Abstract
Objective
Evaluate the long-term adoption of a risk-based caries management program at a university dental clinic.
Methods
We extracted data from electronic records of adult non-edentulous patients who underwent a comprehensive oral evaluation in the university predoctoral clinic, from July 2007 through June 2014 (N=21,984). Consistency with caries management guidelines was measured as the percentage of patients with caries risk designation (low, moderate, high, or extreme) and by the percentage of patients provided non-operative anti-caries agents within each designated caries-risk category. Additionally, we identified patient and provider characteristics associated with risk assessment completion and with provision of anti-caries therapy.
Results
The percentage of patients with documented caries risk grew steadily from 62.3% in 2007-2008 to 92.8% in 2013-2014. Overall, receipt of non-operative anti-caries agents increased with rising caries risk, from low (6.9%), moderate (14.1%), high (36.4%), to extreme (51.4%), but percentages were stable over the study period. Younger patients were more likely to have a completed risk assessment, and among high- and extreme-risk patients, delivery of anti-caries therapy was more common among patients who were younger, identified as Asian or Caucasian, received public dental benefits, or were seen by a student in the four-year doctoral program or in the final year of training.
Conclusions
Extensive compliance in documenting caries risk was achieved within a decade of implementing risk-based clinical guidelines. Caries risk was the most strongly associated of several factors related to delivery of non-operative therapy. In dental education, transition to a risk-based, prevention-focused curriculum may require a long-term commitment.
Keywords: caries management, caries risk assessment, clinical education, predoctoral dental education, CAMBRA, implementation and evaluation, professional education
Introduction
Incorporation of biological and behavioral caries risk factors in the planning and implementation of patient-specific preventive care has long been promoted for dental practice1 and dental education.2 Today, caries risk assessment is widely viewed as central to the realization of minimally invasive and preventive approaches to caries management.3,4 Despite the championing of risk-based and non-operative caries management strategies in the scientific and educational communities, the transition from exclusive reliance on reparative surgical approaches in practice is more fittingly characterized as gradual shift than as a revolution.5
Dental schools play a pivotal role in communicating sound research that readily translates into clinical best practices among their graduates, accelerating the transition toward preventive care in the greater community.6 Formalized caries risk assessments were introduced in clinical and didactic teaching at U.S. dental schools at least at early as the 1980s, for example, at the University of Washington7 and the University of Texas Health Sciences Center at San Antonio.8 In the years that followed, there was a rapid increase in the proportion of dental schools in the U.S. and Canada to emphasize caries risk assessments and non-operative anti-caries therapies in their curricula,9 with risk assessment training programs in place at 90% of schools included in a 2009 survey.10
While many dental schools have integrated caries-risk assessment and risk-based management into their clinical teaching, such curricular transformations have not necessarily yielded synchronous conformity on the part of student dental providers or their faculty instructors. For example, soon after implementation of the Cariology Management Program at the Indiana University School of Dentistry in the early 2000s, only 46% of 350 reviewed patient charts included a completed and faculty-approved caries risk assessment.6 Among 68 moderate and high caries-risk patients seen after a caries management program was introduced at the School of Dental Medicine, Case Western Reserve University in 2008, only 30 had received fluoride varnish, in contrast with clinical protocol.11 These examples suggest that achieving widespread student and faculty buy-in to a prevention-focused, risk-based caries management curriculum may require substantial effort over an extended period of time, as the concept runs contrary to traditional teaching in operative and restorative dentistry that persisted throughout the 20th century.
The School of Dentistry at the University of California San Francisco (UCSF) has embraced Caries Management by Risk Assessment (CAMBRA) for patient-specific caries management since the early 2000s. CAMBRA is a two-step process, in which patient risk is first categorized according to the clinician's assessment of the balance between disease indicators, caries protective factors, and caries predisposing factors.12 Next, caries risk status guides clinical action. CAMBRA recommendations include providing antibacterial therapy and remineralizing agents for adult patients at higher risk.13 Formal caries risk assessment (CRA) forms were introduced in the UCSF student clinic in 2003. As with other academic settings, consistent execution of CAMBRA practices among student providers was not achieved immediately.14 Over the following academic year, CRA forms were at least partially completed at 69% of new patient baseline examinations; however, 42% of CRA forms were missing an overall caries risk category designation.14
We evaluated the long-term implementation of the CAMBRA approach at UCSF more than a decade after its integration into the didactic and clinical curricula. Specifically, consistency with the CAMBRA philosophy in the university student dental clinic from 2007 to 2014 was measured as the percentage of patients with a baseline caries risk designation and in the provision of non-operative anti-caries therapies according to patient risk classification. Secondarily, we evaluated whether certain patient and provider characteristics were associated with CRA completion and non-operative therapy delivery. Under an ideally implemented program, all patients would undergo baseline caries risk assessment, and risk designation would guide preventive therapy, with all patients at high and extreme caries risk offered, and most accepting of, preventive chemical therapy until their disease was controlled.
Methods
Ethical Review
The UCSF Committee on Human Research (institutional review board) approved this study to use electronic dental records for the evaluation of caries management practices at the university teaching clinics. The protocol was approved as number 11-06558.
Study Design
This retrospective time-series study was based on electronic dental records. The main outcomes were caries risk assessment and management practices of student providers at a patient's first comprehensive oral examination in the university clinic, spanning seven academic years (July 1st to June 30th) from 2007-2008 to 2013-2014. Data were retrieved from patient charts using practice management software (axiUm, Exan Group, Vancouver, BC, Canada).
Curriculum Design
In 1999, the UCSF departments of Restorative Dentistry and Dental Public Health were combined, in an effort to coordinate instruction in dental disease prevention and management.15 After a clinical form for patient caries risk assessment was formally introduced at the 2002 CAMBRA consensus conference,16 this form was adopted in the UCSF student dental clinics, first on a pilot basis and then as standard practice beginning July 1, 2003.14 When pre-doctoral patient charts were converted from paper to electronic records during 2005 and 2006, the caries risk assessment form was included. Minor modifications were later incorporated to simplify the form and align it with recommendations from the CAMBRA Coalition national working group.12
Students in both the four-year doctor of dental surgery (DDS) and two-year internationally trained dentist program receive formal didactic instruction in caries risk assessment and management beginning in their first academic quarter and continuing throughout their training. During pre-clinical training, all students must complete CRA test cases. A caries risk assessment competency exam is required during clinical training.
All clinical faculty members, including volunteers, are offered annual training and calibration in CAMBRA guidelines. Under the supervision of faculty dentists, student providers are expected to determine the caries risk status of each patient based on the routine clinical examination and subsequent questions prompted in the caries risk assessment form in the electronic record. This includes appraisal of existing caries risk factors, protective factors, and disease indicators.12,14,17 The caries risk assessment is part of the prescribed sequence for completion of the comprehensive oral evaluation for new patients, although it is possible for student providers to register the evaluation as complete without designating a caries risk category in the electronic chart.
CAMBRA guidelines strongly advise non-operative anti-caries therapy for high- and extreme-risk patients, including antibacterials (e.g. chlorhexidine and/or xylitol products) and remineralizing agents (e.g. high-fluoride concentration toothpaste).13 In the student clinic, such treatments can be provided individually or bundled as a package and can result in additional costs for patients. Patients eligible for Medicaid dental benefits can receive anti-caries agents at no charge through a special arrangement between UCSF and the state Medicaid dental program administrator. Patients can opt not to accept the therapy.
Participants and Procedures
For this study, eligible patients were age 18 years or older, non-edentulous (third molars excluded), and had completed a comprehensive oral evaluation (new patient baseline examination) between July 1, 2007 and June 30, 2014 (N=21,984). Patients were deemed to have a completed caries risk assessment if a risk category (low, moderate, high, or extreme) was documented in the electronic CRA form. A blank form is automatically generated for data entry upon initiation of the comprehensive oral evaluation. We considered a CRA complete if a risk designation was made within 60 days of examination completion date, in recognition that student providers sometimes require multiple appointments to carry out comprehensive examinations.
Patient and provider characteristics were obtained from patient charts. Patient characteristics included age (18-34, 35-44, 45-54, 55-64, or ≥65 years), sex, payer type (private dental insurance, public dental benefits program, or cash), and self-identified race/ethnicity (African American, Asian, Caucasian, Hispanic, or other/declined to state). Student providers were characterized as enrolled in the four-year DDS program or the two-year program for internationally trained dentists, and in their final year of study (fourth year for DDS students; second year for international students) or their next-to-last year (first year of full-time clinical activities).
Among all patients with both a completed comprehensive oral evaluation and caries risk assessment, we calculated the percentage that were provided any form of non-operative anti-caries therapy up to 90 days after examination completion. Potential therapies included chlorhexidine rinse (0.12% chlorhexidine gluconate), topical fluoride (e.g., fluoride toothpaste at 5000 ppm F), and xylitol products (e.g., mint-flavored tablets), provided alone or in combination during at least one clinical visit.
Statistical Analysis
For the two outcomes of interest (the percentage of patients with a caries risk assessment and the percentages of high-risk and extreme-risk patients provided anti-caries therapy) we compared outcome percentages by categories of patient and provider characteristics using Pearson's chi-squared test. To assess trends in outcomes over the seven-year period, we compared the slope for the average annual percentage-point increase or decrease against a null-hypothesis that the slope equaled zero (chi-squared test for linear trend). Results were considered statistically significant at p < 0.05. We did not adjust for multiple tests. Analyses were completed using Stata 12.1 statistical software (StataCorp LP, College Station, TX, USA).
Results
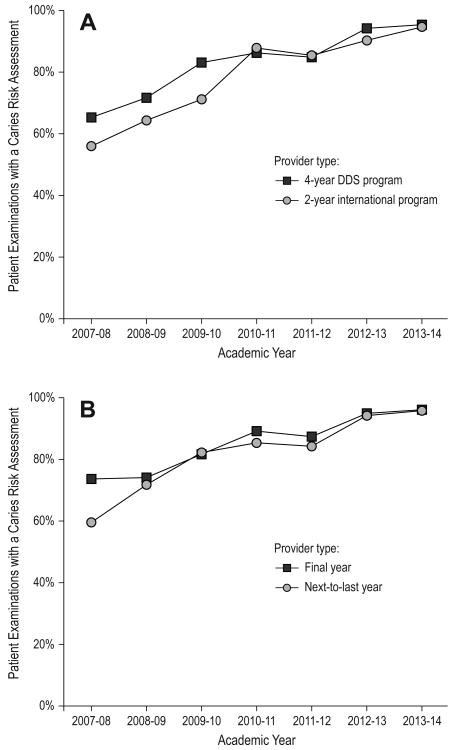
Of the 21,984 unique adult non-edentulous patients who completed a comprehensive oral evaluation at the university student clinic from July 1, 2007 to June 30, 2014, a caries risk assessment was performed for 17,662 (80.3%). The percentage of patients with a completed caries risk assessment rose steadily over the seven-year period, on average increasing by 5.0-percentage points annually (p-for-linear-trend < 0.0001) (Table 1). Over the first three years evaluated, student providers in the four-year DDS program performed caries risk assessments at a greater percentage of comprehensive evaluations than their counterparts in the two-year program for internationally trained dentists; however, this gap closed over the final four years evaluated (Figure 1A). Excepting the 2007-2008 academic year, student providers in their final year of training and in their second-to-last year of training performed risk assessments at a similar percentage of evaluations (Figure 1B).
Table 1. Percentage of patients undergoing caries risk assessment at first comprehensive oral evaluation by academic year, university student clinic (2007-2014).
| Academic Year | Number of comprehensive oral evaluations | Number of evaluations with a caries risk assessment | Percent of evaluations with a caries risk assessment |
|---|---|---|---|
| 2007-2008 | 2476 | 1543 | 62.3 |
| 2008-2009 | 3006 | 2026 | 67.4 |
| 2009-2010 | 3411 | 2675 | 78.4 |
| 2010-2011 | 3831 | 3210 | 83.8 |
| 2011-2012 | 3239 | 2666 | 82.3 |
| 2012-2013 | 2919 | 2664 | 91.3 |
| 2013-2014 | 3102 | 2878 | 92.8 |
| Total | 21,984 | 17,662 | 80.3 |
Figure 1.
Percentage of patients undergoing caries risk assessment at first comprehensive oral evaluation by academic year, according to student provider type, university pre-doctoral clinic (2007-2014)
The percentage of unique patients with a caries risk designation recorded in the electronic patient record at the comprehensive oral (baseline) evaluation increased over the period from 2007-2014. Patterns were similar regardless of whether: (A) student providers were in the 4-year doctor of dental surgery (DDS) program or the 2-year program for internationally trained dentists, or (B) student providers were in their final year or next-to-last year of training.
Table 2 demonstrates the percentage of patients with a formal caries risk assessment among all patients with a completed comprehensive oral evaluation, according to patient characteristics. In general, younger patients were more likely to undergo a caries risk assessment than older patients, as were patients with no dental benefits or insurance (Table 2). Patients who declined to report their race/ethnicity or marked “other” were less likely to complete a caries risk assessment than those who identified with a particular race/ethnicity group; however, there was not a statistically significant difference across the four remaining race/ethnicity categories (p = 0.50).
Table 2. Percentage of patients undergoing caries risk assessment at first comprehensive oral evaluation by patient characteristics, university pre-doctoral clinic (2007-2014).
| Patient characteristic | Number of comprehensive oral evaluations1 | Number of evaluations with a caries risk assessment | Percent of evaluations with a caries risk assessment | p-value (Chi-square test) |
|---|---|---|---|---|
|
| ||||
| Age (years) | <0.001 | |||
| 18-34 | 6479 | 5503 | 84.9 | |
| 35-44 | 3456 | 2856 | 82.6 | |
| 45-54 | 3977 | 3167 | 79.6 | |
| 55-64 | 3955 | 3193 | 80.7 | |
| ≥65 | 3657 | 2871 | 78.5 | |
|
| ||||
| Sex | 0.28 | |||
| Female | 11,299 | 9201 | 81.4 | |
| Male | 9904 | 8122 | 82.0 | |
|
| ||||
| Race/ethnicity | <0.001 | |||
| African American | 2292 | 1855 | 80.9 | |
| Asian | 3405 | 2778 | 82.1 | |
| Caucasian | 9759 | 8014 | 81.6 | |
| Hispanic | 4166 | 3426 | 82.2 | |
| Other/declined to state | 2376 | 1602 | 67.4 | |
|
| ||||
| Payer type | <0.001 | |||
| Private insurance | 2719 | 2222 | 81.7 | |
| Public program | 4424 | 3598 | 81.3 | |
| Cash | 14,004 | 11,752 | 83.9 | |
|
| ||||
| Total | 21,984 | 17,662 | 80.3 | |
Total within some characteristics is less than the grand total due to missing data on patient characteristics
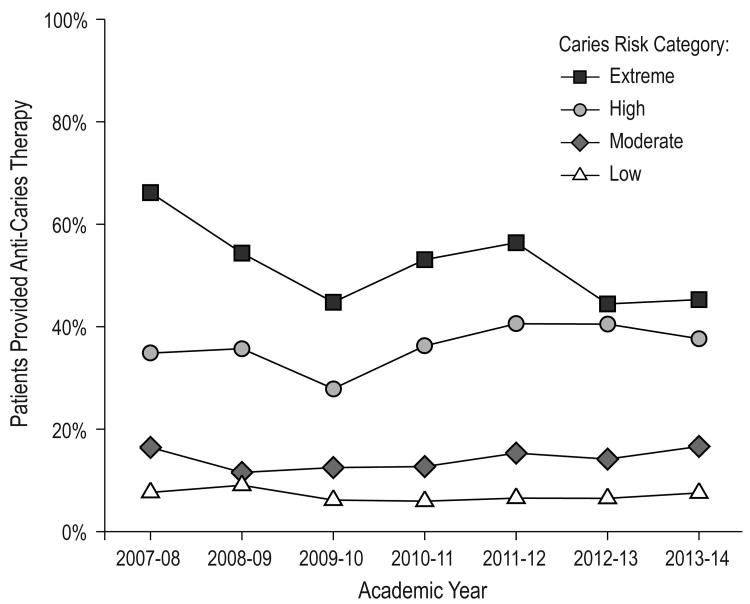
Most patients were classified as high risk (12,415 of 17,662; 70.3%), followed by moderate (14.3%), low (10.8%), and extreme caries risk (4.6%). The percentage of patients who received any form of non-operative anti-caries therapy after the comprehensive oral examination was greater with each rising category of caries risk: low (6.9%), moderate (14.1%), high (36.4%), and extreme (51.4%). The percentage of patients provided anti-caries therapy in each caries risk category was fairly stable over the seven-year period (Figure 2). There was a slight but statistically significant linear trend of 1.2-percentage point annual increase in anti-caries therapy provision among high-risk patients (p-for-linear-trend < 0.0001) but also an average 2.1-percentage points annual decrease for extreme-risk patients (p-for-linear-trend = 0.03).
Figure 2.
Percentage of patients provided non-operative anti-caries therapy by caries risk category and academic year.
In each academic year evaluated, the percentage of patients provided non-operative anti-caries therapy at the comprehensive oral evaluation (baseline exam) increased with each rising level of caries risk, however, therapy provision did not increase steadily over time within risk categories.
Table 3 presents the percentage of patients provided non-operative anti-caries therapy among those patients classified as high caries risk and extreme caries risk, according to patient and provider characteristics. Among high-risk patients, younger patients were more likely to be provided therapy than older patients, as were patients who identified as Asian or Caucasian in comparison to patients who identified as African American or Hispanic (Table 3). Patients without dental insurance (“cash-paying”) were less likely to receive therapy than those patients with either private or public dental benefits. Student providers in the four-year DDS program or in the final year of training were more likely to provide anti-caries therapy to their patients than student providers in the two-year program for internationally trained dentists or in the next-to-last year of training, respectively (Table 3). Patterns were similar among extreme-risk patients, although not all differences reached statistical significance (Table 3).
Table 3. Percentage of high and extreme caries risk patients provided with anti-caries therapy according to patient and provider characteristics, university pre-doctoral clinic (2007-2014).
| High caries risk | Extreme caries risk | |||||
|---|---|---|---|---|---|---|
|
| ||||||
| Patient or provider characteristic | Number of patients1 | Percent of patients provided anti-caries therapy | p-value (Chi-square test) | Number of patients1 | Percent of patients provided anti-caries therapy | p-value (Chi-square test) |
|
| ||||||
| Age (years) | <0.001 | 0.19 | ||||
| 18-34 | 4106 | 40.1 | 129 | 61.2 | ||
| 35-44 | 2069 | 35.9 | 107 | 52.3 | ||
| 45-54 | 2177 | 35.3 | 173 | 49.1 | ||
| 55-64 | 2124 | 34.2 | 222 | 49.5 | ||
| ≥65 | 1884 | 33.8 | 180 | 48.9 | ||
|
| ||||||
| Sex | 0.01 | 0.90 | ||||
| Female | 6303 | 37.8 | 413 | 51.3 | ||
| Male | 5862 | 35.6 | 392 | 51.8 | ||
|
| ||||||
| Race/ethnicity | <0.001 | 0.33 | ||||
| African American | 1407 | 32.4 | 75 | 49.3 | ||
| Asian | 1881 | 37.5 | 89 | 51.7 | ||
| Caucasian | 5497 | 38.3 | 459 | 53.8 | ||
| Hispanic | 2509 | 33.6 | 109 | 49.5 | ||
| Other/declined to state | 1133 | 36.8 | 82 | 41.5 | ||
|
| ||||||
| Payer type | <0.001 | 0.02 | ||||
| Private insurance | 1504 | 36.9 | 74 | 59.5 | ||
| Public program | 2557 | 45.8 | 305 | 56.1 | ||
| Cash | 8304 | 33.7 | 431 | 46.9 | ||
|
| ||||||
| Provider type | <0.001 | 0.08 | ||||
| 4-year DDS | 10,990 | 37.3 | 735 | 52.5 | ||
| 2-year international | 1365 | 31.4 | 76 | 42.1 | ||
|
| ||||||
| Provider year in training | <0.001 | <0.001 | ||||
| Final year | 4730 | 39.2 | 312 | 61.9 | ||
| Next-to-last | 7618 | 35.0 | 496 | 45.0 | ||
|
| ||||||
| Total | 12,415 | 36.4 | 814 | 51.4 | ||
Total within some characteristics is less than the grand total due to missing data on patient or provider characteristics
Abbreviation: DDS = doctor of dental surgery degree program
Discussion
In this university dental clinic, there was a steady rise in student provider compliance with caries risk assessment: since 2012, over 90% of new patients had a documented caries risk designation. Despite widespread curricular reorganization and emphasis on risk assessment in clinical training beginning in 2003, pervasive compliance was not realized for nearly a decade. Caries risk status was strongly related to whether patients received preventive therapy, suggesting that many student dentists appropriately employed caries risk status to guide clinical caries management. However, fewer than half of high-risk patients received therapy, without dramatic improvement in therapy delivery over time, demonstrating a lingering gap between teaching philosophy and students' clinical actions. Considering both the successes and remaining challenges of CAMBRA implementation at UCSF, it appears that even in an educational setting, reorientation of clinical activities toward patient-tailored preventive strategies can be a lengthy process requiring sustained effort, with high levels of compliance attainable over time.
Multiple considerations on the part of patients, students, and supervising faculty likely contributed to whether or not clinical caries management followed a risk-based approach. Focus group interviews conducted with students and faculty at Indiana University School of Dentistry in 2011 and 2012 identified the perceived effectiveness of a caries management strategy to provide a discernable patient benefit as a key factor in determining support for a risk-based approach.18 In a survey administered soon after the implementation of a caries risk assessment and management program at the University of Florida College of Dentistry, many students expressed uncertainty regarding the safety and efficacy of various anti-caries agents.19 With growing evidence supporting the effectiveness of antibacterial and fluoride therapy to reduce caries risk,20 clearer communication of the objectives and expected outcomes of risk assessment in patient care may be needed to enhance buy-in from faculty and student clinicians.18
The percentage of patients with a completed CRA did not differ according to year in training of the student provider. However, final-year providers were more likely to deliver non-operative preventive therapy. In a 2005 survey of UCSF dental students, prior to the period of the current investigation, reported intention to perform CRA or provide prevention counseling did not increase with years of training, and knowledge and perceived confidence related to caries risk assessment did not differ among third- and fourth-year students.21 The differences seen in clinic activities could be ascribed to better time management abilities and improved navigation through clinical procedures with experience, or to greater skill in communicating the value of preventive therapies to patients. Simplifying forms and systems for risk-based management may promote clinician acceptance,18 and simplifying revisions made to the CRA form used at UCSF may have contributed to the rising CRA compliance over the study period. Making it logistically easier to provide non-operative anti-caries agents could improve future compliance with this activity, as well.
Student providers in the four-year DDS program more commonly provided anti-caries therapy for high- and extreme-risk patients than their counterparts in the program for internationally trained dentists. It is possible that internationally trained dentists, on average, were less receptive to a treatment philosophy that might have differed from their prior training. Furthermore, the two additional years of preclinical instruction offered in the DDS program could have bolstered CAMBRA familiarity and acceptability among DDS students. However, the international students receive the same instruction on CAMBRA implementation as the domestic DDS students, although it is done in a compressed time frame together with many other topics. Additionally, support for CAMBRA principles could have differed between supervising clinical faculty members across the two programs.
High-risk patients with dental benefits through a public program were more likely to receive preventive therapy than patients with no dental benefits, as the state Medicaid dental program provided reimbursement for anti-caries agents by special arrangement between the university and the state Medicaid dental program administrator. For patients incurring out-of-pocket expenses for anti-caries therapy, the perceived trade-off between the cost of preventive agents and potential expenses in restorative care presumably factored prominently in the decision whether to pursue non-operative therapy. For dentists in practice, the lack of third-party reimbursement for preventive services, such as sealants for adults and older adolescents,22 is frequently cited as a barrier to service delivery.
We found an association between patient age and the provision of non-operative anti-caries therapy, with younger patient more likely to receive therapy. Similarly, a survey of dentists in private practice in France revealed a preference for delivery of minimally invasive treatments to patients who were younger, healthier, and better insured, although delivery of non-surgical interventions for any patients was rare.23 In addition, delivery of non-operative therapy was more likely for high-risk patients who identified as Asian or Caucasian than those who identified as African American or Hispanic, although this difference was modest. Underlying the age and race/ethnicity differences in therapy delivery are likely numerous considerations related to patient preferences, values, and financial resources, among other influences. In professional dental practice, a wide variety of provider, practice, and patient factors have been associated with delivery of preventive services, including patient socio-economic position.24
In this study, it was possible to use electronic patient records to assemble a large and inclusive study population and to define objective measures of CAMBRA implementation. Extensive investment in electronic records in dentistry has created new opportunities for clinical research.25,26 On the other hand, several key aspects of caries management were not as easily monitored via electronic charts, for example, the content of dietary counseling, development of a comprehensive management plan, and patient adherence to any therapeutic products provided. These elements also merit attention when evaluating the completeness with which the CAMBRA philosophy has been integrated into student-provided dental care and could be a focus of future studies.
While the percentage of patients to undergo documented caries risk assessment reached a near-universal level, the accuracy of student providers in assigning caries risk was not assessed in the present study. Student dentists may underestimate caries risk, particularly for patients presenting with active disease but with few presumptive risk factors or for patients with multiple risk factors but no current pathology.11 Despite the prospect of misclassification, however, baseline caries risk category was strongly related to the presence of cavitated and/or interproximal lesions at first follow-up examination in a previous evaluation of caries risk assessment practices at the same university.17 UCSF does not promote a rigid algorithm for risk estimation or treatment planning, allowing student providers the opportunity to exercise judgment and to develop critical thinking skills, basing the caries risk category on the balance between risk factors, protective factors and the weighting of disease indicators. Fostering critical thinking during professional training has been deemed essential to prepare graduates to incorporate current evidence into clinical decision-making and to adapt as the science of caries management evolves.27
In summary, more than a decade after initially implementing caries risk assessment in clinical training, documented caries risk assessment has become the standard of care for all adult patients at the UCSF student dental clinic. Assigned caries risk status was associated with the delivery of non-operative therapy, strongly suggesting that student providers incorporated caries risk when developing tailored caries management strategies with their patients. However, attaining the currently observed level of compliance with CAMBRA guidelines in clinical activities did not immediately follow didactic and clinical curricular shifts toward preventive practice, and remaining deficiencies in the percentage of high- and extreme-risk patients to receive non-operative anti-caries agents highlight an area for further improvement. Overcoming barriers to implementation of risk-based caries management in clinical training is both achievable and consistent with the role of dental education in expediting the transition toward preventive practice among dental professionals.
Acknowledgments
Thank you to Tom Ferris and Bing Espiritu of UCSF for assistance in data extraction from electronic patient records. Thank you to Amy J. Markowitz, JD of UCSF for helpful comments on the manuscript. Support was provided from the NIH National Center for Advancing Translational Sciences (KL2TR000143). The information presented is solely the responsibility of the authors and does not necessarily represent the official views of the NIH.
Support was provided from the NIH National Center for Advancing Translational Sciences (KL2TR000143). The information presented is solely the responsibility of the authors and does not necessarily represent the official views of the NIH.
Contributor Information
Dr. Benjamin W. Chaffee, Department of Preventive and Restorative Dental Sciences, School of Dentistry, University of California San Francisco.
Dr. John D. B. Featherstone, School of Dentistry, University of California San Francisco.
References
- 1.Krasse B. Caries risk: a practical guide for assessment and control. Chicago: Quintessence; 1985. [Google Scholar]
- 2.Brown JP. Developing clinical teaching methods for caries risk assessment: introduction to the topic and its history. J Dent Educ. 1995;59(10):928–31. [PubMed] [Google Scholar]
- 3.Fontana M, Young DA, Wolff MS. Evidence-based caries, risk assessment, and treatment. Dent Clin North Am. 2009;53(1):149,61, x. doi: 10.1016/j.cden.2008.10.003. [DOI] [PubMed] [Google Scholar]
- 4.Hallett KB. The application of caries risk assessment in minimum intervention dentistry. Aust Dent J. 2013;58(Suppl 1):26–34. doi: 10.1111/adj.12047. [DOI] [PubMed] [Google Scholar]
- 5.Garcia RI, Sohn W. The paradigm shift to prevention and its relationship to dental education. J Dent Educ. 2012;76(1):36–45. [PubMed] [Google Scholar]
- 6.Fontana M, Zero D. Bridging the gap in caries management between research and practice through education: the Indiana University experience. J Dent Educ. 2007;71(5):579–91. [PubMed] [Google Scholar]
- 7.Stoddard JW. Caries risk assessment used as a determinant for caries management and prevention. J Dent Educ. 1995;59(10):957–61. [PubMed] [Google Scholar]
- 8.Dodds MW, Suddick RP. Caries risk assessment for determination of focus and intensity of prevention in a dental school clinic. J Dent Educ. 1995;59(10):945–56. [PubMed] [Google Scholar]
- 9.Brown JP. A new curriculum framework for clinical prevention and population health, with a review of clinical caries prevention teaching in U.S. and Canadian dental schools. J Dent Educ. 2007;71(5):572–8. [PubMed] [Google Scholar]
- 10.Yorty JS, Walls AT, Wearden S. Caries risk assessment/treatment programs in U.S. dental schools: an eleven-year follow-up. J Dent Educ. 2011;75(1):62–7. [PubMed] [Google Scholar]
- 11.Teich ST, Demko C, Al-Rawi W, Gutberg T. Assessment of implementation of a CAMBRA-based program in a dental school environment. J Dent Educ. 2013;77(4):438–7. [PubMed] [Google Scholar]
- 12.Featherstone JD, Domejean-Orliaguet S, Jenson L, Wolff M, Young DA. Caries risk assessment in practice for age 6 through adult. J Calif Dent Assoc. 2007;35(10):703–7. 710–3. [PubMed] [Google Scholar]
- 13.Jenson L, Budenz AW, Featherstone JD, Ramos-Gomez FJ, Spolsky VW, Young DA. Clinical protocols for caries management by risk assessment. J Calif Dent Assoc. 2007;35(10):714–23. [PubMed] [Google Scholar]
- 14.Domejean-Orliaguet S, Gansky SA, Featherstone JD. Caries risk assessment in an educational environment. J Dent Educ. 2006;70(12):1346–54. [PubMed] [Google Scholar]
- 15.Jones DG. Teaching a new philosophy. J Calif Dent Assoc. 2000;28(1):13–5. [PubMed] [Google Scholar]
- 16.Featherstone JD, Adair SM, Anderson MH, Berkowitz RJ, Bird WF, Crall JJ, et al. Caries management by risk assessment: consensus statement, April 2002. J Calif Dent Assoc. 2003;31(3):257–69. [PubMed] [Google Scholar]
- 17.Domejean S, White JM, Featherstone JD. Validation of the CDA CAMBRA caries risk assessment--a six-year retrospective study. J Calif Dent Assoc. 2011;39(10):709–15. [PubMed] [Google Scholar]
- 18.Maupome G, Isyutina O. Dental students' and faculty members' concepts and emotions associated with a caries risk assessment program. J Dent Educ. 2013;77(11):1477–87. [PubMed] [Google Scholar]
- 19.Autio-Gold JT, Tomar SL. Dental students' opinions and knowledge about caries management and prevention. J Dent Educ. 2008;72(1):26–32. [PubMed] [Google Scholar]
- 20.Featherstone JD, White JM, Hoover CI, Rapozo-Hilo M, Weintraub JA, Wilson RS, et al. A randomized clinical trial of anticaries therapies targeted according to risk assessment (caries management by risk assessment) Caries Res. 2012;46(2):118–29. doi: 10.1159/000337241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Calderon SH, Gilbert P, Zeff RN, Gansky SA, Featherstone JD, Weintraub JA, et al. Dental students' knowledge, attitudes, and intended behaviors regarding caries risk assessment: impact of years of education and patient age. J Dent Educ. 2007;71(11):1420–7. [PubMed] [Google Scholar]
- 22.O'Donnell JA, Modesto A, Oakley M, Polk DE, Valappil B, Spallek H. Sealants and dental caries: insight into dentists' behaviors regarding implementation of clinical practice recommendations. J Am Dent Assoc. 2013;144(4):e24–30. doi: 10.14219/jada.archive.2013.0139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Domejean-Orliaguet S, Leger S, Auclair C, Gerbaud L, Tubert-Jeannin S. Caries management decision: influence of dentist and patient factors in the provision of dental services. J Dent. 2009;37(11):827–34. doi: 10.1016/j.jdent.2009.06.012. [DOI] [PubMed] [Google Scholar]
- 24.Brennan DS, Spencer AJ. The role of dentist, practice and patient factors in the provision of dental services. Community Dent Oral Epidemiol. 2005;33(3):181–95. doi: 10.1111/j.1600-0528.2005.00207.x. [DOI] [PubMed] [Google Scholar]
- 25.Filker PJ, Cook N, Kodish-Stav J. Electronic health records: a valuable tool for dental school strategic planning. J Dent Educ. 2013;77(5):591–7. [PubMed] [Google Scholar]
- 26.Liu K, Acharya A, Alai S, Schleyer TK. Using electronic dental record data for research: a data-mapping study. J Dent Res. 2013;92(7 Suppl):90S–6S. doi: 10.1177/0022034513487560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Guzman-Armstrong S, Warren JJ, Cunningham-Ford MA, von Bergmann H, Johnsen DC. Concepts in critical thinking applied to caries risk assessment in dental education. J Dent Educ. 2014;78(6):914–20. [PubMed] [Google Scholar]