Med. 2010;362(7):614–23. doi: 10.1056/NEJMsa0806033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Garces A, McClure EM, Hambridge M, et al. Training traditional birth attendants on the WHO Essential Newborn Care reduces perinatal mortality. Acta Obstet Gynecol Scand. 2012;91(5):593–7. doi: 10.1111/j.1600-0412.2012.01374.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Weaver MR, Crozier I, Eleku S, et al. Capacity-building and clinical competence in infectious disease in Uganda: a mixed-design study with pre/post and cluster-randomized trial components. PLoS One. 2012;7(12):e51319. doi: 10.1371/journal.pone.0051319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Althabe F, Bergel E, Cafferata ML, et al. Strategies for improving the quality of health care in maternal and child health in low-and middle-income countries: an overview of systematic reviews. Paediatr Perinat Epidemiol. 2008;22(Suppl 1):42–60. doi: 10.1111/j.1365-3016.2007.00912.x. [DOI] [PubMed] [Google Scholar]


