Abstract
The 2012 ERA-EDTA Registry Annual Report contains both good news and bad news. On the bright side, the 2-year survival of patients starting renal replacement therapy (RRT) for chronic kidney disease (CKD), on dialysis or receiving a living-related kidney transplantation, has progressively increased to 82.2, 79.7 and 98.3%, respectively, whereas for cadaveric kidney transplantation it remains stable (96.0–96.1%). On the dark side, inequalities persist between European citizens in access to renal transplantation and in incidence and prevalence of RRT. Living in Greece, Belgium (French- or Dutch-speaking) or Portugal (the GBP countries) is associated with higher chances of initiating RRT than living in other European countries. The adjusted RRT incidence for GBP countries was 188, 201-174 and 220* (* unadjusted) pmp in 2012, respectively (versus 122, 114 and 97 pmp in the Netherlands or two Spanish regions bordering Portugal). In lower income countries, a low RRT incidence may represent lack of access to needed healthcare (e.g. Montenegro 26 pmp). However, how can the high incidence and prevalence of RRT in the GBP countries be explained? Do GBP citizens have access to RRT that is denied, rejected or considered unnecessary in other high income countries? Does the GBP healthcare system fail to prevent progression of CKD? Do local genetic or environmental factors favour CKD progression? Unravelling the underlying reasons is an urgent research need: only an understanding of the causes will allow correction of the problem. Unavailability of data from some large countries (e.g. Germany and Italy) is not helpful.
Keywords: access to healthcare, chronic kidney disease, dialysis, inequality, mortality
The recent publication of the 2012 ERA-EDTA Registry Annual Report contains both good news and bad news [1]. On the bright side, survival of patients on renal replacement therapy (RRT) for end-stage chronic kidney disease (CKD) is progressively increasing as observed when 2012 data are compared with 2011 and 2010 data [1–3] (Figure 1). On the dark side, the 2012 report shows persistence of inequalities in the incidence and prevalence of RRT and in access to optimal therapeutic modalities, such as kidney transplantation, across different European countries (Figures 2 and 3), that appear to be unexplained by demography or by per capita gross domestic product (Figure 4). Three countries, Greece, Belgium and Portugal, the GBP (pronounced GeeBeeP) countries, top the charts of incidence and prevalence of RRT one more year. These differences may point out serious issues with public health planning, access or provision of predialysis healthcare or access to RRT in Europe—although it is yet unclear whether the problem lies with the GBPs or the rest of Europe.
Fig. 1.
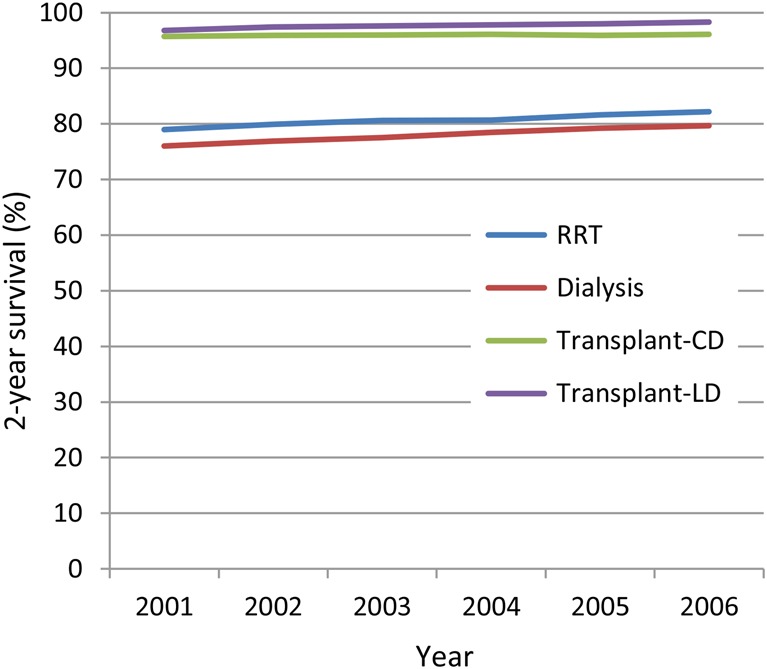
Two-year survival on RRT. Improving life expectancy in RRT, dialysis or living donor transplantation (LD), but stabilization in cadaveric donor transplantation (CD).
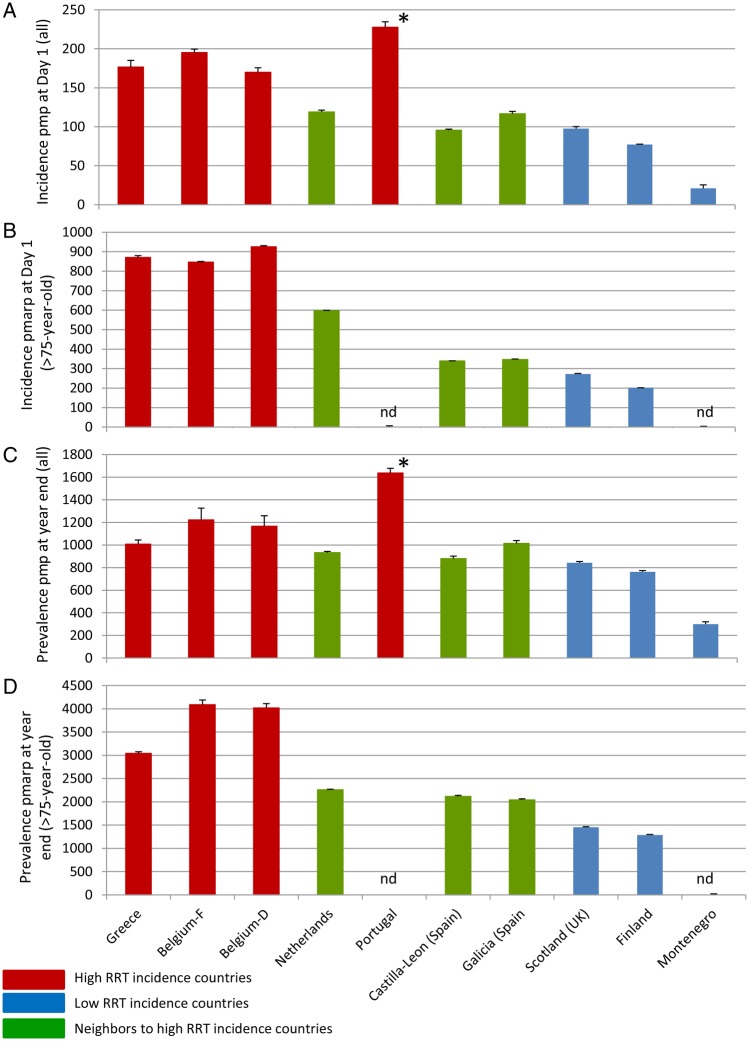
Fig. 2.
Mean 2010–12 adjusted incidence and prevalence data for selected countries and regions. (A) Incidence of RRT, pmp at Day 1 standardized to the age and gender distribution of the EU27 population. (B) Incidence of RRT, pmarp at Day 1 for those over 75 years of age. 2010–11 non-standardized 2012: standardized to the age and gender distribution of the EU27 population. (C) Prevalence of RRT, pmp on 31 December, standardized to the age and gender distribution of the EU27 population. (D) Prevalence of RRT, pmarp on 31 December, for those over 75 years of age. 2010–11 non-standardized 2012: standardized to the age and gender distribution of the EU27 population. Note the difference in scale between whole population values (A and C) and over 75-year-old values (B and D). Data expressed as mean + SD of years 2010–12. Nd: no data, *unadjusted. Belgium-D: Belgium Dutch-speaking (Flanders), Belgium-F: Belgium French-speaking (Wallonia).
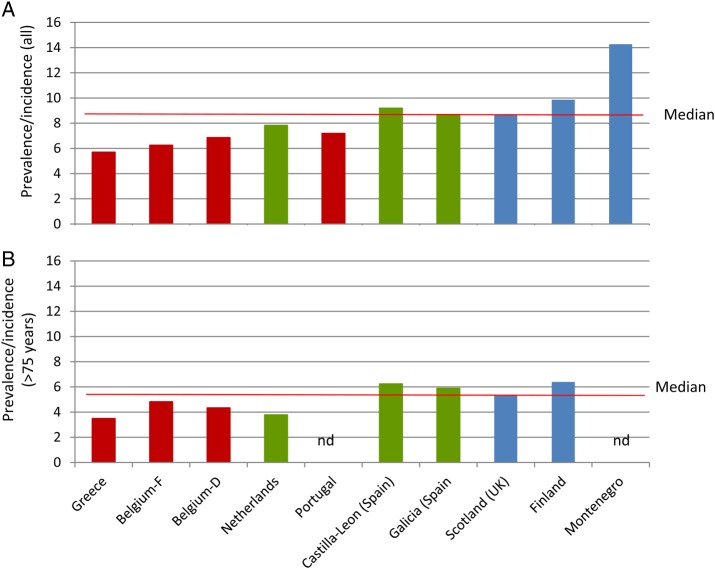
Fig. 3.
Mean 2010–12 adjusted prevalence/incidence for selected countries and regions. (A) Mean 2010–12 adjusted prevalence/incidence for the whole RRT population. (B) Mean 2010–12 adjusted prevalence/incidence for patients >75-year-old. Note same scale for both graphs. *unadjusted. Belgium-D: Belgium Dutch-speaking (Flanders), Belgium-F: Belgium French-speaking (Wallonia).
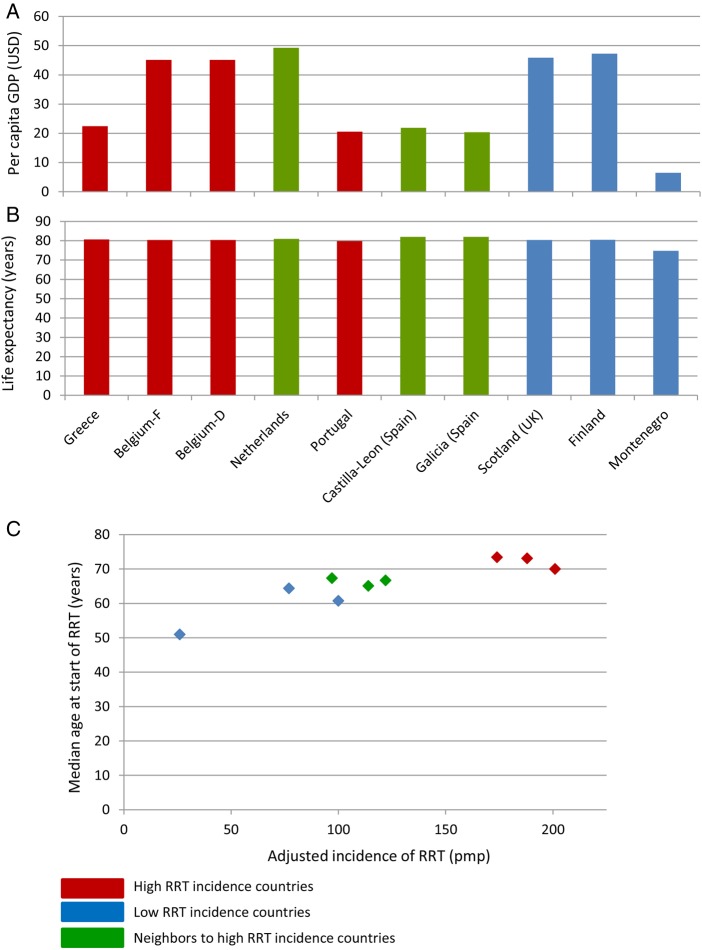
Fig. 4.
Some factors potentially influencing incidence and prevalence of RRT. (A) Per capita GDP at current prices—US dollars.
Source: UNdata 2012 (https://data.un.org/Data), except for Scotland and Spanish Regions 2013 (http://www.ine.es/en/prensa/np835_en.pdf). Belgium GDP for both Belgium regions. Differences in income do not appear to explain differences in RRT incidence and prevalence in neighbouring countries or regions, although the very low income in Montenegro may relate to low RRT prescription. USD: United States dollars. (B) Life expectancy 2010–15. With the exception of low income Montenegro, the life expectancy is very similar for countries with striking differences in RRT prescription. This does not support the hypothesis that early death from other (cardiovascular?) causes explains the low RRT incidence and prevalence in high income countries.
Source: UNdata (https://data.un.org/Data). Country, not regional data presented. (C) Median age at start of RRT in the ERA-EDTA Registry 2012 Report versus incidence of RRT in the same report. In countries with lower RRT incidence, the median age at start of RRT appears to be lower, suggesting that countries with higher RRT incidence start older patients in RRT and this may contribute to differences in RRT epidemiology between countries. In (C) country-level data are presented for Belgium. Belgium-D: Belgium Dutch-speaking (Flanders), Belgium-F: Belgium French-speaking (Wallonia).
Cautious optimism
The 2-year survival of patients starting RRT has progressively increased for cohorts from 2001 to 2006, measured either as overall survival for patients starting RRT (to 82.2% for the cohort starting in 2006 reported in the ERA-EDTA Registry 2012 report), on dialysis (79.7%) or receiving living-related kidney transplantation (98.3%) (Figure 1) [1–3]. In contrast, 2-year survival for cadaveric kidney transplantation remains stable at 96.0–96.1% for cohorts starting from 2003 to 2006 pointing to a plateau that would need novel approaches to be surpassed. These data are in agreement with other registries reporting increasing overall survival of patients starting RRT in the last decade [4–7]. Similar improvements were observed for 5-year survival, pointing to an overall improvement in the standard of care, unlike the US situation in the 1990s, in which progressive increases in survival at 12 and 24 months were associated with decreasing survival at 5 years [4, 8]. The factors that contributed to that U.S. drop in longer-term survival and whether a similar phenomenon occurred outside this country still need detailed studies, in search of lessons that might be learned and applied to improve the current standard of care.
Cause for concern: inequalities
On the dark side, data point to persistent inequalities between European citizens in incidence and prevalence of RRT and in access to transplantation. Living in Greece, Belgium (both French- and Dutch-speaking) or Portugal (the GBP countries) is associated with higher chances of initiating RRT than living in other European countries. Very high incidence of RRT was also reported in Israel and Georgia in 2012 and in Turkey in 2011 and 2010. The adjusted RRT incidence for GBP countries was 188, 201-174 and 220 pmp in 2012, respectively (although Portugal data are unadjusted). This compares with 122, 114 and 97 pmp in the Netherlands or Spanish regions (Galicia, Castilla-Leon) bordering Portugal (Figure 2A). Moreover, these differences persist when prevalence is examined (Figure 2C), although prevalence/incidence values are lower for high incidence countries (Figure 3). That is, higher incidence is not completely matched by a higher prevalence. One potential explanation is more stringent patient selection in low incidence countries, although better on-RRT care may also contribute. In lower income countries, the low incidence of RRT may represent lack of access to needed healthcare (e.g. Montenegro 26 pmp). However, how can the high incidence and prevalence of RRT in the GBP countries be explained? (Table 1). Some potential explanations are cause of grave concern whereas there are innocent alternatives. Do GBP citizens have access to RRT techniques that are denied to citizens in other high income countries, e.g. adjusted incidence of RRT 100 pmp in Scotland and 77 pmp in Finland? Does the healthcare system fail to prevent progression of CKD in the GBP countries? Are there local genetic or environmental factors that favour progression of CKD and have not been tackled by public health authorities? Are there perverse incentives or forces that favour CKD progression or initiation of RRT? Or it is just a matter of reporting methods or of nephrologist beliefs regarding the timing of initiation of RRT when hard evidence is lacking? Unravelling the underlying reasons for the observed inequalities is an urgent research need: only when the causes are known can corrective measures be applied.
Table 1.
Potential causes of differences in RRT incidence and prevalence
| Very concerning |
| Overuse of RRT |
| Denial of access to RRT |
| Financial incentives to initiate RRT |
| Concerning |
| Different incidence or progression of CKD |
| Public health system fails to prevent development of CKD |
| Healthcare system structure or access results in suboptimal CKD care |
| Different views on the relative value of RRT versus conservative management of ESRD |
| Other |
| Different data reporting methods |
| Refusal of RRT by an informed population when RRT is offered |
Several countries with low incidence and prevalence of RRT have higher incomes than countries with higher prevalence (Figure 4A). The differences do not appear to depend on a better public health system or success in preventing CKD progression in those countries with high income. Thus, some countries with higher income and low RRT incidence start RRT at a median younger age than countries which have both lower income and higher incidence of RRT. In this regard, low overall incidence and prevalence of RRT is frequently associated with low incidence and prevalence of RRT in those aged >75 years (Figures 2B, D and 4C). This is potentially unsettling given that the incidence of RRT increases with age. Thus, the age pattern is consistent with denial of RRT to the elderly, refusal of RRT by the elderly or different criteria for indicating conservative treatment versus RRT in younger or elderly patients in countries with low RRT incidence. In these high income countries, low RRT incidence in the elderly does not appear to depend on economic constraints, as is the case in low income countries. The low RRT incidence may be based on the genuine belief that conservative treatment is the best option for elderly patients with ESRD [9, 10]. In this regard, there is an urgent need for hard evidence on the relative merits of conservative treatment versus RRT in the elderly as well as on the optimal timing of RRT start. If indeed conservative management has clear advantages, then in some countries overdialysis might be an issue. In this regard, a recent survey of nephrologists from 11 European countries disclosed very different practices regarding start of RRT in uncomplicated relatively young (60-year-old) patients: the estimated glomerular filtration rates (eGFRs) at which RRT would be started by different nephrologists ranged from 5 to 20 mL/min/1.73 m2 and this was the most important parameter to initiate RRT in such a patient for a majority of nephrologists [10]. Obviously, starting at an eGFR of 5 or 20 mL/min/1.73 m2 may have a great impact on the incidence of RRT. If the same range would be applied to those over 75 years of age (which was not the subject of the study), it would mean the difference between initiating and never initiating RRT for a great number of patients. Interestingly, nephrologists from countries with a high incidence of RRT more often believed that starting at a GFR > 10.5 mL/min/1.73 m2 is always beneficial compared with respondents from low incidence countries (18 versus 6%). Furthermore, the target eGFR was higher for nephrologists working at for-profit centres. This illustrated another potential issue: hidden incentives in the healthcare system. Further information is needed about the GFR at initiation of RRT in different countries as well as on the use of and acceptance by patients and doctors and outcomes of conservative management of ESRD in the elderly. The fact that differences in prevalence are lower than differences in incidence is concordant with prevalence/incidence value data (Figure 3) and can be interpreted as a high rate of patient loss in some high incidence countries. Whether these shorter periods on RRT in some countries with a high incidence of RRT result in improved patient quality of life and are indeed appreciated by the patient should be clarified.
There are additional hypotheses potentially explaining the lower incidence of RRT coupled to a younger mean age at start of RRT in some high income countries. Patients may be dying earlier from cardiovascular disease and, thus, not living long enough to need RRT. However, life expectancy does not differ much between countries selected for this commentary, except for low income Montenegro (Figure 4B). Public health may also impact the incidence and prevalence of CKD and, thus, of ESRD. Factors potentially involved include the presence of toxins in the environment or food (i.e. the exposome, as an example, aristolochic nephropathy), over-the-counter medication policies (allowing unrestricted access to nephrotoxic drugs) or country-level policies regarding salt or phosphate content in the diet. In addition, the healthcare system may also impact, as an example, whether there is universal unrestricted access to healthcare or to nephrologists.
Transplantation
Transplantation is the best therapeutic option for most patients on RRT. However, huge differences in access to transplantation are observed between European countries. The percentage of patients on RRT who have a functioning kidney graft ranges from 7% in Bosnia and Herzegovina to ≥60% in Norway, Finland and Iceland [1].
Black-out
Also worrisome is the fact that RRT epidemiology data from some countries big and small (e.g. Germany, Ireland, Hungary and Italy, among others) at the core of Europe are not available, as it was the case for 2011 and, except for some parts of Italy, for 2010 [1–3]. This virtual black-out makes comparison with other European countries difficult that could improve the standard of care and to detect pockets of substandard care or endemic CKD hotspots.
In summary, the ERA-EDTA Registry continues to provide a wealth of data on the epidemiology of RRT. Key points of this year's report include (i) the improving outcomes for patients on RRT, with exception of recipients of cadaveric donor kidneys, (ii) the persistence of inequalities in RRT incidence and prevalence and transplantation availability in different European countries that may hide CKD hotspots, substandard CKD care, overuse of RRT or lack of access to needed RRT; and (iii) a preoccupying lack of data from key countries. There is an urgent need to study the factors underlying the inequalities in RRT incidence and prevalence and to identify and correct potential substandard care for some European citizens.
Conflict of interest statement
None declared.
Acknowledgements
Grant support was provided by ISCIII and FEDER funds PI13/00047, Sociedad Española de Nefrologia, ISCIII-RETIC REDinREN/RD012/0021, Comunidad de Madrid CIFRA S2010/BMD-2378. Salary support was provided by Programa Intensificación Actividad Investigadora (ISCIII/Agencia Laín-Entralgo/CM) to A.O.
References
- 1.Pippias M, Stel VS, Abad Diez JM, et al. Renal replacement therapy in Europe: a summary of the 2012 ERA-EDTA Registry Annual Report. CKJ 2015; 8: 248–261 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Noordzij M, Kramer A, Abad Diez JM, et al. Renal replacement therapy in Europe: a summary of the 2011 ERA-EDTA Registry Annual Report. Clin Kidney J 2014; 7: 227–238 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kramer A, Stel VS, Abad Diez JM, et al. Renal replacement therapy in Europe—a summary of the 2010 ERA–EDTA Registry Annual Report. Clin Kidney J 2013; 6: 105–115 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ortiz A, Covic A, Fliser D, et al. Epidemiology, contributors to, and clinical trials of mortality risk in chronic kidney failure. Lancet 2014; 383: 1831–1843 [DOI] [PubMed] [Google Scholar]
- 5.Mitsnefes MM, Laskin BL, Dahhou M, et al. Mortality risk among children initially treated with dialysis for end-stage kidney disease, 1990–2010. JAMA 2013; 309: 1921–1929 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Steenkamp R, Shaw C, Feest T. UK Renal Registry 15th annual report: chapter 5 survival and causes of death of UK adult patients on renal replacement therapy in 2011: national and centre-specific analyses. Nephron Clin Pract 2013; 123(Suppl 1): 93–123 [DOI] [PubMed] [Google Scholar]
- 7.Roberts MA, Polkinghorne KR, McDonald SP, et al. Secular trends in cardiovascular mortality rates of patients receiving dialysis compared with the general population. Am J Kidney Dis 2011; 58: 64–72 [DOI] [PubMed] [Google Scholar]
- 8.Collins AJ, Foley RN, Gilbertson DT, et al. The state of chronic kidney disease, ESRD, and morbidity and mortality in the first year of dialysis. Clin J Am Soc Nephrol 2009; 4(Suppl 1): S5–11 [DOI] [PubMed] [Google Scholar]
- 9.Tonkin-Crine S, Okamoto I, Leydon GM, et al. Understanding by older patients of dialysis and conservative management for chronic kidney failure. Am J Kidney Dis 2015; 65: 443–450 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.van de Luijtgaarden MW, Noordzij M, Tomson C, et al. Factors influencing the decision to start renal replacement therapy: results of a survey among European nephrologists. Am J Kidney Dis 2012; 60: 940–948 [DOI] [PubMed] [Google Scholar]