Abstract
Acute appendicitis is one of the most common causes of acute abdominal pain. Accurate diagnosis is often hindered due to various presentations that differ from the typical signs of appendicitis, especially the position of the appendix. A delay in diagnosis or treatment may result in increased risks of complications, such as perforation, which is associated with increased morbidity and mortality rates. Necrotizing fasciitis caused by perforated appendicitis is extremely rare. We herein report a case of 50-year-old man presenting with an appendiceal abscess in local hospital. After ten days of conservative treatment with intravenous antibiotics, the patient complained about pain and swelling of the right lower limb and computed tomography (CT) demonstrated a perforated appendix and gas and fluid collection extending from his retroperitoneal cavity to the subcutaneous layer of his right loin and right lower limb. He was transferred to our hospital and was diagnosed with necrotizing fasciitis caused by perforated appendicitis. Emergency surgery including surgical debridement and appendectomy was performed. However, the patient died of severe sepsis and multiple organ failure two days after the operation. This case represents an unusual complication of a common disease and we should bear in mind that retroperitoneal inflammation and/or abscesses may cause necrotizing fasciitis through lumbar triangles.
Keywords: Necrotizing fasciitis, acute appendicitis, perforation, lumbar triangles
Introduction
Acute appendicitis is one of the most common causes of acute abdomen. So far, no standardized approach is available for the management of complicated appendicitis defined as appendiceal abscess or phlegmon. When managing a patient with complicated appendicitis, the clinical dilemma exists whether to treat the patient conservatively with antibiotics or proceed with immediate operation [1]. Necrotizing fasciitis is characterized by a necrotic infection that rapidly spreads along the fascia and progresses to systemic sepsis [2]. Necrotizing fasciitis developing as a fatal complication of acute appendicitis is extremely rare [3]. The disease is most commonly induced by injury, with the mortality rate of 13.6% [4]. Since delay in diagnosis or treatment may result in a fatal outcome, surgical debridement should be performed immediately after the accurate diagnosis [5].
We present here a case of necrotizing fasciitis of abdominal wall and right flank secondary to a perforated appendix, an extremely rare complication of appendicitis. This patient’s course illustrates the importance of early diagnosis of disease progression and prompt surgical intervention when conservative treatment is used for complicated appendicitis, in an effort to avoid perforation and the sometimes life-threatening complications that may follow.
Case presentation
A 50-year-old man was referred to the local hospital because of right-sided abdominal pain and a fever of 38.5°C. Physical examination revealed a tender mass (5×5 cm in size) in the right iliac fossa. He had no significant medical history. Laboratory evaluation revealed an elevated white blood cell count of 17.54×109/L with 89.6% of neutrophil forms and an elevated C-reactive protein of more than 200 mg/L. A computed tomography (CT) scan of abdomen and pelvis showed a swollen appendix with abscess formation in the retroperitoneum (Figure 1A and 1B). In addition, the right side abdominal muscles and psoas muscle were involved around the abscess. The patient received conservative treatment with intravenous antibiotics (Ceftazidime: 3 g/day, and Metronidazole: 1.5 g/day). Five days after admission, the patient had an increasing abdominal pain and a higher fever (>39°C). The antibiotic treatment was then changed to Imipenem (2 g/day) and Ornidazole (1 g/day). However, there was no improvement in his condition in the following days. Ten days after admission, the patient started complaining about pain and swelling of the right lower limb and the skin of the right lower limb was found to be discolored with signs of cellulitis and bullae. Another CT scan was performed, which showed a perforated appendix and gas and fluid collection extending from his retroperitoneal cavity to the subcutaneous layer of his right loin and right lower limb (Figure 1C and 1D).
Figure 1.
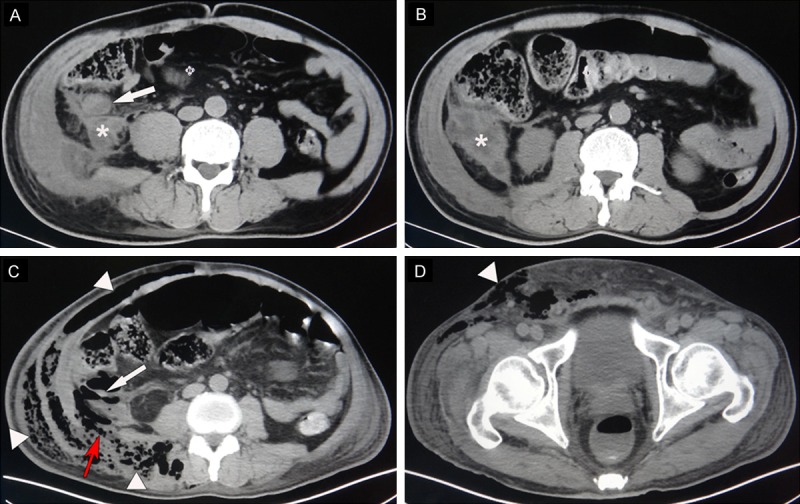
Selected axial views of the abdominal computed tomography scan. A. A swollen appendix (white arrow) with abscess formation in the retroperitoneum (asterisk) was identified on first admission to local hospital. Notably, the right side abdominal muscles and psoas muscle were also swollen. B. The appendiceal abscess (asterisk) was approximately 5×5 cm in size. C. A second abdominal computed tomography showed a perforated appendix (white arrow) and gas and fluid collection extending from his retroperitoneal cavity to the subcutaneous layer of his right loin (white triangle). Notably, the inflammation passed through the inferior lumbar triangle (red arrow) to the flank and the lumbar area. D. Gas and fluid collection were also observed at the right lower limb (white triangle).
He was transferred to our hospital and emergency surgery was performed after appropriate resuscitation with intravenous fluids and antibiotics. An 8-cm right rectus incision was made and a large collection of foulsmelling fluid subcutaneously with associated necrotizing soft tissue infection was seen. Further exploration revealed a perforated, retrocecal appendix with periappendicular abscess and necrotizing fasciitis involving all fascial and muscle layers of the anterior lower abdomen, right flank, and right retroperitoneum. An appendectomy was performed and the necrotic tissues were debrided as much as possible with drainage tubes indwelled. Cultures of the necrotic tissues and abscess revealed a polymicrobial infection consisting of Enterococcus Faecium, Escherichia coli, Fecal Clostridium septicum, Anaerobic bacteria.
The patient was transferred to surgical intensive care unit postoperatively. He had hemodynamic instability and required low-dose infusions of dopamine. He had high fever (39.5°C) and suffered respiratory failure requiring mechanical ventilatory support. Antibiotics were administered every 6 hours and best supportive care was given. However, on postoperative day 2, the patient still died of severe sepsis and multiple organ failure.
Discussion
Necrotizing fasciitis is a rare infection of the deeper layers of skin and subcutaneous tissues, easily spreading across the fascial plane within the subcutaneous tissue. The most consistent feature of necrotizing fasciitis was first described in 1952 as necrosis of the subcutaneous tissue and fascia with relative sparing of the underlying muscle [6]. Necrotizing fasciitis progresses rapidly, having greater risk of developing in the immunocompromised due to conditions such as diabetes or cancer. It is classified as type I (polymicrobial, due to a number of different organisms) or type II (monomicrobial, due to a single infecting organism) [7]. The majority of cases of necrotizing fasciitis are polymicrobial, with 25-45% of cases being type II. The case in this report was classified as type I and was a complication of appendicitis. Early recognition, broad-spectrum antibiotic treatment, and aggressive surgical debridement are the most important principles for management of this potentially lethal disease. However, it is difficult to make the diagnosis of necrotizing fasciitis early as it usually presents only with mild erythema in the skin as the initial manifestation, and may be confused with cellulitis; but it spreads rapidly along fascial planes, resulting in general toxicity for several hours or days [3].
Necrotizing fasciitis due to a perforated appendix is rarely reported. To our knowledge, only 13 cases have been reported in the English literature and the calculated mortality rate was 30.8% (4/13). It is nearly always associated with perforation of a retrocecal appendix due to delayed diagnosis and treatment. Besides, the importance of the lumbar triangles in the potential propagation of infection or abscesses should also be emphasized. There are two orifices that have been described: the inferior lumbar triangle (known as Petit triangle) and the superior lumbar triangle (known as Grynfeltt-Lesshaft triangle) (Figure 2A and 2B). As these two triangles void of muscular layers are areas of relative weakness in the abdominal wall, unusual traumatic lumbar hernias are known to develop through them [8]. Retroperitoneal inflammation and/or abscesses resulting from perforated acute appendicitis can also pass through these two triangles to the flank and/or the lumbar area, leading to the occurrence of necrotizing fasciitis, as the case we reported here.
Figure 2.
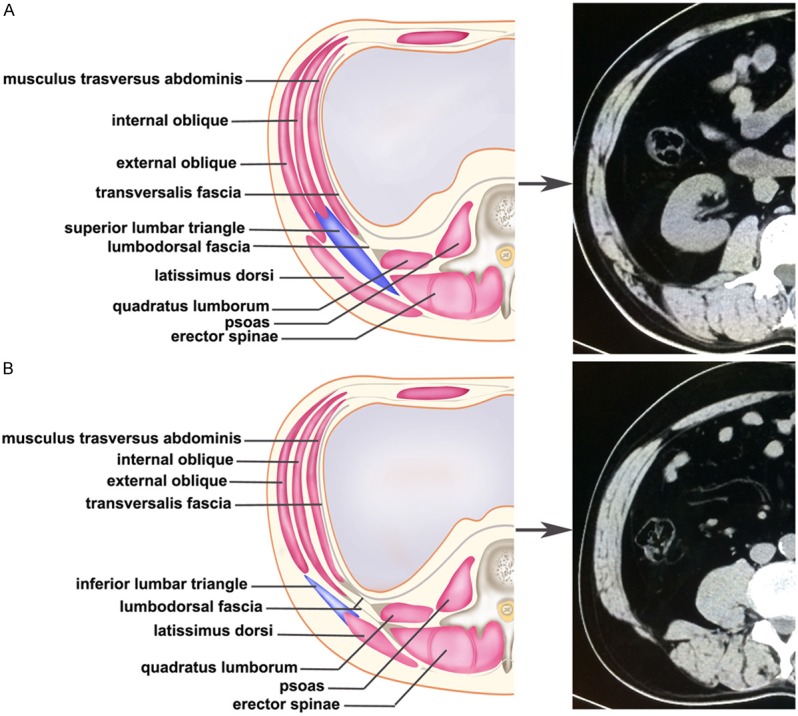
Selected axial views of computed tomography and drawings showing the superior and inferior lumbar triangles. A. The superior lumbar triangle-Grynfeltt-Lesshaft triangle (blue area) is an inverted triangle, or square, located below the 12th rib. The sides are the latissimus dorsi posteriorly, the quadratus lumbarum muscle inside, and the internal oblique muscle laterally just under the latissimus dorsi. B. The inferior lumbar triangle-Petit triangle (blue area) is situated just above the iliac crest representing its basis and limited by the external oblique muscle laterally and the latissimus dorsi medially.
Currently, no consensus exists among surgeons regarding the optimal treatment for patients with complicated appendicitis (abscess or phlegmon) [1]. Traditionally, appendectomy was considered the treatment of choice for complicated appendicitis, based on the surgical principle of removing the offending organ to resolve infection. However, conservative treatment seems to be a safer option for complicated appendicitis. This is because an operation at the peak of the inflammatory process may result in the subsequent stimulation of an already primed inflammatory system with excessive activation of the cytokine cascade. Overstimulation of the inflammatory response may result in complications and morbidity for the patient. An appendectomy can be delayed for a later stage, when the inflammation has subsided and the patient is appropriately prepared [9]. Therefore, the aim of conservative treatment is to localize the inflammatory process and decrease the risk of abscess, which allows time for the edematous inflamed bowel to recover [10]. However, if conservative management of complicated appendicitis is not successful, then it may result in substantial morbidity for patients. The failure rate of conservative treatment was 7.2%, and once the diagnosis is made, adequate abscess drainage or emergency operation will be required before life-threatening complications occur.
Conclusions
In conclusion, we have reported a rare case of necrotizing fasciitis caused by perforated appendicitis. Our case emphasized the role of the lumbar triangles in the progression of retroperitoneal inflammation and/or abscesses caused by retrocecal appendix. Early recognition, broad-spectrum antibiotic treatment, and timely surgical debridement and appendectomy are crucial for the management of patients like this. Although acute appendicitis is one of the most common diseases encountered in clinical practice, we should bear in mind that unusual complications can occur, such as necrotizing fasciitis, which may bring fatal consequences.
Acknowledgements
We thank Qiong Li for her excellant drawing of CT simulation diagram.
Disclosure of conflict of interest
None.
References
- 1.Simillis C, Symeonides P, Shorthouse AJ, Tekkis PP. A meta-analysis comparing conservative treatment versus acute appendectomy for complicated appendicitis (abscess or phlegmon) Surgery. 2010;147:818–829. doi: 10.1016/j.surg.2009.11.013. [DOI] [PubMed] [Google Scholar]
- 2.Lancerotto L, Tocco I, Salmaso R, Vindigni V, Bassetto F. Necrotizing fasciitis: classification, diagnosis, and management. J Trauma Acute Care Surg. 2012;72:560–566. doi: 10.1097/TA.0b013e318232a6b3. [DOI] [PubMed] [Google Scholar]
- 3.Takeda M, Higashi Y, Shoji T, Hiraide T, Maruo H. Necrotizing fasciitis caused by a primary appendicocutaneous fistula. Surg Today. 2012;42:781–784. doi: 10.1007/s00595-012-0140-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.McHenry CR, Piotrowski JJ, Petrinic D, Malangoni MA. Determinants of mortality for necrotizing soft-tissue infections. Ann Surg. 1995;221:558–563. doi: 10.1097/00000658-199505000-00013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Coulier B, Gogoase M, Ramboux A, Pierard F. Extra-abdominal lumbar abscesses caused by retroperitoneal gastrointestinal perforations through the lumbar triangle of Petit: report of two cases diagnosed by CT. Abdom Imaging. 2012;37:1122–1128. doi: 10.1007/s00261-012-9847-9. [DOI] [PubMed] [Google Scholar]
- 6.Kirchmair W. Appendicitis in aged. Wien Klin Wochenschr. 1952;64:435–437. [PubMed] [Google Scholar]
- 7.Giuliano A, Lewis F Jr, Hadley K, Blaisdell FW. Bacteriology of necrotizing fasciitis. Am J Surg. 1977;134:52–57. doi: 10.1016/0002-9610(77)90283-5. [DOI] [PubMed] [Google Scholar]
- 8.Ishigami K, Khanna G, Samuel I, Dahmoush L, Sato Y. Gas-forming abdominal wall abscess: unusual manifestation of perforated retroperitoneal appendicitis extending through the superior lumbar triangle. Emerg Radiol. 2004;10:207–209. doi: 10.1007/s10140-003-0314-3. [DOI] [PubMed] [Google Scholar]
- 9.Brown CV, Abrishami M, Muller M, Velmahos GC. Appendiceal abscess: immediate operation or percutaneous drainage? Am Surg. 2003;69:829–832. [PubMed] [Google Scholar]
- 10.Karaca I, Altintoprak Z, Karkiner A, Temir G, Mir E. The management of appendiceal mass in children: is interval appendectomy necessary? Surg Today. 2001;31:675–677. doi: 10.1007/s005950170068. [DOI] [PubMed] [Google Scholar]


