Abstract
Purpose: The management criterion of thyroid nodules is to evaluate the risk of malignancy, based on cytological examinations. Ultrasound-guided fine-needle aspiration biopsy (US-FNAB) has a highly diagnostic value for thyroid nodules. The aim of this study was to compare the efficacy of US-FNAB for thyroid nodules with different sizes. Material and methods: From August 2013 to November 2013, 344patients with thyroid nodules who had undergone US-FNAB were divided into three groups, according to the largest diameter of their nodules (group A, ≤ 5.0 mm; group B, 5.1-10.0 mm; group C, > 10.0 mm). All the nodules were subsequently verified by histology or follow-up findings. The accuracy, sensitivity, specificity, positive predictive value, negative predictive value of aspiration cytology in each group was compared. Results: Among 344 thyroid nodules diagnosed by cytology, the cytology was classified as nondiagnostic or unsatisfactory for 53 (15.4%) lesions, benign for 144 (41.9%) lesions, atypia of undetermined significance or follicular lesion of undetermined significance for 20 (5.8%) lesions, follicular neoplasm or suspicious for a follicular neoplasm for 26 (7.6%) lesions, suspicious for malignancy for 36 (10.5%) lesions, malignant for 65 (18.9%) lesions. There were 243 benign and 101 malignant nodules confirmed by the pathological or follow-up ultrasound. The sensitivity, specificity, accuracy, positive predictive value, and negative predictive value were confirmed to be 87.5% (14/16), 92.5% (37/40), 91% (51/56), 82.3% (14/17), and 94.8% (37/39) in group A; 92.3% (36/39), 96.9% (94/97), 95.5% (130/136), 92.3% (36/39), and 96.9% (94/97) in group B; and 91.3% (42/46), 93.4% (99/106), 92.7% (141/152) 85.7% (42/49), and 96.1% (99/103), in group C. There were no statistical differences in accuracy, sensitivity, specificity, false positive accuracy, false negative rate of fine needle aspiration of thyroid nodules with different sizes (P > 0.05). Conclusion: US-FNAB has similar diagnostic efficacy to thyroid nodules with different sizes.
Keywords: US-guided fine-needle aspiration biopsy, thyroid nodules, cytopathology, thyroid carcinoma, follow-up
Introduction
High-resolution ultrasound is generally considered as the first choice for the evaluation of thyroid, and the number of detected asymptomatic, impalpable lesions in the gland rapidly increases due to its wide use [1,2]. However, only 5%-15% of thyroid nodules are malignant [3,4], thus it creates dilemmas in the management of the nodules: aggressive or conservative strategies? The management criterion of thyroid nodules is to evaluate the risk of malignancy, based on cytological examinations. Ultrasound-guided fine-needle aspiration biopsy (US-FNAB) is widely regarded as the preferred diagnostic tool in the evaluation of thyroid nodules with a maximal diameter larger than 1-1.5 cm and of nodules that are smaller with US features of suspicious, such as a solid hypo-echoic mass, taller-than-wide shape, irregular border, microcalcifications [5-9]. However, thyroid FNA cytology was limited by the nondiagnostic results, which have been reported to range from 6.4% to 33.6% [10,11].
This retrospective study was carried out to evaluate whether the size can influence the efficacy of US-FNAB for thyroid nodules.
Materials and methods
We retrospectively reviewed 344 thyroid nodules which had undergone US-FNAB from August 2013 to November 2013 in our hospital. The protocol was approved by the local Ethics Committees and written informed consent was obtained from all the patients. The inclusion criteria for US-FNAB evaluation of the thyroid nodules were as following: I) with suspicious sonographic findings included solid hypo-echoic mass, taller-than-wide shape, irregular border, and micro-calcifications; II) nodules with high risk for malignancy: patients with history of thyroid malignancy or family history of thyroid cancer; III) nodules with increasing size during follow up.
Nodules were divided into three groups according to the largest diameter: group A, ≤ 5.0 mm; group B, 5.1-10.0 mm; group C, > 10.0 mm.
US-FNA cytology procedure
Before US-FNAB, all patients routinely underwent serial US examinations, which were performed by one of three experienced operator. US-FNAB was performed by one of three radiologists using a 9-14MHz linear array transducer (Logiq E9; GE Healthcare) and a 23-gauge, 15 cm long needle. The sample was obtained by the needle moving up and down for a few seconds only by movement of the wrist of the operator, mounted immediately onto a glass slide and placed in 95% alcohol solution.
Cytopathological examinations
The Bethesda System for Reporting Thyroid Cytopathology was used as the criteria of standard sample adequacy in our study: the sample was defined as nondiagnostic if it did not have more than 6 groupings of at least 10 thyroid follicular cells each [12].
Follow-up after FNA cytology
In our study, all the nodules that the cytological findings were malignant, suspicious for malignancy, or indeterminate were recommended to operation, while follow-up FNAB cytology or follow-up ultrasound for those with benign or nondiagnostic cytology. Nodules showed no change on follow-up ultrasound after more than one year, were included in the benign group [13].
Statistical analysis
Results were compared with post-operative diagnoses and clinical follow-up findings. For each tested variable, such as the sensitivity, specificity, positive predictive values (PPV) and negative predictive values (NPV) of US-FNAB, SPSS 20.0 was used for statistical analysis using the chi-square test, P < 0.05 was considered statistically significant.
Results
344 patients with a mean age ± standard deviation, 49.8 ± 12.4 years, including 264 women and 80 men, were enrolled in the study. The final diagnoses based on pathology from surgery (n = 171), repeated FNAB cytology (n = 14) or follow-up of over a year (n = 159), and there were 243 benign, 101 malignant in total. Of 56 thyroid nodules diagnosed by cytology in group A, the cytology was classified as nondiagnostic or unsatisfactory for 10 (10/56, 17.8%) lesions, benign for 22 (22/56, 39.3%) lesions, atypia of undetermined significance or follicular lesion of undetermined significance for 3 (3/56, 5.3%) lesions, follicular neoplasm or suspicious for a follicular neoplasm for 4 (4/56, 7.1%) lesions, suspicious for malignancy for 6 (6/56, 10.7%) lesions, malignant for 11 (11/56, 19.6%) lesions. The corresponding numbers were 17 (17/136, 12.5%), 58 (58/136, 42.6%), 12 (12/136, 8.8%), 10 (10/136, 7.4%), 16 (16/136, 11.7%), 23 (23/136, 16.9%), respectively, in group B; and 24 (24/152, 15.8%), 61 (61/152, 40.1%), 11 (11/152, 7.2%), 7 (7/152, 4.6%), 18 (18/152, 11.8%), and 31 (31/152, 20.4%) respectively, in group C (Figure 1). There were no P > 0.05, Table 1). In the benign cytological results of group A, two nodules (2/56, 3.6%) turned out to be malignant even though the cytology findings were benign, three nodules (3/56, 5.4%) turned out to be benign for which the cytology findings were suspicious for malignancy. Three (3/136, 2.2%) and four (4/152, 2.6%) nodules turned out to be malignant even though the cytology findings were benign in group B and C, while three (3/136, 2.2%) and seven (7/152, 4.6%) nodules turned out to be benign for which the cytology findings were suspicious for malignancy, respectively (Table 2).
Figure 1.
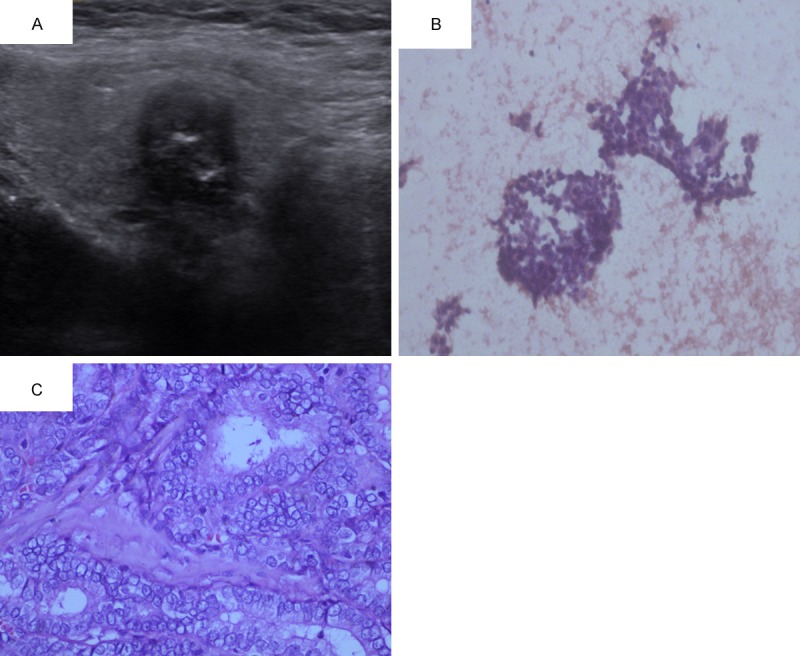
Gray-scale images (A) show suspicious sonographic finding, the diagnoses of Fine-needle aspiration cytology (B) and Thyroidectomy specimen (C) are Thyroid papillary carcinoma.
Table 1.
Result of FNAB
| Cytology | Group A | Group B | Group C |
|---|---|---|---|
| I | 10 (17.8%) | 17 (12.5%) | 24 (15.8%) |
| II | 22 (39.3%) | 58 (42.6%) | 61 (40.1%) |
| III | 3 (5.3%) | 12 (8.8%) | 11 (7.2%) |
| IV | 4 (7.1%) | 10 (7.4%) | 7 (4.6%) |
| V | 6 (10.7%) | 16 (11.7%) | 18 (11.8%) |
| VI | 11 (19.6%) | 23 (16.9%) | 31 (20.4%) |
| Total | 56 | 136 | 152 |
Note: The Bethesda System for Reporting Thyroid Cytopathology. I, Non-diagnostic or unsatisfactory. II, Benign III, Atypia of undetermined significance or follicular lesion of undetermined significance. IV, Follicular neoplasm or suspicious for a follicular neoplasm. V, Suspicious for malignancy. VI, Malignant.
Table 2.
Results of surgery or clinical diagnosis
| Results of cytology | Final results | |
|---|---|---|
|
| ||
| Malignant | Benign | |
| Group A | ||
| Malignant | 14 | 3 |
| Benign | 2 | 37 |
| Group B | ||
| Malignant | 36 | 3 |
| Benign | 3 | 94 |
| Group C | ||
| Malignant | 42 | 7 |
| Benign | 4 | 99 |
The sensitivity, specificity, accuracy, positive predictive value, and negative predictive value were confirmed to be 87.5% (14/16), 92.5% (37/40), 91% (51/56), 82.3% (14/17), and 94.8% (37/39) in group A; 92.3% (36/39), 96.9% (94/97), 95.5% (130/136), 92.3% (36/39), and 96.9% (94/97) in group B; and 91.3% (42/46), 93.4% (99/106), 92.7% (141/152) 85.7% (42/49), and 96.1% (99/103), in group C (Table 3). There were no significant differences in the sensitivity, the specificity, the positive predictive value, the negative predictive value, and the accuracy of US-FNAB among groups A, B and C (chi-square test, all P > 0.05).
Table 3.
Sensitivity, specificity, accuracy, PPV and NPV calculated according to FNAB
| Group A (≤ 5 mm) | Group B (6-10 mm) | Group C (> 10 mm) | P value | |
|---|---|---|---|---|
| Sensitivity | 87.5% (14/16) | 92.3% (36/39) | 91.3% (42/46) | > 0.05 |
| Specificity | 92.5% (37/40) | 96.9% (94/97) | 93.4% (99/106) | > 0.05 |
| Accuracy | 91% (51/56) | 95.5% (130/136) | 92.7% (141/152) | > 0.05 |
| PPV | 82.3% (14/17) | 92.3% (36/39) | 85.7% (42/49) | > 0.05 |
| NPV | 94.8% (37/39) | 96.9% (94/97) | 96.1% (99/103) | > 0.05 |
PPV, Positive predictive value; NPV, negative predictive value.
Discussion
Regardless of the nodule size, malignancy is found in approximately 5% of thyroid nodules [14]. Since the use of US-guided FNAB in the management of thyroid nodules, there has been a decline in the number of surgery to exclude the nodule malignancy. However, it is still controversial for thyroid nodules smaller than 10 mm evaluated on US-FNAB. The American Thyroid Association (ATA) guidelines proposed that only nodules larger than 10 mm in diameter were more usefully evaluated by US-FNAB [14], and some researchers considered that the sensitivity was lower in the nodules smaller than 5 mm compared with other nodule size [11,15].
The present study revealed that there were no statistically significant differences in sensitivity for nodules with different sizes. There were 56 nodules less than 5 mm in diameter, and 10 (17.8%) yielded unsatisfactory results. Of the 136 nodules larger than 5 mm but smaller than 10 mm, 17 yielded unsatisfactory results (12.5%), and the nondiagnostic in third cohorts of our study was 24 (15.8%). The size of the nodule did not appear to influence the inadequacy of the aspirated material in our study; the findings of our study are in agreement with the studies by Kim et al. and Nam-Goong et al. [16,17]. The specificity, accuracy, positive predictive value, and negative predictive value of our study were also similar to the present study [18]. In the procedure of FNAB of the thyroid, there were no severe complications in our study, except for one man with dizziness that might be related to changes in position.
There were several limitations in our study. First, the time of follow-up was only one year; however, it might be not enough to confirm the natures of the thyroid nodules, which would lead to overestimated diagnostic ability of US-FNAB to some extend. Second, our study was not a large-scale study thus future studies with more patients were mandatory.
In conclusion, although nondiagnostic results were observed in the process of US-FNAB, it is a useful technique to evaluate the thyroid nodules, even in the nodules less than 5 mm in maximum diameter. US-FNAB has similar diagnostic efficacy to thyroid nodules with different sizes.
Acknowledgements
This work was supported in part by Grant SHDC12014229 from Shanghai Hospital Development Center, Grant 14441900900 from Science and Technology Commission of Shanghai Municipality, Grant 2012045 from Shanghai Municipal Human Resources and Social Security Bureau, and Grants 81401417 and 81472579 from the National Natural Science Foundation of China.
Disclosure of conflict of interest
None.
References
- 1.Leenhardt L. [Management of thyroid nodule] . J Radiol. 2009;90:354–361. doi: 10.1016/s0221-0363(09)72520-x. [DOI] [PubMed] [Google Scholar]
- 2.Guth S, Theune U, Aberle J, Galach A, Bamberger CM. Very high prevalence of thyroid nodules detected by high frequency (13 MHz) ultrasound examination. Eur J Clin Invest. 2009;39:699–706. doi: 10.1111/j.1365-2362.2009.02162.x. [DOI] [PubMed] [Google Scholar]
- 3.Frates MC, Benson CB, Doubilet PM, Kunreuther E, Contreras M, Cibas ES, Orcutt J, Moore FD Jr, Larsen PR, Marqusee E, Alexander EK. Prevalence and distribution of carcinoma in patients with solitary and multiple thyroid nodules on sonography. J Clin Endocrinol Metab. 2006;91:3411–3417. doi: 10.1210/jc.2006-0690. [DOI] [PubMed] [Google Scholar]
- 4.Sachmechi I, Miller E, Varatharajah R, Chernys A, Carroll Z, Kissin E, Rosner F. Thyroid carcinoma in single cold nodules and in cold nodules of multinodular goiters. Endocr Pract. 2000;6:5–7. doi: 10.4158/EP.6.1.5. [DOI] [PubMed] [Google Scholar]
- 5.Kim MJ, Kim EK, Park SI, Kim BM, Kwak JY, Kim SJ, Youk JH, Park SH. US-guided fine-needle aspiration of thyroid nodules: indications, techniques, results. Radiographics. 2008;28:1869–1886. doi: 10.1148/rg.287085033. [DOI] [PubMed] [Google Scholar]
- 6.Cooper DS, Doherty GM, Haugen BR, Kloos RT, Lee SL, Mandel SJ, Mazzaferri EL, McIver B, Pacini F, Schlumberger M, Sherman SI, Steward DL, Tuttle RM. Revised American Thyroid Association management guidelines for patients with thyroid nodules and differentiated thyroid cancer. Thyroid. 2009;19:1167–1214. doi: 10.1089/thy.2009.0110. [DOI] [PubMed] [Google Scholar]
- 7.Carrillo JF, Frias-Mendivil M, Ochoa-Carrillo FJ, Ibarra M. Accuracy of fine-needle aspiration biopsy of the thyroid combined with an evaluation of clinical and radiologic factors. Otolaryngol Head Neck Surg. 2000;122:917–921. doi: 10.1016/S0194-59980070025-8. [DOI] [PubMed] [Google Scholar]
- 8.Karadeniz Cakmak G, Emre AU, Tascilar O, Gultekin FA, Ozdamar SO, Comert M. Diagnostic adequacy of surgeon-performed ultrasound-guided fine needle aspiration biopsy of thyroid nodules. J Surg Oncol. 2013;107:206–210. doi: 10.1002/jso.23212. [DOI] [PubMed] [Google Scholar]
- 9.Frates MC, Benson CB, Charboneau JW, Cibas ES, Clark OH, Coleman BG, Cronan JJ, Doubilet PM, Evans DB, Goellner JR, Hay ID, Hertzberg BS, Intenzo CM, Jeffrey RB, Langer JE, Larsen PR, Mandel SJ, Middleton WD, Reading CC, Sherman SI, Tessler FN. Management of thyroid nodules detected at US: Society of Radiologists in Ultrasound consensus conference statement. Radiology. 2005;237:794–800. doi: 10.1148/radiol.2373050220. [DOI] [PubMed] [Google Scholar]
- 10.Degirmenci B, Haktanir A, Albayrak R, Acar M, Sahin DA, Sahin O, Yucel A, Caliskan G. Sonographically guided fine-needle biopsy of thyroid nodules: the effects of nodule characteristics, sampling technique, and needle size on the adequacy of cytological material. Clin Radiol. 2007;62:798–803. doi: 10.1016/j.crad.2007.01.024. [DOI] [PubMed] [Google Scholar]
- 11.Kim DW, Lee EJ, Kim SH, Kim TH, Lee SH, Kim DH, Rho MH. Ultrasound-guided fine-needle aspiration biopsy of thyroid nodules: comparison in efficacy according to nodule size. Thyroid. 2009;19:27–31. doi: 10.1089/thy.2008.0106. [DOI] [PubMed] [Google Scholar]
- 12.Cibas ES, Ali SZ. The Bethesda System For Reporting Thyroid Cytopathology. Am J Clin Pathol. 2009;132:658–665. doi: 10.1309/AJCPPHLWMI3JV4LA. [DOI] [PubMed] [Google Scholar]
- 13.Lee MJ, Hong SW, Chung WY, Kwak JY, Kim MJ, Kim EK. Cytological results of ultrasound-guided fine-needle aspiration cytology for thyroid nodules: emphasis on correlation with sonographic findings. Yonsei Med J. 2011;52:838–844. doi: 10.3349/ymj.2011.52.5.838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Gharib H, Papini E, Valcavi R, Baskin HJ, Crescenzi A, Dottorini ME, Duick DS, Guglielmi R, Hamilton CR Jr, Zeiger MA, Zini M. American Association of Clinical Endocrinologists and Associazione Medici Endocrinologi medical guidelines for clinical practice for the diagnosis and management of thyroid nodules. Endocr Pract. 2006;12:63–102. doi: 10.4158/EP.12.1.63. [DOI] [PubMed] [Google Scholar]
- 15.Leenhardt L, Hejblum G, Franc B, Fediaevsky LD, Delbot T, Le Guillouzic D, Menegaux F, Guillausseau C, Hoang C, Turpin G, Aurengo A. Indications and limits of ultrasound-guided cytology in the management of nonpalpable thyroid nodules. J Clin Endocrinol Metab. 1999;84:24–28. doi: 10.1210/jcem.84.1.5418. [DOI] [PubMed] [Google Scholar]
- 16.Kim SJ, Kim EK, Park CS, Chung WY, Oh KK, Yoo HS. Ultrasound-guided fine-needle aspiration biopsy in nonpalpable thyroid nodules: is it useful in infracentimetric nodules? Yonsei Med J. 2003;44:635–640. doi: 10.3349/ymj.2003.44.4.635. [DOI] [PubMed] [Google Scholar]
- 17.Nam-Goong IS, Kim HY, Gong G, Lee HK, Hong SJ, Kim WB, Shong YK. Ultrasonography-guided fine-needle aspiration of thyroid incidentaloma: correlation with pathological findings. Clin Endocrinol (Oxf) 2004;60:21–28. doi: 10.1046/j.1365-2265.2003.01912.x. [DOI] [PubMed] [Google Scholar]
- 18.Gharib H, Papini E, Paschke R, Duick DS, Valcavi R, Hegedus L, Vitti P. American Association of Clinical Endocrinologists, Associazione Medici Endocrinologi, and European Thyroid Association medical guidelines for clinical practice for the diagnosis and management of thyroid nodules: executive summary of recommendations. J Endocrinol Invest. 2010;33:51–56. [PubMed] [Google Scholar]


