Abstract
Background
This article summarizes the 2012 European Renal Association—European Dialysis and Transplant Association Registry Annual Report (available at www.era-edta-reg.org) with a specific focus on older patients (defined as ≥65 years).
Methods
Data provided by 45 national or regional renal registries in 30 countries in Europe and bordering the Mediterranean Sea were used. Individual patient level data were received from 31 renal registries, whereas 14 renal registries contributed data in an aggregated form. The incidence, prevalence and survival probabilities of patients with end-stage renal disease (ESRD) receiving renal replacement therapy (RRT) and renal transplantation rates for 2012 are presented.
Results
In 2012, the overall unadjusted incidence rate of patients with ESRD receiving RRT was 109.6 per million population (pmp) (n = 69 035), ranging from 219.9 pmp in Portugal to 24.2 pmp in Montenegro. The proportion of incident patients ≥75 years varied from 15 to 44% between countries. The overall unadjusted prevalence on 31 December 2012 was 716.7 pmp (n = 451 270), ranging from 1670.2 pmp in Portugal to 146.7 pmp in the Ukraine. The proportion of prevalent patients ≥75 years varied from 11 to 32% between countries. The overall renal transplantation rate in 2012 was 28.3 pmp (n = 15 673), with the highest rate seen in the Spanish region of Catalonia. The proportion of patients ≥65 years receiving a transplant ranged from 0 to 35%. Five-year adjusted survival for all RRT patients was 59.7% (95% confidence interval, CI: 59.3–60.0) which fell to 39.3% (95% CI: 38.7–39.9) in patients 65–74 years and 21.3% (95% CI: 20.8–21.9) in patients ≥75 years.
Keywords: end-stage renal disease, incidence, prevalence, renal replacement therapy, survival
Introduction
The European Renal Association—European Dialysis and Transplant Association (ERA-EDTA) Registry annually collects data on renal replacement therapy (RRT) for end-stage renal disease (ESRD) from national and regional renal registries in Europe and those bordering the Mediterranean Sea. In this article, we provide a summary of the 2012 ERA-EDTA Registry Annual Report (available at www.era-edta-reg.org) on the incidence and prevalence of ESRD patients receiving RRT, on kidney transplant rates and on patient and graft survival. As the older patient (defined in this article as 65 years and over and presented in two age groups, i.e. 65–74 years, and 75 years and over) now represents 42% of the RRT population within Europe, this article will pay particular attention to this patient group.
Materials and methods
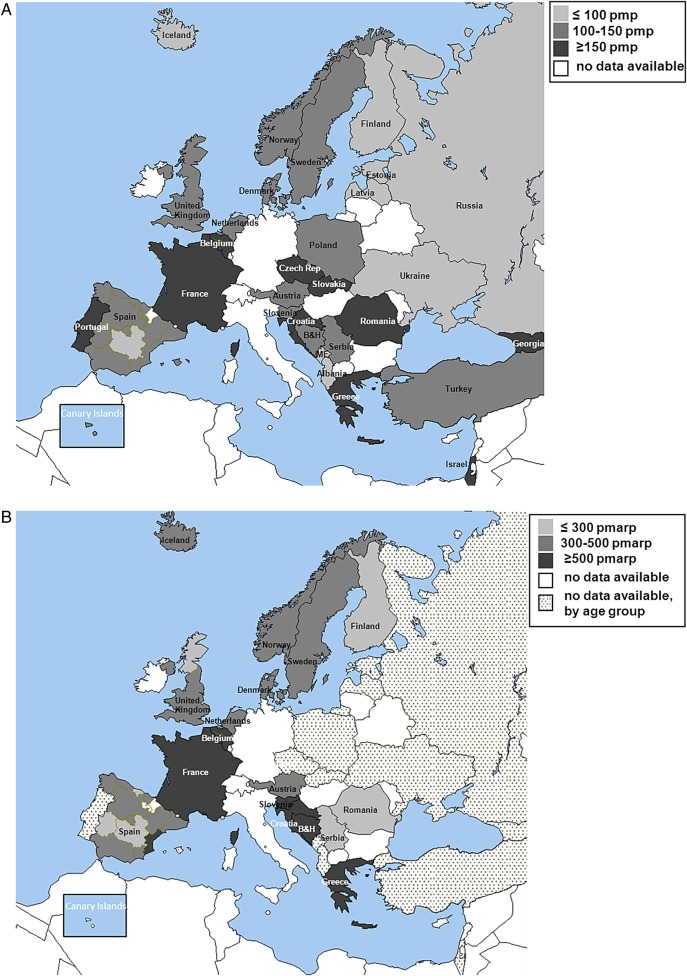
In 2014, the ERA-EDTA Registry received the 2012 data from the national and regional renal registries in 30 countries in Europe and those bordering the Mediterranean Sea (Figure 1A). Data sets with individual patient data were received from 31 national or regional renal registries in 17 countries, whereas 14 national renal registries contributed data in an aggregated form. The percentage coverage of the general population by the renal registries was >98% for all participating countries with the exception of Romania (96%), Latvia (85%) and Georgia (63.5%). The total coverage of the European population by the ERA-EDTA Registry in 2012 was 71.3%. A list of the European countries with available data and those without is provided in Appendix 1.
Fig. 1.
(A) The unadjusted incidence of ESRD patients on RRT, pmp on Day 1, among all national and regional renal registries in 30 countries reporting to the ERA-EDTA Registry in 2012. The incidence data for Czech Republic and Slovakia include dialysis patients only. Dutch- and French-speaking Belgium, the Spanish regions of Cantabria, Castile and León and Castile-La Mancha and the UK; England, Northern Ireland and Wales do not report on patients younger than 20 years. (B) The unadjusted incidence of ESRD patients aged 75 years and older on RRT, per million age-related population (pmarp) at Day 1, among all national and regional renal registries in 17 countries providing individual level data to the ERA-EDTA Registry in 2012. B&H: Bosnia–Herzegovina; ME: Montenegro.
The RRT incidence and prevalence data were presented as unadjusted rates and standardized for the age and sex distribution of the EU27 population in 2010 [1]. Patient survival on RRT and dialysis were based on incident RRT patients. Patient and graft survival post-transplantation only included patients receiving their first renal transplant between 2003 and 2007 or 2006 and 2010. The survival analyses were based solely on data from renal registries providing individual patient records. A detailed description of the methods on patient and graft survival is given in Appendix 1. More detailed data than those presented in this current paper were published in the full 2012 ERA-EDTA Registry Annual Report [2], which is also available online at www.era-edta-reg.org.
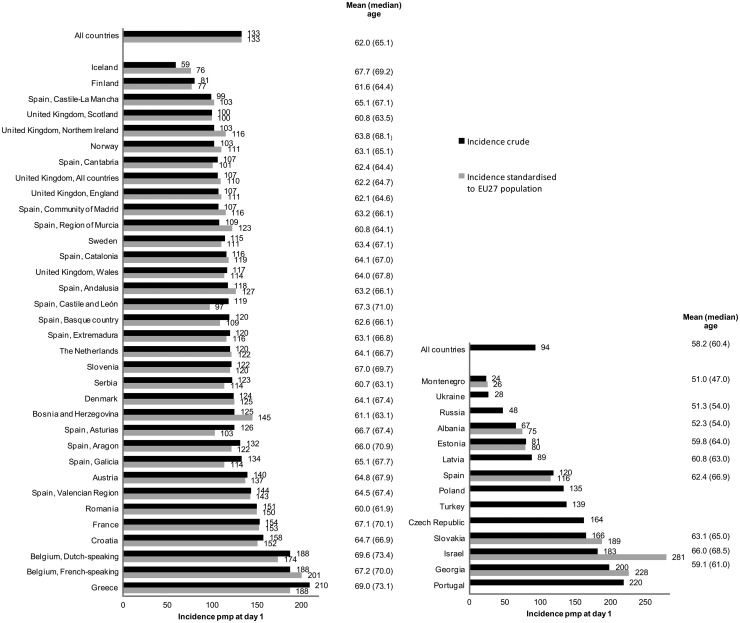
The incidence of RRT for ESRD
In 2012, the total number of patients starting RRT for ESRD among all the registries reporting to the ERA-EDTA Registry was 69 035. These registries covered a total population of 629.7 million, resulting in an unadjusted incidence rate of 109.6 per million population (pmp). Figure 1A and Figure 2 show the incidence of ESRD patients receiving RRT per pmp on Day 1, among all national and regional renal registries in 30 countries reporting to the ERA-EDTA Registry in 2012. The highest unadjusted incidence rates were reported in Portugal (219.9 pmp), Greece (209.7 pmp) and Georgia (199.6 pmp), whereas the lowest unadjusted incidence rates were reported in Montenegro (24.2 pmp), Ukraine (27.6 pmp) and Russia (48.1 pmp). The incidence rate standardized for the EU27 population was highest in Israel (280.5 pmp), Georgia (227.5 pmp) and French-speaking Belgium (201.1 pmp). The mean age at the start of RRT across Europe was 62.0 years in the renal registries providing individual level patient data and 58.2 years in the renal registries providing aggregated data (Figure 2). Figure 1B and Figure 3 provide information on the incidence of RRT, per million age-related population (pmarp), on Day 1 for older patients. For the countries providing individual level data; the incidence of RRT for patients aged 65–74 years or 75 years and over varied considerably between the renal registries (Figure 3). The lowest incidence rate of patients aged 65–74 and 75 years and over was reported in Finland (199.8 and 220.8 pmarp, respectively). A more than three times as high incidence rate was reported in French-speaking Belgium (619.4 pmarp) for patients aged 65–74 years and Dutch-speaking Belgium (893.6 pmarp) for patients aged over 75 years (Figure 3). Within each country or region, there was a wide variation in the proportion of ESRD patients aged 75 years and over commencing RRT with the highest proportion reported in Dutch-speaking Belgium (44%) and Greece (43%) and the lowest proportion in Romania (15%) and Serbia (15%). Within the countries supplying individual level data, the four national or regional registries with the highest adjusted incidence of RRT on Day 1 (Greece, French- and Dutch-speaking Belgium and France) also had the highest incidence of RRT on Day 1 for patients 75 years and over (Figure 1A–B and 3).
Fig. 2.
Incidence of RRT, pmp at Day 1 in 2012, unadjusted (black bars) and standardized to the age and gender distribution of the EU27 population in 2010 (grey bars) and the mean and median age (years) at the start of RRT. Data are from renal registries providing individual level patient data (left panel) and from renal registries providing aggregated data (right panel). The incidence data for the Czech Republic and Slovakia only include dialysis patients. The mean and median age for Slovakia is based on dialysis patients and for Turkey only on haemodialysis patients. Dutch- and French-speaking Belgium, the Spanish regions of Cantabria, Castile and León and Castile-La Mancha and the UK; England, Northern Ireland and Wales do not report on patients younger than 20 years.
Fig. 3.
Incidence of ESRD patients on RRT, pmarp, unadjusted at Day 1, in 2012 for patients aged 65–74 years (black bars) and 75 years and over (grey bars), and with the percentage of patients by the age group.
Table 1 presents the unadjusted incidence of RRT pmp on Day 91, by treatment modality (haemodialysis, peritoneal dialysis and transplantation) for the renal registries providing individual and aggregated data. The incidence rate of haemodialysis was highest in Portugal (184.7 pmp), Greece (171.0 pmp) and Israel (153.7 pmp), whereas the incidence rate of peritoneal dialysis was highest in the Spanish regions of Asturias (38.2 pmp) and Galicia (32.9 pmp) and Sweden (32.6 pmp). The incidence rate of renal transplants on Day 91 was highest in Norway (16.5 pmp), the Netherlands (14.9 pmp) and Iceland (12.5 pmp). Table 2 presents the percentage of patients by established treatment modality (haemodialysis, peritoneal dialysis and transplantation) on Day 91 after the start of RRT, by age group. For patients 75 years and over, the vast majority were treated with haemodialysis, and almost no patients had a kidney transplant. Notably, within this age group the Scandinavian countries (Norway, Sweden, Finland and Denmark) had the highest percentage (about a quarter) of patients treated with peritoneal dialysis.
Table 1.
Incident counts and rates, pmp of RRT at Day 91 (unadjusted) in 2012 by established therapy for countries/regions providing individual patient data and for countries/regions providing aggregated data
| Region | All |
All |
HD |
PD |
Tx |
Unknown/missing |
|---|---|---|---|---|---|---|
| N | pmp | pmp | pmp | pmp | pmp | |
| Country/region providing individual patient data, pmp | ||||||
| Austria | 1054 | 124.8 | 104.1 | 15.0 | 5.7 | 0 |
| Belgium | ||||||
| Dutch-speakinga | 1089 | 171.1 | 150.0 | 16.8 | 4.2 | 0 |
| French-speakinga | 800 | 170.2 | 147.4 | 17.9 | 4.0 | 0.9 |
| Bosnia and Herzegovina | 407 | 116.0 | 112.3 | 3.4 | 0 | 0.3 |
| Croatiab | 595 | 139.4 | 123.4 | 13.7 | 2.0 | 0.2 |
| Denmark | 654 | 115.8 | 75.6 | 31.9 | 8.3 | 0 |
| Finland | 433 | 80.0 | 57.8 | 21.6 | 0.6 | 0 |
| France | 9305 | 142.2 | 117.0 | 14.9 | 6.2 | 4.0 |
| Greece | 2059 | 185.6 | 171.0 | 13.3 | 1.3 | 0 |
| Iceland | 19 | 59.2 | 28.1 | 18.7 | 12.5 | 0 |
| Norway | 499 | 99.4 | 63.4 | 19.5 | 16.5 | 0 |
| Romania | 2518 | 130.8 | 122.0 | 7.4 | 1.4 | 0 |
| Serbia | 837 | 116.3 | 102.2 | 12.4 | 1.7 | 0 |
| Slovenia | 240 | 116.7 | 110.8 | 5.3 | 0.5 | 0 |
| Spain | ||||||
| Andalusia | 947 | 112.9 | 89.3 | 17.9 | 5.7 | 0 |
| Aragon | 171 | 127.5 | 105.1 | 17.9 | 4.5 | 0 |
| Asturias | 131 | 121.9 | 81.0 | 38.2 | 2.8 | 0 |
| Basque country | 251 | 115.1 | 84.4 | 24.3 | 6.4 | 0 |
| Cantabriaa | 55 | 93.0 | 67.7 | 20.3 | 5.1 | 0 |
| Castile and Leóna | 287 | 113.5 | 87.4 | 22.9 | 3.2 | 0 |
| Castile-La Manchaa | 198 | 94.3 | 76.2 | 17.1 | 1.0 | 0 |
| Cataloniab | 854 | 112.8 | 82.3 | 19.0 | 11.5 | 0 |
| Community of Madrid | 659 | 102.6 | 82.1 | 14.5 | 6.1 | 0 |
| Extremadura | 127 | 114.6 | 96.6 | 17.1 | 0.9 | 0 |
| Galicia | 365 | 131.9 | 94.3 | 32.9 | 4.7 | 0 |
| Region of Murciab | 159 | 107.6 | 93.1 | 12.4 | 2.0 | 0 |
| Valencian Region | 711 | 138.6 | 109.8 | 24.6 | 4.3 | 0 |
| Sweden | 969 | 101.8 | 60.8 | 32.6 | 8.4 | 0 |
| The Netherlands | 1892 | 112.9 | 79.6 | 18.5 | 14.9 | 0 |
| UK | ||||||
| All countriesa,b | 6372 | 100.0 | 71.0 | 20.0 | 9.0 | 0 |
| Englanda,b | 5371 | 100.4 | 70.6 | 20.7 | 9.1 | 0 |
| Northern Irelanda,b | 168 | 92.3 | 65.8 | 15.0 | 11.5 | 0 |
| Scotland | 508 | 95.6 | 74.5 | 13.7 | 7.3 | 0 |
| Walesa,b | 332 | 108.0 | 75.4 | 23.2 | 9.4 | 0 |
| Country/region providing aggregated patient data | ||||||
| Albania | 177 | 63.3 | 57.9 | 4.6 | 0.7 | 0 |
| Czech Republicc | 1396 | 134.1 | 126.0 | 8.1 | 0 | |
| Estonia | 105 | 79.4 | 61.2 | 16.6 | 1.5 | 0 |
| Georgia | 475 | 166.3 | 143.2 | 21.0 | 1.1 | 1.1 |
| Israel | 1356 | 171.4 | 153.7 | 12.3 | 5.4 | 0 |
| Latvia | 138 | 80.2 | 64.5 | 15.7 | 0.0 | 0 |
| Montenegro | 13 | 21.0 | 21.0 | 0.0 | 0.0 | 0 |
| Portugald | 2190 | 207.3 | 184.7 | 20.8 | 1.8 | 0 |
| Slovakiac | 772 | 142.7 | 136.8 | 5.9 | 0 | |
HD, haemodialysis; PD, peritoneal dialysis; TX, transplant; pmp, per million population.
aPatients younger than 20 years of age are not reported.
bThe incident counts at Day 91 are estimated.
cData include dialysis patients only.
dOnly pre-emptive transplantations (at Day 1) are included. When cells are left empty, the data are unavailable.
Table 2.
Percentages of established RRT modality at Day 91 (unadjusted) by age group for the countries/regions providing individual patient data
| Region | All |
0–19 |
20–44 |
45–64 |
65–74 |
≥75 |
||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| HD (%) | PD (%) | TX (%) | Oth (%) | HD (%) | PD (%) | TX (%) | Oth (%) | HD (%) | PD (%) | TX (%) | Oth (%) | HD (%) | PD (%) | TX (%) | Oth (%) | HD (%) | PD (%) | TX (%) | Oth (%) | HD (%) | PD (%) | TX (%) | Oth (%) | |
| Austria | 75 | 12 | 5 | 8 | 39 | 17 | 44 | 0 | 55 | 14 | 18 | 13 | 67 | 16 | 6 | 11 | 82 | 13 | 0 | 5 | 88 | 5 | 0 | 7 |
| Belgium | ||||||||||||||||||||||||
| Dutch-speakinga | 59 | 10 | 3 | 29 | 38 | 26 | 11 | 26 | 57 | 15 | 4 | 24 | 61 | 10 | 3 | 26 | 63 | 4 | 0 | 33 | ||||
| French-speakinga | 65 | 11 | 2 | 22 | 48 | 22 | 11 | 19 | 66 | 12 | 3 | 19 | 70 | 6 | 2 | 21 | 65 | 9 | 0 | 26 | ||||
| Bosnia and Herzegovina | 94 | 3 | 0 | 3 | 75 | 25 | 0 | 0 | 88 | 7 | 0 | 5 | 93 | 2 | 0 | 5 | 96 | 2 | 0 | 3 | 98 | 2 | 0 | 0 |
| Croatiab | 88 | 10 | 1 | 1 | 13 | 50 | 38 | 0 | 81 | 10 | 6 | 3 | 85 | 14 | 0 | 0 | 92 | 7 | 0 | 1 | 95 | 5 | 1 | 0 |
| Denmark | 65 | 28 | 7 | 0 | 50 | 25 | 25 | 0 | 64 | 23 | 14 | 0 | 58 | 30 | 12 | 0 | 63 | 31 | 5 | 0 | 78 | 22 | 0 | 0 |
| Finland | 69 | 27 | 1 | 3 | 29 | 57 | 14 | 0 | 51 | 44 | 4 | 2 | 70 | 26 | 0 | 4 | 75 | 22 | 0 | 4 | 77 | 22 | 0 | 1 |
| France | 72 | 11 | 4 | 13 | 35 | 21 | 26 | 19 | 64 | 13 | 12 | 11 | 71 | 9 | 7 | 13 | 76 | 9 | 3 | 12 | 73 | 12 | 0 | 15 |
| Greece | 89 | 7 | 1 | 3 | 61 | 28 | 11 | 0 | 85 | 9 | 4 | 2 | 87 | 9 | 1 | 3 | 89 | 7 | 0 | 4 | 92 | 6 | 0 | 2 |
| Iceland | 47 | 32 | 21 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 44 | 22 | 33 | 0 | 67 | 0 | 33 | 0 | 43 | 57 | 0 | 0 |
| Norway | 64 | 20 | 17 | 0 | 20 | 20 | 60 | 0 | 62 | 17 | 22 | 0 | 56 | 20 | 24 | 0 | 68 | 16 | 16 | 0 | 73 | 24 | 3 | 0 |
| Romania | 93 | 6 | 1 | 0 | 68 | 32 | 0 | 0 | 89 | 6 | 5 | 0 | 93 | 6 | 0 | 0 | 94 | 6 | 0 | 0 | 96 | 4 | 0 | 1 |
| Serbia | 86 | 11 | 1 | 2 | 86 | 0 | 14 | 0 | 67 | 20 | 9 | 4 | 90 | 8 | 0 | 2 | 90 | 9 | 0 | 1 | 87 | 13 | 0 | 1 |
| Slovenia | 95 | 5 | 0 | 0 | 100 | 0 | 0 | 0 | 88 | 12 | 0 | 0 | 90 | 9 | 1 | 0 | 97 | 3 | 0 | 0 | 100 | 0 | 0 | 0 |
| Spain | ||||||||||||||||||||||||
| Andalusia | 79 | 16 | 5 | 0 | 42 | 25 | 33 | 0 | 67 | 19 | 14 | 0 | 75 | 18 | 7 | 0 | 82 | 16 | 2 | 0 | 90 | 10 | 0 | 0 |
| Aragon | 81 | 14 | 4 | 2 | 0 | 0 | 100 | 0 | 58 | 21 | 21 | 0 | 77 | 23 | 0 | 0 | 81 | 15 | 0 | 4 | 93 | 5 | 0 | 2 |
| Asturias | 66 | 31 | 2 | 0 | 0 | 100 | 0 | 0 | 38 | 63 | 0 | 0 | 52 | 43 | 4 | 0 | 77 | 19 | 3 | 0 | 80 | 20 | 0 | 0 |
| Basque country | 73 | 21 | 6 | 0 | 0 | 0 | 100 | 0 | 54 | 26 | 20 | 0 | 65 | 31 | 5 | 0 | 82 | 17 | 2 | 0 | 88 | 12 | 0 | 0 |
| Cantabriaa | 73 | 22 | 5 | 0 | 43 | 14 | 43 | 0 | 64 | 36 | 0 | 0 | 93 | 7 | 0 | 0 | 83 | 17 | 0 | 0 | ||||
| Castile and Leóna | 77 | 20 | 3 | 0 | 52 | 28 | 20 | 0 | 63 | 35 | 2 | 0 | 83 | 16 | 2 | 0 | 91 | 9 | 0 | 0 | ||||
| Castile-La Manchaa | 81 | 18 | 1 | 0 | 56 | 38 | 6 | 0 | 75 | 24 | 1 | 0 | 75 | 25 | 0 | 0 | 98 | 2 | 0 | 0 | ||||
| Cataloniab | 53 | 17 | 10 | 20 | 36 | 27 | 38 | 0 | 40 | 16 | 29 | 15 | 42 | 24 | 17 | 17 | 59 | 16 | 4 | 20 | 66 | 9 | 0 | 25 |
| Extremadura | 84 | 15 | 1 | 0 | 0 | 0 | 0 | 0 | 61 | 39 | 0 | 0 | 76 | 21 | 2 | 0 | 100 | 0 | 0 | 0 | 90 | 10 | 0 | 0 |
| Galicia | 72 | 25 | 4 | 0 | 67 | 33 | 0 | 0 | 43 | 46 | 11 | 0 | 55 | 38 | 7 | 0 | 85 | 15 | 0 | 0 | 87 | 13 | 0 | 0 |
| Community of Madrid | 80 | 14 | 6 | 0 | 57 | 14 | 29 | 0 | 55 | 31 | 13 | 0 | 73 | 20 | 7 | 0 | 87 | 9 | 4 | 0 | 93 | 5 | 2 | 0 |
| Region of Murciab | 87 | 12 | 2 | 0 | 50 | 50 | 0 | 0 | 60 | 30 | 11 | 0 | 92 | 8 | 0 | 0 | 93 | 7 | 0 | 0 | 94 | 6 | 0 | 0 |
| Valencian Region | 79 | 18 | 3 | 0 | 44 | 33 | 22 | 0 | 59 | 32 | 9 | 0 | 69 | 26 | 5 | 0 | 87 | 12 | 1 | 0 | 92 | 8 | 0 | 0 |
| Sweden | 60 | 32 | 8 | 0 | 7 | 41 | 52 | 0 | 51 | 30 | 19 | 0 | 57 | 34 | 9 | 0 | 59 | 37 | 5 | 0 | 74 | 25 | 1 | 0 |
| The Netherlands | 70 | 16 | 13 | 0 | 31 | 10 | 59 | 0 | 50 | 17 | 32 | 0 | 61 | 17 | 21 | 0 | 74 | 19 | 7 | 0 | 87 | 13 | 0 | 0 |
| UK | ||||||||||||||||||||||||
| All countriesa,b | 69 | 20 | 9 | 2 | 51 | 26 | 21 | 2 | 63 | 23 | 12 | 2 | 75 | 18 | 5 | 2 | 83 | 14 | 0 | 3 | ||||
| Englanda,b | 68 | 21 | 9 | 3 | 49 | 27 | 21 | 2 | 62 | 23 | 12 | 2 | 74 | 19 | 5 | 3 | 82 | 14 | 0 | 4 | ||||
| Northern Irelanda,b | 70 | 16 | 12 | 1 | 43 | 22 | 36 | 0 | 65 | 18 | 17 | 0 | 69 | 26 | 3 | 3 | 95 | 4 | 0 | 1 | ||||
| Scotland | 78 | 14 | 8 | 0 | 20 | 40 | 40 | 0 | 67 | 17 | 17 | 0 | 73 | 15 | 11 | 0 | 88 | 12 | 1 | 0 | 86 | 13 | 1 | 0 |
| Walesa,b | 70 | 21 | 9 | 0 | 52 | 29 | 19 | 0 | 60 | 29 | 11 | 0 | 70 | 21 | 9 | 0 | 91 | 9 | 0 | 0 | ||||
HD, haemodialysis; PD, peritoneal dialysis; TX, transplant; oth, other (includes haemofiltration, haemodiafiltration and unknown).
Categories may not add up because of missing values or rounding off; percentages are row percentages. When cells are left empty (complete) data are unavailable.
aPatients younger than 20 years of age are not reported.
bThe incident counts at Day 91, on which the data presented in this table are based, are estimated (see annual report for methods).
For children (aged 0–19 years), we performed a separate analysis of the incidence rate by age group and initial treatment modality from a selected number of renal registries which are presented in Table 3. A more detailed overview of the paediatric RRT data in Europe can be found at www.espn-reg.org.
Table 3.
Incident rates per million age-related population of RRT at Day 1 over the time period 2011–12 for patients aged 0–19 by age and treatment modality
| 0–19 |
0–4 |
5–9 |
10–14 |
15–19 |
||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| All | HD | PD | Tx | All | HD | PD | Tx | All | HD | PD | Tx | All | HD | PD | Tx | All | HD | PD | Tx | |
| pmarp |
pmarp |
pmarp |
pmarp |
pmarp |
||||||||||||||||
| 2011–12 | 7.6 | 3.8 | 2.0 | 1.7 | 7.2 | 2.2 | 4.2 | 0.7 | 3.7 | 1.2 | 0.8 | 1.5 | 6.9 | 3.1 | 1.3 | 2.3 | 12.6 | 8.5 | 1.6 | 2.2 |
HD, haemodialysis; PD, peritoneal dialysis; TX, transplant; pmarp, per million age-related population.
Data from France include a coverage of 99.37% in 2011 and 100% in 2012. The Spanish region of Murcia is only included in 2012.
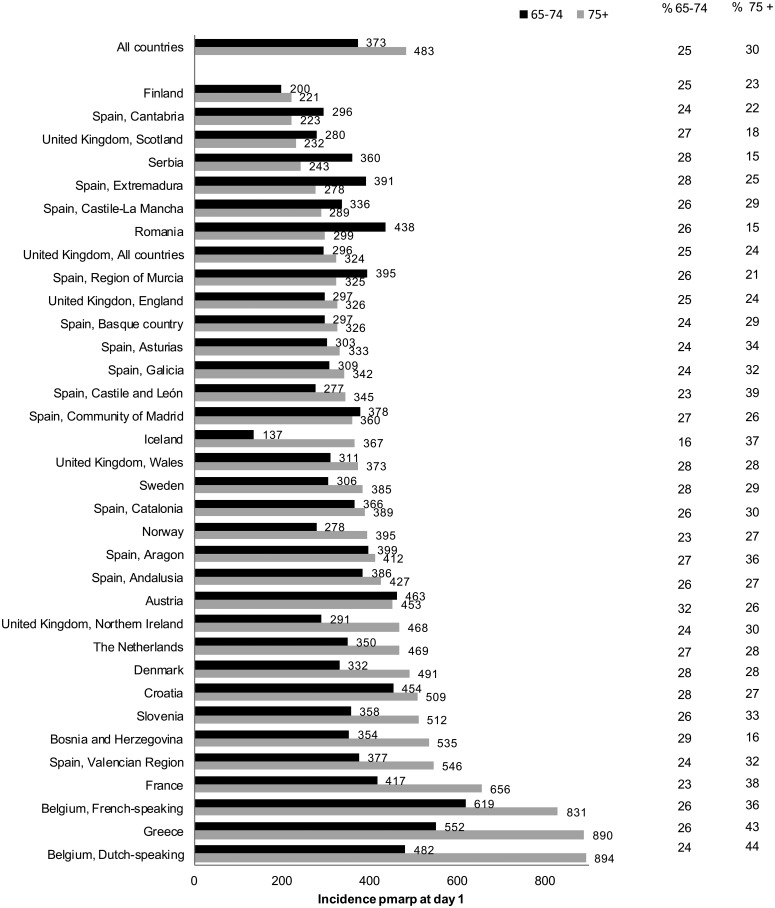
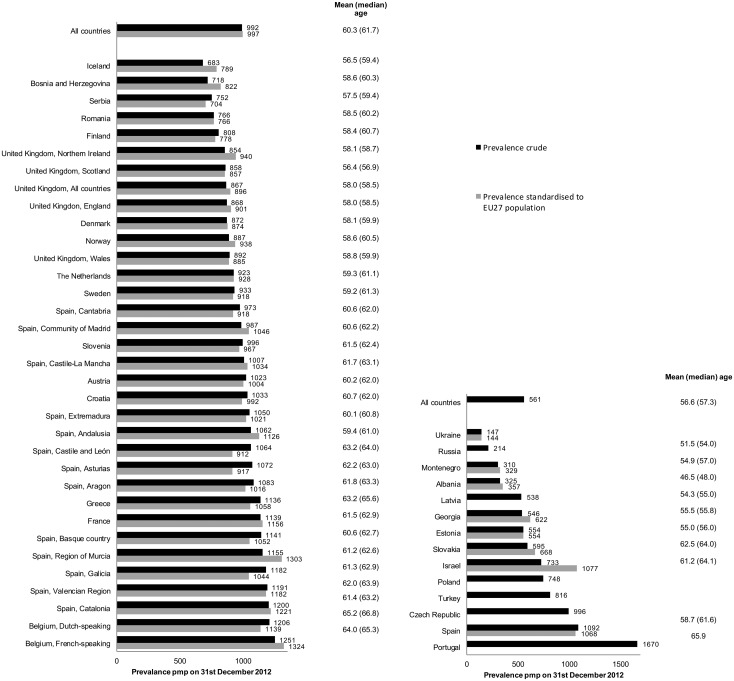
The prevalence of RRT for ESRD
On the 31 December 2012, a total of 451 270 patients with ESRD were receiving RRT among the renal registries reporting to the ERA-EDTA Registry, corresponding to an unadjusted prevalence of 716.7 pmp. There was a substantial difference in the prevalence pmp throughout Europe, both in the unadjusted prevalence and the prevalence standardized for the age and sex distribution of the EU27 population (Figure 4). The unadjusted prevalence was highest in Portugal (1670.2 pmp), French- and Dutch-speaking Belgium (1251.3 and 1206.2 pmp, respectively), whereas the unadjusted prevalence was lowest in Ukraine (146.7 pmp), Russia (213.9 pmp) and Montenegro (309.7 pmp). The prevalence pmp standardized to the EU27 was highest in French-speaking Belgium (1324.1 pmp) and the Spanish regions of Murcia (1303.1 pmp) and Catalonia (1221.3 pmp). In 2012, the mean age of the prevalent RRT patients was 60.3 years within the renal registries providing individual level patient data and 56.6 years within the renal registries providing aggregated data, with considerable variation across renal registries (Figure 4).
Fig. 4:
Prevalence of RRT, pmp on 31 December 2012, unadjusted (black bars) and standardized to the age and gender distribution of the EU27 population (grey bars) and the mean and median age (years). Data are from the renal registries providing individual level patient data (left panel) and from renal registries providing aggregated data (right panel). Data for Israel and Slovakia only include dialysis patients. Dutch- and French-speaking Belgium, the Spanish regions of Cantabria, Castile and León and Castile-La Mancha and the UK; England, Northern Ireland and Wales do not report on patients younger than 20 years.
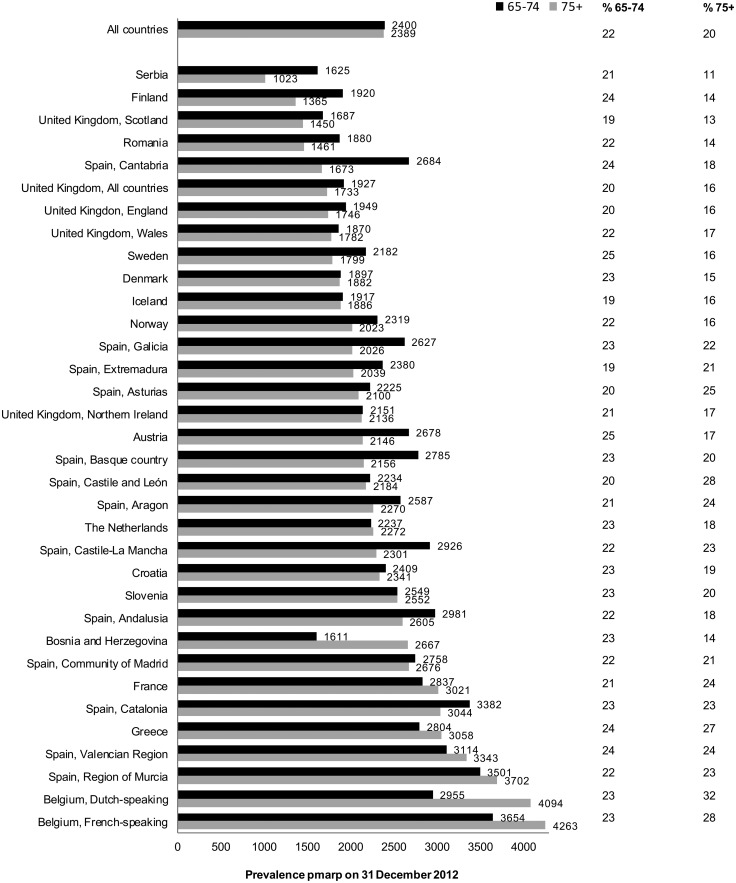
The unadjusted prevalence of patients aged 65–74 years and 75 years and over was 2400.2 and 2388.9 pmarp, respectively, within the renal registries providing individual level patient data (Figure 5). Prevalent patients aged 65–74 years formed 22% of the total prevalent patient population from these registries and patients aged 75 years and over formed 20%. The prevalence pmarp for patients aged 65–74 years was highest in French-speaking Belgium (3654.2 pmarp) and the Spanish regions of Murcia (3501.5 pmarp) and Catalonia (3382.4 pmarp). The prevalence pmarp for patients aged 75 years and above was highest in French- and Dutch-speaking Belgium (4262.6 and 4093.8 pmarp, respectively) and the Spanish region of Murcia (3701.5 pmarp).
Fig. 5.
Prevalence of RRT, pmp on 31 December 2012 for patients with ESRD aged 65–74 years (black bars) and 75 years and over (grey bars), and with the percentage of patients by the age group.
Table 4 presents the unadjusted prevalence of ESRD patients receiving RRT pmp on 31st December 2012, by treatment modality (haemodialysis, peritoneal dialysis and transplantation) for the renal registries providing individual and aggregated data. The prevalence of haemodialysis was highest in Portugal (997.6 pmp), Greece (844.4 pmp) and Israel (691.0 pmp), whereas the prevalence of peritoneal dialysis was highest in the Spanish regions of Galicia (97.6 pmp), Asturias (96.8 pmp) and Basque country (92.6 pmp). The prevalence of patients living with a functioning renal transplant was highest in the Spanish regions of Basque country (670.8 pmp) and Catalonia (659.1 pmp) and Norway (639.2 pmp). Table 5 presents the percentage of patients by established treatment modality (haemodialysis, peritoneal dialysis and transplantation) on 31st December 2012, by age group. For prevalent patients 75 years and over, the percentage of patients receiving haemodialysis varied from 54% in Finland to 98% in Slovenia. In this age group, the percentage of patients receiving peritoneal dialysis was highest in Denmark (16%) and Sweden (15%), whereas Norway reported the highest number of patients living with a functioning kidney allograft (38%). These results were based only on countries with <10% missing values for treatment modality.
Table 4.
Prevalence of RRT on 31 December 2012, by established therapy as pmp (unadjusted) for individual and aggregated data
| Region | All |
All |
HD | PD | Tx | Unknown/missing |
|---|---|---|---|---|---|---|
| N | pmp | pmp | pmp | pmp | pmp | |
| Country/region providing individual patient data | ||||||
| Austria | 8635 | 1022.7 | 460.5 | 46.0 | 516.3 | 0 |
| Belgium | ||||||
| Dutch-speakinga | 7679 | 1206.2 | 641.0 | 57.3 | 507.8 | 0 |
| French-speakinga | 5883 | 1251.3 | 665.1 | 59.8 | 523.0 | 3.5 |
| Bosnia and Herzegovina | 2519 | 718.1 | 642.8 | 23.4 | 51.6 | 0.3 |
| Croatia | 4411 | 1033.2 | 606.5 | 42.9 | 383.9 | 0 |
| Denmark | 4927 | 872.3 | 367.5 | 90.5 | 410.7 | 3.5 |
| Finland | 4373 | 807.7 | 266.0 | 59.3 | 482.5 | 0 |
| France | 74 521 | 1138.7 | 580.3 | 41.9 | 507.4 | 9.2 |
| Greece | 12 598 | 1135.7 | 844.4 | 59.9 | 231.3 | 0 |
| Iceland | 219 | 682.8 | 177.7 | 65.5 | 439.6 | 0 |
| Norway | 4453 | 887.3 | 208.8 | 39.3 | 639.2 | 0 |
| Romaniab | 14 747 | 765.9 | 628.9 | 78.9 | 57.9 | 0.2 |
| Serbia | 5414 | 752.0 | 586.9 | 58.6 | 106.4 | 0.1 |
| Slovenia | 2048 | 995.5 | 662.6 | 22.8 | 310.1 | 0 |
| Spain | ||||||
| Andalusia | 8905 | 1062.0 | 478.0 | 46.6 | 537.2 | 0.1 |
| Aragon | 1452 | 1082.7 | 424.3 | 46.2 | 612.2 | 0 |
| Asturias | 1152 | 1072.3 | 382.6 | 96.8 | 592.9 | 0 |
| Basque country | 2488 | 1140.8 | 377.4 | 92.6 | 670.8 | 0 |
| Cantabriaa | 575 | 972.6 | 340.0 | 66.0 | 566.6 | 0 |
| Castile and Leóna | 2689 | 1063.6 | 432.3 | 69.2 | 552.2 | 9.9 |
| Castile-La Manchaa | 2114 | 1006.6 | 397.1 | 57.1 | 547.1 | 5.2 |
| Catalonia | 9086 | 1200.1 | 492.4 | 48.6 | 659.1 | 0 |
| Community of Madrid | 6338 | 987.2 | 379.6 | 54.7 | 552.9 | 0 |
| Extremadura | 1163 | 1049.5 | 475.6 | 66.8 | 465.6 | 41.5 |
| Galicia | 3271 | 1182.2 | 526.6 | 97.6 | 558.0 | 0 |
| Region of Murcia | 1703 | 1155.0 | 619.2 | 48.8 | 486.3 | 0.7 |
| Valencian Region | 6111 | 1191.4 | 647.7 | 64.9 | 478.4 | 0.4 |
| Sweden | 8882 | 933.0 | 320.2 | 82.9 | 530.0 | 0 |
| The Netherlands | 15 472 | 923.4 | 325.8 | 58.4 | 539.1 | 0.1 |
| United Kingdom | ||||||
| All countriesa | 55 238 | 867.1 | 372.0 | 60.4 | 434.6 | 0.1 |
| Englanda | 46 456 | 868.4 | 373.3 | 62.1 | 433.0 | 0.1 |
| Northern Irelanda | 1557 | 853.8 | 391.0 | 47.2 | 415.7 | 0 |
| Scotland | 4557 | 857.6 | 362.1 | 45.7 | 449.8 | 0 |
| Walesa | 2743 | 892.3 | 358.8 | 67.3 | 465.8 | 0.3 |
| Country/ region providing aggregated patient data | ||||||
| Albania | 909 | 325.1 | 234.6 | 17.9 | 72.6 | 0 |
| Czech Republic | 10 371 | 996.2 | 554.4 | 47.0 | 394.8 | 0 |
| Estonia | 733 | 554.0 | 194.3 | 31.7 | 328.0 | 0 |
| Georgia | 1559 | 545.8 | 479.0 | 14.7 | 48.7 | 3.5 |
| Israelc | 5795 | 732.6 | 691.0 | 41.6 | 0 | |
| Latvia | 926 | 538.2 | 195.3 | 52.9 | 290.0 | 0 |
| Montenegro | 192 | 309.7 | 164.5 | 9.7 | 135.5 | 0 |
| Poland | 28 226 | 747.5 | 463.9 | 29.4 | 254.2 | 0 |
| Portugal | 17 641 | 1670.2 | 997.6 | 70.3 | 602.3 | 0 |
| Russia | 30 349 | 213.9 | 156.8 | 13.2 | 43.9 | 0 |
| Slovakiac | 3220 | 595.1 | 577.5 | 17.6 | 0 | |
| Spain (18 of 19 regions) | 50 909 | 1092.1 | 478.3 | 59.2 | 554.6 | 0 |
| Turkey | 815.6 | |||||
| Ukraine | 6669 | 146.7 | 109.0 | 19.3 | 18.5 | 0 |
HD, haemodialysis; PD, peritoneal dialysis; TX, transplant; pmp, per million population.
aPatients younger than 20 years of age are not reported.
bThe overall prevalence of RRT is underestimated by ∼3% due to an estimated 30% underreporting of patients living with a functioning graft.
cData include dialysis patients only. When cells are left empty, the data are unavailable.
Table 5.
Percentages of established RRT modality (unadjusted) of prevalent patients on 31 December 2012, by age group for the countries/regions providing individual patient data
| Region | All |
0–19 |
20–44 |
45–64 |
65–74 |
≥75 |
||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| HD (%) | PD (%) | TX (%) | Oth (%) | HD (%) | PD (%) | TX (%) | Oth (%) | HD (%) | PD (%) | TX (%) | Oth (%) | HD (%) | PD (%) | TX (%) | Oth (%) | HD (%) | PD (%) | TX (%) | Oth (%) | HD (%) | PD (%) | TX (%) | Oth (%) | |
| Austria | 34 | 4 | 50 | 11 | 9 | 7 | 79 | 5 | 21 | 4 | 65 | 10 | 24 | 5 | 60 | 11 | 39 | 5 | 46 | 11 | 64 | 4 | 19 | 14 |
| Belgium | ||||||||||||||||||||||||
| Dutch-speakinga | 32 | 5 | 42 | 21 | 18 | 8 | 64 | 10 | 19 | 5 | 63 | 13 | 31 | 5 | 44 | 20 | 52 | 3 | 11 | 34 | ||||
| French-speakinga | 41 | 5 | 42 | 13 | 23 | 6 | 62 | 9 | 30 | 4 | 57 | 9 | 39 | 5 | 41 | 15 | 64 | 5 | 13 | 18 | ||||
| Bosnia and Herzegovina | 81 | 3 | 7 | 9 | 65 | 8 | 27 | 0 | 60 | 6 | 20 | 13 | 79 | 3 | 7 | 11 | 91 | 2 | 1 | 5 | 95 | 1 | 0 | 3 |
| Croatia | 58 | 4 | 37 | 1 | 4 | 27 | 69 | 0 | 28 | 6 | 66 | 1 | 46 | 4 | 49 | 1 | 72 | 3 | 23 | 2 | 93 | 3 | 3 | 1 |
| Denmark | 42 | 10 | 47 | 0 | 11 | 7 | 82 | 0 | 25 | 5 | 69 | 1 | 33 | 9 | 58 | 0 | 51 | 14 | 34 | 1 | 78 | 16 | 6 | 0 |
| Finland | 26 | 7 | 60 | 7 | 3 | 7 | 90 | 1 | 16 | 8 | 71 | 5 | 19 | 7 | 68 | 6 | 31 | 7 | 53 | 9 | 54 | 9 | 27 | 10 |
| France | 41 | 4 | 45 | 10 | 11 | 5 | 79 | 6 | 26 | 2 | 67 | 5 | 32 | 2 | 58 | 8 | 44 | 4 | 41 | 11 | 66 | 7 | 10 | 18 |
| Greece | 58 | 5 | 20 | 16 | 31 | 21 | 45 | 3 | 32 | 5 | 45 | 18 | 44 | 5 | 30 | 20 | 66 | 5 | 13 | 16 | 84 | 5 | 1 | 10 |
| Iceland | 26 | 10 | 64 | 0 | 0 | 20 | 80 | 0 | 10 | 4 | 87 | 0 | 23 | 2 | 75 | 0 | 29 | 7 | 64 | 0 | 58 | 36 | 6 | 0 |
| Norway | 24 | 4 | 72 | 0 | 5 | 2 | 93 | 0 | 14 | 2 | 84 | 0 | 16 | 3 | 80 | 0 | 27 | 4 | 69 | 0 | 50 | 12 | 38 | 0 |
| Romaniab | 82 | 10 | 8 | 0 | 53 | 28 | 19 | 0 | 69 | 9 | 21 | 1 | 83 | 9 | 7 | 0 | 88 | 11 | 1 | 0 | 87 | 13 | 0 | 0 |
| Serbia | 66 | 8 | 14 | 12 | 32 | 13 | 48 | 6 | 40 | 6 | 39 | 15 | 66 | 7 | 12 | 14 | 80 | 10 | 1 | 8 | 83 | 9 | 0 | 8 |
| Slovenia | 67 | 2 | 31 | 0 | 29 | 14 | 57 | 0 | 40 | 4 | 56 | 0 | 56 | 3 | 41 | 0 | 74 | 2 | 24 | 0 | 98 | 1 | 1 | 0 |
| Spain | ||||||||||||||||||||||||
| Andalusia | 45 | 4 | 51 | 0 | 9 | 3 | 88 | 0 | 27 | 4 | 69 | 0 | 33 | 4 | 63 | 0 | 52 | 4 | 44 | 0 | 83 | 5 | 12 | 0 |
| Aragon | 39 | 4 | 57 | 0 | 13 | 0 | 88 | 0 | 19 | 8 | 73 | 0 | 27 | 3 | 69 | 0 | 42 | 6 | 51 | 0 | 68 | 2 | 29 | 0 |
| Asturias | 35 | 9 | 55 | 0 | 13 | 25 | 63 | 0 | 21 | 11 | 67 | 0 | 23 | 10 | 67 | 0 | 35 | 6 | 59 | 0 | 64 | 9 | 27 | 0 |
| Basque country | 33 | 8 | 59 | 0 | 3 | 6 | 90 | 0 | 21 | 7 | 72 | 0 | 22 | 10 | 68 | 0 | 34 | 7 | 59 | 0 | 65 | 7 | 28 | 0 |
| Cantabriaa | 35 | 7 | 58 | 25 | 2 | 73 | 0 | 22 | 8 | 70 | 0 | 36 | 6 | 58 | 0 | 71 | 10 | 19 | 0 | |||||
| Castile and Leóna | 41 | 7 | 52 | 1 | 23 | 5 | 71 | 1 | 25 | 6 | 69 | 0 | 38 | 7 | 54 | 0 | 72 | 8 | 18 | 2 | ||||
| Castile-La Manchaa | 39 | 6 | 54 | 1 | 17 | 10 | 73 | 0 | 30 | 6 | 64 | 0 | 40 | 5 | 55 | 1 | 71 | 3 | 26 | 1 | ||||
| Catalonia | 25 | 4 | 55 | 16 | 6 | 5 | 88 | 2 | 13 | 3 | 76 | 8 | 17 | 4 | 66 | 12 | 25 | 5 | 53 | 17 | 48 | 3 | 22 | 27 |
| Extremadura | 45 | 6 | 44 | 4 | 0 | 0 | 100 | 0 | 28 | 10 | 56 | 6 | 30 | 7 | 57 | 5 | 52 | 4 | 40 | 4 | 84 | 4 | 12 | 0 |
| Galicia | 45 | 8 | 47 | 0 | 11 | 28 | 61 | 0 | 24 | 8 | 68 | 0 | 31 | 10 | 60 | 0 | 49 | 6 | 45 | 0 | 81 | 8 | 12 | 0 |
| Community of Madrid | 38 | 6 | 56 | 0 | 11 | 8 | 81 | 0 | 20 | 8 | 72 | 0 | 27 | 6 | 66 | 0 | 41 | 5 | 54 | 0 | 71 | 3 | 26 | 0 |
| Region of Murcia | 54 | 4 | 42 | 0 | 10 | 20 | 70 | 0 | 33 | 7 | 61 | 0 | 36 | 4 | 60 | 0 | 62 | 4 | 34 | 0 | 92 | 3 | 6 | 0 |
| Valencian Region | 54 | 5 | 40 | 0 | 17 | 11 | 72 | 0 | 33 | 7 | 61 | 0 | 41 | 6 | 52 | 0 | 56 | 5 | 39 | 0 | 88 | 4 | 8 | 0 |
| Sweden | 34 | 9 | 57 | 0 | 8 | 9 | 83 | 0 | 20 | 5 | 75 | 0 | 25 | 7 | 68 | 0 | 38 | 11 | 52 | 0 | 69 | 15 | 15 | 0 |
| The Netherlands | 35 | 6 | 58 | 0 | 6 | 5 | 89 | 0 | 20 | 4 | 77 | 0 | 24 | 6 | 70 | 0 | 38 | 7 | 54 | 0 | 74 | 9 | 17 | 0 |
| UK | ||||||||||||||||||||||||
| All countriesa | 41 | 7 | 50 | 2 | 24 | 5 | 69 | 1 | 32 | 6 | 60 | 2 | 50 | 9 | 39 | 2 | 76 | 9 | 12 | 3 | ||||
| Englanda | 41 | 7 | 50 | 2 | 24 | 5 | 69 | 1 | 32 | 6 | 60 | 2 | 50 | 9 | 39 | 3 | 75 | 10 | 11 | 4 | ||||
| Northern Irelanda | 44 | 6 | 49 | 2 | 22 | 7 | 70 | 1 | 33 | 4 | 61 | 2 | 60 | 7 | 30 | 3 | 78 | 7 | 12 | 3 | ||||
| Scotland | 42 | 5 | 52 | 0 | 8 | 15 | 77 | 0 | 27 | 3 | 70 | 0 | 34 | 5 | 61 | 0 | 56 | 8 | 36 | 0 | 80 | 7 | 14 | 0 |
| Walesa | 40 | 8 | 52 | 0 | 22 | 6 | 73 | 0 | 30 | 6 | 64 | 0 | 48 | 10 | 42 | 0 | 77 | 10 | 13 | 0 | ||||
HD, haemodialysis; PD, peritoneal dialysis; TX, transplant; oth, other (includes haemofiltration, haemodiafiltration and unknown).
Categories may not add up because of missing values or rounding off; percentages are row percentages. When cells are left empty (complete) data are unavailable.
aPatients younger than 20 years of age are not reported.
bThe overall prevalence of RRT is underestimated by ∼3% due to an estimated 30% underreporting of patients living with a functioning graft.
The prevalence of children with ESRD by age group and treatment modality is presented in Table 6. Overall on the 31 December 2012 the prevalence of children with ESRD was 54.7 pmarp: the majority (41.5 pmarp) had a functioning renal transplant whereas 8.1 pmarp were receiving haemodialysis and 4.6 pmarp peritoneal dialysis.
Table 6.
Prevalent rates per million age-related population of RRT on 31 December in 2012 for patients aged 0–19 by age and treatment modality
| 0–19 |
0–4 |
5–9 |
10–14 |
15–19 |
||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| All | HD | PD | Tx | All | HD | PD | Tx | All | HD | PD | Tx | All | HD | PD | Tx | All | HD | PD | Tx | |
| pmarp |
pmarp |
pmarp |
pmarp |
pmarp |
||||||||||||||||
| 2012 | 54.7 | 8.1 | 4.6 | 41.5 | 19.4 | 3.9 | 7.3 | 8.1 | 35.9 | 3.5 | 2.9 | 29.3 | 58.4 | 5.9 | 3.4 | 48.8 | 104.0 | 19.0 | 4.8 | 79.1 |
HD, haemodialysis; PD, peritoneal dialysis; TX, transplant; pmarp, per million age-related population.
Renal transplants in 2012
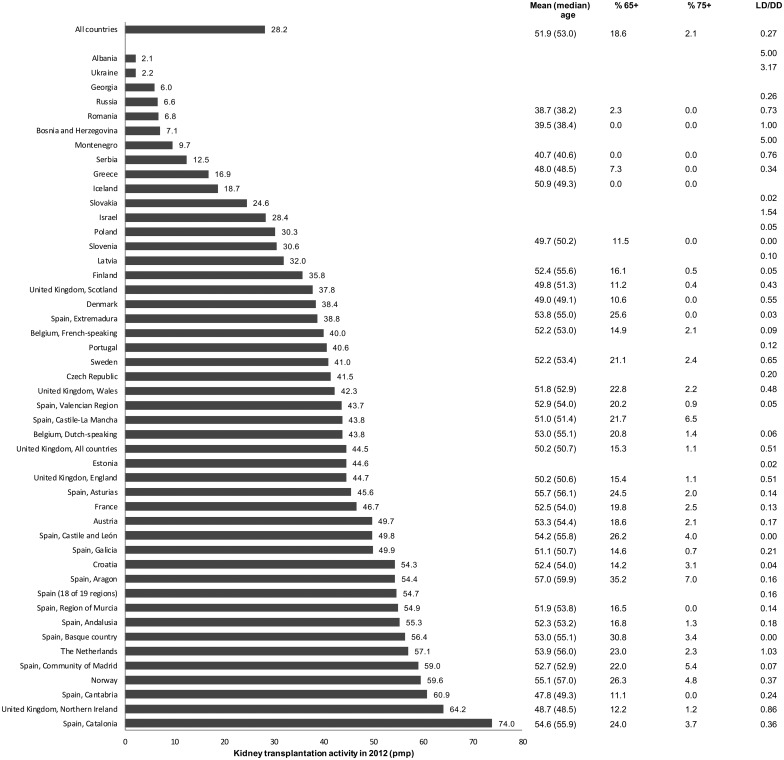
During 2012 there were a total of 15 673 renal transplants performed within the countries and regions reporting to the ERA-EDTA Registry, corresponding to a renal transplantation rate of 28.3 pmp (Figure 6). Of these 12 252 were from a deceased donor source (22.1 pmp, 78%) and 3322 renal transplants were from a living donor source (6.0 pmp, 21%). The kidney transplantation rate varied considerably between the countries and regions reporting to the ERA-EDTA Registry, with the highest rates pmp seen in the Spanish regions of Catalonia and Cantabria (74.0 and 60.9 pmp, respectively) and in Northern Ireland (64.2 pmp). The proportion of living donor to deceased donor transplants also varied considerably within each country and region (Figure 6). Notably, for the countries with a transplantation rate >20.0 pmp, Israel and the Netherlands were the only two countries with a higher proportion of living to deceased donor renal transplants (1.54 and 1.03, respectively).
Fig. 6.
Renal transplants performed, pmp in 2012, unadjusted, with mean and median age at transplantation. Data are from renal registries providing individual patient level data and aggregated data. For the registries providing individual patient data, the percentage of patients aged over 65 years and percentage of patients aged over 75 years at the point of transplantation are presented. For some countries transplantation data were obtained from alternate sources: UK: NHS Blood and Transplant, Slovakia: Slovak Centre of Organ Transplantation, Spain (18 of 19 regions): Organización Nacional de Transplantes. For Romania the transplantation activity reflects 70% of the total transplantation activity in the country, due to an underreporting of pre-emptive transplantations. The mean/median age and percentage over 65 or over 75 years is limited to the adult patient cohort only.
The mean age at renal transplantation (available from the renal registries supplying individual level data and limited to adult patients) was 51.9 years (Figure 6). The mean recipient age at the time of renal transplantation was greatest in the Spanish regions of Aragon (57.0 years) and Asturias (55.7 years) and Norway (55.1 years). The youngest mean recipient ages at the point of renal transplantation were reported by Romania (38.7 years), Bosnia and Herzegovina (39.5 years) and Serbia (40.7 years). The proportion of patients aged 65 years and over at the time of renal transplantation also varied across the registries from 35% in the Spanish region of Aragon to 0% in Iceland, Slovenia and Bosnia and Herzegovina.
Patient and graft survival
Survival analyses included data from 22 registries in 11 countries which provided individual patient data for the period of 2003–2010. The 1-, 2- and 5-year adjusted survival probabilities for patients with ESRD commencing RRT between 2003 and 2007 are presented for the total cohort and for the older age groups in Table 7. Adjustments were made for age, gender and the distribution of primary renal disease (see Appendix 1). Five-year survival for all RRT patients was 59.7% (95% confidence interval, CI: 59.3–60.0) which fell to 39.3% (95% CI: 38.7–39.9) in patients 65–74 years and 21.3% (95% CI: 20.8–21.9) in patients over 75 years.
Table 7.
One, two and five-year patient and graft survival probabilities (95% Confidence interval), for all patients and for patients above 65 years of age, adjusted for age, gender and primary diagnosis
| 2006–10 cohort |
2003–07 cohort |
||||
|---|---|---|---|---|---|
| 1 year | 2 year | 1 year | 2 year | 5 year | |
| Incident RRT patients | |||||
| All patients | 89.7 (89.5–89.8) | 82.2 (82.0–82.5) | 88.7 (88.5–88.9) | 80.6 (80.3–80.9) | 59.7 (59.3–60.0) |
| 65–74 | 82.3 (81.8–82.8) | 70.5 (70.0–71.1) | 80.3 (79.8–80.7) | 67.6 (67.1–68.2) | 39.3 (38.7–39.9) |
| 75+ | 72.6 (72.1–73.2) | 56.7 (56.1–57.3) | 70.4 (69.8–70.9) | 53.2 (52.6–53.8) | 21.3 (20.8–21.9) |
| Patient survival on dialysis | |||||
| All patients | 88.3 (88.1–88.5) | 79.7 (79.4–80.0) | 86.9 (86.7–87.1) | 77.5 (77.2–77.8) | 52.5 (52.0–52.9) |
| 65–74 | 81.9 (81.5–82.4) | 69.7 (69.1–70.2) | 79.9 (79.4–80.4) | 66.9 (66.3–67.4) | 36.7 (36.1–37.3) |
| 75+ | 72.4 (71.9–73.0) | 56.4 (55.8–57.0) | 70.1 (69.5–70.7) | 52.9 (52.2–53.5) | 20.9 (20.4–21.5) |
| Patient survival after first renal transplantation (deceased donor) | |||||
| All patients | 97.4 (97.1–97.6) | 96.1 (95.8–96.4) | 97.2 (97.0–97.4) | 96.0 (95.7–96.2) | 91.5 (91.0–91.9) |
| 65+ | 91.6 (90.4–92.8) | 87.8 (86.4–89.2) | 89.7 (88.3–91.1) | 85.6 (84.0–87.3) | 72.6 (70.5–74.8) |
| Patient survival after first renal transplantation (living donor) | |||||
| All patients | 98.9 (98.7–99.2) | 98.3 (98.0–98.6) | 98.5 (98.1–98.8) | 97.6 (97.1–98.0) | 95.1 (94.4–95.8) |
| 65+ | 95.4 (93.5–97.3) | 92.9 (90.5–95.3) | 95.4 (92.8–98.1) | 92.9 (89.7–96.3) | 84.3 (79.7–89.3) |
| Graft survival after first renal transplantation (deceased donor) | |||||
| All patients | 91.7 (91.3–92.2) | 89.3 (88.8–89.7) | 91.0 (90.6–91.4) | 88.3 (87.9–88.8) | 79.9 (79.2–80.5) |
| 65+ | 85.8 (84.2–87.3) | 81.5 (79.8–83.2) | 82.7 (80.9–84.6) | 78.4 (76.4–80.4) | 64.1 (61.8–66.5) |
| Graft survival after first renal transplantation (living donor) | |||||
| All patients | 95.7 (95.2–96.2) | 93.8 (93.2–94.5) | 95.0 (94.4–95.7) | 93.1 (92.3–93.8) | 86.8 (85.8–87.8) |
| 65+ | 93.0 (90.6–95.4) | 90.2 (87.4–93.1) | 92.5 (89.1–96.0) | 89.4 (85.4–93.5) | 81.3 (76.2–86.6) |
Based on data from Austria, Dutch- and French-speaking Belgium, Denmark, Finland, Greece, Iceland, Norway, the Spanish renal registries of Andalusia, Aragon, Asturias, Basque country, Cantabria, Castile and León, Catalonia, Extremadura and Valencian region, Sweden, the Netherlands and the UK (all countries). Methods are described in Appendix 1.
Affiliated registries
Albania: N. Thereska, A. Strakosha and N. Pasko; Austria: R. Kramar; Belgium, Dutch-speaking: H. Augustijn, B. De Moor and J. De Meester; Belgium, French-speaking: J.M. des Grottes and F. Collart; Bosnia–Herzegovina: H. Resić, B. Prnjavorac and L. Lukić; Croatia: S. Čala; Czech Republic: I. Rychlík, J. Potucek and F. Lopot; Denmark: J.G. Heaf; Estonia: M. Rosenberg, M. Luman and Ü. Pechter; Finland: P. Finne and C. Grönhagen-Riska; France: M. Lassalle and C. Couchoud; Georgia: N. Kantaria and Dialysis Nephrology and Transplantation Union of Georgia; Greece: G.A. Ioannidis; Iceland: R. Palsson; Israel: R. Dichtiar, T. Shohat and E. Golan; Latvia: H. Cernevskis and V. Kuzema; Montenegro: M. Ratkovic, D Radunovic and S. Ivanovic; Norway: T. Leivestad; Poland: B. Rutkowski, G. Korejwo and P. Jagodziński; Portugal: F. Macário, F. Nolasco and R. Filipe; Romania: G. Mircescu, L. Garneata and E. Podgoreanu; Russia: N.A. Tomilina and B.T. Bikbov; Serbia: Working group of Serbian RRT Registry and all of the Serbian renal units; Slovakia: V. Spustová, I. Lajdova and M. Karolyova; Slovenia: J. Buturovic-Ponikvar, J. Gubenšek and M. Arnol; Spain, Andalusia: P. Castro de la Nuez; Spain, Aragon: J.I. Sanchez Miret and J.M. Abad Diez; Spain, Asturias: R. Alonso de la Torre, J.R. Quirós and RERCA working Group; Spain, Basque country: Á. Magaz, J. Aranzabal, M. Rodrigo and I. Moina; Spain, Cantabria: M. Arias Rodríquez and O García Ruiz; Spain, Castile and León: R. González and C. Fernández-Renedo; Spain, Castile-La Mancha: G. Gutiérrez Ávila and I. Moreno Alía; Spain, Catalonia: E. Arcos, J. Comas and J. Tort; Spain, Extremadura: J.M. Ramos Aceitero and M.A. García Bazaga; Spain, Galicia: E. Bouzas-Caamaño and J. Sánchez-Ibáñez; Spain, Community of Madrid: M. Aparicio de Madre and C. Chamorro Jambrina; Spain, Region of Murcia: C. Santiuste de Pablos and I. Marín Sánchez; Spain, Valencian region: O. Zurriaga Llorens and M. Ferrer Alamar; Spain: Spanish RRT National Registry at ONT, Spanish Regional Registries and Spanish Society of Nephrology (SEN); Sweden: K.G. Prütz, L. Bäckman, M. Evans, S. Schön, M. Stendahl and B. Rippe; the Netherlands: A. Hoitsma and A. Hemke; Turkey: G. Süleymanlar, M.R. Maltiparmak and N. Seyahi; Ukraine: M. Kolesnyk, M. Kulyzkyi and S. Nikolaenko; UK, England/Northern Ireland/Wales: all the staff of the UK Renal Registry and of the renal units submitting data; UK, Scotland: all of the Scottish renal units.
ERA-EDTA Registry committee members
R. Vanholder, Belgium (ERA-EDTA President); C. Wanner, Germany (Chairman); F.J. Caskey, UK; F. Collart, Belgium; C. Couchoud, France; D. Fouque, France; J.W. Groothoff, the Netherlands; J.G. Heaf, Denmark; P. Ravani, Italy; I. Rychlik, Czech Republic; F. Schaefer, Germany and S. Schön, Sweden.
ERA-EDTA Registry office staff
K.J. Jager (Managing Director), R. Cornet, F.W. Dekker, G. Guggenheim, A. Kramer, M. Noordzij, M. Pippias, V.S. Stel, K.J. van Stralen and A.J. Weerstra.
Acknowledgements
The ERA-EDTA Registry would like to thank the patients and staff of all the dialysis and transplant units who have contributed data via their national and regional renal registries. In addition, we would like to thank the persons and organizations listed in the paragraph ‘Affiliated registries’ for their contribution to the work of the ERA-EDTA Registry. The ERA-EDTA Registry is funded by the European Renal Association—European Dialysis and Transplant Association (ERA-EDTA).
Conflict of interest statement. None declared. The results presented in this paper have not been published previously in whole or part.
Appendix 1
Coverage of European population by the ERA-EDTA Registry
European countries supplying data to the ERA-EDTA Registry in 2012: Albania, Austria, Belgium, Bosnia and Herzegovina, Croatia, Czech Republic, Denmark, Estonia, Finland, France, Georgia, Greece, Iceland, Latvia, Montenegro, the Netherlands, Norway, Poland, Portugal, Romania, Russia, Serbia, Slovakia, Slovenia, Spain, Sweden, Turkey, Ukraine and the UK.
European countries without renal registries able to supply data to the ERA-EDTA Registry in 2012: Andorra, Armenia, Azerbaijan, Belarus, Bulgaria, Cyprus, Former Yugoslav Republic of Macedonia, Germany, Hungary, Ireland, Italy, Kosovo (under United Nations Security Council Resolution 1244/99), Liechtenstein, Lithuania, Luxembourg, Malta, Moldova, Monaco, San Marino and Switzerland.
The total coverage of the European population by the ERA-EDTA Registry in 2012 was 71.3%. For this calculation only the proportion of the population residing in the European part of Russia and Turkey were considered.
Statistical methods
Patient and graft survival
The survival probabilities of all incident ESRD patients receiving RRT, dialysis patients and of patients receiving a first renal transplant between 2003 and 2007 or between 2006 and 2010 are presented in Table 7. The Cox regression model was used for the adjusted survival analyses for both the total group and the older subgroup of patients (65–74 and 75 years and over). The patients were followed until 31st December 2012.
For the analysis of patient survival on RRT, the first day of RRT was taken as the starting point and the event studied was death. Censored observations were recovery of renal function, loss to follow-up and end of follow-up time. Adjustments were made for fixed values for age (60 years), gender (60% men) and primary renal disease (20% diabetes mellitus, 17% hypertension/renal vascular disease, 15% glomerulonephritis and 48% other cause). In all the analyses of the older subgroups the corresponding fixed values were used with the exception of age.
For the analysis of patient survival on dialysis the first day on dialysis was taken as the starting point, the event studied was death and censored observations were recovery of renal function, loss to follow-up, end of follow-up time and renal transplantation. Adjustments were made for fixed values of age (60 years), gender (60% men) and primary renal disease (20% diabetes mellitus, 17% hypertension/renal vascular disease, 15% glomerulonephritis and 48% other cause).
For the analysis of patient and graft survival after transplantation, the date of the first renal transplantation was defined as the first day of follow-up. The event studied for the patient survival after transplantation was death, while for the graft survival the events were graft failure and death. Censored observations were loss to follow-up and end of the follow-up time. Adjustments were made for fixed values of age (45 years), gender (60% men) and primary renal disease (10% diabetes mellitus, 8% hypertension/renal vascular disease, 28% glomerulonephritis and 54% other cause).
Patients for whom age, gender or primary renal disease was missing were excluded from the analysis.
References
- 1.Eurostat. http://epp.eurostat.ec.europa.eu/portal/page/portal/population/data/database Date of extraction: 15 August 2013. Table: average population by sex and five-year age groups.
- 2.ERA-EDTA Registry: ERA-EDTA Registry Annual Report 2012. Academic Medical Center, Department of Medical Informatics, Amsterdam, the Netherlands, 2014.