Abstract
Risky sexual behavior (RSB) is a current public health concern affecting adolescents and young adults. Conduct disorder, cannabis use and decision making (DM) ability are interrelated constructs that are relevant to RSB; however, there is little research on the association of DM and RSB. Participants were 79 cannabis users assessed through self-report measures of RSB and mental health, and a timeline follow-back procedure for substance use. DM ability was assessed via the Iowa Gambling Task. We found that more conduct disorder symptoms accounted for unique variance in measures of overall RSB and an earlier initiation of oral sex, even when taking into account DM and cannabis use. Amount of cannabis use and DM ability moderated the relationships between number of conduct disorder symptoms and number of oral sex partners and age of initiation for vaginal sex. An increase in conduct disorder symptoms was associated with more oral sex partners when DM was poor and fewer partners when DM was better, however this relationship was only present at higher levels of cannabis use. Furthermore, when DM was poor, more conduct disorder symptoms predicted a younger age of initiation of vaginal sex, with the age decreasing as amount of cannabis use increased. Determining how DM influences RSB may assist in the identification of novel treatment approaches to reduce engagement in RSB.
Keywords: risky sexual behavior, conduct disorder, decision making, cannabis
Introduction
Risky sexual behavior (RSB), defined as sexual behavior without the use of protection (e.g., condom, birth control pills), casual sex, multiple sexual partners and sexual behavior under the influence of alcohol and drugs (Eaton et al., 2012), is prevalent among emerging adults. RSB can have a significant negative impact on an individual's quality of life and contributes to widespread public health problems. Engagement in RSB is more common among young adults compared to other ages and can result in sexually transmitted infections (STIs), including HIV, and unplanned pregnancies. Young adults comprise around half of new STIs diagnosed and 26% of new HIV diagnoses in the United States (CDC, 2011). Individuals who engage in sexual intercourse during early adolescence are more likely to contract a STI (Andersson-Ellström, Forssman, & Milsom, 1996; Coker et al., 1994; Kaestle, Halpern, Miller, & Ford, 2005), to engage more frequently in sexual behavior compared to their peers (Durbin et al., 1993), and to have multiple sexual partners (Andersson-Ellström et al., 1996; Coker et al., 1994; O'Donnell, O'Donnell, & Stueve, 2001). Moreover, adolescents and young adults often fail to consistently use condoms (Leichliter, Chandra, Liddon, Fenton, & Aral, 2007). The factors contributing to RSB are varied and complex, consisting of both psychosocial characteristics and environmental factors. Understanding factors that may contribute to engagement in RSB among emerging adults may help to identify and develop novel approaches for intervention and prevention. In this study, we examine the influence and interactions among cannabis use, conduct disorder symptoms, and decision making (DM) performance on various forms of RSB among young adult cannabis users.
Substance use is a well-known risk factor for engagement in RSB (Bellis et al., 2008; Brodbeck, Matter, & Moggi, 2006; Davis et al., 2009; Santelli, Brener, Lowry, Bhatt, & Zabin, 1998; Tapert, Aarons, Sedlar, & Brown, 2001; Toplak, Sorge, Benoit, West, & Stanovich, 2010). Although it is well documented that alcohol use is related to RSB, and in particular related to the multiple and casual sexual partners (Cooper, 2002), less is known about the relationship between cannabis use and RSB. Few studies have investigated how other factors known to be associated with RSB might interact with cannabis use to predict RSB. Individuals who use cannabis are more likely to engage in RSB, including decreased intentions to use protection, compared to non-users (Brodbeck et al., 2006). In addition, individuals who use cannabis have more sexual partners and engage in more HIV risk behavior than individuals who do not use cannabis (Bechara, Damasio, Damasio, & Lee, 1999; Bonar et al., 2014; Castilla, Barrio, Belza, & de la Fuente, 1999; Poulin & Graham, 2001; Staton et al., 1999). The importance of studying RSB among cannabis users is further underscored by the prevalence of its use among teens and young adults (SAMHSA, 2013) and mounting changes in state laws facilitating legal access (Cerdá, Wall, Keyes, Galea, & Hasin, 2012).
Conduct disorder is an externalizing psychiatric diagnosis that is characterized by a recurring pattern of behavior that violates rules, regulations or the rights of others. Some symptoms of conduct disorder include property destruction, lying, and stealing (APA, 2013) and it is a well-established predictor of RSB (Bryan, Schmiege, & Magnan, 2012; Flory, Molina, Pelham, Gnagy, & Smith, 2006; Ramrakha et al., 2007; Tubman, Gil, Wagner, & Artigues, 2003; Weber, Elfenbein, Richards, Davis, & Thomas, 1989). Individuals with conduct disorder are more likely to exchange sex for money and drugs and have more sexual partners compared to those without this diagnosis (Booth & Zhang, 1997; Flory et al., 2006). Additionally, males with a childhood diagnosis of conduct disorder are more likely to have sex with someone they have known less than twenty-four hours and to have an unplanned pregnancy compared to those without a childhood diagnosis of conduct disorder (Flory et al., 2006). The few studies to date that have examined interactions between conduct disorder and cannabis use report that both predict greater engagement in RSB (Bryan & Stallings, 2002), including absence of condom use during last sexual intercourse among juvenile delinquents who used cannabis prior to sexual engagement (Bryan, Schmiege, & Magnan, 2012).
DM, defined as how an individual makes a choice with ambiguous consequences that requires a tradeoff between reward and risk (Bechara, 2007), is a promising construct to examine in relation to RSB but has received little attention to date. Performance on measures of DM is subserved by brain circuits involving orbitofrontal cortex, anterior cingulate, insula, secondary somatosensory cortex, and hippocampus (Bechara, 2005; Bechara, Damasio, Damasio, & Anderson, 1994; Bechara, Damasio, & Damasio, 2000). Damage and dysfunction to these brain systems have been associated with disinhibited behavior and poor social comportment, including socially inappropriate sexual behavior (Spinella, 2007). Thus, it is possible that poor DM may be related to engagement in RSB or may moderate relationships between conduct disorder symptoms and RSB and between cannabis use and RSB. To our knowledge, only one study has specifically examined how DM influences RSB among cannabis users (Schuster, Crane, Mermelstein, & Gonzalez, 2012). The study sample consisted of young adult cannabis users (derived from the same larger study as the subjects in the current investigation) and results demonstrated that greater amounts of recent cannabis use was associated with more RSB, but only among those individuals with poorer DM performance, as measured by the Iowa Gambling Task. Similarly, other studies have found that more cannabis use is associated with more negative consequences from RSB, but only among those with poorer performance on the Balloon Analogue Risk Task (BART), which evaluates risk-taking in “real time” (Lejuez et al., 2002). Performance on the BART has been found to be associated with RSB among individuals in residential substance use treatment and typically developing young adults (Lejuez et al., 2002; Lejuez, Simmons, Aklin, Daughters, & Dvir, 2004).
Despite evidence to suggest that conduct disorder, cannabis use, and DM may all contribute to greater engagement in RSB, to our knowledge, no published studies have focused on examining these three variables and their interactions simultaneously. Number of conduct disorder symptoms, cannabis use, and DM abilities are likely interrelated. Compared to individuals with fewer symptoms of conduct disorder, those with more symptoms of conduct disorder engage in greater amounts of drug use and are more likely to meet criteria for a substance use disorder (Brown, Gleghorn, Schuckit, Myers, & Mott, 1996; Giancola, Mezzich, & Tarter, 1998; Knop et al., 2009; Molina, & Pelham, 2003; Molina, Bukstein, & Lynch, 2002), including cannabis dependence (Crowley, Macdonald, Whitmore, & Mikulich, 1998). Cannabis use and DM are associated as well. Individuals who use cannabis are more likely to perform poorly on DM tasks by choosing more risky options (Grant, Chamberlain, Schreiber, & Odlaug, 2012; Hermann et al., 2009; Whitlow et al., 2004). Similar to cannabis users, those with conduct disorder perform more poorly on DM tasks compared to those without conduct disorder (Fairchild et al., 2009). Given that number of conduct disorder symptoms, cannabis use, and DM abilities are associated, it is important to study the three variables together in relation to RSB in order to uncover how these variables interact with each other, as well as to understand how each variable may condition relationships between the other variables and RSB.
The current study was conducted to determine the influence of the amount of cannabis use, number of conduct disorder symptoms, and DM ability (as well as their interactions) on RSB among a sample of young adult cannabis users. Amount of cannabis use, conduct disorder symptoms, and DM were included as predictors in the model for two reasons. First, the current literature suggests these two variables are theoretically relevant to engagement in RSB and are known predictors, but are rarely examined simultaneously (revealing their unique variance) with regards to RSB. Second, few studies have assessed number of conduct disorder symptoms concurrently with cannabis use in relation to RSB. We hypothesized that all three variables would account for unique variance in RSB and number of conduct disorder symptoms would be the strongest predictor given current evidence. However, we anticipated that relationships between conduct disorder and RSB, as well as those between cannabis use and RSB will be moderated by DM performance. Individuals with poorer DM and high cannabis use will have a stronger relationship between conduct disorder symptoms and RSB compared to those with better DM and low cannabis use. Because all sexual behaviors are not equally risky (Varghese, Maher, Peterman, Branson, & Steketee, 2002), we explore the aforementioned relationships across a variety of sexual behaviors that vary in their risk (i.e., oral, vaginal and anal sex), as well as with other variables considered to be RSB (e.g., greater number of partners and earlier age of initiation).
Methods
Participants
Participants were 79 cannabis users who were 17 to 24 years old and recruited from the Chicago metropolitan area. All were subjects in a larger study on cannabis use and neurocognition (PI: RG). A small subset was recruited from a longitudinal study about the socio-emotional context of adolescent smoking (PI: Robin Mermelstein). The study was advertised through flyers posted throughout the community and through word of mouth. Demographic information for the sample of participants is located in Table 1.
Table 1.
Participant characteristics
| n = 79 | |
|---|---|
| Age | 20.8 (1.8) |
| Years of Education | 13.3 (1.7) |
| Years of Education (Mother) | 14.1 (2.9) |
| WTAR FSIQ | 100.9 (11.7) |
| Ethnicity/race (%) | |
| White (Hispanic) | 48 (15) |
| African-American | 38 |
| Other | 14 |
| Male (%) | 64 |
| Annual Household Income | 41K (40K) |
| Number of conduct disorder symptoms (MD, IQR) | 2.0 (1.0, 3.0) |
| Average amount per year of cannabis use (in grams; MD, IQR) | 144.33 (48.25, 490.00) |
| RSBQ-Total | 17.82 (13.4) |
| HRBS-Total | 7.6 (3.1) |
| Lifetime number of oral sex partners (MD, IQR) | 4.0 (2.0, 7.5) |
| Lifetime number of vaginal sex partners (MD, IQR) | 6.0 (3.0, 10.0) |
| Lifetime number of anal sex partners (MD, IQR) | 0.0 (0, 1) |
| Age of initiation of oral sex | 16.1 (2.0) |
| Age of initiation of Vaginal Sex | 16.0 (2.2) |
| Iowa Gambling Task (total net raw score) | 4.1 (27.8) |
| Iowa Gambling Task (T-score) | 45.2 (9.2) |
Note: All values are means and standard deviations unless otherwise specified. MD = median; IQR = interquartile range; FSIQ = full scale IQ; RSBQ = Risky Sexual Behavior Questionnaire; HRBS = HIV-Risk Behavior Scale; WTAR = Wechsler Test of Adult Reading.
Inclusion and exclusion criteria were chosen to minimize potential confounds that may influence neuropsychological performance. Inclusion criteria were having more than 8 years of education, being fluent in English, and having an estimated IQ at or greater than 75. All participants were cannabis users who identified cannabis as their drug of choice, used cannabis more than 200 times in their lifetime, used cannabis at least 4 times per week during their peak use, and had used cannabis in the 45 days prior to the lab visit. All participants reported some past engagement in sexual behavior. Participants were excluded if they were currently taking any psychotropic medications, had a history of developmental disorder, learning disability, or neurological injury or disorder. Individuals were excluded if they endorsed using other drugs (except for cannabis, nicotine, alcohol or hallucinogens) more than 10 times in their lifetime or at all during the 30 days prior to the lab visit (except for cannabis, nicotine, or alcohol). During the visit to the lab, all participants underwent rapid 10-panel urine toxicology testing (to test for cocaine, opiates, propoxyphene, phencyclidine, methadone, ecstasy, barbiturates, benzodiazepines, oxycodone, and THC; 10-panel Drug Check Cup; Express Diagnostics, Blue Earth, Minnesota) and participants were excluded if they tested positive for any substance other than cannabis. Seventy-eight percent of participants tested positive for THC, which had a 5-ng/ml limit of detection for 11-nor-Δ9-THC-9-COOH, and no participant tested positive for any other drugs. On an alcohol breath test (AlcoMate Prestige, Model AL6000; Palisades Park, NJ), participants did not evidence significantly elevated breath alcohol levels and none showed signs of intoxication. Participants were also excluded for a history of lifetime abuse or dependence for any other substance (except for nicotine or alcohol). No participant met criteria for current alcohol dependence and only 7 (9%) participants met criteria for current alcohol abuse. Only 3 (4%) participants met criteria for past alcohol dependence and 18 (23%) for past alcohol abuse. Participants were asked to abstain from cannabis use for at least 24 hours prior to their evaluation to minimize acute effects or withdrawal symptoms during testing.
Procedures
All study procedures and protocols were approved by the Institutional Review Board at University of Illinois at Chicago and at Florida International University. All participants gave informed consent or received parental consent and adolescent assent, when applicable, to participate in this study. The assessment for this cross-sectional study consisted of structured interviews, self-report questionnaires and neurocognitive measures which were obtained during that same visit to the laboratory. All participants received monetary compensation for participation in the project.
Measures
Demographics and Mental Health
Demographic information was collected on age, gender, race, years of education, household income, and parental education and income. Full scale IQ was estimated with the Wechsler Test of Adult Reading (WTAR; Wechsler, 2001). The Wender-Utah Rating Scale (WURS) was used to assess for symptoms suggestive of ADHD (Ward, Wender, & Reimherr, 1993). The Barratt-Impulsiveness Scale was used to assess personality dimensions of impulsiveness (Patton, Stanford, & Barratt, 1995). Symptoms of depression were assessed with the Beck Depression Inventory-2nd Edition (Beck, Steer, Ball, & Ranieri, 1996) and symptoms of anxiety were assessed with the Beck Anxiety Inventory (Beck & Steer, 1990). Mood disorders were also assessed with the Structured Clinical Interview for DSM-IV (SCID) which included assessment of both bipolar disorder and depression. A self-report screener based off of the SCID was used to assess for the number of conduct disorder symptoms (First, Spitzer, Gibbon, & Williams, 2002) for each participant and the total number was used to quantify number of conduct disorder symptoms in our analyses.
Substance Use
Detailed substance use history (number of times and amount of use for lifetime, past year, and past 30-days) was obtained from participants using the Drug Use History Questionnaire which was based off of timeline follow-back procedures (Gonzalez et al., 2004; Rippeth et al., 2004). Substance use was evaluated for 13 different classes of substances including alcohol, nicotine, cannabis, benzodiazepines, hallucinogens, opiates, cocaine and other substances. Average amount of cannabis use (in grams) per year (i.e., the total amount of lifetime cannabis use in grams divided by the number of years that the participant reported using cannabis) was used as a predictor in the analysis. We chose average amount of cannabis use per year as the index of use for this study as opposed to total amount of lifetime use, as we were more interested in the intensity of cannabis use among the participants and wanted to control for effects of duration of use on cumulative lifetime estimates.
Risky Sexual Behavior
Two self-report measures were used to assess RSB among the participants. The HIV Risk-Taking Behavior Scale (HRBS) measured overall HIV risk behavior using 12 multiple choice questions (Darke, Hall, Heather, Ward, & Wodak, 1991) including total number of sexual partners, use of dirty needles, and frequency of condom use or other forms of protection. As used in a study by Schuster and colleagues (2012), the Risky Sexual Behavior Questionnaire (RSBQ) is based on the AIDS Risk Behavior Assessment (Donenberg, Emerson, Bryant, Wilson, & Weber-Shifrin, 2001) and is a detailed interview about the individual's past sexual history. Responses from the RSBQ were quantified to generate four subscales: 1) drug use interfering with safe-sex practices, 2) frequency of protection or prevention methods, 3) sexual risk (e.g., number of partners), and 4) consequences from RSB (e.g., STIs and unplanned pregnancies). A composite was generated based on the sum of the three subscales that indicated involvement in RSBs (i.e., sexual risk, frequency of protection and consequences). Amongst other items, RSBQ includes questions about total number of oral, vaginal and anal sex partners as well as age of initiation of oral, vaginal and anal sex. Analyses were run with each of the dependent variables (i.e., RSBQ-total, HRBS-total, and age of initiation and number of partners separately for oral, vaginal and anal sex).
Decision Making Task
The Iowa Gambling Task (IGT; Bechara et al., 1994) was used to assess DM. The IGT was developed to assess DM under conditions of ambiguous risk and was initially tested to capture impairments among individuals with lesions in the orbitofrontal cortex. Participants choose between four decks of cards in which the participant will win some money and sometimes lose money as well. Directions given to the participants included that some decks are better than others. More choices of “good decks” will yield a positive total while more choices from the “bad decks” will yield a negative total at the end of the game. Substance abusers perform more poorly on the IGT compared to healthy controls on a variety of substances (Bechara et al., 2001; Gonzalez, Bechara, & Martin, 2007; Grant, Contoreggi, & London, 2000). Our variable of interest was the total net score (calculated as choices from good decks minus choices from bad decks); we used published demographically corrected T-scores for our analyses (Bechara, 2007).
Statistical Analysis
All analyses were conducted in SPSS 19.0 using multiple linear regression or negative binomial regression (Coxe, West, & Aiken, 2009). When considering relevant covariates, sex and race/ethnicity were not included in the analyses based on results of recent large epidemiological studies that suggests that there are few gender and racial or ethnic differences in the prevalence of cannabis use (Johnston et al., 2014) or engagement in RSB among young adults (Kann et al., 2014). The effects of age as a covariate were examined in analyses that employed total number of partners, RSBQ-total, and HRBS-total as dependent variables. Age was not included as a covariate for age of initiation for specific sexual behaviors. Across all analyses, predictor variables (all analyzed continuously) included total number of conduct disorder symptoms, average amount of cannabis use per year (in grams) and DM performance, as well as all two-way and three-way interactions. All independent variables were mean-centered. Separate regression analyses were conducted for each dependent variable. The first analysis examined relationships among our independent variables and overall RSB, using RSBQ-total and HRBS-total as dependent variables in two separate multiple linear regressions. The second set of analyses employed total number of partners for the various sexual behaviors as dependent variables, with the same independent variables. Due to the positively skewed distributions of number of sexual partners for oral, vaginal, and anal sex, these analyses were conducted using negative binomial regression (Coxe et al., 2009). Finally, we examined the influence of the same set of independent variables on the age of initiation across the various sexual behaviors queried. For the latter, data were included only for those participants that endorsed engaging in the particular behavior (oral, n = 62 and vaginal, n = 62). Age of initiation of anal sex was not examined due to the few participants reporting this behavior (n = 20).
Intercorrelations among independent variables was low (< .34), indicating absence of multicolinearity. Several approaches were used to reduce the influence of potential outliers. First, negative binomial regressions were used for count outcome data (number of partners for oral, vaginal and anal sex). Second, we used bootstrapped regression models. Third, the cannabis use variable underwent square-root transformation for our analyses. Finally, DFBETAS were analyzed for all statistically significant results and revealed three potential outliers (DFBETAS ranging from 1.04 – 1.48) among the various analyses conducted. In these instances, models were run again after Winsorizing values for a specific outlier. In all instances the same analyses remained statistically significant after Winsorization.
For all significant interactions, a simple slope difference test was conducted to determine the change in RSB associated with a one symptom increase in conduct disorder symptoms at varying levels of cannabis use and DM ability (Aiken & West, 1991). Levels of cannabis use were set to correspond to one standard deviation above the mean (labeled as “high” cannabis use), one standard deviation below the mean (labeled as “low” cannabis use) and to the mean of the sample (labeled as “medium” cannabis use). For the current sample, the levels of cannabis use were 746, 327 and 7 grams per year for high, medium and low, respectively, which correspond to approximately 373, 164, and 3.5 joints per year. Levels of IGT performance were set at one standard deviation above the mean (labeled as “better” DM) or one standard deviation below the mean (labeled as “poorer” DM). For the current sample, this corresponded to a T-score of 54.4 and 36, respectively. Post-hoc analyses were run on each significant interaction to determine the level of significance of the independent variables by simple slope difference tests. Only when the three-way interaction was not significant were two-way interactions or main effects examined and interpreted.
Results
Overall HIV-Risk Behavior
The three-way interactions between number of conduct disorder symptoms, amount of cannabis use on RSBQ-total (p = .33) and HRBS-total (p = .25) were not significant. In addition, there were no significant two-way interactions observed; however, number of conduct disorder symptoms predicted RSBQ-total, β = 2.89 (.45), eβ = 17.94, SE = .92, t (71) = 3.14, p < .01, and HRBS-total, β = .54 (.38), eβ = 1.71, SE = .22, t (71) = 2.48, p = .02. Specifically, an increase in one conduct disorder symptom predicted an increase of 2.89 and .54 in RSBQ-total score and HRBS-total score, respectively.
Number of Partners for Different Sexual Behaviors
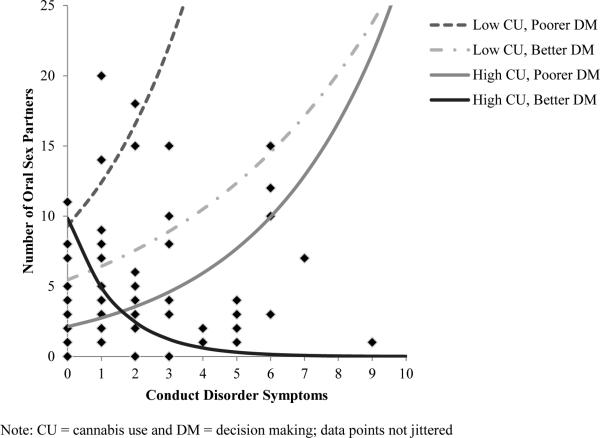
Negative binomial regressions were conducted to determine if interactions among conduct disorder symptoms, amount of cannabis use and DM or the main effects of these variables predicted the number of partners for oral, vaginal, and anal sex. A significant three-way interaction was observed between number of conduct disorder symptoms, amount of cannabis use and DM performance when predicting number of partners for oral sex (p = .003), but not when predicting vaginal (p = .73) or anal (p = .10) sex. However, the model for number of anal sex partners did not produce interpretable results due to a non-positive definite Hessian matrix, which was likely related to the extremely low variance of the outcome variable. The significant three-way interaction for number of oral sex partners remained significant when age was added as a covariate (p = .001).
The significant three-way interaction for number of oral sex partners was followed up with a simple slope difference test (Figure 1), which revealed that with poorer DM performance, an increase in conduct disorder symptoms was associated with more oral sex partners for those with high (β = .31, eβ = 1.36, SE = .11, Wald's χ2 (71) = 7.46, p = .006) and medium levels of cannabis use (β = .28 , eβ = 1.32, SE = .10, Wald's χ2 (71) = 7.00, p = .008). In contrast, we were surprised to see that at better DM performance, more conduct disorder symptoms were associated with fewer oral sex partners for those with high (β = −.74 , eβ = .48, SE = .25, Wald's χ2 (71) = 8.84, p = .003) and medium levels of cannabis use (β = −.27 , eβ = .76, SE = .12, Wald's χ2 (71) = 4.79, p = .029). In other words, at medium and high levels of cannabis use, a greater number of conduct disorder symptoms was associated with opposing relationships with number of oral sex partners that were based on DM performance. At poorer levels of DM, more conduct disorder symptoms were associated with more oral sex partners, and at higher levels of DM, more conduct disorder symptoms were associated with fewer oral sex partners. Relationships between conduct disorder symptoms and number of oral sex partners were not significant at low levels of cannabis use. Although a significant 2-way interaction was observed between cannabis use and DM performance when predicting number of vaginal sex partners, the follow-up simple slope analyses were not significant.
Figure 1.
Simple slopes of the effect of conduct disorder symptoms on number of oral sex partners
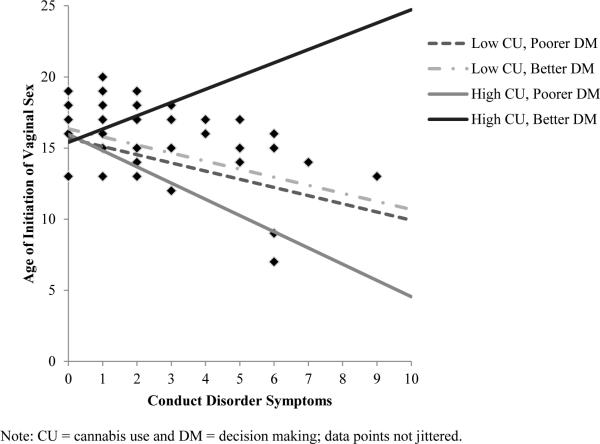
Exploratory Analyses on Age of Initiation for Different Sexual Behaviors
Because of the few participants reporting anal sex (n = 20), analyses examining age of initiation of various sexual behaviors focused only on onset of vaginal and oral sex. A significant three-way interaction between number of conduct disorder symptoms, amount of cannabis use, and DM performance was observed when predicting age of initiation for vaginal (p = .018), but not oral (p = .126) sex. Two-way interactions were not significant for age of initiation for oral sex. However, number of conduct disorder symptoms was significant in predicting age of initiation for oral sex, with an increase of one conduct disorder symptom decreasing the age of initiation for oral sex by .33 years, β = −.33 (−.34), eβ = .72 , SE = .15, t(71) = −2.19, p = .03.
A simple slope difference test was conducted on age of initiation for vaginal sex. When DM was poor, each additional conduct disorder symptom was associated with a .86 to 1.12 year decrease in age of initiation at medium (β = −.86 (−.80), eβ = .42 , SE = .23, t(71) = −3.74, p < .01), and high levels of use (β = −1.12 (−1.04), eβ = .33, SE = .23, t(71) = −4.94, p < .01), with effect sizes growing larger with more cannabis use. In other words, at poor DM levels, more conduct disorder symptoms was associated with younger age of initiation for vaginal sex. At the levels of poor DM and low cannabis use, conduct disorder symptoms were not related to age of vaginal sex initiation. At the better level of DM, there were no significant relationships between number of conduct disorder symptoms and age of vaginal sex initiation regardless of cannabis use level (refer to Figure 2). Refer to Table 2 for all regression coefficients for the analysis and Table 3 for simple slope difference tests of the regression coefficients for the significant three-way interactions.
Figure 2.
Simple slopes of the effect of conduct disorder symptoms on age of initiation of vaginal sex
Table 2.
Unstandardized regression coefficients (if available standardized regression coefficients in parenthesis) of main and interaction effects predicting different RSB outcomes
| RSBQ-Total | HRBS-Total | Age of Vaginal Sex Initiation | Age of Oral Sex Initiation | Number of Vaginal Sex Partners (NB) | Number of Oral Sex Partners (NB) | |
|---|---|---|---|---|---|---|
| CD | 2.89 (.45)** | 0.54 (0.35)* | −0.34 (−0.32)* | −0.33 (−0.34)* | 0.08 | 0.00 |
| DM | 0.04 (.02) | −0.06 (−0.16) | 0.00 (0.01) | −0.04 (−0.16) | 0.02 | 0.03 |
| CU | 0.07 (.06) | −0.04 (−0.12) | −0.02 (−0.08) | 0.03 (0.13) | 0.02 | −0.02 |
| CD × DM | 0.03 (.26) | 0.01 (0.04) | 0.06 (0.41)** | 0.03 (0.27) | 0.00 | −0.03** |
| CD × CU | 0.19 (.25) | 0.00 (0.00) | 0.02 (0.16) | 0.02 (0.19) | 0.01 | −0.02* |
| CU × DM | 0.03 (.26) | 0.00 (−0.00) | −0.00 (−0.14) | −0.01 (−0.30) | 0.00* | 0.01* |
| CD × CU × DM | 0.01 (.16) | 0.00 (0.00) | 0.01 (0.47)* | 0.00 (0.32) | 0.00 | −0.00** |
Note: CD = conduct disorder, CU = cannabis use and DM = DM, NB = negative binomial analysis.
p-value < .05
p-value <.01
Table 3.
Summary of unstandardized regression coefficients (if available standardized regression coefficients in parenthesis) for simple slope difference tests of conduct disorder symptoms on RSB based on level of cannabis use and DM ability
| Low Cannabis Use | Medium Cannabis Use | High Cannabis Use | |
|---|---|---|---|
| Total Number of Oral Partners | |||
| Poor DM | 0.25 | 0.28** | 0.31** |
| Better DM | 0.20 | −0.27* | −0.74** |
| Age of Initiation for Vaginal Sex | |||
| Poor DM | −0.61 (−0.57) | −0.86 (−0.80)** | −1.12(−1.04)** |
| Better DM | −0.53(−0.49) | 0.19 (0.17) | 0.90 (0.84) |
p-value < .05
p-value < .01
Discussion
RSB, especially among adolescents and young adults, is a pressing concern given that this age group constitutes approximately 50% of the individuals who contract an STI within a given year (Control, 2011). The current study was conducted to assess the associations and interactions of three theoretically relevant variables (i.e., cannabis use, conduct disorder symptoms, and DM performance) on various indicators of RSB with the goal of identifying further targets for intervention. Generally, based on the existing literature and our prior work, we anticipated significant associations between all three variables and RSB, as well as moderating effects of DM on relationships between cannabis use and conduct disorder symptoms on RSB. However, we anticipated that relationships may differ based on the specific RSB examined. Our hypotheses were partially supported by our results. We found significant relationships only between conduct disorder symptoms and measures of overall RSB. Symptoms of conduct disorder were also directly related to a younger age of initiation for vaginal sex. Thus, only symptoms of conduct disorder appeared to have direct relationships with any measure of RSB when controlling for cannabis use and DM performance. Nonetheless, levels of cannabis use and DM were not inconsequential. Specifically, only at a high and medium level of cannabis use did we find relationships between conduct disorder symptoms and number of oral sex partners, and this relationship was contingent on DM performance. More conduct disorder symptoms was associated with more oral sex partners among those with poorer DM, but the opposite was the case among those with better DM. Complex interactions among our independent variables were also observed for age of initiation of vaginal sex. Vaginal sex was initiated at earlier ages with increasing conduct disorder symptoms, but only among those with poorer DM ability. The magnitude of this effect appeared to increase with higher levels of cannabis use.
Relationships between conduct disorder symptoms and RSB (including earlier sexual debut) are well established (Flory et al., 2006; Morris, Baker, Valentine, & Pennisi, 1998; Timmermans, Van Lier, & Koot, 2008; Woodward & Fergusson, 1999). However, few studies have examined how cannabis use and laboratory measures of DM influence the association between conduct disorder symptoms and RSB. Seminal work by others has revealed that greater levels of cannabis use in individuals with conduct disorder is associated with steeper declines in condom use over time (Bryan et al., 2012). However, we are aware of only one other study that investigated associations between neurocognitive performance (assessed via a laboratory task that captures real-time performance) and cannabis use on RSB, and it revealed that more cannabis use was associated with more RSB only among individuals with poorer DM (Schuster et al., 2012). The significant interactions in the current study are consistent with previous work suggesting that increases in conduct disorder symptoms are associated with some RSBs. Although these variables have never been evaluated at the same time in a study, the findings that more cannabis use and poorer DM is associated with some sexual behavior is consistent with previous research on these factors.
One possible mechanism underlying the moderating effects of DM and cannabis use on the relationship between number of conduct disorder symptoms and age of initiation for vaginal sex and number of oral sex partners could be explained by the two subtypes of conduct disorder (i.e. childhood onset and adolescent onset subtypes). Childhood onset is diagnosed when symptoms occur before the age of 10 while adolescent onset is diagnosed when symptoms occur after age (APA, 2013). Individuals diagnosed with childhood onset conduct disorder typically have worse outcomes, for example, greater substance dependence, more criminal offending (Moffitt, Caspi, Harrington, & Milne, 2002) and greater neurocognitive impairments compared to individuals with adolescent onset (Moffitt & Caspi, 2001; Raine et al., 2005). Perhaps the relationship between conduct disorder and RSB moderated by DM and cannabis use may be due in part to individuals with childhood onset conduct disorder. Since those with childhood onset have more neurocognitive impairments and greater substance use, it may be the case that this relationship is only apparent for those with childhood onset. This theory is speculative and will need future studies to determine the association between the subtypes of conduct disorder and the variables of interest in this study. Additionally, this study did not examine whether participants met full criteria for conduct disorder, as our study only evaluated number of conduct disorder symptoms. Future research will need to examine if a diagnosis of conduct disorder yields similar findings.
Only number of conduct disorder symptoms predicted overall RSB scores regardless of the level of cannabis use and DM performance. As discussed previously, conduct disorder is characterized by risky behavior like fighting, stealing and fire-setting. Those with a conduct disorder diagnosis perform more poorly on measures of risk-taking via neurocognitive laboratory tasks (Crowley, Raymond, Mikulich-Gilbertson, Thompson, & Lejuez, 2006). The relationship between conduct disorder and overall RSB might be explained by a vulnerability towards risk-taking behavior among individuals with conduct disorder. It may be that those with conduct disorder symptoms who engage in RSB are aware of the risk and choose to proceed anyways. Thus, conduct disorder symptoms appear to directly influence overall RSB. However, the influence of conduct disorder on more specific measures of RSBs (i.e., oral and vaginal sex) is conditioned by DM and amount of cannabis use, at least in this sample of cannabis users. It may be that the willingness to take risk for sexual pleasure increases as a consequence of conduct disorder severity.
Our results should be taken in light of some considerations. First, some of our analyses suffered from relatively small sample sizes, namely those examining age of initiation. Analyses on overall sexual risk and number of partners were able to take into account all participants in the sample, but analyses of age of initiation only included those individuals who had endorsed engaging in a particular behavior. Thus, we had less power to detect significant effects in the latter; however, the sample sizes are adequate for our analyses and would only present a conservative bias in detecting small effects (with the exception of age of initiation of anal sex). Relatedly, there was a very narrow range reported for number of anal sex partners in this sample, which therefore yielded uninterpretable results in one instance. Second, the study sample only included individuals who primarily used cannabis while non-cannabis users were not included. Although this limits generalizing to young adults who may primarily use other substances or those who do not use any cannabis, this was by design, as our goal was to better understand factors that influence RSB among this particular population. However, consistent with the results of others (Bryan et al., 2012), it is worth noting that engagement in RSB among participants in our sample, were somewhat elevated compared to normative samples. For example, among normative samples of young adults (age 18-22), the mean number of vaginal sex partners is 4.45 (Guo, Tong, Xie, & Lange, 2007); however, the mean number of vaginal sex partners in our sample is 7.76. Third, it is worth noting that DM performance was captured in “real-time” during the study visit, whereas measures of RSB, conduct disorder symptoms, and cannabis use were based on retrospective self-report. Additionally, data were not collected on whether participants used cannabis at the same time as engaging in a particular sexual behavior, thus we were unable to determine if cannabis use and RSB occurred concurrently. Fourth, number of conduct disorder symptoms was used as the predictor variable and information about the age of onset of these symptoms or whether the participant met diagnostic criteria for the disorder was not obtained. Future research on the neurocognitive predictors of RSB should concentrate on replicating these findings with a longitudinal design among different populations, such as younger adolescents or a clinical sample of individuals with diagnosed conduct disorder. Determining the neurocognitive predictors at younger ages will have important implications for prevention because determining whether poor DM could predict if someone is more likely to engage in RSB and subsequently if changing these maladaptive patterns of DM could prevent negative consequences. Nonetheless, our results still present valuable information about the association of conduct disorder symptoms and RSB and the moderating effects of cannabis use and DM ability.
The findings of this study have several clinical and policy implications. For example, we found that number of conduct disorder symptoms was the only predictor of overall RSB among the variables we examined. This suggests that interventions focusing on reducing delinquency may have a greater impact on reducing RSB than those focused on reducing cannabis use or improving DM. However, the recommendations may be different if an intervention is designed to target a specific RSB (i.e., oral or vaginal sex) or those aimed to delay age of engagement in specific RSBs among more regular cannabis users. Under those circumstances, strategies for improving DM may help to minimize the impact of conduct disorder symptoms on RSB among cannabis users. A pilot study implementing Goal Management Training and Mindfulness in combination has successfully improved executive functions, for example DM assessed by the IGT, in a sample of abstinent drug abusers (Alfonso, Caracuel, Delgado-Pastor, & Verdejo-García, 2011). Behavioral treatments targeting reduction in conduct disorder symptoms and cannabis use might also prove beneficial in reducing STIs and unplanned pregnancies among youth. Neurocognitive performance may be one assessment tool in an assessment battery to evaluate those who are at risk for engaging in RSB. DM abilities is one potential way to distinguish those who will engage in more risk behavior (RSB or experimenting with other drugs) or are more likely to continue engagement in risk behavior after adolescence, a time in which engagement in risky behavior is seen in greater amounts and perceived as normal (Steinberg, 2004).
Acknowledgements
This work was supported by grant K23 DA023560, R01 DA031176 and R01 DA033156 (PI: Gonzalez) from the National Institute on Drug Abuse. We would also like to acknowledge the contributions of Robin Mermelstein and Kathleen R. Diviak to this research study.
References
- Aiken LS, West SG. Multiple regression: Testing and interpreting interactions. Sage; 1991. [Google Scholar]
- Alfonso JP, Caracuel A, Delgado-Pastor LC, Verdejo-García A. Combined goal management training and mindfulness meditation improve executive functions and decision-making performance in abstinent polysubstance abusers. Drug and Alcohol Dependence. 2011;117(1):78–81. doi: 10.1016/j.drugalcdep.2010.12.025. [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association Diagnostic and statistical manual of mental disorders. 2013.
- Andersson-Ellström A, Forssman L, Milsom I. Age of sexual debut related to life-style and reproductive health factors in a group of Swedish teenage girls. Acta Obstetricia et Gynecologica Scandinavica. 1996;75(5):484–489. doi: 10.3109/00016349609033359. [DOI] [PubMed] [Google Scholar]
- Bechara A. Decision making, impulse control and loss of willpower to resist drugs: a neurocognitive perspective. Nature Neuroscience. 2005;8(11):1458–1463. doi: 10.1038/nn1584. [DOI] [PubMed] [Google Scholar]
- Bechara A. Iowa Gambling Task: Professional Manual. Psychological Assessment Rescources, Inc.; 2007. [Google Scholar]
- Bechara A, Damasio AR, Damasio H, Anderson SW. Insensitivity to future consequences following damage to human prefrontal cortex. Cognition. 1994;50(1):7–15. doi: 10.1016/0010-0277(94)90018-3. [DOI] [PubMed] [Google Scholar]
- Bechara A, Damasio H, Damasio AR. Emotion, decision making and the orbitofrontal cortex. Cerebral Cortex. 2000;10(3):295–307. doi: 10.1093/cercor/10.3.295. [DOI] [PubMed] [Google Scholar]
- Bechara A, Damasio H, Damasio AR, Lee GP. Different contributions of the human amygdala and ventromedial prefrontal cortex to decision-making. The Journal of Neuroscience. 1999;19(13):5473–5481. doi: 10.1523/JNEUROSCI.19-13-05473.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bechara A, Dolan S, Denburg N, Hindes A, Anderson SW, Nathan PE. Decision-making deficits, linked to a dysfunctional ventromedial prefrontal cortex, revealed in alcohol and stimulant abusers. Neuropsychologia. 2001;39(4):376–389. doi: 10.1016/s0028-3932(00)00136-6. [DOI] [PubMed] [Google Scholar]
- Beck AT, Steer RA. Manual for the Beck anxiety inventory. Psychological Corporation; San Antonio, TX: 1990. [Google Scholar]
- Beck AT, Steer RA, Ball R, Ranieri WF. Comparison of Beck Depression Inventories-IA and-II in psychiatric outpatients. Journal of Personality Assessment. 1996;67(3):588–597. doi: 10.1207/s15327752jpa6703_13. [DOI] [PubMed] [Google Scholar]
- Bellis MA, Hughes K, Calafat A, Juan M, Ramon A, Rodriguez JA, Phillips-Howard P. Sexual uses of alcohol and drugs and the associated health risks: a cross sectional study of young people in nine European cities. BMC Public Health. 2008;8(1):155. doi: 10.1186/1471-2458-8-155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bonar EE, Cunningham RM, Chermack ST, Blow FC, Barry KL, Booth BM, Walton MA. Prescription drug misuse and sexual risk behaviors among adolescents and emerging adults. Journal of Studies on Alcohol and Drugs. 2014;75(2):259. doi: 10.15288/jsad.2014.75.259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Booth RE, Zhang Y. Conduct disorder and HIV risk behaviors among runaway and homeless adolescents. Drug and Alcohol Dependence. 1997;48(2):69–76. doi: 10.1016/s0376-8716(97)00113-0. [DOI] [PubMed] [Google Scholar]
- Brodbeck J, Matter M, Moggi F. Association between cannabis use and sexual risk behavior among young heterosexual adults. AIDS and Behavior. 2006;10(5):599–605. doi: 10.1007/s10461-006-9103-9. [DOI] [PubMed] [Google Scholar]
- Brown SA, Gleghorn A, Schuckit MA, Myers MG, Mott MA. Conduct disorder among adolescent alcohol and drug abusers. Journal of Studies on Alcohol and Drugs. 1996;57(3):314. doi: 10.15288/jsa.1996.57.314. [DOI] [PubMed] [Google Scholar]
- Bryan A, Stallings MC. A case control study of adolescent risky sexual behavior and its relationship to personality dimensions, conduct disorder, and substance use. Journal of Youth and Adolescence. 2002;31(5):387–396. [Google Scholar]
- Bryan AD, Schmiege SJ, Magnan RE. Marijuana use and risky sexual behavior among high-risk adolescents: trajectories, risk factors, and event-level relationships. Developmental Psychology. 2012;48(5):1429. doi: 10.1037/a0027547. [DOI] [PubMed] [Google Scholar]
- Castilla J, Barrio G, Belza MJ, de la Fuente L. Drug and alcohol consumption and sexual risk behaviour among young adults: results from a national survey. Drug and Alcohol Dependence. 1999;56(1):47–53. doi: 10.1016/s0376-8716(99)00008-3. [DOI] [PubMed] [Google Scholar]
- Center for Disease Control and Prevention HIV Survillence Report, 2009. 2011;21 [Google Scholar]
- Cerdá M, Wall M, Keyes KM, Galea S, Hasin D. Medical marijuana laws in 50 states: investigating the relationship between state legalization of medical marijuana and marijuana use, abuse and dependence. Drug and Alcohol Dependence. 2012;120(1):22–27. doi: 10.1016/j.drugalcdep.2011.06.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coker AL, Richter DL, Valois RF, McKeown RE, Garrison CZ, Vincent ML. Correlates and consequences of early initiation of sexual intercourse. Journal of School Health. 1994;64(9):372–377. doi: 10.1111/j.1746-1561.1994.tb06208.x. [DOI] [PubMed] [Google Scholar]
- Cooper ML. Alcohol use and risky sexual behavior among college students and youth: Evaluating the evidence. Journal of Studies on Alcohol and Drugs. 2002;(14):101. doi: 10.15288/jsas.2002.s14.101. [DOI] [PubMed] [Google Scholar]
- Coxe S, West SG, Aiken LS. The analysis of count data: A gentle introduction to Poisson regression and its alternatives. Journal of Personality Assessment. 2009;91(2):121–136. doi: 10.1080/00223890802634175. [DOI] [PubMed] [Google Scholar]
- Crowley TJ, Macdonald MJ, Whitmore EA, Mikulich SK. Cannabis dependence, withdrawal, and reinforcing effects among adolescents with conduct symptoms and substance use disorders. Drug and Alcohol Dependence. 1998;50(1):27–37. doi: 10.1016/s0376-8716(98)00003-9. [DOI] [PubMed] [Google Scholar]
- Crowley TJ, Raymond KM, Mikulich-Gilbertson SK, Thompson LL, Lejuez CW. A risk-taking “set” in a novel task among adolescents with serious conduct and substance problems. Journal of the American Academy of Child & Adolescent Psychiatry. 2006;45(2):175–183. doi: 10.1097/01.chi.0000188893.60551.31. [DOI] [PubMed] [Google Scholar]
- Darke S, Hall W, Heather N, Ward J, Wodak A. The reliability and validity of a scale to measure HIV risk-taking behaviour among intravenous drug users. AIDS. 1991;5(2):181–185. doi: 10.1097/00002030-199102000-00008. [DOI] [PubMed] [Google Scholar]
- Davis KC, George WH, Norris J, Schacht RL, Stoner SA, Hendershot CS, Kajumulo KF. Effects of alcohol and blood alcohol concentration limb on sexual risk-taking intentions. Journal of Studies on Alcohol and Drugs. 2009;70(4):499. doi: 10.15288/jsad.2009.70.499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Donenberg GR, Emerson E, Bryant FB, Wilson H, Weber-Shifrin E. Understanding AIDS-risk behavior among adolescents in psychiatric care: Links to psychopathology and peer relationships. Journal of the American Academy of Child & Adolescent Psychiatry. 2001;40(6):642–653. doi: 10.1097/00004583-200106000-00008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Durbin M, DiClemente RJ, Siegel D, Krasnovsky F, Lazarus N, Camacho T. Factors associated with multiple sex partners among junior high school students. Journal of Adolescent Health. 1993;14(3):202–207. doi: 10.1016/1054-139x(93)90006-b. [DOI] [PubMed] [Google Scholar]
- Eaton DK, Kann L, Kinchen S, Shanklin S, Flint KH, Hawkins J, Chyen D. Youth risk behavior surveillance-United States, 2011. MMWR Surveill Summ. 2012;61(4):1–162. [PubMed] [Google Scholar]
- Fairchild G, van Goozen SH, Stollery SJ, Aitken MR, Savage J, Moore SC, Goodyer IM. Decision making and executive function in male adolescents with early-onset or adolescence-onset conduct disorder and control subjects. Biological Psychiatry. 2009;66(2):162–168. doi: 10.1016/j.biopsych.2009.02.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- First MB, Spitzer RL, Gibbon M, Williams JB. Structured clinical interview for DSM-IV-TR axis I disorders, research version, patient edition. Biometrics Research, New York State Psychiatric Institute; New York: 2002. [Google Scholar]
- Flory K, Molina BSG, Pelham WE, Gnagy E, Smith B. Childhood ADHD predicts risky sexual behavior in young adulthood. Journal of Clinical Child and Adolescent Psychology. 2006;35(4):571–577. doi: 10.1207/s15374424jccp3504_8. [DOI] [PubMed] [Google Scholar]
- Giancola PR, Mezzich AC, Tarter RE. Disruptive, delinquent and aggressive behavior in female adolescents with a psychoactive substance use disorder: Relation to executive cognitive functioning. Journal of Studies on Alcohol and Drugs. 1998;59(5):560. doi: 10.15288/jsa.1998.59.560. [DOI] [PubMed] [Google Scholar]
- Gonzalez R, Bechara A, Martin EM. Executive functions among individuals with methamphetamine or alcohol as drugs of choice: preliminary observations. Journal of Clinical and Experimental Neuropsychology. 2007;29(2):155–159. doi: 10.1080/13803390600582446. [DOI] [PubMed] [Google Scholar]
- Gonzalez R, Rippeth JD, Carey CL, Heaton RK, Moore DJ, Schweinsburg BC, Grant I. Neurocognitive performance of methamphetamine users discordant for history of marijuana exposure. Drug and Alcohol Dependence. 2004;76(2):181–190. doi: 10.1016/j.drugalcdep.2004.04.014. [DOI] [PubMed] [Google Scholar]
- Grant JE, Chamberlain SR, Schreiber L, Odlaug BL. Neuropsychological deficits associated with cannabis use in young adults. Drug and Alcohol Dependence. 2012;121(1):159–162. doi: 10.1016/j.drugalcdep.2011.08.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grant S, Contoreggi C, London ED. Drug abusers show impaired performance in a laboratory test of decision making. Neuropsychologia. 2000;38(8):1180–1187. doi: 10.1016/s0028-3932(99)00158-x. [DOI] [PubMed] [Google Scholar]
- Guo G, Tong Y, Xie C-W, Lange LA. Dopamine transporter, gender, and number of sexual partners among young adults. European Journal of Human Genetics. 2007;15(3):279–287. doi: 10.1038/sj.ejhg.5201763. [DOI] [PubMed] [Google Scholar]
- Hermann D, Leménager T, Gelbke J, Welzel H, Skopp G, Mann K. Decision making of heavy cannabis users on the Iowa Gambling Task: stronger association with THC of hair analysis than with personality traits of the Tridimensional Personality Questionnaire. European Addiction Research. 2009;15(2):94–98. doi: 10.1159/000189788. [DOI] [PubMed] [Google Scholar]
- Johnston LD, O'Malley PM, Bachman JG, Schulenberg JE, Miech RA. Monitoring the future national survey results on drug use, 1975-2013: Volume II, college students and adults ages 19-55. Institute for Social Research, The University of Michigan; Ann Arbor: 2014. p. 424. [Google Scholar]
- Kaestle CE, Halpern CT, Miller WC, Ford CA. Young age at first sexual intercourse and sexually transmitted infections in adolescents and young adults. American Journal of Epidemiology. 2005;161(8):774–780. doi: 10.1093/aje/kwi095. [DOI] [PubMed] [Google Scholar]
- Kann L, Kinchen S, Shanklin SL, Flint KH, Kawkins J, Harris WA, Chyen D. Youth risk behavior surveillance-United States, 2013. MMWR: Surveillance Summaries. 2014;63(SS-04):1–168. [PubMed] [Google Scholar]
- Knop J, Penick EC, Nickel EJ, Mortensen EL, Sullivan MA, Murtaza S, Gabrielli WF., Jr Childhood ADHD and conduct disorder as independent predictors of male alcohol dependence at age 40. Journal of Studies on Alcohol and Drugs. 2009;70(2):169. doi: 10.15288/jsad.2009.70.169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leichliter JS, Chandra A, Liddon N, Fenton KA, Aral SO. Prevalence and correlates of heterosexual anal and oral sex in adolescents and adults in the United States. Journal of Infectious Diseases. 2007;196(12):1852–1859. doi: 10.1086/522867. [DOI] [PubMed] [Google Scholar]
- Lejuez CW, Read JP, Kahler CW, Richards JB, Ramsey SE, Stuart GL, Strong DR, Brown RA. Evaluation of a behavioral measure of risk taking: The Balloon Analogue Risk Task (BART). Journal of Experimental Psychology: Applied. 2002;8(2):75–84. doi: 10.1037//1076-898x.8.2.75. [DOI] [PubMed] [Google Scholar]
- Lejuez CW, Simmons BL, Aklin WM, Daughters SB, Dvir S. Risk-taking propensity and risky sexual behavior of individuals in residential substance use treatment. Addictive Behaviors. 2004;29:1643–1647. doi: 10.1016/j.addbeh.2004.02.035. [DOI] [PubMed] [Google Scholar]
- Moffitt TE, Caspi A. Childhood predictors differentiate life-course persistent and adolescence-limited antisocial pathways among males and females. Development and Psychopathology. 2001;13(02):355–375. doi: 10.1017/s0954579401002097. [DOI] [PubMed] [Google Scholar]
- Moffitt TE, Caspi A, Harrington H, Milne BJ. Males on the life-course-persistent and adolescence-limited antisocial pathways: Follow-up at age 26 years. Development and Psychopathology. 2002;14(01):179–207. doi: 10.1017/s0954579402001104. [DOI] [PubMed] [Google Scholar]
- Molina BSG, Pelham WE., Jr. Childhood predictors of adolescent substance use in a longitudinal study of children with ADHD. Journal of Abnormal Psychology. 2003;112(3):497–507. doi: 10.1037/0021-843x.112.3.497. doi: 10.1037/0021-843X.112.3.497. [DOI] [PubMed] [Google Scholar]
- Molina BSG, Bukstein OG, Lynch KG. Attention-deficit/hyperactivity disorder and conduct disorder symptomatology in adolescents with alcohol use disorder. Psychology of Addictive Behaviors. 2002;16(2):161–164. doi: 10.1037//0893-164x.16.2.161. [DOI] [PubMed] [Google Scholar]
- Morris RE, Baker CJ, Valentine M, Pennisi AJ. Variations in HIV risk behaviors of incarcerated juveniles during a four-year period: 1989–1992. Journal of Adolescent Health. 1998;23(1):39–48. doi: 10.1016/s1054-139x(97)00268-1. [DOI] [PubMed] [Google Scholar]
- O'Donnell L, O'Donnell CR, Stueve A. Early sexual initiation and subsequent sex-related risks among urban minority youth: the reach for health study. Family Planning Perspectives. 2001;33(6) [PubMed] [Google Scholar]
- Patton JH, Stanford MS, Barratt ES. Factor structure of the Barratt impulsiveness scale. Journal of Clinical Psychology. 1995;51(6):768–774. doi: 10.1002/1097-4679(199511)51:6<768::aid-jclp2270510607>3.0.co;2-1. [DOI] [PubMed] [Google Scholar]
- Poulin C, Graham L. The association between substance use, unplanned sexual intercourse and other sexual behaviours among adolescent students. Addiction. 2001;96(4):607–621. doi: 10.1046/j.1360-0443.2001.9646079.x. [DOI] [PubMed] [Google Scholar]
- Raine A, Moffitt TE, Caspi A, Loeber R, Stouthamer-Loeber M, Lynam D. Neurocognitive impairments in boys on the life-course persistent antisocial path. Journal of Abnormal Psychology. 2005;114(1):38. doi: 10.1037/0021-843X.114.1.38. [DOI] [PubMed] [Google Scholar]
- Ramrakha S, Bell ML, Paul C, Dickson N, Moffitt TE, Caspi A. Childhood behavior problems linked to sexual risk taking in young adulthood: a birth cohort study. Journal of the American Academy of Child & Adolescent Psychiatry. 2007;46(10):1272–1279. doi: 10.1097/chi.0b013e3180f6340e. [DOI] [PubMed] [Google Scholar]
- Rippeth JD, Heaton RK, Carey CL, Marcotte TD, Moore DJ, Gonzalez R, Grant I. Methamphetamine dependence increases risk of neuropsychological impairment in HIV infected persons. Journal of the International Neuropsychological Society. 2004;10(01):1–14. doi: 10.1017/S1355617704101021. [DOI] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration . Mental Health Services Administration Results from the 2012 National Survey on Drug Use and Health: Summary of National Findings. H-46. Substance Abuse and Mental Health Services Administration; Rockville, MD: 2013. (13-4795) [Google Scholar]
- Santelli JS, Brener ND, Lowry R, Bhatt A, Zabin LS. Multiple sexual partners among US adolescents and young adults. Family Planning Perspectives. 1998:271–275. [PubMed] [Google Scholar]
- Schuster RM, Crane NA, Mermelstein R, Gonzalez R. The influence of inhibitory control and episodic memory on the risky sexual behavior of young adult cannabis users. Journal of International Neuropsychology. 2012;18(5):827–833. doi: 10.1017/S1355617712000586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spinella M. The role of prefrontal systems in sexual behavior. International Journal of Neuroscience. 2007;117(3):369–385. doi: 10.1080/00207450600588980. [DOI] [PubMed] [Google Scholar]
- Staton M, Leukefeld C, Logan T, Zimmerman R, Lynam D, Milich R, Clayton R. Risky sex behavior and substance use among young adults. Health & Social Work. 1999;24(2):147–154. doi: 10.1093/hsw/24.2.147. [DOI] [PubMed] [Google Scholar]
- Steinberg L. Risk taking in adolescence: what changes, and why? Annuals of New York Academy of Sciences. 2004;1021:51–58. doi: 10.1196/annals.1308.005. doi: 10.1196/annals.1308.005. [DOI] [PubMed] [Google Scholar]
- Tapert SF, Aarons GA, Sedlar GR, Brown SA. Adolescent substance use and sexual risk-taking behavior. Journal of Adolescent Health. 2001;28(3):181–189. doi: 10.1016/s1054-139x(00)00169-5. [DOI] [PubMed] [Google Scholar]
- Timmermans M, Van Lier PAC, Koot HM. Which forms of child/adolescent externalizing problems account for late adolescent risky sexual behavior and substance use? The Journal of Child Psychology and Psychiatry. 2008;49(4):386–394. doi: 10.1111/j.1469-7610.2007.01842.x. [DOI] [PubMed] [Google Scholar]
- Toplak ME, Sorge GB, Benoit A, West RF, Stanovich KE. Decision-making and cognitive abilities: A review of associations between Iowa Gambling Task performance, executive functions, and intelligence. Clinical Psychology Review. 2010;30(5):562–581. doi: 10.1016/j.cpr.2010.04.002. [DOI] [PubMed] [Google Scholar]
- Tubman JG, Gil AG, Wagner EF, Artigues H. Patterns of sexual risk behaviors and psychiatric disorders in a community sample of young adults. Journal of Behavioral Medicine. 2003;26(5):473–500. doi: 10.1023/a:1025776102574. [DOI] [PubMed] [Google Scholar]
- Varghese B, Maher JE, Peterman TA, Branson BM, Steketee RW. Reducing the risk of sexual HIV transmission: quantifying the per-act risk for HIV on the basis of choice of partner, sex act, and condom use. Sexually Transmitted Diseases. 2002;29(1):38–43. doi: 10.1097/00007435-200201000-00007. [DOI] [PubMed] [Google Scholar]
- Ward MF, Wender PH, Reimherr FW. The Wender Utah Rating Scale: An Aid in the Retrospective. American Journal of Psychiatry. 1993;1(50):885. doi: 10.1176/ajp.150.6.885. [DOI] [PubMed] [Google Scholar]
- Weber FT, Elfenbein DS, Richards NL, Davis AB, Thomas J. Early sexual activity of delinquent adolescents. Journal of Adolescent Health Care. 1989;10(5):398–403. doi: 10.1016/0197-0070(89)90218-0. [DOI] [PubMed] [Google Scholar]
- Wechsler D. Wechsler Test of Adult Reading: WTAR. Psychological Corporation; 2001. [Google Scholar]
- Whitlow CT, Liguori A, Brooke Livengood L, Hart SL, Mussat-Whitlow BJ, Lamborn CM, Porrino LJ. Long-term heavy marijuana users make costly decisions on a gambling task. Drug and Alcohol Dependence. 2004;76(1):107–111. doi: 10.1016/j.drugalcdep.2004.04.009. [DOI] [PubMed] [Google Scholar]
- Woodward LJ, Fergusson DM. Early conduct problems and later risk of teenage pregnancy in girls. Development and Psychopathology. 1999;11(01):127–141. doi: 10.1017/s0954579499001984. [DOI] [PubMed] [Google Scholar]