Abstract
Introduction
Recent colorectal cancer screening studies focus on optimizing adherence. This study evaluated the cost effectiveness of interventions using electronic health records (EHRs), automated mailings, and stepped support increases to improve 2-year colorectal cancer screening adherence.
Methods
Analyses were based on a parallel-design, randomized trial in which three stepped interventions (EHR-linked mailings [“automated”], automated plus telephone assistance [“assisted”], or automated and assisted plus nurse navigation to testing completion or refusal [navigated”]) were compared to usual care. Data were from August 2008–November 2011 with analyses performed during 2012–2013. Implementation resources were micro-costed; research and registry development costs were excluded. Incremental cost-effectiveness ratios (ICERs) were based on number of participants current for screening per guidelines over 2 years. Bootstrapping examined robustness of results.
Results
Intervention delivery cost per participant current for screening ranged from $21 (automated) to $27 (navigated). Inclusion of induced testing costs (e.g., screening colonoscopy) lowered expenditures for automated (ICER=−$159) and assisted (ICER=−$36) relative to usual care over 2 years. Savings arose from increased fecal occult blood testing, substituting for more expensive colonoscopies in usual care. Results were broadly consistent across demographic subgroups. More intensive interventions were consistently likely to be cost effective relative to less intensive interventions, with willingness to pay values of $600–$1,200 for an additional person current for screening yielding ≥80% probability of cost effectiveness.
Conclusions
Two-year cost effectiveness of a stepped approach to colorectal cancer screening promotion based on EHR data is indicated, but longer-term cost effectiveness requires further study.
Introduction
Strong evidence suggests that screening for colorectal cancer (CRC) reduces its incidence and mortality.1,2 CRC screening is also consistently shown to be cost effective and possibly cost saving. Various screening modalities produce similar reductions in CRC morbidity and mortality, and are similarly cost effective.3,4 However, these reductions assume optimal adherence to recommended intervals. Despite the efficacy of screening, 35%–40% of eligible adults are not screened at recommended intervals, and many have never been screened.5,6 Therefore, studies now focus on methods for optimizing CRC screening adherence. Automated telephone reminders, lowered structural barriers, and one-on-one education have been shown to increase CRC screening rates.7,8 Yet, few, if any, trials have tested the incremental effects of a stepped approach and none has tested whether such an approach improves screening adherence over time.9
A four-group RCT, Systems of Support to Increase Colorectal Cancer Screening (SOS), examined whether interventions using electronic health records (EHRs), automated mailings, and stepped increases in support could improve CRC screening adherence over 2 years.10 Compared to usual care, a centralized, EHR-linked, mailed CRC screening program (automated) led to twice as many people being current for screening over 2 years. Assisted (automated plus telephone assistance) and navigated (assisted plus nurse navigation) interventions generated smaller, yet significant stepped increases compared to automated interventions only.11 This paper reports on the 2-year cost effectiveness of this stepped approach to CRC screening promotion.
Methods
Study design, recruitment details, and results have been published.10–12 The Group Health IRB, Seattle, Washington, approved all study procedures.
Setting and Participants
Participants aged 50–73 years were recruited between August 2008 and November 2009 from 21 primary care clinics of Group Health Cooperative (GH), a large Washington State not-for-profit healthcare system. Patients were identified using EHRs and were eligible if they were not current for CRC screening, defined as not receiving colonoscopy within 9 years, flexible sigmoidoscopy within 4 years, or a fecal occult blood test (FOBT) within 9 months. Exclusions were prior CRC diagnosis or active treatment of another cancer, inflammatory bowel disease, or serious chronic or life-threatening disease (e.g., dementia, renal failure). Participant-level data were collected between August 2008 and November 2011.
Usual Care
Usual care at GH involved CRC screening promotion services, including evidence-based guidelines, patient handouts, and an annual system-delivered, tailored “birthday letter” summarizing the patient’s screening and testing history (including CRC screening) and due dates for preventive care procedures.
During the study, all GH-owned primary care clinics implemented a patient-centered medical home (PCMH) model that included interventions to improve quality of care in prevention and chronic disease. As part of the model, medical assistants (MAs) or nurses used the GH patient registry and EHR to complete a form before a patient visit to identify unmet needs (e.g., CRC screening). At the “in-reach” patient visit, the MA gave the form to the physician. Patients overdue for CRC screening received an FOBT kit before the visit or after a physician discussion, depending on physician preference. MAs also reviewed physicians’ patient lists the month after the birthday letter was sent to identify those with unmet needs, provide phone or secure e-mail outreach, order needed tests, and mail FOBT kits if CRC screening was overdue. About half of participants were exposed to the PCMH model in Year 1 and all were exposed in Year 2. Birthday letters were sent throughout the study. The PCMH in-reach component was fully in place early in implementation, whereas outreach occurred more gradually.
Usual Care Plus Automated Intervention
In addition to usual care, in the automated group, an EHR-linked study registry tracked screening due dates and automatically generated mailings. Patients received a letter informing them that they were due for CRC screening and an informational pamphlet about the tests and different screening options. Patients were informed that FOBT kits would be mailed soon, but that they could call the SOS phone line if they preferred another screening test. A research assistant instructed callers to contact their physician’s office and specifically request a sigmoidoscopy or colonoscopy. Non-callers were mailed FOBT kits with simplified pictorial instructions and a postage-paid return envelope. If there was no evidence of FOBT completion after 3 weeks, patients received a single reminder letter to complete the test or inquire about other screening options. EHR evidence of completion of FOBT or other CRC tests stopped trial interventions until the next due date. Interventions were repeated in Year 2 as necessary, with the cycle starting 12 months after FOBT completion or, if no CRC screening occurred in Year 1, 12 months after study entry. Study-generated FOBT results appeared in the EHR and physician inboxes similar to other tests.
Usual Care Plus Automated Intervention Plus Assisted Care
“Assisted” patients received automated support and telephone assistance to complete CRC screening. Three part-time MAs working a combined 6 hours weekly delivered assisted interventions. MAs worked from their usual clinics, but had protected time to provide assisted care. Because participants came from all 21 western Washington GH primary care clinics, the study MA was rarely part of the patient’s care team. MAs used the study registry to view lists of patients who had called to request alternate screening or had not completed FOBT screening 3 weeks after mailing. The MA made up to three contact attempts to determine patient screening intent (e.g., whether the patient planned to complete FOBT soon, preferred sigmoidoscopy or colonoscopy, did not want to complete screening). MAs could review materials sent to help the patient make a choice or complete FOBT. If the patient preferred sigmoidoscopy or colonoscopy, the MA forwarded the request to the patient’s primary care physician and recontacted the patient about the decision and instructions. No other ongoing care was provided. The MA documented all communications in the patient’s EHR and updated the study registry.
Usual Care Plus Automated Intervention Plus Assisted Care Plus Navigated Care
In addition to automated plus assisted support, “navigated” patients received support from a registered nurse (RN). Two part-time RNs working a combined 10% full-time equivalent weekly delivered navigated interventions. As with MAs, RNs worked from their usual clinic, provided care to patients from all clinics, and were rarely part of the patient’s care team. RNs used study registry lists and had protected time to track CRC screening care. As with assisted patients, an MA contacted navigated patients who did not request an alternative test or complete FOBT after mailings and made up to two attempts to determine screening intent. RNs contacted patients who preferred colonoscopy or sigmoidoscopy, needed assistance in making a screening choice, intended to complete FOBT but had no laboratory results after 3 weeks, could not be contacted by the MA, or called with other questions. RN care included assessing patient CRC risk; reviewing procedural risk; providing motivational counseling to assist patients in defining screening intent; creating patient-shared screening action plans; assisting with referrals, appointments, and preparation for endoscopy; and tracking testing completion. If the RN could not reach the patient, a letter or secure e-mail was sent reiterating the importance of CRC screening, including the RN’s phone number for assistance.
Measures
Using EHR or claims data, two primary outcomes were tracked: receiving any CRC test in the 2-year follow-up period, and being current for CRC testing in both Years 1 and 2. Because all participants were overdue for CRC testing at baseline, “current” was defined using U.S. Preventive Services Task Force screening guidelines (receipt of colonoscopy or flexible sigmoidoscopy in Year 1, FOBT in Years 1 and 2, or FOBT in Year 1 and sigmoidoscopy or colonoscopy in Year 2). Secondary outcomes included completion rates for any type of CRC test (including FOBT) in Year 1 and separately in Year 2 for participants still screening-eligible. The proportion receiving each specific screening test (FOBT, colonoscopy, or sigmoidoscopy) during either year was also calculated.
Costs
Intervention costs were defined as the value of resources used to implement and operate the screening promotion interventions over the 2-year trial period and were measured from the healthcare system perspective. Research-related costs were excluded, as were study registry development costs because they were minimal, given GH’s EHR and extant registries. Organizations often have, and EHRs increasingly support, registries for monitoring and managing populations (such as diabetics). Intervention resources were micro-costed.13 Intervention components were classified as labor (e.g., MA calls) or non-labor (e.g., FOBT kits). Cost data came from expense reports and retrospective labor estimates. Unit costs (e.g., MA wage rate plus fringe) were applied to quantities, most of which were tracked in a project database (e.g., follow-up calls). Joint resources (e.g., hotline monitoring) were shared across groups. CRC testing costs were also included (e.g., follow-up colonoscopy after positive FOBT). Year 2 wage rates were increased by 3%. Resource values (unit cost X resource quantities) were then summed on the basis of intervention costs alone and intervention costs plus induced screening costs. For each intervention group, the incremental cost per incremental person screened for CRC was then estimated relative to each less intensive group. Participant-level economic data were collected between August 2008 and November 2011 with economic analyses performed during 2012–2013.
Trial Results
Baseline characteristics across the four groups have been reported,11 and were without significant differences. Comparisons between SOS participants and non-participants have also been reported.12 Participants were more likely to be white, more educated, and engage in other preventive behaviors (e.g., being current for other cancer screenings). Two-year disenrollment was 8.4%, with no significant difference across groups. Compared with those in usual care, intervention participants were more likely to be current for CRC screening for both years with significant increases by intensity (usual care, 26.3%; automated, 50.8%; assisted, 57.5%; navigated, 64.7%). Increases in screening were due primarily to increased completion of FOBT in both years (usual care, 3.9%; automated, 27.5%; assisted, 30.5%; navigated, 35.8%).
Automated interventions were more effective than usual care for all subgroups. Compared with the automated group, the assisted group had significantly higher rates of being current for CRC testing in both years, but only for men, those aged 50–64 years, and whites. The magnitude of effect of the assisted intervention varied, especially among racial subgroups. Compared with the automated group, the navigated group had significantly higher rates for being current for CRC testing in both years regardless of sex, education, and previous CRC testing, except for those aged 65–73 years and non-whites. Patients reporting no previous CRC testing had lower CRC testing rates overall.
Statistical Analysis
The incremental cost-effectiveness ratio (ICER) was calculated as (costi – costc)/(effecti – effectc), where i = intervention, c = control, and effect = number of screened patients. The four-arm trial design yielded six pairwise comparisons. Inherent uncertainty in the cost effectiveness of the intervention arms was assessed by generating scattergrams and 95% confidence ellipses for the ICERs between intervention arms based on 1,000 bootstrap replications. Cost-effectiveness acceptability curves indicating the probability of one intervention being cost effective relative to another at various willingness to pay (WTP) values for an additional outcome unit were also generated using non-parametric methods.14–16 In these analyses, the outcome was an additional person current for screening. Stata, version 11 was used for all analyses.17
Results
Table 1 presents unit costs for intervention components and procedures, Table 2 presents 2-year intervention costs by study arm and per participant, and Table 3 presents baseline ICERs for each arm. The $1,082 estimate for the average cost per participant current for screening in usual care arose largely from the number of colonoscopies under usual care. The automated arm ICER was negative (−$159) because the automated intervention generated fewer colonoscopies than usual care, more than offsetting intervention and increased FOBT costs. Two-year intervention delivery costs (excluding CRC screening costs) ranged between $12,575 for the automated arm ($11 per participant, $21 per screen) and $20,566 for the navigated arm ($18 per participant, $27 per screen). (These delivery costs include an FOBT unit cost including processing of $6 versus $20 used in preliminary analyses,12 and are therefore lower than previously reported.) Positive ICERs for the assisted ($430) and navigated arms ($496) arose from incremental increases in colonoscopies, with small differences having large cost effects. Results were broadly consistent across demographic groups (i.e., sex, age, education, race/ethnicity, first-degree CRC family history, prior CRC testing history; results not shown).
Table 1.
Intervention Unit Costs
| Flexible sigmoidoscopy | |
| Appointment and monitoring | $15.04 |
| Procedure | $360.00 |
| Colonoscopy | |
| Appointment and monitoring | $45.11 |
| Procedure | $1,017.00 |
| FOBT ordering | $1.00 |
| FOBT results | $4.95 |
| Mailing costs | |
| Introductory mailing | $0.85 |
| FOBT kits | $3.35 |
| Reminder letters | $0.80 |
| Patient communication | |
| Medical assistant | $0.41 |
| Registered nurse | $0.75 |
| Follow-up call attempts (1 to 3) | $0.41 |
| Completed follow-up | |
| Medical assistant | $2.84 |
| Registered nurse | $10.53 |
FOBT, fecal occult blood test
Table 2.
Total 2-year Intervention Costs by Study Arm
| Usual care | Automated | Assisted | Navigated | |
|---|---|---|---|---|
| Participants (N) | 1,166 | 1,169 | 1,159 | 1,170 |
| Intervention cost | ||||
| Mailing | - | $12,528 | $13,051 | $13,325 |
| Patient communication | - | $6 | $40 | $135 |
| Follow-up calls | - | - | $615 | $603 |
| FOBT follow-up by medical assistant | - | - | $1,752 | $2,000 |
| FOBT follow-up by registered nurse | - | - | $1,584 | $4,340 |
| Cost of monitoring hotline | - | $41 | $160 | $163 |
| Total intervention costs (without testing costs) | - | $12,575 | $17,202 | $20,566 |
| Testing cost | ||||
| Colonoscopy appointment and procedure | $308,049 | $247,712 | $269,621 | $312,539 |
| Flexible sigmoidoscopy appointment and procedure | $22,320 | $21,960 | $27,360 | $22,740 |
| FOBT orders for tests not resulted | $649 | $535 | $445 | $455 |
| FOBT total returns (results) | $3,207 | $6,134 | $6,565 | $7,053 |
| Total costs (including testing costs) | $334,225 | $288,916 | $321,193 | $363,353 |
| Intervention cost per participant | - | $11 | $15 | $18 |
| Total cost per participant | $287 | $247 | $277 | $311 |
FOBT, fecal occult blood test
Table 3.
Baseline Incremental Cost-Effectiveness Ratios (ICERs)
| Total Cost | N “current” for screening | Total cost per “current” participant | ICER (relative to Usual Care) | ICER (relative to next most intensive arm) | ICER (Navigated to Automated) | |
|---|---|---|---|---|---|---|
| Usual Care | $ 334,225 | 309 | $1,082 | -- | -- | |
| Automated | $ 288,916 | 594 | $486 | −$159 | −$159 | -- |
| Assisted | $ 321,193 | 669 | $480 | −$36 | $430 | -- |
| Navigated | $ 363,353 | 754 | $482 | $65 | $496 | $465 |
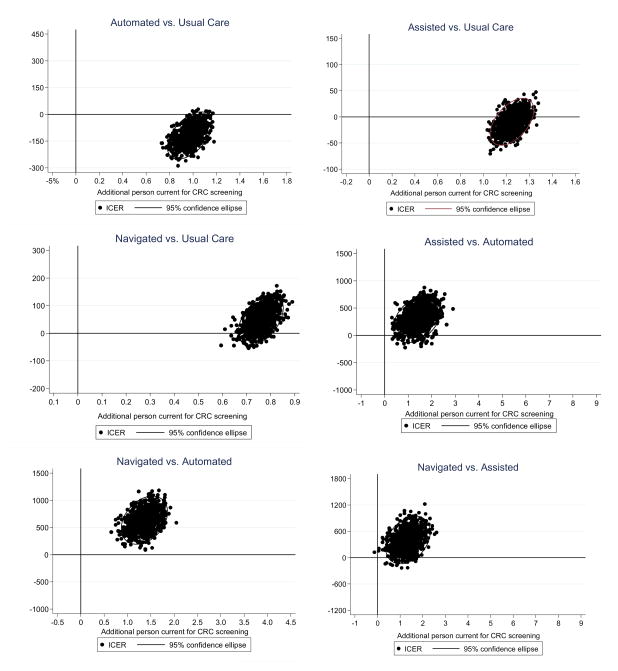
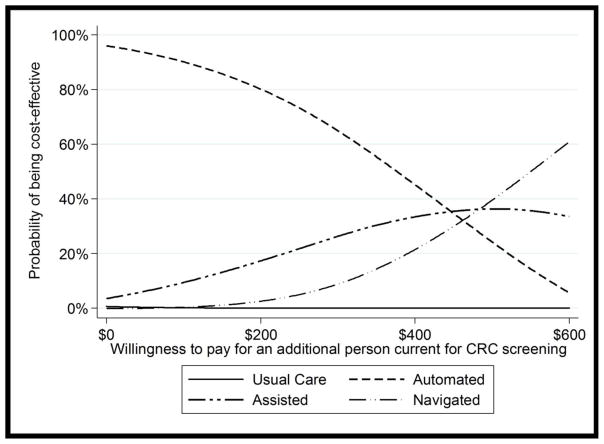
Figure 1 displays scatterplots of incremental costs by incremental increase in the proportion screened with 95% confidence ellipses based on 1,000 bootstrap replications. Figure 2 displays baseline cost-effectiveness acceptability curves for the four arms compared to each other. Figure 2 shows the probability that an intervention is cost effective relative to the other three interventions, given the dollar amount a decision maker is WTP for an additional person current for CRC screening. At low WTP levels, automated intervention is most likely to be cost effective, although this likelihood steadily declines as WTP rises. Above WTP values of approximately $500, navigated intervention is most likely to be cost effective. Table 4 lists, for a specific subgroup and comparison of interventions, WTP values for an additional individual current for CRC screening associated with a given probability of the more intensive intervention being cost effective. For example, for navigated versus assisted, among men a WTP of $758 for an additional screened individual is associated with an 80% probability of navigated being cost effective relative to assisted. A $1,697 WTP is associated with a 95% probability of navigated being cost effective. (All three intervention arms were cost effective, if not cost saving, relative to usual care at all WTP values [results not shown]).
Figure 1.
Scatterplots and 95% confidence ellipses on the incremental cost-effectiveness plane (based on 1,000 replications) – Total sample.
Figure 2.
Cost-effectiveness acceptability curves: Total sample (Probability that an intervention is cost-effective relative to other interventions).
Table 4.
Required WTP Values (for an Additional CRC Screening-Compliant Individual) at Specified Probabilities of Cost-Effectivenessa
| Assisted vs. Automated | Navigated vs. Automated | Navigated vs. Assisted | ||||
|---|---|---|---|---|---|---|
| Probability of being cost-effective | 80% | 95% | 80% | 95% | 80% | 95% |
| Overall | $693 | $1,057 | $589 | $725 | $769 | $1,154 |
| Age | ||||||
| 50–64 | $715 | $1,064 | $594 | $728 | $778 | $1,217 |
| 65–73 | N/A | N/A | $810 | N/A | $1,131 | N/A |
| Any prior CRC testing | ||||||
| No | $738 | $1,473 | $521 | $661 | $650 | $981 |
| Yes | $975 | $2,036 | $804 | $1,100 | $1,571 | N/A |
| First-degree family history of CRC | ||||||
| No | $718 | $1,090 | $576 | $710 | $726 | $1,122 |
| Yes | N/A | N/A | N/A | N/A | N/A | N/A |
The “Automated” intervention is cost saving relative to usual care at any willingness to pay value.
WTP, willingness to pay; CRC, colorectal cancer; N/A, Specified probability of cost-effectiveness never reached
Discussion
These results reinforce the general consensus that CRC screening promotion is cost effective.18 The interventions generated numbers of colonoscopies that increased with resource intensity, but in each case, total colonoscopies over 2 years remained below what was attributed to GH usual care. Reductions in costly colonoscopies largely offset the expense of intervention-generated screening FOBTs. In pairwise comparisons (e.g., navigated versus assisted), more intensive arms were consistently cost effective by conventional standards with no ICER exceeding $500 per additional screened individual.
Studies of similar CRC screening programs yield broadly comparable results.19–23 A 2007 evaluation of basic targeted and tailored behavioral interventions designed to increase CRC screening found that the targeted intervention was highly cost effective at $319 per additional screened individual.21 In a 2012 study, an automated telephone intervention designed to encourage FOBT testing within an integrated healthcare system was very cost effective, especially among patients aged ≥70 years.19 A 2011 comparison of a web-based intervention with a tailored interactive computer-based intervention found that the web-based intervention generated incremental costs of $2,602 per additional screened person.22 A comparison of mailed and tailored screening interventions found that the mailed intervention cost $906 per additional screened individual relative to usual care.20 Tailored interventions were consistently least cost effective, with values per additional screened individual ranging from $1,95820 to $5,84321; in one instance, a web-based comparator dominated (i.e., was more effective and less expensive than) the tailored intervention.22 Yet, although tailored interventions are often the least cost-effective option, this should be interpreted in context, that is, reported ICERs for tailored interventions are typically well within accepted cost-effectiveness standards. Finally, results favorable to CRC screening are not universal; Davis and colleagues24 found that a mailed pamphlet and FOBT with simplified instructions did not improve annual FOBT screening among community clinic patients; furthermore, telephone follow-up by a nurse case manager, although efficacious, was likely too expensive for community clinic implementation.
Limitations
This study has several limitations. Although focusing on promotion and completion of initial CRC screening, 2 years is relatively short for assessing CRC screening cost effectiveness. Over this period, the automated and assisted programs reduced screening expenditures relative to usual care primarily by substituting FOBT for screening colonoscopy. It is acknowledged, however, that the overall risks and benefits of these procedures vary.1 In particular, long-term costs of colonoscopy may decrease over time because such procedures are recommended every 10 years whereas FOBT is needed at least biannually, generating additional screening costs. The 2-year observation period also precluded analysis of more distal health outcomes, such as cancer incidence and mortality. To explore the uncertain long-term cost effectiveness of a screening program that induces substitution of FOBT for colonoscopy, a current follow-up study extends the total SOS observation period to 9 years and focuses on long-term implications for cost and health outcomes.
Another limitation is that all participants were consented, and might not represent the overall GH population, or the general U.S. population, as all GH patients are insured, and the study population was predominantly white. Few meaningful subgroup results were observed; however, the study was not powered to detect subgroup effects. Others have argued that the influence of such variables on screening rates may be large.25 Volunteers had to provide verbal consent and were more likely than non-participants to be educated and white and to practice other preventive behaviors. Study patients also had access to follow-up testing, and no or low copays for screening or diagnostic tests. Higher out-of-pocket costs might lower uptake rates. Thus, the magnitude and relative effect of these results may not generalize, although a co-author (Dr. Green) is currently the co-principal investigator of a large, multisite pragmatic trial that will test the effectiveness of automated strategies such as SOS in raising CRC screening rates in safety-net clinics.
This study focused on delivery of guaiac FOBT, colonoscopy, and flexible sigmoidoscopy, and did not include fecal immunochemical tests, which are becoming more common.26,27 The SOS interventions were designed for implementation inside an integrated healthcare system with an EHR and registry that were integral to patient identification and event tracking. Potential efficiency gains in system-based CRC screening are likely related to access to automated data, and reinforce previous studies.19,23 A patient registry is vital to these interventions, and these results cannot be expected without such a registry.
Conclusions
These results indicate that a stepped approach to CRC screening promotion that exploits EHR-based automated data systems may be cost effective over 2 years. Future work will explore the implications of this approach for the longer-term cost effectiveness of CRC screening promotion.
Acknowledgments
This work was supported by the National Cancer Institute (NCI) of the NIH (R01 CA121125). NCI had no role in study design; data collection, analysis, or interpretation, report writing; or the decision to submit the manuscript for publication. The Systems of Support to Increase Colorectal Cancer Screening study is registered at ClinicalTrials.gov (NCT00158639). We also thank Michael Leo, PhD, for his invaluable assistance with implementing Stata.
Footnotes
No financial disclosures were reported by the authors of this paper.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.U S. Preventive Services Task Force. Screening for colorectal cancer: U.S. Preventive Services Task Force recommendation statement. Ann Intern Med. 2008;149(9):627–637. doi: 10.7326/0003-4819-149-9-200811040-00243. http://dx.doi.org/10.7326/0003-4819-149-9-200811040-00243. [DOI] [PubMed] [Google Scholar]
- 2.Howlader N, Noone AM, Krapcho M, et al., editors. SEER Cancer Statistics Review, 1975–2011. Bethesda, MD: National Cancer Institute; http://seer.cancer.gov/csr/1975_2011/ [Google Scholar]
- 3.Whitlock EP, Lin JS, Liles E, Beil TL, Fu R. Screening for colorectal cancer: a targeted, updated systematic review for the U.S. Preventive Services Task Force. Ann Intern Med. 2008;149(9):638–658. doi: 10.7326/0003-4819-149-9-200811040-00245. http://dx.doi.org/10.7326/0003-4819-149-9-200811040-00245. [DOI] [PubMed] [Google Scholar]
- 4.Zauber AG, Lansdorp-Vogelaar I, Knudsen AB, Wilschut J, van Ballegooijen M, Kuntz KM. Evaluating test strategies for colorectal cancer screening: a decision analysis for the U.S. Preventive Services Task Force. Ann Intern Med. 2008;149(9):659–669. doi: 10.7326/0003-4819-149-9-200811040-00244. http://dx.doi.org/10.7326/0003-4819-149-9-200811040-00244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.CDC. Vital signs: colorectal cancer screening test use--United States, 2012. Morb Mortal Wkly Rep. 2013;62(44):881–888. [PMC free article] [PubMed] [Google Scholar]
- 6.Shapiro JA, Klabunde CN, Thompson TD, Nadel MR, Seeff LC, White A. Patterns of colorectal cancer test use, including CT colonography, in the 2010 National Health Interview Survey. Cancer Epidemiol Biomarkers Prev. 2012;21(6):895–904. doi: 10.1158/1055-9965.EPI-12-0192. http://dx.doi.org/10.1158/1055-9965.EPI-12-0192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Shankaran V, Luu TH, Nonzee N, et al. Costs and cost effectiveness of a health care provider-directed intervention to promote colorectal cancer screening. J Clin Oncol. 2009;27(32):5370–5375. doi: 10.1200/JCO.2008.20.6458. http://dx.doi.org/10.1200/JCO.2008.20.6458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sequist TD, Franz C, Ayanian JZ. Cost-effectiveness of patient mailings to promote colorectal cancer screening. Med Care. 2010;48(6):553–557. doi: 10.1097/MLR.0b013e3181dbd8eb. http://dx.doi.org/10.1097/MLR.0b013e3181dbd8eb. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.CDC. Guide to Community Preventive Services. 2014 www.thecommunityguide.org/index.html.
- 10.Green BB, Wang CY, Horner K, et al. Systems of support to increase colorectal cancer screening and follow-up rates (SOS): design, challenges, and baseline characteristics of trial participants. Contemp Clin Trials. 2010;31(6):589–603. doi: 10.1016/j.cct.2010.07.012. http://dx.doi.org/10.1016/j.cct.2010.07.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Green BB, Wang CY, Anderson ML, et al. An automated intervention with stepped increases in support to increase uptake of colorectal cancer screening: a randomized trial. Ann Intern Med. 2013;158(5 Pt 1):301–311. doi: 10.7326/0003-4819-158-5-201303050-00002. http://dx.doi.org/10.7326/0003-4819-158-5-201303050-00002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Green BB, Bogart A, Chubak J, et al. Nonparticipation in a population-based trial to increase colorectal cancer screening. Am J Prev Med. 2012;42(4):390–397. doi: 10.1016/j.amepre.2011.11.014. http://dx.doi.org/10.1016/j.amepre.2011.11.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hoch JS, Briggs AH, Willan AR. Something old, something new, something borrowed, something blue: a framework for the marriage of health econometrics and cost-effectiveness analysis. Health Econ. 2002;11(5):415–430. doi: 10.1002/hec.678. http://dx.doi.org/10.1002/hec.678. [DOI] [PubMed] [Google Scholar]
- 14.Fenwick E, Byford S. A guide to cost-effectiveness acceptability curves. Br J Psychiatry. 2005;187:106–108. doi: 10.1192/bjp.187.2.106. http://dx.doi.org/10.1192/bjp.187.2.106. [DOI] [PubMed] [Google Scholar]
- 15.Hoch JS, Rockx MA, Krahn AD. Using the net benefit framework to construct cost-effectiveness acceptability curves: an example using data from a trial of external loop recorders versus Holter monitoring for ambulatory monitoring of “community acquired” syncope. BMC Health Serv Res. 2006;6:68. doi: 10.1186/1472-6963-6-68. http://dx.doi.org/10.1186/1472-6963-6-68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Centre for Health Economics. Regression Methods for Health Economic Evaluation Workshop Session Guide. York, UK: University of York; Mar 23–26, 2010. [Google Scholar]
- 17.Frick KD. Micro-costing quantity data collection methods. Med Care. 2009;47(7 Suppl 1):S76–S81. doi: 10.1097/MLR.0b013e31819bc064. http://dx.doi.org/10.1097/MLR.0b013e31819bc064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lansdorp-Vogelaar I, Knudsen AB, Brenner H. Cost-effectiveness of colorectal cancer screening. Epidemiol Rev. 2011;33(1):88–100. doi: 10.1093/epirev/mxr004. http://dx.doi.org/10.1093/epirev/mxr004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Smith DH, Feldstein AC, Perrin N, et al. Automated telephone calls to enhance colorectal cancer screening: economic analysis. Am J Manag Care. 2012;18(11):691–699. [PMC free article] [PubMed] [Google Scholar]
- 20.Lairson DR, Dicarlo M, Deshmuk AA, et al. Cost-effectiveness of a standard intervention versus a navigated intervention on colorectal cancer screening use in primary care. Cancer. 2014;120(7):1042–1049. doi: 10.1002/cncr.28535. http://dx.doi.org/10.1002/cncr.28535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lairson DR, DiCarlo M, Myers RE, et al. Cost-effectiveness of targeted and tailored interventions on colorectal cancer screening use. Cancer. 2008;112(4):779–788. doi: 10.1002/cncr.23232. http://dx.doi.org/10.1002/cncr.23232. [DOI] [PubMed] [Google Scholar]
- 22.Misra S, Lairson DR, Chan W, et al. Cost effectiveness of interventions to promote screening for colorectal cancer: a randomized trial. J Prev Med Public Health. 2011;44(3):101–110. doi: 10.3961/jpmph.2011.44.3.101. http://dx.doi.org/10.3961/jpmph.2011.44.3.101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Wolf MS, Fitzner KA, Powell EF, et al. Costs and cost effectiveness of a health care provider-directed intervention to promote colorectal cancer screening among Veterans. J Clin Oncol. 2005;23(34):8877–8883. doi: 10.1200/JCO.2005.02.6278. http://dx.doi.org/10.1200/JCO.2005.02.6278. [DOI] [PubMed] [Google Scholar]
- 24.Davis TC, Arnold CL, Bennett CL, et al. Strategies to improve repeat fecal occult blood testing cancer screening. Cancer Epidemiol Biomarkers Prev. 2014;23(1):134–143. doi: 10.1158/1055-9965.EPI-13-0795. http://dx.doi.org/10.1158/1055-9965.EPI-13-0795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lansdorp-Vogelaar I, Kuntz KM, Knudsen AB, van Ballegooijen M, Zauber AG, Jemal A. Contribution of screening and survival differences to racial disparities in colorectal cancer rates. Cancer Epidemiol Biomarkers Prev. 2012;21(5):728–736. doi: 10.1158/1055-9965.EPI-12-0023. http://dx.doi.org/10.1158/1055-9965.EPI-12-0023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Goede SL, van Roon AH, Reijerink JC, et al. Cost-effectiveness of one versus two sample faecal immunochemical testing for colorectal cancer screening. Gut. 2013;62(5):727–734. doi: 10.1136/gutjnl-2011-301917. http://dx.doi.org/10.1136/gutjnl-2011-301917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Wilschut JA, Hol L, Dekker E, et al. Cost-effectiveness analysis of a quantitative immunochemical test for colorectal cancer screening. Gastroenterology. 2011;141(5):1648–1655. doi: 10.1053/j.gastro.2011.07.020. http://dx.doi.org/10.1053/j.gastro.2011.07.020. [DOI] [PubMed] [Google Scholar]