Abstract
To examine whether hospital-based physical therapy is associated with functional changes and early hospital readmission among hospitalized older adults with community-acquired pneumonia and declining physical function. Study design was a retrospective observation study. Participants were community-dwelling older adults admitted to medicine floor for community-acquired pneumonia (n = 1,058). Their physical function using Katz activities of daily living (ADL) Index declined between hospital admission and 48 hours since hospital admission (Katz ADL Index 6→5). The intervention group was those receiving physical therapy for ≥ 0.5 hour/day. Outcomes were Katz ADL Index at hospital discharge and all-cause 30-day hospital readmission rate. The intervention and control groups did not differ in the Katz ADL Index at hospital discharge (p = 0.11). All-cause 30-day hospital readmission rate was lower in the intervention than in control groups (OR = 0.65, p = 0.02). Hospital-based physical therapy has the benefits toward reducing 30-day hospital readmission rate of acutely ill older adults with community-acquired pneumonia and declining physical function.
Keywords: hospitalization, patient outcome assessment, physical therapy, pneumonia
Functional decline in older adults is common and occurs in up to one-third of recently hospitalized older adults [1]. The hospital environment accelerates the reduction of functional reserve implicated factors include forced immobilization, disorientation due to unfamiliar hospital environments, and frequent orders not to eat by mouth [2-6]. In fact, hospitalized older adults spend more than 70% of their time lying in bed due to acute medical conditions, despite having the ability to walk [4].
Functional decline during or after hospitalization is associated with adverse health outcomes, prolonged hospital stays due to more frequent occurrences of hospital complications, such as delirium; and more frequent episodes of early hospital readmissions and even higher long-term mortality rate [7-12].
To reduce or delay functional decline during or after hospitalization, physical therapy (PT) has been utilized as an independent rehabilitation measure and a component of multidisciplinary care [14-16]. PT to restore functional reserve has been applied to certain acute illness, such as stroke and hip fracture, with excellent rehabilitation potential in both acute and post-acute hospital settings [13, 14]. There is evidence of dose-dependent effects of PT on functional recovery in a post-acute care setting [16, 17].
However, few studies have investigated the effects of PT on functional changes when applied to common acute medical illnesses aside from stroke and hip fracture [13, 14]. Other studies have evaluated the hospital outcomes of hospital-based PT when applied to pneumonia.
This study attempts to fill this gap by focusing on vulnerable older adults admitted for community-acquired pneumonia whose physical function declined between hospital admission and 48 hours since hospital admission to determine whether hospital-based PT is beneficial for this population in terms of physical and hospital-related outcomes.
MATERIALS AND METHODS
Study Subjects
The study site was a 350-bed metropolitan teaching hospital in the Ohio state of the United States. The present study was a retrospective observation study. The study period was 22 months (July 2007 to April 2009). Figure 1 presents the study participant selection strategy. Inclusion criteria were (1) community-dwelling adults age 65 or older; (2) admission to medicine floor with principal diagnosis of pneumonia (International Classification of Disease, Ninth Revision, Clinical Modification [ICD-9-CM]: 480.8, 480.9, 481, 482.0 - 487.0, 038.0 - 038.9, 518.81 or 518.84); (3) functional decline between hospital admission and 48 hours since hospital admission. Exclusion criteria were (1) hospital length of stay (LOS) of 2 days or less (n = 108), (b) healthcare-associated pneumonia [either from a residential facility or recent hospitalization in the last 14 days) (n = 92), (c) data missing during matching process (n = 77), or (d) deceased in hospital (n = 31). Functional decline was assessed using the Katz Activities of Daily Living (ADL) Index which is the most common measurement of activities of daily living functioning in hospitalized older medical patients [18]. A score of 0 represents total dependence and 6 represents total independence. Nursing staff completed the Katz ADL Index two times - at hospital admission and 48 hours since hospital admission. Functional decline was defined when participants score Katz ADL Index 6 at hospital admission (fully independent) and Katz ADL Index 5 at 48 hours since hospital admission (newly disabled).
Figure 1.
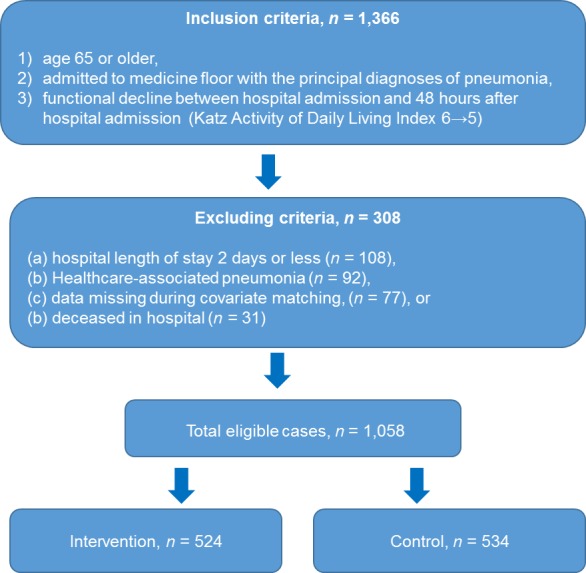
Selection strategy for study participants.
We estimated that a sample of 516 participants in each group was needed for each disease in order to detect a substantial change in the Katz Index (mean difference = 0.6; standard deviation = 1.4) with a power of 80% and significance level of 5% (two-tailed).
The final sample comprised 1,058 patients with pneumonia (524 and 534 in the intervention and control groups, respectively). The study was approved by the institutional review board at Cleveland Clinic Health System. The requirement for individual subject consent was waived because the study relied on existing administrative and clinical data.
Intervention vs. Control
We examined the LOS across all PT hours summed together. We added the total PT hours and divided the sum by the LOS. Patients did not need to receive all therapies to be included in these analyses. To compare our findings with those from previous studies on the relationship between therapy and outcomes, we defined patients receiving PT for ≥ 0.5 hours/day as the intervention group [17, 19]. The control group did not receive any PT during their hospital stay. Therapy staff was not aware of assignment of group assignment or study objective. Covariates between intervention and control groups were matched.
Table 1.
Subject characteristics by study groups
| Covariates | Intervention n = 524 |
Control n = 534 |
P | |
|---|---|---|---|---|
| Age, median (interquartile range) | 86.2 (79.1 - 93.7) | 85.3 (78.5 - 94.2) | 0.45 | |
| Female | 310, 59.2% | 327, 61.2% | 0.58 | |
| Non-Whites | 160, 30.5% | 165, 31.0% | 0.77 | |
| Education year, median (interquartile range) | 9.7 (7.7 - 10.8) | 10.1 (8.1 - 11.3) | 0.26 | |
| Severity of illness | Mild | 68, 12.9% | 85, 16.0% | 0.18 |
| Moderate | 130, 24.9% | 129, 24.1% | ||
| Major | 193, 36.9% | 186, 34.9% | ||
| Extreme | 133, 25.3% | 137, 25.0% | ||
| Cognitive impairment | 151, 28.8% | 161, 30.2% | 0.46 | |
| Charlson comorbidity index, median (interquartile range) | 3.45 (2.30 - 5.38) | 3.41 (2.24 - 5.49) | 0.63 | |
| Hospital length of stay (interquartile range) | 5.36 (4.31 - 6.79) | 5.59 (4.44 - 7.62) | 0.39 | |
Main Outcomes: Katz ADL Index at Hospital Discharge and All-cause 30-day Hospital Readmission Rate
The Katz ADL index was assessed again by the nursing staff at hospital discharge. Thirty-day readmission rate was captured from electronic medical record which could identify study participants’ hospital admission status throughout all local health systems. We defined hospital readmission when hospital readmission was unplanned with any cause within 30-day of hospital discharge.
Table 2.
Unadjusted Katz Activity of Daily Living Index at Hospital Discharge and All-cause 30-day Hospital Readmission Rate
| Outcomes | Intervention n = 524 |
Control n = 534 |
p |
|---|---|---|---|
| Katz Activities of daily living Index at hospital discharge | Mean (95% confidence intervals) | ||
| 4.89 (3.91 - 5.63) | 4.23 (3.65 - 5.30) | 0.07 | |
| All-cause 30-day hospital readmission rate | %, n | ||
| 11.2%, 59/524 | 16.3%, 87/534 | 0.03 | |
Covariates
Age, gender, ethnicity, education, severity of illness, cognitive impairment, the Charlson Comorbidity Index (CCI), and hospital length of stay were included as covariates. The All Patient Refined Diagnostic Related Group (APR-DRG) classification system was used to estimate the severity of illness. APR-DRG has been widely used for assessing severity of illness and reimbursement for hospital care. APR-DRG data were gathered from the department of operation, which was unaware of the study, based on the 3M Health Information System. CCI has been validated to reflect the magnitude of comorbidities in acute hospital settings [20]. Cognitive impairment was determined using the Mini-Cog assessment which has been validated elsewhere [21]. Hospital nursing staff performed the Mini-Cog assessment at 48 hours since hospital admission
Statistical Analysis
Bivariate comparisons of covariates between intervention and control subjects were examined using chi-square tests (categorical data) and either the t-test or Mann-Whitney U test (continuous data), as appropriate. All reported p-values were two-tailed and p < 0.05 was considered statistically significant.
We analyzed the outcomes as follows: We measured unadjusted outcomes by study groups. We used generalized linear models (GLM) with a log link function and gamma distribution to fit the skewed Katz ADL Index [22] and used the multivariate regressions to compute parameter estimates and p-values. Multivariate logistic regressions of all-cause 30-day hospital readmission rate were performed to compute estimates, odds ratios, p-values. SAS version 9.3 (SAS Institute Inc., Cary, NC, USA) was used for all analyses.
RESULTS
Table 3.
Multivariate Regressions of Katz Activity of Daily Living Index at Hospital Discharge
| Covariates | Parameter estimates | p | |
|---|---|---|---|
| Age | Reference = 65 - 74 | ||
| 75 - 84 | - 0.27 | 0.33 | |
| ≥ 85 | - 1.18 | 0.01 | |
| Gender | Reference = Male | ||
| Female | 0.36 | 0.21 | |
| Ethnicity | Reference = Whites | ||
| Non-Whites | - 0.40 | 0.19 | |
| Education | Reference = < High school graduate | ||
| ≥ High school graduate | 0.08 | 0.74 | |
| Severity of illness | Reference = Mild | ||
| Moderate | 0.15 | 0.62 | |
| Major | - 1.16 | 0.07 | |
| Extreme | - 2.08 | < 0.001 | |
| Cognitive impairment | Reference = No | ||
| Yes | - 1.43 | 0.003 | |
| Charlson comorbidity index | Reference = 0 -1 | ||
| 2 - 3 | - 0.94 | 0.058 | |
| ≥ 4 | - 3.15 | < 0.001 | |
| Study groups | Reference = Control | ||
| Intervention | 0.62 | 0.11 | |
DISCUSSION
We examined whether physical therapy for hospitalized older adults is associated with functional changes and early hospital readmission rate. To the best of our knowledge, this study is the first to focus on vulnerable older adults with pneumonia and declining function. Hospital-based PT was associated with reductions in early hospital readmission rate.
Although several previous studies have confirmed functional responses to hospital-based PT [13-15, 19], these were limited to stroke and hip fracture patients. Our study contributes to the literature by providing evidence that PT reduces progressive functional decline, even in common acute illness (pneumonia). The progression of functional decline during or after hospitalization is subject to “traction effects” because there are multiple contributing factors that are difficult to disentangle [23]. Home-based PT plays the role of a “buffer or breaker pedal” to counter these traction effects among acutely ill older adults [19].
Additional effects of hospital-based PT might include “delayed and spillover effects.” Hospital-based PT reduces vulnerability to other episodes of acute illnesses, and consequently reduces the early hospital readmission rate. Bodilsen et al. reported that functional performance in older adults was more vulnerable to decline than muscle strength during hospital stay and during post-discharge recovery [24]. This implies that the effects of hospital-based PT may persist and stabilize functional changes during and after hospitalization. However, this effect should be examined directly in the future by measuring the relationship between hospital-based PT and indicators of functional reserve.
Our findings have several theoretical and practical implications. Increased utilization of hospital-based PT may have system-wide benefits for hospitals. Medicare launched a performance-based payment system for certain medical conditions (heart failure, pneumonia, and acute myocardial infarction) in 2013. Thirty-day hospital readmission, also known as the “revolving door phenomenon,” is one of the core performance indicators linked to hospital reimbursement from Medicare [25]. Reduction of 30-day hospital readmission rates would improve performance indicators, and thus also improve the financial status of hospitals. However, certain precautions should be carefully considered prior to the application of PT. PT for subjects with major cardiovascular diseases, such as acute myocardial infarction, might not be practical, even with a fair restoration potential [9, 19, 24]. The little or no functional benefits of hospital-based PT could be explained by premature length of hospital-based PT. The length of exposure to hospital-based PT could be too short to present the functional benefits by hospital-based PT. Important next steps will be to determine how to optimize the PT outcomes such as extension to home-based PT after hospital discharge and dose-response relationship between the intensity of PT and functional outcomes.
Despite the above contributions, this study has several limitations. First, inter-observer bias might have occurred. Physical function was assessed by different nursing staff (hospital and home health care staff). Second, we matched covariates between the intervention and control groups by using two different data sources (hospital administration and clinical data). Missing data during the matching process was a noteworthy issue (5.6%, 77/1,366). Third, the relatively (not statistically) higher ADL score in the intervention group compared to the control group could be selection bias. Our data were not able to capture premorbid (baseline) ADL score. Physicians tend to refer patients with better functional status for PT services than those with poorer function status. Finally, we were able to capture service time of PT, but unable to capture the specific therapy modality (i.e., gait/bed transfer and muscle strengthening). Thus, the relationship between specific therapy modalities and either hospital or discharge outcomes was not examined. However, we believe that omitting this is not problematic as Jette et al. observed that there was no clear pattern in rehabilitation therapy for patients receiving acute care in hospitals and that the ultimate goal of rehabilitation was on functional recovery [26].
Table 4.
Multivariate Logistic Regressions of All-cause 30-day Hospital Readmission Rate
| Covariates | Estimates | Odds ratio | p | |
|---|---|---|---|---|
| Age | Reference = 65 - 74 | |||
| 75 - 84 | 0.06 | 1.22 | 0.18 | |
| ≥ 85 | 0.29 | 2.08 | < 0.001 | |
| Gender | Reference = Male | |||
| Female | - 0.07 | 0.74 | 0.08 | |
| Ethnicity | Reference = Whites | |||
| Non-Whites | 0.08 | 1.32 | 0.054 | |
| Education | Reference = < High school graduate | |||
| ≥ High school graduate | 0.04 | 1.14 | 0.27 | |
| Severity of illness | Reference = Mild | |||
| Moderate | 0.15 | 1.71 | 0.02 | |
| Major | 0.18 | 1.86 | 0.004 | |
| Extreme | 0.42 | 2.70 | < 0.001 | |
| Cognitive impairment | Reference = No | |||
| Yes | 0.37 | 2.19 | < 0.001 | |
| Charlson comorbidity index | Reference = 0 -1 | |||
| 2 - 3 | 0.04 | 1.26 | 0.15 | |
| ≥ 4 | 0.22 | 1.73 | 0.01 | |
| Study groups | Reference = Control | |||
| Intervention | - 0.09 | 0.65 | 0.02 | |
Acknowledgement
The authors disclose no financial conflicts of interest pertinent to this study.
This study is supported by the American Geriatrics Society (Junior Researcher Seed Grant) and Korean Ministry of Education, Science and Technology (Excellence of Quality of Care Project).
Authors thank to Ms. Susan Garcia who help manuscript preparation and Ms. Brenda Fay for literature search.
References
- [1].Hoogerduijn JG,Schuurmans MJ,Duijnstee MS,de Rooij SE,Grypdonck MF (2007). A systemic review of predictors and screening instruments to identify older hospitalized patients at risk for functional decline. J Clin Nurs, 22: 1322-1331. [DOI] [PubMed] [Google Scholar]
- [2].Boyd CM,Landefeld CS,Counsell SR,Palmer RM,Fortinsky RH,Kresevic D, et al. (2008). Recovery of activities of daily living in older adults after hospitalization for acute medical illness. J Am Geriatr Soc, 56: 2171-2179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Brown CJ,Friedkin RJ,Inouye SK (2004). Prevalence and outcomes of low mobility in hospitalized older persons. J Am Geriatr Soc, 52: 1263-1270. [DOI] [PubMed] [Google Scholar]
- [4].Pedersen MM,Bodilsen AC,Petersen J,Beyer N,Andersen O,Lawson-Smith L,Kehlet H,Bandholm T (2013). Twenty-four-hour mobility during acute hospitalization in older medical patients. J Gerontol A Biol Sci Med Sci, 68: 331-337. [DOI] [PubMed] [Google Scholar]
- [5].Yoo JW,Kim SJ,Geng Y,Shin HP,Nakagawa S (2014). Quality and innovations for caring hospitalized older persons in the Unites States. Aging Dis, 5:41-51 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Covinsky KE,Pierluissi E,Johnston CB (2011). Hospitalization-associated disability: “She was probably able to ambulate, but I’m not sure”. JAMA, 306: 1782-1793. [DOI] [PubMed] [Google Scholar]
- [7].Buurman BM,Hoogerduijn JG,de Haan RJ,Abu-Hanna A,Lagaay AM,Verhaar HJ, et al. (2011). Geriatric conditions in acutely hospitalized older patients: Prevalence and one-year survival and functional decline. PLos One, 6: e26951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Buurman BM,Hoogerduijn JG,van Gemert EA,de Haan RJ,Schuurmans MJ,de Rooij SE (2012). Clinical characters and outcomes of hospitalized older patients with distinct risk profiles for functional decline: A prospective cohort study. PLos One, 7: e29621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Mudge AM,O’Rourke P,Denaro CP (2010). Timing and risk factors for functional changes associated with medical hospitalization in older patients. J Gerontol A Biol Sci Med Sci, 65: 866-872. [DOI] [PubMed] [Google Scholar]
- [10].Sutton M,Grimmer-Somers K,Jeffries L (2008). Screening tools to identify hospitalized elders at risk of functional decline: a systematic review. Int J Clin Pract, 62: 1900-1909. [DOI] [PubMed] [Google Scholar]
- [11].Walter LC,Brand RJ,Counsell SR,Palmer RM,Landefeld CS,Fortinsky RH, et al. (2001). Development and validation of a prognostic index for 1-year mortality in older adults after hospitalization. JAMA, 285: 2987-2894. [DOI] [PubMed] [Google Scholar]
- [12].Gill TM,Allore HG,Gahbauer EA,Murphy TE (2010). Change in disability after hospitalization or restricted activity in older persons. JAMA, 304: 1919-1928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Hoenig H,Rubenstein LV,Sloane R,Horner R,Kahn K (1997). What is the role of timing in the surgical and rehabilitative care of community-dwelling older persons with acute hip fracture? Arch Intern Med, 157: 513-520. [PubMed] [Google Scholar]
- [14].Johnson MF,Kramer AM,Lin M,Kowalsky JC,Steiner JF (2000). Outcomes of older persons receiving rehabilitation for medical and surgical conditions compared with hip fracture and stroke. J Am Geriatr Soc, 48: 1389-1397. [DOI] [PubMed] [Google Scholar]
- [15].Mudge A,Laracy S,Richter K,Denaro C (2006). Controlled trial of multidisciplinary care teams for acutely ill medical inpatients: enhanced multidisciplinary care. Intern Med J, 36: 558-563. [DOI] [PubMed] [Google Scholar]
- [16].Lee W,Cheng Y,Liu C,Peng LN,Liu LK,Chen LK (2012). Dose-dependent effect of rehabilitation in functional recovery of older patients in the post-acute care unit. Arch Gerontol Geriatr, 54: e290-293. [DOI] [PubMed] [Google Scholar]
- [17].Jette D,Warren R,Wirtalla C (2005). Relationship between therapy intensity and outcomes of rehabilitation in skilled nursing facilities. Arch Phys Med Rehabil, 86: 373-379. [DOI] [PubMed] [Google Scholar]
- [18].Buurman BM,van Munster BC,Korevaar JC,de Haan RJ,de Rooij SE (2011). Variability in measuring (instrumental) activities of daily living functioning and functional decline in hospitalized older medical patients: a systemic review. J Clin Epidemiol, 64: 619-627. [DOI] [PubMed] [Google Scholar]
- [19].Yoo JW,Kim S,Ryu W,Choi JH (2013). Intensified rehabilitation therapy and transitions to skilled nursing facilities in community-living seniors with acute medical illness. Geriatr Gerontol Int, 13: 547-554. [DOI] [PubMed] [Google Scholar]
- [20].Charlson ME,Pompei P,Ales KL,MacKenzie CR (1987). A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chron Dis, 40: 373-383. [DOI] [PubMed] [Google Scholar]
- [21].Borson S (2000). The mini-cog: a cognitive “vitals signs” measure for dementia screening in multi-lingual elderly. Int J Geriatr Psychiatry, 15:1021-1027. [DOI] [PubMed] [Google Scholar]
- [22].Harrell F,Lee K,Mark D (1996). Multivariable prognostic models: Issues in developing models, evaluating assumptions and adequacy, and measuring and reducing errors. Stat Med, 15: 361-387. [DOI] [PubMed] [Google Scholar]
- [23].Kim SJ,Lee JH,Nakagawa S,Bukowy E,Biswas A,Han B, et al. (2014). Predictors of hospitalization among newly admitted skilled nursing facility residents: rethinking the role of the functional decline. J Patient Res Rev, 1:70-76. [Google Scholar]
- [24].Bodilsen AC,Pedersen MM,Petersen J,Beyer N,Andersen O,Smith LL, et al. (2013). Acute hospitalization of the older patient: Changes in muscle strength and functional performance during hospitalization and 30 days after discharge. Am J Phys Med Rehabil, 92: 789-796. [DOI] [PubMed] [Google Scholar]
- [25].Hospital inpatient and outpatient services (2013). In: Medicare Payment Advisory Commission report to Congress. Washington, DC: Department of Health and Human Services, 41-74. [Google Scholar]
- [26].Jette DU,Brown R,Collette N,Friant W,Graves L (2009). Physical therapists’ management of patients in the acute care setting: an observational study. Phys Ther, 89: 1158-1181. [DOI] [PubMed] [Google Scholar]


