Abstract
Background:
Breast cancer and its treatment, including mastectomy, can cause feelings of mutilation, depreciation in the value of the body, reduction in attractiveness, and lead to mental disorders and hopelessness.
Objective:
The present study aimed to determine the relationship between appreciating the body, hope and mental health in women with breast cancer after mastectomy.
Materials and Methods:
This study was a descriptive study of 100 breast cancer patients who had undergone mastectomy and referred to the Sayed Al-Shohada Medical Center in Isfahan, Iran. The subjects were selected by convenient sampling. Data gathering tools were the Body Esteem Scale (BES), Herth Hope Index (HHI), and Symptom Checklist 25 (SCL-25) mental health questionnaire. Data analysis was performed using SPSS software.
Results:
Most of the patients had low body esteem. There was a significant direct linear relationship between body esteem and hope and mental health. This relationship was stronger between valuing the body and hope.
Conclusion:
Body esteem has a significant linear relationship with hope and mental health.
Keywords: Breast cancer, Hope, Mastectomy, Mental health
INTRODUCTION
Breast cancer is the most common cancer in women in most societies, including Iran, and is the most important cause of death in the world. Breast cancer after its removal is not a physical disability but perhaps an altered psychological effects on patients.[1] During the treatment process of this disease the patient has to deal with multiple issues. The impact of breast cancer and its treatment methods, such as mastectomy, on patients, include adverse effects on mental health, particularly mood disorders (depression, anxiety, and anger), hopelessness, changes in body esteem, relapse of the illness, and death.[2] Several studies showed that the loss of the breast for women is considered as a major mental injury and this has significant psychological effects on them. Psychological aspects of the patients include body esteem, hope, and mental health.[3] The impact of physical disability on body esteem is an important issue. According to Mayer and Eisenberg valuing the body refers to the positive and negative assessment of the body.[4] Breast cancer can highly impact the body esteem and feeling of attractiveness in the patient. After mastectomy, the patient cannot encounter their desired body and match it with their previous ideal body; thus, their assessment of themselves will change. Physical nature, identity formation, self-esteem, hope, mental health, and eventual success in different aspects of life are among the factors which are affected by body esteem.[5] Valuing the physical body has great influence on the mental health of individuals. Humans have physical, psychological, and social needs, with the fulfillment of which the body's internal equilibrium is established. If this balance is thwarted, many problems will follow. Psychological stress after treatment can cause emotional distress, such as anger, depression, and hopelessness, in the patient.[6] Based on conducted research, hope is a quantifiable quality which can be used in the stage of reviewing and understanding the nursing process. This stage can be followed by intervention to promote hope. Without the promotion of hope, grounds for the acceptance of treatment and care-education will not be established.[7] Experts from the World Health Organization (WHO), have defined mental health as the capability of having harmonious relationships with others, change and modification of individual and social environment, and the logical, fair, appropriate resolving of conflicts and personal desires.[8] They also believe that mental health is not merely the absence of mental illness, but it is the flexible and meaningful reaction against a variety of life experiences.[9] Today, mastectomy is the routine surgical treatment of breast cancer and its appearance as well as psychological and social consequences are not considered; thus, the repeated evaluation of mood and psychological aspects of patients are of higher importance.[10] On the other hand, it is certain that women are the most important pillars of the family and society. Thus, improving the psychological status of women not only improves their survival, but also the mental health of their family and results in more consistency of family structure.[11] Therefore, the present study aimed to identify the relationship between body esteem, hope, and mental health in patients with breast cancer after mastectomy.
MATERIALS AND METHODS
This was a descriptive cross-sectional study aimed to investigate the relationship between body esteem, hope, and mental health in breast cancer patients after mastectomy. The study population included 100 breast cancer patients who had undergone mastectomy and referred to Sayed Al-Shohada Medical Center in Isfahan, Iran. The subjects were selected using convenient sampling. The data gathering tools included the Body Esteem Scale (BES), Herth Hope Index (HHI), and Symptom Checklist 25 (SCL-25) mental health questionnaire. The valuing body questionnaire was used for the first time by Ghoudusi et al. In their study, to determine the reliability of this instrument, the internal reliability method was used. Moreover, using Cronbach's alpha coefficient, the reliability coefficient was estimated at 0.80. This questionnaire included 13 general terms and was scored based on a 5-point Likert scale (totally agree (1), agree (2), no comment (3), disagree (4), and totally disagree (5)). This instrument assessed four subscales that include: (1) physical attractiveness (questions 1 and 9); (2) feeling comfortable about your body (with questions 3, 7, and 13); (3) comparing your body with a healthy body (questions 2, 5, 6, 10, and 12); and (4) sexual attraction based on one's own and others’ opinion (questions 4, 8, and 11). The mean and standard deviation (SD) was calculated for each of the questions separately, and for the total of the questions for each subscale. Valuing the desired body was measured based on the body esteem score of each item, the total score of body esteem, and the overall mean of body esteem. The overall mean score ranged between 13-65; total mean closer to 65 showed higher body esteem, and lower and closer to 13 showed lower body esteem. In this questionnaire, question 3 had reverse score. It should be noted that the questionnaire is designed so that single people can also respond to the questions.[12] The HHI contained 12 items and was based on a 3-point Likert scale, graded from 1-3 (1) disagree, (2) not sure, and (3) agree). The negative items were scored inversely in this questionnaire. Total score ranged from 12-36 and higher scores indicated higher level of hope.[13] The SCL-25 (the short form of SCL25-R) was used to measure the mental health of the patients. The SCL25-R scale had nine dimensions of somatization, obsessive-compulsive, interpersonal sensitivity, depression, anxiety, phobic anxiety, psychosis, paranoid ideation, aggression, and a few additional questions. This scale consisted of 25 items, and each item was assessed based on a 5-point Likert scale; none (0), low (1), somewhat (2), high (3), and intensity (4). The score of this questionnaire ranged from 0-100. Lower scores indicated better mental health and scores above 65 indicated psychological disorders.[14] In the present study, the reliability of the questionnaire was assessed using Cronbach's alpha. The researcher referred to the study environment and distributed the questionnaires among 30 patients. After collecting the questionnaires, using SPSS for Windows (version 16; SPSS Inc., Chicago, IL, USA), Cronbach's alpha coefficients of the BES was calculated as 0.85, the HHI as 0.90, and SCL-25 as 0.92. Characteristics of the study population include: Patients who referred to the hospital to receive health care or medical advice; at least 6 months had past their one-sided mastectomy; they had no other physical or mental illness; the patient was able to respond to the questions; patient was not undergoing chemotherapy; the mastectomy could not be reconstructed; and all the subjects were over 30 years of age. After selecting the eligible subjects, the researcher introduced himself to them, and explained the purpose of the study. After obtaining an informed consent from each participant and assuring them that their information will be kept confidential, the questionnaires were handed to them. It should be mentioned that the researcher personally read the questions for the participants and recorded their responses without any manipulation. The sampling was continued until the completion of the required number and lasted for 3 months. Data analysis was performed using SPSS software. Descriptive statistical methods were used to adjust the tables.
RESULTS
Based on the results of this study, the highest frequency (52%) was in the age group of 50-70 year olds. Moreover, 7% of the subjects were single and 71% were married. The majority of patients (32%) were high school graduates, 33% of them had a history of abortion, and 17% had the experience of cancer in other organs. Additional information about the status of the subjects is shown in [Table 1]. The results indicated that with respect to the BES (2.80) and its overall mean score (36.46), patients had low body esteem. According to the findings, the highest mean (65.2) in the subscales of body esteem was related to physical attractiveness and the lowest mean (51.73) was related to comparing the body with a healthy body. The phrases “if someone told me I am an attractive person, I would doubt it” and “if I did not have this disability, I would be better looking”, respectively, had the highest (3.23) and lowest (2.41) body esteem scores. Based on the results obtained in this study, 27% of the patients had low hope, 49% had moderate hope, and 24% high levels of hope [Table 2]. Furthermore, based on the overall score of mental health, 69 patients were suspected to have mental disorder. In addition, regarding the nine dimensions of mental health, the highest mean (3.05) was associated with depressive disorders in the study units [Table 3]. In this study, according to the results of the Spearman correlation coefficient, there was a direct linear relationship between appreciating the body, hope, and mental health. This relationship was stronger between body esteem and hope (P < 0.001, rs = 0.583) [Table 4].
Table 1.
Demographic distribution of the study subjects
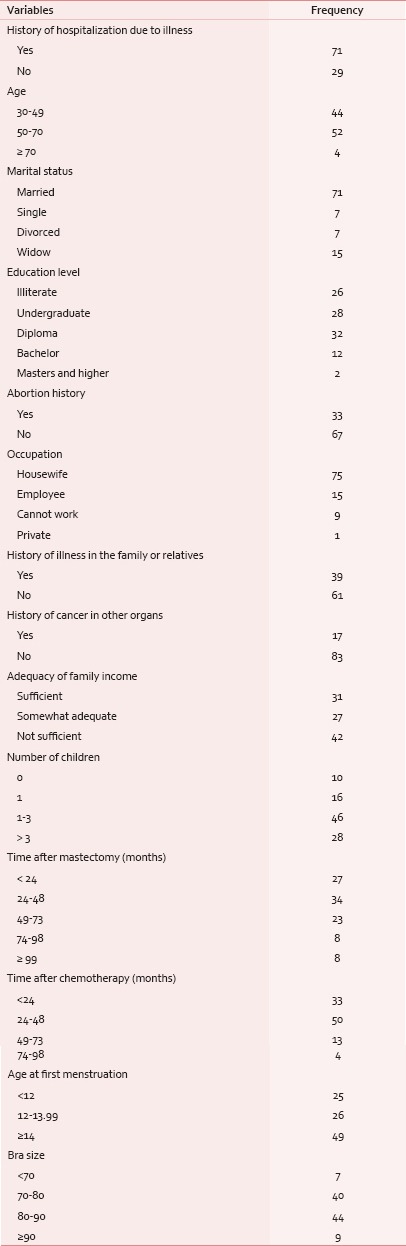
Table 2.
Frequency distribution of hope among the study subjects
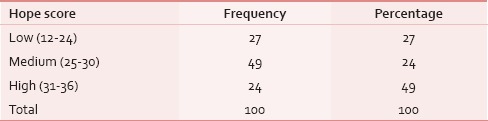
Table 3.
Mean and standard deviation of the mental health subscale of study subjects
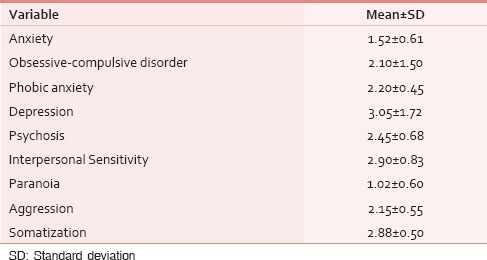
Table 4.
Relationship between body esteem and hope, body esteem and mental health, and hope and mental health
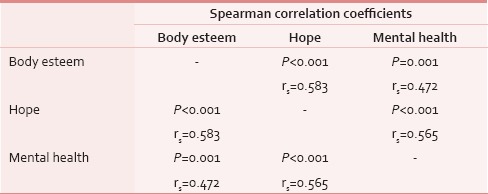
The results of this study showed that patients had low body esteem. Based on the results, the BES was 2.80 ± 1.14. body esteem in people with chronic diseases, such as breast cancer, can be interpreted as a psychological understanding. Negative social attitudes and their internalization will affect the value of the body in women with breast cancer. If people have bad judgment about the value of their own body, they will have a negative and destructive understanding about their body and its different aspects. Feeling of body esteem is the result of the value created in one's mind due to that which one hears, observes, and feels.[15] Seynaeve and Den Heijer, and Pinto and Trunzo also confirm these findings in their studies. Based on their findings, breast cancer and mastectomy have a negative effect on body esteem.[8,9,10,11,12,13,14,15,16] Fallbjork et al., argue that society places high value on physical attractiveness and can affect individuals’ opinions about their body; therefore, one can have negative assumptions towards their body based on their society's beliefs. This is how patients come to the conclusion that if they did not have this disability they would be seen as more attractive.[17] However, the results of the study by Ghoudosi et al., on the relationship between body esteem in people with multiple sclerosis was inconsistent with these results.[12] People with disabilities or limitations have more difficulty in adaptation to different situations than people without disabilities. Disabled people do not have difficulties in adapting but it is the environment that is not conducive to allow for this and one of the most effective methods of improving their adaptation to their physical and mental limitations is to help them gain hope.[13] The results of this study showed that only 24% of the patients had high levels of optimism and hope; however, most of them had moderate levels of hope. In this regard, Aydine Avci and Okanli, in their study on reviewing the judgments of marriage and hopelessness levels after mastectomy, reported low levels of hope in patients.[4] The results of this study confirmed the findings of the study by Hagerty et al., on the relationship between hope and realism in patients with breast cancer.[18] In this study, it is important to note that 27% of the patients had low levels of hope, and researchers believed that the first patients lost hope and then became depressed. Disappointments had negative effects on the health and psychological aspects of patients, and were risk factors for the impairment of these dimensions. Therefore, it is necessary to increase patients’ hope, because hope is the most valuable resource that patients can rely on for immunity to any mental and physical damage.[7] Other findings of this study, regarding the mental health of these patients, showed that based on the nine dimensions of mental health most patients had depression (1.63 ± 0.72). It appears that mastectomy not only affects physical functioning, but it also has a negative impact on emotional, psychological, and social functions. Many of the problems in patients with breast cancer due to mastectomy and its impacts on their quality of life occur after surgery. Because patients after mastectomy experience circumstances similar to that of an amputation; an organ the amputation of which causes women great stress, changes their attitude towards their body after surgery, and renders them prone to mood disorders.[19] Study results of Fallbjork et al., and Isern and Tengrup also confirm these findings.[17,18,19] Results of Spearman correlation coefficients showed that there was a direct linear relationship between body esteem, hope, and mental health, and the intensity of this relationship was greater between body esteem and hope (P < 0.001, rs = 0.583). The results of the present study confirmed the findings of the study by Fallbjork et al., on the dimensions of mental image and mental health of women with breast cancer after mastectomy.[17] Mickley et al., in a study on mental health and hope in women with breast cancer showed a significant relationship between the mentioned variables.[7] The study by Unukovych et al., on health-related quality of life, gender assessment, and mental image of the body in women after mastectomy showed consistent results with the present study.[20] After mastectomy patients have negative valuation of their body. Because they believe that with this type of treatment, their physical appearance and function will change to the extent that they do not believe in their body.[21] Knowing the physical value of the body has great impacts on the meaning of being hopeful and mental health of the person.[22] Hope is a symbol of mental health and the ability to believe in a more positive feeling in the future. Nevertheless, hopelessness is the opposite of hope and the main characteristic and manifestation of depression. Researchers believe that an individual is first hopeless and then becomes depressed. Hopelessness has negative impact on the health and psychological aspects of a person and is a risk factor for impairment of these dimensions.[23]
CONCLUSION
The impacts of mastectomy on body esteem, other psychological aspects, and in general the mental health is undeniable. Thus, providing the above results can be useful for health care organizations and women's health planners and managers who can implement them in the health system planning. It is also necessary that the treatment team assess the psychological dimensions of their patients. Meanwhile, there is an emphasis on the role of nurses, because nurses play an important role in the care of cancer patients after mastectomy and have a suitable situation to educate the patients and their families and provide emotional support.
ACKNOWLEDGEMENT
This study was related to research project number 1422 approved by the research and technology deputy of Shahrekord University of Medical Sciences, Iran. Our appreciation goes to the deputy of research and technology of Shahrekord University of Medical Sciences, all the officials of Sayed Al-Shohada Medical Center in Isfahan, and all the patients who participated in this study.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
REFERENCES
- 1.Esmaili R, Saiidi JA, Majd HA, Esmaieli M. A survey of the body image of mastectomies women referring to imam khomeini and imam hussein hospitals in Tehran, Iran. Indian J Psychol Med. 2010;32:34–7. doi: 10.4103/0253-7176.70528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Li Q, Gao EL, Yang YL, Hu HY, Hu XQ. Traumatic neuroma in a patient with breast cancer after mastectomy: A case report and review of the literature. World J Surg Oncol. 2012;10:35. doi: 10.1186/1477-7819-10-35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Laronga C, Lewis JD, Smith PD. The Changing face of mastectomy: An oncologic and cosmetic perspective. Cancer Control. 2012;19:286–94. doi: 10.1177/107327481201900405. [DOI] [PubMed] [Google Scholar]
- 4.Avci IA, Okanli A, Karabulutlu E, Bilgili N. Women's marital adjustment and hopelessness levels after mastectomy. Eur J Oncol Nurs. 2009;13:299–303. doi: 10.1016/j.ejon.2009.03.011. [DOI] [PubMed] [Google Scholar]
- 5.van den Berg P, Paxton SJ, Keery H, Wall M, Guo J, Neumark-Sztainer D. Body dissatisfaction and body comparison with media images in males and females. Body Image. 2007;4:257–68. doi: 10.1016/j.bodyim.2007.04.003. [DOI] [PubMed] [Google Scholar]
- 6.Yildirim Y, Sertoz OO, Uyar M, Fadiloglu C, Uslu R. Hopelessness in Turkishcancer inpatients: The relation of pain and Hopelessness in patients with canser. Eur J Oncol Nurs. 2009;13:81–6. doi: 10.1016/j.ejon.2009.01.001. [DOI] [PubMed] [Google Scholar]
- 7.Mickley J, Soeken K, Belcher A. Spiritual well-being, religiousness and hope among women with breast cancer. Image J Nurs Sch. 1992;24:267–72. doi: 10.1111/j.1547-5069.1992.tb00732.x. [DOI] [PubMed] [Google Scholar]
- 8.Den Heijer M, Seynaeve C, Timman R, Duivenvoorden HJ, Vanheusden K, Tilanus-Linthorst M, et al. Body image and psychological distress after prophylactic mastectomy and breast reconstruction in genetically predisposed women: A prospective long-term follow-up study. Eur J Cancer. 2012;48:1263–8. doi: 10.1016/j.ejca.2011.10.020. [DOI] [PubMed] [Google Scholar]
- 9.Sharma MK, Chaturvedi SK. Pain in mental health setting and community: An exploration. Indian J Psychol Med. 2014;36:98–100. doi: 10.4103/0253-7176.127268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kash KM, Holland JC, Halper MS, Miller DG. Psychological distress and surveillance behaviours of women with a family history of breast cancer. J Natl Cancer Inst. 2013;84:24–30. doi: 10.1093/jnci/84.1.24. [DOI] [PubMed] [Google Scholar]
- 11.Mullan MH, Wilkins EG, Goldfarb S, Lowery JC, Smith DM, Wickman M, et al. Prospective analysis of psychosocial outcomes after breast reconstruction: Cross-cultural comparisons of 1-year postoperative results. J Plast Reconstr Aesthet Surg. 2007;60:503–8. doi: 10.1016/j.bjps.2005.10.033. [DOI] [PubMed] [Google Scholar]
- 12.Ghodusi M, Heidari M. Evaluation body esteems and related factors in patients with Multiple Sclerosis. J Res Behave Sci. 2013;11:1–13. [Google Scholar]
- 13.Benzein EG, Berg AC. The level of and relation between hope, hopelessness and fatigue in patients and family members in palliative care. Palliat Med. 2005;19:234–40. doi: 10.1191/0269216305pm1003oa. [DOI] [PubMed] [Google Scholar]
- 14.Najarian B, Davoodi I. Making Validation Scl25, Short form Scl90. J Psychol. 2001;2:136–49. [Google Scholar]
- 15.Seal BN, Bradford A, Meston CM. The association between body esteem and sexual desire among college women. Arch Sex Behav. 2009;38:866–72. doi: 10.1007/s10508-008-9467-1. [DOI] [PubMed] [Google Scholar]
- 16.Pinto BM, Trunzo JJ. Body esteem and mood among sedentary and active breast cancer survivors. Mayo Clin Proc. 2004;79:181–6. doi: 10.4065/79.2.181. [DOI] [PubMed] [Google Scholar]
- 17.Fallbjork U, Rasmussen BH, Karlsson S, Salander P. Aspects of body image after mastectomy due to breast cancer-a two-year follow-up study. Eur J Oncol Nurs. 2013;17:340–5. doi: 10.1016/j.ejon.2012.09.002. [DOI] [PubMed] [Google Scholar]
- 18.Hagerty RG, Butow PN, Ellis PM, Lobb EA, Pendlebury SC, Leighl N, et al. Communicating with realism and hope: Incurable cancer patients’ views on the disclosure of prognosis. J Clin Oncol. 2005;23:1278–88. doi: 10.1200/JCO.2005.11.138. [DOI] [PubMed] [Google Scholar]
- 19.Isern AF, Tengrup I, Loman N, Olsson H, Ringberg A. Aesthetic outcome, patient satisfaction, and health-related quality of life in women at high risk undergoing prophylactic mastectomy and immediate breast reconstruction. J Plast Reconstr Aesthet Surg. 2008;61:1177–87. doi: 10.1016/j.bjps.2007.08.006. [DOI] [PubMed] [Google Scholar]
- 20.Unukovych D, Sandelin K, Liljegren A, Arver B, Wickman M, Johansson, et al. Contralateral prophylactic mastectomy in breast cancer patients with a family history: A prospective 2-years follow-up studyof health related quality of life, sexuality and body image. Eur J Cancer. 2012;48:3150–6. doi: 10.1016/j.ejca.2012.04.023. [DOI] [PubMed] [Google Scholar]
- 21.Park HS, Cho GY, Park KY. The effect of rehabilitation program of physical health, psychological indicator and quality of life in breast cancer mastectomy patient. Taehan Kanho Hakhoe Chi. 2006;36:310–20. doi: 10.4040/jkan.2006.36.2.310. [DOI] [PubMed] [Google Scholar]
- 22.Taleghani F, Yekta ZP, Nasrabadi AN. Coping with breast canser in newly diagnosed Iranian women. J Adv Nurs. 2006;54:265–72. doi: 10.1111/j.1365-2648.2006.03808_1.x. [DOI] [PubMed] [Google Scholar]
- 23.Sahu A, Gupta P, Chatterjee B. Depression is more than just sadness: A case ofexcessive anger and its management in depression. Indian J Psychol Med. 2014;36:77–9. doi: 10.4103/0253-7176.127259. [DOI] [PMC free article] [PubMed] [Google Scholar]


