Abstract
The Contraceptive CHOICE Project (CHOICE) sought to reduce unintended pregnancies in the St. Louis Region by removing cost, education, and access barriers to highly effective contraception. CHOICE was a prospective cohort study of over 9,000 women 14–45 years of age who received tiered contraceptive counseling to increase awareness of all reversible methods available, particularly long-acting reversible contraceptive (LARC) methods. Participants were provided with contraception of their choice at no cost for 2–3 years. We studied contraceptive method choice, continuation, and population outcomes of repeat abortion and teen pregnancy. Seventy-five percent of study participants chose one of the three LARC methods (46% levonorgestrel intrauterine system, 12% copper intrauterine device, and 17% subdermal implant). LARC users reported greater continuation than non-LARC users at 12 months (87% versus 57%) and 24 months (77% versus 41%). In our cohort, LARC methods were 20 times more effective than non-LARC methods. As a result, we observed a reduction in the percent of repeat abortions from 2006 to 2010 in St. Louis compared with Kansas City and nonmetropolitan Missouri and found substantial reductions in teen pregnancy, birth, and abortion (34.0, 19.4, and 9.7 per 1000 teens, respectively) compared with national rates among sexually experienced teens (158.5, 94.0, and 41.5 per 1000, respectively). Improved access to LARC methods can result in fewer unintended pregnancies and abortions and considerable cost savings to the health care system.
Introduction
Among all pregnancies in the United States, 51% are unintended, and 40% of unintended pregnancies result in induced abortions.1 Effective family planning could prevent as many as one in every three maternal deaths globally by delaying motherhood, spacing births, avoiding unintended pregnancies and abortions, and allowing women to stop childbearing when they have reached their desired family size.2–4
Unlike the oral contraceptive pill or injection, long-acting reversible contraceptive (LARC) methods, such as the intrauterine device (IUD) and subdermal implant, are designed so that once inserted, a woman does not have to think about using birth control on a daily, weekly, monthly or quarterly basis. Women who use LARC methods experience effectiveness rates of greater than 99%; perfect and typical use effective rates are equivalent. Despite the availability of LARC, less than 8% of women in the United States use an IUD and even fewer report use of the subdermal implant.5 Women and teens experience multiple barriers when accessing and using birth control including prohibitive method costs, limited or nonexistent information about all methods available, and provider bias or outdated clinical practice regarding appropriate candidates for particular contraceptive methods.6–10
The Contraceptive CHOICE Project was launched to promote the use of long-acting, reversible contraception to reduce the number of unintended pregnancies in the St. Louis region. The project removed three key barriers to use of LARC methods: cost, education, and access. The objective of this report is to provide an overview of the key findings of CHOICE once the three barriers were removed for 9,256 St. Louis-area women and teens.
Methods
The CHOICE Project was an observational cohort study that provided each participant with the reversible contraception of her choice at no cost for 2–3 years. The CHOICE protocol was approved by the Washington University in St. Louis School of Medicine Human Research Protection Office before participant recruitment began. Women were eligible to participate if they (1) were 14–45 years of age; (2) resided in the St. Louis region; (3) were English or Spanish speaking; (4) were interested in reversible contraception; (5) were sexually active with a male partner in the past 6 months or anticipated sexual activity in the next 6 months; (6) did not desire pregnancy in the next year; and (7) were not currently using a contraceptive method or interested in starting a new reversible contraceptive method.
Between August 2007 and September 2011, participants were recruited through convenience sampling at 13 recruitment sites that included university-affiliated clinics and providers, two facilities providing abortions services, and community clinics providing family planning, obstetric, gynecologic, and primary care. Participants received standardized tiered contraceptive counseling by trained counselors who presented the contraceptive methods from most to least effective and briefly reviewed the risks, benefits, and common side effects of each method.11 Because none of the methods prevent sexually transmitted infections (STIs), counselors also discussed condom use during each counseling session, and participants were provided with free condoms. After contraceptive counseling and written informed consent, participants completed a baseline survey and were screened for STIs. A brief medical history was performed to rule out medical contraindications to specific contraceptive methods. Participants then received their contraceptive method of choice at no cost and could change their method at any time during the study participation. Study staff were trained to provide timely and accurate responses to participant questions or concerns regarding method use throughout the study. Staff-administered telephone interviews were conducted at 3 and 6 months, and at every 6 months post-enrollment for the duration of study participation. We collected data regarding method continuation, satisfaction, side effects, sexual behaviors (e.g., number of male sexual partners and coital frequency during the previous 30 days), change in reproductive plans (e.g., desire to conceive), and unintended pregnancy.
In this review, we summarize our key findings regarding method continuation, method effectiveness/failure rates, population outcomes (i.e., percentage of abortions that were repeat abortions as well as teen pregnancy rates), and the change in LARC use at select partner clinics in the St. Louis area.
Results
Seventy-five percent of CHOICE participants chose one of the three LARC methods (46% levonorgestrel intrauterine system, 12% copper IUD, and 17% subdermal implant).12 Greater LARC uptake was observed in women over 25 years of age (79%) compared with younger women 14–25 years (69%).13 Among the youngest participants, the selection of LARC method varied by age; 14- to17-year-old LARC users preferred the subdermal implant (64.5%), and 18- to 20-year-old LARC users preferred the IUD (61.4%).14
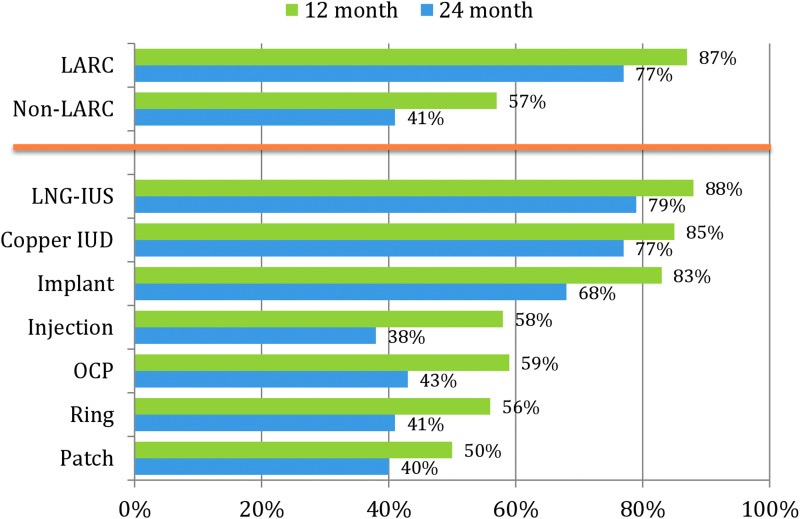
Figure 1 presents continuation data by contraceptive method. LARC users reported higher continuation than users of non-LARC methods at both 12 months (87% vs. 57%) and 24 months (77% vs. 41%).15 Among teen participants aged 14–19 years, 82% of LARC users were using their method at 12 months compared with 49% of non-LARC users. The same pattern was observed at 24 months: 67% of teen LARC users compared with 37% of teen non-LARC users were using their method at 2 years. Among the entire cohort of LARC users in the CHOICE Project, 7% reported discontinuation within the first 6 months of use.16 We found no difference in early LARC discontinuation between teens aged 14–19 and women 20 years and older (8.5% vs. 7.1%, p=0.72).
FIG. 1.
Twelve- and twenty-four-month continuation by contraceptive method. IUD, intrauterine device; LARC, long-acting reversible contraceptive; LNG-IUS, levonorgestrel intrauterine system; OCP, oral contraceptive pill.
Greater LARC uptake in our population did not result in greater sexual risk behavior (i.e., increased number of sexual partners). We found that 71% of study participants reported no change in the number of sexual partners at 12 months compared with baseline, and only 16% reported an increase.17 Of those reporting an increase in sexual partners, more than 80% reported a change from zero partners to one partner.
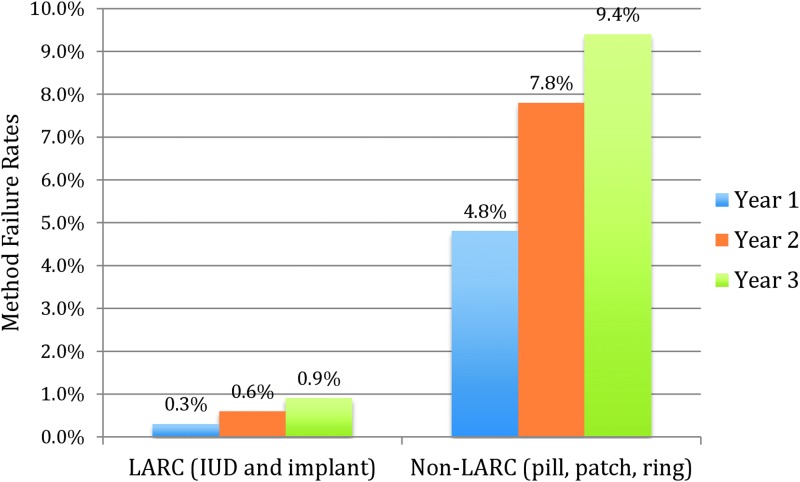
The difference in effectiveness between LARC methods and combined hormonal contraceptive methods (oral contraceptive pills, contraceptive patch, and vaginal ring) was remarkable. The cumulative contraceptive failure rates at 1, 2, and 3 years for the pills, patch, and ring (4.8%, 7.8%, and 9.4%) were more than 20 times higher than for the LARC methods (0.3%, 0.6%, and 0.9%; adjusted hazard ratio=21.8, 95% confidence interval 13.7–34.9; Fig. 2).18
FIG. 2.
Cumulative failure rates at 1, 2, and 3 years for LARC and non-LARC methods.
With respect to repeat abortion rates, we conducted an ecological analysis that compared the St. Louis region to the Kansas City region because they are similar in size and demographic profile. We observed a significant decrease (p=0.002) in the percent of repeat abortions from 2006 to 2010 in St. Louis compared with a significant increase (p=0.003) in Kansas City.12 Our analysis of teen pregnancy, birth, and abortion rates demonstrated a substantial reduction in rates observed in our cohort compared with national rates among sexually experienced teens. The average annual rates of pregnancy, birth, and abortion among CHOICE teen participants were 34.0, 19.4, and 9.7 per 1000 teens, respectively. In comparison, rates of pregnancy, birth, and abortion among sexually experienced U.S. teens in 2008 were 158.5, 94.0, and 41.5 per 1000, respectively.14
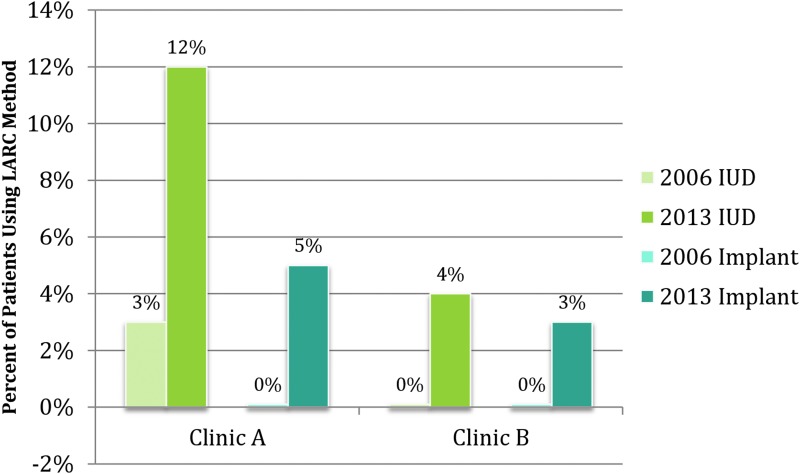
Finally, we obtained contraceptive method use data from two Title X-funded family planning clinics in our area that had partnered with CHOICE to observe the clinic-level change in LARC use from 2006 to 2013. IUD use increased from 3% to 12% and from 0% to 4% among the two clinics. Subdermal implant use increased from 0% to 5% and 0% to 3% (Fig. 3).
FIG. 3.
Change in LARC use from 2006 to 2013 in two St. Louis family planning clinics.
Discussion
The results of the Contraceptive CHOICE Project indicate several ways to address the significant public health concern posed by unintended pregnancies. In CHOICE, we found that when we removed access barriers, cost barriers, and provided women with comprehensive, accurate, unbiased counseling, women preferred the subdermal implant and IUDs: the most effective, reversible contraceptive methods.19 We found that women using LARC methods continue use at a higher rate than women using shorter-acting methods.13,15,20
Overall, the Contraceptive CHOICE Project demonstrated a shift in method use from less to more effective methods, which could provide powerful protection against teen and unintended pregnancies.12 Furthermore, the three LARC methods are among the most cost-effective forms of contraception.21 In addition, we did not find an increase in risky sexual behavior or more STIs with increased LARC use.17 Thus, increased utilization of LARC methods is an important strategy to reduce unintended pregnancies, which would both improve women's health and save health care dollars.22
The CHOICE Project provided a model of contraceptive provision that was unique but adaptable. All women received tiered contraceptive counseling by a trained counselor and were informed that LARC methods are the most effective reversible methods of contraception.11 Cost barriers were removed; all methods were provided at no cost to participants. Finally, access was increased; providers were willing to provide LARC methods to almost all women, regardless of parity, young age, or STI risk factors. In fact, the majority of LARC methods were provided on the same day as enrollment (same-day insertion). A randomized, controlled trial of a 4-hour LARC training program regarding LARC counseling and clinical practice to clinic staff at 40 Planned Parenthood locations showed that women in the intervention group were twice as likely to choose a LARC method than those in the control group.23 The LARC uptake observed in CHOICE was greater than that observed in this study, suggesting the importance of addressing all three barriers of cost, education, and access. Furthermore, the doubling of LARC use in the two Title X clinics where the CHOICE model was available to clinic patients provides encouraging evidence to support the integration of the model in the Title X setting.
Conclusion
The CHOICE Project developed and provided a high level of contraceptive care where barriers to greater LARC use were removed, and ongoing care to maximize method continuation was prioritized through close patient follow-up and responsiveness to participants' concerns and side effects. We believe this model of care, where the entire clinic prioritizes effective family planning and promotes LARC use, can be disseminated and implemented in a variety of settings. Implementation requires training of all staff, including front desk, clinical, management, and finance to ensure that affordable LARC methods are available, the most up-to-date clinical practices are documented and integrated into care, and that women hear accurate and unbiased information regarding contraception throughout their clinic experience. In response, CHOICE has catalogued the research findings, training protocols, and patient care materials used throughout the project to encourage their use by others. These materials can be found at www.CHOICEProject.wustl.edu and www.LARCFIRST.com. If successful, diffusion of the CHOICE approach may finally help reduce the number of unintended pregnancies in the United States.
Acknowledgments
This research was supported in part by (1) an anonymous foundation; (2) Washington University Institute of Clinical and Translational Science grants UL1TR000448 and TL1 TR000449 from the National Center for Advancing Translational Sciences; and (3) award number K23HD070979 from the Eunice Kennedy Shriver National Institute of Child Health and Human Development. The content is solely the responsibility of the authors and does not necessarily represent the official view of the National Institutes of Health.
Author Disclosure Statement
Dr. Madden receives honorarium for serving on an advisory board for Bayer Healthcare Pharmaceuticals and on a data safety monitoring board for phase 4 safety studies of Bayer contraceptive products. Dr. Peipert receives research support from Bayer Healthcare Pharmaceuticals, Merck & Co, Inc., and TEVA Pharmaceuticals, and serves on advisory boards for TEVA Pharmaceuticals and MicroCHIPS. For all other authors, no competing financial interests exist.
References
- 1.Finer LB, Zolna MR. Shifts in intended and unintended pregnancies in the United States, 2001–2008. Am J Public Health 2014;104:S43–48 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Luther NY, Thapa S, Westley SB. Nepal survey shows that “family planning saves lives.” Asia Pac Pop Policy 1999;49:1–4 [PubMed] [Google Scholar]
- 3.Sadik N. Reproductive health/family planning and the health of infants, girls and women. Indian J Pediatr 1997;64:739–744 [DOI] [PubMed] [Google Scholar]
- 4.Bernstein PS, Rosenfield A. Abortion and maternal health. Int J Gynaecol Obstet 1998;63:S115–S122 [DOI] [PubMed] [Google Scholar]
- 5.Finer LB, Jerman J, Kavanaugh ML. Changes in use of long-acting contraceptive methods in the United States, 2007–2009. Fertil Steril 2012;98:893–897 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Stanwood NL, Garrett JM, Konrad TR. Obstetrician-gynecologists and the intrauterine device: A survey of attitudes and practice. Obstet Gynecol 2002;99:275–280 [DOI] [PubMed] [Google Scholar]
- 7.Biggs MA, Harper CC, Malvin J, Brindis CD. Factors influencing the provision of long-acting reversible contraception in California. Obstet Gynecol 2014;123:593–602 [DOI] [PubMed] [Google Scholar]
- 8.Kavanaugh ML, Jerman J, Ethier K, Moskosky S. Meeting the contraceptive needs of teens and young adults: Youth-friendly and long-acting reversible contraceptive services in U.S. family planning facilities. J Adolesc Health 2013;52:284–292 [DOI] [PubMed] [Google Scholar]
- 9.Kavanaugh ML, Frohwirth L, Jerman J, Popkin R, Ethier K. Long-acting reversible contraception for adolescents and young adults: Patient and provider perspectives. J Pediatr Adolesc Gynecol 2013;26:86–95 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Yu JM, Henderson JT, Harper CC, Sawaya GF. Obstetrician-gynecologists' beliefs on the importance of pelvic examinations in assessing hormonal contraception eligibility. Contraception 2014;90:612–614 [DOI] [PubMed] [Google Scholar]
- 11.Madden T, Mullersman JL, Omvig KJ, Secura GM, Peipert JF. Structured contraceptive counseling provided by the Contraceptive CHOICE Project. Contraception 2013;88:243–249 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Peipert JF, Madden T, Allsworth JE, Secura GM. Preventing unintended pregnancies by providing no-cost contraception. Obstet Gynecol 2012;120:1291–1297 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Rosenstock JR, Peipert JF, Madden T, Zhao Q, Secura GM. Continuation of reversible contraception in teenagers and young women. Obstet Gynecol 2012;120:1298–1305 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Secura GM, Madden T, McNicholas C, et al. Provision of no-cost, long-acting contraception and teenage pregnancy. New Engl J Med 2014;371:1316–1323 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.O'Neil-Callahan M, Peipert JF, Zhao Q, Madden T, Secura G. Twenty-four-month continuation of reversible contraception. Obstet Gynecol 2013;122:1083–1091 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Grunloh DS, Casner T, Secura GM, Peipert JF, Madden T. Characteristics associated with discontinuation of long-acting reversible contraception within the first 6 months of use. Obstet Gynecol 2013;122:1214–1221 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Secura GM, Adams T, Buckel CM, Zhao Q, Peipert JF. Change in sexual behavior with provision of no-cost contraception. Obstet Gynecol 2014;123:771–776 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Winner B, Peipert JF, Zhao Q, et al. Effectiveness of long-acting reversible contraception. New Engl J Med 2012;366:1998–2007 [DOI] [PubMed] [Google Scholar]
- 19.Secura GM, Allsworth JE, Madden T, Mullersman JL, Peipert JF. The Contraceptive CHOICE Project: Reducing barriers to long-acting reversible contraception. Am J Obstet Gynecol 2010;203:115..e1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Peipert JF, Zhao Q, Allsworth JE, et al. Continuation and satisfaction of reversible contraception. Obstet Gynecol 2011;117:1105–1113 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Trussell J, Lalla AM, Doan QV, Reyes E, Pinto L, Gricar J. Cost effectiveness of contraceptives in the United States. Contraception 2009;79:5–14 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Cleland K, Peipert JF, Westhoff C, Spear S, Trussell J. Family planning as a cost-saving preventive health service. New Engl J Med 2011;364:e37. [DOI] [PubMed] [Google Scholar]
- 23.Harper CC, Rocca C, Darney PD, Thompson KM, Westhoff C, Speidel JJ. Long-acting reversible contraceptive training intervention: Results from a cluster randomized trial on pregnancy outcomes. Obstet Gynecol 2014;123:106S–107S [Google Scholar]