Abstract
Momentary intervention has been proposed as a cost-effective, generalizable, and ecologically valid method to increase the efficiency of face-to-face cognitive– behavioral therapy (CBT). The purpose of the current pilot study was to evaluate the efficacy of a six-session palmtop computer-assisted Group CBT for generalized anxiety disorder (GAD) (CAGT6) in comparison with a six-session Group CBT for GAD without the computer (CBGT6) and typical (12 session) Group CBT for GAD (CBGT12) in a randomized controlled trial. Thirty-four individuals with a primary diagnosis of GAD were randomized to one of the three conditions and completed measures of GAD and anxiety before therapy, after therapy, and at 6-, and 12-month follow-ups. Results indicated that CAGT6 was superior to CBGT6 at posttreatment, but not significantly different from CBGT12. At 6- and 12-month follow-ups, CAGT6 was neither significantly different from CBGT6, nor from CBGT12. Percentages of individuals achieving reliable change on two of the three GAD measures favored CAGT6 over CBGT6 at posttreatment, suggesting promise for the added value of the mobile technology.
Keywords: ecological momentary intervention, computer-assisted therapy, group therapy, generalized anxiety disorder (GAD)
Generalized anxiety disorder (GAD) is one of the most frequently diagnosed anxiety disorders with a lifetime prevalence estimated at about 5.7% (Kessler & Wang, 2008). Individuals diagnosed with GAD tend to have significant role impairment comparable with what would be found with chronic medical conditions such as arthritis and autoimmune disease (Alonso et al., 2011). In addition, GAD tends to have a chronic course and its symptoms persist unless successfully treated (Yonkers, Bruce, Dyck, & Keller, 2003). Thus, the development and testing of new GAD treatments is important.
Cognitive–behavioral therapy (CBT) has been demonstrated to be efficacious in diminishing symptoms of GAD as well as those of comorbid disorders (Newman et al., 2011; Newman, Przeworski, Fisher, & Borkovec, 2010). However, CBT for GAD is costly and time-consuming (Newman, 2000). A 1995 estimate of the cost of a typical course of individual therapy for GAD was about $2,181 per client and on average required 23.2 billable hours of therapist contact (Turner, Beidel, Spaulding, & Brown, 1995). As a result, researchers have begun to explore the efficacy of cost-effective alternatives.
One means that has been proposed to help defray treatment costs has been computer-delivered treatments. Computer-assisted interventions for GAD, including those delivered via mobile phone technologies, may save as much as a thousand dollars per client in costs (Newman, Consoli, & Taylor, 1999; Newman, Kenardy, Herman, & Taylor, 1996). Additionally, such approaches may reduce barriers to treatment, such as months of weekly travel to therapy sessions for rural individuals and for those who live a great distance from a trained cognitive–behavioral therapist (Griffiths, Lindenmeyer, Powell, Lowe, & Thorogood, 2006; Newman, Erickson, Przeworski, & Dzus, 2003). They may also reduce the difficulties associated with scheduling months of weekly sessions during office hours (Titov, 2007). Computer-assisted therapies may also increase the number of clients that trained cognitive–behavioral therapists can service by reducing the necessary therapist– client contact time for efficacious treatment (Andrews & Erskine, 2003; Marks, Kenwright, McDonough, Whittaker, & Mataix Cols, 2004; Newman, Consoli, & Taylor, 1997). Thus, computer-assisted therapy may reduce waiting lists for trained therapists and permit a greater number of clients to have access to CBT.
To date, several variations of computer treatment programs have been developed. One such variation is in the amount of therapist contact that clients receive. Whereas some treatments have been tested as completely or predominantly self-help, others have been used as an adjunct to therapist-delivered treatment (Newman et al., 2003; Newman, Kenardy, Herman, & Taylor, 1997; Newman, Szkodny, Llera, & Przeworski, 2011a, 2011b; Pallavicini, Algeri, Repetto, Gorini, & Riva, 2009). One advantage of clinician-assisted computer-therapy over predominantly self-help versions is that the involvement of a clinician tends to decrease the number of dropouts (Newman et al., 2011b). However, a disadvantage of such treatment is that it is more costly than treatments that are predominantly self-help. A potential alternative to mitigate costs would be to conduct the clinician-assisted portion in brief groups. It has been suggested that group computer-assisted therapy could decrease the cost of therapy for GAD by approximately half, thereby increasing client access to therapy (Newman, Consoli, & Taylor, 1997). Thus, brief group treatments have the potential to reduce the rate of dropouts incurred by self-help therapies without substantially increasing their cost.
In addition to variations in amount of therapist contact, computer therapies have varied in terms of the devices used and the mode of delivery. These variants have included Internet-based treatments delivered by desktop computers and ambulatory treatments delivered by smartphones, cellphones, or palmtop computers. (Newman, Kenardy, et al., 1997; Newman et al., 2011a, 2011b; Pallavicini et al., 2009). To date most of the controlled trials conducted with regard to GAD have involved Internet treatments delivered by desktop computers. Such studies have shown that a predominantly self-help Internet treatment (Paxling et al., 2011), a clinician-assisted Internet treatment (Titov et al., 2009), and a technician-assisted Internet treatment (Robinson et al., 2010) led to greater gains than a wait-list. An additional uncontrolled study found that an Internet treatment was effective when delivered in the context of primary practice (Mewton, Wong, & Andrews, 2012).
Although most researchers have focused on desktop-delivered Internet treatments, rapidly increasing technological advances have established prospects for creating more mobile interventions. Such interventions have the advantage of being available to clients in real time as well as when and where treatment opportunities might be most desired. The accessibility of treatments used via mobile devices has the potential to increase their ecological validity and generalizability because such accessibility increases the probability that interventions will occur in clients’ everyday lives.
When combined with mobile technology, however, Internet treatments have limitations. For example, they tend to involve text on a webpage, rather than interactive exercises. Such simple text is easier to read when accessed from a desktop computer than from a smartphone. It is also the case that most Internet site-based interventions are not formatted for use on a smartphone, and therefore, such sites may load slowly or not at all on small devices. Reliance on an Internet connection to a cellphone also risks the possibility of hitting a dead zone where connectivity is slow or unavailable. Slow or variable Internet connections on smartphones may also interfere with the use of exercises that involve a timed component, such as exercises that provide feedback regarding the speed of an individual’s paced breathing. Thus the use of portable devices to access Internet intervention programs can be tedious and unreliable.
Although degree of access to the Internet is likely increasing, in 2010 only 35% of individuals who had cellphones had accessed the Internet on their phone and 26% of individuals did not have Internet access in their homes (Pew Internet & American Life Project, 2010); therefore, such interventions are not accessible to all individuals and may not be optimal for dissemination. Moreover, the amply documented “digital divide” can be a major obstacle in accessing Internet-based services among most ethnic minority groups, low socioeconomic status individuals, rural communities, and seniors (Pew Internet & American Life Project, 2010). Reliance on availability of an Internet connection also risks incurring roaming charges when attempting connectivity outside of the range of a particular cellphone company. Moreover, most smartphone plans bill Internet access according to usage, which may add a sizable cost to the individual and may act as a deterrent to usage.
In contrast, software-based interventions offered on a small handheld computer or cellphone can be specifically formatted to be used on the device and can therefore be made more reliably and quickly accessible in all locations. Such interventions can make use of interactive exercises, including exercises that provide feedback to the individual, such as feedback on the appropriate pace of breaths in diaphragmatic breathing and the use of cognitive restructuring. Additionally, self-monitoring may be conducted in an ecologically valid manner by scheduling alerts, which go off periodically throughout the day. Such alerts can also be used to accurately track client symptoms and to prompt homework practice. In addition, personalized interactions could be created through software that takes into account client entries and responses to questions, thereby creating the impression of individualized attention. Another advantage of software-based portable therapy devices is that they allow clients the complete freedom to decide when, where, and for how long they want to make use of a device, thus encouraging a greater sense of control and autonomy and greater opportunities for generalization.
Only one small controlled study has examined a clinician-assisted mobile treatment for GAD. This study compared clinician delivered biofeedback and virtual reality (VR) plus VR and biofeedback delivered by a mobile phone to clinician-delivered biofeedback and VR plus VR delivered by a mobile phone without biofeedback, and to a wait-list control condition (Pallavicini et al., 2009). Four individuals were randomly assigned to each condition. Results showed that the inclusion of mobile biofeedback led to improvement on more measures than the other two conditions. Thus, this study suggested that ambulatory biofeedback augmented the impact of ambulatory VR with stationary biofeedback and VR. In the late 1990s, we began to work on a palmtop computer-assisted treatment for GAD that would be ambulatory and interactive (Newman, 1999; Newman et al., 1999). Our software-based program involved prompts for self-monitoring and homework, as well as tailored guidance in the use of various CBT strategies. The program sought to reinforce the use of techniques in clients’ everyday lives as a means to help engage them in active coping at all times. Our ultimate goal with this program was to increase the efficiency, cost-effectiveness, and dissemination of CBT for GAD through decreased therapist contact, increased homework compliance, and increased generalization of the treatment by prompting greater use of cognitive– behavioral techniques in the real world.
We theorized that an ambulatory treatment program used in conjunction with brief group therapy might help to generalize the impact of the treatment beyond what is the case for treatment without the computer program. Thus, we hoped that there would be added value to a program that provided ecological momentary intervention (Heron & Smyth, 2010). Although we have published several case studies on the impact of this program for GAD (Newman, 1999; Newman, Consoli, & Taylor, 1999) and for social phobia (Przeworski & Newman, 2004), the current study involves the first controlled trial of the treatment for GAD. The purpose of the current pilot study was to evaluate efficacy of a six-session palmtop computer-assisted Group CBT for GAD (CAGT6) in comparison with a six-session Group CBT for GAD without the computer (CBGT6) and typical (12-session) Group CBT for GAD (CBGT12). We predicted that CAGT would be superior to CBGT6 and not significantly different from CBGT12 at post assessment but that by 6- and 12-month follow-ups, there would be no differences between the comparison conditions.
Method
Participants
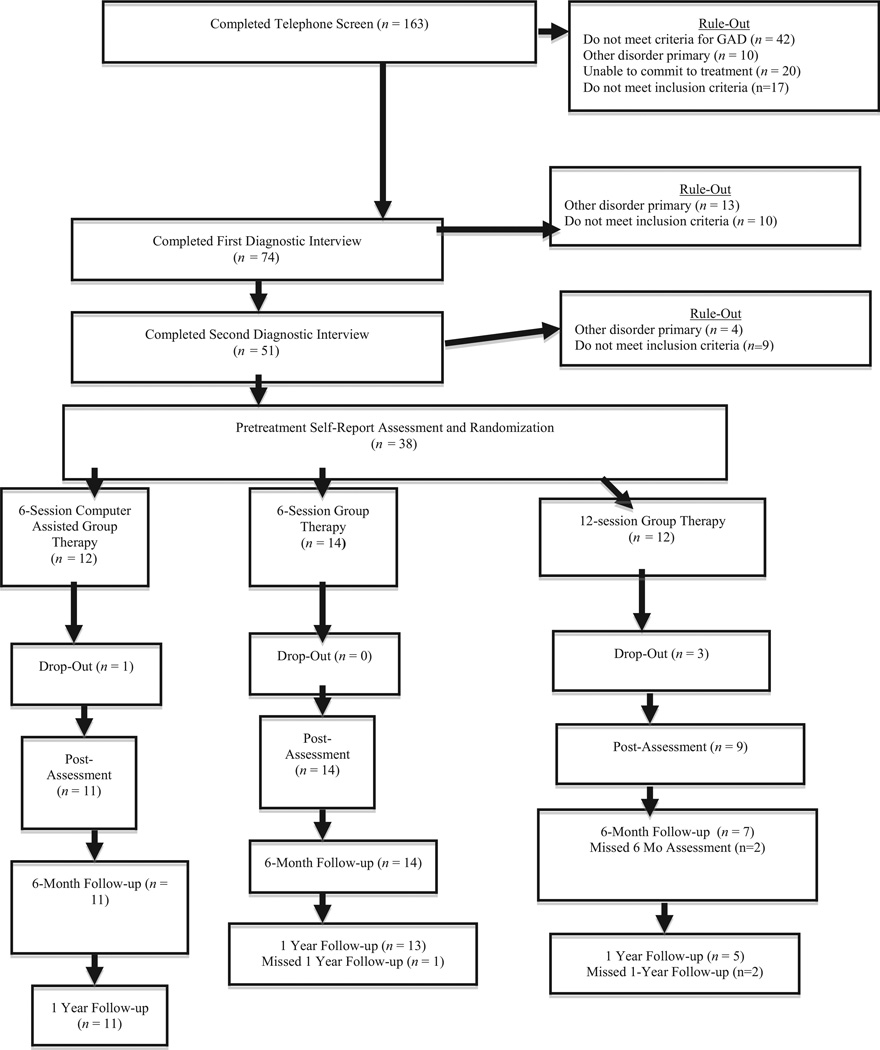
Participants responded by telephone to flyers posted throughout the local community or referrals from mental health practitioners. They received an initial phone screen that ruled out those who did not meet inclusion criteria. They then received two independent structured interviews administered by advanced graduate students who were blind to study assignment. Thirty-four individuals with a principal diagnosis (Diagnostic and Statistical Manual of Mental Disorders, fourth edition [DSM–IV; American Psychiatric Association, 2000]) of GAD (based on two independent interviews using the Anxiety Disorders Interview Schedule for DSM–IV or ADIS-IV) were included in the final sample (see Figure 1 for CONSORT flowchart). Admission criteria included agreement from two separate diagnostic interviews on a principal diagnosis of DSM–IV GAD, a Clinician’s Severity Rating for GAD (part of the ADIS for DSM–IV; Brown, Di Nardo, & Barlow, 1994) of four (moderate) or greater, absence of concurrent psychotherapy or past adequate dosage of CBT (at least eight sessions focused on cognitive and behavioral techniques), current stable dose of psychotropic medication (for at least 4 weeks) or medication-free, willingness to maintain stability in medication use during the 14-week therapy period with their physician’s approval, no medical contributions to the anxiety, absence of substance abuse, psychosis, and organic brain syndrome, and between 18 and 65 years of age. Fifty percent of participants were recruited and treated at Stanford University Medical Center (n = 17) and 50% (n = 17) were recruited and treated from the community of Penn State University with participants roughly equally distributed among the therapy conditions. Baseline participant characteristics are described in Table 1.
Figure 1.
Flow of participants through each stage of the study.
Table 1.
Pretreatment Characteristics Divided by Group
| Pretreatment characteristic |
CAGT6 (n = 11) | CBGT6 (n = 14) | CBGT12 (n = 9) | Total sample (n = 34) |
|---|---|---|---|---|
| Age* | 42.45 (10.95) | 45.19 (12.61) | 37.11 (12.57) | 42.08 (12.15) |
| College degree or higher | 72.7% (8/11) | 57.1% (8/14) | 88.9% (8/9) | 70.59% (24/34) |
| White ethnicity | 90.9% (10/11) | 92.3% (12/13) | 87.5 (7/8) | 90.6% (29/32) |
| Married | 54.5% (6/11) | 71.4% (10/14) | 66.7% (6/9) | 64.7% (22/34) |
| Female | 54.5% (6/11) | 50% (7/14) | 77.8% (7/9) | 58.8% (20/34) |
| Psychotropic medications | 36.4% (4/11) | 42.9% (6/14) | 33.3% (3/9) | 38.2% (13/34) |
| Any comorbid disorder | 72.7% (8/11) | 57.1% (8/14) | 77.8% (7/9) | 67.6% (23/34) |
| Agoraphobia | 18.2% (2/11) | 7.1% (1/14) | 0% | 8.8% (3/34) |
| Panic disorder | 18.2% (2/11) | 21.4% (3/14) | 0% | 14.7% (5/34) |
| Bipolar II | 0% | 0% | 11.1% (1/9) | 2.9% (1/34) |
| Dysthymia | 9.1% (1/11) | 0% | 0% | 2.9% (1/34) |
| MDD | 36.4% (4/11) | 28.6% (4/14) | 11.1% (1/9) | 26.5% (9/34) |
| OCD | 9.1% (1/11) | 0% | 0% | 2.9% (1/34) |
| PTSD | 9.1% (1/11) | 7.1% (1/14) | 0% | 5.9% (2/34) |
| Social phobia | 18.2% (2/11) | 57.1% (8/14) | 33.3% (3/9) | 38.2% (13/34) |
| Somatization/Somatiform | 9.1% (1/11) | 0% | 11.1% (1/9) | 5.9% (2/34) |
| Specific phobia | 9.1% (1/11) | 35.7% (5/14) | 0% | 17.6% (6/34) |
Note. CAGT6 = six session computer-assisted CBT for GAD; CBGT6 = six-session group CBT for GAD without the computer; CBGT12 = 12 session group CBT for GAD without the computer; MDD = major depressive disorder; OCD = obsessive compulsive disorder; PTSD = post-traumatic stress disorder.
Numbers represent mean with standard deviation in parentheses.
Procedure
Advanced clinical psychology graduate students trained to reliability in diagnostic interviewing conducted a 30-minute phone interview to determine likely diagnostic suitability. The phone interview included a description of the study and screening for basic symptoms of GAD, symptoms of common comorbid disorders, exclusion criteria, and availability for therapy. For those not ruled out during the phone screen, interviewers administered in person the ADIS-IV (Brown et al., 1994), which includes the Hamilton Anxiety Rating Scale (HARS; Hamilton, 1959). Data suggest that inconsistent reporting on the part of the client is the most common contributing factor to low reliability in the diagnosis of GAD (Brown, Di Nardo, Lehman, & Campbell, 2001). Therefore, a second ADIS-IV was administered within 2 weeks, to reduce the likelihood of false-positive cases. The second ADIS was administered only to those not ruled out during the first ADIS interview. Pretreatment diagnoses, both primary and comorbid, were based on consensus between the independent structured interviewers, both of whom were unaware of study assignment. Kappa agreement for the presence of GAD was .78. There was also good to excellent agreement on the presence of comorbid diagnoses with kappa coefficients ranging from .68 to 1. Once diagnostic assessment was confirmed, participants were randomly assigned to CBGT6, CAGT6 or CBGT12.
Outcome Measures
State Trait Anxiety Inventory–Trait Version
This 20-item scale is used to measure trait anxiety (Spielberger, Gorsuch, Lushene, Vagg, & Jacobs, 1983). Items are rated from 1 (almost never) to 4 (almost always) to indicate how subjects “generally feel.” Internal consistency reliability was shown to be high (in the .80’s and .90’s), and retest reliability was much higher for the trait form (high .70’s) than the state form (from .27 to .54). Good convergent and discriminant validity has also been demonstrated (Spielberger et al., 1983).
Hamilton Anxiety Rating Scale
This 14-item clinician administered scale provides a rating of severity of each overarching anxiety symptom cluster on a scale from 0 (not present) to 4 (very severe/incapacitating) (Hamilton, 1959). Estimates of internal consistency of the HARS range from adequate to good in one study (α = .77–.81) (Moras, di Nardo, & Barlow, 1992) to excellent (α = .92) in another (Kobak, Reynolds, & Greist, 1993). Retest reliability was intraclass correlation (ICC) = .86 across 2 days and interrater reliability ranged from an ICC of .74 to .96 (Bruss, Gruenberg, Goldstein, & Barber, 1994). HARS scores show strong convergent (Beck & Steer, 1991; Maier, Buller, Philipp, & Heuser, 1988) and discriminant validity (Kobak et al., 1993). A version with less overlap between anxiety and depressive symptomatology (Riskind, Beck, Brown, & Steer, 1987) was used in conjunction with the ADIS-IV. Interrater reliability was ICC = .87 for the current study.
Penn State Worry Questionnaire
This is a 16-item self-report measure of the frequency and intensity of worry (Meyer, Miller, Metzger, & Borkovec, 1990). Items are rated on a 5-point Likert scale rating the degree to which a particular statement is typical of an individual. Factor analysis indicated that the Penn State Worry Questionnaire (PSWQ) assesses a unidimensional construct with an internal consistency coefficient of .91 (Meyer et al., 1990). High retest reliability (ranging from .74 to .93) was also demonstrated across periods ranging from 2 to 10 weeks (Molina & Borkovec, 1994). The PSWQ has also been shown to distinguish individuals with GAD from individuals with other anxiety disorders (Brown, Antony, & Barlow, 1992). Correlations between the PSWQ and measures of anxiety, depression, and emotional control supported the convergent and discriminant validity of the measure (Brown et al., 1992).
Therapy Conditions
One male postdoctoral fellow and three female graduate students who had already received several years of training in CBT as well as at least 1 year of training in the GAD protocol conducted the therapy at an outpatient clinic. Assignment to therapist was random within restraints of availability and caseload. All therapists received ongoing supervision by the first author for 1 hour each week. Several aspects were common to the three conditions. All treatment was conducted in groups of three to eight clients. Clients in all conditions were provided with a self-help manual at the first therapy session detailing the planned interventions. The manual incorporated what had been distributed to clients as separate handouts in a preceding therapy trial conducted by Borkovec and his colleagues (Borkovec, Newman, Pincus, & Lytle, 2002). These handouts encompassed information regarding anxiety as well as a detailed discussion of the therapeutic components including diaphragmatic breathing, progressive muscle relaxation, self-control desensitization (SCD), applied relaxation, and cognitive therapy. In addition, for those in the computer-therapy condition, the manual incorporated instructions on how to use the palmtop computer to implement each therapy technique in daily living.
All clients received CBT that included the various methods previously developed and tested at Penn State University (Borkovec et al., 2002). These methods included a CBT model and rationale. In addition, they received training in self-monitoring of environmental, somatic, imaginal, and thought (especially worry) cues that trigger anxiety spirals. Such training specifically emphasized increasingly early cue detection. Moreover, they received formal progressive relaxation (modified over sessions from 16 muscle groups, four muscle groups, and four group-recall, and counting; Bernstein, Borkovec, & Hazlett-Stevens, 2000). Later clients received training in cue-controlled and differential relaxation, and applied relaxation training. Hierarchies for SCD were constructed from pretherapy questionnaires and ADIS information, daily self-monitoring, and in-session discussion with the client. Such hierarchies included both external and especially internal cues. The treatment also used cognitive therapy (based on Beck, Emery, & Greenberg, 1985) including identification of cognitive predictions, interpretations, beliefs, and assumptions underlying the threatening nature of events or cues. Cognitive restructuring techniques included logical analysis, examination of evidence supporting automatic thoughts, labeling of logical errors, decatastrophization, and generation of alternative thoughts and beliefs. Clients were taught the importance of early application of these alternatives to daily living. The treatment also included the creation of behavioral experiments to obtain evidence for new beliefs and use of cognitive perspective shifts learned in cognitive therapy during SCD rehearsals. An ultimate additional goal for all of the interventions was to have the client learn to pay attention to and live increasingly in the present moment, given that this psychological experience is the opposite adaptive response to excessive thinking about the future.
In an effort to increase the cost-effectiveness of the treatment developed by Borkovec et al. (2002), it was translated from 14 sessions of individual therapy (first four sessions were 2 hours and subsequent sessions lasted 1.5 hours in the original manual) to either 12 sessions of group therapy (CBGT12: 24 hours total group contact), six sessions of group therapy (CBGT6: 12 hours total group contact), or six sessions of computer-assisted group therapy (CAGT6: 12 hours total group contact), while preserving the most fundamental features of the approach. All three treatment conditions covered the same material and provided clients with the same workbook material. The group sessions were 2 hours in length. By translating the individual therapy to a brief group therapy, we significantly reduced the required therapist contact time from 23 hours per person in the original individual therapy to a maximum of 3 hours per person (assuming a minimum of four people per group). Both CAGT6 and CBT6 groups met once each week for four sessions and then biweekly for the last two sessions. CBT12 groups met weekly for 12 weeks. Clients in CAGT6 were asked to carry the computer with them at all times during the 8 weeks they were in therapy and for 4 weeks after the end of treatment, giving them access to a total of 12 weeks of computer-guided therapy. At the end of 12 weeks, the computers were returned to the experimenter and posttherapy assessment occurred in the 13th week. Follow-up assessments were conducted 6 and 12 months later.
The palmtop computer used in this study was a Hewlett Packard ®, 200LX. It weighs about 312 g (approximately 11 oz), and while folded measures 16 × 2.5 × 8.5 cm3 (6.3 × 3.4 × 1 in.). It unfolds into two sections: a QWERTY keyboard with function keys and a screen (16 lines × 40 characters). The model selected has a random access memory capacity of 1 megabyte, sufficient to house the GAD software as well as to store the data entered by participants. The computer is equipped with a connectivity package that allows a simple plug-in connection to a desktop computer, facilitating the uploading and downloading of data and programs.
The software we developed for this study incorporates the basic principles of CBT for GAD specified by Borkovec et al. (Borkovec et al., 2002). The GAD software entitled The Stress Manager© has several modules described in detail elsewhere (Newman, 1999; Newman et al., 1999). The first module is a “diary only” module designed to obtain participants’ baseline information before treatment. In this module, the computer beeps the client at fixed intervals (8:00 a.m., 12:00 p.m., 4:00 p.m., and 8:00 p.m.) to respond to a series of questions. At 10:00 p.m., the computer prompts clients to enter their average level of anxiety, highest level of anxiety, and percentage of time they spent worrying that day. In this module, clients have no access to the treatment components of the program.
After participants have used the computer in the “diary only” module for 2 weeks, they attend their first psychotherapy group session. At this time the program was advanced to the “recognizing triggers” module and the “therapy module.” The “recognizing triggers” module initiated an intensive 2-day monitoring period during which the computer beeped clients every waking hour and asked them to identify current anxiety cues. The “therapy” module includes the same time-defined assessment prompts found in the “diary only” mode. However, contrary to the “diary only” mode, the assessments are followed by words of encouragement to clients scoring within an appropriate range (e.g., less than 3 in a 0–10 scale of anxiety). Moreover, if participants indicate that their present anxiety is above 3 on a 0–10 scale, they are invited to implement a therapy technique (e.g., “Would you like to practice some relaxation techniques?”) and they can initiate any of the therapy program components at any time by choosing from a menu. The “therapy” program permits access to three sets of modules. The first is a relaxation module that includes six different versions of progressive muscle relaxation, as well as diaphragmatic breathing retraining and pleasant imagery. This provides clients with instruction and feedback on the implementation of each technique. The second module prompts clients to use cognitive therapy and invites participants to logically examine the evidence for their fears, to make probability estimations about the likelihood of a negative outcome, to identify logical errors (such as filtering, black/white thinking, mind-reading, catastrophizing, etc.), and based on which error is chosen, raises questions for clients to ask themselves as a means to restructure their cognitions. The module also offers definitions for each logical error and provides examples of ways to redress faulty logic. Participants are encouraged to use the computer when they are anxious or when they want to practice any of the therapy techniques.
At each therapy session, all raw data that had been entered into the computer was downloaded to a desktop computer and saved for future analyses. The GAD software automatically printed out a summary that included information concerning participants’ average daily level of anxiety, number of acute anxiety episodes, percentage of time spent worrying, as well as the most common cognitive error and the average anxiety difference between pre- and post-relaxation or pre- and post-cognitive therapy. The therapist used this information to gauge client progress.
Results
Baseline Characteristics
At baseline, there were no significant differences between the three conditions on participant age F(2, 32) = 1.20, p = .32, partial η2 = .074; education χ2(2, 34) = 2.9, p = .234, Cohen’s d = .583; ethnicity χ2(2, 32) = .13, p = .937, Cohen’s d = .13; marital status χ2(2, 34) = 0.78, p = .678, Cohen’s d = .31; gender χ2(2, 34) = 1.97, p = .374, Cohen’s d = .48; psychotropic medication status χ2(2, 34) = 0.235, p = .889, Cohen’s d = .17; or the presence of a comorbid disorder χ2(2, 34) = 1.26, p = .533, Cohen’s d = .39. There were also no significant differences between the groups on baseline State Trait Anxiety Inventory–Trait Version (STAI-T) F(2, 32) = 0.36, p = .70, partial η2 = .023; PSWQ F(2, 32) = 0.045, p = .96, partial η2 = .003; and HARS F(2, 27) = 0.15, p = .86, partial η2 = .012.
Main Outcome
Table 2 lists the means and standard deviations of each measure at each assessment point. Similar to other outcome studies (Clark et al., 1999; Kenardy et al., 2003), to reduce the probability of Type I error, we created one outcome variable for symptoms of GAD, using a composite score of the STAI-T, PSWQ, and the HARS. A single composite is considered more valid than any one measure of symptomatology, particularly when combining both observer-rated and client-rated measures (Rosenthal & Rosnow, 2007). This GAD-change measure was created by calculating the percentage of individuals who had achieved reliable change using the formula described by Jacobson and Truax to calculate a reliable change index (RCI; Jacobson & Truax, 1991) across at least two of the three GAD outcome measures (STAI-T, PSWQ, and HARS). RCI reflects the degree of change that occurred beyond the fluctuations of an imprecise measure (McGlinchey, Atkins, & Jacobson, 2002). The following values were used in the RCI formulae in the present study: STAI-T: SD = 6.74, reliability = .84; PSWQ: SD = 7.76, reliability = .91; HARS: SD = 7.39, reliability = .80. Standard deviations represent the standard deviation of the pooled sample at pretherapy assessment, and the reliability estimates represent reported retest reliability coefficients for each measure (Bruss et al., 1994; Meyer et al., 1990; Newman et al., 2010; Spielberger et al., 1983). RCIs at each measurement point were calculated for change relative to pretherapy assessment.
Table 2.
Means and Standard Deviations Across Time
| Condition | Measure | Pretreatment M (SD) |
Posttreatment M (SD) |
6 month follow-up M (SD) |
12 month follow-up M (SD) |
|---|---|---|---|---|---|
| CAGT6 (n = 11) | HARS | 22.06 (7.39) | 10.38 (5.05) | 7.86 (6.23) | 7.36 (6.03) |
| CBGT6 (n = 14) | HARS | 23.18 (8.11) | 12.54 (6.28) | 9.63 (6.38) | 11.14 (8.08) |
| CBGT12 (n = 9) | HARS | 24.33 (6.64) | 15.50 (9/11) | 11.17 (6.17) | 13.2 (8.24) |
| CAGT6 (n = 11) | PSWQ | 69.36 (8.03) | 59.09 (11.43) | 54.70 (11.76) | 55.11 (14.08) |
| CBGT6 (n = 14) | PSWQ | 68.38 (7.87) | 63.54 (9.07) | 56.38 (12.76) | 51.75 (18.08) |
| CBGT12 (n = 9) | PSWQ | 68.89 (8.18) | 61.00 (10.20) | 52.64 (17.97) | 54.40 (15.85) |
| CAGT6 (n = 11) | STAI-T | 53.27 (7.02) | 44.55 (7.93) | 43.80 (8.16) | 41.67 (9.21) |
| CBGT6 (n = 14) | STAI-T | 52.50 (6.42) | 49.17 (7.94) | 47.36 (9.53) | 41.25 (13.30) |
| CBGT12 (n = 9) | STAI-T | 55.00 (7.37) | 47.78 (9.09) | 43.07 (6.92) | 46.20 (12.34) |
Note. CAGT6 = six session computer-assisted CBT for GAD; CBGT6 = six-session group CBT for GAD without the computer; CBGT12 = 12 session group CBT for GAD without the computer; HARS = Hamilton Anxiety Rating Scale; PSWQ = Penn State Worry Questionnaire; STAI-T = State Trait Anxiety Inventory.
Comparison between CAGT6 and CBGT6 on the percentage of individuals who achieved change on at least 2/3 GAD-specific measures (STAI-T, PSWQ, and HARS) at posttreatment showed that CAGT6 was superior to CBGT6, χ2(1, 25) = 4.975, p = .026, Cohen’s d = .997, but not significantly different from CBGT12, χ2(1, 20) = 1.664, p = .197, Cohen’s d = .602. At 6-month follow-up, CAGT6 was neither significantly different from CBGT6, χ2(1, 25) = 1.948, p = .165, Cohen’s d = .581, nor from CBGT12, χ2(1, 18) = .118, p = .731, Cohen’s d = .162. At 1-year follow-up, CAGT6 was neither significantly different from CBGT6, χ2(1, 24) = 2.55, p = .110, Cohen’s d = .69, nor from CBGT12, χ2(1, 17) = .712, p = .399, Cohen’s d = .418.
Although CAGT6 was only significantly superior to CBGT6 at posttreatment, examination of Table 3 shows that the percentages of individuals achieving reliable change on two of the three GAD measures favors CAGT6 over CBGT6 at each time-point and it even appears to do slightly better than CBGT12 at posttreatment and at 1-year follow-up, suggesting promise for the added value of the mobile technology.
Table 3.
Percentage of Participants Achieving Reliable Change
| Treatment | Reliable change 2/3 GAD measures |
Reliable change 2/3 GAD measures |
Reliable change 2/3 GAD measures |
|---|---|---|---|
| Condition | Posttherapy | 6 mo follow-up | 12 mo follow-up |
| CAGT6 | 72.7% (8/11)* | 63.6% (7/11) | 54.5% (6/11) |
| CBGT6 | 28.6% (4/14)* | 35.7% (5/14) | 23.1% (3/13) |
| CBGT12 | 44.4% (4/9) | 71.4% (5/7) | 40% (2/5) |
Note. CAGT6 = six session computer-assisted CBT for GAD; CBGT6 = six-session group CBT for GAD without the computer; CBGT12 = 12 session group CBT for GAD without the computer.
χ2(1, 25) = 4.975, p = .026, GAD measures included the Penn State Worry Questionnaire, Trait version of the State-Trait Anxiety Scale, and the Hamilton Anxiety Rating Scale.
Discussion
This study suggested that brief palmtop computer-assisted group therapy may be an efficacious and cost-effective alternative to standard treatments. At posttherapy, six-session group computer-assisted therapy was not significantly different from 12-session group therapy without a computer and was more efficacious than six-session group therapy without a computer. Therapies did not statistically differ at 6- and 12-month follow-ups. Nonetheless, attrition at these time points reduced our power to find differences where they may have existed. Overall our findings suggest the promise of portable computer-assisted therapy for GAD as a cost-effective and efficient means of providing efficacious CBT with gains largely maintained over time.
There are several possible reasons why the computer-assisted brief group treatment was more effective than the brief group treatment without the computer at posttherapy. One possibility is that the portable device and associated alarm prompts increased homework compliance, thereby allowing for more intensive therapy, despite the abbreviated sessions. Although we did not formally assess homework compliance in the current study, such compliance has been found to be an important ingredient for the success of CBT (Mausbach, Moore, Roesch, Cardenas, & Patterson, 2010; Westra, Dozois, & Marcus, 2007). It is also possible that the portable device and associated options for momentary intervention increased the generalizability of the treatment by providing instructions to clients about what to do in the moment to cope with their worry and anxiety. It may also be the case that having the device available provided a greater sense of safety than was the case with clients who were provided written handouts. Nonetheless, it is important to underscore that clients in the computer therapy condition were required to relinquish their devices immediately after the last therapy session. Therefore, the security of the device would not explain the large percentages of reliable change in this condition at 6- and 12-month follow-ups.
Clients in the brief computer-assisted therapy attended half of the number of sessions of standard treatment packages and achieved the same gains over long-term follow-up. Because this therapy was conducted in groups, brief computer therapy reduced therapist contact hours per session from 23 hours per person to 4 hours per person. This reduction in therapist contact may lead to a savings of over a thousand dollars per client, even after factoring in the cost of the technology (Newman et al., 1999). The reduced therapist– client contact hours permit CBT therapists to see a greater number of clients (Andrews & Erskine, 2003; Marks et al., 2004); thereby increasing client access to trained cognitive–behavioral therapists. Further, the use of computers to decrease therapist contact may provide a means to reduce barriers to treatment such as a need to drive long distances for months of weekly sessions, childcare for weekly sessions, and time away from work to attend sessions (for a review see Newman et al., 2011b; Titov, 2007).
The current study is the first to examine the efficacy of a computer-assisted brief group therapy for GAD relative to an active face-to-face control. Previous studies have demonstrated that predominantly self-help Internet treatment (Paxling et al., 2011), clinician-assisted Internet treatment (Titov et al., 2009) and technician-assisted Internet treatment (Robinson et al., 2010) were superior to a wait-list. An open trial of Internet treatment was also effective when delivered in primary practice (Mewton et al., 2012). However, none of these studies compared computer-based treatment with an active treatment control, such as treatment as usual; therefore, it is not known how these computer-based treatments would fare when compared with face-to-face treatments.
Additionally, these studies examined Internet treatment. As we have noted previously treatments administered via mobile devices that do not rely on the Internet may be preferable for numerous reasons including the variability of the speed of the Internet on many smartphones and the poor visibility of text on websites not designed to be viewed specifically via smartphones or cellphones. To date, only one very small sample study has examined a clinician-assisted mobile treatment for GAD that did not involve the Internet (Pallavicini et al., 2009). However, this study did not include an active therapist-delivered treatment without the device. As such, the current study adds to the literature by demonstrating the preliminary efficacy of brief group computer-assisted CBT for GAD relative to gold standard face-to-face therapy.
Limitations and Future Directions
There are numerous limitations to the current study. First, the sample size in the current study was small, potentially limiting the ability to find differences between groups. This may be especially problematic at follow-up points where there was some attrition. We plan to use many of the features in the current software package in a newer updated version that can be used on cellphones and smartphones. Such software will then be tested with a larger sample. Additionally, the majority of the current sample was Caucasian and highly educated, therefore it is difficult to know how generalizable the findings are to more diverse samples. Future studies should examine the efficacy of ambulatory software-assisted group therapy in individuals of diverse backgrounds and socioeconomic statuses. Additionally, studies should examine client satisfaction with ambulatory computer-assisted therapy and the ease of using such devices for therapy in individuals of varying levels of technological knowledge and experience. In previous studies testing palmtop computer-assisted therapy for panic disorder, we found no significant differences between those in computer therapy and standard therapy conditions on measures of expectancy or treatment satisfaction (Kenardy et al., 2003; Newman, Kenardy, et al., 1997). Another possible future focus of research would be to actively monitor homework compliance to determine whether the ambulatory devices lead to increases compared with treatments without the devices. It would also be interesting to examine the use of virtual synchronous or asynchronous groups in place of face-to- face groups. Finally, studies should examine the efficacy of an entirely self-help computer therapy without therapist contact (other than to monitor for deterioration/suicidality and to answer brief questions). This may provide the most cost-effective means of implementing and disseminating CBT for GAD.
Hundreds of CBT applications are beginning to appear for use on cellphones and smartphones. Although such applications have yet to be empirically tested, they have been downloaded by thousands of individuals. It is important to note that the current study used software that was designed by the first author and that this software was used in conjunction with psychotherapy. Thus the current study results may not generalize to other software packages and/or to software used without the guidance of a trained therapist. It will be important to test any one application separately before drawing conclusions about its efficacy as well as the conditions under which it is optimally effective.
Acknowledgments
This research was supported in part by National Institute of Mental Health Research Grant R01 MH-309172-01. We thank Tom Borkovec for his feedback on our computer program.
Contributor Information
Michelle G. Newman, Department of Psychology, The Pennsylvania State University
Amy Przeworski, Department of Psychology, Case Western Reserve University.
Andrés J. Consoli, Department of Counseling, San Francisco State University
C. Barr Taylor, Department of Psychiatry, Stanford University School of Medicine.
References
- Alonso J, Petukhova M, Vilagut G, Chatterji S, Heeringa S, Ustun TB, Kessler RC. Days out of role due to common physical and mental conditions: Results from the WHO World Mental Health surveys. Molecular Psychiatry. 2011;16:1234–1246. doi: 10.1038/mp.2010.101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4th ed. Washington, DC: American Psychiatric Association; 2000. [Google Scholar]
- Andrews G, Erskine A. Reducing the burden of anxiety and depressive disorders: The role of computerized clinician assistance. Current Opinion in Psychiatry. 2003;16:41–44. [Google Scholar]
- Beck AT, Emery G, Greenberg RL. Anxiety disorders and phobias: A cognitive perspective. New York: Basic Books; 1985. [Google Scholar]
- Beck AT, Steer RA. Relationship between the Beck Anxiety Inventory and the Hamilton Anxiety Rating Scale with anxious outpatients. Journal of Anxiety Disorders. 1991;5:213–223. [Google Scholar]
- Bernstein DA, Borkovec TD, Hazlett-Stevens H. New directions in progressive relaxation training: A guidebook for helping professionals. Westport, CT: Praeger Publishers/Greenwood Publishing Group, Inc.; 2000. [Google Scholar]
- Borkovec TD, Newman MG, Pincus AL, Lytle R .A component analysis of cognitive-behavioral therapy for generalized anxiety disorder and the role of interpersonal problems. Journal of Consulting and Clinical Psychology. 2002;70:288–298. [PubMed] [Google Scholar]
- Brown TA, Antony MM, Barlow DH. Psychometric properties of the Penn State Worry Questionnaire in a clinical anxiety disorders sample. Behaviour Research and Therapy. 1992;30:33–37. doi: 10.1016/0005-7967(92)90093-v. [DOI] [PubMed] [Google Scholar]
- Brown TA, Di Nardo PA, Barlow DH. Anxiety Disorders Interview Schedule for DSM–IV. New York: Oxford University Press; 1994. [Google Scholar]
- Brown TA, Di Nardo PA, Lehman CL, Campbell LA. Reliability of DSM–IV anxiety and mood disorders: Implications for the classification of emotional disorders. Journal of Abnormal Psychology. 2001;110:49–58. doi: 10.1037//0021-843x.110.1.49. [DOI] [PubMed] [Google Scholar]
- Bruss GS, Gruenberg AM, Goldstein RD, Barber JP. Hamilton Anxiety Rating Scale Interview Guide: Joint interview and test-retest methods for interrater reliability. Psychiatry Research. 1994;53:191–202. doi: 10.1016/0165-1781(94)90110-4. [DOI] [PubMed] [Google Scholar]
- Clark DM, Salkovskis PM, Hackmann A, Wells A, Ludgate J, Gelder M. Brief cognitive therapy for panic disorder: A randomized controlled trial. Journal of Consulting and Clinical Psychology. 1999;67:583–589. doi: 10.1037//0022-006x.67.4.583. [DOI] [PubMed] [Google Scholar]
- Griffiths F, Lindenmeyer A, Powell J, Lowe P, Thorogood M. Why are health care interventions delivered over the internet? A systemic review of the published literature. Journal of Medical Internet Research. 2006;8:e10. doi: 10.2196/jmir.8.2.e10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hamilton M. The assessment of anxiety states by rating. British Journal of Medical Psychology. 1959;32:50–55. doi: 10.1111/j.2044-8341.1959.tb00467.x. [DOI] [PubMed] [Google Scholar]
- Heron KE, Smyth JM. Ecological momentary interventions: Incorporating mobile technology into psychosocial and health behaviour treatments. British Journal of Health Psychology. 2010;15:1–39. doi: 10.1348/135910709X466063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jacobson NS, Truax P. Clinical significance: A statistical approach to defining meaningful change in psychotherapy research. Journal of Consulting and Clinical Psychology. 1991;59:12–19. doi: 10.1037//0022-006x.59.1.12. [DOI] [PubMed] [Google Scholar]
- Kenardy JA, Dow MGT, Johnston DW, Newman MG, Thomson A, Taylor CB. A comparison of delivery Methods of cognitive-Behavioral therapy for panic disorder: An international multicenter trial. Journal of Consulting and Clinical Psychology. 2003;71:1068–1075. doi: 10.1037/0022-006X.71.6.1068. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Wang PS. The descriptive epidemiology of commonly occurring mental disorders in the United States. Annual Review of Public Health. 2008;29:115–129. doi: 10.1146/annurev.publhealth.29.020907.090847. [DOI] [PubMed] [Google Scholar]
- Kobak KA, Reynolds WM, Greist JH. Development and validation of a computer-administered version of the Hamilton Rating Scale. Psychological Assessment. 1993;5:487–492. [Google Scholar]
- Maier W, Buller R, Philipp M, Heuser I. The Hamilton Anxiety Scale: Reliability, validity and sensitivity to change in anxiety and depressive disorders. Journal of Affective Disorders. 1988;14:61–68. doi: 10.1016/0165-0327(88)90072-9. [DOI] [PubMed] [Google Scholar]
- Marks IM, Kenwright M, McDonough M, Whittaker M, Mataix Cols D. Saving clinicians’ time by delegating routine aspects of therapy to a computer: A randomized controlled trial in phobia/panic disorder. Psychological Medicine. 2004;34:9–17. doi: 10.1017/s003329170300878x. [DOI] [PubMed] [Google Scholar]
- Mausbach BT, Moore R, Roesch S, Cardenas V, Patterson TL. The relationship between homework compliance and therapy outcomes: An updated meta-analysis. Cognitive Therapy and Research. 2010;34:429–438. doi: 10.1007/s10608-010-9297-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McGlinchey JB, Atkins DC, Jacobson NS. Clinical significance methods: Which one to use and how useful are they? Behavior Therapy. 2002;33:529–550. [Google Scholar]
- Mewton L, Wong N, Andrews G. The effectiveness of internet cognitive behavioural therapy for generalized anxiety disorder in clinical practice. Depression and Anxiety. 2012;29:843–849. doi: 10.1002/da.21995. [DOI] [PubMed] [Google Scholar]
- Meyer TJ, Miller ML, Metzger RL, Borkovec TD. Development and validation of the Penn State Worry Questionnaire. Behaviour Research and Therapy. 1990;28:487–495. doi: 10.1016/0005-7967(90)90135-6. [DOI] [PubMed] [Google Scholar]
- Molina S, Borkovec TD. The Penn State Worry Questionnaire: Psychometric properties and associated characteristics. In: Davey GCL, Tallis F, editors. Worrying: Perspectives on theory, assessment and treatment. Oxford, England: Wiley; 1994. pp. 265–283. [Google Scholar]
- Moras K, di Nardo PA, Barlow DH. Distinguishing anxiety and depression: Reexamination of the reconstructed Hamilton scales. Psychological Assessment. 1992;4:224–227. [Google Scholar]
- Newman MG. The clinical use of palmtop computers in the treatment of generalized anxiety disorder. Cognitive and Behavioral Practice. 1999;6:222–234. [Google Scholar]
- Newman MG. Recommendations for a cost-offset model of psychotherapy allocation using generalized anxiety disorder as an example. Journal of Consulting and Clinical Psychology. 2000;68:549–555. [PubMed] [Google Scholar]
- Newman MG, Castonguay LG, Borkovec TD, Fisher AJ, Boswell J, Szkodny LE, Nordberg SS. A randomized controlled trial of cognitive-behavioral therapy for generalized anxiety disorder with integrated techniques from emotion-focused and interpersonal therapies. Journal of Consulting and Clinical Psychology. 2011;79:171–181. doi: 10.1037/a0022489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Newman MG, Consoli A, Taylor CB. Computers in assessment and cognitive behavioral treatment of clinical disorders: Anxiety as a case in point. Behavior Therapy. 1997;28:211–235. [Google Scholar]
- Newman MG, Consoli AJ, Taylor CB. A palmtop computer program for the treatment of generalized anxiety disorder. Behavior Modification. 1999;23:597–619. doi: 10.1177/0145445599234005. [DOI] [PubMed] [Google Scholar]
- Newman MG, Erickson T, Przeworski A, Dzus E. Self-help and minimal-contact therapies for anxiety disorders: Is human contact necessary for therapeutic efficacy? Journal of Clinical Psychology. 2003;59:251–274. doi: 10.1002/jclp.10128. [DOI] [PubMed] [Google Scholar]
- Newman MG, Kenardy J, Herman S, Taylor CB. The use of hand-held computers as an adjunct to cognitive-behavior therapy. Computers in Human Behavior. 1996;12:135–143. [Google Scholar]
- Newman MG, Kenardy J, Herman S, Taylor CB. Comparison of palmtop-computer-assisted brief cognitive-behavioral treatment to cognitive-behavioral treatment for panic disorder. Journal of Consulting and Clinical Psychology. 1997;65:178–183. doi: 10.1037//0022-006x.65.1.178. [DOI] [PubMed] [Google Scholar]
- Newman MG, Przeworski A, Fisher AJ, Borkovec TD. Diagnostic comorbidity in adults with generalized anxiety disorder: Impact of comorbidity on psychotherapy outcome and impact of psychotherapy on comorbid diagnoses. Behavior Therapy. 2010;41:59–72. doi: 10.1016/j.beth.2008.12.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Newman MG, Szkodny LE, Llera SJ, Przeworski A. A review of technology-assisted self-help and minimal contact therapies for drug and alcohol abuse and smoking addiction: Is human contact necessary for therapeutic efficacy? Clinical Psychology Review. 2011a;31:178–186. doi: 10.1016/j.cpr.2010.10.002. [DOI] [PubMed] [Google Scholar]
- Newman MG, Szkodny LE, Llera SJ, Przeworski A. A review of technology-assisted self-help and minimal contact therapies for anxiety and depression: Is human contact necessary for therapeutic efficacy? Clinical Psychology Review. 2011b;31:89–103. doi: 10.1016/j.cpr.2010.09.008. [DOI] [PubMed] [Google Scholar]
- Pallavicini F, Algeri D, Repetto C, Gorini A, Riva G. Biofeedback, virtual reality and mobile phones in the treatment of generalized anxiety disorder (GAD): A phase-2 controlled clinical trial. Journal of CyberTherapy and Rehabilitation. 2009;2:315–327. [Google Scholar]
- Paxling B, Almlov J, Dahlin M, Carlbring P, Breitholtz E, Eriksson T, Andersson G. Guided Internet-delivered cognitive behavior therapy for generalized anxiety disorder: A randomized controlled trial. Cognitive Behaviour Therapy. 2011;40:159–173. doi: 10.1080/16506073.2011.576699. [DOI] [PubMed] [Google Scholar]
- Pew Internet & American Life Project. Internet, broadband, and cell phone statistics. Washington, DC: Pew Research Center; 2010. [Google Scholar]
- Przeworski A, Newman MG. Palmtop computer-assisted group therapy for social phobia. Journal of Clinical Psychology. 2004;60:179–188. doi: 10.1002/jclp.10246. [DOI] [PubMed] [Google Scholar]
- Riskind JH, Beck AT, Brown G, Steer RA. Taking the measure of anxiety and depression: Validity of the reconstructed Hamilton scales. Journal of Nervous and Mental Disease. 1987;175:474–479. doi: 10.1097/00005053-198708000-00005. [DOI] [PubMed] [Google Scholar]
- Robinson E, Titov N, Andrews G, McIntyre K, Schwencke G, Solley K. Internet treatment for generalized anxiety disorder: A randomized controlled trial comparing clinician vs. technician assistance. PLoS One. 2010;5:e10942. doi: 10.1371/journal.pone.0010942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosenthal R, Rosnow RL. Essentials of behavioural research: Methods and data analysis. 3rd ed. New York: McGraw Hill; 2007. [Google Scholar]
- Spielberger CD, Gorsuch RL, Lushene R, Vagg PR, Jacobs GA. Manual for the State-Trait Anxiety Inventory STAI (Form Y) Palo Alto, CA: Mind Garden; 1983. [Google Scholar]
- Titov N. Status of computerized cognitive behavioural therapy for adults. Australian and New Zealand Journal of Psychiatry. 2007;41:95–114. doi: 10.1080/00048670601109873. [DOI] [PubMed] [Google Scholar]
- Titov N, Andrews G, Robinson E, Schwencke G, Johnston L, Solley K, Choi I. Clinician-assisted Internet-based treatment is effective for generalized anxiety disorder: Randomized controlled trial. Australian and New Zealand Journal of Psychiatry. 2009;43:905–912. [Google Scholar]
- Turner SM, Beidel D, Spaulding S, Brown J. The practice of behavior therapy: A national survey of cost and methods. Behavior Therapist. 1995;18:1–4. [Google Scholar]
- Westra HA, Dozois DJA, Marcus M. Expectancy, homework compliance, and initial change in cognitive-behavioral therapy for anxiety. Journal of Consulting and Clinical Psychology. 2007;75:363–373. doi: 10.1037/0022-006X.75.3.363. [DOI] [PubMed] [Google Scholar]
- Yonkers KA, Bruce SE, Dyck IR, Keller MB. Chronicity, relapse, and illness-course of panic disorder, social phobia, and generalized anxiety disorder: Findings in men and women from 8 years of follow-up. Depression and Anxiety. 2003;17:173–179. doi: 10.1002/da.10106. [DOI] [PubMed] [Google Scholar]