Abstract
Background and study aims: 19-gauge (19G) needles are used for EUS-guided tissue acquisition and interventions. The aim of the current study was to compare the functional characteristics of 19G EUS needles by means of using various echoendoscopes in a bench simulator.
Methods: The angles achieved for 19G needles (EchoTip: ET-19G, EchoTip Flex: ExF-19G, Expect: Ex-19G, and ProCore: PC-19G) and for the distal tip of the echoendoscope were evaluated for maximal angulation settings of the distal tip and the elevator. Also the resistance to advancement of the 19G needles at these endoscope settings was assessed. All evaluations were done with endoscopes in a straight and in a curved position.
Results: There was no large discrepancy for scope and needle angles among all echoendoscopes except for the slim Pentax scope (EG-3270UK). The ExF-19G and PC-19G needles showed better optimal angles in various conditions compared to standard 19G needles. In straight scope position, out of the 20 conditions (5 endoscopes × 2 positions of the distal tip × 2 elevator positions) the numbers of optimal angulations achieved for the Ex-19G, ExF-19G, ET-19G, and PC-19G, were 11 /20 (55 %), 20 /20 (100 %), 14 /20 (70 %) and 18 /20 (90 %), respectively. However, regarding resistance, it was impossible to advance theneedle with 14 /20 settings (70 %) for the Ex-19G, 3 /20 (15 %) for the ExF-19G, 10 /20 (50 %) for the ET-19G and 7 /20 (35 %) for the PC-19G. When the scopes were bent, with regard to the force needed to advance the needle, the numbers of optimal settings, for the Ex-19G, ExF-19G, ET-19G, and PC-19G, were 1 (5 %), 13 (65 %), 6 (30 %) and 8 (40 %), respectively. The mean maximum resistance to advancement was less for the ExF-19G than for the other needless in almost all scope and angle conditions (p < 0.05).
Conclusion: Although there was no difference between needles, the resistance to passage was least with the flexible 19-gauge needle (ExF-19G).
Introduction
Several 19-gauge needles are currently available for endoscopic ultrasonography-guided fine-needle aspiration (EUS-FNA) and interventions 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18. However, the large bore and inherent stiffness of these needles hinder their maneuverability for puncture. In addition, other factors such as scope position (bent or curved), echoendoscope tip angulation, and elevator use affect the maneuverability of the needle.
In a prior study from our group that evaluated one particular 19G FNA needle (EchoTip, Cook Endoscopy, Winston-Salem, N.C.), we found that the needle was suboptimal for performing transduodenal FNA of pancreatic head and uncinate lesions 19. We observed that when the tip of the echoendoscope was angulated or when the elevator was used, there was increased resistance to passage of the 19G needle that precluded sampling of lesions. Recently, several 19-gauge needles and small diameter echoendoscopes have been developed. In this study, we compared the characteristics of different 19-gauge EUS needles using various echoendoscopes in a bench simulator (see below) to provide standardized, reproducible, comparative performance data.
Materials and methods
Echoendoscopes
Five curved linear array echoendoscopes (GF-UCT260, GF-UCT240, and GF-UC240P: Olympus Medical Systems, Tokyo, Japan; EG-3870UTK and EG-3270UK: Pentax, Tokyo, Japan), were examined using the bench simulator. The specifications of these echoendoscopes are described in Table 1.
Table 1. Specifications of echoendoscopes.
| Olympus | Pentax | |||
| GF-UCT260 /GF-UCT240 | GF-UC240P | EG-3870UTK | EG-3270UK | |
| Outer diameter (mm) | ||||
| Distal end | 14.6 | 14.2 | 14.3 | 12 |
| Insertion tube | 12.6 | 11.8 | 12.8 | 10.8 |
| Bending section (degree) | ||||
| Up/down | 130/90 | 130/90 | 130/130 | 130/130 |
| Right/left | 90/90 | 90/90 | 120/120 | 120/120 |
| Working length (mm) | 1,250 | 1,250 | 1,250 | 1,250 |
| Working channel diameter (mm) | 3.7 | 2.8 | 3.8 | 2.8 |
| Elevator angle (degree) | 90 | 90 | 90 | 90 |
19G needles
The characteristics of commercially available 19-gauge EUS needles were evaluated by bench simulation for both extent of possible angulation and for resistance to passage under various conditions. Four 19-gauge EUS needles were evaluated: 1) ExpectTM standard type (Ex-19G) (Boston Scientific Japan, Tokyo, Japan), 2) ExpectTM flexible type (ExF-19G) (Boston Scientific Japan), 3) EchoTip® ULTRA (ET-19G) (Cook Endoscopy), 4) EchoTip® ProCoreTM (PC-19G) (Cook Endoscopy).
Before the bench simulation, the diameter of each needle was accurately measured by a digital micrometer caliper (MDC-25, Mitsutoyo, Kanagawa, Japan).
Bench simulation
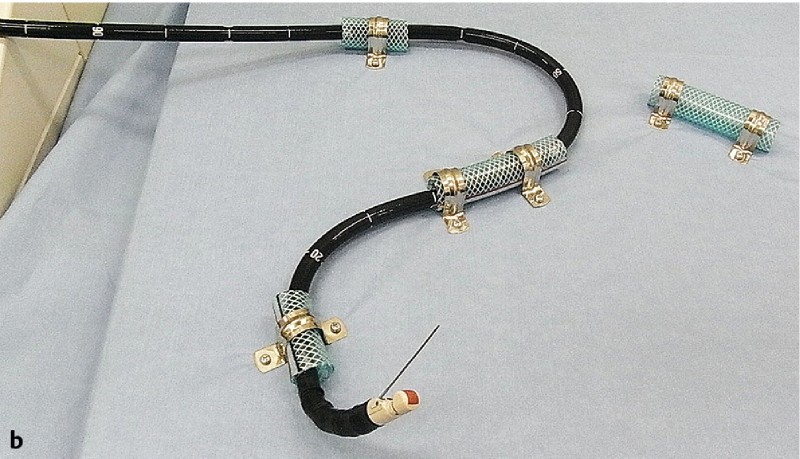
The bench simulator was designed and constructed by one of the authors (T.I.), specifically for the comparative evaluation of different EUS-FNA needles as previously described 19. The operating portion of the echoendoscope was fixed using a vise, and the insertion portion was fixed in straight Fig 1a and curved Fig 1b positions using a wooden board, vinyl chloride tubing with a diameter of 19 mm (ST-19, Toyocs Co., Ltd., Toyama, Japan), and stainless steel saddle grips.

We repeated all the tests with the endoscopes held in both straight and curved positions.
Range of angulation of echoendoscope distal tips and consequent angulation of needles
We measured the maximum achievable angulation for each possible combination of the five echoendoscopes and the four 19G needles. The maximum distal tip “up” and elevator “up” settings were used. Thus the “big knob” (up-down) and not the small knob (left-right) of the echoendoscope was used. This was set at 0° and at maximum in each echoendoscope and the elevator was set at 0° and 90° (maximum). When the tip of the needle was flexed, the angle between the echoendoscope and the sheath of the needle was measured.
The echoendoscope angle and the needle angle, were defined as angle A and angle B, respectively, as shown in Fig 2. Optimal angulation was defined as angle A and angle B being more than 90° and 110°, respectively.
Fig. 2.
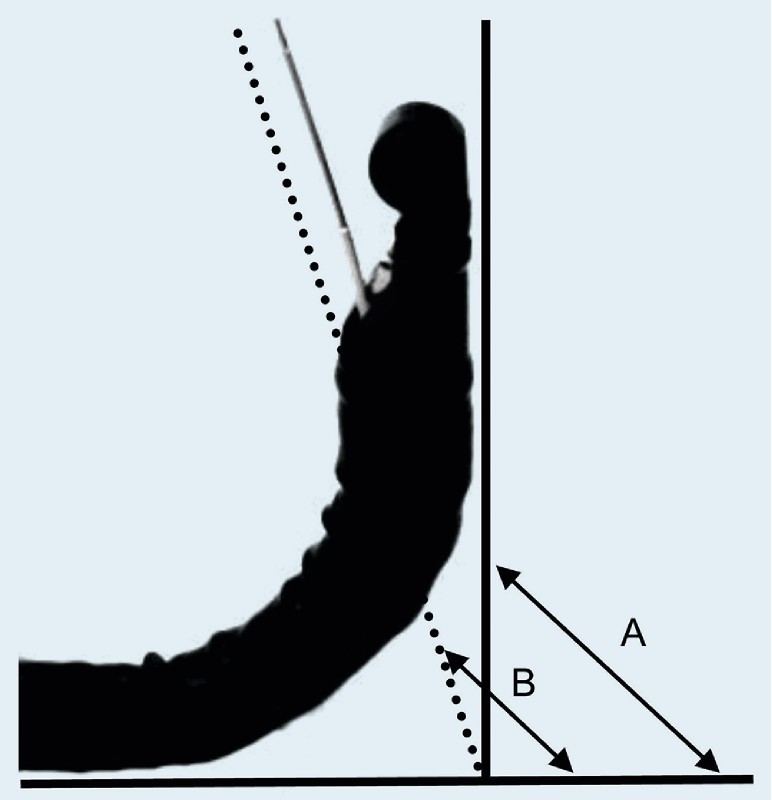
Measurement of angulations of distal tip of echoendoscope and needle: A, distal tip angulation; B, needle angulation.
All measurements were repeated with the scopes held in both the “straight” and the “curved” positions (see Fig 1).
Fig. 1 Bench simulator: a straight therapeutic scope position; b curved scope position.
Resistance of needles
The resistance to needle advancement through the endoscope was measured using an Autograph (AGS-H, Shimadzu Corporation, Kyoto, Japan), which has a highest tolerable force of 1,000 newtons (1,000 N) (Fig 3). The needles were advanced at a speed of 500 mm/min. The length of the needle insertion was 30 mm. The resistance to advancement of the needle was recorded continuously during insertion. The data were analyzed by dedicated software (Factory Shikibu 2000, Shimazu Factory Manufacture).
Fig. 3.

Autograph equipment for examination of resistance to needle insertion.
In this study, the resistance of each FNA needle was measured more than 3 times to obtain reproducible results (mean 3.2 times, range 3 to 5 times) using each scope at each of the possible settings. We prepared and used five each of the four 19G needles for the examination.
As there were five scopes, each with two settings of the distal tip (up/down) and two settings of the elevator (up/down), 20 values were obtained for each needle. Again, all of these measurements were repeated with the scopes held in both the “straight” and the “curved” positions (see Fig 1).
We used our prior data for resistance to needle advancement (R needle) 18 for grading the resistance: R needle < 8 N, optimal setting; R needle > 8 N, suboptimal; R needle > 11 N, impossible to advance the needle.
Statistics
Statistical analyses were performed with StatMate III (ATMS Co. Ltd., Tokyo, Japan). Normally distributed data are presented as the mean ± standard deviation (SD). Kruskal-Wallis test as non-parametric statistic was used to compare between each needle resistances. A P value less than 0.05 was regarded as indicating a statistically significant difference.
Results
Actually achieved distal tip and needle angulations
Type of echoendoscopes
Olympus
The results for all the combinations of scopes and needles, with the scope held in a straight position, are shown in Table 2. In the straight scope position, for both angle A and angle B, the new therapeutic Olympus scope (GF-UCT260) showed optimal angulation using various 19-gauge needles (Table 2). However, both angle A and angle B in two echoendoscopes (GF-UCT240 and GF-UCP240) using standard FNA needles (Ex-19G and ET-19G) were suboptimal.
Table 2. Angles of echoendoscope and needle using the various 19-guage EUS needles in the straight scope position.
| Angle of echoendoscope (angle A) (degree) | Angle of needle (angle B) (degree) | |||||||
| Ex-19G | ExF-19G | ET-19G | PC-19G | Ex-19G | ExF-19G | ET-19G | PC-19G | |
| Olympus | ||||||||
| GF-UCT260 | 93 | 96 | 90 | 94 | 113 | 115 | 114 | 116 |
| GF-UCT240 | 77 | 90 | 88 | 92 | 96 | 115 | 108 | 115 |
| GF-UCP240 | 85 | 92 | 88 | 90 | 105 | 115 | 105 | 115 |
| Pentax | ||||||||
| EG-3870UTK | 90 | 100 | 100 | 110 | 113 | 125 | 135 | 136 |
| EG-3270UK | 55 | 70 | 72 | 80 | 95 | 95 | 104 | 104 |
Abbreviations: ET, EchoTip; EUS, endoscopic ultrasonography; EX, Expect; ExF, Expect Flex; G, gauge; PC, ProCore.
In the curved scope position, angle A and angle B were each optimal in only one of the 16 possible settings. In both the straight and the curved scope position, the GF-UCT260 allowed in 50 % of possible settings better optimal angles compared to others (Table 3).
Table 3. Angles of echoendoscope and needle using the various 19-gauge EUS needles in the curved scope position.
| Angle of echoendoscope (angle A) (degree) | Angle of needle (angle B) (degree) | |||||||
| Ex-19G | ExF-19G | ET-19G | PC-19G | Ex-19G | ExF-19G | ET-19G | PC-19G | |
| Olympus | ||||||||
| GF-UCT260 | 92 | 95 | 82 | 90 | 108 | 112 | 100 | 115 |
| GF-UCT240 | 78 | 90 | 84 | 87 | 104 | 104 | 106 | 115 |
| GF-UCP240 | 80 | 80 | 80 | 88 | 105 | 104 | 106 | 111 |
| Pentax | ||||||||
| EG-3870UTK | 85 | 95 | 88 | 92 | 105 | 124 | 125 | 130 |
| EG-3270UK | 55 | 65 | 68 | 70 | 75 | 90 | 94 | 91 |
Abbreviations: ET, EchoTip; EUS, endoscopic ultrasonography; EX, Expect; ExF, Expect Flex; G, gauge; PC, ProCore.
Pentax
Regardless of scope positions, the therapeutic Pentax scope (EG-3870UTK) showed optimal angles compared to the slim echoendoscope (E6-3270UK) (Table 3).
The type of needles
Standard FNA needles (Ex-19G and ET-19G)
In the straight scope position, using the Ex-19G showed optimal angles A and B in only two echoendoscopes the (GF-UCT260 and the EG-3870UTK). With the curved scope position, in almost all conditions, angles A and B were suboptimal angles. The results for the ET-19G were similar to those of the EX-19G.
PC-19G
In the straight scope position, the PC-19G showed optimal angle A and B in all but one echoendoscope (EG-3270UK). Similarly, with the curved scope position, angle B was optimal in all but one echoendoscope (EG-3270UK) though angle A in three echoendoscopes (GF-UCT240, GF-UCP240 and EG-3270UK) was suboptimal.
ExF-19G
When the scope was straight, the ExF-19G showed optimal Angle A and B in all but one echoendoscope (EG-3270UK). With the curved scope position, 5 out of the 10 values forof angles A and B were optimal.
Resistance to advancement of 19-gauge needles
The maximum resistance to advancement of the FNA needles is shown in Table 4 for the straight scope position and in Table 5 for the curved scope position. The results show high reproducibility with only small SDs (Table 4 and Table 5). In all cases, the resistance to the passage of the FNA needles, R needle, was greater with greater angulation of the distal tip and of the elevator. Increased resistance was observed irrespective of the type of echoendoscope.
Table 4. The maximum resistance to advancement of needle in the straight scope position (in newtons, N, mean ± SD).
| Echoendoscope | Distal tip angulation | Elevator angulation | Ex-19G | ExF-19G | ET-19G | PC-19G |
| Olympus | ||||||
| GF-UCT260 | 0° | 0° | 5.03 ± 0.53 | 2.01 ± 0.21 | 3.04 ± 0.05 | 3.35 ± 0.09 |
| Max | 10.73 ± 0.34 | 4.10 ± 0.20 | 6.60 ± 0.43 | 7.03 ± 0.13 | ||
| Max | 0° | 7.78 ± 0.27 | 4.75 ± 0.53 | 5.04 ± 0.14 | 6.78 ± 0.15 | |
| Max | 11.55 ± 0.52 | 5.13 ± 0.13 | 6.12 ± 0.10 | 7.59 ± 0.22 | ||
| GF-UCT240 | 0° | 0° | 4.68 ± 0.20 | 2.75 ± 0.10 | 4.48 ± 0.16 | 2.81 ± 0.17 |
| Max | 8.60 ± 0.43 | 4.34 ± 0.19 | 8.28 ± 0.40 | 6.23 ± 0.32 | ||
| Max | 0° | 7.00 ± 0.21 | 4.98 ± 0.45 | 7.48 ± 0.21 | 5.05 ± 0.10 | |
| Max | 9.47 ± 0.12 | 5.61 ± 0.36 | 9.09 ± 0.19 | 6.93 ± 0.08 | ||
| GF-UCP240 | 0° | 0° | 7.82 ± 0.25 | 1.61 ± 0.09 | 4.38 ± 0.18 | 3.14 ± 0.43 |
| Max | 9.30 ± 0.37 | 3.78 ± 0.21 | 6.93 ± 0.03 | 5.58 ± 0.08 | ||
| Max | 0° | 13.63 ± 0.40 | 3.77 ± 0.08 | 7.58 ± 0.52 | 5.40 ± 0.09 | |
| Max | 14.58 ± 0.20 | 5.60 ± 0.87 | 8.58 ± 0.10 | 6.87 ± 0.10 | ||
| Pentax | ||||||
| EG-3870UTK | 0° | 0° | 4.23 ± 0.25 | 1.57 ± 0.08 | 3.12 ± 0.06 | 2.83 ± 0.16 |
| Max | 6.02 ± 0.39 | 2.98 ± 0.03 | 6.05 ± 0.05 | 4.77 ± 0.08 | ||
| Max | 0° | 7.98 ± 0.30 | 3.53 ± 0.33 | 6.83 ± 0.13 | 4.28 ± 0.53 | |
| Max | 9.30 ± 0.99 | 4.05 ± 0.23 | 8.55 ± 0.23 | 7.03 ± 0.10 | ||
| EG-3270UK | 0° | 0° | 3.63 ± 0.21 | 1.57 ± 0.03 | 4.10 ± 0.15 | 2.82 ± 0.13 |
| Max | 5.00 ± 0.17 | 7.30 ± 0.64 | 10.90 ± 0.20 | 8.42 ± 0.23 | ||
| Max | 0° | 7.95 ± 0.30 | 3.68 ± 0.08 | 7.33 ± 0.08 | 5.23 ± 0.13 | |
| Max | 8.88 ± 0.33 | 7.42 ± 1.01 | 10.93 ± 0.17 | 9.32 ± 0.13 | ||
Abbreviations: ET, EchoTip; Ex, Expect; ExF, Expect Flex; Max, maximum angulation; PC, ProCore.
Table 5. The maximum resistance to advancement of needle in the curved scope position (in newtons N, mean ± SD).
| Echoendoscope | Distal tip angulation | Elevator angulation | Ex-19G | ExF-19G | ET-19G | PC-19G |
| Olympus | ||||||
| GF-UCT260 | 0° | 0° | 10.29 ± 0.32 | 2.51 ± 0.17 | 5.23 ± 0.15 | 3.83 ± 0.22 |
| Max | 13.52 ± 0.49 | 7.84 ± 0.52 | 12.78 ± 0.51 | 11.75 ± 0.14 | ||
| Max | 0° | 10.61 ± 0.74 | 5.29 ± 0.09 | 7.39 ± 0.15 | 7.29 ± 0.23 | |
| Max | 14.53 ± 0.77 | 9.16 ± 0.49 | 12.80 ± 0.34 | 11.91 ± 0.63 | ||
| GF-UCT240 | 0° | 0° | 10.13 ± 0.62 | 3.05 ± 0.17 | 6.91 ± 0.54 | 4.61 ± 0.34 |
| Max | 12.37 ± 0.38 | 10.55 ± 0.34 | 16.35 ± 0.76 | 12.08 ± 0.97 | ||
| Max | 0° | 13.80 ± 0.22 | 7.47 ± 0.10 | 10.65 ± 0.66 | 8.33 ± 0.34 | |
| Max | 15.23 ± 0.33 | 11.42 ± 0.08 | 17.35 ± 0.44 | 14.43 ± 0.86 | ||
| GF-UCP240 | 0° | 0° | 8.87 ± 0.32 | 3.39 ± 0.20 | 7.66 ± 0.23 | 4.53 ± 0.18 |
| Max | 12.05 ± 0.40 | 9.25 ± 0.15 | 14.50 ± 0.83 | 10.10 ± 0.15 | ||
| Max | 0° | 12.45 ± 0.26 | 6.23 ± 0.06 | 10.22 ± 0.20 | 7.60 ± 0.21 | |
| Max | 14.70 ± 0.25 | 12.15 ± 0.72 | 15.11 ± 0.71 | 11.67 ± 0.24 | ||
| Pentax | ||||||
| EG-3870UTK | 0° | 0° | 10.77 ± 0.12 | 2.03 ± 0.08 | 5.64 ± 0.07 | 3.15 ± 0.10 |
| Max | 12.62 ± 0.15 | 5.43 ± 0.10 | 12.30 ± 0.30 | 9.33 ± 0.53 | ||
| Max | 0° | 14.95 ± 0.48 | 4.55 ± 0.09 | 9.18 ± 0.08 | 7.10 ± 0.05 | |
| Max | 16.00 ± 0.35 | 5.88 ± 0.26 | 11.35 ± 0.20 | 9.95 ± 0.36 | ||
| EG-3270UK | 0° | 0° | 7.72 ± 0.53 | 2.47 ± 0.08 | 4.47 ± 0.23 | 3.33 ± 0.10 |
| Max | 11.27 ± 0.31 | 10.11 ± 0.55 | 15.80 ± 0.22 | 14.78 ± 0.28 | ||
| Max | 0° | 11.65 ± 0.54 | 6.65 ± 0.17 | 9.70 ± 0.23 | 8.05 ± 0.22 | |
| Max | 13.00 ± 0.18 | 12.08 ± 0.40 | 17.77 ± 0.63 | 13.12 ± 0.51 | ||
Abbreviations: ET, EchoTip; EX, Expect; ExF, Expect Flex; Max, maximum angulation; PC, ProCore.
Straight scope position
With a straight scope, the numbers of optimal settings of the distal tip and the elevator in the Ex-19G, ExF-19G, ET-19G, and PC-19G, were 11 /20 (55 %), 20 /20 (100 %), 14 /20 (70 %) and 18 /20 (90 %), respectively (Table 4). These were the settings where the resistance to advancement of the needle was ≤ 8 N. The mean maximum R needle was smaller for the ExF-19G than for others in all scope and angle conditions (p < 0.05).
Curved scope position
With the scope in a curved position, needle advancement was graded as “impossible” in 14 /20 settings (70 %) for the Ex-19G, 3 /20 (15 %) for the ExF-19G, 10 /20 (50 %) for the ET-19G and 7 /20 (35 %) for the PC-19G (Table 5). On the other hand, the numbers of optimal settings for the Ex-19G, ExF-19G, ET-19G, and PC-19G, were 1 (5 %), 13 (65 %), 6 (30 %) and 8 (40 %), respectively. In almost all conditions, the mean maximum R needle for the ExF-19G was smaller than that of others (p < 0.05).
Discussion
Interventional EUS procedures frequently require the use of a 19-gauge needle in conjunction with a 0.035-inch guidewire. However, most 19-gauge needles, given their large caliber, encounter resistance when the echoendoscope tip is angulated resulting in poor maneuverability. Our experimental study 19 revealed that the distal tipup and elevator-up positions lead to higher resistance for the needle, resulting in difficulty in puncture by the needle and contributing to shearing of the guidewire. To overcome this limitation, recently, newer 19-gauge needles and a slim echoendoscope (the EG-3270UK) have been developed.
Until now, although there have been several experimental and clinical comparative studies between 19-gauge needle and others (Trucut, 22 – and 25-gauge needles) 19 20 21 22 23, there has been no comparative study for various 19-gauge needles including newer ones in combination with various old and newer echoendoscopes.
Angles A and B may represent, respectively, the abilitiesto delineate and to puncture targeted lesions. Smaller angles may mean less needle maneuverability, thereby limiting the various interventions. In the present study, although initially we postulated that there was no difference between the angles A and B among the standard echoendoscopes equipped with a 19G needle, the standard Pentax scope (EG-3870UTK) showed optimal angulation with a variety of 19G needles compared with standard Olympus echoendoscopes. However, we should consider actual clinical situations because the echoendoscopic delineation of targeted lesions depends on both the flexibility of the scope and the direction of the ultrasound probe. The direction of the ultrasound probe differs between the Pentax and Olympus echoendoscopes, which have a side and an oblique direction, respectively, for the ultrasound beam direction. Therefore, the actual differentiation between the standard Pentax and Olympus scopes may be unclear because we did not image any real lesions by means of EUS with a 19G needle. The diagnostic slim Pentax echoendoscope (EG-3270UK) showed comparatively lower scope angulations than others. These data suggest that the standard large-diameter EUS scope has a robust wire that enables the large tip of the endoscope to be safely bent, while the diagnostic slim echoendoscope does not have a such a robust wire. That may lead to lower angulations when the 19-gauge needle is used. Since the needle angulation (angle B) is the most important parameter for various interventional EUS procedures, the Pentax slim echoendoscope in combination with a 19-gauge needle seems to be suboptimal for interventional EUS.
In terms of selection of a 19-gauge needle, from the aspect of the scope–needle angles allowed by various echoendoscopes, our data suggested that among the various 19-gauge needles, the ExpectTM flexible type needle (Boston Scientific) and/or the ProCoreTM needle (Cook Endoscopy) appear to be optimal for interventional EUS including EUS-FNA, because of the optimal angulation in various scope settings. However, the two needles are quite different in concept: theProCoreTM needle is basically used for dedicated EUS-FNA procedures and the ExpectTM flexible needle for both FNA and interventions. In terms of cytological/histological performance, we suggest that there may be differences between the classic 19-G needle and the ProCoreTM 19-G/ ExpectTM 19-G flexible type needle in special settings, e. g. the trans-duodenal approach to lesion puncture. In addition, they seem to be optimal for EUS-FNA when core tissues, obtained using a 19-G needle are preferable for accurate diagnosis in special settings such as malignant lymphoma and autoimmune pancreatitis, although current 22-G and/or 25-G needles are sufficient for EUS-FNA in patients with common diseases such as pancreatic cancers.
Even when lesions can be well delineated, the puncture is not always successful because of lack of sharpness of the needle and the resistance to its advancement. Resistance to the needle is caused by various factors, e. g. torque, kinking of working channel due to scope position, and use of distal tip/elevator angulation. These limited the performance of the needle, resulting in failure of puncture during EUS-FNA. Our previous study evaluating resistance to the needle revealed that resistance to needle advancement was moderate at s resistance of 5 N or more and high at 8 N or more, and that it was impossible to advance the needle when the resistance was 11 N or more 19. In the short scope position, the transgastric approach, unless the maximum up-angulation was applied in the distal tip and the elevator at the same time, needle punctures was possible using any 19-gauge needle. The results of the present study were similar to our previous data 19. In the straight scope position, the new flexible 19-gauge needle encountered comparatively less resistance than other needles and all needles encountered lower resistance (< 8 N). When the scope was curved, most of the 19G needles met resistance greater than 10 N. In particular, in the case of both distal-tipup and elevator-up angulation, resistances to the needle were more than 11 N, meaning that puncture was impossible. Also surprisingly, the R needle for the new flexible 19-gauge needle was lower than that of others. Our results suggest that for needle puncture in difficult situations, such as trans-duodenal approach, the flexible 19G needle may be most appropriate. However, even when the flexible 19-gauge needle is used, the tight bending of distal tip-up and elevator-up angulation hinders advancement of the needle and at times, puncture by the needle is impossible, in particular when diagnostic thinner echoendoscopes (GF-UCP240 and EG-3270UK) are used. We speculate that in such thinner scopes, the needle compliance decreases because of kinking of the smaller working channel by distal tip angulation, or because of strong friction when the the needle is pinned by the elevator mechanism.
The up-to-date findings of our study may be important because they are an important step in knowing which 19-gauge needles and endoscopes are better for EUS-related procedures. Our results suggest that both the ExpectTM flexible type needle and the ProCoreTM needle seem to be optimal for EUS-FNA used with either therapeutic Olympus (GF-UCT260 and GF-UCT240) or Pentax scopes (EG-3870UTK). However, for interventional EUS that requires the use of a guidewire, the ExpectTM flexible needle appears to be optimal, in particular for the trans-duodenal approach.
The current 19-gauge needles, however, are still not the best for EUS-related procedures. For instance, the 19G ProCoreTM needle and the ExpectTM 19G flexible needle are still not as flexible compared to current 22 – and 25-gauge needles. Thus, we still need of better technology to overcome this limitation.
There are several limitations in this study. Since various factors, such as echoendoscope position, the patient’s pathology, anatomical differences, and torque of the scope cannot be reproduced in an experimental model, the conclusions may not hold true for all clinical scenarios.
In conclusion, our experimental data suggests that both the ExpectTM flexible type needle and the ProCoreTM needle seems to be most suitable for EUS-FNA procedures. The ExpectTM flexible type needle appears to be particularly suitable for the trans-duodenal approach and for interventional EUS procedures.
Acknowledgement
The authors are indebted to Professor J. Patrick Barron of the International Medical Communications Center of Tokyo Medical University for his review of this manuscript.
Footnotes
Competing interests: None.
References
- 1.Iwashita T, Yasuda I, Doi S. et al. Use of samples from endoscopic ultrasound-guided 19-gauge fine-needle aspiration in diagnosis of autoimmune pancreatitis. Clin Gastroenterol Hepatol. 2012;10:316–322. doi: 10.1016/j.cgh.2011.09.032. [DOI] [PubMed] [Google Scholar]
- 2.Varadarajulu S, Bang J Y, Hebert-Magee S. Assessment of the technical performance of the flexible 19-gauge EUS-FNA needle. Gastrointest Endosc. 2012;76:336–343. doi: 10.1016/j.gie.2012.04.455. [DOI] [PubMed] [Google Scholar]
- 3.Varadarajulu S, Lopes T L, Wilcox C M. et al. EUS versus surgical cyst-gastrostomy for management of pancreatic pseudocysts. Gastrointest Endosc. 2008;68:649–655. doi: 10.1016/j.gie.2008.02.057. [DOI] [PubMed] [Google Scholar]
- 4.Itoi T, Binmoeller K F, Shah J. et al. Clinical evaluation of a novel lumen-apposing metal stent for endosonography-guided pancreatic pseudocyst and gallbladder drainage (with video) Gastrointest Endosc. 2012;75:870–876. doi: 10.1016/j.gie.2011.10.020. [DOI] [PubMed] [Google Scholar]
- 5.Park D H, Lee S S, Moon S H. et al. Endoscopic ultrasound-guided versus conventional transmural drainage for pancreatic pseudocysts: a prospective randomized trial. Endoscopy. 2009;41:842–848. doi: 10.1055/s-0029-1215133. [DOI] [PubMed] [Google Scholar]
- 6.Seewald S, Ang T L, Richter H. et al. Long-term results after endoscopic drainage and necrosectomy of symptomatic pancreatic fluid collections. Dig Endosc. 2012;24:36–41. doi: 10.1111/j.1443-1661.2011.01162.x. [DOI] [PubMed] [Google Scholar]
- 7.Giovannini M, Dotti M, Bories E. et al. Hepaticogastrostomy by echo-endoscopy as a palliative treatment in a patient with metastatic biliary obstruction. Endoscopy. 2003;35:1076–1078. doi: 10.1055/s-2003-44596. [DOI] [PubMed] [Google Scholar]
- 8.Horaguchi J, Fujita N, Noda Y. et al. Endosonography-guided biliary drainage in cases with difficult transpapillary endoscopic biliary drainage. Dig Endosc. 2009;21:239–244. doi: 10.1111/j.1443-1661.2009.00899.x. [DOI] [PubMed] [Google Scholar]
- 9.Itoi T, Isayama H, Sofuni A. et al. Stent selection and tips on placement technique of EUS-guided biliary drainage: transduodenal and transgastric stenting. J Hepatobiliary Pancreat Sci. 2011;18:664–672. doi: 10.1007/s00534-011-0410-9. [DOI] [PubMed] [Google Scholar]
- 10.Artifon E L, Pinhata Otoch J. et al. Endoscopy Ultra- Sonography -guided biliary drainage in the surgical -endoscopy era. Rev Gastroenterol Peru. 2001;31:365–375. [PubMed] [Google Scholar]
- 11.Park D H, Koo J E, Oh J. et al. EUS-guided biliary drainage with one-step placement of a fully covered metal stent for malignant biliary obstruction: A prospective feasibility study. Am J Gastroenterol. 2009;104:2168–2174. doi: 10.1038/ajg.2009.254. [DOI] [PubMed] [Google Scholar]
- 12.Hara K, Yamao K, Niwa Y. et al. Prospective clinical study of EUS-guided choledochoduodenostomy for malignant lower biliary tract obstruction. Am J Gastroenterol. 2011;106:1239–1245. doi: 10.1038/ajg.2011.84. [DOI] [PubMed] [Google Scholar]
- 13.Kahaleh M. Therapeutic and advanced endoscopic retrograde cholangiopancreatography. Gastrointest Endosc Clin N Am. 2012 Jul. 22:xv. doi: 10.1016/j.giec.2012.06.001. [DOI] [PubMed] [Google Scholar]
- 14.Baron T H, Topazian M D. Endoscopic transduodenal drainage of the gallbladder: implications for endoluminal treatment of gallbladder disease. Gastrointest Endosc. 2007;65:735–737. doi: 10.1016/j.gie.2006.07.041. [DOI] [PubMed] [Google Scholar]
- 15.Eum J, Park do Hyun, Ryu C H. et al. EUS-guided biliary drainage with a fully covered metal stent as a novel route for natural orifice transluminal endoscopic biliary interventions: a pilot study (with videos) Gastrointest Endosc. 2011;72:1279–1284. doi: 10.1016/j.gie.2010.07.026. [DOI] [PubMed] [Google Scholar]
- 16.Itoi T, Itokawa F, Kurihara T. Endoscopic ultrasonography-guided gallbladder drainage: actual technical presentations and review of the literature (with videos) J Hepatobiliary Pancreat Sci. 2011;18:282–286. doi: 10.1007/s00534-010-0310-4. [DOI] [PubMed] [Google Scholar]
- 17.Giovannini M. Endoscopic ultrasonography-guided pancreatic drainage. Gastrointest Endosc Clin N Am. 2012;22:221–230. doi: 10.1016/j.giec.2012.04.004. [DOI] [PubMed] [Google Scholar]
- 18.Itoi T, Kikuyama M, Ishii K. et al. EUS-guided rendezvous with single-balloon enteroscopy for treatment of stenotic pancreaticojejunal anastomosis in post-Whipple patients (with video) Gastrointest Endosc. 2011;73:398–401. doi: 10.1016/j.gie.2010.07.010. [DOI] [PubMed] [Google Scholar]
- 19.Itoi T, Itokawa F, Kurihara T. et al. Experimental endoscopy: objective evaluation of EUS needles. Gastrointest Endosc. 2009;69:509–516. doi: 10.1016/j.gie.2008.07.017. [DOI] [PubMed] [Google Scholar]
- 20.Varadarajulu S, Fraig M, Schmulewitz N. et al. Comparison of EUS-guided 19-gauge trucut needle biopsy with EUS-guided fine-needle aspiration. Endoscopy. 2004;36:397–401. doi: 10.1055/s-2004-814316. [DOI] [PubMed] [Google Scholar]
- 21.Itoi T, Itokawa H, Sofuni A. et al. Puncture of solid pancreatic tumors guided by endoscopic ultrasonography: A pilot study series comparing trucut and 19-gauge and 22-gauge aspiration needle. Endoscopy. 2005;37:362–366. doi: 10.1055/s-2004-826156. [DOI] [PubMed] [Google Scholar]
- 22.Song T J, Kin J, Lee S S. et al. The prospective tandomized, controlled trial of endoscopic ultrasound-guided fine-needle aspiration using 22G and 19G aspiration needles for solid pancreatic or peripancreatic masses. Am J Gastroenterol. 2010;105:1739–1745. doi: 10.1038/ajg.2010.108. [DOI] [PubMed] [Google Scholar]
- 23.Sakamoto H, Kitano M, Komaki T. et al. Prospective comparative study of the EUS guided 25-gauge FNA needle with the 19-gauge Trucut needle and 22-gauge FNA needle in patients with solid pancreatic masses. J Gastroenterol Hepatol. 2009;24:384–390. doi: 10.1111/j.1440-1746.2008.05636.x. [DOI] [PubMed] [Google Scholar]


