Abstract
Background
Research suggests stereotyping by clinicians as one contributor to racial and gender-based health disparities. It is necessary to understand the origins of such biases before interventions can be developed to eliminate them. As a first step toward this understanding, we tested for the presence of bias in senior medical students.
Objective
The purpose of the study was to determine whether bias based on race, gender, or socioeconomic status influenced clinical decision-making among medical students.
Design
We surveyed seniors at 84 medical schools, who were required to choose between two clinically equivalent management options for a set of cardiac patient vignettes. We examined variations in student recommendations based on patient race, gender, and socioeconomic status.
Participants
The study included senior medical students.
Main Measures
We investigated the percentage of students selecting cardiac procedural options for vignette patients, analyzed by patient race, gender, and socioeconomic status.
Key Results
Among 4,603 returned surveys, we found no evidence in the overall sample supporting racial or gender bias in student clinical decision-making. Students were slightly more likely to recommend cardiac procedural options for black (43.9 %) vs. white (42 %, p = .03) patients; there was no difference by patient gender. Patient socioeconomic status was the strongest predictor of student recommendations, with patients described as having the highest socioeconomic status most likely to receive procedural care recommendations (50.3 % vs. 43.2 % for those in the lowest socioeconomic status group, p < .001). Analysis by subgroup, however, showed significant regional geographic variation in the influence of patient race and gender on decision-making. Multilevel analysis showed that white female patients were least likely to receive procedural recommendations.
Conclusions
In the sample as a whole, we found no evidence of racial or gender bias in student clinical decision-making. However, we did find evidence of bias with regard to the influence of patient socioeconomic status, geographic variations, and the influence of interactions between patient race and gender on student recommendations.
KEY WORDS: students, medical; decision-making; health care disparities
Introduction
Disparities in health and health care continue to plague our nation. Extensive evidence shows differences across racial/ethnic, gender, and geographic groupings.1 Access to health care, cultural and language differences, communication and trust barriers, and socioeconomic differences are clearly contributors to these disparities.1 However, there is evidence that stereotyping or decisional biases by clinicians in some situations may also play a role.1–12 For example, Schulman, et al. found that recommendations among practicing clinicians for standardized video vignette patients presenting with cardiac symptoms varied according to patient race and gender.13 Another study showed variations by patient race and socioeconomic status in clinician expectations of post-angiogram cardiac patients.14 Similarly, pain medication administered for major fractures in the emergency setting was shown to vary by patient ethnicity.15
Evidence of decisional bias among practicing clinicians raises questions regarding the origin of such biases as well as ways to eliminate them. Do they originate from similar biases that exist prior to entry into a medical career, are they a reflection of training processes, or are they a product of the practice environment? Answers to these questions could be of value to medical educators and policymakers.
Preliminary investigations seeking similar evidence of decisional bias among medical students have shown mixed findings. In one study, students shown videotapes of standardized black female or white male patients ascribed a lower value to the quality of life of the black female “patient” than to the white male “patient.”16 On the other hand, a more recent study failed to show that student assessments of patient vignettes varied by race or social class.17 Both of these studies, however, were based on students who were early in their medical school training and had no clinical experience, and the studies did not assess clinical decision-making. A third study used clinical-level students from a single institution to demonstrate evidence of situational gender bias in vignette patient diagnoses.18 We are unaware of any other published studies investigating evidence of bias regarding race, gender, or socioeconomic status in clinical decision-making among clinical-level medical students.
As a first step toward determining the origins of these biases, we undertook a study to test for the presence of such bias among medical students nearing the end of their medical school clinical training. Specifically, we tested for bias with respect to patient race, gender, and socioeconomic status (SES) in student recommendations for cardiac care vignette patients. We chose to study senior medical students in order to test whether such biases are present early in clinical training.
Methods
Design and Overview
We invited a national sample of senior medical students during the 2011–2012 academic year to participate in a brief online survey in which they were asked to choose between two clinically equivalent diagnostic or therapeutic options for a set of patient vignettes. We evaluated differences in student recommendations among the vignettes, when we varied the patient race, gender, and SES across the sample, with all other elements remaining fixed.
Survey Instrument
Three academic practicing cardiologists developed a set of eight vignettes of patients requiring cardiac diagnostic or treatment services. We focused these vignettes on cardiac care, given the well-supported evidence that blacks and women, despite clinically equivalent circumstances, are less likely to receive cardiac care procedures.1,19–31 Two clinically equivalent options for recommendations, one involving a procedure and the other a non-procedural option, were developed for each vignette. The vignettes were created under the premise that in situations where clinical equivalency does not allow a clear choice, social psychology concepts would suggest that students would then be forced to base their decisions on secondary, non-clinical factors, such as patient demographics.
We included an additional 15 patient vignettes (“non-cardiac” vignettes) in the survey in order to divert attention from the research questions related to cardiac care patients. These non-cardiac vignettes presented the student with clinical scenarios involving controversy in preventive care services (e.g., age to begin mammography), medication choices (brand vs. generic equivalent), or management strategies for newly diagnosed chronic illness (behavior change vs. medication).
In the cardiac care vignettes, we varied the race and gender of the patient in each vignette across the sample such that individual students receiving the same vignette in their survey versions might see the patient as either male or female and/or black or white. Patient SES (as determined solely by the Hollingshead occupational scale32) was fixed for each individual vignette, but varied across the set of eight cardiac vignettes. Patient attributes were not varied for the non-cardiac vignettes.
We designed all vignettes to be quickly readable. Each participating student received a total of eight vignettes—three cardiac and five non-cardiac—randomly mixed and distributed across the sample to reduce the probability of neighboring students receiving the same vignettes. In order to further support students’ use of non-clinical factors in decision-making, the accompanying instructions clearly emphasized the clinical equivalence of the options presented and that students should not attempt to determine the “correct” option, as either option would be appropriate.
After students had completed the vignettes, they were asked to provide certain demographic information. They were also offered an opportunity to be entered into drawings to win one of two $50 gift certificates to be drawn at each medical school and one of 20 iPad 2s to be drawn nationally.
Survey invitations and administration were conducted online. We tracked screen time to record the length of time students took to answer each vignette. We preserved participant anonymity by directing survey data and contact email addresses for the drawings to separate, unlinked databases.
Survey Piloting
Cardiac care vignettes were piloted first with family medicine residents at two medical schools and then with earlier classes of graduating seniors at seven medical schools. Readers may view a final version of the survey at: http://www.medical-decision-making.com/.
Distribution Process
We contacted students through their medical schools. Depending on school preference, we sent invitations with embedded links to the survey either directly to the students (with up to five solicitations to non-responders), to a student LISTSERV, or to a contact person at the school, who then forwarded the invitation to the senior students. When a student clicked on the link to the survey, a unique version of the survey in mix of vignettes and cardiac patient race/gender was generated. In addition, we varied the order in which the options for each vignette were presented to the student. Automated re-invitation messages were forwarded every 7 days after the initial invitation.
Review and Approval Process
The study protocol was reviewed by the University of New Mexico Institutional Review Board and was determined to be exempt. Subsequently, we sought approval to survey school seniors from the administrators at 130 of the 131 U.S. allopathic medical school campuses graduating seniors in 2012. We also sought approval from the institutional review board at each school whose administrators agreed to participate.
Analysis
We eliminated from analysis any returned survey for which the mean recorded viewing time for the cardiac vignettes was less than 10 seconds—considered as the minimum valid length of time needed to read and respond to a vignette—in order to reduce contamination by respondents participating solely to be entered in the incentive drawings. We examined our remaining sample using standard descriptive statistics. We then compared proportions of seniors recommending cardiac procedural options by vignette patient gender, race, and SES using chi-square statistics. We tested for variation in procedural recommendations by student demographics, again with chi-square statistics. Because national database studies have suggested some regional disparities in delivery of cardiac services, we next examined the data for geographic regional differences in recommendations.33,34 To search for similar geographic patterns in our findings, we grouped students by the Association of American Medical Colleges (AAMC) approach to regional grouping of states: Northeast, South, Central, and West (Appendix).35We also used each school’s self-description (obtained from its website) as “public” or “private” to categorize the schools. Finally, we used weighted multilevel multivariate models to estimate the effects of patient gender, race, and SES on student recommendations, while controlling for student and school descriptors, as well as for clustering by medical school and for variation in medical school senior class size and response rate. These models were weighted by size of medical school class and individual school response rate. We looked for and found in one of the eight cardiac vignettes response patterns indicating a first position response bias (p < .01), so we included a variable for response order.
Results
Sample Characteristics
We successfully contacted administrators of 109 of the 130 school campuses over the 9-month enrollment period from August 2011 to March 2012. Twenty-five contacted schools declined to participate (Fig. 1), for a variety of reasons (e.g., administrator denial, local institutional review board process not open to outside investigators, etc.), resulting in a total of 84 participating schools (77 % of successfully contacted schools, 65 % of eligible schools). Data showed that public schools were more likely than private schools to participate (public 73 % vs. private 50 % participation, p < 0.01), and participating schools had a higher median percentage of students entering primary care in 2011 (41 % vs. 38 %, p < .01, Wilcoxon signed-rank test).36
Fig. 1.
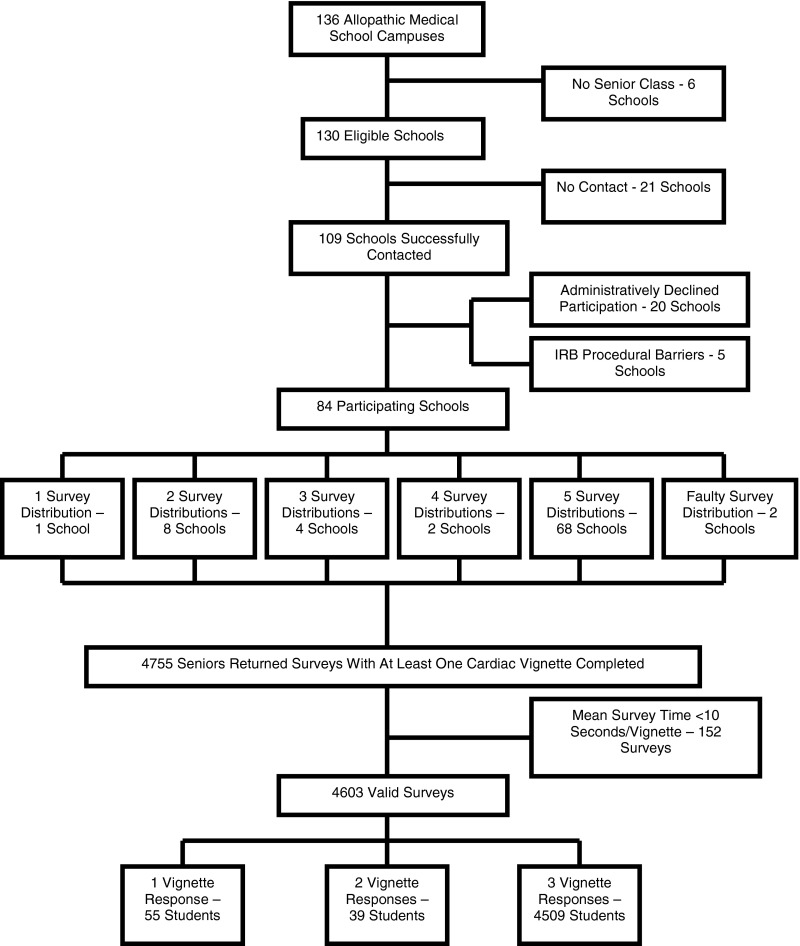
Flow chart of participation in senior medical student survey
We received a total of 4,603 valid surveys from 11,438 seniors at the 84 schools (overall response rate 40.2 %). Demographic characteristics of these students compared with the students participating in the 2012 AAMC Graduate Questionnaire are presented in Table 1. Overall, the two samples were similar, though participants in our survey were slightly more likely to be white and non-Hispanic, and slightly more likely to be entering family medicine, internal medicine, or pediatrics.
Table 1.
Comparison of Survey Participants to Association of American Medical Colleges (AAMC) Senior Medical Student Survey Participants, 2012*
| Survey respondents | 2012 AAMC Graduate Questionnaire respondents* | p value | |
|---|---|---|---|
| n = 4,603 | n = 13,681 | ||
| Age (median) | 26 | 27 | – |
| Female (%) | 50.4 | 48.9 | 0.08 |
| Race/ethnicity (%) | |||
| Hispanic/Latino | 5.2 | 7 | <0.001 |
| Not Hispanic/Latino | 94.8 | 93 | |
| White | 76.3 | 71.6 | <0.001 |
| Black/African American | 5.2 | 6.9 | <0.001 |
| Asian | 17.7 | 23.8 | <0.001 |
| Native Hawaiian/Pacific Islander | 0.5 | 0.3 | 0.02 |
| American Indian/Alaska Native | 1.1 | 0.9 | 0.15 |
| Socioeconomic status, family of origin (%) | |||
| Upper | 6.4 | – | – |
| Upper middle | 38.6 | – | – |
| Middle | 40.6 | – | – |
| Lower middle, lower | 14.4 | – | – |
| Specialty training plans (%) | |||
| N = 10,167 | |||
| Anesthesiology | 6.8 | 7.9 | <0.001 |
| Dermatology | 2.1 | 2.6 | |
| Emergency medicine | 7.6 | 9.0 | |
| Family medicine | 9.9 | 5.9 | |
| Internal medicine, incl. subspecialties | 20.0 | 16.1 | |
| Neurology | 2.1 | 2.6 | |
| Obstetrics & gynecology | 6.6 | 6.4 | |
| Ophthalmology | 2.4 | 3.1 | |
| Pathology | 1.2 | 2.0 | |
| Pediatrics | 12.2 | 9.9 | |
| Physical medicine & rehabilitation | 1.2 | 1.3 | |
| Preventive medicine | <0.1 | 0.1 | |
| Psychiatry | 3.4 | 4.0 | |
| Radiology | 4.6 | 5.8 | |
| Surgery, incl. subspecialties | 17.6 | 18.9 | |
| Other | 1.5 | 4.3 | |
| Unknown | 0.7 | N/A | |
*Association of American Medical Colleges: “2012 Medical School Graduation Questionnaire.” Available at: https://www.aamc.org/download/300448/data/2012gqallschoolssummaryreport.pdf
Sample size variations: age/gender n = 4,460; race/ethnicity n = 4,463; SES n = 4,414; specialty training plans n = 4,429
Principal Analysis: Relationship of Vignette Race, Gender, and SES to Student Recommendations
Table 2 presents the results of bivariate analyses of student recommendations for cardiac vignette patients based on patient race and gender. Overall, students were slightly but statistically significantly more likely to recommend a procedural option for patients who were described as black (43.9 %) than patients described as white (42.0 %) (p = .03). With regard to gender, there was no statistically significant difference in recommendations between vignette patients presented as male (43.5 % procedural recommendation) vs. female (42.4 %) (p = .18). On the other hand, patient SES was a strong and significant predictor of student recommendations, as shown in Table 3, with the highest SES grouping (SES levels 7–9) most likely to receive procedural recommendations (p < .001).
Table 2.
Comparison of Senior Medical Student Recommendations for Cardiac Vignette Patients Based on Vignette Patient Gender and Race, 2012
| Student group | Vignette gender | Vignette race | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Male | Female | Χ2 (p value) | Black | White | Χ2 (p value) | |||||
| N | Procedure (%) | N | Procedure (%) | N | Procedure (%) | N | Procedure (%) | |||
| Overall | 6,758 | 43.5 | 6,902 | 42.4 | 1.76 (0.18) | 6,845 | 43.9 | 6,815 | 42.0 | 4.75 (0.03) |
| Vignette SES* | ||||||||||
| 1–2 | 2,501 | 41.1 | 2,586 | 38.8 | 2.66 (0.10) | 2,541 | 41.6 | 2,546 | 38.2 | 6.20 (0.01) |
| 3–4 | 1,738 | 42.8 | 1,713 | 40.1 | 2.49 (0.11) | 1,773 | 42.6 | 1,678 | 40.2 | 1.97 (0.16) |
| 7–9 | 2,519 | 46.5 | 2,603 | 47.4 | 0.47 (0.49) | 2,531 | 47.0 | 2,591 | 46.9 | 0.004 (0.95) |
| Student gender | ||||||||||
| Male | 3,325 | 42.7 | 3,309 | 41.7 | 0.72 (0.39) | 3,371 | 43.2 | 3,263 | 41.3 | 2.48 (0.12) |
| Female | 3,312 | 44.0 | 3,431 | 42.8 | 1.05 (0.31) | 3,333 | 44.1 | 3,410 | 42.7 | 1.36 (0.24) |
| Unknown | 121 | 51.2 | 162 | 48.1 | 141 | 55.3 | 142 | 43.7 | ||
| Student race/ethnicity | ||||||||||
| AA, H, NA† | 717 | 45.6 | 767 | 45.8 | 0.004 (0.95) | 751 | 45.8 | 733 | 45.6 | 0.01 (0.93) |
| Other | 5,838 | 43.1 | 5,875 | 41.8 | 2.11 (0.15) | 5,869 | 43.4 | 5,844 | 41.6 | 3.88 (0.05) |
| Unknown | 203 | 47.3 | 260 | 45.8 | 225 | 5.7 | 238 | 42.4 | ||
| Student SES | ||||||||||
| Low or lower middle | 908 | 45.5 | 993 | 42.5 | 1.72 (0.19) | 911 | 44.2 | 990 | 43.6 | 0.07 (0.79) |
| Middle | 2,692 | 42.5 | 2,690 | 41.6 | 0.48 (0.49) | 2,758 | 42.6 | 2,624 | 41.4 | 0.77 (0.38) |
| Upper middle | 2,546 | 44.0 | 2,561 | 42.7 | 0.79 (0.37) | 2,528 | 44.9 | 2,579 | 41.8 | 4.74 (0.03) |
| Upper | 420 | 4.7 | 429 | 43.4 | 0.61 (0.44) | 434 | 41.2 | 415 | 42.9 | 0.24 (0.63) |
| Unknown | 192 | 49.0 | 229 | 46.3 % | 214 | 52.3 % | 207 | 42.5 | ||
| Geographic region | ||||||||||
| Central | 1,836 | 44.0 | 1,894 | 41.3 | 2.82 (0.09) | 1,906 | 42.4 | 1,824 | 42.9 | 0.09 (0.77) |
| Northeast | 1,470 | 43.7 | 1,504 | 39.8 | 4.68 (0.03) | 1,484 | 43.7 | 1,490 | 39.7 | 4.73 (0.03) |
| South | 2,599 | 43.4 | 2,674 | 45.0 | 1.48 (0.22) | 2,638 | 45.7 | 2,635 | 42.7 | 4.64 (0.03) |
| West | 853 | 42.7 | 830 | 41.2 | 0.37 (0.54) | 817 | 41.9 | 866 | 42.0 | 0.01 (0.94) |
| School ownership | ||||||||||
| Private | 1,852 | 44.4 | 1,836 | 40.6 | 5.31 (0.02) | 1,848 | 43.6 | 1,840 | 41.5 | 1.65 (0.20) |
| Public | 4,906 | 43.2 | 5,066 | 43.0 | 0.03 (0.87) | 4,997 | 44.0 | 4,975 | 42.2 | 3.13 (0.08) |
* Socioeconomic Status Grouped by Ranking, with Level 1 Lowest SES and Level 9 Highest SES
†African American, Hispanic, and Native American
Table 3.
Comparison of Senior Medical Student Recommendations for Cardiac Vignette Patients Based on Vignette Patient Socioeconomic Status (SES), 2012
| Variable | Vignette patient SES* | Χ2 (p value) | |||||
|---|---|---|---|---|---|---|---|
| 1–2 | 3–4 | 7–9 | |||||
| N | Procedure (%) | N | Procedure (%) | N | Procedure (%) | ||
| Total | 5,087 | 39.9 | 3,451 | 41.4 | 5,122 | 47.0 | 56.06 (<0.001) |
| Vignette patient | |||||||
| Black male | 1,232 | 41.9 | 911 | 44.5 | 1,246 | 46.1 | 4.62 (0.10) |
| Black female | 1,309 | 41.4 | 862 | 40.6 | 1,285 | 47.9 | 15.19 (<0.001) |
| White male | 1,269 | 40.3 | 827 | 40.9 | 1,273 | 46.8 | 12.96 (0.002) |
| White female | 1,277 | 36.2 | 851 | 39.6 | 1,318 | 47.0 | 32.76 (<0.001) |
| Student gender | |||||||
| Male | 2,516 | 38.6 | 1,654 | 42.4 | 2,464 | 45.8 | 26.08 (<0.001) |
| Female | 2,461 | 41.1 | 1,740 | 39.9 | 2,542 | 48.0 | 35.13 (<0.001) |
| Unknown | 110 | 42.7 | 57 | 59.6 | 118 | 50.9 | |
| Student race/ ethnicity | |||||||
| AA, H, NA | 561 | 44.0 | 396 | 44.2 | 527 | 48.6 | 2.75 (0.25) |
| Other | 4,355 | 39.4 | 2,952 | 40.5 | 4,406 | 46.7 | 53.48 (<0.001) |
| Unknown | 171 | 38.6 | 103 | 56.3 | 189 | 48.1 | |
| Student SES† | |||||||
| Low/lower middle | 727 | 40.2 | 490 | 44.3 | 684 | 47.7 | 8.07 (0.02) |
| Middle | 2,040 | 39.5 | 1,335 | 40.1 | 2,007 | 45.9 | 20.21 (<0.001) |
| Upper middle | 1,836 | 40.3 | 1,327 | 41.3 | 1,944 | 47.6 | 23.39 (<0.001) |
| Upper | 326 | 39.0 | 204 | 39.2 | 319 | 47.0 | 5.19 (0.07) |
| Unknown | 158 | 42.4 | 95 | 52.6 | 168 | 49.4 | |
| Geographic region | |||||||
| Central | 1,401 | 38.3 | 947 | 40.4 | 1,382 | 48.5 | 31.79 (<0.001) |
| Northeast | 1,089 | 38.9 | 733 | 38.7 | 1,152 | 46.2 | 15.57 (<0.001) |
| South | 1,956 | 41.1 | 1,361 | 42.8 | 1,956 | 48.3 | 22.16 (<0.000) |
| West | 641 | 41.5 | 410 | 44.1 | 632 | 41.0 | 1.11 (0.57) |
| School ownership | |||||||
| Private | 1,350 | 40.3 | 932 | 39.4 | 1,406 | 46.7 | 16.69 (<0.001) |
| Public | 3,737 | 39.8 | 2,519 | 42.2 | 3,716 | 47. | 41.36 (<0.001) |
*Socioeconomic status, grouped by ranking, with level 1 lowest SES and level 9 highest SES
†Self-categorized socioeconomic status of family of origin
Interactions of Race, Gender, and SES
We next examined recommendation proportions for the four combinations of patient race and gender (Table 4). Overall, there was a non-significant difference in white females being offered procedures less frequently than any other group. With inclusion of SES, when the patient was presented as being in the lowest SES group (SES 1–2), students were more likely to recommend procedures for black patients (Table 2), and least likely to do so for white female patients (Table 4).
Table 4.
Comparison of Senior Medical Student Recommendations for Cardiac Vignette Patients Based on Combinations of Vignette Patient Race and Gender, 2012
| Variable | Vignette race and gender | Χ2 (p value) | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Black male | Black female | White male | White female | ||||||
| N | Procedure (%) | N | Procedure (%) | N | Procedure (%) | N | Procedure (%) | ||
| Total | 3,389 | 44.1 | 3,456 | 43.6 | 3,369 | 42.9 | 3,446 | 41.2 | 6.99 (0.07) |
| Vignette SES* | |||||||||
| 1–2 | 1,232 | 41.9 | 1,309 | 41.4 | 1,269 | 40.3 | 1,277 | 36.2 | 10.70 (0.01) |
| 3–4 | 911 | 44.5 | 862 | 40.6 | 827 | 40.9 | 851 | 39.6 | 4.96 (0.17) |
| 7–9 | 1,246 | 46.1 | 1,285 | 47.9 | 1,273 | 46.8 | 1,318 | 47.0 | 0.76 (0.86) |
| Student gender | |||||||||
| Male | 1,660 | 43.6 | 1,711 | 42.8 | 1,665 | 41.9 | 1,598 | 40.6 | 3.32 (0.34) |
| Female | 1,672 | 44.3 | 1,661 | 43.9 | 1,640 | 43.8 | 1,770 | 41.7 | 2.90 (0.41) |
| Unknown | 57 | 57.9 | 84 | 53.6 | 64 | 45.3 | 78 | 42.3 | |
| Student race/ethnicity | |||||||||
| AA, H, NA† | 360 | 45.0 | 391 | 46.5 | 357 | 46.2 | 376 | 44.9 | 0.31 (0.96) |
| Other | 2,936 | 43.8 | 2,933 | 42.9 | 2,902 | 42.5 | 2,942 | 40.7 | 6.21 (0.10) |
| Unknown | 93 | 51.6 | 132 | 50.0 | 110 | 43.6 | 128 | 41.4 | |
| Student SES | |||||||||
| Low/lower middle | 440 | 44.3 | 471 | 44.2 | 468 | 46.6 | 522 | 41.0 | 3.20 (0.36) |
| Middle | 1,370 | 42.4 | 1,388 | 42.8 | 1,322 | 42.6 | 1,302 | 40.2 | 2.28 (0.52) |
| Upper middle | 1,279 | 45.9 | 1,249 | 43.8 | 1,267 | 42.0 | 1,312 | 41.7 | 5.90 (0.12) |
| Upper | 208 | 40.4 | 226 | 42.0 | 212 | 41.0 | 203 | 44.8 | 0.97 (0.81) |
| Unknown | 92 | 53.3 | 122 | 51.6 | 100 | 45.0 | 107 | 40.2% | |
| Geographic region | |||||||||
| Central | 943 | 44.8 | 963 | 40.1 | 893 | 43.2 | 931 | 42.5 | 4.42 (0.22) |
| Northeast | 725 | 44.8 | 759 | 42.6 | 745 | 42.6 | 745 | 36.9 | 10.39 (0.02) |
| South | 1,305 | 44.5 | 1,333 | 46.8 | 1,294 | 42.2 | 1,341 | 43.3 | 6.34 (0.10) |
| West | 416 | 40.4 | 401 | 43.4 | 437 | 44.9 | 429 | 39.2 | 3.64 (0.30) |
| School ownership | |||||||||
| Private | 932 | 45.0 | 916 | 42.1 | 920 | 43.8 | 920 | 39.1 | 7.27 (0.06) |
| Public | 2,457 | 43.8 | 2,540 | 44.1 | 2,449 | 42.6 | 2,526 | 41.9 | 3.37 (0.34) |
*Socioeconomic status, grouped by ranking, with level 1 lowest SES and level 9 highest SES
†African American, Hispanic, and Native American
Subgroup Analysis: Relationship of Student Demographics, Geographic Region, and School Type to Student Recommendations. Student Demographics
We found that students who described their family of origin as upper middle class or who described their race/ethnicity as other than African American, Hispanic, or Native American were more likely to recommend procedural options for patients described as black (Table 2). Recommendations based on patient vignette gender and on patient SES did not vary across student demographic subgroups, with one exception: students who described themselves as African American, Hispanic, or Native American showed no differences in recommendations based on the patient SES (Table 3).
Geographic Region
In examining geographic area subgroups, we found that students from schools in the Northeast and the South demonstrated greater preference for procedural options with black patients (Table 2), and those from schools in the Northeast were significantly less likely to recommend procedural options if the patient was presented as a female (Table 2). Students across geographic areas showed the same preference for procedural options among higher SES patients (Table 3), with the exception of students attending schools in the West, where that difference was not seen.
School Type
Type of school, private or public, had no influence on overall group patterns with regard to patient race or SES (Tables 2 and 3), but those from private schools were significantly less likely to recommend procedural options for female patients (Table 2).
Multilevel Analysis
Results of multilevel modeling (Table 5) showed findings similar to bivariate analyses. Black male patients were statistically significantly more likely to receive procedural recommendations than white female patients; patients in the highest SES were most likely to receive procedural recommendations. Students from the Northeast were least likely and those from the South most likely to recommend procedural options. The intraclass correlation coefficient was 0.005, indicating a low level of cluster bias.
Table 5.
Results of Multilevel Multivariable Analysis of Student Recommendations for Cardiac Vignette Patients
| Variables included in the analysis | Procedure (%) | p value | Significant differences |
|---|---|---|---|
| Vignette race and gender | |||
| Black male | 47.4 | 0.02 | Black male vs. white female |
| Black female | 47.0 | ||
| White male | 46.4 | ||
| White female | 44.1 | ||
| Vignette SES | |||
| 1–2 | 43.2 | <0.001 | 1–2 vs. 7–9 |
| 3–4 | 45.2 | 3–4 vs. 7–9 | |
| 7–9 | 50.3 | ||
| Student gender | |||
| Male | 44.4 | 0.64 | N/A |
| Female | 44.8 | ||
| Unknown | 49.5 | ||
| Student race/ethnicity - black, Hispanic, or American Indian | |||
| Yes | 48.4 | 0.03 | No vs. yes |
| No | 45.0 | ||
| Unknown | 45.3 | ||
| Student SES* | |||
| Low/lower middle | 46.5 | 0.20 | N/A |
| Middle | 44.2 | ||
| Upper middle | 45.8 | ||
| Upper | 46.2 | ||
| Unknown | 48.4 | ||
| Type of school | |||
| Private | 46.3 | 0.93 | N/A |
| Public | 46.2 | ||
| Location of school | |||
| Central | 46.8 | 0.02 | Northeast vs. South |
| Northeast | 44.9 | ||
| South | 47.9 | ||
| West | 45.3 | ||
*Self-described socioeconomic status of family of origin
Discussion
We found no evidence in the overall sample of racial bias in clinical decision-making leading to fewer recommendations for cardiac procedural services for black vignette patients. Indeed, students recommended procedural services slightly more frequently for black than white patients. We also found no evidence in our overall sample of clinical decision-making bias related to patient gender. We did find a clear variation in student recommendations by patient SES, with the highest SES patients more likely to receive procedural recommendations.
Our results present a more complex picture, however, when subjected to detailed secondary analyses. We found regional differences, with students graduating from schools in the Northeast more likely to recommend procedures if the patient was black or was male. Students from private schools were less likely to recommend procedural choices for female patients.
Our findings are open to a variety of interpretations, the most optimistic of which is that, overall, they reveal evolving clinical decision-making, perhaps reflecting increasing sensitivity to the problem of racial and gender-based disparities. The variations by patient SES, however, suggest that even with the overall findings related to race, more work needs to be done to fully eliminate bias in clinical decision-making.
An alternative interpretation is that overall rates related to racial and gender-based decision-making may obscure important differences within the population of students. Counterbalancing pockets (e.g., geographic regions) of bias might still exist within the larger medical student population. Evidence of differences in rates of procedural choice by region and type of school support this interpretation, especially with regard to white female patients. These latter results emphasize the work that lies ahead in determining the basis for these observations, and they also underscore the importance of considering the interaction between race, gender, and SES in disparities in decision-making.
A further interpretation of our findings is that, in general, they demonstrate success in reducing or eliminating explicit bias, while not addressing implicit bias. Explicit bias, operating at a conscious level, is under an individual’s control, and is therefore subject to training, reflection, social pressure, and correction.37 Implicit bias, on the other hand, operates at a subconscious level, is not under voluntary control, and surfaces only under certain conditions, such as fatigue, decisional time pressures, or situational stresses, without the individual’s awareness.38
Haider et al. studied matriculating medical students and found evidence among these students that implicit bias may exist in the absence of explicit bias.17 Our design attempted to elicit implicit as well as explicit bias through our emphasis on rapid response to the survey questions and use of toss-up scenarios. However, it is quite possible that this effort was ineffective in evoking implicit biases. This study, therefore, should not be considered a test for the presence or absence of implicit bias.
Limitations
Although our study had none of the quality flaws noted in a recent systematic review of research on racial bias in health care practitioners,11 it does have several potential limitations. It is possible that our efforts at blinding students to our interest in stereotyping in decision-making were not successful, and as a result, our findings are not valid representations of the students’ true decision-making tendencies. In this case, a social desirability bias may have influenced student recommendations, resulting in the slightly increased rate of procedural recommendations for blacks. However, this possibility would be difficult to reconcile with our findings demonstrating evidence of decision-making bias in interactions between race, gender, and SES. Another concern might be the use of vignettes to search for evidence of stereotyping in decision-making, although several studies have shown vignettes to be accurate in reflecting actual clinical practice.39–43 The survey response rate among students at participating schools (40.2 %) is low enough that some might question the validity of the sample. Although our data show relatively few differences among survey respondents and the larger population of senior medical students as depicted by the AAMC survey, suggesting sample validity, it is possible that non-participants and students from non-participating schools may demonstrate different decision-making tendencies than those reflected in these data. Finally, with regard to variations in student recommendations by patient SES, it is possible that cost-of-care perspectives led students to select care options based on expected ability to pay.
Because of the large sample size, we were able to demonstrate statistically significant results despite relatively small absolute differences in recommendations among study groups. Given the high prevalence of cardiac disease, however, even small variations across the population can translate into large numbers of individuals affected. This importance of small differences is comparable to that seen in the post-myocardial infarction use of beta-blocker medications, which have been shown to produce a 1.8 % reduction in long-term mortality rates compared with patients not using beta-blockers.44
Conclusions
Our national survey of senior medical students is reason for cautious optimism that racial bias in clinical decision-making may be less common in the future. Much work still needs to be done, however, as reflected in our findings of variations by region and between public and private schools, of the strong influence of patient SES on students’ approach to toss-up clinical scenarios, and of the interplay between race, gender, and SES. We need to better understand these differences and their origins, whether subsequent medical training changes the picture painted by our findings, and the influence, if any, of implicit bias on clinical decision-making. Research to explore the driving influences on decision-making among medical students and the elements present in the training environment that promote or eliminate bias is an important next step. Most importantly, we need to use such understanding to promote effective solutions for preventing these tendencies in the future and for eliminating any lingering biases in current clinical decision-making.
Acknowledgments
Contributors
The authors greatly appreciate the important contributions of a number of individuals without whose support this work would not have been possible: Denise Ruybal (administrative support); Robert Finkelhor, MD (cardiac vignette design); Craig Timm, MD (cardiac vignette design); Charles North, MD, MSPH, Brian Solan, MD, MPH, and Daniel Stulberg, MD (vignette design,); Jacque Garcia, MPH (data collection); Joseph Betancourt, MD (consultation on analysis); Catherine Pino, BA and Joseph Colbert, BA (student research assistants). In addition, many faculty and staff at participating medical schools provided invaluable help through their assistance with approval processes and survey distribution.
Funder
Research reported in this publication was supported by the National Institute on Minority Health And Health Disparities of the National Institutes of Health under Award Number R01MD006073. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Prior Presentation
This study was presented at the annual meeting of the North American Primary Care Research Group, December 2, 2012, New Orleans.
Conflict of Interest
The authors each declare that they have no conflict of Interest
Appendix
Table 6
Table 6.
Association of American Medical Colleges Geographic Categorization of Medical Schools33
| Northeast | Central | South | West |
|---|---|---|---|
| University of Connecticut School of Medicine | Loyola University Chicago Stritch School of Medicine | University of Alabama School of Medicine | University of Arizona College of Medicine |
| Georgetown University School of Medicine | Southern Illinois University School of Medicine | University of South Alabama College of Medicine | University of California, Davis, School of Medicine |
| Howard University College of Medicine | University of Chicago Division of the Biological Sciences The Pritzker School of Medicine | University of Arkansas for Medical Sciences College of Medicine | University of California, Irvine, School of Medicine |
| Johns Hopkins University School of Medicine | University of Illinois - Chicago | University of Florida College of Medicine | University of California, San Diego School of Medicine |
| Boston University School of Medicine | University of Illinois - Urbana | University of Miami Leonard M. Miller School of Medicine | University of California, San Francisco, School of Medicine |
| Tufts University School of Medicine | University of Illinois - Peoria | University of South Florida College of Medicine | University of Colorado School of Medicine |
| University of Massachusetts Medical School | University of Illinois - Rockford | Emory University School of Medicine | University of Nevada - Las Vegas |
| Dartmouth Medical School | Indiana University School of Medicine | Medical College of Georgia School of Medicine | University of Nevada School of Medicine - Reno |
| Albany Medical College | University of Kansas School of Medicine | Mercer University School of Medicine | University of New Mexico School of Medicine |
| Albert Einstein College of Medicine of Yeshiva University | Michigan State University College of Human Medicine | Morehouse School of Medicine | Oregon Health & Science University School of Medicine |
| Mount Sinai School of Medicine | University of Michigan Medical School | University of Kentucky College of Medicine | University of Utah School of Medicine |
| State University of New York Downstate Medical Center College of Medicine | Wayne State University School of Medicine | Louisiana State University School of Medicine in Shreveport | University of Washington School of Medicine |
| The School of Medicine at Stony Brook University Medical Center | Saint Louis University School of Medicine | Duke University School of Medicine | |
| University at Buffalo State University of New York School of Medicine & Biomedical Sciences | University of Missouri-Columbia School of Medicine | The Brody School of Medicine at East Carolina University | |
| University of Rochester School of Medicine and Dentistry | Washington University in St. Louis School of Medicine | University of North Carolina at Chapel Hill School of Medicine | |
| Pennsylvania State University College of Medicine | Creighton University School of Medicine | University of Oklahoma College of Medicine | |
| University of Pennsylvania School of Medicine | University of Nebraska College of Medicine | Ponce School of Medicine and Health Sciences | |
| The Warren Alpert Medical School of Brown University | University of North Dakota School of Medicine and Health Sciences | Medical University of South Carolina College of Medicine | |
| University of Vermont College of Medicine | Case Western Reserve University School of Medicine | University of Tennessee Health Science Center College of Medicine | |
| Northeastern Ohio Universities Colleges of Medicine and Pharmacy | Baylor College of Medicine | ||
| Ohio State University College of Medicine | Texas A&M Health Science Center College of Medicine | ||
| Wright State University Boonshoft School of Medicine | Texas Tech University Health Sciences Center School of Medicine | ||
| Sanford School of Medicine The University of South Dakota | The University of Texas School of Medicine at San Antonio | ||
| University of Wisconsin School of Medicine and Public Health | University of Texas Medical Branch School of Medicine | ||
| University of Texas Medical School at Houston | |||
| University of Texas Southwestern Medical Center at Dallas Southwestern Medical School | |||
| Eastern Virginia Medical School | |||
| University of Virginia School of Medicine | |||
| Virginia Commonwealth University School of Medicine | |||
| West Virginia University School of Medicine |
References
- 1.Smedley BD, Stith AY, Nelson AR, editors. Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care. Washington, DC: National Academies Press; 2003. [PubMed] [Google Scholar]
- 2.Dovidio JF, Fiske ST. Under the radar: how unexamined biases in decision-making processes in clinical interactions can contribute to health care disparities. Am J Public Health. 2012;102:945–52. doi: 10.2105/AJPH.2011.300601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.van Ryn M. Research on the provider contribution to race/ethnicity disparities in medical care. Med Care. 2002;40(1 Suppl):I140–51. doi: 10.1097/00005650-200201001-00015. [DOI] [PubMed] [Google Scholar]
- 4.Fincher C, Williams JE, MacLean V, Allison JJ, Kiefe CI, Canto J. Racial disparities in coronary heart disease: a sociological view of the medical literature on physician bias. Ethn Dis. 2004;14:360–71. [PubMed] [Google Scholar]
- 5.Blair IV, Steiner JF, Fairclough DL, et al. Clinicians’ implicit ethnic/racial bias predicts patients’ perceptions of care among black but not Latino patients. Ann Fam Med. 2013;11:43–52. doi: 10.1370/afm.1442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Maserejian NN, Link CL, Lutfey KL, Marceau LD, McKinlay JB. Disparities in physicians’ interpretations of heart disease symptoms by patient gender: results of a video vignette factorial experiment. J Womens Health (Larchmt) 2009;18:1661–7. doi: 10.1089/jwh.2008.1007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lutfey KE, McKinlay JB. What happens along the diagnostic pathway to CHD treatment? Qualitative results concerning cognitive processes. Sociol Health Illn. 2009;31:1077–92. doi: 10.1111/j.1467-9566.2009.01181.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Green AR, Carney DR, Pallin DJ, et al. Implicit bias among physicians and its prediction of thrombolysis decisions for Black and White patients. J Gen Intern Med. 2007;22:1231–8. doi: 10.1007/s11606-007-0258-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cooper LA, Roter DL, Carson KA, et al. The associations of clinicians’ implicit attitudes about race with medical visit communication and patient ratings of interpersonal care. Am J Public Health. 2012;102:979–87. doi: 10.2105/AJPH.2011.300558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sabin JA, Greenwald AG. The influence of implicit bias on treatment recommendations for 4 common pediatric conditions: pain, urinary tract infection, attention deficit hyperactivity disorder, and asthma. Am J Public Health. 2012;102:988–95. doi: 10.2105/AJPH.2011.300621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Paradies Y, Truong M, Priest N. A systematic review of the extent and measurement of healthcare provider racism. J Gen Intern Med. 2013;29:364–87. doi: 10.1007/s11606-013-2583-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Chapman EN, Kaatz A, Carnes M. Physicians and implicit bias: how doctors may unwittingly perpetuate health care disparities. J Gen Intern Med. 2013;28:1504–10. doi: 10.1007/s11606-013-2441-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Schulman KA, Berlin JA, Harless W, et al. The effect of race and sex on physicians’ recommendations for cardiac catheterization. N Engl J Med. 1999;340:618–25. doi: 10.1056/NEJM199902253400806. [DOI] [PubMed] [Google Scholar]
- 14.Van Ryn M, Burke J. The effect of patient race and socio-economic status on physicians’ perceptions of patients. Soc Sci Med. 2000;50:813–28. doi: 10.1016/S0277-9536(99)00338-X. [DOI] [PubMed] [Google Scholar]
- 15.Todd KH, Samaroo N, Hoffman JR. Ethnicity as a risk factor for inadequate emergency department analgesia. JAMA. 1993;269:1537–9. doi: 10.1001/jama.1993.03500120075029. [DOI] [PubMed] [Google Scholar]
- 16.Rathore SS, Lenert LA, Weinfurt KP, et al. The effects of patient sex and race on medical students’ ratings of quality of life. Am J Med. 2000;108:561–6. doi: 10.1016/S0002-9343(00)00352-1. [DOI] [PubMed] [Google Scholar]
- 17.Haider AH, Sexton J, Sriram N, et al. Association of unconscious race and social class bias with vignette-based clinical assessments by medical students. JAMA. 2011;306:942–51. doi: 10.1001/jama.2011.1248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Chiaramonte GR, Friend R. Medical students’ and residents’ gender bias in the diagnosis, treatment, and interpretation of coronary heart disease symptoms. Health Psychol. 2006;25:255–66. doi: 10.1037/0278-6133.25.3.255. [DOI] [PubMed] [Google Scholar]
- 19.Goldberg KC, Hartz AJ, Jacobsen SJ, Krakauer H, Rimm AA. Racial and community factors influencing coronary artery bypass graft surgery rates for all 1986 Medicare patients. JAMA. 1992;267:1473–7. doi: 10.1001/jama.1992.03480110049032. [DOI] [PubMed] [Google Scholar]
- 20.Carlisle DM, Leake BD, Shapiro MF. Racial and ethnic differences in the use of invasive cardiac procedures among cardiac patients in Los Angeles County, 1986 through 1988. Am J Public Health. 1995;85:352–6. doi: 10.2105/AJPH.85.3.352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ford E, Cooper R, Castaner A, Simmons B, Mar M. Coronary arteriography and coronary bypass survey among whites and other racial groups relative to hospital-based incidence rates for coronary artery disease: findings from NHDS. Am J Public Health. 1989;79:437–40. doi: 10.2105/AJPH.79.4.437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ayanian JZ, Udvarhelyi IS, Gatsonis CA, Pashos CL, Epstein AM. Racial differences in the use of revascularization procedures after coronary angiography. JAMA. 1993;269:2642–6. doi: 10.1001/jama.1993.03500200056033. [DOI] [PubMed] [Google Scholar]
- 23.Whittle J, Conigliaro J, Good CB, Lofgren LP. Racial differences in the use of invasive cardiovascular procedures in the Department of Veterans Affairs medical system. N Engl J Med. 1993;329:621–7. doi: 10.1056/NEJM199308263290907. [DOI] [PubMed] [Google Scholar]
- 24.Giles WH, Anda RF, Casper ML, Escobedo LG, Taylor HA. Race and sex differences in rates of invasive cardiac procedures in US hospitals: data from the National Hospital Discharge Survey. Arch Intern Med. 1995;155:318–24. doi: 10.1001/archinte.1995.00430030116013. [DOI] [PubMed] [Google Scholar]
- 25.Weitzman S, Cooper L, Chambless L, et al. Gender, racial and geographic differences in the performance of cardiac diagnostic and therapeutic procedures for hospitalized acute myocardial infarction in four states. Am J Card. 1997;79:722–6. doi: 10.1016/S0002-9149(96)00857-0. [DOI] [PubMed] [Google Scholar]
- 26.Rathore SS, Berger AK, Weinfurt KP, et al. Race, sex, poverty and the medical treatment of acute myocardial infarction in the elderly. Am Heart J. 2000;102:642–8. doi: 10.1161/01.cir.102.6.642. [DOI] [PubMed] [Google Scholar]
- 27.Sheifer SE, Escarce JJ, Schulman KA. Race and sex differences in the management of coronary artery disease. Am Heart J. 2000;139:848–57. doi: 10.1016/S0002-8703(00)90017-6. [DOI] [PubMed] [Google Scholar]
- 28.Ford E, Newman FE, Deosaransingh K. Racial and ethnic differences in the use of cardiovascular procedures: findings from the California Cooperative Cardiovascular Project. Am J Public Health. 2000;90:1128–34. doi: 10.2105/AJPH.90.7.1128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Daumit GL, Hermann JA, Coresh J, Powe NR. Use of cardiovascular procedures among black persons and white persons: a 7-year nationwide study in patients with renal disease. Ann Intern Med. 1999;130:173–82. doi: 10.7326/0003-4819-130-3-199902020-00002. [DOI] [PubMed] [Google Scholar]
- 30.Hannan EL, van Ryn M, Burke J, et al. Access to coronary artery bypass surgery by race/ethnicity and gender among patients who are appropriate for surgery. Med Care. 1999;37:68–77. doi: 10.1097/00005650-199901000-00010. [DOI] [PubMed] [Google Scholar]
- 31.Ayanian JZ, Epstein AM. Differences in the use of procedures between women and men hospitalized for coronary heart disease. N Engl J Med. 1991;325:221–5. doi: 10.1056/NEJM199107253250401. [DOI] [PubMed] [Google Scholar]
- 32.Hollingshead, AA. Four-factor index of social status. Unpublished manuscript, New Haven, CT: Yale University;1975.
- 33.Escarce JJ, Epstein KR, Colby DC, Schwartz JS. Racial differences in the elderly’s use of medical procedures and diagnostic tests. Am J Pub Health. 1993;83:948–54. doi: 10.2105/AJPH.83.7.948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Lee AJ, Gehlbach S, Hosmer D, Reti M, Baker CS. Medicare treatment differences for blacks and whites. Med Care. 1997;35:1173–89. doi: 10.1097/00005650-199712000-00002. [DOI] [PubMed] [Google Scholar]
- 35.Association of American Medical Colleges. AAMC Survey of Resident/Fellow Stipends and Benefits: States by Region. Available at: https://www.aamc.org/download/60992/data/regions.pdf. Accessed on June 29, 2014.
- 36.U.S. News and World Report. Best medical schools: primary care. Available at: http://grad-schools.usnews.rankingsandreviews.com/best-graduate-schools/top-medical-schools/primary-care-rankings. Accessed on June 29, 2014.
- 37.Dovidio JF, Penner LA, Albrecht TL, Norton WE, Gaertner SL, Shelton JN. Disparities and distrust: the implications of psychological processes for understanding racial disparities in health and health care. Soc Sci Med. 2008;67:478–86. doi: 10.1016/j.socscimed.2008.03.019. [DOI] [PubMed] [Google Scholar]
- 38.Stepanikova I. Racial-ethnic biases, time pressure, and medical decisions. J Health Soc Behav. 2012;53:329–43. doi: 10.1177/0022146512445807. [DOI] [PubMed] [Google Scholar]
- 39.Peabody JW, Luck J, Glassman P, Dresselhaus TR, Lee M. Comparison of vignettes, standardized patients, and chart abstraction. JAMA. 2000;283:1715–22. doi: 10.1001/jama.283.13.1715. [DOI] [PubMed] [Google Scholar]
- 40.Kirwan JR, Chaput de Saintonge DM, Joyce CRB, Currey HL. Clinical judgment in rheumatoid arthritis. I. Rheumatologists’ opinions and the development of “paper patients”. Ann Rheum Dis. 1983;42:644–7. doi: 10.1136/ard.42.6.644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Rice N, Robone S, Smith P. Analysis of the validity of the vignette approach to correct for heterogeneity in reporting health system responsiveness. Eur J Health Econ. 2011;12:141–62. doi: 10.1007/s10198-010-0235-5. [DOI] [PubMed] [Google Scholar]
- 42.Peabody JW, Luck J, Glassman P, et al. Measuring the quality of physician practice by using clinical vignettes: a prospective validation study. Ann Intern Med. 2004;141:771–80. doi: 10.7326/0003-4819-141-10-200411160-00008. [DOI] [PubMed] [Google Scholar]
- 43.Dresselhaus TR, Peabody JW, Lee M, Wang MM, Luck J. Measuring compliance with preventive care guidelines. J Gen Intern Med. 2000;15:782–8. doi: 10.1046/j.1525-1497.2000.91007.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Yusuf S, Wittes J, Friedman L. Overview of results of randomized clinical trials in heart disease: 1. Treatments following myocardial infarction. JAMA. 1988;2088–93. [PubMed]


