Abstract
An international group of clinicians working in the field of dysmorphology has initiated the standardization of terms used to describe human morphology. The goals are to standardize these terms and reach consensus regarding their definitions. In this way, we will increase the utility of descriptions of the human phenotype and facilitate reliable comparisons of findings among patients. Discussions with other workers in dysmorphology and related fields, such as developmental biology and molecular genetics, will becomemore precise. Here we introduce the anatomy of the male and female genitalia, and define and illustrate the terms that describe the major characteristics of these body regions.
Keywords: nomenclature, definitions, ontology, genitalia, male genitalia, female genitalia, anatomy, anthropometry, morphology, dysmorphology
INTRODUCTION
General
This paper is part of a series of papers defining the morphologic variations of the human body detectable by surface examination [Biesecker et al., 2009; Carey et al., 2009; Hall et al., 2009;Hennekam et al., 2009; Hunter et al., 2009; Allanson et al., 2009b]. Additional papers on the morphology of the limbs and trunk are in preparation. The series is accompanied by an introductory paper describing general aspects of this project [Allanson et al., 2009a]. The reader is encouraged to consult the introduction when using the definitions.
MALE EXTERNAL GENITALIA
Anatomy of the Male External Genitalia
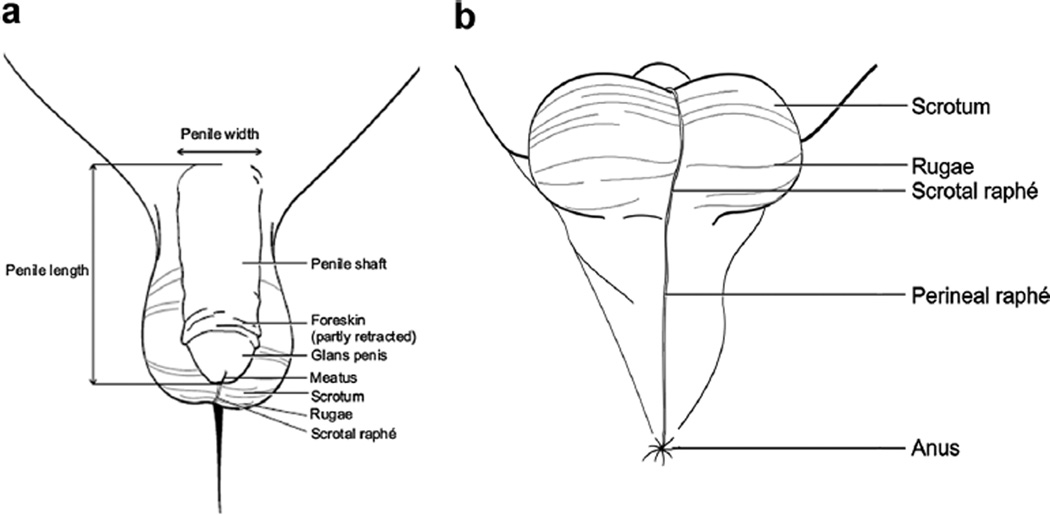
The normal anatomy of the male external genitalia is shown in Figures 1 and 2. Some anatomical landmarks deserve specific mention as these are not used consistently.
FIG. 1.
Anatomy of external male genitalia. a: Anterior overview. b: Inferior overview.
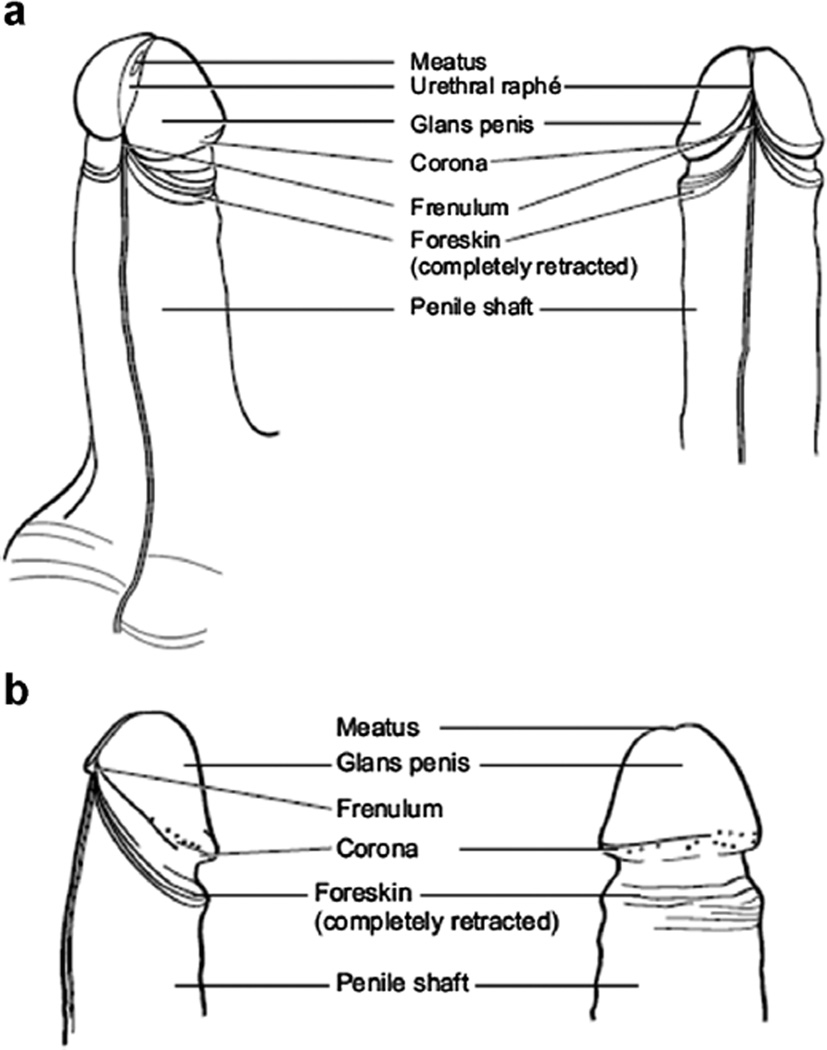
FIG. 2.
Anatomy of external male genitalia. a: Anterior and side view of the penis with the preputium removed. b: Detailed side and posterior view of the penis with the preputium removed.
Penile shaft: the part of the penis running from the abdominal wall to the corona.
Penile raphé: slightly elevated line of tissue on the ventral aspect of the shaft of the penis, continuing on to the foreskin.
Corona: a semi-circular prominence of the glans of the penis, situated on the dorsum of the penile shaft. In a flaccid penis it is usually covered by the foreskin except in men who have been fully circumcised.
Glans penis: the rounded tip of the penis, demarcated from the shaft by the sulcus. In a flaccid penis it is usually covered by the foreskin except in men who have been fully circumcised.
Meatus: a slit-like opening on the tip of the glans of the penis, running in a ventral–dorsal direction.
Urethral raphé: a slightly elevated ridge of skin extending from the ventral aspect of the meatus to the frenulum.
Foreskin: a loose fold of skin (outer) and mucous membrane (inner) arising from the shaft of the penis, and in a flaccid penis usually covering the glans. In young boys, the demarcation of the foreskin and glans is often not fully formed, prohibiting retraction of the foreskin below the corona.
Frenulum of the foreskin: a band of elastic tissue covered by mucous membrane on the ventral side of the penis attaching the foreskin to the glans of the penis.
Scrotum: a loose sac of skin containing the testes and located inferior to the base of the penis. Scrotal skin has small elevations (rugae) on the surface and is more pigmented than the remainder of the body, irrespective of ethnic background, although this distinction is more obvious in individuals with a dark skin.
Scrotal raphé: a slightly elevated ridge of tissue running from the base of the penis to the midline of the perineum. The scrotal raphe is in continuity with the penile raphé superiorly and the perineal raphé inferiorly. Slight hyperpigmentation of the genital raphés (penile, scrotal, and perineal) is almost invariably present.
Perineal raphé: a slightly elevated ridge of tissue in the midline of the perineum running from the inferior attachment of the scrotum to the anus and in continuity with the scrotal raphé.
Testis: a mobile ovoid-shaped organ palpable and usually partly visible through the skin of the scrotum.
Epididymis: an oblong organ attached to the testis. The epididymis can be visualized by trans-illumination and is palpable in the scrotum.
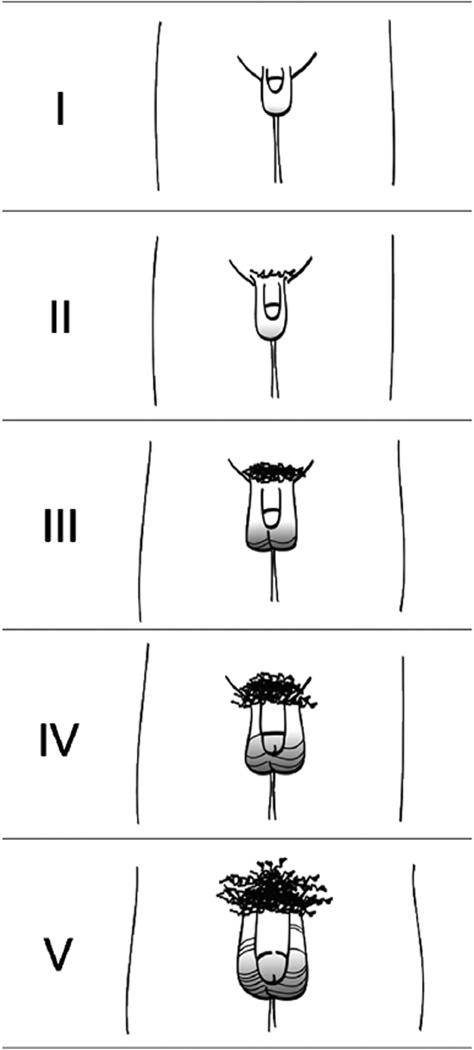
Pubertal Stages
The timing of puberty varies greatly in the general population and is influenced by genetic and environmental factors [Gajdon et al., 2009]. In evaluating the pubertal development in a child, ethnic background and intra-familial variation should be taken into account. Tanner stages are commonly used to score pubertal development [Tanner, 1986]. In males, the stages are determined by assessing the length and width of the penis, size of the testes, and pubic hair growth (Fig. 3). As each of these components is defined here separately, the pubertal stages are not discussed in further detail.
FIG. 3.
Puberty stages males according to Tanner [1986].
Measurements of the Male External Genitalia
Measurements of the penis are possible using sliding calipers or a straight-edged plastic ruler. The reliability of measurements using a tape measure is poor. Penile length is measured from the base of the gently stretched penis at the pubic symphysis to the tip of the glans without including the foreskin. Fat pads at the base of the penis influence this measurement and the ruler should be pressing against the pubic symphysis. Determining of the size of the testes are performed either by estimation of the size of the testes by palpation and comparison with a Prader orchidometer (Fig. 4), or by measuring width and length of the testis using calipers, straight ruler, or tape measure. Results of measurements determined by calipers, rulers or tape measures typically yield larger estimates of the testicular volume than those by Prader orchidometers, and, over time, measurements in individual patients should be performed using the same method.
FIG. 4.
Prader orchidometer.
The reader is referred to the Handbook of Normal Physical Measurements [Hall et al., 2007] for detailed descriptions of measurement techniques and growth standards. Except for pubertal developmental stages, growth standards are provided for Caucasians of Northern European extraction only, but abundant data on penile growth in individuals of other ethnic backgrounds have been published.
Anatomical Variation
Variations of the anatomy of the male external genitalia may be assessed as quantitative (objective or anthropometric) traits and qualitative (subjective or categorical) features:
Variations in length: long penis; short penis.
Variations in width: wide penis; narrow penis.
Variations in length and width: absent penis; absent foreskin; small scrotum; absent scrotum, (apparently) absent testis; small testis; large testis; supernumerary testis.
Variations in shape or position: ambiguous genitalia; bladder exstrophy, bifid penis; penile torsion, epispadias; hypospadias; microphallus; penile chordee; webbed penis; penoscrotal transposition; accessory scrotum, bifid scrotum; shawl scrotum; ectopic scrotum, cryptorchidism; hydrocele.
Variations in cutaneous manifestations: freckled genitalia; hyperpigmented genitalia; hypopigmented genitalia; sparse pubic hair.
The various findings are listed alphabetically. If a feature is indicated in bold -italics, the feature is listed and a definition is available. The terms are alphabetized based on the physical feature, not the modifier.
Investigating the genitalia should always be performed with the observed person in a relaxed position. The presence of a nurse or parent is advisable.Small children are best investigated in theirparent’s lap. The testes can be palpated in a supine position but itmay be useful to ask the observed person to squat as this allows better palpation. Repeat genital examinations may be embarrassing for the subject [Lee et al., 2006] and should be performed only when indicated.
DEFINITIONS
Anorchia: See Testis, (apparently) absent
Aphallia: See Penis, absent
Aposthia: See Foreskin, absent
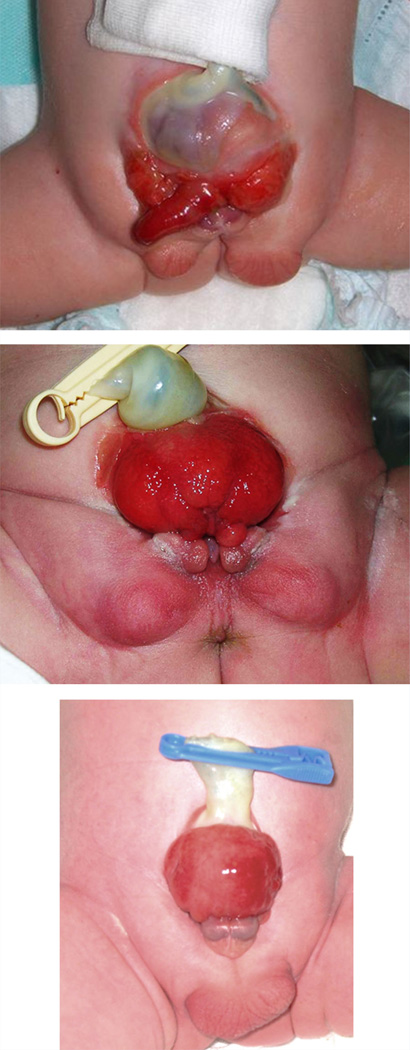
Bladder, Exstrophy
Definition: Eversion of the posterior bladder wall through the congenitally absent lower anterior abdominal wall and anterior bladder wall (Fig. 5). objective
FIG. 5.
Bladder exstrophia. Courtesy of Dr. Anne-Karoline Ebert. Reprinted with permission from Ebert et al. [2009].
Comments: Exstrophy of the bladder can be associated with Epispadias and Bifid penis or in females with Bifid clitoris, a bifid uterus, and a Septated vagina, each of which should be coded separately.
Chordee
Definition: Ventral, lateral, or ventrolateral bowing of the shaft and glans penis of more than 30 degrees (Fig. 6). objective
FIG. 6.
Chordee. Courtesy of Dr. Montasser El-Koutby. Reprinted with permission from El-Koutby and El Gohary [2010].
Comments: The degree of variation of penis curvature is a continuum, but traditionally 30 degrees is considered the threshold for surgical intervention on chordee [Bologna et al., 1999]. Bowing usually becomes more obvious in an erect penis, but is frequently also palpable when stretching a flaccid penis. Chordee can be congenital or acquired; if the former, it can be associated with Webbed Penis or Hypospadias, which should be coded separately.
Cryptorchidism
Definition: Testis in inguinal canal. objective
Comments: The gonad is mobile and can be retracted superiorly by the cremaster muscle reflex stimulated, for instance, by cold or touch. A retracted testis is not cryptorchidism. An abdominal testis cannot be distinguished by physical examination from an (Apparently) absent testis and requires radiological (or, rarely, surgical) procedures for assessment.
Synonym: Testis, undescended
Diphallus: See Penis, bifid
Epispadias
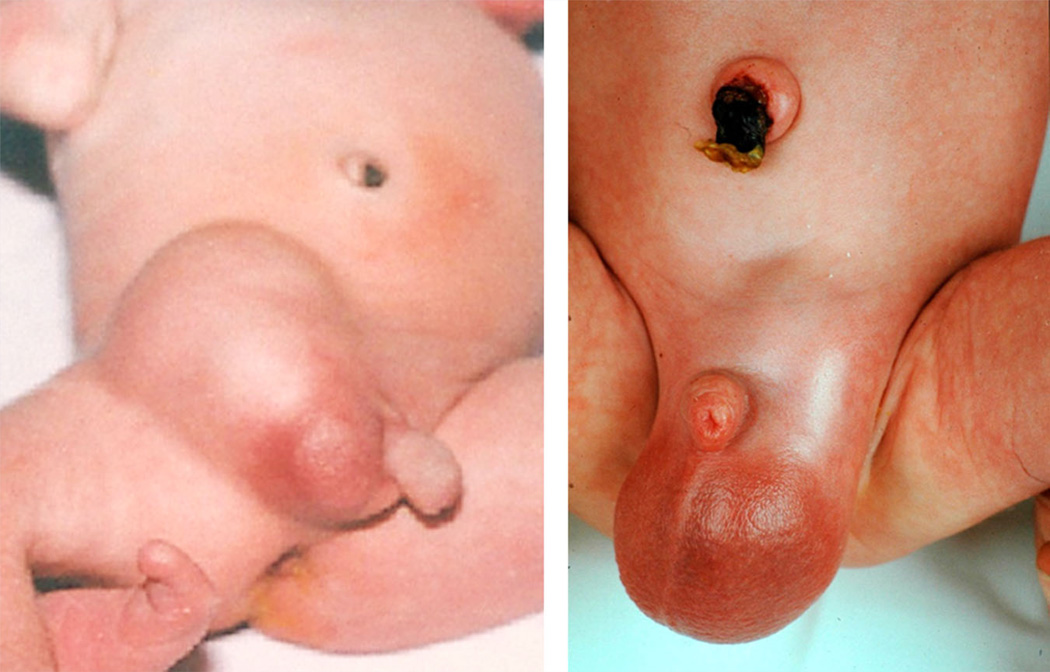
Definition: Dorsal placement of the urethral opening (Fig. 7). objective
FIG. 7.
Epispadias. Courtesy of Dr. Anne-Karoline Ebert. Reprinted with permission from Ebert et al. [2009].
Comments: Epispadias may be present in a phenotypic male, female, or an individual with ambiguous genitalia. A meatus in a phenotypic male may be positioned either on the glans (glandular or balanic epispadias), the shaft (penile epispadias) or at the attachment of the penis to the abdominal wall (penopubic epispadias). Alternatively, the urethra may be an open groove along the dorsal shaft of the penis, with no readily recognized meatus. Epispadias is a frequent component of Bladder exstrophy, but should be coded separately.
Foreskin, Absent
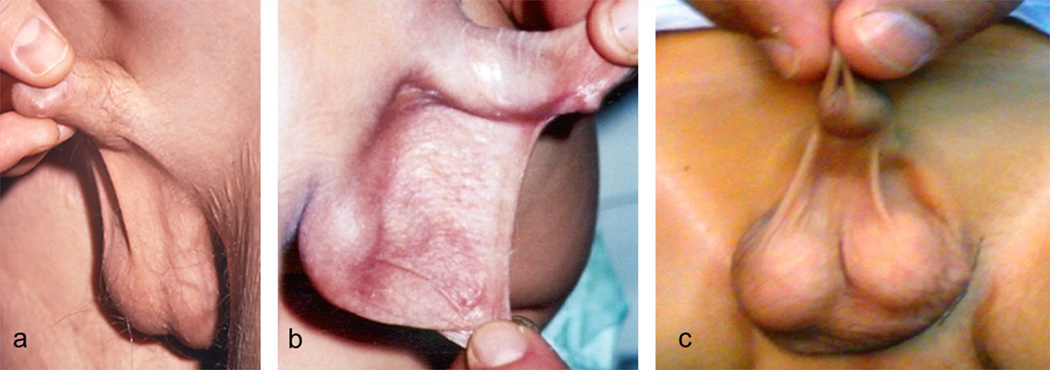
Definition: Complete absence of the foreskin (Fig. 8). objective
FIG. 8.
Foreskin, absence. Courtesy of Dr. S. Sadeghipour and Dr. N. Esmailzadehha. Reprinted with permission from Sadeghipour and Esmailzadehha [2010].
Comments: Absence of the foreskin can be accompanied by Cryptorchidism and Hypospadias, which should be coded separately.
Synonym: Aposthia
Foreskin, aposthia: See Foreskin, absent
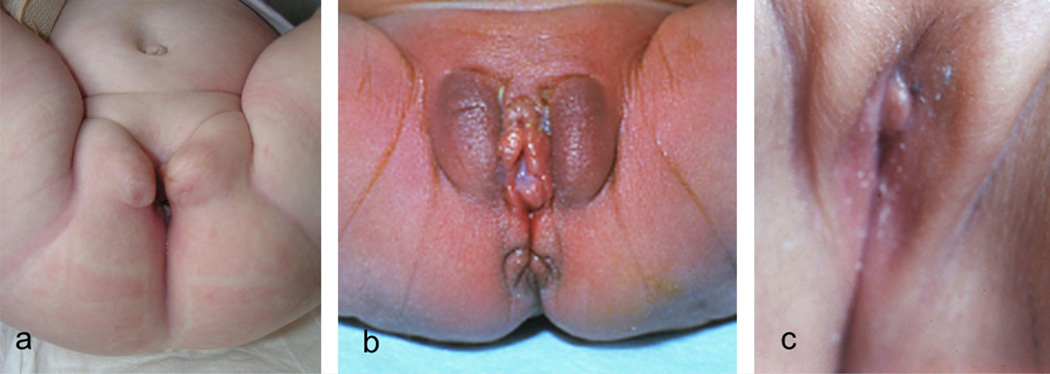
Genitalia, Ambiguous
Definition: External genitalia without typical male or female appearance (Fig. 9). subjective
FIG. 9.
Ambiguous genitalia.
Comments: Note that this term can include or combine variations in size and shape, with partial or complete absence of structures. It is preferable to describe the individual components, which are defined below. It is nonetheless a widely used bundled term and as such is retained here (for the definition of a “bundled term” see Allanson et al. [2009a]). The distinction of this finding from a marked degree of Hypospadias is an example of how this term can be problematic.
Synonym: Intersex genitalia
Genitalia, ephelides: See Genitalia, freckled
Genitalia, Freckled
Definition: One or more brown punctate macules on the skin of the genitalia (Fig. 10). objective
FIG. 10.
Freckled genitalia.
Comments: This should be differentiated from Hyperpigmented genitalia in which an area larger than a freckle or the complete external genitalia are hyperpigmented. The description should be qualified by a description of the affected part(s).
Synonym: Genitalia, ephelides
Genitalia, Hyperpigmented
Definition: Localized or generalized increased genital pigmentation (Fig. 11). subjective
FIG. 11.
Hyperpigmented genitalia in males (left and middle) and female (right).
Comments: This is an assessment of the relative pigmentation of the genitalia compared to the overall pigmentation of the individual. Hyperpigmentation can affect other parts of the body or be restricted to the genitalia. Genital hyperpigmentation can be generalized or localized. Localized areas of hyperpigmentation of the glans of the penis are especially common. This should be differentiated from Freckled genitalia in which one or more small, focal areas of hyperpigmentation are present. Localized hyperpigmentation can be objectively determined due to the difference from the immediate surrounding tissue color, while generalized hyperpigmentation may be more difficult to determine and is therefore a subjective manifestation. If the finding is localized, the description should be appended with a description of the affected part(s).
Replaces: Penile melanosis
Genitalia, Hypopigmented
Definition: Localized or generalized decreased genital pigmentation (Fig. 12). subjective
FIG. 12.
Hypopigmented genitalia in male (left) and females (middle and right).
Comments: This is an assessment of the relative pigmentation of the genitalia compared to the overall pigmentation of the individual. Hypopigmentation can affect other parts of the body or be restricted to the genitalia. Genital hypopigmentation can be generalized or localized. Localized hypopigmentation can be objectively determined due to the difference fromthe immediate surrounding tissue color, while generalized hypopigmentation may bemore difficult to determine and is therefore a subjective manifestation.
Genitalia, intersex: See Genitalia, ambiguous
Hydrocele
Definition: Presence of increased fluid around testis leading to an enlarged scrotum or hemiscrotum (Fig. 13). Subjective
FIG. 13.
Hydrocele.
Comments: The testis itself may not be palpable in the presence of large fluid amounts. The assessment of this finding may be aided by trans-illumination.
Hypospadias
Definition: Ventral placement of the urethral opening (Fig. 14). objective
FIG. 14.
Various forms of hypospadias. There are various classification systems (see text).
Comments: Hypospadias is categorized in several ways, the most classical one being first degree (urethral opening on the ventral glans), second degree (urethral opening on the ventral shaft), and third degree (urethral opening on the perineum). Second degree hypospadias is frequently accompanied by Chordee of the penis, which should be coded separately. The widely used Duckett classification [Baskin and Duckett, 1996] categorizes hypospadias into glandular, coronal, distal penile shaft (or “anterior”) subgroup, mid-shaft (or “middle”) subgroup, or proximal penile shaft, penoscrotal, and perineal (or “posterior”) subgroup. A surgically oriented categorization to classify hypospadias has been developed based on the position of the division of the corpus spongiosum relative to the penile shaft and bony structures of the pelvis [Orkiszewski, 2012].
Macro-orchidism: See Testis, large
Macropenis: See Penis, long
Megalopenis: See Penis, long
Micropenis: See Penis, short
Microphallus
Definition: Length of penis more than 2 SD below the mean for age accompanied by hypospadias (Fig. 15). objective OR
FIG. 15.
Microphallus.
Apparently decreased length of penis for age with hypospadias. Subjective
Comments: Traditionally a distinction is made between a Short penis, a short penis with otherwise normal anatomy, versus microphallus, a short penis with hypospadias. Penile length is the distance between the midline attachment of the gently stretched, flaccid penis above the pubic symphysis and tip of the glans. Details on measurement of the penis can be found elsewhere [Hall et al., 2007]. There are no reliable studies showing a relation between ethnicity and penile length [Adams, 1996]. There are some data on interethnic differences in the lower limit of penile length in newborns [Cheng and Chanoine, 2001].Ashort penis should be differentiated from an inconspicuous penis, for instance due to excessive suprapubic fat (“buried”) [Bergeson et al., 1993]. We also recognize that shortnessof a penis is defined by some subspecialists as penile length more than 2.5 SD below the mean.
Replaces: Penis, hypoplastic; Penis, hypotrophic; Penis, small
Penile melanosis: See Genitalia, hyperpigmented
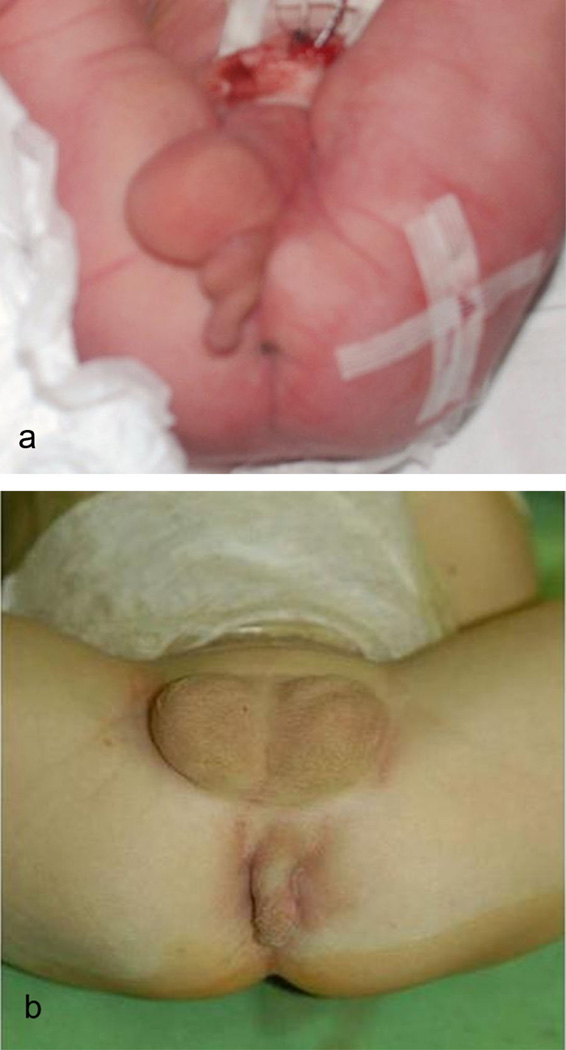
Penis, Absent
Definition: Lack of recognizable penile structures (Fig. 16). objective
FIG. 16.
Absent penis. Courtesy of Dr. Ruchi Gupta (panel A) and Dr. Li Fubiao (panel B). Panel A reprinted with permission from Rattan et al. [2010]. Panel B reprinted with permission from Wang et al. [2011].
Comments: Absence of the penis is always accompanied by abnormal position of the meatus (usually in the perineum, sometimes in the rectum), may be accompanied by Cryptorchidism [Chibber et al., 2005], and is often associated with non-genital anomalies [Roth et al., 1981], which all should be coded separately. Absent penis should be differentiated froma penis concealed within pre-pubic fat tissue.
Synonym: Aphallia
Penis, Bifid
Definition:Twopenile structures, separated from the tip to the base of the shaft (Fig. 17). ObjectiveOR
FIG. 17.
Bifid penis.
Longitudinal indentation, cleft, or depressionof the glans with or without involvement of the shaft of the penis. Objective
Comments:Note the second definition denotes a bundled term, but as it is commonly used in practice it is kept here. In individuals with complete duplication often one will find Hypospadias, Epispadias, Bladder exstrophy, or Bifid scrotum, which should be coded separately, as well as urinary tract duplications, renal anomalies, and gastrointestinal duplications [Keckler et al., 2009]. The terms indicate the presence of (part of) two penises, but do not indicate whether they are caused by splitting or double formation.
Synonym: Diphallus; Penis, duplicated
Penis, duplicated: See Penis, bifid
Penis, hyperplastic: See Penis, long
Penis, hypertrophic: See Penis, long
Penis, hypoplastic: See Penis, short
Penis, hypotrophic: See Penis, shor
Penis, large: Not defined as this is a bundled term encompassing both a Long penis and Wide penis
Penis, Long
Definition: Penile length more than 2 SD above the mean for age (Fig. 18). objective OR
FIG. 18.
Long penis (in newborn children).
Apparently increased penile length for age. Subjective
Comments: Penile length is the distance between the midline attachment of the gently stretched, flaccid penis above the pubic symphysis and tip of the glans. Details on measurement of the penis can be found elsewhere [Hall et al., 2007]. This measurement and assessment may not be possible for an individual with Chordee. There are no reliable studies showing a relation between ethnicity and penile length [Adams, 1996].
Replaces: Penis, hyperplastic; Penis hypertrophic; Megalopenis; Macropenis; Penis, large
Penis, Narrow
Definition: Penile width more than 2 SD below the mean for age. objective OR
Circumference of the flaccid penis more than 2 SD below the mean for age. objective OR
Apparently decreased penile width for age. subjective
Comments: Penile width is the distance between left and right side of the flaccid penis at the attachment to the skin above the pubic symphysis. Normal values for penile width only exist for newborns [Cheng and Chanoine, 2001] and adults [Schneider et al., 2001]. Alternatively, penile circumference can be measured, as normal values are available at all ages [Damon et al., 1990]. Note the site of measurement (base; mid-shaft; under glans) may differ in the various studies [Ajmani et al., 1985; Ponchietti et al., 2001; Cinaz et al., 2012]. It is important that the measurement site be consistent with that of the published norms.
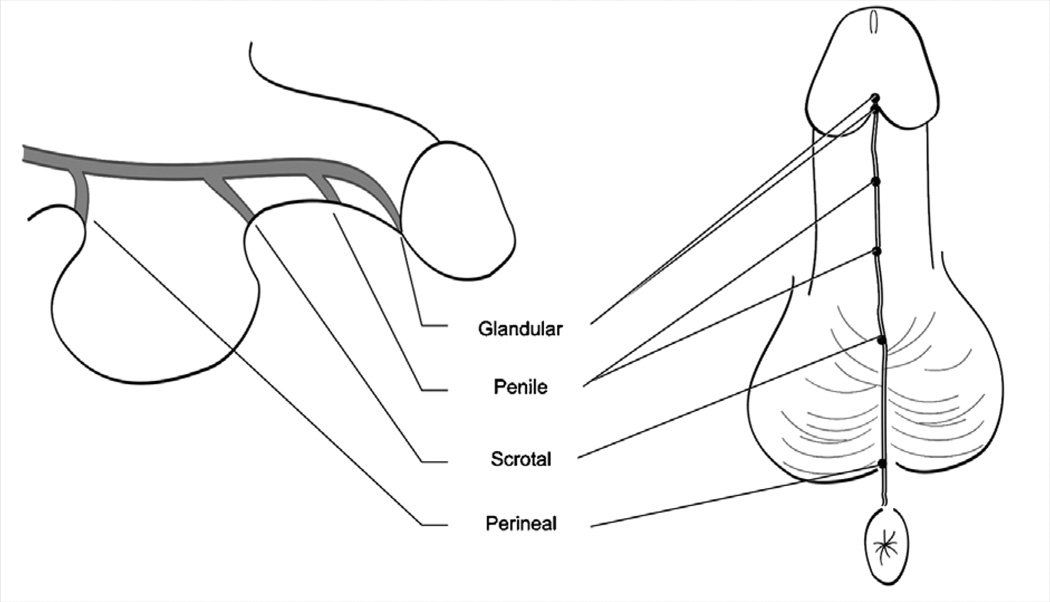
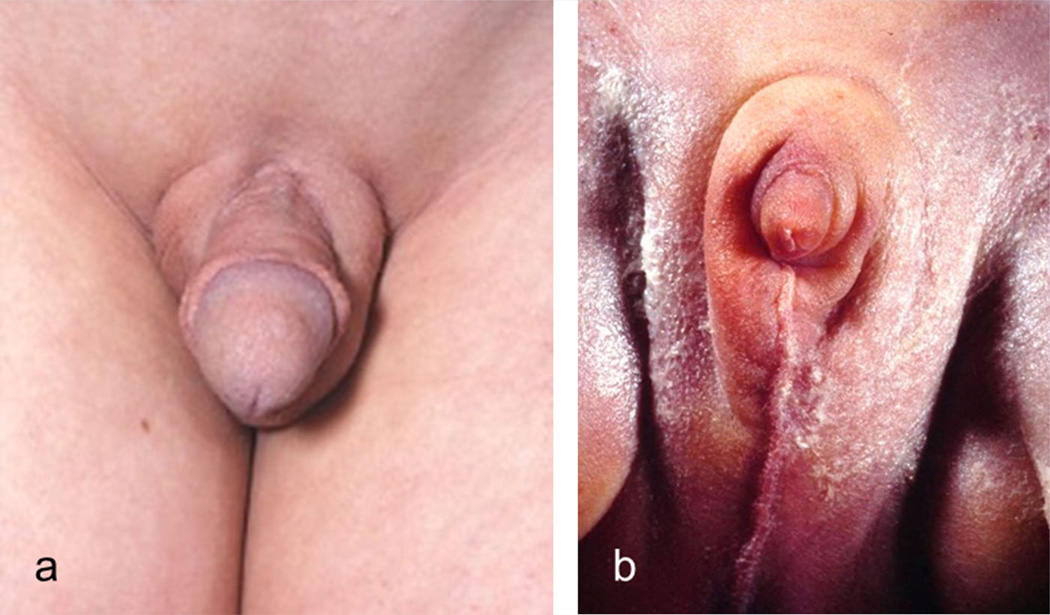
Penis, Short
Definition: Penile length more than 2 SD below the mean for age (Fig. 19). objective OR
FIG. 19.
Short penis. Please note that on panel C the penis seems to be absent, but can be made visible in the same patient in panel D by pushing surrounding tissues backward.
Apparently decreased penile length for age. subjective
Comments: Traditionally a distinction is made between micropenis, a short penis with otherwise normal anatomy versus Microphallus, a short penis with hypospadias. Penile length is the distance between the midline attachment of the gently stretched, flaccid penis above the pubic symphysis and tip of the glans. Details on measurement of the penis can be found elsewhere [Hall et al., 2007]. There are no reliable studies showing a relation between ethnicity and penile length [Adams, 1996]. There are some data on interethnic differences in the lower limit of penile length in newborns [Cheng and Chanoine, 2001]. A short penis should be differentiated from an inconspicuous penis, for instance due to excessive suprapubic fat (“buried”) [Bergeson et al., 1993]. Micropenis (or small penis) is sometimes used as a bundled term for short and narrow penis. We recommend that the term not be used in this way and that narrowness be coded separately. We also recognize that shortness of a penis is defined by some subspecialists as penile length more than 2.5 SD below the mean.
Synonym: Micropenis
Replaces: Penis, hypoplastic; Penis, hypotrophic; Penis, small Penis, small: Not defined as this is a bundled term encompassing both Short penis and Narrow penis.
Penis, Torsion of the
Definition: Rotated position of the glans, with or without the penile shaft, of 30 degrees or more (Fig. 20). objective
FIG. 20.
Torsion of the penis. Courtesy of Dr. Barry Kogan. Reprinted with permission from Bauer and Kogan [2009].
Comments: Penile torsion is defined traditionally as being between 30 and 180 degrees rotation [Montag and Palmer, 2011]. Penile torsion is usually counter clockwise and is often associated with Chordee and Hypospadias, which should be coded separately.
Penis, Webbed
Definition: Ventral skinfold extending from penis to scrotum (Fig. 21). objective
FIG. 21.
Webbed penis. Panels B and C courtesy of Dr. Montasser El-Koutby. Reprinted with permission from El-Koutby and El Gohary [2010].
Comments: The distal limit of the skinfold can be located on the penile shaft or the tip of the penis. Webbing has been subclassified into a primary form and secondary form (for instance after circumcision) [El-Koutby and Amin el Gohary, 2010] and may be accompanied by Chordee, which should be coded separately.
Penis, Wide
Definition: Distance between left and right side of the flaccid penis at the attachment to the skin above the pubic symphysis more than 2 SD above the mean for age (Fig. 22). objective OR
FIG. 22.
Wide penis (newborn child). Courtesy of Dr. Sheela Nampoothiri.
Circumference of the flaccid penis more than 2 SD above the mean for age. objective OR
Apparently increased distance for age between the left and right side of the flaccid penis at the attachment to the skin above the pubic symphysis. subjective
Comments: Normal values for penile width only exist for newborns [Cheng and Chanoine, 2001] and adults [Schneider et al., 2001]. Alternatively penile circumference can be measured, as normal values are available at all ages [Damon et al., 1990]. Note the site ofmeasurement (base; mid-shaft; under glans) may differ in the various studies [Ajmani et al., 1985; Ponchietti et al., 2001; Cinaz et al., 2012]. It is important that the measurement site be consistent with that of the published norms.
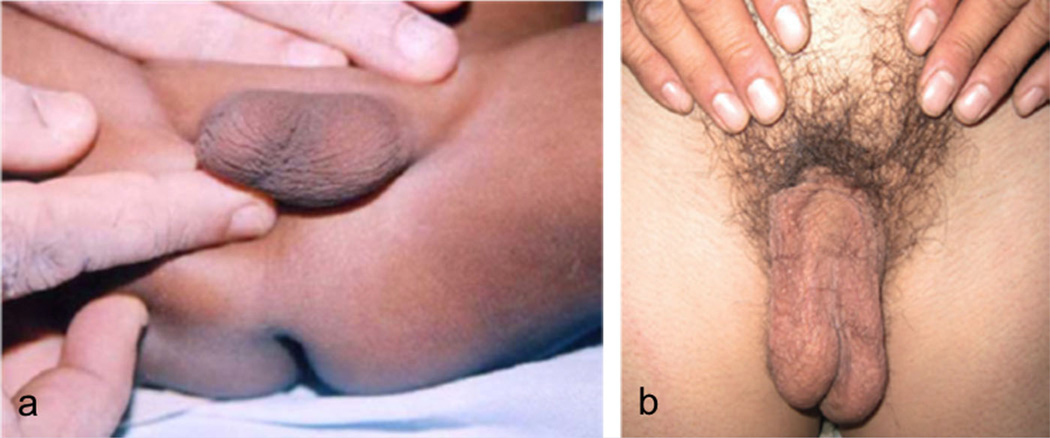
Penoscrotal transposition
Definition: Positioning of the scrotum superior to the penis (Fig. 23). objective
FIG. 23.
Penoscrotal transposition. Courtesy of Dr. Trine Prescott and Dr. Kathrine Bj?rgo (panel A) and Dr Khaled Fathi (panel B). Panel B reprinted with permission from Fathi et al. [2010].
Comments: The base of the penis is entirely covered by the scrotum, which may be Bifid. If so, this should then be coded separately. If only part of the scrotum is located superior to the penis, the term Overriding scrotum is used instead.
Synonyms: Prepenile scrotum
Replaces: Doughnut scrotum
Polyorchidism: See Testis, supernumerary
Pubic hair, hypotrichosis of: See Pubic hair, sparse
Pubic hair, Sparse
Definition: Apparently decreased number of hairs per unit area relative to the pubertal development as judged by other components of pubertal maturity (Fig. 24) subjective
FIG. 24.
Sparse pubic hair (in a pubertal male).
Comments: (Pubic) hypotrichosis should not be used as a synonym as, formally, it means underdevelopment of the hair. No normal values for the number of hairs per unit area exist.
Replaces: Pubic hair, thinning; Pubic hair, thin; Pubic hypotrichosis
Pubic hair, thin(ning): See Pubic hair, sparse
Scrotum, Absent
Definition: Absence of scrotal sac (Fig. 25). objective
FIG. 25.
Absent scrotum.
Comments: Both the sac and rugae are absent. This finding may be accompanied by an (Apparently) absent testis and Cryptorchidism [Janoff and Skoog, 2005], which should be coded separately.
Scrotum, Accessory
Definition: Additional scrotum, or part of a scrotum in an abnormal location (Fig. 26). objective
FIG. 26.
Accessory scrotum. Courtesy of Dr. Paval Ganesan (panel A) and Dr. Zoran Gucev (panel B). Panel B reprinted with permission from Gucev et al. [2010].
Comments: An accessory scrotum is typically located on the perineum, frequently associated with perineal lipoma, and occasionally with Hypospadias or Bifid penis, which should be coded separately.
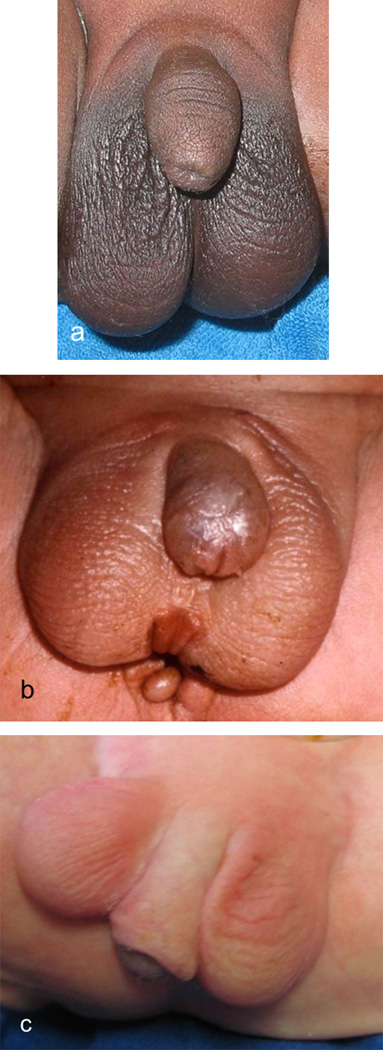
Scrotum, Bifid
Definition: Midline indentation or cleft of the scrotum (Fig. 27). objective
FIG. 27.
Bifid scrotum. Note that in panels A and B the scrotum shows only a mild indentation and in panel C the scrotum is completely bifid.
Comments:Atestis may or may not be present in each half of the scrotum.
Scrotum, doughnut: See Penoscrotal transposition
Scrotum, Ectopic
Definition: Scrotum in a position other than the usual position inferior to the base of the penis (Fig. 28). objective
FIG. 28.
Ectopic scrotum (panel a courtesy of Dr. Zoran Gucev, panel b courtesy of Dr Stefanos Gardikis). Panel A reprinted with permission from Gucev et al. [2010]. Panel B reprinted with permission from Gardikis et al. [2012].
Comments: This term is distinguished from Accessory scrotum, as there is no significant scrotal tissue in the normal position in ectopic scrotum. This definition excludes the finding of Penoscrotal transposition or Overriding scrotum. Usually the scrotum is split and there is unilateral ectopia. The ectopic scrotum is typically located supra-inguinally, but may be located elsewhere such as on the upper thigh. A testis is commonly present in the ectopic scrotum. Ectopic scrotum can be accompanied by Chordee or Bifid penis [Hoar et al., 1998], which should be coded separately, and by renal and non-urogenital malformations
Scrotum, hypoplastic: See Scrotum, small
Scrotum, hypotrophic: See Scrotum, small
Scrotum, Overriding: See Scrotum, shawl
Scrotum, prepenile: See Penoscrotal transposition
Scrotum, Shawl
Definition: Superior margin of the scrotum superior to the base of the penis (Fig. 29). Subjective
FIG. 29.
Shawl scrotum. Note only partly overriding scrotum in panel A and complete overriding in panel B.
Comments: A congenital overriding scrotum may disappear with growth and development, especially during puberty. If the entire scrotum is located superior to the penis, the term Penoscrotal transposition is used instead.
Synonym: Overriding scrotum
Scrotum, Small
Definition: Apparently small scrotum for age (Fig. 30). subjective
FIG. 30.
Small scrotum.
Comments: A small scrotum is often accompanied by Cryptorchidism which should be coded separately. The size of the scrotum is dependent on the ambient temperature: a low temperature may cause the testes to retract, leading to the false impression of a small scrotum.
Synonym: Scrotum, underdeveloped
Replaces: Scrotum, hypotrophic; Scrotum, hypoplastic
Scrotum, underdeveloped: See Scrotum, small
Testis, (Apparently) Absent
Definition: Testis not palpable in the scrotum or inguinal canal.objective
Comments: Absence can be congenital or not (vanishing testis). Definitive assessment can only be made by imaging or surgical studies, in order to exclude an intra-abdominal testis, which should be coded as Cryptorchidism. True absence of a testis can be difficult to prove. Anorchia is true absence of both testes, and can only be determined by imaging or surgical studies.
Testis, enlarged: See Testis, large
Testis, hyperplastic: See Testis, large
Testis, hypertrophic: See Testis, large
Testis, hypoplastic: See Testis, small
Testis, hypotrophic: See Testis, small
Testis, Large
Definition: Size of the testis more than 2 SD above the mean for age (Fig. 31). objective OR
FIG. 31.
Large testis.
Apparently increased size of the testis for age. subjective
Comments: Details on measurement of the testis can be found elsewhere [Hall et al., 2007]. This is in fact a bundled term indicating an increase in testis length and width but is retained here because of its utility and the availability of objective normal values.
Synonym: Macro-orchidism; Testis, overdeveloped
Replaces: Testis, hyperplastic; Testis, hypertrophic, Testis enlarged
Testis, overdeveloped: See Testis, large
Testis, Small
Definition: Size of the testis more than 2 SD below the mean for age (Fig. 32). objective OR
FIG. 32.
Small testis (in a pubertal boy).
Apparently decreased size of the testis for age. subjective
Comments: Details on measurement of the testis can be found elsewhere [Hall et al., 2007].
Synonym: Testis, underdeveloped
Replaces: Testis, hypoplastic; Testis, hypotrophic
Testis, Supernumerary
Definition: More than two testes present in a hemi-scrotum or one inguinal canal (Fig. 33). objective
FIG. 33.
Supernumerary testis (two testes in left hemiscrotum indicated by arrows). Courtesy of Dr. Ali Feyzullah S?ahin. Reprinted with permission from Yalcinkaya et al. [2011].
Comments: Urologists use a subclassification of supernumerary testes [Bergholz and Wenke, 2009]. A supernumerary testis may reside in the abdomen, but this is not included in the present definition as it cannot be determined by physical examination. A supernumerary testis can be difficult to distinguish from a large epididymis. Triorchidism is sometimes used to describe a single supernumerary testis.
Synonym: Polyorchidism
Testis, underdeveloped: See Testis, small
Testis, undescended: See Cryptorchidism
FEMALE EXTERNAL GENITALIA
Anatomy of the Female External Genitalia
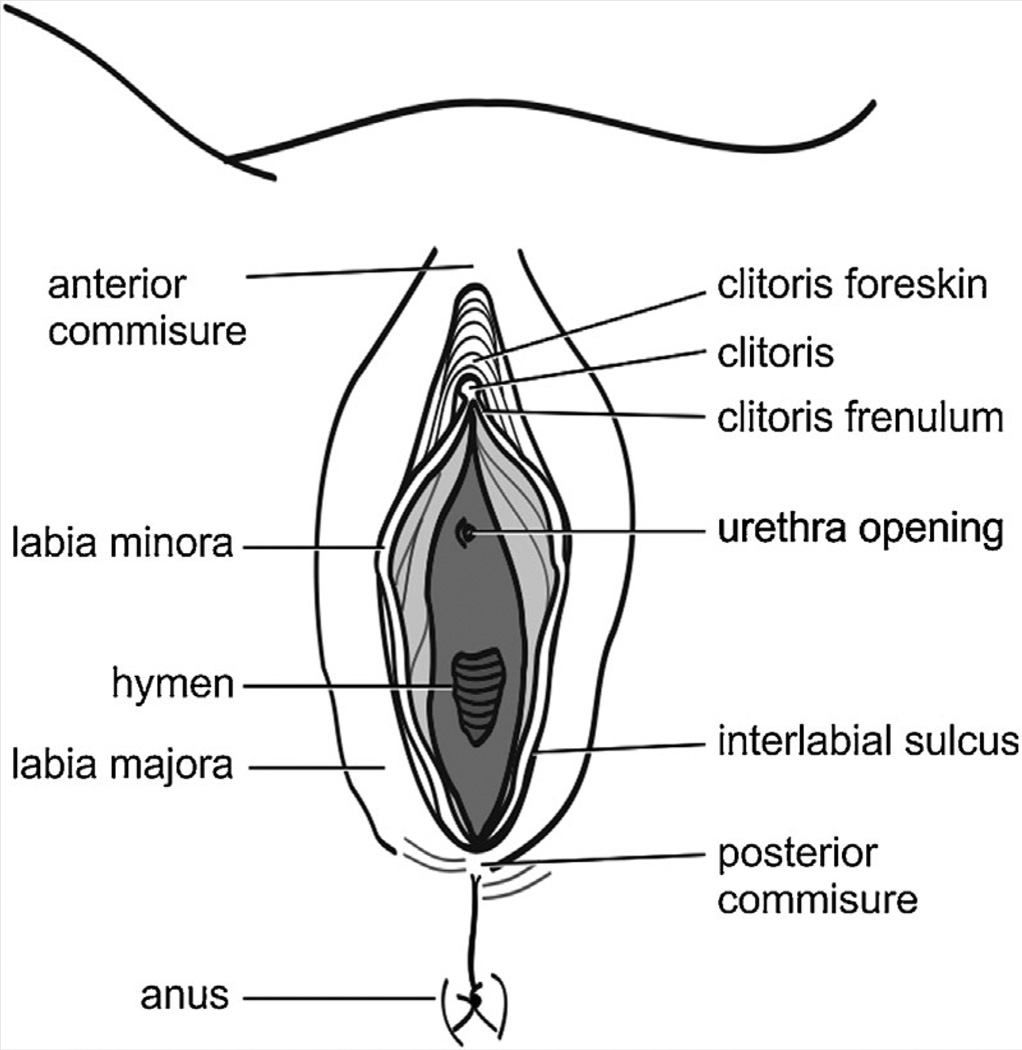
Normal anatomy of the female external genitalia is shown in Figure 34. Some anatomical landmarks deserve specific mention as these are not always used consistently.
FIG. 34.
Anatomy of female external genitalia.
Labia majora: Two relatively broad soft tissue skin-covered swellings running alongside one another inferoposteriorly, in close proximity anteriorly at the mons pubis (sometimes called anterior commissure) and joining at the posterior commissure. They encircle the vulval vestibule, which contains the urethra and vagina. In young girls the skin is smooth and only slightly hyperpigmented, but the skin gradually undergoes further hyperpigmentation, hair growth and rugae formation. The inner part is covered by thin skin and mucous membrane and contains many sebaceous glands.
Labia minora: Two relatively narrow, hairless soft tissue swellings medial to the labia majora, covered with mucous membranes, running inferoposteriorly from the base of the clitoris to fuse posteriorly at the fourchette. There is marked variation in size of the labia minora, and, in postpubertal females, they often protrude beyond the labia majora.
Interlabial sulci: the regions between the inner parts of the labia majora and outer parts of the labia minora.
Clitoris: Cap-shaped organ supero-anterior to the entrance of the vagina, partly covered by a foreskin (hood). The size of the clitoris depends on whether it is erect or flaccid.
Clitoral foreskin (hood ): Skin fold overriding and partially covering the glans of the clitoris and inferioposteriorly continuous with the labia minora.
Clitoral frenula: Small elastic tissue folds covered by mucous membranes running from the glans of the clitoris to the labia minora.
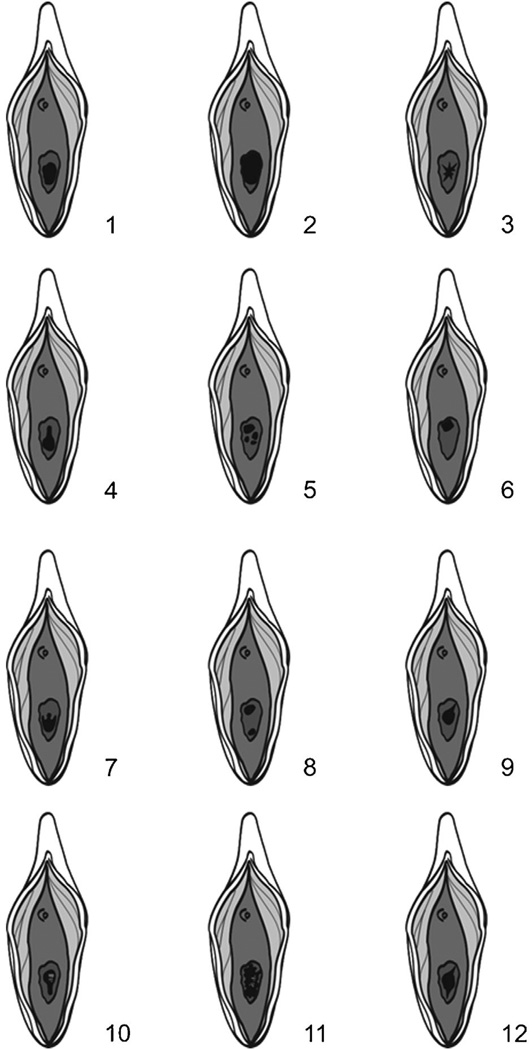
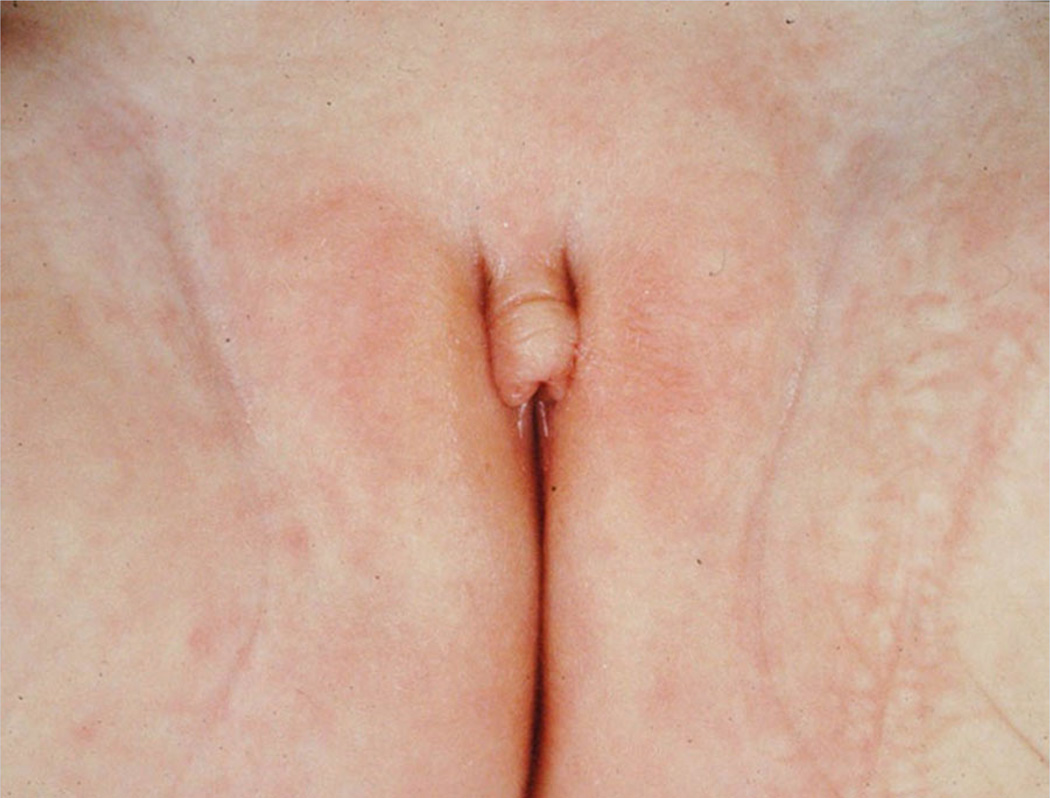
Hymen: Epithelial fold partly covering the inferior opening of the vagina. The virginal hymen has an opening that is variable in size, shape, and position (Fig. 35).
FIG. 35.
Variation in opening of virginal hymen in newborns.
Vagina: Hollow organ ending inferiorly at the vulval vestibule (introitus) between the labia minora, and superiorly at the cervix of the uterus. The vagina is collapsed most of the time.
Vulva: Region delimited by the labia majora and containing the labia minora, clitoris, urethral meatus, and introitus. The vulval vestibule (introitus) is the region between the labia minora.
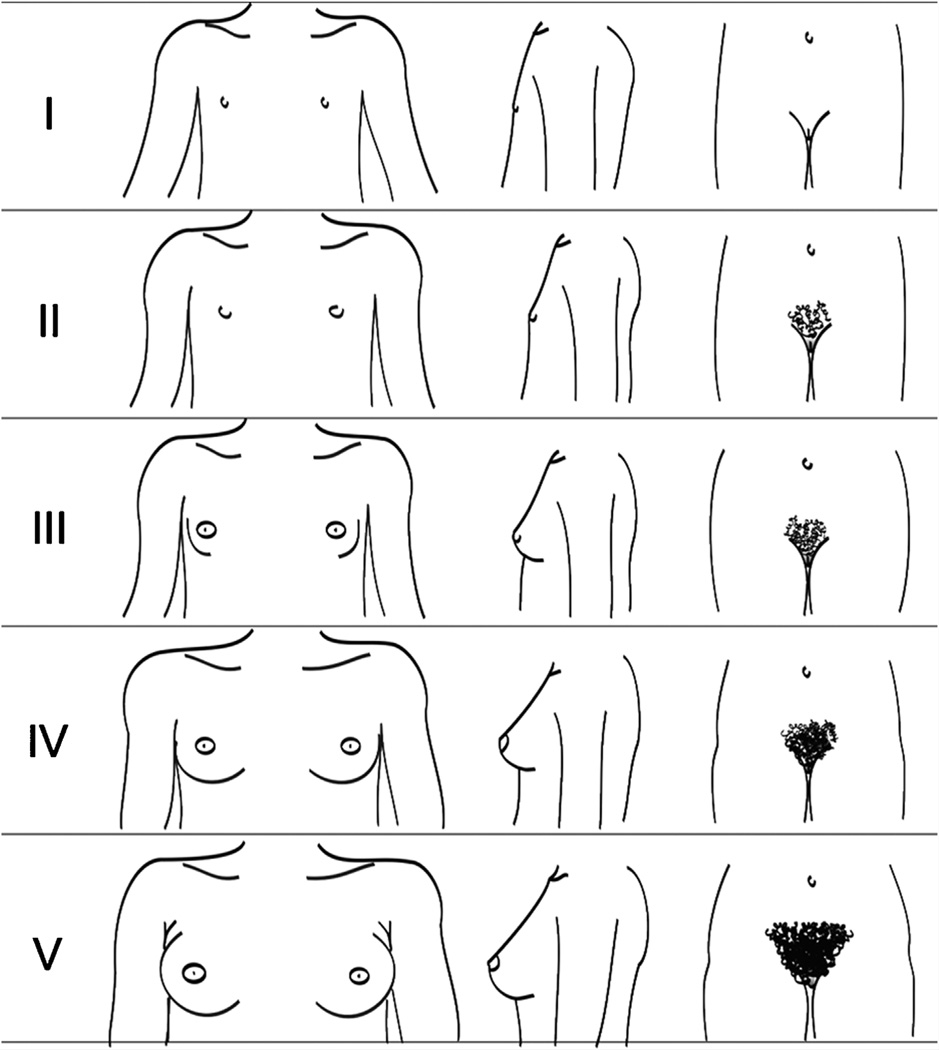
Puberty
The timing of puberty varies greatly in the general population and is influenced by genetic and environmental factors [Gajdon et al., 2009]. In evaluating the pubertal development, ethnic background and intra-familial variation should be taken into account. Tanner stages are used to score pubertal development [Marshall and Tanner, 1969; Tanner, 1986]. In females the stages are determined by the size of the breasts and nipples, pigmentation and rugae formation of the labia, and pubic and axillary hair growth (Fig. 36). As each of these components is defined here separately, the pubertal stages are not discussed in further detail.
FIG. 36.
Puberty stages females according to Tanner [1986].
Measurements of the Female External Genitalia
Measurement of the clitoris is the only measurement of female external genitalia commonly used in the clinic. Measurements of the clitoris are possible using sliding calipers, or a straight-edged plastic ruler. Reliability of measurements using a tape measure is poor. Length is measured from the base of the clitoris at the pubic symphysis to the tip without including the foreskin. Fat pads at the base of the clitoris influence this measurement and the ruler should be pressing against the pubic ramus. The reader is referred to the Handbook of Normal Physical Measurements [Hall et al., 2007] for detailed descriptions of measurement techniques and growth standards. Except for pubertal developmental stages growth standards are provided for Caucasians of Northern European origin only.
Anatomical Variation
Anomalies of the female external genitalia may be classified into quantitative (objective or anthropometric) traits and qualitative (subjective or categorical) features:
Variations in length and width: large clitoris; small clitoris; absent labia majora; absent labia minora; large labia majora; small labia majora; prominent labia minora.
Variations in shape, number, or position: bifid clitoris; duplicated clitoris; fused labia minora; epispadias; hypospadias; atretic vaginal opening; septated vagina.
Variations in skin manifestations: freckled genitalia; hyperpigmented genitalia; hypopigmented genitalia; exaggerated rugosity of the labia majora; sparse pubic hair.
The various features are listed alphabetically. If a feature is indicated in bold-italics, the feature is listed and a definition is available. The terms are alphabetized based on the physical feature, not the modifier.
Investigating the genitalia should always be performed with the observed person in a relaxed position. The presence of a nurse or parent is advisable. Small children are best investigated in their parent’s lap. Repeated genital examinations may be embarrassing for the subject [Lee et al., 2006] and should be performed only when indicated.
DEFINITIONS
Clitoris, Bifid
Definition: Two clitorides located side by side (Fig. 37). objective
FIG. 37.
Bifid clitoris. Note the co-occurrence of epispadias. Courtesy of Dr. Anne-Karoline Ebert. Reprinted with permission from Ebert et al. [2009].
Comments: The word bifid indicates the presence of a split clitoris, as opposed to a supernumerary clitoris, which could be described as Duplicated clitoris. A bifid clitoris is almost invariably accompanied by Epispadias, which should be coded separately.
Clitoris, Duplicated
Definition: A supernumerary clitoris (Fig. 38) objective
FIG. 38.
Duplicated clitoris. Reprinted with permission from Kurth [1958].
Comments: A duplicated clitoris is much less common than a Bifid clitoris, which should be considered first in most cases [Kurth, 1958].
Synonym: Clitoris, supernumerary
Clitoris, hyperplastic: See Clitoris, large
Clitoris, hypertrophic: See Clitoris, large
Clitoris, hypoplastic: See Clitoris, small
Clitoris, hypotrophic: See Clitoris, small
Clitoris, Large
Definition: Clitoral length more than 2 SD above the mean for age (Fig. 39). objective OR
FIG. 39.
Large clitoris.
Apparently increased length of the clitoris for age. subjective
Comments: Clitoral length is the distance between the attachment of the clitoris anterior to the pubic bone and tip of the clitoris. Details on measurement of the clitoris can be found elsewhere [Oberfield et al., 1989; Litwin et al., 1991; Sane and Pescovitz, 1992; Verkauf et al., 1992; Phillip et al., 1996; Akbiyik and Kutlu, 2010]. Subjective assessment of clitoral size can be confounded by Small labia majora and therefore objective assessment is preferred. The word “large” literally indicates an increase in bothwidth and length, but in practice only the length of the clitoris is measured.
Synonym: Clitoromegaly; Clitoris, overdeveloped; Clitoris, long
Replaces: Clitoris, hypertrophic; Clitoris, hyperplastic
Clitoris, long: See Clitoris, large
Clitoris, overdeveloped: See Clitoris, large
Clitoris, Small
Definition: Clitoral length more than 2 SD below the mean for age (Fig. 40). objective OR
FIG. 40.
Small clitoris.
Apparently decreased length of the clitoris for age. subjective
Comments: Clitoral length is the distance between the attachment of the clitoris anterior to the pubic bone and tip of the clitoris. Details on measurement of the clitoris can be found elsewhere [Oberfield et al., 1989; Litwin et al., 1991; Sane and Pescovitz, 1992; Verkauf et al., 1992; Phillip et al., 1996; Akbiyik and Kutlu, 2010]. Subjective assessment of clitoral size can be confounded by obesity and therefore objective assessment is preferred. The word small literally indicates a decrease in both width and length, but in practice only the length of the clitoris is measured.
Synonym: Clitoris, underdeveloped
Replaces: Clitoris, hypotrophic; Clitoris, hypoplastic
Clitoris, supernumerary: See Clitoris, duplicated
Clitoris, underdeveloped: See Clitoris, small
Clitoromegaly: See Clitoris, large
Epispadias
Definition:Dorsalplacementof the urethral opening (Fig. 37). objective
Comments: In a phenotypic female, epispadias may be accompanied by a Bifid clitoris, which should be coded separately. Epispadias is a frequent component of Bladder exstrophy, but should be coded separately.
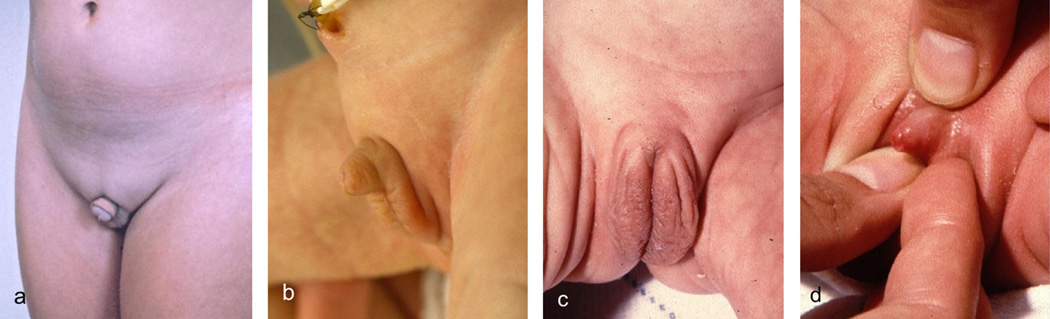
Genitalia, Ambiguous
Definition: External genitalia without typical male or female appearance (Fig. 9). subjective
Comments: Note that this term can include or combine variations in size and shape, with partial or complete absence of structures. It is preferable to describe the individual components, which are defined below. It is nonetheless a widely used bundled term and as such is retained here (for the definition of a “bundled term” see Allanson et al. [2009a]).
Synonym: Intersex genitalia
Genitalia, ephelides: See Genitalia, freckled
Genitalia, Freckled
Definition: One or more brown punctate macules on the skin of the genitalia (Fig. 10). objective
Comments: This should be differentiated from Hyperpigmented genitalia in which an area larger than a freckle is/the complete external genitalia are hyperpigmented. The description should be qualified by a description of the affected part(s).
Synonym: Genitalia, ephelides
Genitalia, Hyperpigmented
Definition: Localized or generalized increased genital pigmentation (Fig. 11). subjective
Comments: This is an assessment of the relative pigmentation of the genitalia compared to the overall pigmentation of the individual. Hyperpigmentation can affect other parts of the body or be restricted to the genitalia. Genital hyperpigmentation can be generalized or localized. It should be differentiated from Freckled genitalia in which one or more small, focal areas of hyperpigmentation are present. Localized hyperpigmentation can be objectively determined due to the difference from the immediate surrounding tissue color, while generalized hyperpigmentation may be more difficult to determine and is therefore a subjective manifestation. If the finding is localized, the description should be appended with a description of the affected part(s).
Genitalia, Hypopigmented
Definition: Localized or generalized decreased genital pigmentation (Fig. 12). subjective
Comments: This is an assessment of the relative pigmentation of the genitalia compared to the overall pigmentation of the individual. Hypopigmentation can affect other parts of the body or be restricted to the genitalia. Genital hypopigmentation can be generalized or localized. Localized hypopigmentation can be objectively determined due to the difference from the immediate surrounding tissue color, while generalized hypopigmentation may be more difficult to determine and is therefore a subjective manifestation.
Genitalia, intersex: See Genitalia, ambiguous
Hypospadias
Definition: Urethral meatus located on the anterior vaginal wall (Fig. 41). objective
FIG. 41.
Hypospadias (a catheter being in hypospadiac opening high in the anterior vaginal wall). Courtesy of Dr. Amilal Bhat. Reprinted with permission from Bhat et al. [2010].
Comments: The location of the meatus can be from just above the introitus up to deep into the vagina near the cervix (fornix). Female hypospadias can be associated with Bladder exstrophy, which should be coded separately
Labia Majora, Absent
Definition: No discernable labia majora (Fig. 42). subjective
FIG. 42.
Absent labia majora.
Comments: None of the three attributes of labia majora is present: no tissue mass, no hyperpigmentation, no rugae formation.
Labia majora, hyperplastic: See Labia majora, large
Labia majora, hypertrophic: See Labia majora, large
Labia majora, hypoplastic: See Labia majora, small
Labia majora, hypotrophic: See Labia majora, small
Labia Majora, Large
Definition: Increased volume of the labia majora (Fig. 43). subjective
FIG. 43.
Large labia majora. Courtesy of Dr. Ariachery Ammini. Reprinted with permission from Kulshreshtha et al. [2010].
Comments: Large labia majora may be accompanied by Hyperpigmented genitalia or Exaggerated rugosity of the labia majora, which should be coded separately.
Synonym: Labia majora, overdeveloped
Replaces: Labia majora, hypertrophic; Labia majora, hyperplastic
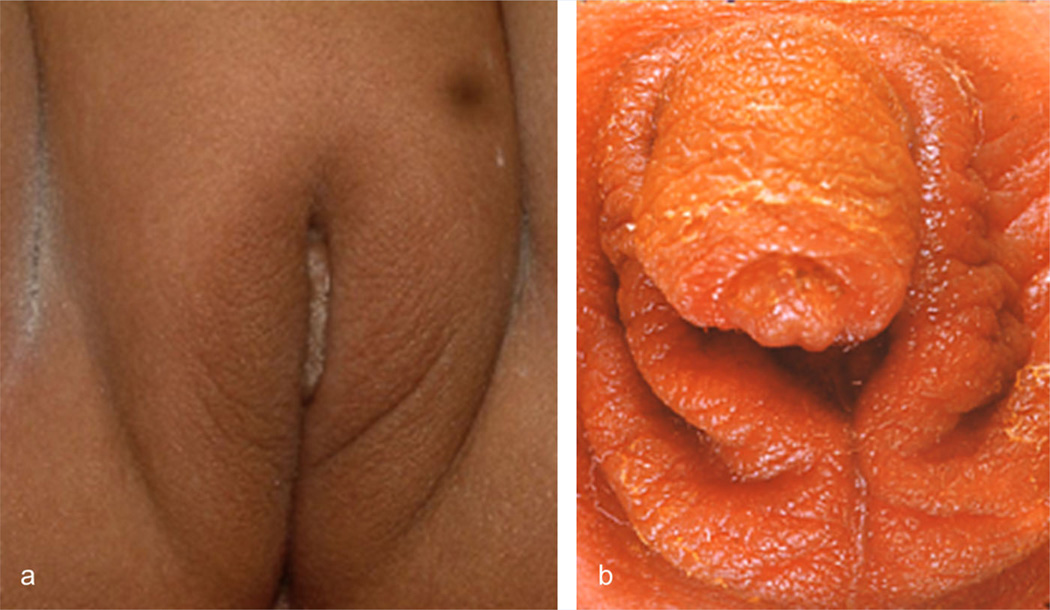
Labia Majora, Exaggerated Rugosity of the
Definition: Marked rugae formation of the skin of the labia majora (Fig. 44). subjective
FIG. 44.
Labia majora with mild (a) and more marked (b) rugae formation. Note enlargement of clitoris as well in panel B. Panel a courtesy of Dr. Ariachery Ammini. Panel a reprinted with permission from Atilgan et al. [2009].
Comments: Some rugae formation is typically found on the labia majora, but less than on the scrotum.
Replaces: Scrotum-like labia majora
Labia majora, overdeveloped: See Labia majora, large
Labia majora, scrotum-like: See Labia majora, exaggerated rugosity of the
Labia Majora, Small
Definition: Apparently decreased soft tissue volume of the labia majora (Fig. 45). subjective
FIG. 45.
Small upper part (panels a and b) and lower part (panel C) of labia majora.
Comments: The hyperpigmentation and mild rugae formation of the labia majora may or may not be decreased.
Synonym: Labia majora, underdeveloped
Labia majora, underdeveloped: See Labia majora, small
Labia Minora, Absent
Definition: No recognizable soft tissue folds medial to the labia majora (Fig. 46). subjective
FIG. 46.
Absent labia minora. Note this causes a seemingly large clitoris which is in fact of normal size.
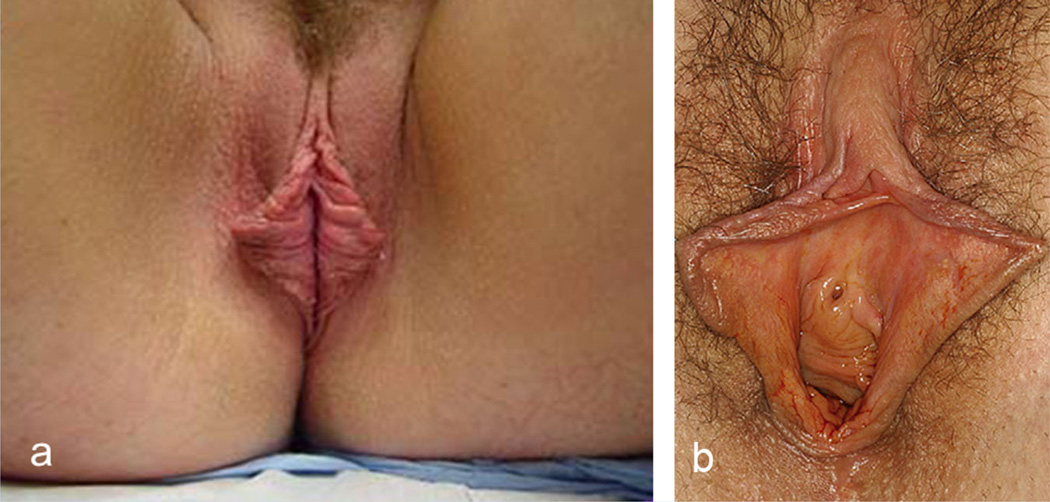
Labia Minora, Fused
Definition: Lack of separation of the labia minora over part or all of their length (Fig. 47). Objective
FIG. 47.
Fused labia minora. Courtesy of Dr. AKC Leung.
Comments: Fusion is not infrequent in newborn girls and separation may occur spontaneously in the first few years of life.
Labia Minora, Prominent
Definition: Apparent increase in volume of the labia minora (Fig. 48). subjective
FIG. 48.
Prominent labia minora which is unilateral on the right panel. Panel a courtesy of Dr. Warren Ellsworth, panel b courtesy of Dr. Charles Malata. Panel a reprinted with permission from Ellsworth et al. [2010]. Panel B reprinted with permission from Solanki et al. [2010].
Comments: Variation in the size of labia minora is considerable. This is in fact a bundled term as itmay indicate an increase of length, width and/or thickness, but it is useful in practice and therefore kept here. Labia minora may appear prominent in the presence of Small labia majora .
Pubic hair, hypotrichosis: See Pubic hair, sparse
Pubic hair, Sparse
Definition: Apparently decreased number of hairs per unit area relative to the pubertal development as judged by other components of pubertal maturity (Fig. 49) subjective
FIG. 49.
Sparse pubic hair (in a pubertal female).
Comments: (Pubic) hypotrichosis should not be used as a synonym as, formally, it means underdevelopment of the hair. No normal values for the number of hairs per unit area exist.
Replaces: Pubic hair, thinning; Pubic hair, thin; Pubic hypotrichosis
Pubic hair, thin(ning): See Pubic hair, sparse
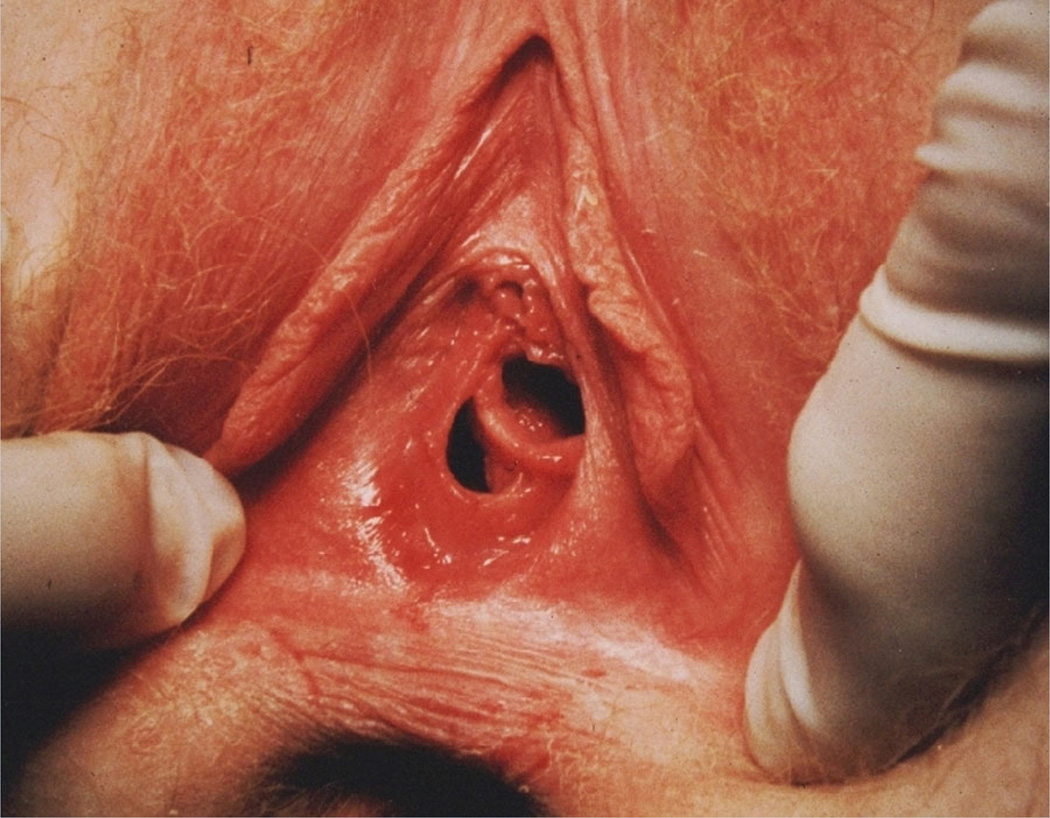
Vagina, Atretic Opening of the
Definition: No discernable entrance to the vagina on the vulva (Fig. 50). Objective
FIG. 50.
Atretic opening of the vagina.
Comments: An atretic opening may occur independent of atresia of the remainder of the vagina, which needs further radiological and/or surgical investigations to diagnose.
Vagina, Septated
Definition: Apparent lateral division of the vagina by a thin tissue wall visible at the introitus (Fig. 51). objective
FIG. 51.
Septated vagina.
Comments: The term does not indicate the pathogenetic mechanism and does not distinguish a double vagina from a septum within a single vagina. Neither a transverse vaginal septum nor a septum present in the deeper two-thirds of the vagina can be assessed on external physical examination.
ACKNOWLEDGMENTS
We are pleased to thank Astrid Sibbes, Medical Photography and Illustration, Academic Medical Centre, Amsterdam for all drawings, and Dr. F.B. Lammes, pediatric gynecologist, for making his photography collection available to us. E.V. is partially funded by the DSD Translational Research Network (NIH grant # 1 R01 HD068138), and L.G.B. is supported by the Intramural Research Program of the National Human Genome Research Institute.
Grant sponsor: NIH; Grant number: # 1 R01 HD068138; Grant sponsor: Intramural Research Program of the National Human Genome Research Institute.
REFERENCES
- Adams MV. The multicultural imagination: Race, color, and the unconscious. London: Routledge; 1996. p. 164. [Google Scholar]
- Ajmani ML, Jain SP, Saxena SK. Anthropometric study of male external genitalia of 320 healthy Nigerian adults. Anthropol Anz. 1985;43:179–186. [PubMed] [Google Scholar]
- Akbiyik F, Kutlu AO. External genital proportions in prepubertal girls:Amorphometric reference for female genitoplasty. J Urol. 2010;184:1476–1481. doi: 10.1016/j.juro.2010.06.023. [DOI] [PubMed] [Google Scholar]
- Allanson JE, Biesecker LG, Carey JC, Hennekam RCM. Elements of morphology: Introduction. Am J Med Genet Part A. 2009a;149A:2–5. doi: 10.1002/ajmg.a.32601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Allanson JE, Cunniff C, Hoyme HE, McGaughan J, Muenke M, Neri G. Elements of morphology: Standard terminology for the head and face. Am J Med Genet Part A. 2009b;149A:6–28. doi: 10.1002/ajmg.a.32612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Atilgan D, Uluocak N, Erdemir F, Parlaktas BS. Female epispadias: A case report and review of the literature. Kaohsiung J Med Sci. 2009;25:613–616. doi: 10.1016/S1607-551X(09)70565-0. [DOI] [PubMed] [Google Scholar]
- Baskin LS, Duckett JW. Hypospadias, in adult and pediatric urology. In: Gillenwater J, Grayhack J, Howards S, Mitchell M, editors. Adult and pediatric urology. 4th edition. St. Louis: Mosby; 1996. [Google Scholar]
- Bauer R, Kogan BA. Modern technique for penile torsion repair. J Urol. 2009;182:286–291. doi: 10.1016/j.juro.2009.02.133. [DOI] [PubMed] [Google Scholar]
- Bergeson PS, Hopkin RJ, Bailey RB, Mc Gill LC, Piatt JP. The inconspicuous penis. Pediatrics. 1993;92:794–799. [PubMed] [Google Scholar]
- Bergholz R, Wenke K. Polyorchidism: A meta-analysis. J Urol. 2009;182:2422–2427. doi: 10.1016/j.juro.2009.07.063. [DOI] [PubMed] [Google Scholar]
- Bhat A, Saxena R, Bhat MP, Dawan M, Saxena G. Female hypospadias with vaginal stones: A rare congenital anomaly. J Pediatr Urol. 2010;7:70–74. doi: 10.1016/j.jpurol.2009.03.014. [DOI] [PubMed] [Google Scholar]
- Biesecker LG, Aase JM, Clericuzio C, Gurrieri F, Temple IK, Toriello H. Elements of morphology: Standard terminology for the hands and feet. Am J Med Genet Part A. 2009;149A:93–127. doi: 10.1002/ajmg.a.32596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bologna RA, Noah TA, Nasrallah PF, McMahon DR. Chordee: Varied opinions and. treatments as documented in a survey of the American Academy of Pediatrics, Section of Urology. Urology. 1999;53:608–612. doi: 10.1016/s0090-4295(98)00656-6. [DOI] [PubMed] [Google Scholar]
- Carey JC, Cohen MM, Jr, Curry CJR, Devriendt K, Holmes LB, Verloes A. Elements of morphology: Standard terminology for the lips, mouth and oral region. Am J Med Genet Part A. 2009;149A:77–92. doi: 10.1002/ajmg.a.32602. [DOI] [PubMed] [Google Scholar]
- Cheng PK, Chanoine JP. Should the definition of micropenis vary according to ethnicity? Horm Res. 2001;55:278–281. doi: 10.1159/000050013. [DOI] [PubMed] [Google Scholar]
- Chibber PJ, Shah HN, Jain P, Yadav P. Male gender assignment in aphallia: A case report and review of the literature. Int Urol Nephrol. 2005;37:317–319. doi: 10.1007/s11255-004-7974-0. [DOI] [PubMed] [Google Scholar]
- Cinaz P, Yeşilkaya E, Onganlar YH, Boyraz M, Bideci A, Camurdan O, Baki Karaoğlu A. Penile anthropometry of normal prepubertal boys in Turkey. Acta Paediatr. 2012;101:e33–e36. doi: 10.1111/j.1651-2227.2011.02386.x. [DOI] [PubMed] [Google Scholar]
- Damon V, Berlier P, Durozier B, François R. Study of the dimensions of the penis from birth to adult age and as a function of testicular volume. Pediatrie. 1990;45:519–522. [PubMed] [Google Scholar]
- Ebert AK, Reutter H, Ludwig M, Rösch WH. The extrophy–epispadias complex. Orphanet J Rare Dis. 2009;4:23. doi: 10.1186/1750-1172-4-23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- El-Koutby M, Aminel Gohary M. Webbedpenis:Anew classification. J Indian Assoc Pediatr Surg. 2010;15:50–52. doi: 10.4103/0971-9261.70637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ellsworth WA, Rizvi M, Lypka M, Gaon M, Smith B, Cohen B, Dinh T. Techniques for labia minora reduction: An algorithmic approach. Aesth Plast Surg. 2010;34:105–110. doi: 10.1007/s00266-009-9454-5. [DOI] [PubMed] [Google Scholar]
- Fathi K, Perovic S, Pinter A. Successful surgical correction of an extreme form of ectopic penis. J Pediatr Urol. 2010;6:426–428. doi: 10.1016/j.jpurol.2009.12.007. [DOI] [PubMed] [Google Scholar]
- Gajdon ZKZ, Hirschhorn JN, Palmert MR. What controls the timing of puberty? An update on progress from genetic investigation. Curr Opin Endocrinol Diabetes Obes. 2009;16:16–24. doi: 10.1097/MED.0b013e328320253c. [DOI] [PubMed] [Google Scholar]
- Gardikis S, Kambouri K, Tsalkidis A, Angelidou M, Pitiakoudis M, Vaos G. Inguinal ectopic scrotum in a neonate: Case report and literature review. Pediatr Int. 2012;54:575–576. doi: 10.1111/j.1442-200X.2012.03656.x. [DOI] [PubMed] [Google Scholar]
- Gucev Z, Castori M, Tasic V, Popjordanova N, Hasani A. A patient with unilateral tibial aplasia and accessory scrotum: A pure coincidence or nonfortuitous association? Case Report Med. 2010;2010:898636. doi: 10.1155/2010/898636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hall JG, Allanson JA, Gripp K, Slavotinek A. Handbook of normal physical measurements. 2nd edition. New York: Oxford University Press; 2007. [Google Scholar]
- Hall BD, Graham JM, Jr, Cassidy SB, Opitz JM. Elements of morphology: Standard terminology for the periorbital region. Am J Med Genet Part A. 2009;149A:29–39. doi: 10.1002/ajmg.a.32597. [DOI] [PubMed] [Google Scholar]
- Hennekam RCM, Cormier-Daire V, Hall JG, Méhes K, Patton M, Stevenson RE. Elements of morphology: Standard terminology for the nose and philtrum. Am J Med Genet Part A. 2009;149A:61–76. doi: 10.1002/ajmg.a.32600. [DOI] [PubMed] [Google Scholar]
- Hoar RM, Calvano CJ, Reddy PP, Bauer SB, Mandell J. Unilateral suprainguinal ectopic scrotum. The role of the gubernaculum in the formation of an ectopic scrotum. Teratology. 1998;57:54–59. doi: 10.1002/(SICI)1096-9926(199802)57:2<64::AID-TERA4>3.0.CO;2-6. [DOI] [PubMed] [Google Scholar]
- Hunter A, Frias J, Gillessen-Kaesbach G, Hughes H, Jones K, Wilson L. Elements of morphology: Standard terminology for the ear. Am J Med Genet Part A. 2009;149A:40–60. doi: 10.1002/ajmg.a.32599. [DOI] [PubMed] [Google Scholar]
- Janoff DM, Skoog SJ. Congenital scrotal agenesis: Description of a rare anomaly and management strategies. J Urol. 2005;173:589–591. doi: 10.1097/01.ju.0000151136.56430.53. [DOI] [PubMed] [Google Scholar]
- Keckler S, Stephany HA, Spilde TL, Snyder CL. Isolated diphallia: Case report and literature review. Eur J Pediatr Surg. 2009;19:254–255. doi: 10.1055/s-2008-1038882. [DOI] [PubMed] [Google Scholar]
- Kulshreshtha B, Khadgawat R, Eunice M, Ammini AC. Congenital adrenal hyperplasia: Results of medical therapy on appearance of external genitalia. J Pediatr Urol. 2010;6:555–559. doi: 10.1016/j.jpurol.2010.01.001. [DOI] [PubMed] [Google Scholar]
- Kurth ME. Incomplete duplication of the female external genitalia or double clitoris. Am J Surg. 1958;96:596–599. doi: 10.1016/0002-9610(58)90986-3. [DOI] [PubMed] [Google Scholar]
- Lee PA, Houk CP, Ahmed SF, Hughes IA. Consensus statement on management of intersex disorders. International Consensus Conference on Intersex. Pediatrics. 2006;118:e488–e500. doi: 10.1542/peds.2006-0738. [DOI] [PubMed] [Google Scholar]
- Litwin A, Aitkin I, Merlob P. Clitoral length assessment in newborn infants of 30 to 41 weeks gestational age. Eur J Obstet Gynecol Reprod Biol. 1991;38:209–212. doi: 10.1016/0028-2243(91)90293-t. [DOI] [PubMed] [Google Scholar]
- Marshall WA, Tanner JM. Variations in the pattern of pubertal changes in girls. Arch Dis Child. 1969;44:291–303. doi: 10.1136/adc.44.235.291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Montag S, Palmer LS. Abnormalities of penile curvature: Chordee and penile torsion. Sci World J. 2011;11:1470–1478. doi: 10.1100/tsw.2011.136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oberfield SE, Mondok A, Shahrivar F, Klein JF, Levine LS. Clitoral size in full-term infants. Am J Perinatol. 1989;6:453–454. doi: 10.1055/s-2007-999638. [DOI] [PubMed] [Google Scholar]
- Orkiszewski M. A standardized classification of hypospadias. J Pediatr Urol. 2012;8:410–414. doi: 10.1016/j.jpurol.2011.08.011. [DOI] [PubMed] [Google Scholar]
- Phillip M, De Boer C, Pilpel D, Karplus M, Sofer S. Clitoral and penile sizes of full term newborns in two different ethnic groups. J Pediatr Endocrinol Metab. 1996;9:175–179. [PubMed] [Google Scholar]
- Ponchietti R, Mondaini N, Bonafé M, Di Loro F, Biscioni S, Masieri L. Penile length and circumference: A study on 3,300 young Italian males. Eur Urol. 2001;39:183–186. doi: 10.1159/000052434. [DOI] [PubMed] [Google Scholar]
- Rattan KN, Kajal P, Pathak M, Kadian YS, Gupta R. Aphallia: Experience with 3 cases. J Pediatr Surg. 2010;45:e13–e16. doi: 10.1016/j.jpedsurg.2009.10.057. [DOI] [PubMed] [Google Scholar]
- Roth JK, Jr, Marshall RH, Angel JR, Daftary M, Lewis RW. Congenital absence of penis. Urology. 1981;17:579–583. doi: 10.1016/0090-4295(81)90080-7. [DOI] [PubMed] [Google Scholar]
- Sadeghipour RS, Esmailzadehha N. Aposthia: A case report. J Pediatr Surg. 2010;45:317–319. doi: 10.1016/j.jpedsurg.2010.05.030. [DOI] [PubMed] [Google Scholar]
- Sane K, Pescovitz OH. The clitoral index: A determination of clitoral size in normal girls and in girls with abnormal sexual development. J Pediatr. 1992;120:264–266. doi: 10.1016/s0022-3476(05)80439-1. [DOI] [PubMed] [Google Scholar]
- Schneider T, Sperling H, Lümmen G, Syllwasschy J, Rübben H. Does penile size in younger men cause problems in condom use? A prospective measurement of penile dimensions in 111 young and 32 older men. Urology. 2001;57:314–318. doi: 10.1016/s0090-4295(00)00925-0. [DOI] [PubMed] [Google Scholar]
- Solanki NS, Tejero-Trujeque R, Stevens-King A, Malata CM. Aesthetic and functional reduction of the labia minora using the Maas and Hage technique. J Plast Reconstr Aesth Surg. 2010;63:1181–1185. doi: 10.1016/j.bjps.2009.05.053. [DOI] [PubMed] [Google Scholar]
- Tanner JM. Normal growth and techniques of growth assessment. Clin Endocrinol Metab. 1986;15:411–451. doi: 10.1016/s0300-595x(86)80005-6. [DOI] [PubMed] [Google Scholar]
- Verkauf BS, Von Thron J, O’Brien WF. Clitoral size in normal women. Obstet Gynecol. 1992;80:41–44. [PubMed] [Google Scholar]
- Wang H, Guo K, Wang J, Liu L, Li F. Aphallia in an adult male with 46, XY karyotype. Int J Urol. 2011;18:540–542. doi: 10.1111/j.1442-2042.2011.02785.x. [DOI] [PubMed] [Google Scholar]
- Yalcinkaya S, Sahin C, Sahin AF. Polyorchidism: Sonographic and magnetic resonance imaging findings. Can Urol Assoc J. 2011;5:e84–e86. doi: 10.5489/cuaj.10077. [DOI] [PMC free article] [PubMed] [Google Scholar]