Summary
The objective of this study was to evaluate the incidence, types and severity of burn injuries, including sites involved, morbidities, operative procedures, and their outcomes, to prevent or reduce the frequency and morbidity of such injuries in epileptic patients. This retrospective study was conducted at our centre between February 2008 and January 2012. The study included 54 patients who sustained burn injuries due to epileptic seizures, accounting for 1.3% of all burn admissions. All patients, irrespective of the severity of their injuries, were admitted to our centre, assessed, treated and educated regarding specific preventive measures. All study data were evaluated from patient medical records. Causes of burn injury were as follows: scald burns (30), contact with hot surfaces (12), electrical burns in the bathroom (6), and flame burns (6). Second degree burns were the most common (18 out of 54 patients) and third degree burns were the least common. Upper limb and trunk were the most common sites involved (36 out of 54 patients). Thirty patients required surgical intervention whereas the remainder was conservatively managed. Most of the injuries occurred in the age group between 30-37 years. Injuries occurred predominantly in females [42 females, 12 males; F:M=3.5:1]. The study revealed that patients with epilepsy should be categorized as a high risk group considering the sudden and unpredictable attack of epileptic seizures leading to loss of consciousness and accidental burn injuries. Early surgical intervention and targeting of all epileptic patients for education and instituting the specific preventive measures gives good outcomes.
Keywords: burn injury, epilepsy, preventive measures
Abstract
L’objectif de cette étude était d’évaluer l’incidence, le type et la gravité des brûlures, y compris les organes impliqués, les morbidités, les chirurgies, et les résultats des chirurgies, et de prévenir ou de réduire la fréquence et la morbidité de ces blessures chez les patients épileptiques. Cette étude rétrospective a été menée dans notre centre entre Février 2008 et Janvier 2012. L’étude a inclus 54 patients ayant subi des brûlures dues à des crises d’épilepsie, ce qui représente 1,3% de toutes les admissions pour brûlures. Tous les patients, quelle que soit la gravité de leurs blessures, ont été admis dans notre centre, évalués, traités et éduqués sur les mesures de prévention spécifiques. Toutes les données de l’étude ont été évaluées à partir des dossiers médicaux des patients. Les causes de brûlure ont été les suivants : de l’eau chaud (30), le contact avec des surfaces chaudes (12), les brûlures électriques dans la salle de bain (6), et les brûlures causées par la flamme (6). Les brûlures au deuxième degré étaient les plus courantes (18 patients sur 54) et les brûlures au troisième degré étaient les moins fréquentes. Le membre supérieur et le tronc étaient les sites les plus fréquemment impliqués (36 sur 54 patients). Trente patients ont nécessité une intervention chirurgicale tandis que le reste a été géré avec prudence. La plupart des blessures sont survenues dans le groupe d’âge entre 30-37 ans. Blessures sont survenues principalement chez les femmes [42 femmes, 12 hommes ; F : M = 3,5 : 1]. L’étude a révélé que les patients souffrant d’épilepsie devraient être classés comme un groupe à risque élevé compte tenu de l’attaque soudaine et imprévisible des crises d’épilepsie conduisant à la perte de conscience et des brûlures accidentelles. Les meilleurs résultats sont obtenus avec une intervention chirurgicale précoce dans certains groupes de patients, ainsi que par le ciblage de tous les patients épileptiques pour l’enseignement des mesures préventives spécifiques.
Introduction
Epileptic patients are usually encouraged to live a normal life, as much as possible. The incidence and nature of the various kinds of injuries in epileptic patients are different from those that occur in people who do not have epilepsy. The risk associated with this is an important factor in managing such patients.1 Some epileptic patients pose a threat to themselves and others during the peri-ictal period. 2,3 The attack of epilepsy comes without any warning signs, leading to loss of consciousness and convulsions. Therefore the relationship between epilepsy and burn injury is obvious, especially if the attack takes place in the vicinity of burn agents. It is important to identify this high risk group of patients and provide them with specific treatment, along side the institution of targeted preventive measures. Such burn patients must be treated in collaboration with a neurologist to provide targeted antiepileptic treatment and prevention strategies.
In this series, we have studied 54 epileptic patients who sustained burn injuries. The type of burn injury sustained, burn severity, site involved, morbidities, operative procedures conducted, overall outcomes and measures to prevent or reduce the frequency and morbidity of such injuries in epileptic patients were evaluated.
Materials and methods
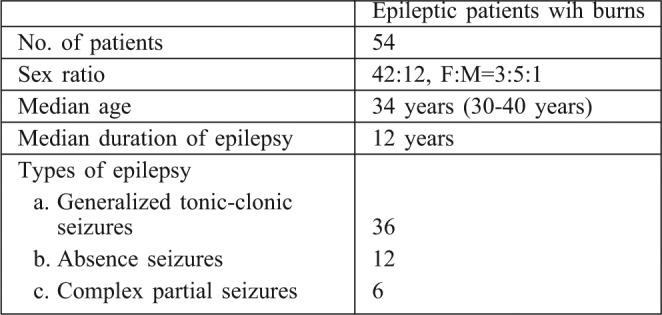
This retrospective study was conducted at the authors’ centre between February 2008 and January 2012. This study included 54 patients who sustained burn injuries due to epileptic seizures, accounting for 1.3% of total burn admissions. All patients, irrespective of the severity of their injuries, were admitted to our centre, assessed and then provided with treatment. All of the patients were taken to a physician for consultation on the treatment of epilepsy. Type, total body surface area (TBSA), severity and morbidities of burn injuries, operative procedures performed and their outcomes were evaluated from the patient medical records. Thirty six patients were diagnosed as a case of generalized tonic-clonic seizure, 12 patients as absence seizures and 6 as complex partial seizures. The median duration of epilepsy was 12 years (Table I).
Table I. Patient profile.
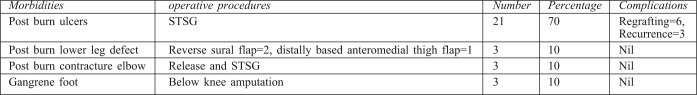
Early surgical intervention was considered in all the operative cases. Eighteen patients with second degree deep burns required split thickness skin graft (STSG) and 3 developed contracture of the elbow (2 right and 1 left) that required release and STSG (Table V). Three patients with third degree burns required STSG and another three required flap cover. Out of the 3 flaps, 2 were reverse sural flaps for coverage of a distal leg defect and 1 was a distally pedicled anteromedial thigh flap for the infrapaterllar region. Three patients with third degree burns developed gangrene of the right foot requiring below knee amputation (Table V). The TBSA involved for the first degree burns was less than 5 % in all the patients, and wounds healed within a week.
Table V. Morbidities, operative procedures and complications.
Results
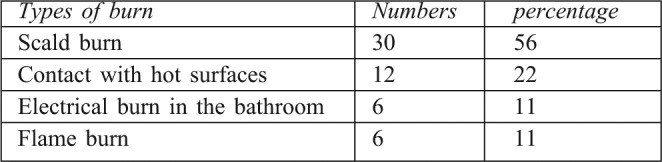
Injuries resulted from scald burns (30), contact with hot surfaces (12), electrical burns in the bathroom (6) and flame burns (6) (Table II). Eighty-seven percent (47 out of 54) of injuries took place at home and 13% (7 out of 54) at work. All of the patients with scald burns sustained injury at home: 22 in the kitchen due to hot liquids from cooking and 8 in the bathroom due hot tap water. Most of the patients (46 out of 54; 85%) had a TBSA involvement of less than 20% and only 15% had more than 20%.
Table II. Types of burn.
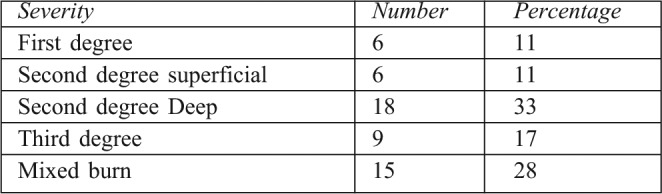
Eighteen patients developed second degree deep burns, there were 6 second degree superficial burns, 6 first degree burns, 9 third degree burns, and 15 patients sustained mixed burn injuries, including first and second degree (Table III). Eighteen patients sustained burn injuries involving the upper limb, 15 involving the trunk, 3 involving both the upper limb and trunk, 6 involving the face and neck, 6 involving both the trunk and the right lower limb, and 6 involving exclusively the lower limb (Table IV). All of the first degree burn injuries healed within 1 week, the second degree superficial burns healed within 2 weeks, the second degree deep burns required 3 weeks to heal, with the exception of the 3 which required split thickness grafting (STSG). Most of the injuries occurred in the age group between 30-37 years. Injuries occurred predominantly in females (42 females, 12 males; F:M =3.5:1). As regards the STSG, there was a 100% take up recorded in approximately 70% of the patients on post operative day 4. Six patients were partially regrafted and 3 experienced ulcer recurrence in the following 6 months. The most common sites involved were the trunk and upper limb.
Table III. Severity of burn injuries.
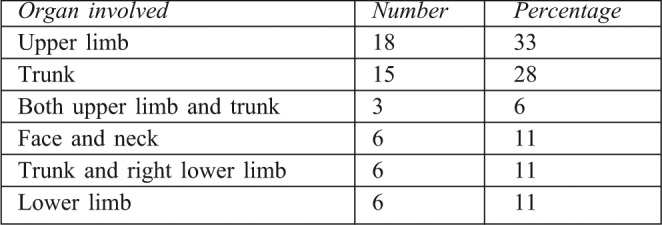
Table IV. Sites involved.
Discussion
Epileptic patients may sustain dramatic burn injuries during the acute episodes. Burn injuries received during acute seizures have been reported by various authors in association with cerebral cysticercosis4 and in subjects wearing grass skirts.5 These patients must be identified, provided with specific treatment, and educated to prevent an unpredictable attack that may lead to burn injuries. Due to a lack of orientation to time, place and person during the attack, such burn injuries can be deeper and may lead to more difficult management and subsequently to higher costs, increased morbidity, and even mortality. Severe burns as a result of epileptic seizures that require surgical interventions are well described by those who treat such patients,6-8 and these are usually deep burns.9 These studies correspond to our study showing deep burns in 42 out of 54 patients (77%) as compared to burn injuries in nonepileptic patients, where this percentage would be lower. In our series, this could be due to the majority of patients coming from rural areas and having a poor socioeconomic status, coupled with illiteracy and a longer contact time with the agent during the attack. In contrast, Buck et al.10 found that 16% of the epileptic patients studied sustained burn injuries during a seizure at some stage, but only 1% of these patients required admission, and only 0.3% required operative interventions. Josty et al.2 retrospectively reviewed 111 patients admitted with burn injuries, secondary to an epileptic seizure. They concluded that scald injuries are the major cause of burns in epileptic patients. In our study, 55% (30 out of 54) of epileptic patients sustained scald burns. All of them sustained their injuries at home: 22 due to hot cooking liquids and 8 due to hot tap water in the bathroom. A deep burn involves more skin components, preventing the skin from early and scar-free healing. Operative interventions are required in deep dermal and full-thickness burns to accelerate healing and reduce scarring. This can be achieved by burn excision and split-thickness skin grafting in most of cases.2
In our series, all of the patients with deep burn required operative interventions in the form of skin grafts, local flaps and below knee amputation. Adigun et al.11 studied “Amputation from Burn following Epileptic Seizure’’ in their burn unit. A total of 250 patients were managed during the 5 year study period. Two patients (0.8%) fulfilled the criteria for inclusion and the extent of injury was quite severe: one patient required disarticulation of a gangrenous left hand at the wrist joint and disarticulation of gangrene of the right 3rd, 4th and 5th toes at the metatarsophalangeal joint, the other patient required disarticulation of the gangrenous fingers of the left hand at the metacarpophalangeal joints. We performed below knee amputation in 3 patients who sustained electric burns over the right foot and presented late leading to gangrene of the foot.
In the study by Adigun et al.11 study, both of the epileptic patients who sustained burn injuries while cooking in the kitchen were female. This coincides with the findings of Meirelles et al.,12 who noticed that a large number of patients had visual contact with the flame prior to the accident, suggesting that fire could be a photostimulator for the onset of seizure attack. We also noticed in our study that most of the patients were female and sustained injury while cooking in the kitchen. The greatest risk factors for the increased incidence of burns in epileptic patients are the frequency of seizure attack, the duration of the epileptic episode,13-15 and a lack of awareness and education about the risk of burns among epileptic patients.12 Napoli et al.16 reviewed the medical records of 14 patients whose burns occurred because of an epileptic seizure. They concluded that epileptic seizures are an important predisposing factor in burns; the burn agent emits light stimuli that trigger the onset of epileptic seizures and can affect the important areas including the face and hand. Tiamkao et al.17 concluded in their study that soft-tissue injury was the most common in epileptic patients followed by burns, head injury, orthopaedic injury, and seizure related events in water. It has also been found that epileptic patients can live a normal life but certain precautions are required to prevent seizure-related injury.18
It is important to identify a small group of epileptic patients who require repeated admission. One of the major problems in epileptic patients is their noncompliance19 and patient medication should be regularly monitored as per the advice from physicians. All of the patients in our series were under treatment by consultation from the neurology unit of the department of medicine. Burn injury in epileptic patients can be prevented by taking simple measures including the use of fire and radiator guards14,20,21 flame-retardant clothing,20,21 and following advice about showering.22 In the kitchen, the incidence of burn injuries can be prevented by use of microwave ovens,14 self-sealing deep-fat fryers, insulated plastic kettles, and cooker guards.14
All of the patients in our series were educated regarding the above mentioned preventive measures, and were taking their medications regularly, adjusting them in accordance with the neurophysician’s consultation and lifestyle changes to avoid further contact with the burning agents.
Various authors report the incidence of burn injury in epileptic patients accounting for 5%21 and 10%9 of total admissions to a burn unit.
Compared to the studies conducted by Bull et al. (5%) and Meirelles et al. (10%), our study reveals a tendency toward a lower percentage of burn injury in epileptic patients in our centre despite the rural catchment area (1.3%). Possible factors influencing this trend could be the increase in education of a selected group of patients by various epileptic organizations, and a shift towards the scald burn from the previously reported thermal burn.
Conclusion
The study revealed that patients with epilepsy should be categorized as a ‘high risk group’ in view of the sudden and unpredictable attack of epileptic seizures, which lead to loss of consciousness and accidental burn injuries. Had these patients been identified as belonging to a high risk group, the majority of them could have been saved from burn injuries. As well as having to undergo burn care management, these patients will have early and late morbidities. Although, superficial burn injuries can be managed by conservative means, deeper burn injuries require surgical interventions. The best outcomes are achieved through early surgical intervention in selected groups of patients, as well as through targeting all epileptic patients for education and instituting specific preventive measures.
Acknowledgments
Confict of interest. None.
References
- 1.Neufeld MY, Vishne T, Chistik V, Korezyn AD. Life-long history of injuries related to seizures. Epilepsy Res. 1999;34:123–7. doi: 10.1016/s0920-1211(98)00105-3. [DOI] [PubMed] [Google Scholar]
- 2.Josty IC, Narayanan V, Dickson WA. Burns in patients with epilepsy: Changes in epidemiology and implications for burn treatment and prevention. Epilepsia. 2000;41:453–6. doi: 10.1111/j.1528-1157.2000.tb00188.x. [DOI] [PubMed] [Google Scholar]
- 3.Spitz MC. Severe burns as a consequence of seizures in patients with epilepsy. Epilepsia. 1992;33:103–7. doi: 10.1111/j.1528-1157.1992.tb02290.x. [DOI] [PubMed] [Google Scholar]
- 4.Subianto DB, Tumada LR, Margono SS. Burns and epileptic fits associated with cysticercosis in mountain people of Irian Jaya. Trop Geogr Med. 1978;30:275–7. [PubMed] [Google Scholar]
- 5.Barss P, Wallace K. Grass-skirt burns in Papua New Guinea. Lancet. 1983;321:733–4. doi: 10.1016/s0140-6736(83)92026-3. [DOI] [PubMed] [Google Scholar]
- 6.Durward WF, Harrington MG. Burning and the inadequate management of epilepsy. Br Med J. 1979;2:12–18. doi: 10.1136/bmj.2.6199.1218-b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.De Castro AB, Zegri IV, Galvez C del F. Burns and epilepsy. An analytical study. Cirugia Plastica Ibero-Latinomericana. 1978;4:307–14. [Google Scholar]
- 8.Bhatnagar SK, Srivastava JL, Gupta JL. Burns: A complication of epilepsy. Burns. 1977;3:93–5. [Google Scholar]
- 9.Maisels DO, Corps BVM. Burned epileptics. Lancet. 1964;1:1298–1301. doi: 10.1016/s0140-6736(64)91693-9. [DOI] [PubMed] [Google Scholar]
- 10.Buck D, Baker GA, Jacoby A, Smith DF, Chadwick DW. Patients’ experiences of injury as a result of epilepsy. Epilepsia. 1997;38:439–44. doi: 10.1111/j.1528-1157.1997.tb01733.x. [DOI] [PubMed] [Google Scholar]
- 11.Adigun IA, Ogundipe KO, Abiola OO, et al. Amputation from burn following epileptic seizure. Surgery Journal. 2008;3:78–81. [Google Scholar]
- 12.Meirelles RPC, Piccolo NP, Piccolo PP, et al. Epileptic burn patient’s profile: Prospective and retrospective study of epileptic patients admitted at pronto scorropara Oueimaduras, Goiania, Brazil. Burns. 2007;33:102–3. [Google Scholar]
- 13.Richards EH. Aspects of epilepsy and burns. Epilepsia. 1968;9:127–35. doi: 10.1111/j.1528-1157.1968.tb05134.x. [DOI] [PubMed] [Google Scholar]
- 14.Hampton KK, Peatfield RC, Pullar T, et al. Burns because of epilepsy. BMJ. 1988;296:1659–60. doi: 10.1136/bmj.296.6637.1659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Spitz MC, Towbin JA, Shantz D, et al. Risk factors for burns as a consequence of seizures in persons with epilepsy. Epilepsia. 1994;35:764–7. doi: 10.1111/j.1528-1157.1994.tb02508.x. [DOI] [PubMed] [Google Scholar]
- 16.Napoli B, D’Arpa N, Masellis M. Epilepsy and burns. Annals of the MBC. 1992;5:155–9. [Google Scholar]
- 17.Tiamkao S, Shorvon SD. Seizure-related injury in an adult tertiary epilepsy clinic. Hong Kong Med J. 2006;12:260–3. [PubMed] [Google Scholar]
- 18.Spitz MC. Injuries and death as a consequence of seizures in people with epilepsy. Epilepsia. 1998;39:904–7. doi: 10.1111/j.1528-1157.1998.tb01189.x. [DOI] [PubMed] [Google Scholar]
- 19.Buck D, Jacoby A, Baker GA, Chadwick DW. Factors influencing compliance with antiepileptic drug regimes. Seizure. 1997;6:87–93. doi: 10.1016/s1059-1311(97)80060-x. [DOI] [PubMed] [Google Scholar]
- 20.Tempest MN. A survey of domestic burns and scalds in Wales during 1955. Br Med J. 1955;1:1387–92. doi: 10.1136/bmj.1.4980.1387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bull JP, Jackson DM, Walton C. Causes and prevention of domestic burning accidents. Rr Med J. 1964;2:1421–7. doi: 10.1136/bmj.2.5422.1421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Livingston S, Pauli LL, Pruce I, Kramer II. Bathing instructions for patients with epilepsy. JAMA. 1981;245:702–3. [PubMed] [Google Scholar]


