Abstract
Objective:
Spiritual health locus of control reflects a person’s beliefs about the role of a higher power in one’s health and can take an active or a passive perspective. The purpose of this study was to examine the moderating role of active and passive spiritual health locus of control beliefs on select health risk behaviors—alcohol use and smoking—in a national sample of African Americans.
Method:
A national U.S. probability sample of study participants (N = 2,370; 906 men; 1,464 women) completed a telephone survey assessing religious involvement, active and passive spiritual health locus of control beliefs, and alcohol consumption and smoking status. Because of previous research suggesting gender-specific associations among these variables, moderation analyses were conducted separately for men and women.
Results:
For women, higher religious behaviors were associated with less alcohol use, and this effect was more pronounced among those high in active spiritual health locus of control. For men, the combination of lower religious beliefs and higher passive spiritual health locus of control was associated with more alcohol consumption and more days of consuming five or more alcoholic drinks. No moderation effects were found for smoking.
Conclusions:
This study identified unique patterns of religious involvement and spiritual health locus of control beliefs that are associated with alcohol use, including heavy drinking, among African Americans. These findings have implications for pastoral counseling and other faith-based approaches for addressing heavy drinking in African Americans.
Spiritual health locus of control reflects the belief that a higher power (e.g., God) plays a role in one’s health (Debnam et al., 2012; Holt et al., 2003). The construct is a specialized form of general health locus of control, based on the multidimensional health locus of control work of Wallston and colleagues (1978), and originally derived from Rotter’s (1966) locus of control theory. The current spiritual health locus of control theoretical framework is based on a two-dimensional model, with an active and a passive dimension (Debnam et al., 2012; Holt et al., 2003). Active spiritual health locus of control involves the belief that God empowers individuals to take care of their health. This is similar to the collaborative religious coping style of working with God, as discussed by Pargament and colleagues (1988). Passive spiritual health locus of control involves a belief that one’s health is entirely up to God, with the role or responsibilities of the individual largely minimized. This is conceptually consistent with the deferring religious coping style (Pargament et al., 1988).
Spiritual health locus of control beliefs can play a positive or negative role in health. In previous research, passive spiritual health locus of control beliefs were associated with lower knowledge about mammography, breast cancer, breast cancer treatment, and mammography use in a sample of African American women (Holt et al., 2007). More recently, gender-specific analyses were conducted for African American men and women relating spiritual health locus of control beliefs with a variety of health-related behaviors (Debnam et al., 2012). Among African American women, passive spiritual health locus of control beliefs were negatively associated with daily vegetable servings. Among African American men, the same was true; in addition, passive spiritual health locus of control beliefs were positively associated with more days with five or more alcoholic beverages consumed and with the largest number of drinks consumed per month. In addition, active spiritual health locus of control beliefs were negatively associated with number of drinking days per month and average drinks consumed per month. These findings suggest a direct relationship between spiritual health locus of control and alcohol use among African American men. However, we do not know if there are more complex relationships at work, perhaps involving other aspects of religiosity.
In related research on religious coping, positive religious coping (e.g., seeking forgiveness, collaborative religious coping, spiritual support) is proposed to have a positive impact on health, and negative religious coping (e.g., spiritual discontent, seeing God as punishing, interpersonal religious discontent) is proposed to have a negative impact on health-related outcomes (Pargament et al., 1998). Positive religious coping is typically associated with good physical health outcomes (George et al., 2002; Koenig et al., 2012). Negative religious coping is related to the concept of “spiritual struggle” or “religious struggle” (Pargament et al., 2001, 2005) and has been associated with increased mortality (Pargament et al., 2001). Although less prevalent than positive religious coping beliefs (Pargament et al., 2001), spiritual struggle involves feeling punished by God, anger at God, or thoughts that evil forces may play a role in illness (Koenig et al., 1998). Religious struggle (as assessed by negative religious coping) has been associated with higher alcohol use in a community sample (Drerup et al., 2011). Gender differences in religious coping and health have been reported in college students, in which a negative relationship between religious coping and drinking was more pronounced among women (Daugherty & McLarty, 2003), and older women and those of a racial/ethnic minority background reported using religious coping to manage chronic pain to a greater degree than did older White men (Dunn & Horgas, 2004).
Religious involvement and health
We will use the term religious involvement to refer to “an organized system of [religious] beliefs, practices, rituals, and symbols” (Thoresen, 1998, p. 415). Religious involvement is widely recognized to be multidimensional (Hill & Pargament, 2003). Our religious involvement model includes a belief/private (e.g., presence of God in one’s life, perceiving a personal relationship with God) and a behavioral/public (e.g., religious service attendance, involvement in other religious activities) dimension (Roth et al., 2012). Use of a multidimensional model recognizes the possibility that different components (e.g., beliefs, behaviors, or public/private) of religious involvement may relate to outcomes differently. However, religious involvement often plays a positive role in health-related outcomes (Koenig et al., 2001, 2012), particularly for those who are highly involved (Ellison et al., 2010), such as African Americans (Levin et al., 1994; Taylor et al., 1996).
Religious involvement, smoking, and alcohol use in African Americans.
Religious involvement has shown previous associations with smoking and alcohol use in African Americans. In a sample of students attending a historically Black university, low religious well-being and limited relationship with God were associated with increased odds of smoking and heavy alcohol use (Turner-Musa & Lipscomb, 2007). Among African American women, being of Pentecostal affiliation was associated with lower odds of being a current smoker and higher odds of quitting smoking than being affiliated with another denomination; however, there was no relationship with degree of religiosity (Brown et al., 1994). In a community sample of African American men, no or low frequency of church attendance was associated with current smoking and daily drinking (Brown & Gary, 1994).
Examining a longitudinal cohort from age 6 to 32, Bowie and colleagues (2006) reported that major depression, low education, unemployment, frequent relocations, and not attending religious services were associated with problem alcohol use in African Americans. Moreover, attending church service played a positive, or buffering, role in the relationship between depression and alcohol use. Other measures of religiosity were not associated with alcohol problems. Alcohol use problems for depressed participants were lower for frequent church attenders, and, although this effect was true for both men and women, it was stronger among men.
An investigation of ethnic identity and drinking behaviour revealed that, among a national sample of African Americans, ethnic identity was negatively associated with alcohol consumption (Herd & Grube, 1996). This was the case for one aspect of ethnic identity involving participation in “black social networks” (e.g., church, friends, neighborhood). The authors concluded that this is attributable to norms around abstinence and social control of drinking in African American communities.
Locus of control as a moderator.
Given the salience of control constructs in religion–health research (Hayward & Krause, 2013; Holt et al., 2013), it is plausible that spiritual health locus of control will play a moderating role with religious involvement dimensions as related to health behaviors. This is an idea untested in previous research. Different orientations comprising religious involvement interacting with spiritual health locus of control beliefs may be associated, based on theory, with value-laden lifestyle behaviors in accord with religious proscriptions such as those against alcohol and tobacco use. General locus of control has been found to act in an interactive (moderator) fashion with other psychosocial variables in health-related research (Liang & Bogat, 1994; Solomon et al., 1988; Vander Zee et al., 1997; Voils et al., 2005), but there is no previous research on spiritual health locus of control as a moderating influence in health-related research or on health behaviors. There is also little known about gender differences in these potential relationships.
Present study
The purpose of the present study was to examine the interaction of religious involvement and spiritual health locus of control in association with alcohol consumption and smoking status for a national sample of African Americans. Heavy drinking and tobacco use are two important health risk behaviors in the development of the top chronic diseases and causes of death among African Americans, such as heart disease, cancer, stroke, diabetes, and unintentional injuries (Centers for Disease Control and Prevention, 2014). Even when African Americans smoke about as many cigarettes as Whites do, they are at increased risk for lung cancer (Ries et al., 2009). Although African American women smoke less than White women, their rates of lung cancer are similar (American Lung Association, 2010). Although Whites have higher rates of alcohol use than African Americans, once dependence occurs African Americans have greater rates of recurrence or persistent dependence than Whites (Chartier & Caetano, 2010). African Americans are also more likely than Whites to report social consequences from their drinking (Mulia et al., 2009). More specifically, African Americans show lower levels of alcohol-related problems in younger adulthood but higher levels by their mid-thirties (Muthén & Muthén, 2000; Wagner et al., 2002). In addition, African Americans are more likely than Whites to develop liver disease (Flores et al., 2008).
Based on previous research on the role of religious involvement in health-related outcomes (Koenig et al., 2001, 2012; Turner-Musa & Lipscomb, 2007), we hypothesized that religious beliefs/behaviors would be negatively associated with alcohol consumption and smoking status. Consistent with previous theory in spiritual health locus of control (Holt et al., 2003) and religious coping (Pargament et al., 1998), we expected that this association would be attenuated in persons with high active spiritual health locus of control and amplified in persons with high passive spiritual health locus of control. This study used data from our Religion and Health in African Americans (RHIAA) study (Holt et al., 2014). This is a national telephone survey of African American households, designed to examine the nature of and reasons for the religion–health connection. Given the differential patterns of religious involvement between men and women (Levin et al., 1994) and previous findings from the RHIAA study suggesting gender differences in the relationships between spiritual health locus of control and alcohol consumption (Debnam et al., 2012), the religious involvement–spiritual health locus of control moderation effects were examined separately for men and women in the present analyses. Other research has suggested gender differences in the role of religious involvement in alcohol use in African Americans (Bowie et al., 2006). Findings around gender differences could have implications for health promotion interventions, particularly given that African American men remain one of the most medically underserved and understudied groups (Elder et al., 2014). It is important to gain insights on the role of religion in the health of African Americans (Ellison et al., 2010) and to apply these insights to health-promotion interventions in this often-overlooked group.
Method
Telephone survey methods
Data-collection methods for the RHIAA study have been previously reported (Holt et al., 2014). A sampling firm used probability-based methods to develop a call list of households from the 50 U.S. states. This information was derived from publicly available data such as motor vehicle records. Professional interviewers randomly dialed telephone numbers from the call list and introduced the project to the first adult who lived at the household being dialed. If that adult indicated interest, the interviewers screened him or her for eligibility, including being a self-identified African American age 21 or older, with no cancer history. Cancer diagnosis served as an exclusion criterion for other RHIAA analyses that included cancer screening behaviors. Those who were interested and eligible heard an informed consent script, provided verbal assent, and completed the 45-minute interview. Only one individual per household could complete the interview. Participants received a $25 gift card by mail as a token of appreciation. The study protocol was approved by the University of Alabama at Birmingham and University of Maryland Institutional Review Boards.
Measures
Religious involvement.
A validated Religiosity Scale previously used with African Americans was used to assess religious beliefs (e.g., presence of God in one’s life, perceiving a personal relationship with God) and behaviors (e.g., church service attendance, involvement in other church activities) (Lukwago et al., 2001). Items were assessed in a 5-point Likert-type format, with the exception of two monthly service attendance items that were assessed in a 3-point format (0, 1–3, ≥4). Scores range from 4 to 20 for beliefs and 5 to 21 for behaviors, with higher scores indicating higher religious involvement. The internal reliability of the beliefs (α = .89) and behaviors (α = .73) subscales was reasonable to high in this sample.
Spiritual health locus of control.
The Spiritual Health Locus of Control Scale is a 13-item instrument that includes two dimensions of these beliefs (Holt et al., 2003). It was developed for use with African American populations. The active spiritual subscale (11 items; range: 11–55) reflects the belief that a higher being empowers a person to be proactive about health behaviors and that one works in partnership with God to stay in good health (e.g., “Even though I trust that God will take care of me, I still need to take care of myself”; α = .90 in the current sample). The passive spiritual subscale (two items; range: 2–10) assesses the belief that because a higher power has control over one’s health, the individual does not have to engage in healthy behaviors (e.g., “There is no point in taking care of myself when it’s all up to God anyway”; r = .59 in the current sample). The items use a 5-point Likert-type format (strongly disagree, disagree, neutral, agree, and strongly agree). The two-factor structure was supported in previous research, and evidence has been provided for the predictive validity of the instrument (Holt et al., 2003).
Alcohol consumption and smoking status.
Alcohol consumption was assessed using items from the Behavioral Risk Factor Surveillance System (BRFSS). This established interview is administered nationally, including with the study population. The BRFSS has demonstrated adequate test–retest reliability over a 21-day period among African Americans (Stein et al., 1993). The alcohol consumption section includes an initial item asking about any alcohol use during the previous 30 days. Those who indicated “yes” were asked items assessing heavy drinking (“Considering all types of alcoholic beverages, how many times during the past 30 days did you have 4 [for women] /5 [for men] or more drinks on an occasion?” “During the past 30 days, what is the largest number of drinks you had on any occasion?”). Regarding smoking status, participants were asked whether they smoke every day, some days, or not at all. Those who answered every day or some days were classified as current smokers.
Demographics.
A series of demographic items assessed participant characteristics such as gender, age, educational attainment, self-rated health status, relationship status, work status, and household income before taxes (response categories listed in Table 1).
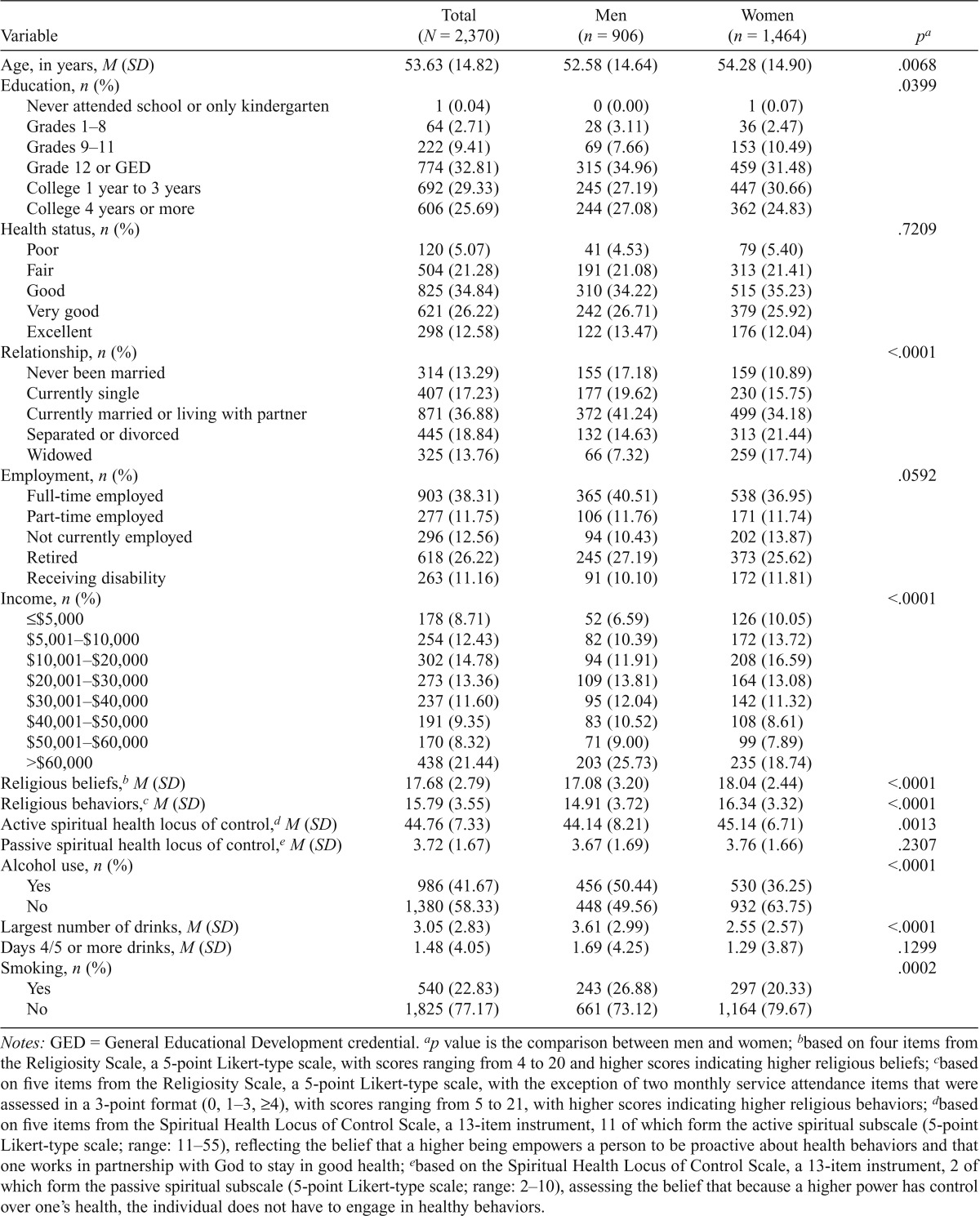
Table 1.
Descriptive data and comparisons by gender
| Variable | Total (N = 2,370) | Men (n = 906) | Women (n = 1,464) | pa |
| Age, in years, M (SD) | 53.63 (14.82) | 52.58 (14.64) | 54.28 (14.90) | .0068 |
| Education, n (%) | .0399 | |||
| Never attended school or only kindergarten | 1 (0.04) | 0 (0.00) | 1 (0.07) | |
| Grades 1–8 | 64 (2.71) | 28 (3.11) | 36 (2.47) | |
| Grades 9–11 | 222 (9.41) | 69 (7.66) | 153 (10.49) | |
| Grade 12 or GED | 774 (32.81) | 315 (34.96) | 459 (31.48) | |
| College 1 year to 3 years | 692 (29.33) | 245 (27.19) | 447 (30.66) | |
| College 4 years or more | 606 (25.69) | 244 (27.08) | 362 (24.83) | |
| Health status, n (%) | .7209 | |||
| Poor | 120 (5.07) | 41 (4.53) | 79 (5.40) | |
| Fair | 504 (21.28) | 191 (21.08) | 313 (21.41) | |
| Good | 825 (34.84) | 310 (34.22) | 515 (35.23) | |
| Very good | 621 (26.22) | 242 (26.71) | 379 (25.92) | |
| Excellent | 298 (12.58) | 122 (13.47) | 176 (12.04) | |
| Relationship, n (%) | <.0001 | |||
| Never been married | 314 (13.29) | 155 (17.18) | 159 (10.89) | |
| Currently single | 407 (17.23) | 177 (19.62) | 230 (15.75) | |
| Currently married or living with partner | 871 (36.88) | 372 (41.24) | 499 (34.18) | |
| Separated or divorced | 445 (18.84) | 132 (14.63) | 313 (21.44) | |
| Widowed | 325 (13.76) | 66 (7.32) | 259 (17.74) | |
| Employment, n (%) | .0592 | |||
| Full-time employed | 903 (38.31) | 365 (40.51) | 538 (36.95) | |
| Part-time employed | 277 (11.75) | 106 (11.76) | 171 (11.74) | |
| Not currently employed | 296 (12.56) | 94 (10.43) | 202 (13.87) | |
| Retired | 618 (26.22) | 245 (27.19) | 373 (25.62) | |
| Receiving disability | 263 (11.16) | 91 (10.10) | 172 (11.81) | |
| Income, n (%) | <.0001 | |||
| ≤$5,000 | 178 (8.71) | 52 (6.59) | 126 (10.05) | |
| $5,001–$10,000 | 254 (12.43) | 82 (10.39) | 172 (13.72) | |
| $10,001–$20,000 | 302 (14.78) | 94 (11.91) | 208 (16.59) | |
| $20,001–$30,000 | 273 (13.36) | 109 (13.81) | 164 (13.08) | |
| $30,001–$40,000 | 237 (11.60) | 95 (12.04) | 142 (11.32) | |
| $40,001–$50,000 | 191 (9.35) | 83 (10.52) | 108 (8.61) | |
| $50,001–$60,000 | 170 (8.32) | 71 (9.00) | 99 (7.89) | |
| >$60,000 | 438 (21.44) | 203 (25.73) | 235 (18.74) | |
| Religious beliefs,b M (SD) | 17.68 (2.79) | 17.08 (3.20) | 18.04 (2.44) | <.0001 |
| Religious behaviors,c M (SD) | 15.79 (3.55) | 14.91 (3.72) | 16.34 (3.32) | <.0001 |
| Active spiritual health locus of control,d M (SD) | 44.76 (7.33) | 44.14 (8.21) | 45.14 (6.71) | .0013 |
| Passive spiritual health locus of control,e M (SD) | 3.72 (1.67) | 3.67 (1.69) | 3.76 (1.66) | .2307 |
| Alcohol use, n (%) | <.0001 | |||
| Yes | 986 (41.67) | 456 (50.44) | 530 (36.25) | |
| No | 1,380 (58.33) | 448 (49.56) | 932 (63.75) | |
| Largest number of drinks, M (SD) | 3.05 (2.83) | 3.61 (2.99) | 2.55 (2.57) | <.0001 |
| Days 4/5 or more drinks, M (SD) | 1.48 (4.05) | 1.69 (4.25) | 1.29 (3.87) | .1299 |
| Smoking, n (%) | .0002 | |||
| Yes | 540 (22.83) | 243 (26.88) | 297 (20.33) | |
| No | 1,825 (77.17) | 661 (73.12) | 1,164 (79.67) |
Notes: GED = General Educational Development credential.
p value is the comparison between men and women;
based on four items from the Religiosity Scale, a 5-point Likert-type scale, with scores ranging from 4 to 20 and higher scores indicating higher religious beliefs;
based on five items from the Religiosity Scale, a 5-point Likert-type scale, with the exception of two monthly service attendance items that were assessed in a 3-point format (0, 1–3, ≥4), with scores ranging from 5 to 21, with higher scores indicating higher religious behaviors;
based on five items from the Spiritual Health Locus of Control Scale, a 13-item instrument, 11 of which form the active spiritual subscale (5-point Likert-type scale; range: 11–55), reflecting the belief that a higher being empowers a person to be proactive about health behaviors and that one works in partnership with God to stay in good health;
based on the Spiritual Health Locus of Control Scale, a 13-item instrument, 2 of which form the passive spiritual subscale (5-point Likert-type scale; range: 2–10), assessing the belief that because a higher power has control over one’s health, the individual does not have to engage in healthy behaviors.
Statistical methods
All analyses were conducted using SAS Version 9.3 (SAS Institute Inc., Cary, NC). The dichotomous outcomes of any alcohol use in the past 30 days and current smoking status were assessed using binary logistic regression analyses. For the subset of participants who indicated some alcohol use, ordinary linear regression models were used to examine the largest number of drinks consumed and the number of days in the past month where four or more (for women) or five or more (for men) drinks were consumed. All analyses included three covariates (age, education, health status), four main effects (religious beliefs, religious behaviors, active spiritual health locus of control, passive spiritual health locus of control), and four two-way interactions among the main effects (religious beliefs by active control, religious beliefs by passive control, religious behaviors by active control, religious behaviors by passive control). Before the analysis, the main effect terms were standardized into z scores by subtracting the overall mean and dividing by the standard deviation. The multiplicative interaction terms then comprised the products of the z scores. As mentioned previously, separate analytic models were executed for women and for men.
Results
Interviewers contacted 12,418 households, and 2,370 individuals completed the telephone interview. The overall response rate was calculated as accepted / [accepted + noninterviewed], and was 19%. Of those who were contacted but did not participate (N = 10,048), 8,240 refused before eligibility could be assessed, and 1,658 were not eligible (81 were younger than 21 years of age, 444 did not provide an age for eligibility screening, 878 did not self-report as African American, 224 reported a history of cancer, and 5 refused to respond to the cancer history question). Twenty-six people were not capable of participating. Only 150 were eligible but refused, resulting in an upper bound response rate of 94% (2,370 / 2,520). The upper bound response rate is the most liberal and includes only refusals, terminations, and completions (Centers for Disease Control and Prevention, 1998).
Descriptive analysis
Participant demographic characteristics are reported in Table 1. Men and women differed in education, with men being more likely to have had 4 or more years of college than women. Men were more likely than women to have never been married, to be currently single, or to be living with a partner, whereas women were more likely to be separated or divorced. Men earned more money than women. Women reported higher religious beliefs and behaviors than did men. Women had higher active spiritual health locus of control beliefs than men; however, there were no differences in passive spiritual health locus of control beliefs. Men were more likely than women to report alcohol use in the past 30 days and had higher scores on the largest number of drinks per drinking day. Last, men were more likely than women to report being a current smoker.
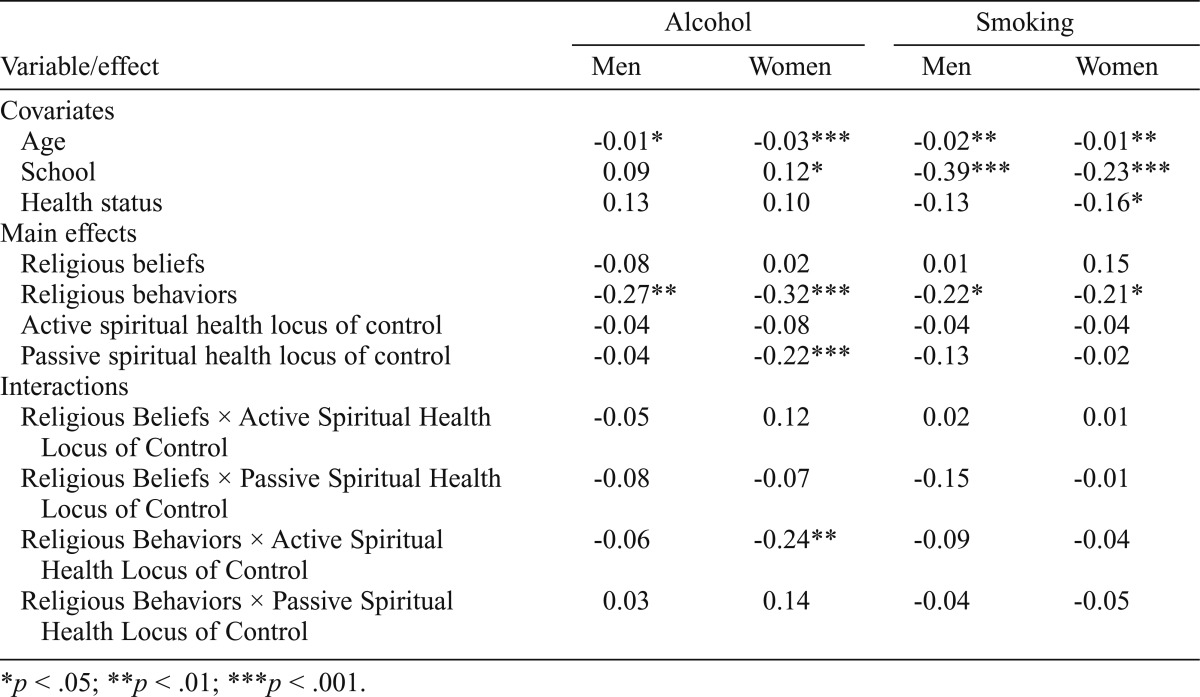
Any alcohol use and smoking
The results of the binary logistic regression analyses for any alcohol use in the past 30 days and current smoking status are summarized in Table 2. For both men and women, main effects for religious behaviors were found such that higher religious behaviors were associated with reduced odds of alcohol use in the past 30 days and with reduced odds of current smoking (all ps < .05). The covariate-adjusted main effects for religious beliefs were not statistically significant. Exponentiating the estimates in Table 2 yields the associated odds ratios for each effect. For example, for the effect of religious behaviors on any alcohol use among the men, an odds ratio of 0.76 is obtained from the estimate of -0.27 (e-0.27 = 0.76). This means that, for every standard deviation increase in religious behaviors for men, the odds of alcohol use decrease by 24% [(1 – 0.76) × 100]. For women, the corresponding odds ratio is 0.73, or a 27% reduction per standard deviation increase. There were no active spiritual health locus of control main effects on any alcohol consumption or smoking, but passive spiritual health locus of control was negatively associated with odds of alcohol use in the past 30 days for women only (p < .001).
Table 2.
Estimates from binary logistic regression analyses for any alcohol use and smoking
| Variable/effect | Alcohol |
Smoking |
||
| Men | Women | Men | Women | |
| Covariates | ||||
| Age | -0.01* | -0.03*** | -0.02** | -0.01** |
| School | 0.09 | 0.12* | -0.39*** | -0.23*** |
| Health status | 0.13 | 0.10 | -0.13 | -0.16* |
| Main effects | ||||
| Religious beliefs | -0.08 | 0.02 | 0.01 | 0.15 |
| Religious behaviors | -0.27** | -0.32*** | -0.22* | -0.21* |
| Active spiritual health locus of control | -0.04 | -0.08 | -0.04 | -0.04 |
| Passive spiritual health locus of control | -0.04 | -0.22*** | -0.13 | -0.02 |
| Interactions | ||||
| Religious Beliefs × Active Spiritual Health Locus of Control | -0.05 | 0.12 | 0.02 | 0.01 |
| Religious Beliefs × Passive Spiritual Health Locus of Control | -0.08 | -0.07 | -0.15 | -0.01 |
| Religious Behaviors × Active Spiritual Health Locus of Control | -0.06 | -0.24** | -0.09 | -0.04 |
| Religious Behaviors × Passive Spiritual Health Locus of Control | 0.03 | 0.14 | -0.04 | -0.05 |
p < .05;
p < .01;
p < .001.
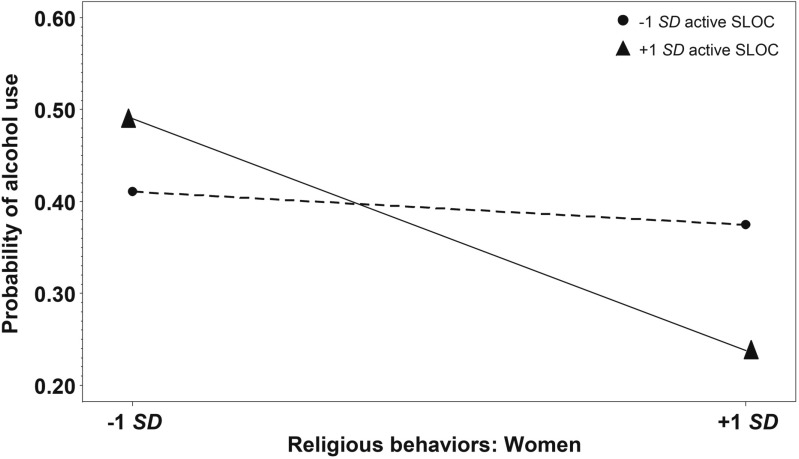
The interaction analyses summarized in Table 2 indicated no significant moderator effects for men. For women, as expected, the religious behaviors by active spiritual health locus of control interaction was statistically significant (p < .01). The predicted probabilities of alcohol use for women are displayed in Figure 1 and aid in the interpretation of this interaction effect. High religious behaviors were associated with lower odds of alcohol use, and this effect was statistically more pronounced for those high in active spiritual health locus of control.
Figure 1.
Effect of interaction between religious behaviors and active spiritual health locus of control on probability of alcohol use among women. SLOC = spiritual health locus of control.
Excessive alcohol consumption
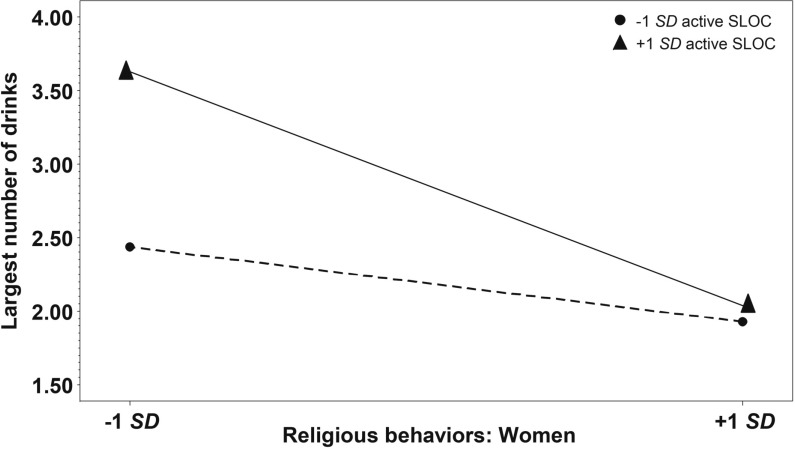
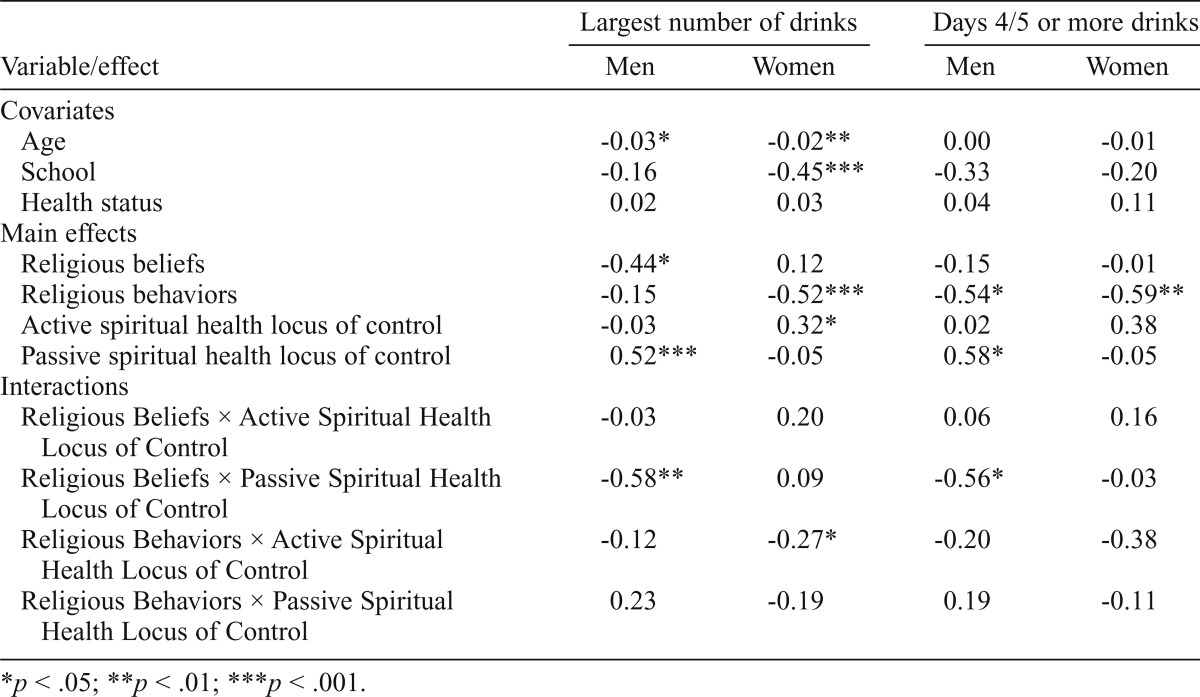
The results of the linear regression analyses for excessive alcohol use among the subsets of participants who reported any alcohol use are summarized in Table 3. In these analyses, the main effects for religious involvement and spiritual health locus of control must be interpreted in the context of their significant interaction effects, which were observed to be different for men and women. For men, as expected, religious beliefs by passive spiritual health locus of control interaction was statistically significant for both measures of excessive drinking (ps < .05). The effects were similar across both measures and are illustrated graphically in Figure 2 for the largest number of drinks consumed. It can be seen from this figure of model-predicted outcome values that African American men who were both low on religious beliefs and high on passive spiritual health locus of control reported more excessive drinking than other combinations on these predictors. For women, the religious behavior by active spiritual health locus of control interaction was statistically significant for the largest number of drinks (p = .04) and approached significance for the number of days with excessive drinking (p = .06). Figure 3 displays the model-predicted values for largest number of drinks and illustrates that women who were both low on religious behaviors and high on active spiritual health locus of control reported more excessive drinking.
Table 3.
Estimates from ordinary least squares regression analyses for heavy drinking
| Variable/effect | Largest number of drinks |
Days 4/5 or more drinks |
||
| Men | Women | Men | Women | |
| Covariates | ||||
| Age | -0.03* | -0.02** | 0.00 | -0.01 |
| School | -0.16 | -0.45*** | -0.33 | -0.20 |
| Health status | 0.02 | 0.03 | 0.04 | 0.11 |
| Main effects | ||||
| Religious beliefs | -0.44* | 0.12 | -0.15 | -0.01 |
| Religious behaviors | -0.15 | -0.52*** | -0.54* | -0.59** |
| Active spiritual health locus of control | -0.03 | 0.32* | 0.02 | 0.38 |
| Passive spiritual health locus of control | 0.52*** | -0.05 | 0.58* | -0.05 |
| Interactions | ||||
| Religious Beliefs × Active Spiritual Health Locus of Control | -0.03 | 0.20 | 0.06 | 0.16 |
| Religious Beliefs × Passive Spiritual Health Locus of Control | -0.58** | 0.09 | -0.56* | -0.03 |
| Religious Behaviors × Active Spiritual Health Locus of Control | -0.12 | -0.27* | -0.20 | -0.38 |
| Religious Behaviors × Passive Spiritual Health Locus of Control | 0.23 | -0.19 | 0.19 | -0.11 |
p < .05;
p < .01;
p < .001.
Figure 2.
Effect of interaction between religious beliefs and passive spiritual health locus of control on largest number of drinks among men. SLOC = spiritual health locus of control.
Figure 3.
Effect of interaction between religious behaviors and active spiritual health locus of control on largest number of drinks among women. SLOC = spiritual health locus of control.
Discussion
The current study identified unique patterns of religious involvement and spiritual health locus of control beliefs that are associated with alcohol use, including heavy drinking, among a national sample of African Americans. Interactions between religious involvement and spiritual health locus of control beliefs were identified as being different for men and women. The current findings support the positive and negative role that faith beliefs can play in one’s health and highlight gender-specific differences. They are also consistent with previous research that has identified relationships between spiritual health locus of control and health behaviors (Debnam et al., 2012; Holt et al., 2003; Kinney et al., 2002). The focus on African Americans increases the significance in light of the health disparities that affect this population, which suffers a greater burden of chronic disease than other populations in the United States.
The importance of faith communities for African American women
The current findings suggested that, for African American women, the combination of high religious behaviors and holding active spiritual health locus of control beliefs were associated with having lower odds of alcohol consumption in the prior 30 days. This combination suggests a synergistic effect, where active spiritual health locus of control beliefs play a particularly strong protective role against alcohol consumption for church-attending African American women. However, for African American women who use some alcohol and who are not active in faith communities, or those low in religious behaviors, the interaction with active spiritual health locus of control beliefs is very different. For these women, holding active spiritual health locus of control beliefs is positively associated with both study measures of heavy drinking. Taken together, these three interactions suggest a highly important role of the social environment of the church for African American women. This is not surprising, given that, although faith-based organizations provide African American men with leadership opportunities (Taylor et al., 2004), church attendance is greater among African American women than among their male counterparts (Levin et al., 1994). It is intriguing that active spiritual health locus of control beliefs would react in a positive way for African American women high in religious behaviors but in a negative way for African American women low in religious behaviors. Apparently holding these beliefs, in the absence of the religious support offered by a faith community, is not adaptive, at least not with regard to alcohol consumption.
Previous research has suggested the importance of religious social support in health-related outcomes, especially for African Americans (Ellison et al., 2010). For example, in national samples of African Americans, religious support mediated the relationship between religious behaviors and emotional functioning and depressive symptoms in African Americans (Holt et al., 2013), and in another sample the impact of religiosity on distress was mediated by congregational support (Jang & Johnson, 2004). With regard to the interaction with active spiritual health locus of control, perhaps without the grounding and support provided by a religious community, African American women are using active spiritual health locus of control beliefs as a mechanism for coping with stress (Pargament et al., 1998) or life events, along with heavy alcohol use. The current findings, at least among women, are supportive of a previous examination of the role of ethnic identity in alcohol use among African Americans, suggesting that participation in African American social networks is associated with lower use (Herd & Grube, 1996). This situation is consistent with the idea that African American women are more likely than their male counterparts to be engaged in faith communities, and therefore are more likely to receive this protective effect.
Spiritual struggle may put African American men at risk
The gender-stratified analyses suggest that some African American men appear to be experiencing a religious manifestation similar to spiritual struggle, involving lower religious beliefs and higher passive spiritual health locus of control. This combination is associated with heavy, and potentially problem, drinking. Spiritual struggle has been previously defined by concepts such as negative religious coping or beliefs such as abandonment by God or feeling that God has punished a person for sin or lack of belief (Pargament et al., 2005). Given the significant gap in the literature around health among men of color, these findings have important implications for health promotion among African American men. This same pattern was not evidenced among women, perhaps because women are more connected in their faith community through religious participation, or maybe because of gender differences in social acceptability of heavy drinking.
The smoking interactions were not significant for either men or women, suggesting that smoking behavior is not connected in the same way to these religious patterns as is alcohol use. This finding may be because of differences in religious proscriptions around health risk behaviors or because people engage in these behaviors for different reasons (e.g., stress, coping, socially).
Bowie and colleagues (2006) reported that alcohol use problems for depressed participants were lower for frequent church attenders, but that the effect, although significant for both men and women, was stronger for men than for women. This finding is somewhat different from the current pattern of religious behaviors playing an important role in alcohol use for women and religious beliefs playing a prominent role for men. Perhaps the difference in findings may be attributable to examination of the role of depression in the previous sample.
Limitations
There are some important limitations that should be taken into account when considering the current findings. First, as with any survey research method, the use of telephone interviews conveys a particular type of bias, and the overall response rate was low, which may manifest itself in the sample characteristics. Relative to the U.S. Black population, the current sample is older than the U.S. median age of 32.7 years (current sample median = 54.0); contains fewer men (current = 38.2%; U.S. = 47.7% men); is more educated (current % attended ≥4 years of college = 26%; U.S. = 18.4%) (United States Census Bureau, 2011); and is as likely to report attending religious services at least once per week (current = 50.6%; U.S. = 53%) (Pew Research Center, 2009).
Second, although there are a number of important lifestyle behaviors involved in chronic disease control, the current analysis focused on alcohol consumption and smoking. The instruments used to assess these constructs, although widely recognized and validated, were brief in nature and do not capture deeper nuances in these behaviors. Third, the passive spiritual health locus of control subscale contained only two items, and the correlation between them was modest. That these items produced significant associations with study outcomes in this and previous research suggests that this construct is robust and holds promise for future development.
Fourth, that the religious beliefs dimension of the religious involvement scale and spiritual health locus of control both reflect a type of religious-oriented belief may lead to the question of independence of constructs. However, the religious beliefs dimension reflects private religiosity and a personal relationship with God/higher power, whereas spiritual health locus of control is a specialized form of the original health locus of control construct (Wallston et al., 1999) and is based on Rotter’s expectancy-value theory (1966). The correlations between the constructs were small to moderate (r = .49 for active; r = -.04 for passive), indicating sufficient distinctiveness.
Fifth, we recognize that African Americans are not a homogeneous group. The current study was not designed to examine factors such as geographic region or other subgroup differences that could play an important role in these relationships. Last, we cannot draw conclusions about causality with the present cross-sectional data. A multiple-wave analysis would strengthen the current model and is something on which the RHIAA team is currently working as a next step.
Implications and future research
Overall, these findings support the importance of examining the role of religiously based beliefs, particularly spiritual health locus of control, when considering health risk behaviors among African American men and women. Future studies should be conducted in other demographic groups to assess these relationships. Findings have implications for pastoral counseling around negative religious beliefs and spiritual struggle, in the context of faith-based alcohol overuse programs. For example, African American women may be encouraged to activate faith-based support networks, which may provide a protective effect against heavy drinking, in conjunction with active spiritual health locus of control beliefs. Church-based health ministry activities around healthy lifestyle and stress reduction can be helpful here, particularly if they use evidence-based interventions. The “SISTAS” group-based alcohol misuse prevention intervention that incorporates both racial identity and spirituality could be used in such a context (McCurtis Witherspoon & Williams Richardson, 2006). “Bridges to Community” is a faith-based intervention for African American women dependent on cocaine (Stahler et al., 2005, 2007). Bridges uses the church as a sustainable social network with supportive mentors who help recovering women to maintain abstinence following treatment. Results from two evaluations were promising (Stahler et al., 2005, 2007). Such an intervention strategy could be adapted for alcohol use disorder treatment for African American women.
For African American men, alcohol-related counselling may attempt to address issues related to spiritual struggle and empower a personal role and responsibility in men’s health. However, with limited previous focus on religiously based interventions among men of color, there is much more to learn about whether this approach would be optimal and what strategies would be most effective for reaching this often-underserved group. This is an important area among men of color, given that they are consuming alcohol at rates higher than women, engaged in faith communities at rates lower than women, may be disengaged from healthcare systems, and suffer a high burden of chronic disease. The current study demonstrates the importance of examining the complex relationships between religious beliefs and behaviors, spiritual health locus of control beliefs, and gender in understanding alcohol use in African American communities.
Acknowledgments
The team acknowledges the work of OpinionAmerica (www.opinionamericagroup.com), which conducted participant recruitment and data collection activities for the present study.
Footnotes
This work was supported by National Cancer Institute Grant 1 R01 CA105202 and was approved by the University of Maryland Institutional Review Board (#08-0328).
References
- Ahmed F., Brown D. R., Gary L. E., Saadatmand F. Religious predictors of cigarette smoking: Findings for African American women of childbearing age. Behavioral Medicine. 1994;20:34–43. doi: 10.1080/08964289.1994.9934614. [DOI] [PubMed] [Google Scholar]
- American Lung Association 2010African Americans and tobaccoRetrieved from http://www.lung.org/stop-smoking/about-smoking/factsfigures/african-americans-and-tobacco.html
- Bowie J. V., Ensminger M. E., Robertson J. A. Alcohol-use problems in young black adults: Effects of religiosity, social resources, and mental health. Journal of Studies on Alcohol. 2006;67:44–53. doi: 10.15288/jsa.2006.67.44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown D. R., Gary L. E. Religious involvement and health status among African-American males. Journal of the National Medical Association. 1994;86:825–831. [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. 1995 BRFSS Summary quality control report. 1998, January 6 Retrieved from www.cdc.gov/brfss/rtf/1995SummaryDataQualityReport.rtf.
- Centers for Disease Control and Prevention. Minority health: Black or African American populations. 2014, February 10 Retrieved from http://www.cdc.gov/minorityhealth/populations/remp/black.html.
- Chartier K., Caetano R. Ethnicity and health disparities in alcohol research. Alcohol Research & Health. 2010;33:152–160. [PMC free article] [PubMed] [Google Scholar]
- Daugherty T. K., McLarty L. M. Religious coping, drinking motivation, and sex. Psychological Reports. 2003;92:643–647. doi: 10.2466/pr0.2003.92.2.643. [DOI] [PubMed] [Google Scholar]
- Debnam K. J., Holt C. L., Clark E. M., Roth D. L., Foushee H. R., Crowther M., Southward P. L. Spiritual health locus of control and health behaviors in African Americans. American Journal of Health Behavior. 2012;36:360–372. doi: 10.5993/AJHB.36.3.7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Drerup M. L., Johnson T. J., Bindl S. Mediators of the relationship between religiousness/spirituality and alcohol problems in an adult community sample. Addictive Behaviors. 2011;36:1317–1320. doi: 10.1016/j.addbeh.2011.07.013. [DOI] [PubMed] [Google Scholar]
- Dunn K. S., Horgas A. L. Religious and nonreligious coping in older adults experiencing chronic pain. Pain Management Nursing. 2004;5:19–28. doi: 10.1016/s1524-9042(03)00070-5. [DOI] [PubMed] [Google Scholar]
- Elder K., Meret-Hanke L., Dean C., Wiltshire J., Gilbert K. L., Wang J., Moore T. How do African American men rate their health care? An analysis of the consumer assessment of health plans 2003-2006. American Journal of Men’s Health. Advance online publication. 2014, April 30 doi: 10.1177/1557988314532824. [DOI] [PubMed] [Google Scholar]
- Ellison C. G., Hummer R. A., Burdette A. M., Benjamins M. R. Race, religious involvement, and health: The case of African Americans. In: Ellison C. G., Hummer R. A., editors. Religion, families, and health: Population-based research in the United States. New Brunswick, NJ: Rutgers University Press; 2010. pp. 321–48. [Google Scholar]
- Flores Y. N., Yee H. F., Jr., Leng M., Escarce J. J., Bastani R., Salmerón J., Morales L. S. Risk factors for chronic liver disease in Blacks, Mexican Americans, and Whites in the United States: Results from NHANES IV, 1999-2004. American Journal of Gastroenterology. 2008;103:2231–2238. doi: 10.1111/j.1572-0241.2008.02022.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- George L. K., Ellison C. G., Larson D. B. Explaining the relationships between religious involvement and health. Psychological Inquiry: An International Journal for the Advancement of Psychological Theory. 2002;13:190–200. [Google Scholar]
- Hayward R. D., Krause N. Trajectories of late-life change in God-mediated control. The Journals of Gerontology Series B: Psychological Sciences and Social Sciences. 2013;68:49–58. doi: 10.1093/geronb/gbs054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Herd D., Grube J. Black identity and drinking in the US: A national study. Addiction. 1996;91:845–857. doi: 10.1046/j.1360-0443.1996.91684510.x. [DOI] [PubMed] [Google Scholar]
- Hill P. C., Pargament K. I. Advances in the conceptualization and measurement of religion and spirituality. Implications for physical and mental health research. The American Psychologist. 2003;58:64–74. doi: 10.1037/0003-066x.58.1.64. [DOI] [PubMed] [Google Scholar]
- Holt C. L., Clark E. M., Klem P. R. Expansion and validation of the spiritual health locus of control scale: Factorial analysis and predictive validity. Journal of Health Psychology. 2007;12:597–612. doi: 10.1177/1359105307078166. [DOI] [PubMed] [Google Scholar]
- Holt C. L., Clark E. M., Kreuter M. W., Rubio D. M. Spiritual health locus of control and breast cancer beliefs among urban African American women. Health Psychology. 2003;22:294–299. doi: 10.1037/0278-6133.22.3.294. [DOI] [PubMed] [Google Scholar]
- Holt C. L., Roth D. L., Clark E. M., Debnam K. Positive self-perceptions as a mediator of religious involvement and health behaviors in a national sample of African Americans. Journal of Behavioral Medicine. 2014;37:102–112. doi: 10.1007/s10865-012-9472-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holt C. L., Wang M. Q., Clark E. M., Williams B. R., Schulz E. Religious involvement and physical and emotional functioning among African Americans: The mediating role of religious support. Psychology & Health. 2013;28:267–283. doi: 10.1080/08870446.2012.717624. [DOI] [PubMed] [Google Scholar]
- Jang S. J., Johnson B. R. Explaining religious effects on distress among African Americans. Journal for the Scientific Study of Religion. 2004;43:239–260. [Google Scholar]
- Kinney A. Y., Emery G., Dudley W. N., Croyle R. T. Screening behaviors among African American women at high risk for breast cancer: Do beliefs about God matter? Oncology Nursing Forum. 2002;29:835–843. doi: 10.1188/02.ONF.835-843. [DOI] [PubMed] [Google Scholar]
- Koenig H. G., King D. E., Carson V. B. Handbook of religion and health. 2nd ed. New York, NY: Oxford University Press; 2012. [Google Scholar]
- Koenig H. G., McCullough M. E., Larson D. B. Handbook of religion and health. New York, NY: Oxford University Press; 2001. [Google Scholar]
- Koenig H. G., Pargament K. I., Nielsen J. Religious coping and health status in medically ill hospitalized older adults. Journal of Nervous and Mental Disease. 1998;186:513–521. doi: 10.1097/00005053-199809000-00001. [DOI] [PubMed] [Google Scholar]
- Levin J. S., Taylor R. J., Chatters L. M. Race and gender differences in religiosity among older adults: Findings from four national surveys. Journal of Gerontology. 1994;49:S137–S145. doi: 10.1093/geronj/49.3.s137. [DOI] [PubMed] [Google Scholar]
- Liang B., Bogat G. A. Culture, control and coping: New perspectives on social support. American Journal of Community Psychology. 1994;22:123–147. [Google Scholar]
- Lukwago S. N., Kreuter M. W., Bucholtz D. C., Holt C. L., Clark E. M. Development and validation of brief scales to measure collectivism, religiosity, racial pride, and time orientation in urban African American women. Family & Community Health. 2001;24:63–71. doi: 10.1097/00003727-200110000-00008. [DOI] [PubMed] [Google Scholar]
- McCurtis Witherspoon K., Williams Richardson A. Sisters in support together against substances (SISTAS): An alcohol abuse prevention group for Black women. Journal of Ethnicity in Substance Abuse. 2006;5:49–60. doi: 10.1300/j233v05n03_03. [DOI] [PubMed] [Google Scholar]
- Mulia N., Ye Y., Greenfield T. K., Zemore S. E. Disparities in alcohol-related problems among white, black, and Hispanic Americans. Alcoholism: Clinical and Experimental Research. 2009;33:654–662. doi: 10.1111/j.1530-0277.2008.00880.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muthén B. O., Muthén L. K. The development of heavy drinking and alcohol-related problems from ages 18 to 37 in a U.S. national sample. Journal of Studies on Alcohol. 2000;61:290–300. doi: 10.15288/jsa.2000.61.290. [DOI] [PubMed] [Google Scholar]
- Pargament K. I., Kennell J., Hathaway W., Grevengoed N., Newman J., Jones W. Religion and the problem-solving process: Three styles of religious coping. Journal for the Scientific Study of Religion. 1988;27:90–104. [Google Scholar]
- Pargament K. I., Koenig H. G., Tarakeshwar N., Hahn J. Religious struggle as a predictor of mortality among medically ill elderly patients: A 2-year longitudinal study. Archives of Internal Medicine. 2001;161:1881–1885. doi: 10.1001/archinte.161.15.1881. [DOI] [PubMed] [Google Scholar]
- Pargament K. I., Murray-Swank N., Magyar G., Ano G. Spiritual struggle: A phenomenon of interest to psychology and religion. In: Miller W. R., William R., editors. Judeo-Christian perspectives on psychology: Human nature, motivation, and change. Washington, DC: APA Press; 2005. pp. 245–268. [Google Scholar]
- Pargament K. I., Smith B. W., Koenig H. G., Perez L. Patterns of positive and negative religious coping with major life stressors. Journal for the Scientific Study of Religion. 1998;37:710–724. [Google Scholar]
- Pew Research Center. A religious portrait of African-Americans. 2009, January 30 Retrieved from http://www.pewforum.org/A-Religious-Portrait-of-African-Americans.aspx.
- Ries L. A. G., Melbert D., Krapcho M., Stinchcomb D. G., Howlader N., Horner M. J., Edwards B. K, editors. Bethesda, MD: National Cancer Institute; 2009, February 6. SEER Cancer Statistics Review, 1975–2005. Retrieved from http://seer.cancer.gov/csr/1975_2005/ [Google Scholar]
- Roth D. L., Mwase I., Holt C. L., Clark E. M., Lukwago S. N., Kreuter M. W. Religious involvement measurement model in a national sample of African Americans. Journal of Religion and Health. 2012;51:567–578. doi: 10.1007/s10943-011-9475-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rotter J. B. Generalized expectancies for internal versus external control of reinforcement. Psychological Monographs. 1966;80:1–28. [PubMed] [Google Scholar]
- Solomon Z., Mikulincer M., Avitzur E. Coping, locus of control, social support, and combat-related posttraumatic stress disorder: A prospective study. Journal of Personality and Social Psychology. 1988;55:279–285. doi: 10.1037//0022-3514.55.2.279. [DOI] [PubMed] [Google Scholar]
- Stahler G. J., Kirby K. C., Kerwin M. E. A faith-based intervention for cocaine-dependent Black women. Journal of Psychoactive Drugs. 2007;39:183–190. doi: 10.1080/02791072.2007.10399877. [DOI] [PubMed] [Google Scholar]
- Stahler G. J., Shipley T. E., Jr., Kirby K. C., Godboldte C., Kerwin M. E., Shandler I., Simons L. Development and initial demonstration of a community-based intervention for homeless, cocaine-using, African-American Women. Journal of Substance Abuse Treatment. 2005;28:171–179. doi: 10.1016/j.jsat.2004.12.003. [DOI] [PubMed] [Google Scholar]
- Stein A. D., Lederman R. I., Shea S. The Behavioral Risk Factor Surveillance System questionnaire: Its reliability in a statewide sample. American Journal of Public Health. 1993;83:1768–1772. doi: 10.2105/ajph.83.12.1768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor R. J., Chatters L. M., Jayakody R., Levin J. S. Black and white differences in religious participation: A multisample comparison. Journal for the Scientific Study of Religion. 1996;35:403–410. [Google Scholar]
- Taylor R. J., Chatters L. M., Levin J. Religion in the lives of African Americans: Social, psychological, and health perspectives. Thousand Oaks, CA: Sage; 2004. [Google Scholar]
- Thoresen C. E. Spirituality, health, and science: The coming revival? In: Roth-Roemer S., Kurpius S. R., editors. The emerging role of counseling psychology in health care. New York, NY: W. W. Norton; 1998. pp. 409–431. [Google Scholar]
- Turner-Musa J., Lipscomb L. Spirituality and social support on health behaviors of African American undergraduates. American Journal of Health Behavior. 2007;31:495–501. doi: 10.5555/ajhb.2007.31.5.495. [DOI] [PubMed] [Google Scholar]
- United States Census Bureau. 2011 American Community Survey 1-Year Estimates [Data file] 2011 Retrieved from http://factfinder.census.gov.
- Vander Zee K. I., Buunk B. P., Sanderman R. Social support, locus of control, and psychological well-being. Journal of Applied Social Psychology. 1997;27:1842–1859. [Google Scholar]
- Voils C. I., Steffens D. C., Bosworth H. B., Flint E. P. Social support and locus of control as predictors of adherence to antidepressant medication in an elderly population. American Journal of Geriatric Psychiatry. 2005;13:157–165. doi: 10.1176/appi.ajgp.13.2.157. [DOI] [PubMed] [Google Scholar]
- Wagner E. F., Lloyd D. A., Gil A. G. Racial/ethnic and gender differences in the incidence and onset age of DSM-IV alcohol use disorder symptoms among adolescents. Journal of Studies on Alcohol. 2002;63:609–619. doi: 10.15288/jsa.2002.63.609. [DOI] [PubMed] [Google Scholar]
- Wallston K. A., Malcarne V. L., Flores L., Hansdottir I., Smith C. A., Stein M. J., Clements P. J. Does God determine your health? The God Locus of Health Control Scale. Cognitive Therapy and Research. 1999;23:131–142. [Google Scholar]
- Wallston K. A., Wallston B. S., DeVellis R. Development of the Multidimensional Health Locus of Control (MHLC) Scales. Health Education Monographs. 1978;6:160–170. doi: 10.1177/109019817800600107. [DOI] [PubMed] [Google Scholar]