Abstract
Background and study aims: A study was undertaken to describe the management of post-cholecystectomy biliary fistula according to the type of cholecystectomy.
Patients and methods: A retrospective analysis of 111 patients was undertaken. They were divided into open cholecystectomy (OC) and laparoscopic cholecystectomy (LC) groups.
Results: Of the 111 patients, 38 (34.2 %) underwent LC and 73 (65.8 %) underwent OC. Endoscopic retrograde cholangiopancreatography (ERCP) diagnosed major bile duct injury (BDI) in 27 patients (38.6 %) in the OC group and in 3 patients (7.9 %) in the LC group (P = 0.001). Endoscopic management was not feasible in 15 patients (13.5 %) because of failed cannulation (n = 3) or complete ligation of the common bile duct (n = 12). Endoscopic therapy stopped leakage in 35 patients (92.1 %) and 58 patients (82.9 %) following LC and OC, respectively, after the exclusion of 3 patients in whom cannulation failed (P = 0 0.150). Major BDI was more commonly detected after OC (P < 0.001). Leakage was controlled endoscopically in 77 patients (98.7 %) with minor BDI and in 16 patients (53.3 %) with major BDI (P < 0.001).
Conclusions: Major BDI is more common in patients presenting with bile leakage after OC. ERCP is the first-choice treatment for minor BDI. Surgery plays an important role in major BDI. Magnetic resonance cholangiopancreatogrphy (MRCP) should be used before ERCP in patients with bile leakage following OC or converted LC.
Introduction
Despite the fact that laparoscopic cholecystectomy (LC) is the gold standard treatment for symptomatic gallbladder disease, open cholecystectomy (OC) is the ultimate approach when the laparoscopic route fails. Furthermore, OC is still widely performed in many parts of the world. The lack of necessary laparoscopic equipment in government hospitals and the fact that private practices handle a large share of the medical services are two important reasons for the popularity of OC in countries like Egypt 1.
Several classifications of bile duct injury (BDI) exist that address different types of injuries, management modalities, prognosis, and associated injuries 2. Biliary leakage or fistula is one of the common presentations of BDI 3 and is included in many of the most widely used classifications of BDI 4 5 6.
Endoscopic modalities, including endoscopic sphincterotomy, stenting, and the placement of nasobiliary drains, have replaced surgery as a first-line approach to the management of minor BDI 7 8 9, whereas surgical reconstruction is the ideal treatment for major BDI 9 10 11.
In this article, we aim to share our experience of patients referred to our endoscopy unit for the management of post-cholecystectomy biliary leakage, with special emphasis on the incidence of major BDI following open or laparoscopic procedures and the role of magnetic resonance cholangiopancreatography (MRCP) before endoscopic retrograde cholangiopancreatography (ERCP).
Patients and methods
Between May 1994 and May 2011, 111 patients with the diagnosis of post-cholecystectomy biliary leakage or biliary fistula were identified in the computerized database of the ERCP unit of the Gastro-enterology Surgical Center, Mansoura University, Mansoura, Egypt. Our unit is the referral unit for the Egyptian Delta area, which serves more than 5 million persons. We treat patients referred from private practices, government district hospitals, and university hospitals, as well as patients who undergo LC at our center.
The diagnosis of biliary leak was based on the presence of bile in abdominal drains or abdominal collections, or bile exiting through abdominal wounds. The medical records and follow-up visits of these patients were reviewed. The study population was divided into OC and LC groups. Patients who had undergone OC and T-tube insertion were included in the OC group.
We classified BDI as major or minor based on the classification of Bergman et al. 5. Major BDI was defined as ligation or stricture of the common bile duct (CBD), common hepatic duct (CHD), or right hepatic duct (RHD). Cystic duct and cholecystohepatic duct leaks were classified as minor BDI. Bile leakage around a T-tube with no associated strictures was considered a minor BDI.
All patients were discharged after cessation of the bile leak or progressive reduction of the daily effluent. Patients were followed up in the outpatient clinic for 8 to 12 weeks or until definitive treatment of the cause of the leakage. Plain abdominal X-ray studies were ordered for patients who underwent stent placement before another ERCP was scheduled for stent removal and follow-up cholangiography. ERCP was not considered for patients with stents that had migrated and no symptoms.
The primary outcome was the incidence of major BDI after OC or LC. Secondary outcomes were the success of ERCP in resolving bile leak (initial success rate) and treating its cause, in addition to the adverse effects of ERCP and subsequent procedures.
Definitions
Pre-ERCP management includes all procedures performed before ERCP, whether before or after admission to our hospital. Primary management is defined as management during the initial ERCP procedure. Secondary management is defined as all therapeutic procedures used to control persistent biliary leakage following the primary procedure until resolution of the leakage. Definitive management is defined as the therapeutic procedures undertaken to definitively treat the underlying cause of biliary leakage if it was not corrected previously (e. g., missed stones or biliary strictures).
Statistical analysis
Continuous variables are presented as median with range. Categorical variables are presented as proportions. Continuous variables were compared over the LC group and OC group with the two-tailed Mann-Whitney U test, whereas categorical variables were compared with the chi-squared test or Fischer’s exact test if applicable. A P value of less than 0.05 was considered statistically significant. All analyses were performed with SPSS 17.0 for Windows (SPSS, Chicago, Illinois).
Results
During the study period, more than 9000 ERCP procedures were performed in our unit, including procedures in 111 patients who underwent ERCP for the management of post-cholecystectomy biliary leakage. The patients’ demographics and symptoms are shown in Table 1. The OC group includes 2 patients whose procedure was converted from an LC.
Table 1. Epidemiology and symptoms of the study population.
| Parameter | LC(n = 38) | OC(n = 73) | Total(n = 111) | P value |
| Sex | ||||
| Male | 12 (32 %) | 37 (51 %) | 49 (44 %) | 0.07 |
| Female | 26 (68 %) | 36 (49 %) | 62 (56 %) | |
| Age, y | ||||
| Mean (SD) | 42.6 (14) | 47.5 (12) | 46 | 0.136 |
| Median (range) | 41 (16 – 65) | 48 (17 – 80) | (16 – 80) | |
| Bile leak | ||||
| Surgical drain | 26 (68 %) | 38 (52 %) | 64 (58 %) | 0.085 |
| US-guided tube drain | 12 (32 %) | 22 (30 %) | 34 (30 %) | |
| Drain site | 0 | 4 (6 %) | 4 (4 %) | |
| Wound | 0 | 9 (12 %) | 9 (8 %) | |
| Referral | ||||
| Private | 15 (40 %) | 55 (75 %) | 70 (63 %) | < 0.001 |
| Governmental hospital | 8 (21 %) | 16 (22 %) | 24 (22 %) | |
| Tertiary referral center | 15 (39 %) | 2 (3 %) | 17 (15 %) | |
| Symptoms | ||||
| Pain | 34 (90 %) | 58 (80 %) | 92 (83 %) | 0.143 |
| Jaundice | 11 (29 %) | 42 (58 %) | 53 (48 %) | 0.005 |
| Fever | 17 (45 %) | 30 (41 %) | 47 (42 %) | 0.840 |
| Abdominal distension | 8 (21 %) | 21 (29 %) | 29 (26 %) | 0.496 |
| Total | 38 | 73 | 111 |
LC, laparoscopy cholecystectomy; OC, open cholecystectomy; US, ultrasound.
Pre-ERCP management (Table 2)
Table 2. Pre-ERCP management, procedure – ERCP interval, and diagnostic ERCP success rate.
| LC(n = 38) | OC(n = 73) | Total(n = 111) | P value | |
| Pre-ERCP imaging | ||||
| Collection | 18 (47 %) | 43 (59 %) | 61 (55 %) | 0.169 |
| Missed stones | 3 (8 %) | 7 (10 %) | 10 (9 %) | 0.525 |
| Pre-ERCP management | ||||
| US-guided tube drain | 14 (37 %) | 25 (34 %) | 39 (35 %) | 0.458 |
| Exploration and drainage | 2 (5 %) | 8 (11 %) | 10 (9 %) | < 0.001 |
| Exploration and T-tube | 0 | 2 (3 %) | 2 (2 %) | |
| Interval to ERCP, days | ||||
| Mean (SD) | 8.3 ± 1.5 | 28.5 ± 4 | 18.9 ± 2.2 | < 0.001 |
| Median (range) | 5 (1 – 45) | 15 (2 – 100) | 9 (1 – 00) | |
| Diagnostic ERCP success rate | 38 (100 %) | 70 (96 %) | 108 (97 %) | 0.550 |
ERCP, endoscopic retrograde cholangiopancreatography; LC, laparoscopy cholecystectomy; OC, open cholecystectomy; US, ultrasound.
The cholecystectomy-ERCP interval was significantly shorter in the LC group (median, 5 days; range, 1 – 45) than in the OC group (median, 15 days; range, 2 – 100; P < 0.001). Ultrasound-guided tube drain placement was used in 39 patients (35 %), with no significant difference between the groups. Surgical exploration and drainage with or without T-tube placement was done in 2 patients (5 %) in the LC group and 10 patients (13.7 %) in the OC group (P = < 0.001).
ERCP findings and primary management (Table 3, Table 4 and Fig. 1)
Table 3. ERCP findings in 108 cases, excluding 3 cases in which diagnostic ERCP failed.
| ERCP findings | LC (n = 38) | OC (n = 70) | Total (108) | P value |
| Major bile duct injury | 3 (7.9 %) | 27 (38.6 %) | 30 (27.8 %) | 0.0011 |
| Ligated CHD | 1 (2.6 %) | 11 (15.1 %) | 12 (11.1 %) | |
| CHD stricture | 1 (2.6 %) | 14 (19.2 %) | 15 (13.8 %) | |
| RHD injury | 1 (2.6 %) | 2 (2.7 %) | 3 (2.7 %) | |
| Minor bile duct injury | 35 (92.1 %) | 43 (61.4 %) | 78 (72.2 %) | |
| Cystic duct leak | 31 (81.6 %) | 35 (47.9 %) | 66 (61.1 %) | |
| Cholecystohepatic duct | 4 (10.5 %) | 0 | 4 (3.7) | |
| Around T-tube | 0 | 7 (9.6 %) | 7 (6.4) | |
| No escape of dye | 0 | 1 (1.4 %) | 1 (0.9) | |
| Associated findings | ||||
| Missed stone | 7 (18.4 %) | 13 (20 %) | 20 (18.5 %) | 1.00 |
| Ampullary tumor | 0 | 1 (1.4 %) | 1 (0.9 %) | |
| Distal CBD stricture | 0 | 1 (1.4 %) | 1 (0.9 %) |
ERCP, endoscopic retrograde cholangiopancreatography; LC, laparoscopic cholecystectomy; OC, open cholecystectomy; CHD, common hepatic duct; RHD, right hepatic duct; CBD, common bile duct.
Major bile duct injury versus minor bile duct injury.
Table 4. Therapeutic ERCP success rate and initial endoscopic management.
| Initial endoscopic treatment | Total (%) (n = 108) |
| Successful (leak resolved) | 93 (83.8 %) |
| Stent (single) | 80 (72.1 %) |
| Stent (+ stone extraction) | 5 (4.5 %) |
| Stent (+ dilation) | 2 (1.8 %) |
| Stent (double) | 1 (0.9 %) |
| ES | 2 (1.8 %) |
| ES (+ stone extraction) | 8 (7.2 %) |
| Guidewire failed to pass | 12 (11.1 %) |
ERCP, endoscopic retrograde cholangiopancreatography; ES, endoscopic sphincterotomy.
Fig. 1.
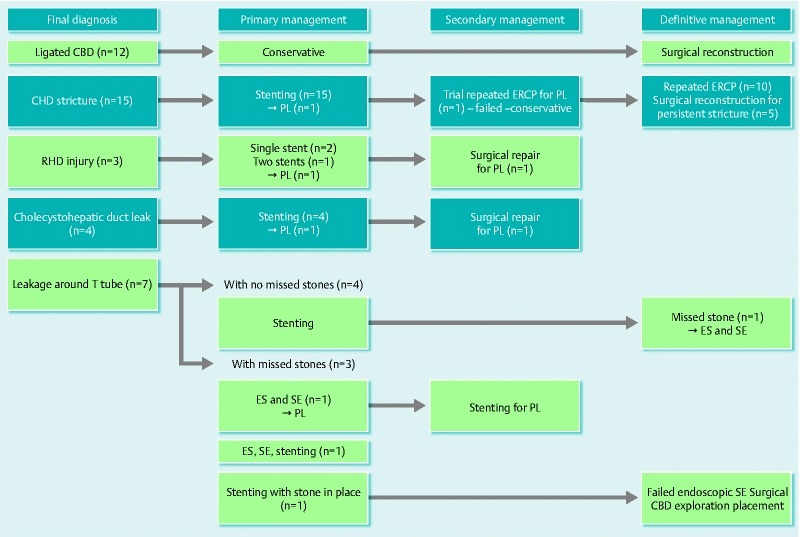
Primary, secondary, and definitive management of biliary leakage according to diagnosis at endoscopic retrograde cholangiopancreatography, excluding patients with cystic duct leak. CBD, common bile duct; CHD, common hepatic duct; PL, persistent leak; RHD, right hepatic duct; ES, endoscopic sphincterotomy; SE, stone extraction.
Diagnostic ERCP was successful in 108 patients (97.3 %) and successfully identified the site of leakage in 107 patients (96.4 %). Cholangiography was not possible in 3 patients in the OC group because of failed cannulation. In 1 patient, there was no extravasation of contrast material; he underwent ERCP 1 month after OC, and a short stent was placed to ensure proper drainage.
ERCP diagnosed major BDI in 27 patients (38.6 %) in the OC group and in 3 patients (7.9 %) in the LC group (P = 0.001). On multivariate analysis, the only significant factor that influenced the occurrence of major BDI was the type of cholecystectomy (Table 5).
Table 5. Univariate and multivariate analyses of different factors influencing the development of major bile duct injury.
| Minor BDI | Major BDI | Univariate P value | Multivariate P value | |
| Cholecystectomy – ERCP interval, days | 17 ± 19.1 | 34 ± 46.4 | 0.005 | 0.136 |
| Type of cholecystectomy | ||||
| LC | 35 (92.1 %) | 3 (7.95 %) | 0.001 | 0.008 |
| OC | 43 (61.4 %) | 27 (38.6 %) | ||
| Age, years | 46.6 ± 13.3 | 43.9 ± 13.2 | 0.973 | 0.087 |
| Sex | ||||
| Male | 35 (71.4 %) | 14 (28.6 %) | 0.867 | 0.803 |
| Female | 43 (72.9 %) | 16 (27.1 %) | ||
| Referral | ||||
| Private | 46 (68.7 %) | 21 (31.3 %) | 0.27 | 0.885 |
| Government hospital | 17 (70.8 %) | 7 (29.2 %) | ||
| Tertiary referral center | 15 (88.2 %) | 2 (11.8 %) |
BDI, bile duct injury; ERCP, endoscopic retrograde cholangiopancreatography; LC, laparoscopic cholecystectomy; OC, open cholecystectomy.
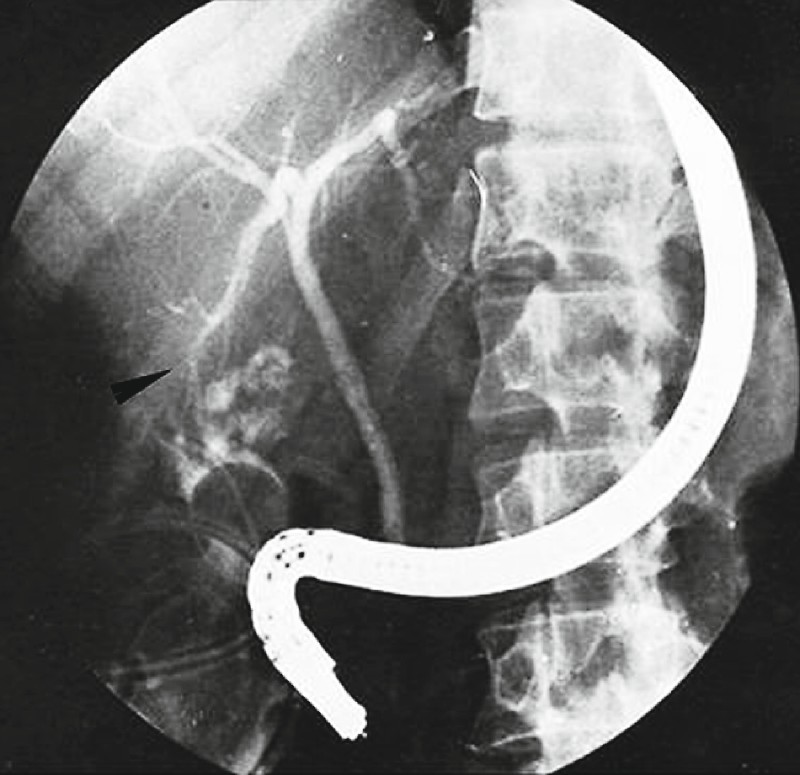
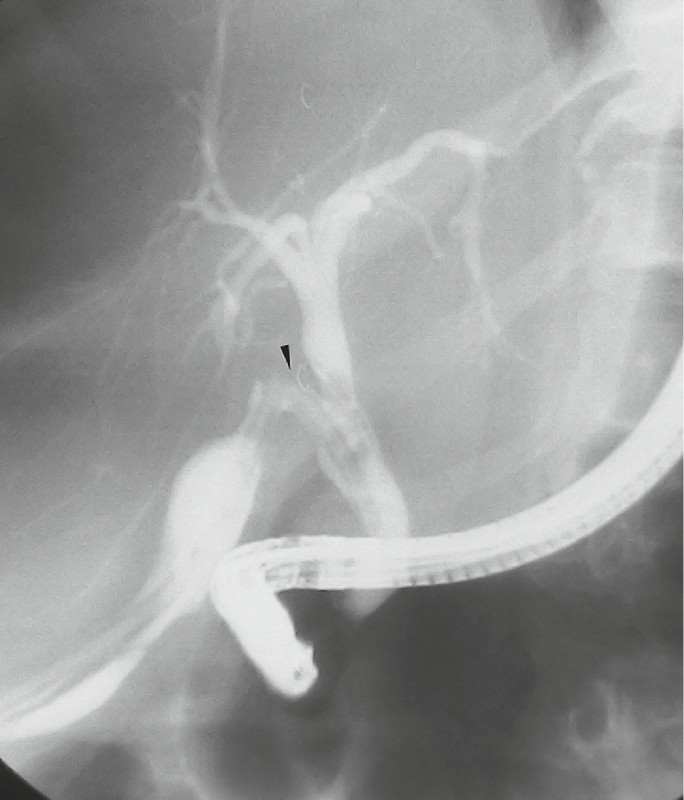
The 12 patients who had a ligated or transected duct with no contrast passing into the proximal biliary tree were referred for definitive surgical reconstruction. CHD strictures (Fig. 2) were managed by stent placement, with 2 patients requiring dilation of the stricture before stent placement. The source of biliary leakage was the RHD (Fig. 3) in 3 patients (2.7 %). This was managed by the insertion of a single stent in 2 patients and double stents in 1 patient.
Fig. 2.
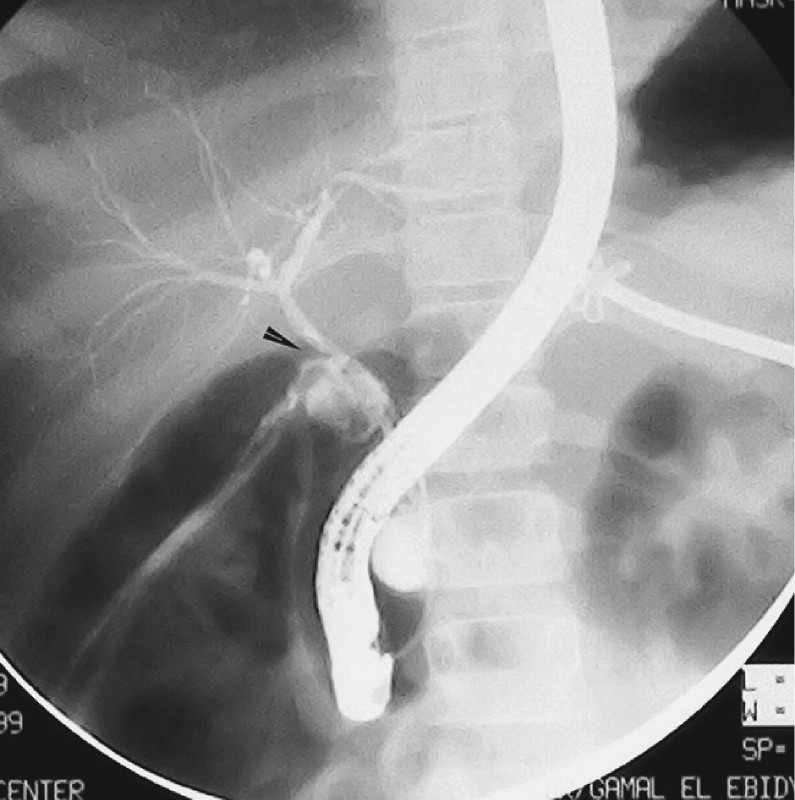
Endoscopic retrograde cholangiopancreatography showing common hepatic duct injury (major bile duct injury), with contrast escaping from the biliary tree (arrowhead). (Note the ultrasound-guided tube drainage.)
Fig. 3.
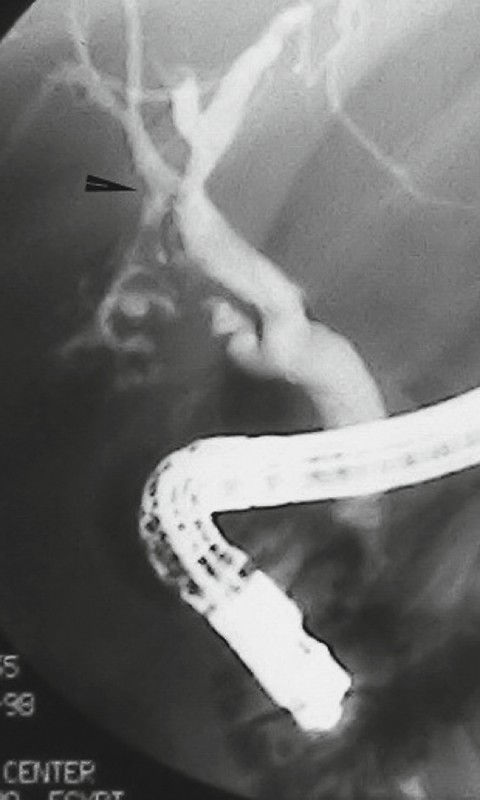
Endoscopic retrograde cholangiopancreatography showing contrast leakage (arrowhead) associated with right hepatic duct injury (major bile duct injury).
The management of cystic duct leaks (Fig. 4) is shown in Table 6. Cholecystohepatic duct leaks (Fig. 5) were identified in 4 patients, with a missed CBD stone in 1 patient. All cholecystohepatic leaks were in the LC group and were managed by stent placement.
Fig. 4.
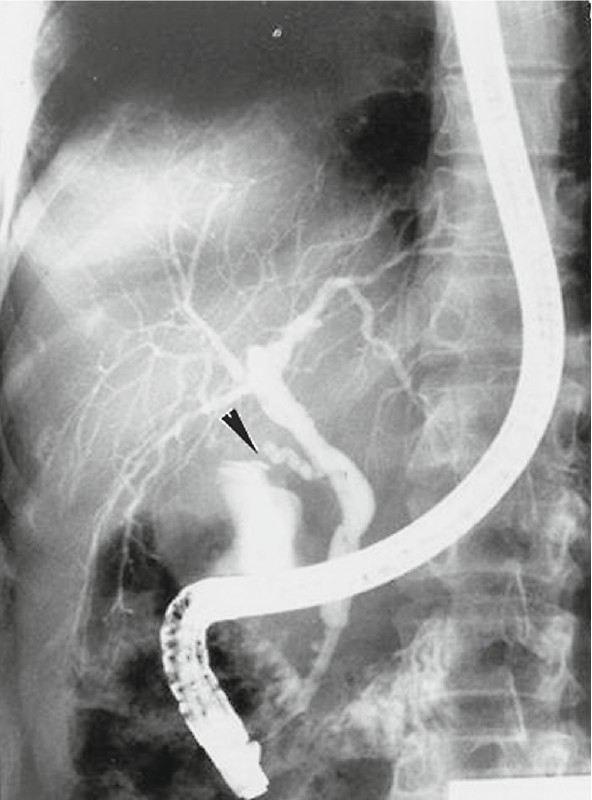
Endoscopic retrograde cholangiopancreatography showing cystic duct leak (arrowhead) (minor bile duct injury).
Table 6. Cystic duct leak management and success rate.
| Cystic duct leak with missed stone (n = 16) | Cystic duct leak with no missed stone (n = 50) | |||
| Primary management | Stent (n = 5) | ES and SE (n = 7) | ES, SE, and stent (n = 4) | Stent (n = 50) |
| Primary management success rate | 100 % | 5 (71.4 %) | 100 % | (49) 98 % |
| Complications | 0 | Persistent leak (n = 2) | 0 | Mild pancreatitis (n = 2) → conservativePersistent leak (n = 1) |
| Secondary management | Stent for persistent leak (n = 2) | Longer stent for persistent leak (n = 1) | ||
| Overall endoscopic success rate | 100 % | 100 % | ||
| Definitive management procedures | ES and SE (n = 5) | |||
| Number of ERCP procedures | ||||
| Mean | 2 ± 0 | 1.6 ± 1 | 1.5 ± 0.6 | 1.8 ± 0.5 |
| Median (range) | 2 | 1 (1 – 3) | 1.5 (1 – 2) | 2 (1 – 3) |
| Duration until stoppage of leak, days | ||||
| Median (range) | 3.6 ± 0.5 | 4.3 ± 1.8 | 4.3 ± 1.9 | 3.4 ± 1.1 |
| Mean (SD) | 4 (3 – 4) | 5 (2 – 7) | 3.5 (3 – 7) | 3 (2 – 7) |
ES, endoscopic sphincterotomy; SE, stone extraction; ERCP, endoscopic retrograde cholangiopancreatography.
Fig. 5.
Endoscopic retrograde cholangiopancreatography showing contrast leakage (arrowhead) from the cholecystohepatic duct (minor bile duct injury).
Of 10 patients who presented with a bile leak after OC and T-tube placement, 2 patients had a ligated CBD, and they were referred to surgery. The leak was shown to be from the choledochotomy around the T-tube in 7 patients (6.3 %) (Fig. 6). Management was with stent placement in 4 patients. Cholangiography revealed associated missed stones in the remaining 3 of these 7 patients. They were managed with stent insertion (n = 1), stone extraction and stenting (n = 1), and endoscopic sphincterotomy with stone extraction (n = 1). In the last patient, the source of the leak was the cystic duct in association with a missed stone. The missed stone was extracted, and a stent was placed.
Fig. 6.
Endoscopic retrograde cholangiopancreatography showing contrast leakage (arrowhead) around the T-tube (minor bile duct injury).
Missed CBD stones were identified in 20 patients (19.4 %). They were associated with a cystic duct leak in 16 cases, leakage around the T-tube in 3 cases, and a cholecystohepatic duct leak in 1 case. Missed stones were managed by endoscopic sphincterotomy and stone extraction in 8 patients (7.2 %) and by endoscopic sphincterotomy, stone extraction, and stent placement in 5 patients (4.5 %). Placement of a stent, reaching above the stone, was the preferred initial management in 7 patients (6.3 %), to be followed by stone extraction during stent removal.
Follow-up, adverse effects, secondary and definitive management (Fig. 1, Table 7)
Table 7. Comparison of endoscopic success rates and complications in patients with minor and major bile duct injuries based on ERCP diagnosis.
| Endoscopic treatment | Minor BDI (n = 78) | Major BDI (n = 30) | Failed ERCP (n = 3) | Total (%) (n = 111) |
| Primary management success rate, No. (%) | 73 (93.6 %) | 16 (53.3 %) | 0 | 89 (80.1 %) |
| Complications, No. (%) | ||||
| Persistent leak | 5 (6.4 %) | 2 (6.6 %) | 7 (6.3 %) | |
| Mild pancreatitis | 2 (2.6 %) | 5 (16.6 %) | 7 (6.3 %) | |
| Obstructed stent | 2 (2.6 %) | 2 (6.6 %) | 4 (3.6 %) | |
| Missed diagnosis of CBD stones | 1 (1.3 %) | 1 (0.9 %) | ||
| Cholangitis | 1 (1.3 %) | 1 (0.9 %) | ||
| Sepsis/mortality | 1 (1.3 %) | 1 (33.3 %) | 2 (1.8 %) | |
| Duration until resolution of leak, days | ||||
| Mean (SD) | 3.7 (1.2) | 5.4 (3.1)1 | ||
| Median (range) | 4 (2 – 7) | 4 (3 – 15) | ||
| Secondary management procedures | ||||
| Endoscopic | 4 | 12 | ||
| Surgical | 1 | 1 | ||
| Overall endoscopic success rate, No. (%) | 77 (98.7 %) | 16 (53.3 %)3 | 93 (83.7 %) | |
| Number of ERCP sessions required | ||||
| Mean (SD) | 1.9 (0.7) | 2.4 (1) | ||
| Median (range) | 2 (1 – 4) | 2 (1 – 4) | ||
| Definitive management procedures | ||||
| Endoscopic | 6 | |||
| Surgical | 2 | 17 |
ERCP, endoscopic retrograde cholangiopancreatography; BDI, bile duct injury.
P = 0.012.
Failed to control bile leak.
P < 0.0001.
Patients in whom diagnostic ERCP failed
Endoscopic management was not feasible in 15 patients (13.5 %) because of failed cannulation (n = 3) or complete ligation of the CBD (n = 12). These patients were referred for surgical reconstruction (definitive management).
Patients with major bile duct injury
Initial endoscopic management with stenting resolved the leakage in 14 of 15 patients (93.4 %). In 1 patient, the leak persisted despite repeated endoscopy and the placement of a stent through a choledochoduodenal fistula, and this patient was referred for surgical reconstruction. The remaining 14 patients underwent an endoscopic treatment regimen. On long-term follow-up, 4 of the 14 patients (28.6 %) were referred for surgical reconstruction because of a poor response to endoscopic treatment. Mild pancreatitis developed in 2 patients (13.4 %).
Mild pancreatitis developed in 2 patients with RHD injuries. The third patient’s condition did not improve, and operative repair of the injured duct with the stent in place was required. All 3 patients had their stents removed after 2 months, with an intact biliary system on cholangiography.
Patients with minor bile duct injury
In 1 of 4 patients in whom a cholecystohepatic duct leak was diagnosed, leakage persisted for 5 days after ERCP. This patient underwent exploration and control of the leaking point, and drainage was performed with subsequent resolution of the leak.
Of the 4 patients with an established diagnosis of bile leakage around the T-tube with no missed stones, 2 had their stents removed after 2 months. A missed stone was noticed and extracted during stent removal in the third patient. The leak resolved 4 days after stent insertion in the fourth patient, who was referred for ERCP 28 days after the initial surgery. Sepsis was already irreversible, and he died 18 days after ERCP.
On initial endoscopy, 3 patients had missed stones. On follow-up, the patient who underwent endoscopic sphincterotomy and stone extraction had a persistent leak and required stenting. The leakage stopped after 6 days, and the stent was removed after 2 months. On X-ray films, the stent was found to have migrated in 1 patient who underwent stone extraction and stent placement. The third patient who underwent stent placement without stone extraction underwent another 2 ERCP procedures in an attempt to extract the stone endoscopically, which failed. He underwent surgery 14 months later and the CBD was explored, with stone extraction and T-tube placement.
Cystic duct leak (Table 6)
Overall, endoscopic management was successful in all patients with cystic duct leaks. Primary management was successful in 63 patients (95.5 %), with 3 patients requiring a longer stent. The median time required for disappearance of a leak was 3 days (mean, 3.6; range, 2 – 7). Table 6 shows the different approaches for managing cystic duct leaks, their initial success rates, their adverse effects, including persistent leak, and the number of ERCP procedures needed.
Difference between the open cholecystectomy and laparoscopic cholecystectomy groups/minor and major bile duct injuries
Endoscopic therapy stopped leakage in 35 patients (92.1 %) and 58 patients (82.9 %) following LC and OC, respectively, after the exclusion of 3 patients in whom cannulation failed (P = 0.15). Leakage was controlled endoscopically in 77 patients (98.7 %) with minor BDI and in 16 patients (53.3 %) with major BDI (P < 0.001). Leakage stopped earlier in the group with minor BDI after endoscopic treatment (P = 0.01), whereas the numbers of ERCP procedures needed for leak control did not differ significantly between the groups (P = 0.20).
Discussion
Biliary leak is common after cholecystectomy. Minor leaks can be detected by radioactive nuclear scanning in about 10 % to 15 % of patients, and most of them will be clinically insignificant. Significant post-cholecystectomy bile leaks occur in about 0.8 % to 1.1 % of patients 12 13. Clinically detected leaks herald the presence of some sort of BDI 14.
In this study, we relied on the classification proposed in 1996 by Bergman et al. of the Amsterdam Academic Medical Center 5 because it is very helpful for categorizing leaks as minor or major and accurately reporting ERCP results. We considered RHD leak as a major BDI, despite its not being included in the original classification, in accordance with Hii et al. 8. Also, we considered leakage at the site of choledochotomy after T-tube placement, not associated with stricture, to be a minor BDI.
Early in the 1990 s, bile leaks were usually managed conservatively; if no improvement was noted, laparotomy and abdominal drainage were performed. With the advent of minimally invasive techniques like ultrasound-guided percutaneous tube drainage and ERCP, the management protocol changed profoundly 15. This change was even more evident as laparoscopic techniques progressed, especially intracorporeal suturing, which allowed the early control of bile leakage from slipped clips or minor bile duct injuries discovered in the early postoperative period 15.
In this study, we included only patients with proven, clinically significant bile leak who were referred to our endoscopy unit after either OC or LC. There were more OC patients than LC patients (2 : 1 ratio). The ratio is similar to that in two large series reported from countries with similar economic circumstances 7 16. This series included 17 patients whose index operations were performed at our institute. All except two operations were LCs; the first of these was open from the start for suspected gallbladder perforation, and the second was converted because of gallbladder empyema that obscured the biliary anatomy.
To our knowledge, this is the first study to compare OC and LC in a subset of patients to investigate differences in the underlying injuries. It is well known that the incidence of BDI has risen with the advent of LC. Many reports quote a BDI incidence for OC in the range of 0.1 % to 0.2 %, whereas it has been in the range of 0.4 % to 0.7 % since the introduction of LC 2 17 18. In this study, the nature of the BDIs differed significantly between the groups. We can state that persistent bile leakage after OC is much more dangerous, with a high possibility of underlying major BDI (P = 0.001).
In the current study, the median time interval from surgery to ERCP was significantly shorter for the LC group (5 days), which is similar to the time in many reports on biliary leakage following LC 3 19. In series in which most of procedures are OCs, this time interval is much longer and also similar to our result 7 16. It reflects the low threshold for tolerating bile leakage following LC, leading to early referral.
The management of post-cholecystectomy injuries in our center is based on a multidisciplinary team approach. Broadly, the steps for management are (1) drainage of significant bilomas, (2) evaluation of the biliary anatomy, and (3) a decision to have the patient undergo endoscopic treatment or surgical treatment. The choice of endoscopic or surgical treatment usually depends on the nature and extent of the injury. Endoscopic treatment has almost replaced surgery for minor BDIs, such as cystic duct leaks and mild biliary strictures 20.
Before ERCP, imaging studies detected collections in 55 % of patients, and ultrasound-guided tube drains were used in 35 % of patients. Abdominal ultrasound was the initial investigation of choice. It is safe, and it accurately screens collections or ascites. During the period of this study, MRCP was increasingly used to evaluate the biliary tree after abdominal ultrasound and before ERCP. The main reasons are the noninvasive nature of MRCP and its diagnostic accuracy 21. ERCP is reserved for patients with preserved biliary tree continuity.
As in many other studies, cystic duct leak was the most common cause of post-cholecystectomy biliary leakage, accounting for about 60 % of cases 3 7 14 19. Cystic duct leaks can result from slipped clips or ligatures, thermal injuries proximal to clips, or blowout (e. g., because of missed CBD stones) 14. Major BDI was identified in 28 % of patients, which is less than the rate of more than 40 % recently reported by Singh et al. 22. They described their experience of 85 cases with post-cholecystectomy biliary leakage and found that 37.6 % of patients had a ligated CBD and 7.5 % had a middle CBD stricture. Their study did not compare patients who underwent OC (61 %) with those who underwent LC (39 %). Such a comparison in the current study showed an increased incidence of major BDI among patients undergoing OC and presenting with postoperative bile leakage. We cannot state a clear cause for this result; however, it may be explained by looking the other way around. Minor leaks are much less common with OC, in which ligatures or even sutures are easily taken to control difficult cystic ducts.
The success rate of endoscopic therapy in controlling bile leak is reported to be in the range of 66 % to 100 %. Different techniques are described in the literature, including endoscopic sphincterotomy, stent placement, and nasobiliary drains. Endoscopic sphincterotomy has a higher complication rate, while nasobiliary drains are poorly tolerated by patients 14. Early in our experience, endoscopic sphincterotomy in two patients with cystic duct leaks and no missed stones did not result in rapid control of the leak, so stenting became our first option. Patients with missed stones were managed with endoscopic sphincterotomy and stone extraction alone if the leak appeared minimal, or with a combination of endoscopic sphincterotomy, stone extraction, and stent placement if the leak appeared to be significant during cholangiography or if the patient’s condition required rapid control of the leak. Our routine practice is to place 10-Fr stents, bypassing the site of the leak if possible. With this approach, we have reached a success rate of 97 %.
According to the results of this series, we would suggest MRCP early in the course of managing bile leakage or suspected BDIs, especially following OC or converted LC. We think it should precede ERCP, which is invasive, may be complicated, or prove useless. Endoscopic therapy is successful in the majority of patients with minor BDIs and has accepted success rates in major BDIs with the exception of complete cutoff or tight strictures, for which surgery is the best treatment.
Footnotes
Competing interests: None
References
- 1.Fathy O, Wahab M A, Hamdy E. et al. Post-cholecystectomy biliary injuries: one center experience. Hepatogastroenterology. 2011;58:719–724. [PubMed] [Google Scholar]
- 2.Lau W Y, Lai E C. Classification of iatrogenic bile duct injury. Hepatobiliary Pancreat Dis Int. 2007;6:459–463. [PubMed] [Google Scholar]
- 3.Ryan M E, Geenen J E, Lehman G A. et al. Endoscopic intervention for biliary leaks after laparoscopic cholecystectomy: a multicenter review. Gastrointest Endosc. 1998;47:261–266. doi: 10.1016/s0016-5107(98)70324-4. [DOI] [PubMed] [Google Scholar]
- 4.Strasberg S M, Hertl M, Soper N J. An analysis of the problem of biliary injury during laparoscopic cholecystectomy. J Am Coll Surg. 1995;180:101–125. [PubMed] [Google Scholar]
- 5.Bergman J J, van den Brink G R, Rauws E A. et al. Treatment of bile duct lesions after laparoscopic cholecystectomy. Gut. 1996;38:141–147. doi: 10.1136/gut.38.1.141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Neuhaus P, Schmidt S C, Hintze R E. et al. Classification and treatment of bile duct injuries after laparoscopic cholecystectomy [in German] Chirurg. 2000;71:166–173. doi: 10.1007/s001040051033. [DOI] [PubMed] [Google Scholar]
- 7.Singh V, Singh G, Verma G R. et al. Endoscopic management of postcholecystectomy biliary leakage. Hepatobiliary Pancreat Dis Int. 2010;9:409–413. [PubMed] [Google Scholar]
- 8.Hii M W, Gyorki D E, Sakata K. et al. Endoscopic management of post-cholecystectomy biliary fistula. HPB (Oxford) 2011;13:699–705. doi: 10.1111/j.1477-2574.2011.00353.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Fatima J, Barton J G, Grotz T E. et al. Is there a role for endoscopic therapy as a definitive treatment for post-laparoscopic bile duct injuries? J Am Coll Surg. 2010;211:495–502. doi: 10.1016/j.jamcollsurg.2010.06.013. [DOI] [PubMed] [Google Scholar]
- 10.Murr M M Gigot J F Nagorney D M et al. Long-term results of biliary reconstruction after laparoscopic bile duct injuries Arch Surg 1999134604–609.; discussion 609 – 610 [DOI] [PubMed] [Google Scholar]
- 11.Lubikowski J, Post M, Bialek A. et al. Surgical management and outcome of bile duct injuries following cholecystectomy: a single-center experience. Langenbecks Arch Surg. 2011;396:699–707. doi: 10.1007/s00423-011-0745-3. [DOI] [PubMed] [Google Scholar]
- 12.Trondsen E, Ruud T E, Nilsen B H. et al. Complications during the introduction of laparoscopic cholecystectomy in Norway. A prospective multicentre study in seven hospitals. Eur J Surg. 1994;160:145–151. [PubMed] [Google Scholar]
- 13.Barkun A N, Rezieg M, Mehta S N. et al. Postcholecystectomy biliary leaks in the laparoscopic era: risk factors, presentation, and management. McGill Gallstone Treatment Group. Gastrointest Endosc. 1997;45:277–282. doi: 10.1016/s0016-5107(97)70270-0. [DOI] [PubMed] [Google Scholar]
- 14.Rauws E A, Gouma D J. Endoscopic and surgical management of bile duct injury after laparoscopic cholecystectomy. Best Pract Res Clin Gastroenterol. 2004;18:829–846. doi: 10.1016/j.bpg.2004.05.003. [DOI] [PubMed] [Google Scholar]
- 15.Ahmad F, Saunders R N, Lloyd G M. et al. An algorithm for the management of bile leak following laparoscopic cholecystectomy. Ann R Coll Surg Engl. 2007;89:51–56. doi: 10.1308/003588407X160864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ghazanfar S, Qureshi S, Leghari A. et al. Endoscopic management of postoperative bile duct injuries. J Pak Med Assoc. 2012;62:257–262. [PubMed] [Google Scholar]
- 17.Adamsen S, Hansen O H, Funch-Jensen P. et al. Bile duct injury during laparoscopic cholecystectomy: a prospective nationwide series. J Am Coll Surg. 1997;184:571–578. [PubMed] [Google Scholar]
- 18.Flum D R, Cheadle A, Prela C. et al. Bile duct injury during cholecystectomy and survival in medicare beneficiaries. JAMA. 2003;290:2168–2173. doi: 10.1001/jama.290.16.2168. [DOI] [PubMed] [Google Scholar]
- 19.Kaffes A J, Hourigan L, De Luca N. et al. Impact of endoscopic intervention in 100 patients with suspected postcholecystectomy bile leak. Gastrointest Endosc. 2005;61:269–275. doi: 10.1016/s0016-5107(04)02468-x. [DOI] [PubMed] [Google Scholar]
- 20.Karvonen J, Gullichsen R, Laine S. et al. Bile duct injuries during laparoscopic cholecystectomy: primary and long-term results from a single institution. Surg Endosc. 2007;21:1069–1073. doi: 10.1007/s00464-007-9316-7. [DOI] [PubMed] [Google Scholar]
- 21.Khalid T R, Casillas V J, Montalvo B M. et al. Using MR cholangiopancreatography to evaluate iatrogenic bile duct injury. AJR Am J Roentgenol. 2001;177:1347–1352. doi: 10.2214/ajr.177.6.1771347. [DOI] [PubMed] [Google Scholar]
- 22.Singh V K Khashab M A Okolo P I 3rd et al. ERCP or laparoscopic exploration for the treatment of suspected choledocholithiasis? Arch Surg 2010145796; author reply 796 [DOI] [PubMed] [Google Scholar]


