Abstract
Objective:
The purpose of this study was to examine prevalences and concordances between Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV), and Fifth Edition (DSM-5) substance use disorders (SUDs) in a newly completed U.S. epidemiologic survey.
Method:
The National Epidemiologic Survey on Alcohol and Related Conditions–III surveyed 36,309 civilian, noninstitutionalized adults. SUDs were assessed using the Alcohol Use Disorder and Associated Disabilities Interview Schedule–5. Concordances between DSM-IV and DSM-5 disorders were assessed using kappa statistics.
Results:
Prevalences of past-year substance-specific DSM-5 disorders (2+ criteria) were modestly higher than those of DSM-IV dependence and abuse combined for alcohol, sedatives/tranquilizers, opioids, and heroin, but lower for cannabis, cocaine, and stimulants. Lifetime prevalences were lower under DSM-5. Prevalences were similar between moderate to severe (4+ criteria) DSM-5 disorders and dependence, whereas prevalences of DSM-5 disorders at 3+ criteria (DSM-5 [3+]) were higher, particularly for cannabis. Past-year concordances were excellent for DSM-IV dependence and abuse combined versus any DSM-5 and DSM-IV dependence versus DSM-5 moderate to severe disorders; lifetime concordances were fair to excellent. Past-year concordances between DSM-IV and DSM-5 (3+) were generally similar to or modestly higher than those with any DSM-5 disorder; lifetime concordances were mostly lower.
Conclusions:
Findings are consistent with those informing the development of DSM-5. Future research should examine differences in patterns between past-year and lifetime disorders, particularly for cannabis. Other questions warranting investigation include whether different combinations of the same numbers of criteria carry different clinical or nosologic implications, whether changes innosology yield changes in treatment demand, and whether changes in characteristics of individuals with DSM-5 SUDs dictate modifications to screening and intervention.
Since the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV; American Psychiatric Association, 1994), was published, knowledge has advanced greatly about psychiatric disorders, including alcohol use disorders (AUDs) and other drug use disorders (DUDs). As described in detail by Hasin et al. (2013), major cross-substance and substance-specific revisions were made to the classification of substance use disorders (SUDs) in the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5; American Psychiatric Association, 2013). Cross-substance changes to the definition of SUDs included eliminating separate abuse and dependence diagnoses and their hierarchical relationship as well as combining the criteria into a single diagnosis. Other changes included dropping legal problems from and adding craving to the criteria set, establishing a diagnostic threshold of 2+ criteria, and creating a severity metric based on counts of criteria met. Substance-specific changes included the addition of cannabis withdrawal.
Cross-substance revisions
The combination of abuse and dependence into a single diagnosis reflected substantial evidence from factor and item response theory (IRT) analyses supporting a single latent construct underlying all DSM-IV SUDs, with abuse and dependence criteria always intermixed along the severity spectrum (e.g., Compton et al., 2009; Mewton et al., 2011; Saha et al., 2006, 2007, 2010, 2012; Shmulewitz et al., 2010). Additional considerations included the well-documented reliability (Hasin et al., 2006a) and validity (Compton et al., 2007; Dawson et al., 2000; Grant et al., 2004; Hasin et al., 2007) of dependence but less desirable psychometric properties of abuse. Moreover, whereas a syndrome by definition requires more than one symptom, almost half of all abuse cases received a diagnosis by meeting only one criterion, typically hazardous use (Hasin et al., 1999; Hasin & Paykin, 1999). Assumptions about abuse were shown to be incorrect, including that abuse was milder than or prodromal to dependence (Grant et al., 2001; Hasin et al., 1990, 1997b; Schuckit & Smith, 2001; Schuckit et al., 2000), and that all cases of dependence also met criteria for abuse (Grant et al., 2007; Hasin & Grant, 2004; Hasin et al., 2005). Furthermore, the DSM-IV hierarchy gave rise to concerns about “diagnostic orphans” (Hasin & Paykin, 1998, 1999; McBride et al., 2009), who met two dependence but no abuse criteria and remained undiagnosable despite manifesting a condition potentially more serious than abuse.
The elimination of substance-related legal problems (Hasin et al., 2013) was based on their very low prevalence (e.g., Saha et al., 2006), low discrimination (e.g., Hasin et al., 2012; Saha et al., 2006, 2007), poor fit with other SUD criteria (Langenbucher et al., 2004; Mewton et al., 2011; Saha et al., 2006; Teesson et al., 2002), and limited information contributed by these problems in IRT analyses (Lynskey & Agrawal, 2007; Saha et al., 2012; Shmulewitz et al., 2010). Moreover, despite concerns that dropping this criterion would leave some SUD treatment clients undiagnosed, no patients in methadone and dual-diagnosis settings “lost” a DSM-5 diagnosis without it (Hasin et al., 2012). Conversely, the addition of craving was supported indirectly by findings from behavioral (Heinz et al., 2009; Miller & Goldsmith, 2001; Waters et al., 2004), imaging, pharmacology (O’Brien, 2005), and genetics research (Agrawal et al., 2013; Foroud et al., 2007). Findings from IRT studies (Cherpitel et al., 2010; Hasin et al., 2012; Keyes et al., 2011; Mewton et al., 2011) showed equivocal psychometric benefit from adding this criterion. However, from a clinical perspective, some (O’Brien, 2005; Tiffany & Wray, 2012) but not all (Munafò & Hitsman, 2010; Perkins, 2009) investigators view craving as key to an SUD diagnosis and its reduction as central to treatment. Craving is also an International Classification of Diseases, Tenth Edition (World Health Organization, 1992), dependence criterion; therefore, its addition increased consistency between the nosologies (Hasin et al., 2013).
In setting a diagnostic threshold, the Work Group sought both to harmonize prevalences between DSM-IV (dependence and abuse combined) and DSM-5 SUDs and to maximize concordances between diagnoses under the two systems. Data from general population and clinical samples showed similar prevalences at thresholds from 2+ to 4+ DSM-5 criteria, whereas concordances were generally maximized at 2+ criteria (Hasin et al., 2013). Therefore, the threshold for any DSM-5 SUD was set at 2+, except that tolerance and withdrawal associated with supervised medical use of prescribed substances (Hasin et al., 2013) were not to lead to SUD diagnoses absent other criteria.
A simple count of criteria was chosen to measure severity because the likelihood of SUD risk factors and consequences increases with the count (Beseler & Hasin, 2010; Dawson et al., 2010; Hasin & Beseler, 2009; Hasin et al., 2006b). Mild disorders are defined by 2 to 3 criteria, moderate by 4 to 5, and severe by 6+ (Hasin et al., 2013). The Work Group considered weighting the count by IRT severity parameters; however, comparisons of associations of weighted and unweighted counts to consumption, functioning, and family history identified no advantages of weighting (Dawson et al., 2010). Furthermore, because severity parameters differed across samples (Gillespie et al., 2007), no universally applicable weights could be identified.
Cannabis withdrawal
Sufficient evidence had not yet accumulated to support the inclusion of cannabis withdrawal in DSM-IV. However, its reliability and validity have since been demonstrated in preclinical, clinical, and epidemiologic studies (Agrawal et al., 2008; Budney & Hughes, 2006; Budney et al., 2004; Copersino et al., 2006; Goldstein & Volkow, 2011; Hasin et al., 2008; Martinez et al., 2007). The clinical significance of cannabis withdrawal is indicated by the use of cannabis or similar substances to relieve withdrawal symptoms, its association with difficulty quitting (Budney et al., 2004; Copersino et al., 2006; Levin et al., 2010), and worse treatment outcomes with greater withdrawal severity (Chung et al., 2008; Cornelius et al., 2008).
Aims of the present study
The DSM-5 revisions to SUD classification reflect multifaceted efforts to identify and resolve problems in DSM-IV based on the best available evidence. Nevertheless, the amount of data bearing on particular issues varied, and the data sets that informed the process were collected 10 or more years ago. In addition, questions and concerns were raised about the revisions, including the relevance of particular criteria across substances (Room, 2011) and across sex, race or ethnicity, age groups, and developmental phases (Babor, 2011; Beynon, 2011; Caetano, 2011; Room, 2011; Winters et al., 2011). Others reflected the possibility that some criteria, largely but not exclusively those for abuse, may be social class and culture bound (Babor, 2011; Caetano, 2011; Meyer, 2011; Room, 2011). Concerns were also raised about assigning equal diagnostic importance to core dependence criteria and to “problems” or psychosocial consequences operationalized by abuse criteria on the basis of statistical considerations, despite conceptual differences between these criteria sets and their differential implications for intervention approaches (Babor, 2011; Drummond, 2011; Meyer, 2011; Poznyak et al., 2011; Room, 2011; Uchtenhagen, 2011).
With the publication of DSM-5 in 2013, an important knowledge gap concerns the performance of DSM-IV versus DSM-5 SUD definitions in current populations, which may differ importantly on characteristics including greater sociodemographic diversity and changes in substance use patterns from those that informed DSM-5. In addition, data used to guide the DSM-5 diagnostic thresholds and severity cut points were based largely on current disorders (Hasin et al., 2013). Although current disorders are less likely to be prone to recall biases (Grant et al., 2004), lifetime diagnoses are also relevant in contexts including identification of indications and contraindications for specific treatments, assessing risk and targeting prevention for chronologically secondary disorders (Grant et al., 2009), and phenotypic classifications for genetic studies (e.g., Bi et al., 2014; Kilcoyne et al., 2014). Furthermore, although the DSM-IV abuse diagnosis required only one criterion to be positive, the DSM-5 threshold of 2+ criteria has been criticized as too low on the grounds that large numbers of individuals manifesting very mild symptomatology will be diagnosed (e.g., Martin et al., 2011; Mewton et al., 2011, 2013). As such, concerns have been raised about the DSM-5 classification’s usefulness in indicating a need for treatment and informing its appropriate provision.
Accordingly, this study compared current and lifetime prevalences and examined within-respondent concordances between DSM-IV AUDs and specific DUDs and DSM-5 disorders at severity thresholds of 2+, 3+, and 4+ criteria in the newly completed National Epidemiologic Survey on Alcohol and Related Conditions–III (NESARC-III) (Grant et al., 2014). Because only nicotine dependence, not abuse, was diagnosable under DSM-IV, and alignment of nicotine use disorder with DSM-5 criteria for other SUDs involved additional questions about the utility and applicability of some generic SUD criteria to nicotine, nicotine use disorder is not considered herein.
Method
Sample
The research protocol, including informed consent procedures, received full approval from the institutional review boards of the National Institutes of Health and Westat. The target population of the NESARC-III was the noninstitutionalized civilian U.S. population 18 years or older (the 50 states and the District of Columbia), including residents of selected group quarters such as group homes and dormitories for workers (Grant et al., 2014). Respondents were selected through multistage probability sampling. Primary sampling units were individual counties or groups of contiguous counties. Secondary sampling units comprised groups of Census-defined blocks; in the third stage, households within the sampled secondary sampling units were selected. The last stage of sampling involved the random selection of eligible adults within sampled households. Minority individuals (Hispanic, Black, Asian) were assigned higher selection probabilities than nonminority household members. Further, in households with four or more eligible minority persons (n = 1,661), two respondents were selected. The total sample size was 36,309, with a household-level response rate of 72.0% and a person-level response rate of 84.0%. The overall response rate, the product of household- and person-level rates, was 60.1%, comparable to other national surveys (Centers for Disease Control and Prevention, 2014; Substance Abuse and Mental Health Services Administration, 2013) currently conducted in the United States.
Assessments
The diagnostic interview was the fully structured Alcohol Use Disorder and Associated Disabilities Interview Schedule– DSM-5 Version (AUDADIS-5; Grant et al., 2011), designed for experienced nonclinician interviewers. Extensive AUDADIS-5 questions covered both DSM-IV and DSM-5 criteria for SUDs associated with alcohol and 10 specific drug categories. A lifetime DSM-IV abuse diagnosis required 1 or more of 4 abuse criteria, whereas a DSM-IV dependence diagnosis required 3 or more of 7 dependence criteria (3 or more of 6 for drugs such as cannabis that did not have a withdrawal criterion defined), and a DSM-5 SUD diagnosis required at least 2 of 11 criteria. Under both diagnostic systems, the requisite number of criteria had to be met within the same 12-month period, either during or prior to the past year, for the same substance. Drug-specific DSM-IV abuse and dependence and DSM-5 disorders were aggregated to yield diagnoses of any drug abuse, any drug dependence, and any DUD, respectively.
Past-year and prior-to-past-year AUD and DUD diagnoses demonstrated fair to good test–retest reliability over a mean interval of 2.86 weeks (range: 1–10 weeks), whereas dimensional substance-specific criteria scales showed fair to excellent reliability (Grant et al., 2015). In a clinical reappraisal, AUD and DUD diagnoses showed fair to good agreement, whereas dimensional substance-specific criteria scales showed fair to excellent agreement across time frames with the clinician-administered, semistructured Psychiatric Research Interview for Substance and Mental Disorders (Hasin et al., 2015).
Statistical analysis
Standard contingency table approaches were used to derive weighted past-year and lifetime prevalences of substance-specific DSM-IV dependence and abuse combined; dependence with or without abuse; and any (2+ criteria), mild (2–3 criteria), and moderate to severe (4+ criteria) DSM-5 disorders, as well as DSM-5 disorders at thresholds of 3+ criteria (DSM-5 [3+]). We report results for alcohol, any drug, sedatives or tranquilizers, nonheroin opioids, cannabis, cocaine, stimulants, and heroin. Disorders associated with club drugs, hallucinogens, and “other drugs,” although included in the aggregated category of any drug, were too rare to yield stable estimates when considered separately.
Concordances of substance-specific DSM-IV dependence and DSM-IV dependence and abuse combined with DSM- 5 disorders at the various thresholds were assessed using Cohen’s kappa (Fleiss, 1981). Kappa measures chance-corrected agreement and generally ranges from -1.00 (perfect disagreement on all cases) to +1.00 (perfect concordance). Agreement was considered fair for κ values between .40 and .64, good between .65 and .74, and excellent for values ≥.75 (Fleiss, 1981). Pairs of kappa values were considered significantly different at the .05 level if their 95% confidence intervals did not overlap. SUDAAN software, Version 11.0 (Research Triangle Institute, 2012), which adjusts for the complex sample design characteristics of the NESARC-III, was used for all analyses.
The results reported herein are based on the entire NESARC-III respondent sample, consistent with previous nosologic comparison studies (e.g., Hasin et al., 1997a). To determine whether results differed for subpopulations of users of specific substances (e.g., past-year drinkers for past-year AUDs), analyses were also conducted separately among users. Patterns were similar, although the smaller denominators meant that SUD prevalences were higher. For specific comparisons (e.g., DSM-IV dependence and abuse combined vs. any DSM-5 [2+] past-year AUD), concordances were somewhat lower in user subsamples, but no differences in kappa values between the total sample and users materially altered the conclusions to be drawn. Given the overall similarity in results from the total sample and user subsamples, the latter will not be considered in detail but are available on request from the first author and will be mentioned briefly and as relevant in the discussion.
Results
Past year
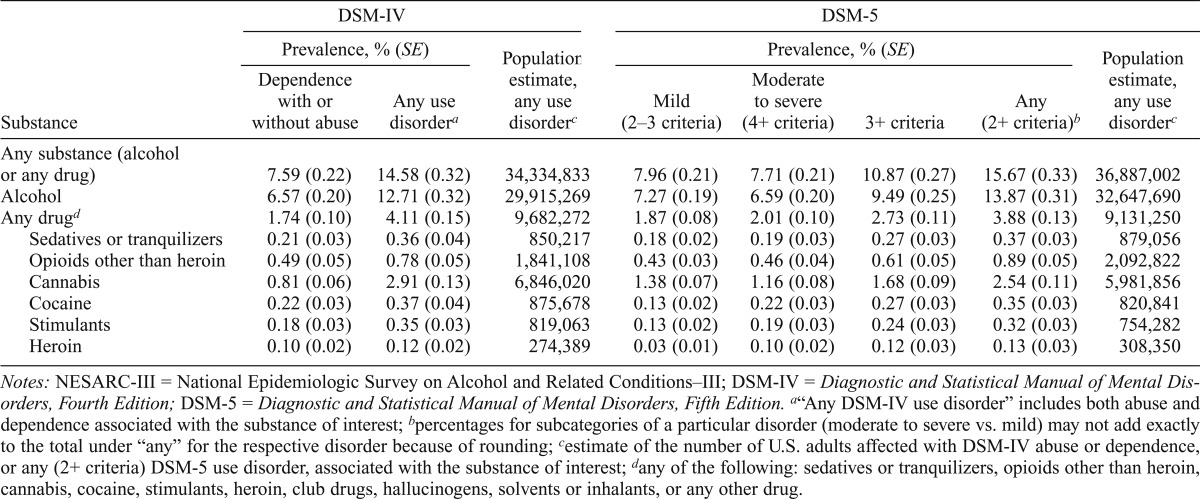
Prevalences of past-year DSM-IV and DSM-5 SUDs and population estimates of U.S. adults affected under each diagnostic system are given in Table 1. DSM-5 disorders were approximately evenly split between mild (2–3 criteria) and moderate to severe (4+) for all substances examined. Prevalences of any DSM-5 (2+) disorders were lower than those of DSM-IV dependence and abuse combined for cannabis, cocaine, and stimulants and were higher for alcohol, sedatives or tranquilizers, opioids, and heroin but differed by less than 10% except for opioids (14% higher) and cannabis (13% lower). Similarly, prevalences of specific DSM-5 moderate to severe disorders differed from those of DSM-IV dependence by less than 10% except for cannabis (DSM- 5 moderate to severe disorder, 43% higher). By contrast, prevalences of specific DSM-5 (3+) disorders other than cannabis ranged from 20% (heroin) to 44% (alcohol) higher than that of dependence, and that of DSM-5 (3+) cannabis use disorder was more than double.
Table 1.
Prevalences (%, SE) and population estimates of past-year substance use disorder diagnoses by classification system among NESARC-III respondents (n = 36,309)
| Substance | DSM-IV |
DSM-5 |
||||||
| Prevalence, % (SE) |
Population estimate, any use disorderc | Prevalence, % (SE) |
Population estimate, any use disorderc | |||||
| Dependence with or without abuse | Any use disordera | Mild (2–3 criteria) | Moderate to severe (4+ criteria) | 3+ criteria | Any (2+ criteria)b | |||
| Any substance (alcohol or any drug) | 7.59 (0.22) | 14.58 (0.32) | 34,334,833 | 7.96 (0.21) | 7.71 (0.21) | 10.87 (0.27) | 15.67 (0.33) | 36,887,002 |
| Alcohol | 6.57 (0.20) | 12.71 (0.32) | 29,915,269 | 7.27 (0.19) | 6.59 (0.20) | 9.49 (0.25) | 13.87 (0.31) | 32,647,690 |
| Any drugd | 1.74 (0.10) | 4.11 (0.15) | 9,682,272 | 1.87 (0.08) | 2.01 (0.10) | 2.73 (0.11) | 3.88 (0.13) | 9,131,250 |
| Sedatives or tranquilizers | 0.21 (0.03) | 0.36 (0.04) | 850,217 | 0.18 (0.02) | 0.19 (0.03) | 0.27 (0.03) | 0.37 (0.03) | 879,056 |
| Opioids other than heroin | 0.49 (0.05) | 0.78 (0.05) | 1,841,108 | 0.43 (0.03) | 0.46 (0.04) | 0.61 (0.05) | 0.89 (0.05) | 2,092,822 |
| Cannabis | 0.81 (0.06) | 2.91 (0.13) | 6,846,020 | 1.38 (0.07) | 1.16 (0.08) | 1.68 (0.09) | 2.54 (0.11) | 5,981,856 |
| Cocaine | 0.22 (0.03) | 0.37 (0.04) | 875,678 | 0.13 (0.02) | 0.22 (0.03) | 0.27 (0.03) | 0.35 (0.03) | 820,841 |
| Stimulants | 0.18 (0.03) | 0.35 (0.03) | 819,063 | 0.13 (0.02) | 0.19 (0.03) | 0.24 (0.03) | 0.32 (0.03) | 754,282 |
| Heroin | 0.10 (0.02) | 0.12 (0.02) | 274,389 | 0.03 (0.01) | 0.10 (0.02) | 0.12 (0.03) | 0.13 (0.03) | 308,350 |
Notes: NESARC-III = National Epidemiologic Survey on Alcohol and Related Conditions–III; DSM-IV = Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition; DSM-5 = Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition.
“Any DSM-IV use disorder” includes both abuse and dependence associated with the substance of interest;
percentages for subcategories of a particular disorder (moderate to severe vs. mild) may not add exactly to the total under “any” for the respective disorder because of rounding
estimate of the number of U.S. adults affected with DSM-IV abuse or dependence, or any (2+ criteria) DSM-5 use disorder, associated with the substance of interest
any of the following: sedatives or tranquilizers, opioids other than heroin, cannabis, cocaine, stimulants, heroin, club drugs, hallucinogens, solvents or inhalants, or any other drug.
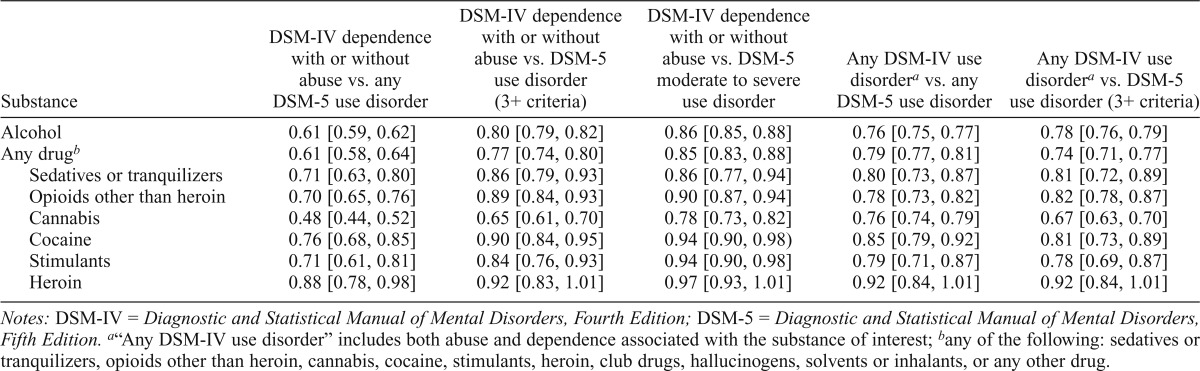
As shown in Table 2, concordances were excellent for any DSM-IV (dependence and abuse combined) versus any DSM- 5 (2+) disorders and for dependence versus DSM-5 moderate to severe (4+) disorders. Concordances of any DSM-IV with DSM-5 (3+) disorders were modestly higher than those of any DSM-IV with any DSM-5 disorders for alcohol, sedatives or tranquilizers, and nonheroin opioids, but significantly lower for cannabis, nonsignificantly lower for cocaine, and almost identical for stimulants and heroin. Whether or not the differences were statistically significant, kappa values for DSM-IV dependence and DSM-5 (3+) disorders were lower than those of dependence with moderate to severe DSM-5 disorders. For DSM-IV dependence and any DSM-5 disorders, they varied by substance: excellent for heroin and cocaine; good for nonheroin opioids, sedatives or tranquilizers, and stimulants; and fair for cannabis and alcohol.
Table 2.
Concordances (κ [95% confidence interval]) of past-year substance-specific DSM-IV and DSM-5 diagnoses
| Substance | DSM-IV dependence with or without abuse vs. any DSM-5 use disorder | DSM-IV dependence with or without abuse vs. DSM-5 use disorder (3+ criteria) | DSM-IV dependence with or without abuse vs. DSM-5 moderate to severe use disorder | Any DSM-IV use disordera vs. any DSM-5 use disorder | Any DSM-IV use disordera vs. DSM-5 use disorder (3+ criteria) |
| Alcohol | 0.61 [0.59, 0.62] | 0.80 [0.79, 0.82] | 0.86 [0.85, 0.88] | 0.76 [0.75, 0.77] | 0.78 [0.76, 0.79] |
| Any drugb | 0.61 [0.58, 0.64] | 0.77 [0.74, 0.80] | 0.85 [0.83, 0.88] | 0.79 [0.77, 0.81] | 0.74 [0.71, 0.77] |
| Sedatives or tranquilizers | 0.71 [0.63, 0.80] | 0.86 [0.79, 0.93] | 0.86 [0.77, 0.94] | 0.80 [0.73, 0.87] | 0.81 [0.72, 0.89] |
| Opioids other than heroin | 0.70 [0.65, 0.76] | 0.89 [0.84, 0.93] | 0.90 [0.87, 0.94] | 0.78 [0.73, 0.82] | 0.82 [0.78, 0.87] |
| Cannabis | 0.48 [0.44, 0.52] | 0.65 [0.61, 0.70] | 0.78 [0.73, 0.82] | 0.76 [0.74, 0.79] | 0.67 [0.63, 0.70] |
| Cocaine | 0.76 [0.68, 0.85] | 0.90 [0.84, 0.95] | 0.94 [0.90, 0.98) | 0.85 [0.79, 0.92] | 0.81 [0.73, 0.89] |
| Stimulants | 0.71 [0.61, 0.81] | 0.84 [0.76, 0.93] | 0.94 [0.90, 0.98] | 0.79 [0.71, 0.87] | 0.78 [0.69, 0.87] |
| Heroin | 0.88 [0.78, 0.98] | 0.92 [0.83, 1.01] | 0.97 [0.93, 1.01] | 0.92 [0.84, 1.01] | 0.92 [0.84, 1.01] |
Notes: DSM-IV = Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition; DSM-5 = Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition.
“Any DSM-IV use disorder” includes both abuse and dependence associated with the substance of interest;
any of the following: sedatives or tranquilizers, opioids other than heroin, cannabis, cocaine, stimulants, heroin, club drugs, hallucinogens, solvents or inhalants, or any other drug.
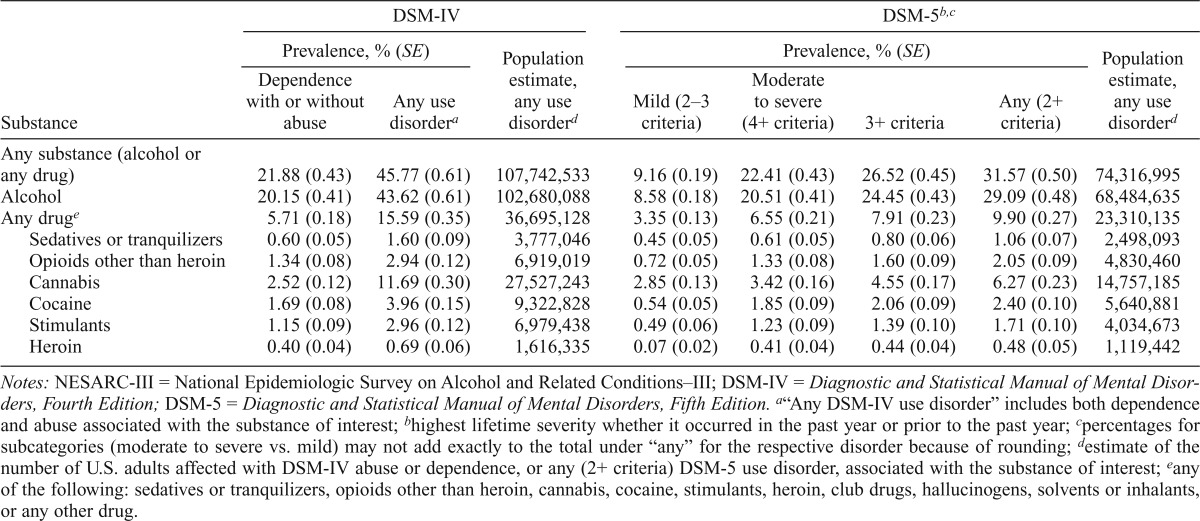
Lifetime
Prevalences of lifetime DSM-IV and DSM-5 SUDs and population estimates of U.S. adults affected under each diagnostic system are shown in Table 3. In contrast to past-year diagnoses, most DSM-5 disorders examined were moderate to severe (4+). Also in contrast to past-year diagnoses, prevalences of any DSM-5 (2+) disorder were 30% (nonheroin opioids) to 54% (cannabis) lower than those of DSM-IV dependence and abuse combined. Conversely, prevalences of DSM-5 moderate to severe disorders differed by less than 10% from those of dependence except for cannabis (36% higher under DSM-5). Prevalence of DSM-5 (3+) cannabis use disorder was more than double, whereas prevalences of other DSM-5 (3+) disorders were 10% (heroin) to 33% (sedatives or tranquilizers) higher than those of dependence.
Table 3.
Prevalences (%, SE) and population estimates of lifetime substance use disorder diagnoses by classification system among NESARC-III respondents (n = 36,309)
| Substance | DSM-IV |
DSM-5b,c |
||||||
| Prevalence, % (SE) |
Population estimate, any use disorderd | Prevalence, % (SE) |
Population estimate, any use disorderd | |||||
| Dependence with or without abuse | Any use disordera | Mild (2–3 criteria) | Moderate to severe (4+ criteria) | 3+ criteria | Any (2+ criteria) | |||
| Any substance (alcohol or any drug) | 21.88 (0.43) | 45.77 (0.61) | 107,742,533 | 9.16 (0.19) | 22.41 (0.43) | 26.52 (0.45) | 31.57 (0.50) | 74,316,995 |
| Alcohol | 20.15 (0.41) | 43.62 (0.61) | 102,680,088 | 8.58 (0.18) | 20.51 (0.41) | 24.45 (0.43) | 29.09 (0.48) | 68,484,635 |
| Any druge | 5.71 (0.18) | 15.59 (0.35) | 36,695,128 | 3.35 (0.13) | 6.55 (0.21) | 7.91 (0.23) | 9.90 (0.27) | 23,310,135 |
| Sedatives or tranquilizers | 0.60 (0.05) | 1.60 (0.09) | 3,777,046 | 0.45 (0.05) | 0.61 (0.05) | 0.80 (0.06) | 1.06 (0.07) | 2,498,093 |
| Opioids other than heroin | 1.34 (0.08) | 2.94 (0.12) | 6,919,019 | 0.72 (0.05) | 1.33 (0.08) | 1.60 (0.09) | 2.05 (0.09) | 4,830,460 |
| Cannabis | 2.52 (0.12) | 11.69 (0.30) | 27,527,243 | 2.85 (0.13) | 3.42 (0.16) | 4.55 (0.17) | 6.27 (0.23) | 14,757,185 |
| Cocaine | 1.69 (0.08) | 3.96 (0.15) | 9,322,828 | 0.54 (0.05) | 1.85 (0.09) | 2.06 (0.09) | 2.40 (0.10) | 5,640,881 |
| Stimulants | 1.15 (0.09) | 2.96 (0.12) | 6,979,438 | 0.49 (0.06) | 1.23 (0.09) | 1.39 (0.10) | 1.71 (0.10) | 4,034,673 |
| Heroin | 0.40 (0.04) | 0.69 (0.06) | 1,616,335 | 0.07 (0.02) | 0.41 (0.04) | 0.44 (0.04) | 0.48 (0.05) | 1,119,442 |
Notes: NESARC-III = National Epidemiologic Survey on Alcohol and Related Conditions–III; DSM-IV = Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition; DSM-5 = Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition.
“Any DSM-IV use disorder” includes both dependence and abuse associated with the substance of interest;
highest lifetime severity whether it occurred in the past year or prior to the past year
percentages for subcategories (moderate to severe vs. mild) may not add exactly to the total under “any” for the respective disorder because of rounding
estimate of the number of U.S. adults affected with DSM-IV abuse or dependence, or any (2+ criteria) DSM-5 use disorder, associated with the substance of interest
any of the following: sedatives or tranquilizers, opioids other than heroin, cannabis, cocaine, stimulants, heroin, club drugs, hallucinogens, solvents or inhalants, or any other drug.
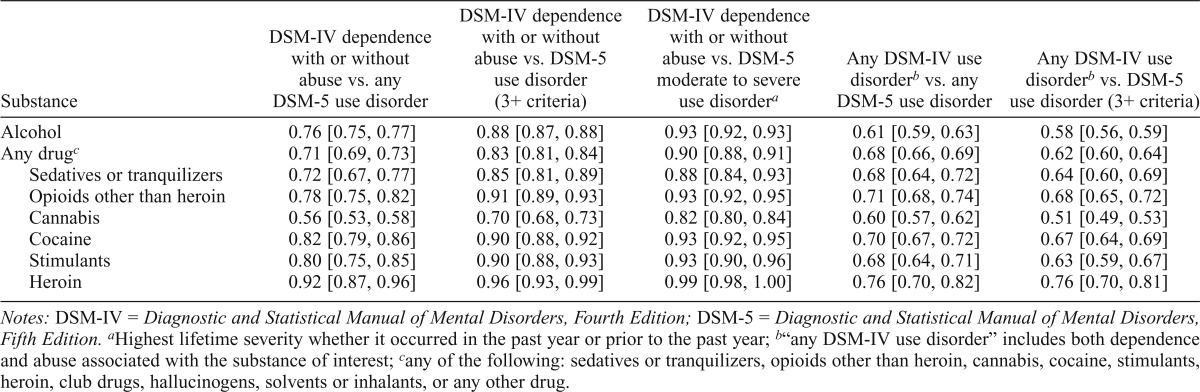
As shown in Table 4, kappa values for any DSM-IV (dependence and abuse combined) versus any DSM-5 (2+) disorders were excellent for heroin, fair for alcohol and cannabis, and good for all other substances. Whether or not differences were statistically significant, concordances for any DSM-IV versus DSM-5 (3+) disorders were lower except for heroin: good for nonheroin opioids and cocaine, fair for all other substances. Conversely, all concordances for DSM-IV dependence versus DSM-5 moderate to severe (4+) disorders were excellent. Between DSM-IV dependence and DSM-5 (3+) disorders, kappa values were lower than those for dependence with moderate to severe DSM-5 disorders but good for cannabis and excellent in all other substances. As with past-year diagnoses, concordances of DSM-IV dependence and any DSM-5 disorders varied by substance: good for sedatives or tranquilizers, fair for cannabis, and excellent for all others.
Table 4.
Concordances (κ [95% confidence interval]) of lifetime substance-specific DSM-IV and DSM-5 diagnoses
| Substance | DSM-IV dependence with or without abuse vs. any DSM-5 use disorder | DSM-IV dependence with or without abuse vs. DSM-5 use disorder (3+ criteria) | DSM-IV dependence with or without abuse vs. DSM-5 moderate to severe use disordera | Any DSM-IV use disorderb vs. any DSM-5 use disorder | Any DSM-IV use disorderb vs. DSM-5 use disorder (3+ criteria) |
| Alcohol | 0.76 [0.75, 0.77] | 0.88 [0.87, 0.88] | 0.93 [0.92, 0.93] | 0.61 [0.59, 0.63] | 0.58 [0.56, 0.59] |
| Any drugc | 0.71 [0.69, 0.73] | 0.83 [0.81, 0.84] | 0.90 [0.88, 0.91] | 0.68 [0.66, 0.69] | 0.62 [0.60, 0.64] |
| Sedatives or tranquilizers | 0.72 [0.67, 0.77] | 0.85 [0.81, 0.89] | 0.88 [0.84, 0.93] | 0.68 [0.64, 0.72] | 0.64 [0.60, 0.69] |
| Opioids other than heroin | 0.78 [0.75, 0.82] | 0.91 [0.89, 0.93] | 0.93 [0.92, 0.95] | 0.71 [0.68, 0.74] | 0.68 [0.65, 0.72] |
| Cannabis | 0.56 [0.53, 0.58] | 0.70 [0.68, 0.73] | 0.82 [0.80, 0.84] | 0.60 [0.57, 0.62] | 0.51 [0.49, 0.53] |
| Cocaine | 0.82 [0.79, 0.86] | 0.90 [0.88, 0.92] | 0.93 [0.92, 0.95] | 0.70 [0.67, 0.72] | 0.67 [0.64, 0.69] |
| Stimulants | 0.80 [0.75, 0.85] | 0.90 [0.88, 0.93] | 0.93 [0.90, 0.96] | 0.68 [0.64, 0.71] | 0.63 [0.59, 0.67] |
| Heroin | 0.92 [0.87, 0.96] | 0.96 [0.93, 0.99] | 0.99 [0.98, 1.00] | 0.76 [0.70, 0.82] | 0.76 [0.70, 0.81] |
Notes: DSM-IV = Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition; DSM-5 = Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition.
Highest lifetime severity whether it occurred in the past year or prior to the past year;
“any DSM-IV use disorder” includes both dependence and abuse associated with the substance of interest
any of the following: sedatives or tranquilizers, opioids other than heroin, cannabis, cocaine, stimulants, heroin, club drugs, hallucinogens, solvents or inhalants, or any other drug.
Discussion
Consistent with findings reported by Hasin et al. (2013), and despite concerns that the DSM-5 threshold of 2+ criteria would yield large increases in SUD prevalences (Martin et al., 2008, 2011; Mewton et al., 2011), this study found generally modest changes in past-year prevalences from DSM-IV (dependence and abuse combined) in the general U.S. adult population. Prevalences increased for some substances but decreased for others, yielding a net increase of 2.55 million U.S. adults with any DSM-5 AUD or DUD. Past-year concordances between DSM-IV dependence and abuse combined and any DSM-5 disorder were excellent for all substances, although generally slightly lower than those reported by Hasin et al. (2013). Results for thresholds of 2+ versus 3+ criteria varied by substance, both in the total sample and among users: modestly better between DSM-IV and DSM-5 at 3+ than at 2+ for alcohol, sedatives, nonheroin opioids, and heroin, but lower for cannabis and cocaine. For stimulants, total-sample concordance was modestly lower, but concordance among users was slightly higher between any DSM-IV and DSM-5 (3+) than between any DSM-IV and any DSM-5 diagnosis.
In contrast to past-year findings, lifetime prevalences decreased from any DSM-IV to any DSM-5 disorder for all substances examined, with lower concordances. Discrepancies between DSM-IV and DSM-5 primarily reflected prior-to-past-year abuse, usually diagnosed on the basis of a single criterion (most commonly hazardous use). Respondents with prior-to-past-year abuse who were negative under DSM-5 also commonly endorsed one or more dependence criteria or, less often, craving, but denied same-year clustering of symptoms. Of note, and contrasting with past-year findings, concordances were lower between any DSM-IV disorder and DSM-5 (3+) than between any DSM-IV and any DSM-5 disorder except for heroin among users.
Revisions to diagnostic classification systems must balance the competing considerations of consistency versus improvement. Although there are no formal definitions of how much change is acceptable, results are expected to differ across systems; nevertheless, if they differ dramatically, then continuity of clinical and research endeavors is threatened. Taken together, the present findings suggest that, consistent with evidence used to inform the DSM-5 Work Group’s deliberations (Hasin et al., 2013), the diagnostic threshold of 2+ criteria has met reasonably well the Work Group’s goals of harmonizing prevalences and optimizing concordances with DSM-IV, particularly for past-year disorders. Nevertheless, the differences between past-year and lifetime patterns of results regarding both prevalences and concordances may warrant further examination. Past-year and lifetime diagnoses may be differentially relevant to particular endeavors. For example, past-year diagnoses may be most relevant to epidemiologic determination of period prevalence and resource allocation to screening and treatment services. Conversely, purposes for which lifetime diagnoses are most relevant include phenotypic definitions for genetic studies and development and implementation of preventive interventions against chronologically secondary disorders. Still, it is important to understand time frame–specific patterns of convergence and divergence with potential implications for further evaluations of DSM-5 nosology.
Future research is also needed to address concerns that cases captured by the 2+ threshold are too heterogeneous and that not all are clinically significant enough to be considered “true” cases (Hasin et al., 2013). Relatedly, recent findings (Saha & Grant, 2014) point to important differences in severity among various combinations of the same numbers of criteria, concerns also raised with regard to DSM-IV dependence and abuse criteria by Grant (2000). Although the Work Group concluded that a simple count of criteria was preferable for measuring severity (Hasin et al., 2013), further investigations of the clinical significance of heterogeneity among different combinations of the same counts of criteria and their implications for course, prognosis, and treatment appear warranted. Additional work with confirmatory factor analyses may also help elucidate the structure of the 11 DSM-5 symptom criteria.
The very close resemblances for substances other than cannabis between prevalences of past-year and lifetime DSM-IV dependence and moderate to severe DSM-5 disorders are compatible with findings for past-year AUDs reported by Dawson et al. (2013). As well, paralleling findings on DSM-5 disorders and past-year dependence reported by Compton et al. (2013), concordances between dependence and DSM-5 disorders for substances other than cannabis were maximized at DSM-5 thresholds of 4+ criteria (data on concordances at thresholds of >4 criteria not shown). The close agreement between DSM-IV dependence and DSM-5 moderate to severe disorders other than those associated with cannabis adds to the evidence (Compton et al., 2013; Dawson et al., 2013; Peer et al., 2013) that pharmacologic treatments for alcohol and opioid dependence can be reasonably applied to DSM-5 disorders of at least moderate severity. Future work on medications to treat cocaine use disorders can likewise focus on moderate and higher severity. However, the appropriateness of treatments for dependence to mild alcohol, opioid, and cocaine use disorders warrants further examination. The application of psychosocial treatments to DSM-5 disorders at various levels of severity also merits appraisal.
Cannabis use disorders showed the greatest divergences between DSM-IV and DSM-5. Lifetime prevalence of any disorder showed the largest decrease, whereas DSM-5 moderate to severe and DSM-5 (3+) showed the greatest increases over dependence. The decrease in prevalence of any disorder from DSM-IV to DSM-5 is also much larger than that reported by Mewton et al. (2013); however, the lifetime prevalence under DSM-5 (5.4%) reported by Mewton et al. (2013) and the proportions of mild versus moderate to severe disorders were similar to those in the present sample. The prevalence of dependence and abuse combined (6.2%) reported by Mewton et al. (2013) was much lower than that in the present study, likely reflecting differences in operationalization of the hazardous use criterion (Mewton et al., 2013). Concordances between DSM-IV dependence and DSM-5 disorders were maximized at 5+ DSM-5 criteria, 1 fewer than observed by Compton et al. (2013) but 1 more than for other drugs (data not shown).
To a limited degree, the divergence of results for cannabis from those for other substances reflects the lack of a cannabis withdrawal criterion under DSM-IV and its addition in DSM-5. The DSM-5 definition of cannabis withdrawal is complex, requiring manifestations in at least three of seven domains (irritability, anger, or aggression; nervousness or anxiety; sleep disturbance; decreased appetite or weight; restlessness; depressed mood; and at least one somatic symptom causing significant discomfort from among abdominal pain, shakiness or tremors, sweating, fever, chills, or headache). Cannabis withdrawal criteria also specify a more stringent definition of “heavy and prolonged” use preceding cessation and withdrawal symptomatology (usually daily or near-daily use over at least a few months) than for other substances (American Psychiatric Association, 2013). Prevalences of DSM-IV diagnoses increased slightly when the DSM-5 withdrawal criterion was added to DSM-IV cannabis dependence (past-year dependence: 0.94% vs. 0.81%; any past-year DSM-IV disorder: 2.95% vs. 2.91%; lifetime dependence: 2.81% vs. 2.52%; any lifetime DSM-IV disorder: 11.76% vs. 11.69%). Concordances improved slightly in both past year and lifetime between DSM-IV dependence and any DSM-5 disorder (past year: 0.53 vs. 0.48; lifetime: 0.60 vs. 0.56), DSM-IV dependence and DSM-5 (3+) (past year: 0.72 vs. 0.65; lifetime: 0.76 vs. 0.70), and DSM-IV dependence and DSM-5 moderate to severe disorders (past year: 0.82 vs. 0.78; lifetime: 0.86 vs. 0.82) while remaining unchanged between any DSM-IV and any DSM-5 use disorders, and between any DSM-IV and DSM-5 (3+). Even with a withdrawal criterion specified for DSM-IV dependence, however, concordances for cannabis-related diagnoses remained generally poorer than those for disorders associated with other substances.
These findings also reflect unique patterns of criterion endorsement associated with cannabis (Compton et al., 2013; Mewton et al., 2013) that lead to a higher ratio under DSM-IV of abuse to dependence (past year: 2.58:1; lifetime: 3.64:1; when withdrawal was added to DSM-IV dependence criteria, 2.14:1 and 3.19:1) than for other substances (past year: 0.10:1 for heroin to 0.94:1 for stimulants; lifetime: 0.70:1 for heroin to 1.68:1 for sedatives or tranquilizers). Taken together, these results indicate a need to reexamine the appropriateness of treatments currently being tested for cannabis dependence at DSM-5 thresholds lower than five criteria. More broadly, the question of whether cannabis-specific symptom thresholds are indicated may warrant further study.
Limitations of this study include its reliance on retrospectively self-reported data. Symptoms that occurred long ago, and their temporal clustering, may not have been accurately recalled or reported, especially among individuals in long-term, stable recovery (cf. Rueter et al., 2000). Such errors may have contributed to disparate patterns in past-year versus lifetime diagnoses and led to some underestimation of prevalences. In addition, the NESARC-III by design examined AUDs and DUDs in the general adult population. Recent work in clinical samples (Hasin et al., 2013) suggests that patients in SUD treatment are unlikely to present importantly different patterns of convergence and divergence between DSM-IV and DSM-5 SUDs. Nevertheless, the exclusion of individuals in correctional and other institutional settings means that the applicability of present findings to them is unclear.
The NESARC-III response rate, 60.1%, although comparable with rates in other current U.S. national surveys, is lower than in previous surveys of similar scope (cf. Grant, 1997; Grant et al., 2009), reflecting a general trend of declining response rates (Galea & Tracy, 2007). Response-related sociodemographic differences can be eliminated as a source of bias through appropriate adjustments to case weights. In addition, previous studies have found only modest nonresponse biases in survey estimates of alcohol consumption (Dawson et al., 2014; Lahaut et al., 2003; Lemmens et al, 1988; Meiklejohn et al., 2012) and little evidence for biases in estimates of related harms (Dawson et al., 2014). Low response rates do not necessarily yield biased estimates of associations of interest (Galea & Tracy, 2007).
Despite these limitations, this study importantly extends previous nosologic research (Grant, 1992; Grant et al., 1992; Hasin & Grant, 1994a, 1994b; Hasin et al., 1996, 1997a) by examining both past-year and lifetime prevalences and concordances between specific DSM-IV and DSM-5 SUD diagnoses in a newly collected sample of U.S. adults with an assessment specifically designed to query both classification systems. Findings generally accord with those from analyses of previously collected data that informed the development of DSM-5. Aspects of SUD epidemiology under DSM-IV versus DSM-5 criteria, including disability, comorbidity, and clinical characteristics, warrant investigation for further elucidation of the nosologic performance of the two diagnostic systems in contemporary populations.
In addition to the implications of these results for further nosologic work, potential changes in treatment demand for DSM-5 SUDs warrant examination. Dawson et al. (2013) found that only about 2% of general population adults with mild, and 13% to 15% with moderate to severe, past-year AUDs sought services. Therefore, at least for AUDs, low rates of utilization combined with this study’s findings of modest increases in overall past-year prevalence and a nearly even split between mild and moderate to severe disorders make it unlikely that there will be large increases in demand for services from newly diagnosable cases, particularly at the milder end of the spectrum. Nevertheless, research using current data is indicated to determine how changes in prevalences of a broader range of past-year SUD diagnoses will affect treatment demand. In addition, the extent to which individuals with partially or fully remitted prior-to-past-year mild and moderate to severe DSM-5 SUDs will use help to further their recoveries, and implications for service provision, warrant investigation. Similarly, implications for use of DSM-5 in prevention warrant examination, for example, its utility in matching up and aiding assessment and intervention at different levels of problem severity and, relatedly, in tracking the dimensional criteria count over time to document effects of primary, secondary, and tertiary preventive approaches on the natural history of SUDs (Babor, 2011; Slade et al., 2011).
Last, the sociodemographic and clinical profiles of individuals with specific DSM-IV versus DSM-5 disorders have received limited attention. Mewton et al. (2013) compared individuals with any lifetime cannabis use disorders under both systems and those with disorders only under DSM-5 (2+ criteria), finding elevated odds of being male and of having a comorbid AUD but no other differences. Similarly, Dawson et al. (2013) found few differences in the characteristics of individuals with past-year dependence versus DSM-5 moderate to severe AUDs. However, respondents with DSM-IV abuse differed sociodemographically from those with DSM-5 mild AUD in ways indicating both greater diversity (more women and Black individuals) and greater economic disadvantage (lower incomes, higher rates of public and lower rates of private insurance) among the latter category. Those with DSM-5 mild AUD were also more likely to endorse physiologic dependence and craving and carry a comorbid anxiety disorder diagnosis (Dawson et al., 2013). To our knowledge, similarities and differences between respondents diagnosed under either system with prior-to-past-year AUDs that have remitted, or DUDs in either time frame, have not been investigated. Approaches to screening and intervention for individuals who would have been classified with DSM-IV abuse may thus require reexamination both on clinical grounds and for cultural, ethnic, and sex and gender appropriateness. Also in light of possible differences in insurance coverage and recent developments in U.S. health care reform, implications for reimbursement of treatment for mild disorders should be examined.
Footnotes
The National Epidemiologic Survey on Alcohol and Related Conditions- III (NESARC-III) is funded by the National Institute on Alcohol Abuse and Alcoholism (NIAAA) with supplemental support from the National Institute on Drug Abuse. This research was supported in part by the Intramural Program of the National Institutes of Health, NIAAA. The views and opinions expressed in this report are those of the authors and should not be construed to represent the views of sponsoring organizations, agencies, or the U.S. government.
References
- Agrawal A., Pergadia M. L., Lynskey M. T. Is there evidence for symptoms of cannabis withdrawal in the National Epidemiologic Survey of Alcohol and Related Conditions? American Journal on Addictions. 2008;17:199–208. doi: 10.1080/10550490802019519. [DOI] [PubMed] [Google Scholar]
- Agrawal A., Wetherill L., Bucholz K. K., Kramer J., Kuperman S., Lynskey M. T., Bierut L. J. Genetic influences on craving for alcohol. Addictive Behaviors. 2013;38:1501–1508. doi: 10.1016/j.addbeh.2012.03.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4th ed. Washington, DC: Author; 1994. [Google Scholar]
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 5th ed. Arlington, VA: Author; 2013. [Google Scholar]
- Babor T. F. Substance, not semantics, is the issue: Comments on the proposed addiction criteria for DSM-V. Addiction. 2011;106:870–872. doi: 10.1111/j.1360-0443.2010.03313.x. discussion 895–897. [DOI] [PubMed] [Google Scholar]
- Beseler C. L., Hasin D. S. Cannabis dimensionality: Dependence, abuse and consumption. Addictive Behaviors. 2010;35:961–969. doi: 10.1016/j.addbeh.2010.06.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beynon C. Diagnosing the use of illegal drugs by older people— comments on the proposed changes to DSM-V. Addiction. 2011;106:884–885. doi: 10.1111/j.1360-0443.2010.03283.x. discussion 895–897. [DOI] [PubMed] [Google Scholar]
- Bi J., Gelernter J., Sun J., Kranzler H. R. Comparing the utility of homogeneous subtypes of cocaine use and related behaviors with DSM-IV cocaine dependence as traits for genetic association analysis. American Journal of Medical Genetics Part B: Neuropsychiatric Genetics. 2014;165:148–156. doi: 10.1002/ajmg.b.32216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Budney A. J., Hughes J. R. The cannabis withdrawal syndrome. Current Opinion in Psychiatry. 2006;19:233–238. doi: 10.1097/01.yco.0000218592.00689.e5. [DOI] [PubMed] [Google Scholar]
- Budney A. J., Hughes J. R., Moore B. A., Vandrey R. Review of the validity and significance of cannabis withdrawal syndrome. American Journal of Psychiatry. 2004;161:1967–1977. doi: 10.1176/appi.ajp.161.11.1967. [DOI] [PubMed] [Google Scholar]
- Caetano R.2011There is potential for cultural and social bias in DSM-V Addiction 106885–887., discussion 895–897 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. Summary health statistics for U.S. adults: National Health Interview Survey, 2012. Vital and Health Statistics, Series 10, Number 260. 2014 Retrieved from http://www.cdc.gov/nchs/data/series/sr_10/sr10_260.pdf.
- Cherpitel C. J., Borges G., Ye Y., Bond J., Cremonte M., Moskalewicz J., Swiatkiewicz G. Performance of a craving criterion in DSM alcohol use disorders. Journal of Studies on Alcohol and Drugs. 2010;71:674–684. doi: 10.15288/jsad.2010.71.674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chung T., Martin C. S., Cornelius J. R., Clark D. B. Cannabis withdrawal predicts severity of cannabis involvement at 1-year follow-up among treated adolescents. Addiction. 2008;103:787–799. doi: 10.1111/j.1360-0443.2008.02158.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Compton W. M., Dawson D. A., Goldstein R. B., Grant B. F. Crosswalk between DSM-IV dependence and DSM-5 substance use disorders for opioids, cannabis, cocaine and alcohol. Drug and Alcohol Dependence. 2013;132:387–390. doi: 10.1016/j.drugalcdep.2013.02.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Compton W. M., Saha T. D., Conway K. P., Grant B. F. The role of cannabis use within a dimensional approach to cannabis use disorders. Drug and Alcohol Dependence. 2009;100:221–227. doi: 10.1016/j.drugalcdep.2008.10.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Compton W. M., Thomas Y. F., Stinson F. S., Grant B. F. Prevalence, correlates, disability, and comorbidity of DSM-IV drug abuse and dependence in the United States: Results from the National Epidemiologic Survey on Alcohol and Related Conditions. Archives of General Psychiatry. 2007;64:566–576. doi: 10.1001/archpsyc.64.5.566. [DOI] [PubMed] [Google Scholar]
- Copersino M. L., Boyd S. J., Tashkin D. P., Huestis M. A., Heishman S. J., Dermand J. C., Gorelick D. A. Cannabis withdrawal among non-treatment-seeking adult cannabis users. American Journal on Addictions. 2006;15:8–14. doi: 10.1080/10550490500418997. [DOI] [PubMed] [Google Scholar]
- Cornelius J. R., Chung T., Martin C., Wood D. S., Clark D. B. Cannabis withdrawal is common among treatment-seeking adolescents with cannabis dependence and major depression, and is associated with rapid relapse to dependence. Addictive Behaviors. 2008;33:1500–1505. doi: 10.1016/j.addbeh.2008.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dawson D. A. Drinking patterns among individuals with and without DSM-IV alcohol use disorders. Journal of Studies on Alcohol. 2000;61:111–120. doi: 10.15288/jsa.2000.61.111. [DOI] [PubMed] [Google Scholar]
- Dawson D. A., Goldstein R. B., Grant B. F. Differences in the profiles of DSM-IV and DSM-5 alcohol use disorders: Implications for clinicians. Alcoholism: Clinical and Experimental Research, 37, Supplement. 2013;S1:E305–E313. doi: 10.1111/j.1530-0277.2012.01930.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dawson D. A., Saha T. D., Grant B. F. A multidimensional assessment of the validity and utility of alcohol use disorder severity as determined by item response theory models. Drug and Alcohol Dependence. 2010;107:31–38. doi: 10.1016/j.drugalcdep.2009.08.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dawson D. A., Goldstein R. B., Pickering R. P., Grant B. F. Nonresponse bias in survey estimates of alcohol consumption and its association with harm. Journal of Studies on Alcohol and Drugs. 2014;75:695–703. doi: 10.15288/jsad.2014.75.695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Drummond C. The end of the dependence syndrome as we know it? Addiction. 2011;106:892–894. doi: 10.1111/j.1360-0443.2010.03314.x. discussion 895–897. [DOI] [PubMed] [Google Scholar]
- Fleiss J. L. Statistical methods for rates and proportions. 2nd ed. New York, NY: John Wiley and Sons; 1981. [Google Scholar]
- Foroud T., Wetherill L. F., Liang T., Dick D. M., Hesselbrock V., Kramer J., Edenberg H. J. Association of alcohol craving with alpha-synuclein (SNCA) Alcoholism: Clinical and Experimental Research. 2007;31:537–545. doi: 10.1111/j.1530-0277.2007.00337.x. [DOI] [PubMed] [Google Scholar]
- Galea S., Tracy M. Participation rates in epidemiologic studies. Annals of Epidemiology. 2007;17:643–653. doi: 10.1016/j.annepidem.2007.03.013. [DOI] [PubMed] [Google Scholar]
- Gillespie N. A., Neale M. C., Prescott C. A., Aggen S. H., Kendler K. S. Factor and item-response analysis DSM-IV criteria for abuse of and dependence on cannabis, cocaine, hallucinogens, sedatives, stimulants and opioids. Addiction. 2007;102:920–930. doi: 10.1111/j.1360-0443.2007.01804.x. [DOI] [PubMed] [Google Scholar]
- Goldstein R. Z., Volkow N. D. Dysfunction of the prefrontal cortex in addiction: Neuroimaging findings and clinical implications. Nature Reviews Neuroscience. 2011;12:652–669. doi: 10.1038/nrn3119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grant B. F. DSM-III-R and proposed DSM-IV alcohol abuse and dependence, United States 1988: A nosological comparison. Alcoholism: Clinical and Experimental Research. 1992;16:1068–1077. doi: 10.1111/j.1530-0277.1992.tb00701.x. [DOI] [PubMed] [Google Scholar]
- Grant B. F. Prevalence and correlates of alcohol use and DSM-IV alcohol dependence in the United States: Results of the National Longitudinal Alcohol Epidemiologic Survey. Journal of Studies on Alcohol. 1997;58:464–473. doi: 10.15288/jsa.1997.58.464. [DOI] [PubMed] [Google Scholar]
- Grant B. F. Theoretical and observed subtypes of DSM-IV alcohol abuse and dependence in a general population sample. Drug and Alcohol Dependence. 2000;60:287–293. doi: 10.1016/s0376-8716(00)00115-0. [DOI] [PubMed] [Google Scholar]
- Grant B. F., Amsbary M., Chu A., Sigman R., Kali J., Sugawana Y., Smith S. M. Source and accuracy statement: National Epidemiologic Survey on Alcohol and Related Conditions–III (NESARC-III). Rockville, MD: National Institute on Alcohol and Abuse and Alcoholism; 2014. [Google Scholar]
- Grant B. F., Compton W. M., Crowley T. J., Hasin D. S., Helzer J. E., Li T.-K., Woody G. E.2007Errors in assessing DSM-IV substance use disorders [Letter to the editor] Archives of General Psychiatry 64379–380., author reply 381–382 [DOI] [PubMed] [Google Scholar]
- Grant B. F., Goldstein R. B., Chou S. P., Huang B., Stinson F. S., Dawson D. A., Compton W. M. Sociodemographic and psychopathologic predictors of first incidence of DSM-IV substance use, mood and anxiety disorders: Results from the Wave 2 National Epidemiologic Survey on Alcohol and Related Conditions. Molecular Psychiatry. 2009;14:1051–1066. doi: 10.1038/mp.2008.41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grant B. F., Goldstein R. B., Chou S. P., Saha T. D., Ruan W. J., Huang B., Hasin D. S. The Alcohol Use Disorder and Associated Disabilities Interview Schedule – DSM-5 Version (AUDADIS-5). Rockville, MD: National Institute on Alcohol Abuse and Alcoholism; 2011. [Google Scholar]
- Grant B. F., Goldstein R. B., Smith S. M., Jung J., Zhang H., Chou S. P., Hasin D. S. The Alcohol Use Disorder and Associated Disabilities Interview Schedule-5 (AUDADIS-5): Reliability of substance use and psychiatric disorder modules in a general population sample. Drug and Alcohol Dependence. 2015;148:27–33. doi: 10.1016/j.drugalcdep.2014.11.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grant B. F., Harford T. C., Hasin D. S., Chou P., Pickering R. DSM-III-R and the proposed DSM-IV alcohol use disorders, United States 1988: A nosological comparison. Alcoholism: Clinical and Experimental Research. 1992;16:215–221. doi: 10.1111/j.1530-0277.1992.tb01366.x. [DOI] [PubMed] [Google Scholar]
- Grant B. F., Stinson F. S., Dawson D. A., Chou S. P., Dufour M. C., Compton W., Kaplan K. Prevalence and co-occurrence of substance use disorders and independent mood and anxiety disorders: Results from the National Epidemiologic Survey on Alcohol and Related Conditions. Archives of General Psychiatry. 2004;61:807–816. doi: 10.1001/archpsyc.61.8.807. [DOI] [PubMed] [Google Scholar]
- Grant B. F., Stinson F. S., Harford T. C. Age at onset of alcohol use and DSM-IV alcohol abuse and dependence: A 12-year follow-up. Journal of Substance Abuse. 2001;13:493–504. doi: 10.1016/s0899-3289(01)00096-7. [DOI] [PubMed] [Google Scholar]
- Hasin D. S., Beseler C. L. Dimensionality of lifetime alcohol abuse, dependence and binge drinking. Drug and Alcohol Dependence. 2009;101:53–61. doi: 10.1016/j.drugalcdep.2008.10.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hasin D. S., Fenton M. C., Beseler C., Park J. Y., Wall M. M. Analyses related to the development of DSM-5 criteria for substance use related disorders: 2. Proposed DSM-5 criteria for alcohol, cannabis, cocaine and heroin disorders in 663 substance abuse patients. Drug and Alcohol Dependence. 2012;122:28–37. doi: 10.1016/j.drugalcdep.2011.09.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hasin D. S., Grant B. Nosological comparisons of DSM-III-R and DSM-IV alcohol abuse and dependence in a clinical facility: Comparison with the 1988 National Health Interview Survey results. Alcoholism: Clinical and Experimental Research. 1994a;18:272–280. doi: 10.1111/j.1530-0277.1994.tb00014.x. [DOI] [PubMed] [Google Scholar]
- Hasin D., Grant B. 1994 Draft DSM-IV criteria for alcohol use disorders: Comparison to DSM-III-R and implications. Alcoholism: Clinical and Experimental Research. 1994b;18:1348–1353. doi: 10.1111/j.1530-0277.1994.tb01435.x. [DOI] [PubMed] [Google Scholar]
- Hasin D. S., Grant B. F. The co-occurrence of DSM-IV alcohol abuse in DSM-IV alcohol dependence: Results of the National Epidemiologic Survey on Alcohol and Related Conditions on heterogeneity that differ by population subgroup. Archives of General Psychiatry. 2004;61:891–896. doi: 10.1001/archpsyc.61.9.891. [DOI] [PubMed] [Google Scholar]
- Hasin D., Grant B. F., Cottler L., Blaine J., Towle L., Ustün B., Sartorius N. Nosological comparisons of alcohol and drug diagnoses: A multisite, multi-instrument international study. Drug and Alcohol Dependence. 1997a;47:217–226. doi: 10.1016/s0376-8716(97)00092-6. [DOI] [PubMed] [Google Scholar]
- Hasin D. S., Grant B., Endicott J. The natural history of alcohol abuse: Implications for definitions of alcohol use disorders. American Journal of Psychiatry. 1990;147:1537–1541. doi: 10.1176/ajp.147.11.1537. [DOI] [PubMed] [Google Scholar]
- Hasin D. S., Greenstein E., Aivadyan C., Stohl M., Aharonovich E., Saha T., Grant B. F. The Alcohol Use Disorder and Associated Disabilities Interview Schedule – 5 (AUDADIS-5): Procedural validity of substance use disorders modules through clinical re-appraisal in a general population sample. Drug and Alcohol Dependence. 2015;148:40–46. doi: 10.1016/j.drugalcdep.2014.12.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hasin D., Hatzenbuehler M. L., Keyes K., Ogburn E. Substance use disorders: Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV) and International Classification of Diseases, Tenth Edition (ICD-10) Addiction, 101, Supplement. 2006a;1:59–75. doi: 10.1111/j.1360-0443.2006.01584.x. [DOI] [PubMed] [Google Scholar]
- Hasin D. S., Hatzenbueler M., Smith S., Grant B. F. Co-occurring DSM-IV drug abuse in DSM-IV drug dependence: Results from the National Epidemiologic Survey on Alcohol and Related Conditions. Drug and Alcohol Dependence. 2005;80:117–123. doi: 10.1016/j.drugalcdep.2005.03.010. [DOI] [PubMed] [Google Scholar]
- Hasin D. S., Keyes K. M., Alderson D., Wang S., Aharonovich E., Grant B. F. Cannabis withdrawal in the United States: Results from NESARC. Journal of Clinical Psychiatry. 2008;69:1354–1363. doi: 10.4088/jcp.v69n0902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hasin D., Li Q., McCloud S., Endicott J. Agreement between DSM-III, DSM-III-R, DSM-IV and ICD-10 alcohol diagnoses in US community-sample heavy drinkers. Addiction. 1996;91:1517–1527. doi: 10.1046/j.1360-0443.1996.9110151710.x. [DOI] [PubMed] [Google Scholar]
- Hasin D. S., Liu X., Alderson D., Grant B. F. DSM-IV alcohol dependence: A categorical or dimensional phenotype? Psychological Medicine. 2006b;36:1695–1705. doi: 10.1017/S0033291706009068. [DOI] [PubMed] [Google Scholar]
- Hasin D. S., O’Brien C. P., Auriacombe M., Borges G., Bucholz K., Budney A., Grant B. F. DSM-5 criteria for substance use disorders: Recommendations and rationale. American Journal of Psychiatry. 2013;170:834–851. doi: 10.1176/appi.ajp.2013.12060782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hasin D., Paykin A. Dependence symptoms but no diagnosis: Diagnostic ‘orphans’ in a community sample. Drug and Alcohol Dependence. 1998;50:19–26. doi: 10.1016/s0376-8716(98)00007-6. [DOI] [PubMed] [Google Scholar]
- Hasin D., Paykin A. DSM-IV alcohol abuse: Investigation in a sample of at-risk drinkers in the community. Journal of Studies on Alcohol. 1999;60:181–187. doi: 10.15288/jsa.1999.60.181. [DOI] [PubMed] [Google Scholar]
- Hasin D., Paykin A., Endicott J., Grant B. The validity of DSM-IV alcohol abuse: Drunk drivers versus all others. Journal of Studies on Alcohol. 1999;60:746–755. doi: 10.15288/jsa.1999.60.746. [DOI] [PubMed] [Google Scholar]
- Hasin D. S., Stinson F. S., Ogburn E., Grant B. F. Prevalence, correlates, disability, and comorbidity of DSM-IV alcohol abuse and dependence in the United States: Results from the National Epidemiologic Survey on Alcohol and Related Conditions. Archives of General Psychiatry. 2007;64:830–842. doi: 10.1001/archpsyc.64.7.830. [DOI] [PubMed] [Google Scholar]
- Hasin D. S., Van Rossem R., McCloud S., Endicott J. Differentiating DSM-IV alcohol dependence and abuse by course: Community heavy drinkers. Journal of Substance Abuse. 1997b;9:127–135. doi: 10.1016/s0899-3289(97)90011-0. [DOI] [PubMed] [Google Scholar]
- Heinz A., Beck A., Grüsser S. M., Grace A. A., Wrase J. Identifying the neural circuitry of alcohol craving and relapse vulnerability. Addiction Biology. 2009;14:108–118. doi: 10.1111/j.1369-1600.2008.00136.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keyes K. M., Krueger R. F., Grant B. F., Hasin D. S. Alcohol craving and the dimensionality of alcohol disorders. Psychological Medicine. 2011;41:629–640. doi: 10.1017/S003329171000053X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kilcoyne B., Shmulewitz D., Meyers J. L., Aharonovich E., Greenstein E., Frisch A., Hasin D. S. Alcohol consumption mediates the relationship between ADH1B and DSM-IV alcohol use disorder and criteria. Journal of Studies on Alcohol and Drugs. 2014;75:635–642. doi: 10.15288/jsad.2014.75.635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lahaut V. M., Jansen H. A., van de Mheen D., Garretsen H. F., Verdurmen J. E. E., van Dijk A. Estimating non-response bias in a survey on alcohol consumption: Comparison of response waves. Alcohol and Alcoholism. 2003;38:128–134. doi: 10.1093/alcalc/agg044. [DOI] [PubMed] [Google Scholar]
- Langenbucher J. W., Labouvie E., Martin C. S., Sanjuan P. M., Bavly L., Kirisci L., Chung T. An application of item response theory analysis to alcohol, cannabis, and cocaine criteria in DSM-IV. Journal of Abnormal Psychology. 2004;113:72–80. doi: 10.1037/0021-843X.113.1.72. [DOI] [PubMed] [Google Scholar]
- Lemmens P. H. H. M., Tan E. S., Knibbe R. A. Bias due to nonresponse in a Dutch survey on alcohol consumption. British Journal of Addiction. 1988;83:1069–1077. doi: 10.1111/j.1360-0443.1988.tb00534.x. [DOI] [PubMed] [Google Scholar]
- Levin K. H., Copersino M. L., Heishman S. J., Liu F., Kelly D. L., Boggs D. L., Gorelick D. A. Cannabis withdrawal symptoms in non-treatment-seeking adult cannabis smokers. Drug and Alcohol Dependence. 2010;111:120–127. doi: 10.1016/j.drugalcdep.2010.04.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lynskey M. T., Agrawal A. Psychometric properties of DSM assessments of illicit drug abuse and dependence: Results from the National Epidemiologic Survey on Alcohol and Related Conditions (NESARC) Psychological Medicine. 2007;37:1345–1355. doi: 10.1017/S0033291707000396. [DOI] [PubMed] [Google Scholar]
- Martin C. S., Chung T., Langenbucher J. W. How should we revise diagnostic criteria for substance use disorders in the DSM-V? Journal of Abnormal Psychology. 2008;117:561–575. doi: 10.1037/0021-843X.117.3.561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martin C. S., Steinley D. L., Vergés A., Sher K. J. The proposed 2/11 symptom algorithm for DSM-5 substance-use disorders is too lenient. Psychological Medicine. 2011;41:2008–2010. doi: 10.1017/S0033291711000717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martinez D., Kim J.-H., Krystal J., Abi-Dargham A. Imaging the neurochemistry of alcohol and substance abuse. Neuroimaging Clinics of North America. 2007;17:539–555. doi: 10.1016/j.nic.2007.07.004. [DOI] [PubMed] [Google Scholar]
- McBride O., Adamson G., Bunting B. P., McCann S. Characteristics of DSM-IV alcohol diagnostic orphans: Drinking patterns, physical illness, and negative life events. Drug and Alcohol Dependence. 2009;99:272–279. doi: 10.1016/j.drugalcdep.2008.08.008. [DOI] [PubMed] [Google Scholar]
- Meiklejohn J., Connor J., Kypri K. The effect of low survey response rates on estimates of alcohol consumption in a general population survey. PLoS ONE. 2012;7(4):e35527. doi: 10.1371/journal.pone.0035527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mewton L., Slade T., McBride O., Grove R., Teesson M. An evaluation of the proposed DSM-5 alcohol use disorder criteria using Australian national data. Addiction. 2011;106:941–950. doi: 10.1111/j.1360-0443.2010.03340.x. [DOI] [PubMed] [Google Scholar]
- Mewton L., Slade T., Teesson M. An evaluation of the proposed DSM-5 cannabis use disorder criteria using Australian national survey data. Journal of Studies on Alcohol and Drugs. 2013;74:614–621. doi: 10.15288/jsad.2013.74.614. [DOI] [PubMed] [Google Scholar]
- Meyer R. E. A commentary on ‘Addiction and dependence in DSM-V’. Addiction. 2011;106:873–874. doi: 10.1111/j.1360-0443.2010.03238.x. discussion 895–897. [DOI] [PubMed] [Google Scholar]
- Miller N. S., Goldsmith R. J. Craving for alcohol and drugs in animals and humans: Biology and behavior. Journal of Addictive Diseases. 2001;20:87–104. doi: 10.1300/J069v20n03_08. [DOI] [PubMed] [Google Scholar]
- Munafò M. R., Hitsman B. What’s the matter with cue-induced craving? A commentary on Perkins. Addiction. 2010;105:1860–1861. doi: 10.1111/j.1360-0443.2010.03127.x. [DOI] [PubMed] [Google Scholar]
- O’Brien C. P. Anticraving medications for relapse prevention: A possible new class of psychoactive medications. American Journal of Psychiatry. 2005;162:1423–1431. doi: 10.1176/appi.ajp.162.8.1423. [DOI] [PubMed] [Google Scholar]
- Peer K., Rennert L., Lynch K. G., Farrer L., Gelernter J., Kranzler H. R. Prevalence of DSM-IV and DSM-5 alcohol, cocaine, opioid, and cannabis use disorders in a largely substance dependent sample. Drug and Alcohol Dependence. 2013;127:215–219. doi: 10.1016/j.drugalcdep.2012.07.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perkins K. A. Does smoking cue-induced craving tell us anything important about nicotine dependence? Addiction. 2009;104:1610–1616. doi: 10.1111/j.1360-0443.2009.02550.x. [DOI] [PubMed] [Google Scholar]
- Poznyak V., Reed G. M., Clark N. Applying an international public health perspective to proposed changes for DSM-V. Addiction. 2011;106:868–870. doi: 10.1111/j.1360-0443.2011.03381.x. discussion 895–897. [DOI] [PubMed] [Google Scholar]
- Research Triangle Institute. SUDAAN language manual, Release 11.0. Research Triangle Park, NC: Author; 2012. [Google Scholar]
- Room R.2011Substance use disorders—a conceptual and terminological muddle Addiction 106879–882., discussion 895–897 [DOI] [PubMed] [Google Scholar]
- Rueter M. A., Chao W., Conger R. D. The effect of systematic variation in retrospective conduct disorder reports on antisocial personality disorder diagnoses. Journal of Consulting and Clinical Psychology. 2000;68:307–312. [PubMed] [Google Scholar]
- Saha T. D., Chou S. P., Grant B. F. Toward an alcohol use disorder continuum using item response theory: Results from the National Epidemiologic Survey on Alcohol and Related Conditions. Psychological Medicine. 2006;36:931–941. doi: 10.1017/S003329170600746X. [DOI] [PubMed] [Google Scholar]
- Saha T. D., Compton W. M., Chou S. P., Smith S., Ruan W. J., Huang B., Grant B. F. Analyses related to the development of DSM-5 criteria for substance use related disorders: 1. Toward amphetamine, cocaine and prescription drug use disorder continua using Item Response Theory. Drug and Alcohol Dependence. 2012;122:38–46. doi: 10.1016/j.drugalcdep.2011.09.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saha T. D., Compton W. M., Pulay A. J., Stinson F. S., Ruan W. J., Smith S. M., Grant B. F. Dimensionality of DSM-IV nicotine dependence in a national sample: An item response theory application. Drug and Alcohol Dependence. 2010;108:21–28. doi: 10.1016/j.drugalcdep.2009.11.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saha T. D., Grant B. F. Dimensionality and scale properties of DSM-5 alcohol use disorder [Abstract 0256] Alcoholism: Clinical and Experimental Research, 38, Supplement. 2014;S1:64A. [Google Scholar]
- Saha T. D., Stinson F. S., Grant B. F. The role of alcohol consumption in future classifications of alcohol use disorders. Drug and Alcohol Dependence. 2007;89:82–92. doi: 10.1016/j.drugalcdep.2006.12.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schuckit M. A., Smith T. L. A comparison of correlates of DSM-IV alcohol abuse or dependence among more than 400 sons of alcoholics and controls. Alcoholism: Clinical and Experimental Research. 2001;25:1–8. [PubMed] [Google Scholar]
- Schuckit M. A., Smith T. L., Landi N. A. The 5-year clinical course of high-functioning men with DSM-IV alcohol abuse or dependence. American Journal of Psychiatry. 2000;157:2028–2035. doi: 10.1176/appi.ajp.157.12.2028. [DOI] [PubMed] [Google Scholar]
- Shmulewitz D., Keyes K., Beseler C., Aharonovich E., Aivadyan C., Spivak B., Hasin D. The dimensionality of alcohol use disorders: Results from Israel. Drug and Alcohol Dependence. 2010;111:146–154. doi: 10.1016/j.drugalcdep.2010.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Slade T., Teesson M., Carragher N., Farrell M. Commentary on Agrawal et al. (2011): Assessing the impact of changes to diagnostic criteria on the estimated prevalence of alcohol use disorders in general population surveys. Addiction. 2011;106:1944–1945. doi: 10.1111/j.1360-0443.2011.03597.x. [DOI] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration. Results from the 2012 National Survey on Drug Use and Health: Summary of National Findings. Appendix B: Statistical methods and measurement (NSDUH Series H-46, HHS Publication No. SMA 13–4795) Rockville, MD: Author; 2013. Retrieved from http://www.samhsa.gov/data/nsduh/2012summnatfinddettables/nationalfindings/nsduhresults2012.htm#AppB. [Google Scholar]
- Teesson M., Lynskey M., Manor B., Baillie A. The structure of cannabis dependence in the community. Drug and Alcohol Dependence. 2002;68:255–262. doi: 10.1016/s0376-8716(02)00223-5. [DOI] [PubMed] [Google Scholar]
- Tiffany S. T., Wray J. M. The clinical significance of drug craving. Annals of the New York Academy of Sciences. 2012;1248:1–17. doi: 10.1111/j.1749-6632.2011.06298.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Uchtenhagen A. New and remaining problems with DSM-V. Addiction. 2011;106:888–889. doi: 10.1111/j.1360-0443.2010.03328.x. discussion 895–897. [DOI] [PubMed] [Google Scholar]
- Waters A. J., Shiffman S., Sayette M. A., Paty J. A., Gwaltney C. J., Balabanis M. H. Cue-provoked craving and nicotine replacement therapy in smoking cessation. Journal of Consulting and Clinical Psychology. 2004;72:1136–1143. doi: 10.1037/0022-006X.72.6.1136. [DOI] [PubMed] [Google Scholar]
- Winters K. C., Martin C. S., Chung T. Substance use disorders in DSM-V when applied to adolescents. Addiction. 2011;106:882–884. doi: 10.1111/j.1360-0443.2010.03334.x. discussion 895–897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10th revised ed, editor. World Health Organization. ICD-10: International statistical classification of diseases and related health problems. Geneva, Switzerland: Author; 1992. [Google Scholar]


