Abstract
A better understanding of human-to-mosquito transmission is crucial to control malaria. In order to assess factors associated with gametocyte carriage, 2083 samples were collected in a cross-sectional survey in Papua New Guinea. Plasmodium species were detected by light microscopy and qPCR and gametocytes by detection of pfs25 and pvs25 mRNA transcripts by reverse-transcriptase PCR (qRT-PCR). The parasite prevalence by PCR was 18.5% for Plasmodium falciparum and 13.0% for P. vivax. 52.5% of all infections were submicroscopic. Gametocytes were detected in 60% of P. falciparum-positive and 51% of P. vivax-positive samples. Each 10-fold increase in parasite density led to a 1.8-fold and 3.3-fold increase in the odds of carrying P. falciparum and P. vivax gametocytes. Thus the proportion of gametocyte positive and gametocyte densities was highest in young children carrying high asexual parasite densities and in symptomatic individuals. Dilution series of gametocytes allowed absolute quantification of gametocyte densities by qRT-PCR and showed that pvs25 expression is 10-20 fold lower than pfs25 expression. Between 2006 and 2010 parasite prevalence in the study site has decreased by half. 90% of the remaining infections were asymptomatic and likely constitute an important reservoir of transmission. However, mean gametocyte densities were low (approx. 1-2 gametocyte/μL) and it remains to be determined to what extent low-density gametocyte positive individuals are infective to mosquitos.
Introduction
Understanding Plasmodium spp. transmission from the human host to the mosquito vector is a key priority in the attempt to control and eventually eliminate malaria. While most malaria parasites in the human host replicate asexually, a small proportion of them enter the sexual pathway and form morphologically and functionally different gametocytes. Malaria transmission depends on mosquitos taking up both male and female gametocytes and transmitting their progeny to the next human host.
The biology of Plasmodium falciparum and P. vivax gametocytes differ [1]. P. falciparum gametocytes are sequestered during development and only mature gametocytes circulate. They appear 7–15 days after the initial wave of asexual stages in the blood stream [2], thus usually after the first febrile symptoms. In contrast P. vivax gametocytes appear in the blood stream shortly after the first appearance of asexual blood stage parasites and before the onset of clinical disease [3]. In addition individual P. falciparum gametocytes circulate for 3–4 weeks [4,5], while P. vivax gametocytes only survive for a few days [6].
By light microscopy (LM), the proportion P. falciparum gametocyte positive (i.e. the proportion of gametocyte carriers among all P. falciparum positive individuals) in symptomatic individuals with high asexual parasite densities (often >5000 parasites/μL) ranged from 2.4 to 17% in Thailand and West Africa [7–11]. When gametocyte carriage was assessed by LM in both P. falciparum and P. vivax clinical cases, the proportion P. vivax gametocyte positive was 6–8 times higher than that of P. falciparum [8,12,13] reaching rates of 57–92% in different Asian countries [8,14,15]. The prevalence of gametocytes in the general population, in particular in asymptomatic individuals, has been studied in only few malaria-endemic regions [16–18]. A study in Madang Province, Papua New Guinea reported that 9.8% of P. falciparum- compared to 36.3% of P. vivax-infected individuals carried gametocytes [19]. The proportion gametocyte positive was highest in children and decreased rapidly with age.
As the amount of blood examined is limited and only a small fraction of all parasites are gametocytes, microscopic detection of gametocytes has limited sensitivity of around 10–20 gametocytes/μL blood. Molecular assays, based on amplification of gametocyte specific RNA transcripts, have revealed 2–8 times higher gametocyte prevalence than light microscopy [20–24]. Using molecular assays, proportions of P. falciparum gametocyte carriers amongst P. falciparum positive individuals ranged from 12% in asymptomatic carriers [25] to 15% in a cross-sectional survey [20] and 89–91% in clinical infections [21,24]. The proportion P. vivax gametocyte positive reached 95% both in febrile patients [24] and in cross-sectional surveys [26].
In mosquito feeding experiments it has been repeatedly shown that individuals that carry gametocytes at submicroscopic levels are infective, both for P. falciparum [23,27,28] and P. vivax [29,30]. While individuals who were gametocyte positive by LM were considerably more infective than individuals with only asexual parasites [13,28,30,31], the latter likely contribute substantially to transmission due to the large proportion of asymptomatic individuals carrying low-moderate density infections, [23].
Little is known about the factors associated with gametocyte prevalence and density, such as acquired immunity, clinical disease and age. To identify carriers of P. falciparum and P. vivax gametocytes, we conducted a cross-sectional survey in Papua New Guinea. Blood-stage parasites and gametocytes were detected by highly sensitive quantitative PCR (qPCR) and reverse-transcriptase qPCR (qRT-PCR) assays.
Material and Methods
Ethical statement
Written informed consent was obtained from all study participants or their parents or legal guardians. The study was approved by PNG IMR IRB, the PNG Medical Research Advisory Committee (MRAC 05.20 & 12.06) and the WEHI Human Research Ethics Committee.
Sample collection
The study was conducted in May-June 2010 in 3 communities (Malala, Mugil and Utu) in Madang Province PNG, approximately two years after long-lasting insecticide treated bed nets (LLINs) were distributed to all households [32]. The region receives over 3,000 mm of rainfall annually with a short dry season (June to October) and has hyper-endemic malaria transmission that is moderately seasonal (lower in the drier season).
From each participant demographic data was recorded, history of febrile illness and data on bed net use. Axillary temperature was measured, 250–300μL of capillary blood collected into a K+EDTA microtainers, thick/thin films were prepared and haemoglobin measured (Hemocue). For statistical purposes individuals were classified as non-anaemic (Hb ≥11g/dL), having mild anaemia (Hb 8–10.9 g/dL), and having moderate-to-severe anaemia (Hb <8g/dL). In the case of reported febrile illness or axillary temperature >37.5°C, a rapid malaria diagnostic test (ICT Combo) was performed and those positive by RDT treated with Artemether-Lumefantrine (Coartem). For RNA preservation, 50μL of whole blood was transferred to a tube containing 250μL of RNAProtect (Qiagen) within 8 hours of collection and stored at -80°C until RNA extraction. In previous studies, transfer of blood to RNAprotect within 4 hours after collection was shown to maintain high-quality RNA and thus optimal sensitivity of gametocyte detection [33]. In addition, no effect on RNA quality was observed when samples were stored at ambient temperature for up to 24 hours prior to long-term storage at -80° (A. Waltmann, S. Karl et al, manuscript in preparation). The remaining blood was centrifuged, the plasma removed and stored at -80°C, and the red cell pellet stored at -20°C until DNA extraction.
Parasite detection
Blood slides were examined (minimum of 200 high-powered fields) independently by two experienced microscopists with discrepancies adjudicated by a third microscopist. Parasite densities were calculated from the number of parasites per 200 or 500 white blood cells (WBCs) (depending on parasitaemia) and an assumed total peripheral WBC count of 8,000/μL [34] with the final density taken as the arithmetic mean of the two values.
DNA was extracted from the equivalent of 200μL blood using the Favorgen 96-well Genomic DNA Extraction Kit and eluted in 200μL buffer. A genus-specific quantitative PCR (qPCR) that amplifies a conserved region of the 18S rRNA gene was run on all samples [33]. For P. falciparum, P. vivax, P. malariae and P. ovale species typing, species-specific qPCRs were run as described [35]. The 18S rRNA gene amplified by qPCR is present in 3 copies per genome. Copy numbers were quantified based on serial dilutions of plasmid controls run in parallel. The detection limit (defined as >50% of plasmid standards positive) was 1–2 copies per μL for all qPCRs.
Gametocyte detection and quantification
The number of P. falciparum and P. vivax gametocytes were recorded separately from asexual stages during microscopic examination of all blood slides.
For gametocyte detection by qRT-PCR, RNA was extracted from all P. falciparum or P. vivax qPCR-positive samples using the Qiagen RNeasy plus 96 kit, including Genomic DNA removal by gDNA eliminator columns and DNase (Qiagen). Absence of gDNA in all samples was confirmed by the same genus-specific, DNA-based qPCR used for parasite detection. In a separate PCR reaction, presence of parasite RNA after extraction was verified by quantitative reverse-transcriptase PCR (qRT-PCR) detecting 18S-RNA with the same primers and probe as the genus-specific qPCRs.
P. falciparum and P. vivax gametocytes were detected by qRT-PCR of the highly expressed gametocyte markers pfs25 and pvs25 as described [33]. The number of pfs25 transcripts per P. falciparum gametocyte had previously been calculated based on comparisons of microscopy counts and qRT-PCR results of different dilutions of cultured P. falciparum gametocytes. A non-linear relation was found and it was estimated that the qRT-PCR detects 50–180 pfs25 transcripts per circulating P. falciparum gametocyte, depending on gametocyte density [33].
Two independent P. vivax gametocyte trend-lines were generated from enriched gametocytes from P. vivax patients from Thailand (2 isolates, 21–24% gametocytes, 64–70% of all gametocytes female) and Brazil (3 isolates, 23–42% gametocytes, 24–71% of all gametocytes female). Leukocyte-depleted blood was passed through a MidiMacs column (Miltenyi Biotec), gametocytes and other stages (mostly trophozoites) were eluted and resuspended in RPMI medium. Two samples were stored in TRIzol, and a 10-fold serial dilution (5 steps) was made after RNA extraction. Three samples were diluted 10-fold (3 steps) before adding RNAprotect and storing. The final RNA concentration corresponded to densities of 104 to 1 gametocytes/μL blood. Pvs25 transcripts/μL were quantified by qRT-PCR; plasmid standards were run in parallel for absolute quantification. Conversion factors for pvs25 transcript numbers into numbers of gametocytes were calculated with a random-effect model from log10-transformed quantities of the gametocyte trend-lines. Samples were set as random effect.
Data analysis
Malaria episodes were defined as febrile illness (axillary temperature >37.5°C measured at time of sampling and/or fever reported from previous 48 hours) in the presence of P. vivax or P. falciparum asexual parasites by LM (any density). Parasite and gametocyte densities were log transformed and geometric means per μL whole blood calculated wherever densities are reported. Multivariate analysis of factors associated with gametocyte carriage was conducted using logistic regression and associations with gametocyte density investigated by linear regression. All analyses were performed using Stata 12 or R version 2.14.0.
Results
A total of 2083 individuals with age distribution representative for the population were surveyed; demographic and clinical characteristics are summarized in Table 1.
Table 1. Demographic, clinical and parasitological characteristics of study participants.
| n | % | ||
|---|---|---|---|
| 2083 | 100 | ||
| Area | Malala | 936 | 44.9 |
| Mugil | 799 | 38.4 | |
| Utu | 348 | 16.7 | |
| Age group (n = 1967) | 0–3 | 291 | 14.0 |
| >3–6 | 228 | 10.9 | |
| >6–9 | 224 | 10.6 | |
| >9–12 | 175 | 8.5 | |
| >12–20 | 198 | 9.5 | |
| >20 | 851 | 40.9 | |
| Bednet use (n = 2065) | Yes | 1594 | 76.5 |
| Malaria last 2 weeks (n = 2973) | Yes | 166 | 8.0 |
| Anti-malarials in last 2 weeks (n = 2078) | Yes | 61 | 2.9 |
| Anaemia (n = 1816) | No | 763 | 36.6 |
| Mild | 942 | 45.2 | |
| Moderate | 111 | 5.3 | |
| Current or recent febrile illness (n = 2083) | Yes | 199 | 9.5 |
| Clinical Malaria | P. falciparum | 21 | 1.0 |
| P. vivax | 9 | 0.4 | |
| Pf/Pv mixed | 5 | 0.2 | |
| Plasmodium spp. infection by LM | P. falciparum | 155 | 7.4 |
| asexuals only | 82 | ||
| gametocytes only | 38 | ||
| both | 35 | ||
| P. vivax | 146 | 7.0 | |
| asexuals only | 103 | ||
| gametocytes only | 3 | ||
| both | 40 | ||
| P. malariae | 6 | 0.3 | |
| P. ovale | 0 | 0 | |
| Pf/Pv mixed | 10 | 0.9 |
Overall, the prevalence rate (PR) by light microscopy was 7.4% P. falciparum, 7.0% P. vivax, 0.29% P. malariae, 0% P. ovale and 0.9% mixed P. falciparum/P. vivax. The overall prevalence of clinical malaria was 1.6% (n = 34); 88.1% of all LM-positive infections were asymptomatic (Table 1).
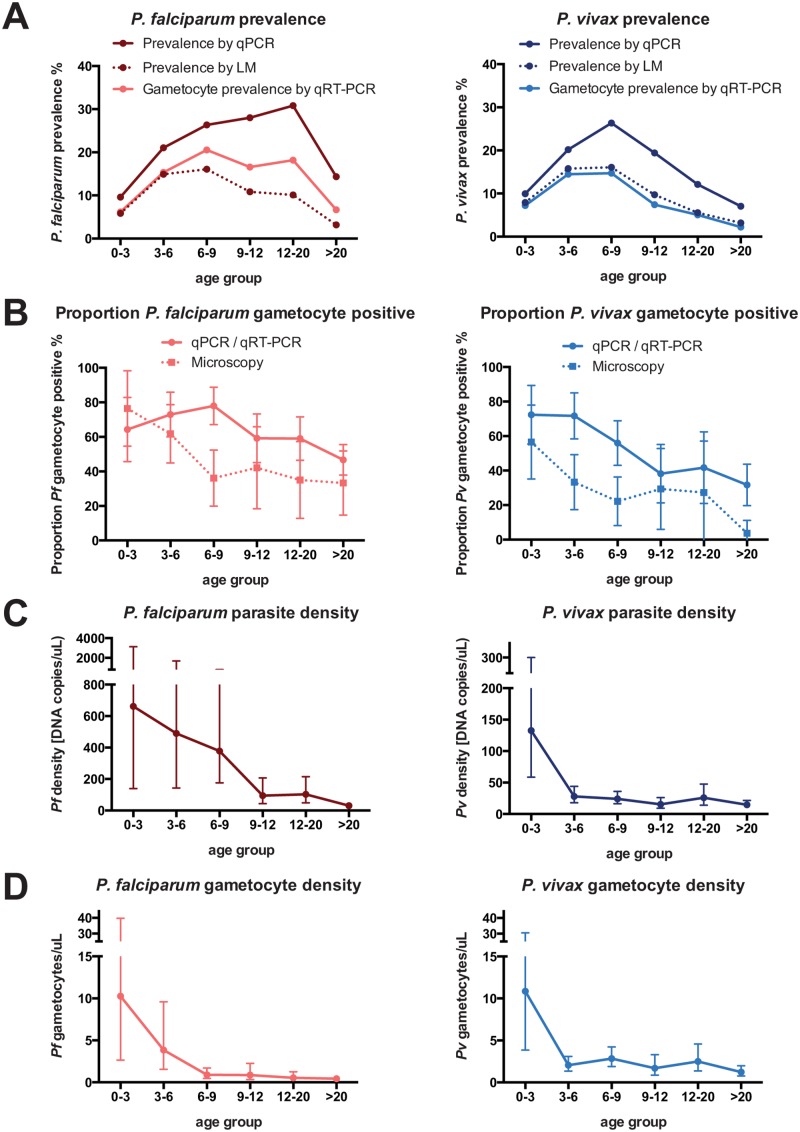
52.9% of P. falciparum-positive samples had only asexual stages, 24.5% only gametocytes and 22.6% both. Of P. vivax-positive samples 70.5% had asexual stages only, 2.1% gametocytes only and 27.4% both. By LM P. falciparum gametocytes were thus detected in 73 (3.5%) individuals and P. vivax gametocytes in 43 (2.1%) individuals. Geometric mean asexual and sexual parasite densities by LM were 808.0 (CI95[579.3–1127.0]) and 158.3 (CI95[117.4–213.3]) P. falciparum parasites/μL and 117.6 (CI95[97.3–142.1]) and 34.9 (CI95[26.9–45.3]) P. vivax parasites/μL. For both species, overall prevalence (Fig 1A, P<0.001) and the proportion gametocyte positive (Fig 1B, Pf: P = 0.010, Pv: P = 0.002) differed significantly between age groups.
Fig 1. Age trends in P. falciparum and P. vivax blood-stage and gametocyte prevalence and density.
Error bars represent CI95.
Parasite prevalence by PCR
By qPCR, 385 out of 2083 samples (18.5%) were positive for P. falciparum and 270 (13.0%) for P. vivax. Of these, 81 (3.9%) carried both species. P. malariae and P. ovale were rare (28 and 2 infections) and occurred mostly (17/30) in participants concurrently infected with P. falciparum and/or P. vivax. Of all individuals positive by PCR, 52.5% were negative by LM, 89.6% were asymptomatic and 5.6% met the definition of clinical malaria (fever and parasites detected by LM). Prevalence for P. falciparum and P. vivax showed pronounced differences between age groups (Fig 1A, P<0.001) with P. falciparum peaking in individuals 12–20 years of age and P. vivax peaking in children 6–9 years of age. P. falciparum prevalence was higher in mild-moderately anaemic and febrile individuals, whereas P. vivax was less common in individuals with recent malaria episodes (Tables 2 and 3).
Table 2. Multivariate predictors of P. falciparum parasite prevalence and proportion of gametocyte positive.
| Parasite prevalence (n = 1,714) | Proportion gametocyte positive (n = 349) | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| % | aOR | 95% CI | P-value | % | aOR | 95% CI | P-value | ||
| Gene copies/μL (log) 1 | 1.85 | [1.50, 2.28] | <0.001 | ||||||
| Mixed Pf/Pv (by pcr) | No | 63.8 | 1 | ||||||
| Yes | 48.2 | 0.40 | [0.23, 0.71] | 0.002 | |||||
| Age group | 0–3 | 9.6 | 1 | <0.001 | 64.3 | ||||
| >3–6 | 21.1 | 2.34 | [1.38, 3.97] | 72.9 | |||||
| >6–9 | 26.3 | 3.40 | [2.04, 5.68] | 78.0 | |||||
| >9–12 | 28.0 | 3.65 | [2.12, 6.29] | 59.2 | |||||
| >12–20 | 30.8 | 4.87 | [2.88, 8.24] | 59.0 | |||||
| >20 | 14.3 | 1.78 | [1.13, 2.81] | 46.7 | |||||
| Malaria last 2 weeks | No | 18.1 | 57.7 | 1 | |||||
| Yes | 22.3 | 83.8 | 3.78 | [1.42, 10.1] | 0.008 | ||||
| Febrile | No | 17.8 | 1 | 0.001 | 58.0 | ||||
| Yes | 24.6 | 1.87 | [1.27, 2.75] | 77.6 | |||||
| Anaemia | No | 14.7 | 1 | <0.001 | 49.1 | 1 | 0.019 | ||
| Mild | 23.0 | 1.78 | [1.36, 2.34] | 66.1 | 1.63 | [0.99, 2.70] | |||
| Moderate | 20.7 | 1.70 | [1.01, 2.84] | 52.2 | 0.46 | [0.16, 1.33] | |||
aOR = adjusted odds ratio (adjusted for multivariate analysis), CI = confidence interval
1 Increase in the probability that gametocytes are detected in a P. falciparum positive sample, if the parasite density increases 10-fold
Table 3. Multivariate predictors of P. vivax parasite prevalence and proportion gametocyte positive.
| Parasite prevalence (n = 1,958) | Proportion gametocyte positive (n = 224) | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| % | aOR | 95% CI | P-value | % | aOR | 95% CI | P-value | ||
| Gene copies/μL (log) 1 | 2.85 | [1.74, 4.67] | <0.001 | ||||||
| Mixed Pf/Pv (by pcr) | No | 48.7 | |||||||
| Yes | 49.4 | ||||||||
| Age group | 0–3 | 10.0 | 1 | <0.001 | 72.4 | 1 | 0.011 | ||
| >3–6 | 20.2 | 2.35 | [1.41, 3.90] | 71.7 | 1.10 | [0.32, 3.75] | |||
| >6–9 | 26.3 | 3.30 | [2.02, 5.40] | 55.9 | 0.53 | [0.17, 1.68] | |||
| >9–12 | 19.4 | 2.26 | [1.31, 3.88] | 38.2 | 0.36 | [0.10, 1.33] | |||
| >12–20 | 12.1 | 1.26 | [0.71, 2.25] | 41.7 | 0.33 | [0.08, 1.31] | |||
| >20 | 7.0 | 0.69 | [0.43, 1.11] | 31.7 | 0.20 | [0.06, 0.67] | |||
| Malaria last 2 weeks | No | 13.5 | 0.029 | 49.2 | |||||
| Yes | 6.0 | 0.48 | [0.25, 0.93] | 40.0 | |||||
| Febrile | No | 13.2 | 48.8 | ||||||
| Yes | 11.1 | 50.0 | |||||||
| Anaemia | No | 11.0 | 41.7 | 1 | 0.048 | ||||
| Mild | 15.5 | 47.3 | 0.66 | [0.34, 1.30] | |||||
| Moderate | 9.0 | 90.0 | 8.56 | [0.94, 77.7] | |||||
aOR = adjusted odds ratio (adjusted for multivariate analysis), CI = confidence interval
1 Increase in the probability that gametocytes are detected in a P. vivax positive sample, if the parasite density increases 10-fold
Geometric mean parasite densities by qPCR were very low with 126.8 (CI95 [91.1–176.5]) copies per μL/blood for P. falciparum and 23.8 (CI95 [19.5–29.1]) copies/μL for P. vivax. Assuming that all 3 copies of the marker gene were amplified, this corresponds to 42 P. falciparum and 8 P. vivax genomes per μL. Densities of P. falciparum and P. vivax were 14- and 10-fold lower in adults as compared to children <3 years (Fig 1C), and P. vivax densities dropped more rapidly with age than P. falciparum densities (Fig 1C). In samples that were positive by both qPCR and LM, densities were more highly correlated for P. falciparum (r S = 0.81, n = 144) than P. vivax (r S = 0.39, n = 139, S1 Fig).
Gametocyte prevalence by qRT-PCR
By qRT-PCR, 233/385 (60.5%) of P. falciparum positive and 132/270 (48.9%) of P. vivax positive individuals carried detectable gametocytes, resulting in a population gametocyte prevalence of 11.2% and 6.3%.
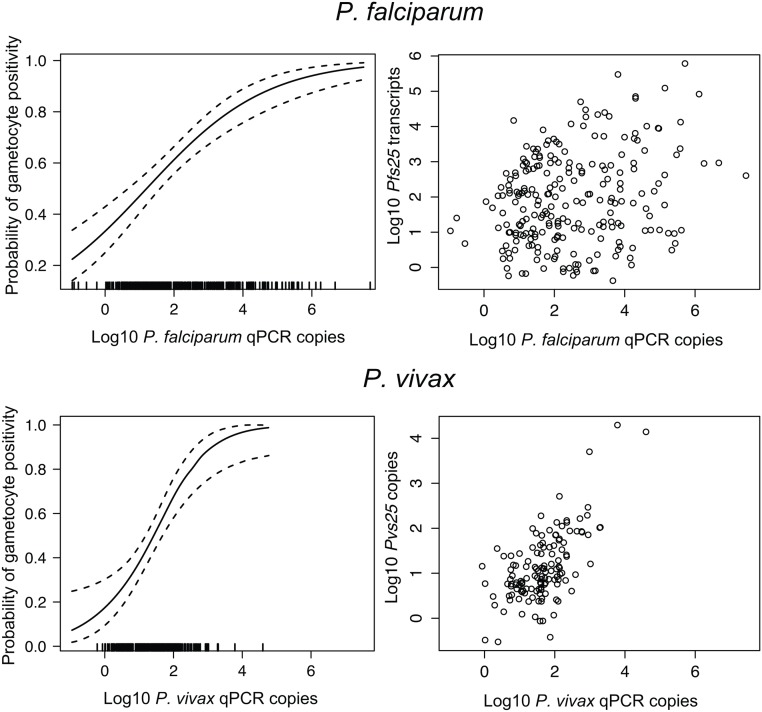
For both species, the likelihood to detect gametocytes was considerably higher in samples with high blood-stage parasitaemia (Fig 2). Each log increase in parasite genome copy density was associated with a 1.77-fold increase (CI95[1.47–2.13], P<0.001) in the odds of carrying P. falciparum and a 3.27-fold increase (CI95[2.16–4.95], P<0.001) in the odds of carrying P. vivax gametocytes. As a result gametocytes were detected in nearly all LM-positive infections (Pf: 88.2%, Pv: 79.3%) but in a much lower proportion of submicroscopic infections (Pf: 44.0%, Pv: 16.1%, P<0.001). P. falciparum gametocyte densities were 6-fold higher in samples positive by microscopy as compared to submicroscopic infections (2.45 [1.50–3.99] vs. 0.39 [0.28–0.56] gametocytes/uL), while P. vivax gametocyte densities were similar in both groups (2.77 [2.07–3.71] vs. 2.22 [1.37–3.61] gametocytes/uL). Co-infections with P. vivax resulted in a significantly lower proportion P. falciparum gametocyte positive (48.1% vs. 63.8%, P = 0.010) but not vice versa.
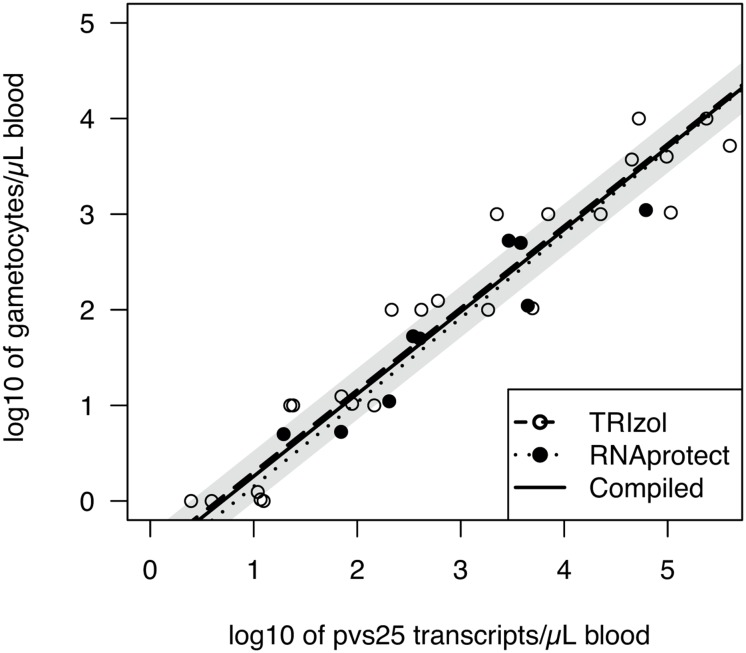
Fig 2. pvs25 transcript numbers versus light microscopically determined P. vivax gametocyte counts.
Dilution series were made before storing samples in RNAprotect (5 dilution steps) or after RNA extraction of samples stored in TRIzol (3 dilution steps). Dots represent means of technical triplicates (TRIzol) or quintuplicates (RNAprotect) of dilutions except for the highest concentration (no replicates). Shaded grey shows the CI95 of the intercept of the regression of compiled sample sets.
P. falciparum gametocyte prevalence and the proportion gametocyte positive peaked in children 6–9 years of age (20.5% and 78.0%) and was lowest (6.7% and 46.7%) in adults (P = 0.001, Fig 1, Table 2). P. vivax gametocyte prevalence among all study participants decreased from 14.6% in children 3–9 years to 2.2% in adults (P<0.001; Table 3) while the proportion P. vivax gametocyte positive dropped from 71–72% in children below 6 years to 31.7% in adults.
The proportion gametocyte positive for both species was also associated with haemoglobin levels, albeit in different ways. P. falciparum gametocytes were most commonly present in participants with mild anaemia (Table 2, Hb 8.0–10.9g/dL, 66.0%, P = 0.008), whereas P. vivax gametocytes were most common in participants with moderate-to-severe anaemia (Hb <8g/dL; Table 3, 90.0%). Lastly, participants who reported a malaria episode in the last 2 weeks were more likely to have P. falciparum gametocytes (83.8% vs. 57.7%, P = 0.002; Table 2). After accounting for all other factors, blood-stage parasitaemia remains the most important predictor of carriage of gametocytes (Tables 2 and 3).
All symptomatic P. falciparum and 11/13 P. vivax infections carried gametocytes. However, when corrected for asexual densities clinical malaria itself was not significantly associated with gametocyte carriage for either species. Blood-stage P. falciparum and P. vivax parasitaemia was 570- and 5-fold higher in symptomatic than in asymptomatic individuals (Pf: 48212 CI95[14358–161888] vs. 84.0 CI95 [62.1–113.6] parasites/μL, Pv: 104.4 CI95[28.2–387.1] vs. 21.8 CI95[17.9–26.6] parasites/μL).
Quantification of gametocytes by qRT-PCR
pfs25 densities were converted to P. falciparum gametocyte densities based on published trend-lines: gametocytes/μL = 10−1.6225*tpfs25 0.8518, where tpfs25 is the number of pfs25 transcripts/μL detected by qRT-PCR [33]. This corresponds to approximately 50–180 pfs25 transcripts per cultured P. falciparum gametocyte. For pvs25 expression, storage in TRIzol or RNAprotect resulted in very similar trend-lines (Fig 3). The conversion [with CI95] obtained from samples stored in TRIzol was: gametocytes/μL = 10−0.5546[-0.8973;-0.2120]*tpvs25 0.8576[0.8057;0.9095]. Conversion of samples stored in RNAprotect was: gametocytes/μl = 10−0.7283[-1.3802; -0.0765]*tpvs25 0.8804[0.7041; 1.0567]. For all further analysis, data was pooled and the following conversion applied: gametocytes/μL = 10−0.5171[-0.7452;-0.2890]*tpvs25 0.8339[0.8033;0.8645]. Thus one gametocyte roughly corresponds to 4.17 [2.16–8.47] pvs25 transcripts, though this is not a linear, but a logarithmic relationship, where higher gametocyte densities show a higher number of transcripts/gametocyte.
Fig 3. Relationship between parasite density and probability that a sample is gametocyte positive.
Left: Probability (with CI95) that a sample is gametocyte positive vs. parasite density, calculated using a general additive model. Right: correlation between gametocyte density (measured as pfs25 or pvs25 transcripts/uL) and parasite density by qPCR.
Among qRT-PCR positive participants, mean pfs25 density was 86.4 transcripts/μL (CI95[58.7–127.1]), and mean pvs25 density was 13.6 transcripts/μL (CI95[10.0–18.4]). This corresponds to 1.06 (CI95[0.77–1.48]) P. falciparum and 2.67 (CI95[2.07–3.45]) P. vivax gametocytes/μL. Gametocyte densities were significantly higher in participants with LM-detectable gametocytaemia (Pf: 12.1 vs. 0.37/μL P<0.001; Pv: 6.5 vs. 1.75/μL, P<0.01). For samples with ≥1 gametocyte/μL by qRT-PCR, a strong correlation between densities by LM and qRT-PCR was observed (Pf: r = 0.696, P<0.001, Pv: r = 0.574, P = 0.001, for log-transformed values).
P. vivax gametocyte densities were strongly correlated with P. vivax blood-stage parasitaemia by qPCR (r = 0.636, P<0.001, log-transformed values). A small but still highly significant correlation was also found between P. falciparum gametocyte and genome copy numbers (r = 0.259, P<0.001) (Fig 2).
The age-associated reduction in gametocyte densities was even faster than that for blood-stage parasite densities (Fig 1D, P<0.001). P. falciparum and P. vivax gametocyte densities dropped 2.7-fold and 5.3-fold between children 0–3 and 3–6 years of age. P. falciparum gametocyte densities were significantly higher in individuals who reported a recent malaria episode (5.7 vs. 0.83 gametocytes/μL P<0.001). These factors remain significantly associated in multivariate analyses (Table 4).
Table 4. Determinants of P. falciparum and P. vivax gametocyte density.
| P. falciparum | P. vivax | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| GMD | β | 95% CI | P-value | GMD | β | 95% CI | P-value | ||
| Gene copies/μL (log) | 0.13 | [0.02, 0.24] | 0.022 | 0.57 | [0.43, 0.72] | <0.001 | |||
| Age group | 0–3 | 21.1 | 0 | <0.001 | 10.5 | 0 | 0.026 | ||
| >3–6 | 15.2 | -0.46 | [-1.14, 0.21] | 2.8 | -0.47 | [-0.81, -0.13] | |||
| >6–9 | 2.8 | -1.04 | [-1.70, -0.39] | 2.0 | -0.23 | [-0.57, 0.11] | |||
| >9–12 | 8.9 | -1.06 | [-1.77, -0.35] | 1.8 | -0.55 | [-0.97, -0.13] | |||
| >12–20 | 5.0 | -1.31 | [-2.00, -0.63] | 1.9 | -0.45 | [-0.90, -0.00] | |||
| >20 | 3.2 | -1.39 | [-2.05, -0.74] | 1.9 | -0.55 | [-0.95, -0.16] | |||
| Malaria last 2 weeks | Yes | 28.3 | 0.94 | [0.48, 1.40] | <0.001 | 61.9 | NS | ||
| No | 4.3 | 2.5 | |||||||
| Intercept | 0.53 | [-0.15, 1.20] | -0.46 | [-0.88, -0.04] | 0.032 | ||||
GMD = geometric mean density, β = regression coefficient, CI = confidence interval
Discussion
Mass-distribution of LLINs in 2008 resulted in ~70% coverage [32] and led to a substantial reduction in malaria transmission in the study area. Compared to 2006 the prevalence of P. falciparum and P. vivax infections dropped from 39% to 18% and from 32% to 13%, respectively [36,37]. Considerably fewer mixed-species infections were detected as compared to previous studies in PNG, where up to 32% of all individuals sampled were infected by several species concurrently [38,39]. Nevertheless, transmission of P. falciparum and P. vivax on the north coast of PNG remains high, clinical immunity is acquired rapidly and—as a consequence—the vast majority of infections are asymptomatic (90%) and of low density (52% submicroscopic). These infections are not targeted by the current control strategy of ACT-based case management plus LLINs, and thus constitute a potentially important reservoir of transmission.
qRT-PCR detected gametocytes in 60% of P. falciparum and 51% of P. vivax positive individuals. The results corresponded very well with an earlier PNG study that used identical methods and found 59% of P. falciparum and 52% of P. vivax positive children aged 5–10 carrying gametocytes [33]. Gametocyte carriage was low compared to other studies, where nearly all infected individuals carried gametocytes [22–24,26] and contradicts earlier studies based on light microscopy that reported that considerably higher proportions of P. vivax than P. falciparum infections carried gametocytes [8,13]. However, most of these other studies were conducted on symptomatic patients with relatively high parasitaemia (>5000 parasites/μL) [8,13,22,24,26].
In this cross-sectional study, blood-stage parasite density was the strongest predictor for gametocyte carriage. Thus for both species gametocytes were detected in almost all symptomatic and the vast majority of LM-positive infections.
Parasite densities decrease at an early age, because in areas of intense transmission many individuals are immune or semi-immune to malaria [38,39]. Thus, the proportion of gametocyte positive individuals was highest in young children. As only a small fraction of all parasites were gametocytes, the number of gametocyte carriers detected among individuals carrying low parasite densities was heavily dependent on the sensitivity of the assays and the amount of blood assessed. Both the pfs25 and pvs25 qRT-PCRs were able to detect as little as 1–2 transcripts/μL blood. Using the same detection techniques for P. falciparum gametocytes from culture [33] and serial dilutions of P. vivax gametocytes from clinical cases, around 10-times more pfs25 than pvs25 transcripts/gametocyte were detected. Thus in field samples as little as a single P. falciparum gametocyte can be detected in 50μL blood, assuming it provides 1–2 pfs25 transcripts/μL extracted RNA. For P. vivax, however, a density of 10 gametocytes/50μL blood would be required for an equal probability of detection. This explains why no gametocytes were detected in 84% of all submicroscopic P. vivax infections, and where detected, their similar densities in microscopy positive and submicroscopic infections. Likely gametocytes were present in some of the submicroscopic, gametocyte negative infections, yet at densities below the detection limit of qRT-PCR.
The sensitivity of an assay for detection of blood-stage parasites, and thus the number of parasite positive individuals, can greatly influence the proportion of gametocyte carriers and therefore can explain differences between studies. The qPCR used in this study has a detection limit of one 18S rRNA gene copy/μL and detects even very low parasite densities typical for asymptomatic individuals. The same samples were screened with a nested PCR for Pfmsp2 and Pvmsp1F3 followed by gel electrophoresis [40,41]. This assay was less sensitive and yielded lower parasite prevalence rates but higher proportions of gametocyte positive samples (Pf: 69.5%, Pv: 66.7%). In a different study, detection of parasites based on highly abundant RNA instead of DNA led to a pronounced increase in prevalence, but the proportion of gametocyte positive samples dropped from 59 to 41% for P. falciparum and from 53 to 36% for P. vivax [33]. In conclusion, the more sensitive the assay to detect blood-stage parasites, the more very low-density infections are detected, and the lower the proportion of gametocyte positive samples among all positive samples.
In this cross-sectional survey 56% P. falciparum and 81% P. vivax carriers had <100 18S rRNA gene copies/μL. The smaller proportion of P. vivax than P. falciparum gametocyte carriers is thus a consequence of the lower expression level of pvs25 as compared to pfs25 and the lower average densities of P. vivax infections.
As expected qRT-PCR estimates of gametocytaemia were much more closely linked to parasite densities by qPCR for P. vivax than for P. falciparum. P. vivax gametocytes mature rapidly [1] and follow levels of asexual parasitaemia [3]. Blood-stage parasitaemia is therefore a good surrogate marker for P. vivax gametocytaemia. P. falciparum gametocytes develop for 7–10 days in the bone marrow [42] before stage V gametocytes start appearing in the blood stream [1]. In P. falciparum, gametocytaemia is thus likely to be more related to the parasitaemia two weeks earlier than to concurrent parasitaemia.
LM and qRT-PCR estimates of gametocyte density were much more closely correlated for P. falciparum than P. vivax, possibly because the characteristic ‘banana-shaped’ P. falciparum gametocytes are more easily identifiable than P. vivax gametocytes, which resemble asexual parasites. At lower densities there was no correlation between the two measures for either species. By LM a maximum of 0.0625μL blood was counted making estimates of densities error-prone. Furthermore, Plasmodium spp. are probably not randomly distributed in blood, autoagglutination of asexual parasites was reported for P. falciparum [43]. It is possible that gametocytes also cluster to increase the chance that at least one male and one female gametocyte being taken up in a 2–5μL mosquito blood meal [44]. At densities <1 gametocyte/μL, detection of gametocytes in such small volumes of blood examined by LM becomes stochastic. Estimates of gametocytaemia by qRT-PCR based on RNA extracted from 50μL blood are thus likely more accurate than those by LM.
The contribution of very low-density gametocyte carriers to transmission is not clear. Infectiveness of individuals negative by microscopy has been repeatedly reported. P. falciparum infections with sub-patent gametocytaemia in children from Burkina Faso [45] and Kenya [27] infected 24.2% and 43.5% of Anopheles gambiae, mosquitoes, respectively. Similarly, the infectivity of sub-microscopic P. vivax infections has been shown in studies from Thailand [46–48], Sri Lanka [49], Peru [30] and PNG [19]. The qRT-PCR applied detects 1–5 gametocytes/50μL blood. At such low gametocyte densities, a mosquito might not always take up at least one male and one female gametocyte in its 3–5μL blood meal [44] and therefore not all qRT-PCR positive individuals might be infective. Further studies comparing gametocyte quantification by qRT-PCR to infectivity in mosquito feeding assays are thus needed to accurately quantify the contribution of these very low-density infections to malaria transmission.
Supporting Information
The Spearman correlation for P. falciparum was 0.81 and for P. vivax 0.39.
(PDF)
Acknowledgments
First and foremost, we wish to sincerely thank all members of the communities that participated in the surveys. We thank PNGIMR Madang microscopy, laboratory, field and administration staff, in particular the efforts of Jack Taraika, Danga Mark, Maggie Raiko, Nandao Tarongka, Lina Lorry, John Taime and Andrew Raiko. We thank Stephan Karl and Nattawan Rachaphaew for help with sample preparation and microscopy of gametocytes for the pvs25 trend-line, and Connie SN Li Wai Suen for statistical support.
Data Availability
Data are available from Dryad with accession number: doi:10.5061/dryad.550p3.
Funding Statement
This study was supported by the TransEPI consortium funded by the Bill & Melinda Gates Foundation (www.gatesfoundation.org), and an NHMRC project grant (#1021455, www.nhmrc.gov.au), Swiss National Science Foundation grant (310030_134889, www.snf.ch), and NIH International Centers of Excellence in Malaria Research grant (U19 AI089686, www.niaid.nih.gov). Samples were collected as part of the Bill & Melinda Gates Foundation funded PNG IPTi study. This work was made possible through Victorian State Government Operational Infrastructure Support and Australian Government NHMRC IRIISS. LJ Robinson is supported by an NHMRC Early Career Fellowship (#1016443). IM is supported by an NHMRC Senior Research Fellowship (#1043345). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1. Bousema T, Drakeley C. Epidemiology and infectivity of Plasmodium falciparum and Plasmodium vivax gametocytes in relation to malaria control and elimination. Clin Microbiol Rev. 2011;24(2):377–410. 10.1128/CMR.00051-10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Garnham PCC. Malaria Parasites And Other Heamosporidia. Oxford: Blackwell Scientific Publications; 1966. [Google Scholar]
- 3. McCarthy JS, Griffin PM, Sekuloski S, Bright AT, Rockett R, Looke D, et al. Experimentally induced blood-stage Plasmodium vivax infection in healthy volunteers. J Infect Dis. 2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Smalley ME, Sinden RE. Plasmodium-Falciparum Gametocytes—Their Longevity and Infectivity. Parasitology. 1977;74(Feb):1–8. [DOI] [PubMed] [Google Scholar]
- 5. Bousema T, Okell L, Shekalaghe S, Griffin JT, Omar S, Sawa P, et al. Revisiting the circulation time of Plasmodium falciparum gametocytes: molecular detection methods to estimate the duration of gametocyte carriage and the effect of gametocytocidal drugs. Malaria J. 2010;9:136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Carter R, Graves PM. Gametocytes In: Wernsdorfer WH, McGregor IA, editors. Malaria: principles and practice of malariology. Edinburgh, United Kingdom: Churchill Livingstone; 1988. p. 253–306. [Google Scholar]
- 7. Price R, Nosten F, Simpson JA, Luxemburger C, Phaipun L, ter Kuile F, et al. Risk factors for gametocyte carriage in uncomplicated falciparum malaria. Am Journal Trop Med Hyg. 1999;60(6):1019–23. [DOI] [PubMed] [Google Scholar]
- 8. McKenzie FE, Wongsrichanalai C, Magill AJ, Forney JR, Permpanich B, Lucas C, et al. Gametocytemia in Plasmodium vivax and Plasmodium falciparum infections. J Parasitology. 2006;92(6):1281–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Mawili-Mboumba DP, Nikiema R, Bouyou-Akotet MK, Bahamontes-Rosa N, Traore A, Kombila M. Sub-microscopic gametocyte carriage in febrile children living in different areas of Gabon. Malaria J. 2013;12:375 10.1186/1475-2875-12-375 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Sowunmi A, Fateye BA, Adedeji AA, Fehintola FA, Happi TC. Risk factors for gametocyte carriage in uncomplicated falciparum malaria in children. Parasitology. 2004;129(Pt 3):255–62. [DOI] [PubMed] [Google Scholar]
- 11. von Seidlein L, Drakeley C, Greenwood B, Walraven G, Targett G. Risk factors for gametocyte carriage in Gambian children. Am Journal Trop Med Hyg. 2001;65(5):523–7. [DOI] [PubMed] [Google Scholar]
- 12. Hasugian AR, Purba HL, Kenangalem E, Wuwung RM, Ebsworth EP, Maristela R, et al. Dihydroartemisinin-piperaquine versus artesunate-amodiaquine: superior efficacy and posttreatment prophylaxis against multidrug-resistant Plasmodium falciparum and Plasmodium vivax malaria. Clin Infect Dis. 2007;44(8):1067–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Gamage-Mendis AC, Rajakaruna J, Carter R, Mendis KN. Infectious reservoir of Plasmodium vivax and Plasmodium falciparum malaria in an endemic region of Sri Lanka. Am Journal Trop Med Hyg. 1991;45(4):479–87. [DOI] [PubMed] [Google Scholar]
- 14. Douglas NM, Simpson JA, Phyo AP, Siswantoro H, Hasugian AR, Kenangalem E, et al. Gametocyte Dynamics and the Role of Drugs in Reducing the Transmission Potential of Plasmodium vivax . J Infect Dis 2013;208(5):801–12. 10.1093/infdis/jit261 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Huh AJ, Kwak YG, Kim ES, Lee KS, Yeom JS, Cho YK, et al. Parasitemia characteristics of Plasmodium vivax malaria patients in the Republic of Korea. J Korean Med Sci. 2011;26(1):42–6. 10.3346/jkms.2011.26.1.42 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Cattani JA, Tulloch JL, Vrbova H, Jolley D, Gibson FD, Moir JS, et al. The epidemiology of malaria in a population surrounding Madang, Papua New Guinea. Am J Trop Med Hyg. 1986;35(1):3–15. [DOI] [PubMed] [Google Scholar]
- 17. Gneme A, Guelbeogo WM, Riehle MM, Tiono AB, Diarra A, Kabre GB, et al. Plasmodium species occurrence, temporal distribution and interaction in a child-aged population in rural Burkina Faso. Malaria J. 2013;12:67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Bousema JT, Gouagna LC, Drakeley CJ, Meutstege AM, Okech BA, Akim IN, et al. Plasmodium falciparum gametocyte carriage in asymptomatic children in western Kenya. Malaria J. 2004;3:18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Graves PM, Burkot TR, Carter R, Cattani JA, Lagog M, Parker J, et al. Measurement of malarial infectivity of human populations to mosquitoes in the Madang area, Papua, New Guinea. Parasitology. 1988;96 (Pt 2):251–63. [DOI] [PubMed] [Google Scholar]
- 20. Shekalaghe SA, Bousema JT, Kunei KK, Lushino P, Masokoto A, Wolters LR, et al. Submicroscopic Plasmodium falciparum gametocyte carriage is common in an area of low and seasonal transmission in Tanzania. Trop Med Int Health. 2007;12(4):547–53. [DOI] [PubMed] [Google Scholar]
- 21. Bousema JT, Schneider P, Gouagna LC, Drakeley CJ, Tostmann A, Houben R, et al. Moderate effect of artemisinin-based combination therapy on transmission of Plasmodium falciparum . J Infect Dis. 2006;193(8):1151–9. [DOI] [PubMed] [Google Scholar]
- 22. Beurskens M, Mens P, Schallig H, Syafruddin D, Asih PB, Hermsen R, et al. Quantitative determination of Plasmodium vivax gametocytes by real-time quantitative nucleic acid sequence-based amplification in clinical samples. Am J Trop Med Hyg. 2009;81(2):366–9. [PubMed] [Google Scholar]
- 23. Ouedraogo AL, Bousema T, Schneider P, de Vlas SJ, Ilboudo-Sanogo E, Cuzin-Ouattara N, et al. Substantial contribution of submicroscopical Plasmodium falciparum gametocyte carriage to the infectious reservoir in an area of seasonal transmission. PloS One. 2009;4(12):e8410 10.1371/journal.pone.0008410 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Kuamsab N, Putaporntip C, Pattanawong U, Jongwutiwes S. Simultaneous detection of Plasmodium vivax and Plasmodium falciparum gametocytes in clinical isolates by multiplex-nested RT-PCR. Malaria J. 2012;11:190 10.1186/1475-2875-11-190 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. El-Sayed B, El-Zaki SE, Babiker H, Gadalla N, Ageep T, Mansour F, et al. A randomized open-label trial of artesunate- sulfadoxine-pyrimethamine with or without primaquine for elimination of sub-microscopic P. falciparum parasitaemia and gametocyte carriage in eastern Sudan. PloS One. 2007;2(12):e1311 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Lima NF, Bastos MS, Ferreira MU. Plasmodium vivax: reverse transcriptase real-time PCR for gametocyte detection and quantitation in clinical samples. Exp Parasitol. 2012;132(3):348–54. 10.1016/j.exppara.2012.08.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Schneider P, Bousema JT, Gouagna LC, Otieno S, van de Vegte-Bolmer M, Omar SA, et al. Submicroscopic Plasmodium falciparum gametocyte densities frequently result in mosquito infection. Am J Trop Med Hyg. 2007;76(3):470–4. [PubMed] [Google Scholar]
- 28. Coleman RE, Kumpitak C, Ponlawat A, Maneechai N, Phunkitchar V, Rachapaew N, et al. Infectivity of asymptomatic Plasmodium-infected human populations to Anopheles dirus mosquitoes in western Thailand. J Med Entomol. 2004;41(2):201–8. [DOI] [PubMed] [Google Scholar]
- 29. Sattabongkot J, Maneechai N, Rosenberg R. Plasmodium vivax: gametocyte infectivity of naturally infected Thai adults. Parasitology. 1991;102 Pt 1:27–31. [DOI] [PubMed] [Google Scholar]
- 30. Bharti AR, Chuquiyauri R, Brouwer KC, Stancil J, Lin J, Llanos-Cuentas A, et al. Experimental infection of the neotropical malaria vector Anopheles darlingi by human patient-derived Plasmodium vivax in the Peruvian Amazon. Am J Trop Med Hyg. 2006;75(4):610–6. [PMC free article] [PubMed] [Google Scholar]
- 31. Pethleart A, Prajakwong S, Suwonkerd W, Corthong B, Webber R, Curtis C. Infectious reservoir of Plasmodium infection in Mae Hong Son Province, north-west Thailand. Malaria J. 2004;3:34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Hetzel MW, Gideon G, Lote N, Makita L, Siba PM, Mueller I. Ownership and usage of mosquito nets after four years of large-scale free distribution in Papua New Guinea. Malaria J. 2012;11:192 10.1186/1475-2875-11-192 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Wampfler R, Mwingira F, Javati S, Robinson L, Betuela I, Siba P, et al. Strategies for Detection of Plasmodium species Gametocytes. PloS One. 2013;8(9). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Laman M, Moore BR, Benjamin J, Padapu N, Tarongka N, Siba P, et al. Comparison of an assumed versus measured leucocyte count in parasite density calculations in Papua New Guinean children with uncomplicated malaria. Malaria J. 2014;13:145 10.1186/1475-2875-13-145 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Rosanas-Urgell A, Mueller D, Betuela I, Barnadas C, Iga J, Zimmerman PA, et al. Comparison of diagnostic methods for the detection and quantification of the four sympatric Plasmodium species in field samples from Papua New Guinea. Malaria J. 2010;9:361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Schultz L, Wapling J, Mueller I, Ntsuke PO, Senn N, Nale J, et al. Multilocus haplotypes reveal variable levels of diversity and population structure of Plasmodium falciparum in Papua New Guinea, a region of intense perennial transmission. Malaria J. 2010;9:336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Arnott A, Barnadas C, Senn N, Siba P, Mueller I, Reeder JC, et al. High Genetic Diversity of Plasmodium vivax on the North Coast of Papua New Guinea. Am J Trop Med Hyg. 2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Michon P, Cole-Tobian JL, Dabod E, Schoepflin S, Igu J, Susapu M, et al. The risk of malarial infections and disease in Papua New Guinean children. Am J Trop Med Hyg. 2007;76(6):997–1008. [PMC free article] [PubMed] [Google Scholar]
- 39. Lin E, Kiniboro B, Gray L, Dobbie S, Robinson L, Laumaea A, et al. Differential patterns of infection and disease with P. falciparum and P. vivax in young Papua New Guinean children. PloS One. 2010;5(2):e9047 10.1371/journal.pone.0009047 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Schoepflin S, Valsangiacomo F, Lin E, Kiniboro B, Mueller I, Felger I. Comparison of Plasmodium falciparum allelic frequency distribution in different endemic settings by high-resolution genotyping. Malaria J. 2009;8:250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Koepfli C, Ross A, Kiniboro B, Smith TA, Zimmerman PA, Siba P, et al. Multiplicity and Diversity of Plasmodium vivax Infections in a Highly Endemic Region in Papua New Guinea. PLoS Negl Trop Dis. 2011;5(12):e1424 10.1371/journal.pntd.0001424 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Aguilar R, Magallon-Tejada A, Achtman AH, Moraleda C, Joice R, Cistero P, et al. Molecular evidence for the localization of Plasmodium falciparum immature gametocytes in bone marrow. Blood. 2014;123(7):959–66. 10.1182/blood-2013-08-520767 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Pain A, Ferguson DJ, Kai O, Urban BC, Lowe B, Marsh K, et al. Platelet-mediated clumping of Plasmodium falciparum-infected erythrocytes is a common adhesive phenotype and is associated with severe malaria. Proc Natl Acad Sci USA. 2001;98(4):1805–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Clements AN. The biology of mosquitoes, Volume 1: development, nutrition and reproduction.: CABI Publishing, United Kingdom; 2000. 511 p. [Google Scholar]
- 45. Ouedraogo AL, Schneider P, de Kruijf M, Nebie I, Verhave JP, Cuzin-Ouattara N, et al. Age-dependent distribution of Plasmodium falciparum gametocytes quantified by Pfs25 real-time QT-NASBA in a cross-sectional study in Burkina Faso. Am J Trop Med Hyg. 2007;76(4):626–30. [PubMed] [Google Scholar]
- 46. Coleman RE, Kumpitak C, Ponlawat A, Maneechai N, Phunkitchar V, Rachapaew N, et al. Infectivity of asymptomatic Plasmodium-infected human populations to Anopheles dirus mosquitoes in western Thailand. J Med Entomol. 2004;41(2):201–8. [DOI] [PubMed] [Google Scholar]
- 47. Sattabongkot J, Maneechai N, Rosenberg R. Plasmodium-Vivax—Gametocyte Infectivity of Naturally Infected Thai Adults. Parasitology. 1991;102:27–31. [DOI] [PubMed] [Google Scholar]
- 48. Sattabongkot J, Maneechai N, Phunkitchar V, Eikarat N, Khuntirat B, Sirichaisinthop J, et al. Comparison of artificial membrane feeding with direct skin feeding to estimate the infectiousness of Plasmodium vivax gametocyte carriers to mosquitoes. Am J Trop Med Hyg. 2003;69(5):529–35. [PubMed] [Google Scholar]
- 49. Gamagemendis AC, Rajakaruna J, Carter R, Mendis KN. Infectious Reservoir of Plasmodium-Vivax and Plasmodium-Falciparum Malaria in an Endemic Region of Sri-Lanka. Am J Trop Med Hyg. 1991;45(4):479–87. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
The Spearman correlation for P. falciparum was 0.81 and for P. vivax 0.39.
(PDF)
Data Availability Statement
Data are available from Dryad with accession number: doi:10.5061/dryad.550p3.